
Nanostructured Platforms for the Sustained and Local Delivery
of Antibiotics in the Treatment of Osteomyelitis
Vuk Uskoković
Advanced Materials and Nanobiotechnology Laboratory, Richard and Loan Hill Department of
Bioengineering, College of Medicine, University of Illinois at Chicago, 851 South Morgan St, #205
Chicago, Illinois, 60607-7052
Vuk Uskoković: [email protected]
Abstract
This article provides a critical view of the current state of the development of nanoparticulate and
other solid-state carriers for the local delivery of antibiotics in the treatment of osteomyelitis.
Mentioned are the downsides of traditional means for treating bone infection, which involve
systemic administration of antibiotics and surgical debridement, along with the rather imperfect
local delivery options currently available in the clinic. Envisaged are more sophisticated carriers
for the local and sustained delivery of antimicrobials, including bioresorbable polymeric,
collagenous, liquid crystalline, and bioglass- and nanotube-based carriers, as well as those
composed of calcium phosphate, the mineral component of bone and teeth. A special emphasis is
placed on composite multifunctional antibiotic carriers of a nanoparticulate nature and on their
ability to induce osteogenesis of hard tissues demineralized due to disease. An ideal carrier of this
type would prevent the long-term, repetitive, and systemic administration of antibiotics and either
minimize or completely eliminate the need for surgical debridement of necrotic tissue. Potential
problems faced by even hypothetically “perfect” antibiotic delivery vehicles are mentioned too,
including (i) intracellular bacterial colonies involved in recurrent, chronic osteomyelitis; (ii) the
need for mechanical and release properties to be adjusted to the area of surgical placement; (iii)
different environments in which in vitro and in vivo testings are carried out; (iv) unpredictable
synergies between drug delivery system components; and (v) experimental sensitivity issues
entailing the increasing subtlety of the design of nanoplatforms for the controlled delivery of
therapeutics.
Keywords
calcium phosphate; composites; controlled drug delivery; nanoparticle; osteomyelitis
I. INTRODUCTION
Osteomyelitis, the infectious inflammation of bone and one of the oldest documented
diseases, the earliest descriptions of which date back to Hippocrates (fifth century BC),
1
is
an illness particularly prevalent among the elderly, diabetics, children, and indigenes of
©2015 Begell House, Inc.
HHS Public Access
Author manuscript
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Published in final edited form as:
Crit Rev Ther Drug Carrier Syst. 2015 ; 32(1): 1–59.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

Third World countries (Fig. 1a). Before the advent of antibiotics, the mortality rate because
of osteomyelitis was 25–45%. Although morbidity due to chronic bone infection has
drastically decreased from the pre-penicillin era, down to ~3% in the past 20 years,
2
it is still
high on the global scale, and treating the disease continues to be considerably challenging.
3
The incidence of osteomyelitis in the United States is 1–2%, but the disease is far more
prevalent in developing countries, as well as among particular patient populations:
approximately 1 in 5000 children, 1 in 1000 neonates, 1 in 250 patients with sickle cell
disease, 1 in 7 diabetics, and 1 in 3 patients with punctured foot.
4–7
Its comparatively low
prevalence can be explained by the fact that bone is an organ well protected from external
pathogens and is not readily prone to infection. The difficulty faced by invasive pathogens in
an attempt to colonize the bone is, however, directly proportional to the difficulty faced by
clinicians in ensuring the delivery of antibiotics to the site of infection and curing it. The
prevalence of chronic osteomyelitis among patients treated for at least one episode of acute
osteomyelitis is consequently high, in the range of 5–25%.
8
Strategies for improving the
therapeutic approach in the treatment of osteomyelitis have thus been explored for over a
century,
9
with a steadily increasing annual number of publications related to it—from 1 to
10 until 1944 to 100–300 from 1944 to 1974 to 713 in 2012 (US National Library of
Medicine), more than in any of the preceding years—going in step with the anticipated
increase in the number of cases of bone disease as the corollary of the aging population
worldwide (Fig. 1b). The number of hip and knee replacement procedures performed in the
United States has, for example, doubled in the past decade, whereas the number of the
reported cases of bone infection accompanying those procedures also has steadily increased
in proportion to the number of surgeries performed (Fig. 2). In spite of using aseptic
techniques and antibiotic prophylaxis, osteomyelitis is estimated to develop in 22–66% of
patients following orthopedic operations, and the corresponding mortality rate could be as
high as 2%.
10
This review describes (1) the pathologies that cause osteomyelitis; (2) the
traditional therapeutic approach to curing it; and (3) advanced therapeutic methods based on
the design of nanostructured platforms for the sustained and local delivery of antibiotics.
II. PATHOLOGIES AND THE DOWNSIDES OF THE TRADITIONAL CLINICAL
APPROACH
Osteomyelitis is mainly caused by pyogenic bacteria found in healthy oral flora, although
cases of infection caused by fungi are also common.
13–15
Bone infections caused by
Brucella suis,
16
Haemophilus influenzae,
17
Mycobacterium tuberculosis,
18
Mycobacterium
ulcerans,
19
and pox viruses,
20,21
as well as those whereby bone lesions are secondary to
Bacille Calmette-Guérin
22
or smallpox
23
vaccination, also have been reported in the
literature. Although many gram-negative and gram-positive bacteria were reported to have
caused osteomyelitis; the great majority of bone infections, however, is staphylococcal in
origin and mostly caused by a single bacterium: Staphylococcus aureus.
24,25
In addition to
S. aureus, S. epidermidis is another common cause of osteomyelitis; it is present in up to
90% of bone infections following intraoperative implantation of a foreign material. Because
most cases of osteomyelitis are caused by bacteria that reside on healthy skin and in healthy
oral flora, osteomyelitis is an illness often caused by a bizarrely small scratch or a bite where
Uskoković
Page 2
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

by body fluids become exposed to external pathogens, which then go on to induce septic
arthritis and/or osteomyelitis.
26
The onset of the infection induces an acute suppurative inflammation, and numerous factors
synergistically contribute to the necrosis of the hard tissues, demineralization of the bone,
and degradation of its collagen matrix: bacteria, pH change, local edema that accumulates
under pressure, vascular obstruction, and leukocyte collagenase.
27
As the infection
progresses locally, it extends to the adjacent osseous structures through the Haversian and
Volkmann canals, leading to an increased obstruction of vascular channels and necrosis of
more osteocytes in the lacunae. By the time the infection reaches the outer part of the cortex,
it has already caused an inversion of the periosteal blood flow and gained access to the
subperiosteal space, which results in a subperiosteal abscess and the formation of
involucrum, a layer of new bone grown from periosteum stripped from the original bone
under the pressure of pus. Figure 3 shows radiological images of cases of acute and chronic
osteomyelitis (the former came from a clinic and the latter from an animal model),
28
along
with involucrum formed around the area of necrotic infection and a periosteal reaction in the
proximal area of the bone, respectively.
Osteomyelitis is particularly prevalent in the facial skeleton because of its accessibility to a
variety of external pathogens and commensal microorganisms.
29
It also presents a major
complication following orthopedic and maxillofacial surgeries,
30
including even the most
routine dental extractions.
31
Although the resistance to infection of healthy bone is naturally
high, implants reduce it by a factor of 10
3
(i.e., the number of pathogens sufficient to cause
an infection is reduced from 10
8
to 10
5
). As a result, intraoperative introduction of bacteria
accounts for the largest number of osteomyelitis cases, with the hip being a particularly
common orthopedic site of infection. Timely treatment of osteomyelitis is required to
prevent its spread to new sites in the body and to avoid systemic osteonecrosis or unaesthetic
facial disfigurement in the case of maxillofacial infection. The typical treatment regimen for
bone infection consists of (1) intravenous administration of antibiotics lasting 2–6 weeks,
frequently followed by a 6-month course of oral antibiotics in the case of chronic infection;
and (2) surgical removal of bone that has undergone necrosis due to restriction of blood flow
by the formed abscesses.
32,33
Correspondingly, the major downsides of the conventional
therapeutic approach include (1) systemic administration of the therapeutic agent and its side
effects; (2) low concentration of the therapeutic agent around the site of infection,
potentially inducing resistance of the pathogen to the antibiotic therapy; and (3) irretrievable
bone loss that often requires the insertion of implants or prostheses as lasting bone
substitutes. Moreover, in the advanced stages of infection, when bone necrosis has become
significant, the blood supply to the infected area is inadequate and the lesion is largely
inaccessible to antimicrobial agents transported by the blood stream. All these downsides
provide strong incentives in favor of the development of appropriate carriers for the local
delivery of antibiotics in the treatment of osteomyelitis.
III. CLINICALLY AVAILABLE MATERIALS FOR LOCAL DELIVERY
Because of the apparent downsides of traditional therapy, including primarily the systemic
and repetitive administration of antibiotics whereby the therapeutic concentrations in the
Uskoković
Page 3
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

target area constantly fluctuate between toxic and ineffective, steps have been taken to
develop particulate carriers for the local and sustained delivery of antibiotics following their
implantation directly at the zone of infection. Ever since the pioneering research in this field
carried out in Europe in the 1970s,
34,35
poly(methyl methacrylate) (PMMA) beads, first
clinically applied in 1972, have been the gold standard for the local delivery of antibiotics to
bone cavities. Currently, there is no clinical alternative to PMMA as a local delivery carrier
for osteomyelitis since they are the only preloaded option approved by the US Food and
Drug Administration (FDA).
36
PMMA beads loaded with hydrophilic antibiotics, including gentamicin, ceftriaxone,
tobramycin, and vancomycin, have been used with experimental and clinical success in the
past.
37–41
Despite this, numerous limitations are associated with the use of PMMA beads.
First, they are not biodegradable and require a secondary surgical procedure for removal
after the antibiotic is released through their porous polymeric structure. Second, PMMA
beads and spacers exhibit burst release
42
that depletes the drug from the carrier and is
followed by a rather insubstantial release period that may be insufficient to maintain a
therapeutic concentration for the desired 3–4 weeks and may even promote antibiotic
resistance.
43
Although release kinetics could be extended by increasing the size of the beads
and increasing the polymerization time, burst release has seemed unavoidable so far.
44
Because the release is conditioned by the diffusion of the drug through the porous polymeric
network and microscopic cracks in the cement—and not by the degradation of the polymer
the elution profiles show broad variations depending on the nature of the antibiotic,
exhibiting intense burst release and a prompt decrease in concentration below the
therapeutic level in some cases.
45,46
Relatively low toxicity results from the absorption of methyl methacrylate monomers and
the associated carboxylesterase-mediated conversion of methyl methacrylate to methacrylic
acid,
47,48
whereas biofilm frequently forms on antibiotic-laden PMMA beads, hindering the
antimicrobial action.
49,50
Although products preloaded with gentamicin are available on the
market (Septopal), most clinically applied PMMA beads are loaded with the antibiotic just
before surgical insertion
51
(Fig. 4), which can lead to inconsistent release profiles.
52
This
nullifies the producer’s liability for the product and makes it therapeutically applicable only
with the patient’s consent.
53
Finally, a comprehensive clinical study has yet to prove that
PMMA beads are more effective than the systemic antibiotic delivery approach in treating
orthopedic infections.
54
No significant difference in the treatment success rate was typically
observed when debridement was followed by the implantation of antibiotic-containing
PMMA beads for local release or the prescription of systemic antibiotics.
55
The lower cost
of the therapy is often considered the only advantage of local delivery using PMMA
beads.
56
Consequently, a large population of clinicians is skeptical about the benefits of
local delivery in the management of osteomyelitis compared with the traditional approach
and resorts to the latter in their practice.
With no nonbiodegradable bone substitutes for load-bearing applications in sight for either
the biomedical device market or anywhere in clinical testing, for many decades now the
greatest potential among the bone engineers has been logically ascribed to bioresorbable
implants. However, the only currently clinically available bioresorbable alternative to
Uskoković
Page 4
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

PMMA beads, predominantly used outside the United States, is calcium sulfate cements.
57
Unlike PMMA, whose monomeric absorption has previously caused intraoperative
cardiopulmonary complications during arthroplasty,
58
calcium sulfates are nontoxic and
inexpensive and have been successfully used as a drug carrier in the treatment of
osteomyelitis.
59,60
In addition to being used since the late 19th century as a bone filler in
their hemihydrate form, also known as plaster of Paris,
61
calcium sulfates have been applied
in reparative dentistry for maxillary sinus floor augmentation
62
and for the repair of
periodontal defects
63
and root perforations.
64
In addition to their exceptional softness and
poor handling features, the main downside is that they are resorbed rapidly, in a matter of
weeks—faster than the bone ingrowth rate—which can lead to mechanical implant failure.
65
An ideal bioresorbable implant provides a mechanical support that is gradually transferred to
the newly formed bone, a requirement that calcium sulfates do not satisfy. They can also
cause severe drainage at the wound site after the surgical implantation,
66
as well as the
formation of a fibrous gap in the area where the slowly ingrowing bone replaces the rapidly
resorbing cement,
67
the same effect that is expected to result from the use of aragonite
68
or
calcium phosphate phases, such as tricalcium
69
or dicalcium
70,71
phosphates, as bone fillers;
these are more soluble than hydroxyapatite, the calcium phosphate constituent of bone. Also,
as a result of their relatively fast degradation in the body, the concentration of the antibiotic
at the target site and its mean blood serum concentration over the first month following
implantation are lower when compared with hydroxyapatite.
72
For this reason, and in view
of the fact that calcium sulfates have not led to therapeutic outcomes any better than those of
PMMA implants,
73
their use as an ideal bioresorbable delivery vehicle for antibiotics and a
void filler in bony defects has been questioned.
74
IV. ADVANCED DRUG DELIVERY PLATFORMS IN THE RESEARCH STAGE
As noted earlier, two main disadvantages of the traditional treatment of osteomyelitis
include (1) systemic distribution of the therapeutic agent and (2) the need for surgical
removal of necrotic bone. Options for sustained antibiotic release that can ensure high local
concentrations and low serum concentrations of the drug
75
already exist, and progress in
terms of promoting the osteogenic activity of the carrier is expected in the future. Whereas
local and sustained release of the drug could overcome the need for prolonged oral and/or
intravenous antibiotic therapies, the induction of osteogenesis by the carrier itself or the
growth factors released from it could eliminate or at least minimize the surgical removal of
affected bone, along with the frequent skeletal deformations and unaesthetic physical
disfigurements it entails. Patients with diabetic neuropathy are prone to developing
osteomyelitis of the forefoot, which often leads to minor amputation
76
; with the
development of osteogenic carriers that could revitalize the diseased bone, however, such
clinical cases could be coped with in a manner less traumatic for the patient. For example, in
parallel with the drug release process, the particles may decompose, dissipating their
osteogenic contents and thus fostering the bone healing process and natural restoration of the
portion of bone damaged by the pathogen. The therapeutic approach to treating
osteomyelitis would clearly yield a whole new dimension by using one such osteogenic drug
delivery platform. After all, with an ideal therapeutic agent serving a dual purpose of (1)
eliminating the source of illness and (2) revitalizing the organism, the conception of drug
Uskoković
Page 5
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

delivery carriers that exhibit simultaneous bactericidal and osteogenic performance is
natural.
A. Calcium Phosphates
Calcium phosphates occupy a special place among the biodegradable drug carriers of
antibiotics in bone repair. They have been traditionally considered a convenient choice for
the synthetic substitute of hard tissues because of their excellent biocompatibility,
osteoconductivity, lack of cytotoxicity, nonimmunogenicity, and sufficient loading
capacities, thanks to which hydroxyapatite, their least soluble phase, has been used as a
chromatographic adsorbent of proteins,
77–79
nucleic acids,
80–82
and microorganisms.
83
Excellent adsorption properties of hydroxyapatite are the result of its positively charged
surface Ca
2+
ions engaging in an anion-exchange interaction with deprotonated carboxyl
groups of proteins and the negatively charged PO
4
3−
groups engaging in a cation-exchange
interaction with protonated amino groups of proteins.
84
Moreover, hydroxyapatite possesses
different net charges on the a and c planes of its hexagonal crystal lattice—positive and
negative, respectively,
85
which renders it effective in the crystallographically selective
binding of multiple molecular entities. Other variations of hydroxyapatite, such as
carbonated apatite
86
and biphasic calcium phosphate,
87
possessed an even greater protein
adsorption capacity, given an identical particle size and specific surface area, which was
hypothesized to be due to their greater solubility, which increases the ionic strength in the
medium and the surface exposition of the polar residues of proteins, thus increasing the
binding efficacy.
88
Hydroxyapatite also has been used as an amphiphilic stabilizer in
Pickering emulsions, suggesting its ability to interact with both hydrophilic and hydrophobic
compounds.
89
Unlike PMMA, calcium phosphates are fully bioresorbable, and the rate of their degradation
could be tentatively tuned by controlling the phase composition of the compound.
90
Namely,
as can be seen in Table 1, calcium phosphates can adopt a variety of stoichiometries,
covering a range of solubility product values, from 0.07 for anhydrous and monohydrous
monocalcium phosphates to 10
−7
for monetite and brushite to 10
−25
for α-tricalcium
phosphate to 10
−117
for hydroxyapatite.
91
Of course, because more ionic species exist in the
stoichiometric formulas of the less soluble phases, the difference in solubility is of a lesser
magnitude than that in the solubility product, amounting to approximately 6 · 10
4
, 1.6 · 10
2
,
and 8.3 times higher solubility for monocalcium phosphate, monetite, and α-tricalcium
phosphate, respectively, compared with hydroxyapatite (0.3 mg/dm
3
) in water at 37°C and
at a physiological pH.
Particle size presents an important consideration in the design of most optimal degradation
and release profiles, and nanosized calcium phosphates have proved to be far more
advantageous than the microsized ones,
92
a natural consequence of the fact that bone itself
contains apatite particles with nanosized dimensions
93
(20 × 10 × 2 nm, on average
94
).
Furthermore, porosity that is controllable via sintering at elevated temperatures could be
used to vary the degradation rate in vivo within a wide window of values; again, nanosized
and fully dispersed hydroxyapatite is highly bioresorbable and the denser formulations are
resorbable to a significantly lesser degree,
95
leading to hypotheses that nonporous, sintered
Uskoković
Page 6
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

hydroxyapatite blocks should be stable in biological milieus for centuries.
96
In this case the
drug release rate tends to be directly proportional to the resorption rate, that is, significantly
higher for the more porous calcium phosphate microstructures.
97
Stoichiometry of single-
phase compositions, implant geometry, ionic substitutions, crystallinity, and macro- and
microporosity are other factors known to greatly affect the degradation rate of calcium
phosphates in vivo.
98–100
When self-setting calcium phosphates pastes are used, the powder-
to-liquid ratio, initial viscosity, pH, and the presence of additives, such as crystallization
seeds, inhibitors, or dispersants, are additional factors that influence the hardening
properties, the degradation kinetics, and the rates of resorption and new bone ingrowth,
101
which usually range anywhere between 3 months and 3 years.
102
Calcium phosphates are also a component of the mineral phase of hard tissues, which makes
them a natural candidate for bone-filling drug carriers. With bone acting as a natural
reservoir for calcium and phosphate ions,
109
any excessive amounts thereof could be
regulated in favor of new bone growth. Calcium and phosphate ions released upon the
degradation of these compounds can also stimulate osteoblastic differentiation
110,111
and
proliferation
112
and be used as ionic ingredients for the formation of new bone. Another
advantage of calcium phosphates is that they could be sterilized by a variety of techniques,
including γ-irradiation, gas plasma, supercritical carbon dioxide, or even steam autoclaving
(in the case of hydroxyapatite), without causing adverse effects to their structure and
properties. By contrast, in general there is currently no established sterilization procedure for
polymers that does not modify their structure to some degree, due to (1) physical
deformations and chemical changes—scission and cross-linking that occur upon
autoclaving,
113
alongside practically inevitable degradation of an encapsulated drug
114
; (2)
surface chemistry modifications that occur upon the application of ethylene oxide, hydrogen
peroxide, or ozone
115
; (3) bulk structural changes and a decrease in the molecular weight
that occur during γ-irradiation,
116
while a difficult regulatory path is posed before novel or
nontraditional sterilization methods.
Calcium phosphates are also relatively easy to prepare in a variety of morphological
forms,
117
although not at a particle size below 20 nm, as is the case with metals. Different
calcium phosphate particle morphologies possess different bioactivities,
118,119
which allows
for the optimization of their biological response by means of controlling morphological and
specific crystal face exposition. Calcium phosphates are also naturally precipitated in a
nanosized form, and the use of nanoparticulate calcium phosphates could be considered as a
win–win solution in the quest for simultaneous bactericidal and osteogenic properties.
Namely, the drug adsorption efficiency is directly proportional to the specific surface area of
the adsorbent and inversely proportional to the particle size.
120
The large surface area of
nanosized calcium phosphates thus increases their drug-loading capacity and makes them a
more effective bactericidal agent.
121
At the same time, nanosized calcium phosphates
possess higher bioactivity than their microsized counterparts,
122,123
an insight that is natural
in view of the nanosized dimensions (30 × 20 × 2 nm)
124
of mineral particles in bone. Last
but not least, calcium phosphates are one of the safest nanomaterials evaluated for toxicity
so far.
125
Figure 5a displays round hydroxyapatite nanoparticles obtained by precipitation
from alkaline aqueous solutions and highlights their ability to capture large amounts of drug
Uskoković
Page 7
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

molecules in the pores between the particles upon desiccation at low pressure.
Mechanistically similar intraporous loading of hydroxyapatite with a drug was reported
earlier for isepamacin sulfate, an aminoglycoside antibiotic.
126
The same effect of extended
release could be achieved by compacting the antibiotic-loaded calcium phosphate powders
under pressure.
127
PerOssal, a commercial mixture comprising 51.5% nanocrystalline
hydroxyapatite and 48.5% calcium sulfate, for example, relies on such compaction of
nanoparticles to ensure sustained release of antibiotics.
128
1. Concerns Pertaining to the Use of Calcium Phosphates—The application of
calcium phosphate particles as drug delivery carriers naturally has its downsides, and the
main one comes from their difficult surface functionalization. This is, in part, the effect of
their ionic nature, which dictates that the surface layers undergo rapid reorganization via
dissolution/reprecipitation phenomena in ionic media. As evidence of this effect, ζ potential
of hydroxyapatite particles changed with the immersion time, indicating an exchange of ions
across the interface layer and its restructuring following local changes in the solvent
medium.
129,130
Despite the presence of calcium, phosphate, and hydroxyl ionic groups on
the particle surface, which, in theory, would allow the binding of an array of functional
groups, the intense ionic exchange between the particle surface and its ionic milieu renders
this approach inoperative for dispersed particles. Compared with calcium phosphate
nanoparticles, silanol groups on the surface of silica nanoparticles offer greater stability and
more facile functionalization with organic molecules, having the same role as monolayers of
thiol groups chemisorbed on the surface of silver, copper, or gold
132
and carboxylic or
phosphonic acid moieties on the surface of metal oxides or quantum dots. Their downside,
however, is an uncertain fate in the body and an array of inflammatory and oxidative
stresses possibly induced in it, ranging from mitochondrial dysfunction to genotoxicity to
pulmonary congestion to hepatocyte necrosis.
133–135
Unlike polymeric materials (e.g., hyaluronic acid), whose viscosity could be controlled to a
greater degree by means of chemical or photochemical cross-linking, thixotropic calcium
phosphate cements exhibit a far narrower window of setting rates, which significantly limits
the flexibility of their surgical handling. Variations in the concentration of plasticizing
additives, liquid-to-solid ratio, particle size and sphericity, and ionic strength of the liquid
phase have all been studied in a search for the optimal conditions for the fabrication of
injectable but cohesive calcium phosphate pastes and putties.
136
On the other side of the
spectrum, occupied by solid and strictly implantable materials, nonsintered calcium
phosphates in particular—which are strong but fragile and most interesting for drug delivery
applications are hardly formable and also are difficult to surgically attach to bone with
screws and intramedullary rods, for which reason they are often combined with a tougher,
more ductile organic phase to mimic the mechanical properties of bone itself.
137
Also, as a
consequence of uncontrolled ripening in the nucleation and crystal growth stages,
monodisperse calcium phosphates are difficult to prepare in a broad array of sizes, which
poses obstacles to systematic studies of the effect of calcium phosphate particle size on
bioactivity.
138
Last but not least, the most important disadvantage of calcium phosphates is that they have
little or no ability to be loaded with organic molecules via intercalation, which limits the
Uskoković
Page 8
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

loading mechanism to physisorption only and makes prolonged release difficult to achieve.
Namely, burst release typically results when the drug is adsorbed on the surface of the
carrier, and while, on one hand, this effect is favorable in terms of ensuring that the minimal
inhibitory concentration for the given pathogen is exceeded, it can also deplete the carrier
from the antibiotic and make its further release therapeutically ineffective. Still, a
tremendous difference between microsized and nanosized calcium phosphate particles was
found: Whereas the concentration of vancomycin released from the former was below the
detection limit 10 days after the implantation, nanoparticles of the same composition were
able to sustain the therapeutic level of release for up to 6 weeks.
139
Extended release from
porous calcium phosphate cements and its therapeutic effects in vivo were confirmed on
numerous other occasions.
140–143
Finally, because of relatively low ζ potentials (<15 mV on
the absolute scale), calcium phosphates form sols of low stability; simple and rapid
precipitation procedures for their formation in the low crystalline and nanoparticulate form,
on the other hand, enable them to be prepared before their clinical application.
2. Calcium Phosphate as an Intrinsically Osteoinductive Material—Calcium
phosphates have been generally considered as osteoconductive materials in the sense that
they support bone growth on them, although their ability to upregulate the expression of
osteogenic markers and boost osteoblastic differentiation, making them osteoinductive, too,
has been reported on numerous occasions.
144–146
The addition of growth factors, such as
bone morphogenetic proteins (BMPs), also has made calcium phosphates
osteoinductive,
147,148
although the same osteoinductive effect achieved by BMP-2 on
human mesenchymal stem cells was accomplished by nanosized hydroxyapatite particles.
149
In a corresponding study composites for the delivery of recombinant human BMP-2 (rH-
BMP-2) to mice and rabbits, comprising poly(D, L-lactic acid), p-dioxanone, polyethylene
glycol (PEG), and β-tricalcium phosphate needed less of the BMP than the same composites
that excluded hydroxyapatite from their composition to induce the same osteopromoting
effect and new bone formation.
150,151
Another study demonstrated that the expression of
BMP-2 in human periodontal ligament cells increased upon stimulation with nanosized
hydroxyapatite.
152
Optimization of substrate topography was able to yield the same
differentiation–induction effect as the chemical differentiation agents in the transformation
of mesenchymal stem cells to osteoblastic ones,
153
and a similar approach that could be
applied to ensure induced osteogenic response of bone cells without the use of expensive
growth factors would be great news, especially since bone infection is an illness known to
be particularly prevalent among patients in the Third World countries, for whom
affordability presents a vital feature of a marketed drug. This does not even consider that the
use of rHBMP-2 in bone augmentation procedures has induced ectopic bone formation,
osteolysis, pseudoarthrosis, inflammatory reactions in soft tissues, increased risk of
malignancies, and other adverse effects,
154,155
raising significant concerns over its safety in
the recent years.
156
The combination of rHBMP-2 with calcium phosphates has, however,
mitigated these adversities associated with the direct infusion of the given growth factor or
its delivery using organic carriers.
157
The naturally bactericidal citrate ion, accounting for
5.5 wt% of the organic content of bone, where it coats hydroxyapatite crystals at 0.5
molecules/nm
2
and stabilizes them in the collagen matrix,
158
increases in concentration in
parallel with the differentiation of mesenchymal stem cells into osteoblasts
159
and has been
Uskoković
Page 9
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

proposed as an alternative to BMPs in view of the ability of composites comprising
hydroxyapatite, in combination with polymers based on citric acid, to facilely regenerate
necrotic bone.
160
To render calcium phosphates as a base for an authentically osteogenic material by including
cell components capable of bone production, such as osteoprogenitor cells or differentiated
osteoblasts, however, the formation of porous scaffolds based on calcium phosphates is
needed, comprising a difficult but not impossible task.
161–164
For example, with the addition
of only 3 vol% gelatin, electrospinning, the method traditionally used to obtain polymeric
scaffolds, could be used to prepare calcium phosphate scaffolds as well.
165
Biomimetic
methods based on the usage of porous biological hard tissues as casting molds for the
synthesis of structurally similar inorganic scaffolds also have recently gained popularity.
166
In addition, a combination of self-setting pastes and porogens, such as mannitol
crystals,
167,168
pectin,
169
hydrogen peroxide,
170
inorganic crystals,
171
surfactants,
172,173
poly-(D,L-lactide-co-glycolide) (PLGA),
174,175
oils,
176
or other hydrophobic compounds,
was also used to create macroporous calcium phosphate formulations. Calcium phosphate
nanoparticles were successfully incorporated in polymeric,
177
collagen,
178
or carbon
nanotube
179
scaffolds with the purpose of promoting greater adsorption of adhesive serum
proteins and inducing bone growth. Simple admixing of microsized polymeric spheres into
calcium phosphate cements is another method used to produce macroporosity sufficient to
provide a proliferation milieu for host cells after the degradation of the polymeric phase.
180
3. Prospect of Ion-Substituted Calcium Phosphates—By affecting their lattice
parameters, crystallinity, and the solubility product, ionic substitutions in calcium
phosphates seem to have a large effect on a range of their physicochemical
properties.
181–183
While geological apatite can accommodate half of all the elements of the
periodic table in its crystal lattice,
184
biological apatite contains about a dozen different ions
as impurities, which has provided a rationale for the expected improvement in the biological
response to ion-substituted calcium phosphates.
185
Substitution of Ca
2+
with K
+
, Na
+
, or
other alkali ions can, for example, increase the solubility of hydroxyapatite beyond that of
tricalcium phosphate.
186
Like Na
+
, Mg
2+
is an ion that inhibits the nucleation of
apatite.
187,188
However, it is also the ion for which bone is the biggest reservoir in the body
and whose deficiency logically reduces bone growth,
189
explaining numerous attempts to
augment existing calcium phosphate formulations by doping them with Mg
2+
.
190,191
Together with Mg
2+
, Zn
2+
has been found in subnormal concentrations in osteoporotic
patients, suggesting the vital role of these two cations in proper bone remodeling.
192,193
Because of the essential role of Zn
2+
in the production of more than one bone growth
protein, including the zinc finger containing transcription factor Osterix,
194
the deficiency of
this micronutrient was proven to have detrimental repercussions on bone development, as
well,
195
which is another argument in favor of its incorporation into calcium phosphates
designed for bone substitutes. Zinc-substituted hydroxyapatite containing 1.6 wt% of Zn
2+
possessed a more pronounced antibacterial effect against S. aureus compared with pure
hydroxyapatite.
196
Selenium is another element with strong antimicrobial properties that has
been introduced to carbonated hydroxyapatite via CO
3
2−
→ SeO
3
2−
substitution, with the
Uskoković
Page 10
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

resulting material being able to inhibit the formation of Pseudomonas aeruginosa and S.
aureus biofilm on its surface.
197
Silicon (Si) and strontium (Sr) are present in newly formed bone in the amounts of 0.5
198
and 0.03 wt%, respectively, and a more viable biological response was detected upon the
implantation of Si-doped and Sr-doped hydroxyapatite compared with pure
hydroxyapatite.
199–201
The most probable reason for this lies in the osteopromotive
properties of Si and Sr ions per se; Si has been demonstrated to increase bone mass density
and angiogenesis during new bone growth,
202
whereas Sr upregulates the expression of the
osteoblastic protein osteoprotegerin, which inhibits the production of RANKL and hinders
the differentiation and activation of osteoclasts.
203
Incorporation of either of these two ions
in the crystal lattice of hydroxyapatite increased the degradation of the compound in
vitro.
204,205
Vanadium is another element critical for healthy bone development because of
its ability to stimulate mineralization of collagen and proliferation of osteoblasts,
206
but the
bioactivity of vanadium-doped calcium phosphates
207
has yet to be assessed.
Calcium phosphates are able to sequester heavy ions from the environment, such as Pb
2+
and As
5+
, which is why they have been used as adsorbents in water purification.
208
Calcium
phosphate particles could thus be easily doped with Eu
3+
, Tb
3+
, Gd
3+
, La
3+
, or other
lanthanides and be made luminescent and used for imaging applications.
209,210
Hydroxyapatite labeled with
99
Tm,
125
I,
90
Yt,
153
Sm, or
3
H radionuclides could also be
considered for simultaneous bone substitution and imaging applications.
211–213
Doping
hydroxyapatite with alkaline earth metals and magnetic elements, such as cobalt
214
or
iron,
215–217
yielded other impure forms of calcium phosphate that have been intensively
researched for their unique bioactive properties.
218–220
Superparamagnetic hydroxyapatite
obtained by doping with approximately 10 wt% Fe
2+
/Fe
3+
was hailed as a far less toxic
alternative to magnetite when used as a heating material for hyperthermia-based bone cancer
therapies.
221
Finally, carbonated hydroxyapatite, structurally similar to its biomineralized
form, has been frequently demonstrated to be superior in terms of its bioactivity compared
with its stoichiometric, noncarbonated counterpart.
222,223
Explored alternatives to calcium phosphates and the two aforementioned materials in actual
clinical use, PMMA and calcium sulfate, include mainly various polymeric materials,
bioactive glasses, liquid crystals, collagen, and titanium nanotubes; these are discussed in
the sections that follow.
B. Synthetic Biodegradable Polymers
Synthetic biodegradable polymers proposed as potential antibiotic carriers in the site-
specific treatment of osteomyelitis are predominantly poly(α-hydroxy esters).
224–226
Among
them, poly(L-lactic acid) (PLLA), poly(glycolic acid) (PGA), PLGA,
227
and poly(ε-
caprolactone)
228
(PCL) have been studied most. All of these compositions have a proven
history of encapsulating arrays of both hydrophilic and hydrophobic compounds, including
antibiotics,
229
and enabling their sustained, first-order release over prolonged periods of
time.
230
While being formable in situ and capable of fitting practically any shape of a bone
defect to be filled, they also allow for fine-tuning of their mechanical and degradation
properties via control over their chemical structure, including parameters such as molecular
Uskoković
Page 11
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

weight, crystallinity, cross-linking ratio, and end-group identity. For example, the
decomposition kinetics of PLGA could be easily controlled by varying the lactide-to-
glycolide ratio and made to match the rate of new bone formation; namely, while PLLA has
a relatively lengthy degradation time scale, ranging from 3 months to over a year, depending
on the molecular weight, crystallinity, and other physicochemical factors, a gradual increase
in PGA content shortens this degradation to a matter of weeks for PLGA 50:50 as a result of
the decreased crystallinity and higher hydrolysis rate of PGA, after which the crystallinity
and resistance to degradation increase again at higher PGA contents, producing the
characteristic U-shaped curve (Fig. 6a).
231,232
An example of how sensitive the kinetics of
degradation and drug release could be to cross-linking ratio is shown in Fig. 6b; whereas 0.5
% of cross-linking in an acrylic hydrogel completes release in less than 5 hours, 1% of
cross-linking promotes sustained release over a period of 8 days.
233
Other biodegradable
synthetic polymers developed and tested as potential carriers of antibiotics in the treatment
of osteomyelitis include poly(trimethylene carbonate)
234,235
; polyamide fibers
236
;
polyhydroxyalkanoates, e.g., poly(3-hydroxybutyrate-co-3-hydroxyvalerate)
237
; and
polyanhydrides, e.g., poly(sebacic anhydride)
238
; poly(sebacic-co-ricinoleic-ester-
anhydride)
239
; or Septacin,
240
a copolymer of dimeric erucic acid and sebacic acid.
Polymeric composites are also the subjects of intense research. For example, a layer-by-
layer technique was used to grow multilayered polyelectrolyte films incorporating
gentamicin and comprising a cationic poly(β-amino ester) and anionic poly(acrylic acid) on
top of nondegradable poly(ethyleneimine) and poly(sodium 4-styrenesulfonate). Despite the
fact that more than two-thirds of the drug content were released in the first 3 days, the
implants were successful in treating S. aureus infection in a rabbit bone model.
241
1. Concerns Pertaining to the Use of Aliphatic Polyesters—Although poly(α-
hydroxy esters) have been successfully used in bone tissue engineering since the early
1990s,
242–244
there exists a concern that their acidic degradation products may favor
bacterial growth and promote hard-tissue resorption and bone mass loss,
245,246
effects
experimentally evidenced in the past. In spite of the supposed safe inclusion of the
byproducts of the degradation of PLLA-based polymers in the metabolic cycles of the host
organism (e.g., lactic acid is secreted by osteoclasts to resorb bone and is also one of the
compounds in the Krebs cycle), chronic inflammation has often resulted as a response to
their implantation in bone tissue engineering.
247–249
Another concern is that this
acidification effect may render rather ineffective antibiotics whose antimicrobial
effectiveness exists within only a narrow window of pH values. A decrease in pH from 7.4
to 5.5, for example, has led to a 16-fold increase in the minimum inhibitory concentration of
clindamycin with respect to S. aureus.
250
Poly(α-hydroxy esters) also lack the mechanical
properties required for load-bearing applications; PLGA, combining the adsorptive stability
of PLA with the mechanical strength of PGA, is the most favored and thus the most
researched option with respect to this intrinsic drawback.
C. Gels and Bioderived Polymers
Aqueous monoolein gels are an example of a liquid crystal system that was used to deliver
gentamicin sulfate for 3 weeks without the burst effect.
252
A mannosylated poly-
phosphoester gel with the capability of targeting macrophages and releasing the antibiotic
Uskoković
Page 12
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

payload in a site-activated manner, that is, only after being degraded by the bacterial
enzymes, was developed.
253
Use of the osteointegrating effects of calcium phosphates was
attempted by incorporating them into cubic liquid crystals of gentamicin–mono-olein–water
formulations.
254
Various combinations of calcium phosphates with gelatins, that is, mixtures
of peptides and proteins resulting from partial degradation of collagen, also were
investigated.
255,256
Among other bioderived polymers, some have been used to encapsulate
antibiotics, such as albumin
257,258
or dextran,
259
but have not been reported in bone-related
experimental trials, except in combination with more mechanically stable, inorganic phases.
Albumin coatings around allografts, for example, improved cell adhesion and
proliferation
260
and enhanced bone healing,
261
whereas the use of dextran as a porogen in
PMMA beads boosted the release of vancomycin, daptomycin, and amika-cin.
262
Conversely, silk fibroin coating around PCL microspheres managed to reduce the initial
burst release of vancomycin and extend the timeframe of its release.
263
Silk–alginate
copolymers are particularly interesting because of their tunable stiffness as the function of
the silk-to-alginate ratio and the concentration of the crosslinker,
264
but they have not been
used yet for the controlled delivery of antibiotics. Other natural polysaccharides, such as
chitosan,
265–267
pectin,
268
amylose,
269
alginate,
270
and hyaluronic acid,
271
have been both
used for the controlled release of antibiotics in vitro and tested as a component of
antimicrobial bone grafts in vivo. Pectin microspheres, alone and in combination with
chitosan, were used to encapsulate ciprofloxacin and were more effective in treating
osteomyelitis than intramuscularly administered antibiotic in a rat model.
272
A cross-linked
amylose starch matrix loaded with ciprofloxacin prevented and eradicated infection more
effectively than oral ciprofloxacin treatments in dogs with an infected femur.
273
Vancomycin encapsulated within alginate beads and distributed in a fibrin gel scaffold was
used to treat infected tibiae in rabbits.
274
Still, the most researched among bioderived
polymers as a potential carrier of antibiotics in the treatment and prevention of orthopedic
infection is collagen.
D. Collagen Sponges
Outside the United States in the 1980s, collagen sponges, also known as fleeces, began to be
used as the major alternative to PMMA beads for the local delivery of antibiotics. Their
application has been justified by a moderate number of clinical and in vivo studies.
275
For
example, compared with PMMA beads, sponge-like collagen carriers of gentamicin were 7
times more effective in reducing the bacterial colony count in the treatment of osteomyelitis
caused by S. aureus in the tibiae of rats.
276
Also, the placement of gentamicin-eluting
collagen fleece around the fixation plate during the surgical treatment of open bone fracture
prevented surgical site infection from occurring and promoted bone union in a large
population of patients.
277
In fact, rather than as a bone filler, collagen has been mostly used
as a material for postsurgical prophylaxis in the treatment of infectious disease.
1. Concerns Pertaining to the Use of Collagen—In spite of (1) the viable tensile
strength of collagen, (2) its ability to foster cellular attachment, and (3) the fact that collagen
sponges have been successfully used in the past,
278
the choice of antibiotics in their
clinically applicable versions has been limited to gentamicin only, alongside other
disadvantages that collagen intrinsically possesses. The main problem associated with the
Uskoković
Page 13
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

application of collagen and its derivatives as bone fillers comes from the intrinsic
immunogenicity of the collagen molecule,
279
namely, most of it is xenogenic in origin
because it is difficult to obtain directly from a patient, and recombinant technologies and the
methods to extract the immunogenic, telopeptide portion of collagen molecules are not only
of limited availability but also lead to reduced bioactivity of the protein.
280
Although
collagen has been successfully applied topically, for example, in biodegradable sutures and
as a prophylactic wound dressing carrier of antibiotics,
281–283
its mere subcutaneous
epithelialization may lead to undesired immunogenic or antigenic responses.
284,285
While it
can lead to antigenic and inflammatory responses, collagen is also typified by comparatively
uncontrolled degradation and drug release rates in the body.
286,287
For this reason, a
combination of collagen sponges with other polymers has been used to render more
sustained drug release profiles. One such composite material enriched with chitosan
microspheres and delivering recombinant human BMP-2 considerably outperformed a pure
collagen sponge loaded with the same growth factor in terms of new bone growth
enhancement, bone/implant integration, and the duration of drug release.
288
E. Silicon-Based Materials
Porous bioactive glass scaffolds loaded with ceftriaxone demonstrated a higher local
concentration of the antibiotic 6 weeks after the implantation compared with a parenteral
treatment composed of two injections per day.
289
Silicate-to-borate replacement in bioactive
glasses produced materials that also were used for the controlled delivery of vancomycin or
teicoplanin and repair of infected bone in rabbits.
290,291
Partial substitution of PO
4
3−
groups
of hydroxyapatite with SiO
4
4−
species resulted in a calcium phosphate–based glass ceramic
able to release vancomycin in a sustained manner over 2 weeks after cross-linking with
chitosan.
292
The addition of Ag
+
ions to phosphate-based glasses led to their sustained
release and bactericidal effect against S. aureus biofilms.
293
Further research will, however,
be necessary to show whether such antibiotic-free methods are capable of acting against
severe bone infections. As far as silica-containing materials are concerned, xerogels
obtainable from a solgel process were used to encapsulate and ensure the prolonged release
of vancomycin, with the water-to-alkoxysilane molar ratio being discerned as a parameter
for the control of release kinetics.
294
Zeolites, microporous aluminosilicates with
pronounced (1) antibacterial,
295
(2) adsorptive,
296
and (3) bone-protective dietary
297
properties, inhibited osteoclast-mediated bone resorption in vitro,
298
but their application as
a component of bone fillers in combination with calcium phosphates or other
osteoconductive phases is still a largely unexplored area. Metal-organic frameworks,
mesoporous materials structurally related to zeolites,
299
have been proposed as potentially
efficient drug delivery carriers,
300
including in applications that pertain to bone
regeneration,
301
which, however, they have yet to be tested for. Their main weakness is
rapid degradability in aqueous media, and structural variants with increased stability in
water are being intensively sought.
302
F. Metals
The widespread rise in the resistance of common pathogens to organic antibiotics has led to
a greater degree of consideration of the use of metals to prevent or treat infection,
303
with
many of them, such as silver-impregnated fabrics used as prophylactic dressings during
Uskoković
Page 14
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

wound healing,
304
regularly applied in the clinic. Because of its antimicrobial properties,
305
the first metal proposed for use in the treatment of osteomyelitis was silver; be it alone or in
the form of nylon wire composites, clinical testing resulted in a 65% success rate and no
evidence of postoperative argyria.
306
Titania nanotubes formed by electrochemical
anodization on the surface of titanium nanowires used for bone fixation were capable of
being loaded with gentamicin and releasing it over a period of 2 weeks.
307
In another study,
however, the same combination of gentamicin and TiO
2
nanotubes with an 80-nm diameter
and 400-nm length led to prompt release of the drug in only 1–2 hours, but it still reduced
the adhesion of Staphylococcus epidermis on the surface compared with pure titanium.
308
Surface etching and anodization parameters could be used to modify the diameter of the
nanotubes and thereby control the rate of diffusion of the drug stored in them into the
biological environment.
309
Surface texture of the material is also a property of interest; for example, electropolishing of
a Ti-6Al-7Nb alloy decreased the amount of S. aureus adhering to it.
310
A tradeoff,
however, is expected to arise because osteoblasts, which compete with the bacteria for the
bioactive surface of the implant in a process that greatly determines the clinical outcome,
311
also prefer to attach to rougher surfaces, such as those that typify naturally topographically
irregular calcium phosphates.
312
To that end, titanium implants are being subjected to
sandblasting and etching procedures,
313,314
as well as coated with bioactive layers,
predominantly hydroxyapatite,
315–317
to make up for their intrinsic bioinertness and have
their bioactivity boosted before surgical insertion.
G. Composites
In the design of nanoparticles for biomedical applications great emphasis has been placed on
particles capable of simultaneously aiding in prevention, early detection, and treatment of a
medical condition. With antibiotic calcium sulfate cements already in use in prophylaxis
against surgical wound infection, it can be expected that theranostic particles able to
simultaneously prevent, monitor, or diagnose the onset of infection and release antimicrobial
agents to prevent its early spread may be developed in the future. In that sense fantastic
multifunctional composite nanoparticles can be considered to be the ideal toward which the
nanoparticle fabrication field will advance (Fig. 7a). The difficulties in achieving stable,
chemical functionalization of calcium phosphate particles with therapeutic ligands can be
mitigated by coating them with a chemically bondable layer, such as PLGA
318,319
or
PCL
320
or by forming around the calcium phosphate core multilayered composite particle
structures
321
with an ability to carry various therapeutic agents either between the calcium
phosphate layers or within the polymeric coatings (Fig. 5b–d). Through a simple series of
chemical steps, polymeric coatings can also be conjugated with various targeting or
therapeutic ligands.
322
Binding amino acids with appropriate physical properties via PEG
linkers, for example, phenylalanine as a hydrophobic residue, lysine as a positively charged
one, and glutamic acid as a negatively charged one, can be used to increase the drug-binding
affinity of the polymeric surface.
323
Tailoring of the nanodiamond particle surface with
carboxylic or amino groups to render it negatively or positively charged under physiological
conditions, respectively, greatly affected the binding and release of various drugs; binding of
the negatively charged drug by physisorption to an amine-functionalized surface is so
Uskoković
Page 15
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

intensive that virtually no release in vitro occurred.
324
Such combinations of various loading
locations on the particle could potentially yield multiple-stage release profiles that might not
only favor the antimicrobial efficacy of the particles in vivo but also prove to be beneficial in
increasing the regenerative capacity of the carriers, given that the tissue regeneration process
following injury can be divided into multiple stages (Fig. 7b), each of which could be
targeted and augmented by a specific particle additive released within a precisely tailored
time window. To avoid adverse outcomes resulting from obviation or incompletion of any
single one of the interconnected steps in the bone-healing cascade (Fig. 7c, d), the
biomolecular machinery involved in every one of these stages could be targeted separately
and triggered at the right time by using such a smart composite particle that sequentially
releases its multiple payload in a highly controlled, spatiotemporal manner. An interesting
approach to achieving such multimodal release profiles is through cooperative assembly of
block copolymers as elemental building blocks of the particle, each of which carries a
unique therapeutic payload and degrades at a different rate.
325
The combination of calcium phosphates with a polymeric component can also be beneficial
for the second essential function to be achieved by these nanoparticulate drug carriers, in
addition to their antibacterial role: assistance in bone regeneration. Namely, since bone itself
is a composite material comprising a soft, collagenous component and a hard, ceramic one,
it is natural to expect that a soft/hard composite of a similar nature should prove an ideal
material for bone replacement therapies. In view of this, a range of properties of calcium
phosphates is improved upon their combination with a polymeric phase, starting, most
essentially, with the mechanical ones. Namely, it is generally assumed that the
microstructure and nanoarchitecture of calcium phosphates alone cannot be modified in such
a manner as to make the material mechanically compatible with the grafted bone and
prevent the frequent fracture of the filler upon its surgical placement to substitute natural
bone.
326
Only a combination with a soft component is thought to be able to ameliorate these
fundamental issues associated with the clinical application of calcium phosphates. The
combination of viscoelastic properties of the polymers and osteoconductivity of calcium
phosphates has yielded composites that surpassed the resistance to fracture, structural
integrity, and stiffness of the individual components,
327
making up for the low compressive
strength of the former and the brittleness and lack of malleability of the latter.
328
Reinforcement with polypropylene fumarate,
329
for example, improved the flexural strength
of brushite from 1.8 to 16.1 MPa and increased the fracture surface energy from 2.7 to 249
J/m
2
. Although calcium phosphates exhibit relatively high values of compressive strength
(10–100 MPa), as opposed to tensile and shear strengths (1–10 MPa), even these values
could be improved with the addition of a polymer, as exemplified by the doubling of the
compressive strength of a biphasic calcium phosphate cement, from 35 to 60 MPa, upon the
incorporation of only 0.5 vol% of a superplasticizer based on a vinyl-modified
copolymer,
330
as well as upon the addition of gelatin
331
or ammonium polyacrylate.
332
Polymers could also increase the plastic flow and enhance the viscosity of the material, thus
making possible its preparation in the form of an injectable self-setting paste,
333
although
there is usually a fine line dividing an excessive increase in the setting time from improved
mechanical properties.
334,335
Finally, the resorption time and the corresponding bone
ingrowth rate significantly increased when hydroxyapatite was implanted as a bone
Uskoković
Page 16
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

substitute in vivo in a composite form, in combination with PLGA,
336,337
a polymer that is
able to accelerate the resorption of calcium phosphates by releasing its acidic degradation
products.
338
Yet another tradeoff exists here: An increase in the porosity of the ceramic
substructure of the composite leads to improved bioresorption characteristics but
simultaneously entails an increased susceptibility of the material to crack propagation and
the corresponding proneness to fail under load-bearing conditions.
339
Such composite particles showed promise in earlier research. Gentamicin-containing
granules composed of hydroxyapatite nanoparticles, chitosan, and ethyl cellulose, for
example, were effective in the treatment of chronic osteomyelitis.
340
Another prospective
hybrid organic–inorganic system was formed by dispersing silsesquioxane microspheres
loaded with acetylsalicylic acid as an anti-inflammatory model drug in a calcium phosphate
cement.
341
Similar composites reduced in size to the nano scale may be recognized as a
trend toward which this field will be moving (Fig. 8). Polymeric coatings may also increase
the loading capacity and prevent the burst release of the drug merely adsorbed on the
particle surface. Coating chitosan/tricalcium phosphate composites with 2.5w/v% PCL has
thus mitigated the burst release effect and promoted zero-order kinetics for the release of
vancomycin during the first 6 weeks.
342
Impregnation of the poly(α-hydroxy esters) with
bone morphogenetic proteins has been shown to (1) overcome the inflammatory response,
(2) induce full bioresorption of the polymer, and (3) enhance bone growth,
343–345
while the
addition of demineralized bone particles to PLGA reduced (1) inflammation, (2) fibrous
tissue encapsulation, and (3) foreign body giant cell response.
346
The combinations of
alkaline calcium phosphate phases, such as hydroxyapatite or octacalcium phosphate, with
acidic poly(α-hydroxy esters) are thus particularly interesting because of their ability to
mutually compensate for potentially harmful pH changes that follow their degradation. The
wide range of pH conditions provided by the synergetic action of osteoblasts and osteoclasts
in the degradation of calcium phosphates in vivo makes the use of pH-sensitive coatings
potentially interesting, too. Poly(aspartic acid) presents one such pH-sensitive polymer; its
swelling is more pronounced at the physiological pH than at pH ~3 and can be facilely
controlled by the degree of cross-linking.
347
Another type of environmentally responsive
polymers are thermosensitive polymers, which transform from sols to hydrogels at body
temperature and enable in situ gelling at the target site promptly after injection.
348
Some of
the biodegradable polymers of this type include N-isopropylacrylamide copolymers,
poly(ethylene oxide)/poly(propylene oxide) block copolymers, and PEG/poly(D,L-lactide-
co-glycolide) block copolymers, the latter of which have been successfully applied to
encapsulate teicoplanin with 100% efficacy and treat osteomyelitis in rabbits.
349
That even the activity of antibiotics can be improved with a proper coating is illustrated by
the more effective prevention of the formation of S. aureus biofilms when vancomycin was
delivered encapsulated within cationic liposomes and carried in a porous nano-
hydroxyapatite/chitosan/konjac glucomannan scaffold.
350
The same antibiofilm effect was
achieved by the delivery of liposomal gentamicin from scaffolds containing β-tricalcium
phosphate with release kinetics able to be controlled by the liposome size.
351
Functionalization of particulate carriers with anionic amphiphiles that may disrupt the
bacterial biofilm and neutralize the carbohydrates by the action of which bacteria penetrates
Uskoković
Page 17
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

the cell membrane is another unexplored but potentially fruitful direction for research. With
antioxidant therapy being one of the hotspots of medicine, endowing carriers with reducing
agents, such as ceria domains
352
or ascorbic acid,
353
could be an avenue for abating the
reactive oxygen species and minimizing the oxidative stress that entail infectious disease.
Nanoparticle uptake by the cells can be controlled using ζ potential,
354
a ubiquitous physical
property,
355
but precise correlations between the surface charge and the therapeutic efficacy
of nanoparticles in the treatment of osteomyelitis have yet to be established, even though
wound healing could be enhanced by endowing cells with relatively high ζ potentials.
356
The usage of dispersion agents or the application of other strategies from the repertoire of
colloid chemistry
357
to promote greater dispersion and penetration of the antibiotic-carrying
particle to the infected tissue—a general challenge for the developers of injectable drug
delivery materials
358
—is another unexplored avenue.
Conjugation of the carrier particles to moieties that would have an affinity for various bone
components
359
and act as either targeting agents or metabologens is yet another unexplored
research directive in the design of antiosteomyelitis composite particles. Human
recombinant BMPs, two of which—BMP-2 and BMP-7—were approved for specific
clinical cases by the FDA, have been successfully delivered using various types of
nanoparticles, ranging from poly(α-hydroxy esters) to PEG-based hydrogels to dextran to
polymeric composites with hydroxyapatite to calcium phosphates alone,
360
and their
covalent binding on the polymeric particle surface may prove to be a more effective
approach for their delivery compared with internal encapsulation, especially in view of the
extraordinary sensitivity of their osteoinductive effect to the release kinetics.
361
These
conjugates could also include biomolecules that inhibit specific bacterial ingredients, such as
(1) lipoteichoic acids, components of gram-positive cell walls that induce bone resorption;
(2) polysaccharides in the bacterial capsules, which play a role in the adhesion of bacteria
onto an osseous or implant surface and the formation of a biofilm, the basis for proliferation
of pathogens in hard tissues; or (3) other osteolytic factors, including cytokines or other
signaling molecules, which may interfere with the pathway of the osteoblast lineage.
364
Such efforts may have a chance to bring researchers from drug delivery and drug discovery
fields closer because, after all, the synergy between the drug and the particle will prove to be
of ever more vital importance in the design of ultrapotent therapeutic agents in general.
Inclusion of peptides with strong antibacterial properties, which tend to be more immune to
promoting bacterial resistance if delivered in concentrations lower than minimal inhibitory
ones, would present another interesting approach.
365,366
The polymeric surface of a
composite particle could be functionalization with arginylglycylaspartic acid, a tripeptide
involved in cellular recognition and capable of triggerinxg adhesion of fibroblasts.
367
Bisphosphonates, molecules with a strong affinity for the mineral component of bone
368,369
and most commonly prescribed in the prevention and treatment of osteoporosis and other
conditions featuring bone loss and fragility,
370
could be used further to ensure particle
localization and the delivery of therapeutics directly in the area of infected tissue. Although
a possible concern comes from the clinically observed adverse consequences of
oversuppressed bone resorption and disrupted bone metabolism by the prolonged use of
bisphosphonates,
371
the risk for developing these side effects is still small compared to the
benefits.
372
Uskoković
Page 18
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

ZnO has been added to implantable PMMA beads as a radiographic contrast medium for the
past 30 years,
373
yet calcium phosphates and other carriers could be doped with heavy metal
atoms such as
111
In,
99m
Tc, Gd, or Mn or bound to optically active molecules and used for
the same imaging purpose with far greater sensitivity. Combinations of calcium phosphate,
PLGA, and semiconductor quantum dots
374,375
at the nanoparticle scale have enabled
monitoring of the particle route in the body, and the distribution of the locally implanted
therapeutics could be monitored in a similar manner. Quantum dots are, however, known for
their cytotoxic nature,
376
with only a few exceptions, including silica-based compositions,
the only type currently approved for use in clinical trials by the FDA.
377
Proposed as
bioimaging alternatives to inherently toxic quantum dots and nonbiodegradable aromatic
polymers are aliphatic, biodegradable, and tunably photoluminescent oligomers,
378
but they
have yet to be explored as components of bone tissue substitutes.
Porosity of composites in the compact, fully set form could be modified using other
additives, such as glucose,
379
calcium sulfate,
380
calcite,
381
gelatin,
382
or others, and set to a
specific pore size, pore size distribution, and pore interconnectivity that maximize the
internal cell proliferation and the transfer of nutrients and metabolic products. For example,
combinations of silica and calcium phosphate allowed for a control over porosity of the
resulting gentamicin-loaded nanocomposites in the mesoporous (2–50 nm) and macroporous
(>50 nm) ranges by means of controlling their silica content.
383
Porosity also could be
limited to the surface only
384
to promote a bioactive response while preserving the
compactness and stability of the core of the system against attack from the corrosive
biological environment, or the other way around, porous on the inside and compact on the
outside,
385
like bone itself. It could be also made gradient, extending throughout the bulk of
the composite in different ways.
386
As a matter of fact, Janus-faced
387
and functionally
gradient structuring
388
on the nano and molecular scales are other largely unexplored, yet
incredibly potent features of the next generation of advanced materials. Finally, enriching
antibiotic carriers with pluripotent cells, such as mesenchymal stem cells able to
differentiate into osteoblasts,
389,390
would be another research step in the direction of
advanced therapeutic platforms for simultaneous bactericidal and osteogenic performance.
In that sense, understanding the role of the extracellular matrix and an array of
microenvironmental cues in directing the pluripotent cell fate currently stands as a major
challenge to be overcome to minimize cells’ chances of acquiring neoplasticity and to
maximize their chances of acquiring the best possible phenotype for the given therapy.
391
V. ADDITIONAL CHALLENGES
A. Inconsistencies Arising from Different Analytical Contexts
An essential wisdom conveyed from the drug delivery field is that context is everything.
When not delivered in a proper manner, even the most effective therapeutics will be
deprived of their remedial effectiveness. A direct corollary of this insight is that drug
discovery and drug delivery could be imagined as two sides of the same coin,
complementing each other in a complete drug therapy. In other words, in a wrong setting
even the most therapeutically potent agent will be ineffective, whereas even the most toxic
chemicals applied in the right amount and setting could strengthen an organism, as data in
Uskoković
Page 19
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

support of the effect of hormesis could indicate. Therefore, it should not be surprising that
problems and challenges will continue to abound even if we were to succeed in the design of
a perfect drug delivery carrier.
An example of the effect of the environmental context on a drug elution profile from a
particulate carrier is shown in Fig. 9. Namely, two kinetically distinct release profiles from
an identical drug-containing powder result, depending on the release measurement method
applied: zero-order when a comparatively small volume of the solvent is replenished daily
and first-order when a larger volume of the solvent is used without its daily replenishments.
Whereas the drug is released with a burst effect when large amounts of solvent surround the
powder, a limited volume of the solvent limits the maximal amount of the drug that could be
released before saturation, leading to identical concentrations of the drug in the solution
sampled at regular time spans (24 hours). In such a manner reprecipitation of sparsely
soluble hydroxyapatite on the surface of more soluble di- and tricalcium phosphates in the
form of a protective layer that hinders further dissolution, which might have occurred in vivo
or at smaller solvent volumes, and higher corresponding degrees of supersaturation can be
prevented by frequently replenishing the solvent and used to speed up the dissolution of
these calcium phosphate phases under physiological conditions. Neither of these two
methods, however, mimics the biological conditions under which fast clearance of the
released drug is typically observed, nor do they account for the effects of the complex
interface between the device and various macromolecules and cells of the host organism on
the drug release. Although the size, shape, and elasticity of nanoparticles in biological
milieus do influence their biodistribution profiles, the route of uptake and the mechanism of
interaction with a cell are mainly determined by the protein corona adsorbed on the particles
and the surface propensities that it endows them with.
394,395
How to devise in vitro drug
release testing procedures that would be able to replicate in vivo conditions better, typically
characterized by (1) a more dynamic flow of fluids, (2) specific local pH profiles that are
often disease-dependent, and (3) much more complex and selective media, is another
colossal challenge for the drug delivery field.
Incompatibility between in vitro and in vivo tests has been frequently observed
396
; what has
been shown as toxic or inflammatory in vitro can have the same effect in vivo but can also
provide the right level of inflammation that follows every successful reaction toward unity
between the bone and the implant.
397
The trivial observation that pure water momentarily
destroys cells in culture via osmotic rupture of the cell membrane, whereas we consume it
every day without serious consequences, could be used to illustrate the inevitable
discrepancy between testing materials in culture and in a more complex, organismic
environment. Moreover, not only do different lines of the same cell type often respond
differently to identical chemical stimuli
398
; the same insight applies to cells from the same
line but at different stages of cell cycle progression.
399
On the other hand, techniques for
replicating the exact microenvironment in which cocultured primary cells exist in the body,
which is one of the key factors that determine their fate,
400
have yet to be developed.
As for animal models of osteomyelitis, different species and experimental protocols have
been used in the past. The rabbit is the oldest animal model of osteomyelitis, dating back to
1941,
401
and it has traditionally involved injections of a suspension comprising S. aureus
Uskoković
Page 20
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

and 5 wt% sodium morrhuate, a sclerosing agent causing aseptic necrosis of bone, to induce
suppuration and subperiosteal abscesses in the bone. Fibrin glue and other sealants often are
used to prevent bacterial leakage.
402
The most common, however, is the rat model, typically
involving the insertion of screws or other fixation devices inoculated with S. aureus.
403
An
alternative method involves the creation of a defect in the tibia or femur by drilling a hole in
it and stabilizing it with screws, plates, and wires. The defect then is filled with collagen or
gelatin sponges soaked in S. aureus and kept there for up to 24 hours, which is superseded
by injection or implantation of an antibiotic-releasing material.
404
Mice and chickens are
other common small-animal models, whereas dogs, goats, and sheep are the most common
large-animal models, whose main advantage is the ability to accommodate real-size devices
and tolerate multiple interventions, alongside more veritably mimicking the mechanical
loads born by bones in the human body. A central challenge in all of these models is how to
create bone lysis that is sufficient but not excessive and does not threaten the fixation
stability. Avoiding the formation of virtually untreatable biofilm on fixation devices is cited
as another challenge faced by these animal models,
405
even though it presents a more
faithful model for cases in which infection is secondary to surgical foreign body
implantation. Yet another detail common to these models is that chemically induced necrosis
or mechanical trauma, such as fracture (as in most mouse models) or the insertion of
intramedullary pins, plates, or other fixation devices, need to be coupled to dispersal of the
pathogen to induce chronic infection.
406
Still, in spite of more than 70 years since the first
reproducible animal model of chronic osteomyelitis was reported and continuous
advancements since then, inconsistent correlations between in vitro and in vivo antibacterial
efficacies of therapeutic agents still commonly occur.
407
As for the drug elution rate, values obtained in vitro may drastically increase in vivo for
various reasons, including the complex interface with chemical and biological species (e.g.,
enzymatic activity, the concentration of free radicals that induce oxidative scission of
covalent bonds between monomers, the types of antibodies adsorbed, or the extent of fibrous
capsule formation, if any) or different rheological properties, demanding new strategies to
ensure the optimal 4–6 weeks of release time. PLGA scaffolds, for instance, degraded faster
in vivo than in vitro,
408
and in addition to phagocytosis, enzymatic hydrolysis, the regions of
low pH at the cell–material interface, and biomechanical stress, increased wetting in
biological conditions can be another factor responsible for this effect.
409
This is especially
relevant for hydrophobic polymers, the category to which unmodified PLGA belongs. This
disparity between the carrier degradation and the drug release kinetics estimated using in
vitro and in vivo measurement modes is expected to be even higher for calcium phosphates
than for polymers because while the degradation of the latter is primarily driven by
hydration and hydrolysis both in vivo and in vitro, the degradation of ceramic implants is
mainly caused by the phagocytic and acidifying (pH 7.4 → 3–4)
410
action of multinucleated
osteoclasts and macrophages.
411
This discrepancy is further added up to by knowing that
calcium phosphate phases more soluble than octacalcium phosphate transform to a certain
degree into the most stable phase, hydroxyapatite under physiological conditions.
412,413
Factors that dictate to what degree this transformation takes place in vivo are not clearly
defined; on one hand its precursors are classified as biosoluble ceramics,
414
unlike
bioresorbable hydroxyapatite, and indisputably degrade faster than the latter, whereas on the
Uskoković
Page 21
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

other hand this transformation has been both theoretically predicted and experimentally
verified on numerous occasions.
415–417
Comparatively soluble calcium phosphates,
including monetite, brushite, and amorphous calcium phosphate, were also found in vivo,
418
suggesting that this transformation may frequently be limited to a few surface layers that
undergo intense dissolution/reprecipitation, thus protecting the inherently unstable and
soluble particle or implant core. The chemical propensity of more soluble calcium
phosphates to be resorbed at a higher rate, however, is complicated by knowing that
osteoclasts anchor more steadily on the less soluble calcium phosphate phases; the
substantial release of Ca
2+
ions from the surface of the more soluble ones disrupts the
ordering of actin microfilaments in the osteoclast podosomes, leading to the periodic
detachment of the cells from the material surface.
419
Similarly, whereas the degradation of
aliphatic polyesters(e.g., PLGA)is slowed under fluid flow because of dissipation of acidic
byproducts that would have sped up the degradation process, fluid flow prevents local
supersaturation and accelerates the degradation of alkaline calcium phosphates such as
hydroxyapatite. Hence, despite the excellent release profiles in vitro, the possibility that the
minimum inhibitory concentration in sections of the target tissue may not be exceeded in a
time-sustained manner, be it due to biofilm formation, intracellular colonization, premature
biodegradation, or other factors, will always exist. In such a way exist threats that antibiotic
resistance could be inadvertently promoted, an effect that directly contributes to the global
loss of antibiotic efficacy in use.
420
In those cases even a direct injection of a bolus dose of
the antibiotic may lead to more favorable outcomes than the implantation of the drug–carrier
composite.
421
B. Antibiotic Specificities
Antibiotics differ according to their mechanism of action; some, such as β-lactam
antimicrobials, are time-dependent, requiring prolonged presence in the target zone for
effective suppression or eradication of the pathogen, whereas others, such as quinolones and
aminoglycosides, are concentration-dependent, requiring higher concentrations over shorter
periods of time.
422
Therefore, depending on the nature of the drug, differently structured
carriers may prove to be most optimal. As expected from the synergetic background of drug
carrier interaction, the properties of the carrier influence the efficacy of the drug therapy, but
the drug identity, amount, and binding mechanism in turn influence the properties of the
carrier. The anionic group of gentamicin sulfate, for example, had an inhibitory effect on the
crystallization of brushite during coprecipitation of the antibiotic and the carrier, resulting in
smaller particles, lower porosity, and slower drug release compared with pure
gentamicin.
423
The morphology, crystallinity, and dispersability of particles coprecipitated
with the drug may thus all be affected by the drug properties. The loading efficiency and the
release rate of a drug from a particle is consequently dependent on the molecular nature of
the drug, as exemplified by the different elution profiles for different antibiotics
424
The
release from PMMA beads, for example, varied drastically, reaching completion anywhere
between 3 and 21 days, depending on the antibiotic admixed.
425
Also, whereas the release of
vancomycin from a brushite cement reached completion between days 1 and 2, only one
quarter of tetracycline loaded within the same carrier was released on day 5.
426
Synergetic
effects are important here; for example, the elution rates for tobramycin and vancomycin
released together from a PMMA cement were higher than those when the drugs were
Uskoković
Page 22
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

released alone.
427
Then, not only does the identity of the drug have an effect on release
profiles, but its amount can drastically modify them, too, as exemplified the case where 25
μg/cm
2
of paclitaxel deposited on the surface of a phosphonohexadecanoic acid coated
cobalt chromium alloy released 90% of the drug in the first week, whereas quadrupling the
paclitaxel concentration to 100 μg/cm
2
resulted in zero-order release throughout a 5-week
period of time.
428
The release zone of the antibiotic following surgical insertion is generally only a few
centimeters, and the rheology of the fluid in which the drug carrier is immersed, including
hematoma and seroma, might redirect the released drug away from the target site. Therefore,
continuous-flow chambers have been designed to assess drug elution profiles under more
dynamic conditions that resemble the in vivo context to a greater extent.
429
Still, different
implantation sites greatly affect the biodegradation rate of the implant, including the release
profile of the drug that it contains.
430
Subcutaneous implantations of a biomaterial
composed of PEG and poly(butylene terephthalate) thus degraded faster than the
intramuscular ones,
431
whereas polydioxanone orthopedic pins were resorbed faster when
implanted in the medullar canal rather than intramuscularly or subcutaneously.
432
Mechanical loading, sheer, and friction are other factors that contribute to the different
release from orthopedic drug delivery devices implanted at different sites in the body.
433
Also, hypochlorites generated smaller polymeric fragments with higher toxicity than
peroxides,
434
suggesting that the dominant reactive oxygen species as inflammatory
compounds in the implantation area, which are involved in the degradation of polymeric
carriers, inevitably define the toxic propensities of the biomaterial in question. In that sense
the art of surgical implantation has to complement the reliability of the drug release pattern
of the implanted drug–carrier composite. That different target areas in the body require
unique drug delivery platforms for optimal release has been confirmed many times, and it is
logical to expect that the same will prove to be true in the treatment of different segments of
bone. Mandibular infection, for example, typically requires a shorter duration of antibiotic
therapy compared with long-bone infection. Intensely vascular cancellous bone, with a
comparatively high rate of turnover, may thus be expected to require more intense release
kinetics compared with less vascular and more slowly remodeled cortical bone.
435
In
general, the principle similia similibus curantur, dictating the substitution of like with like,
is expected to apply in every aspect of tissue engineering, including the province of bone.
C. Intracellular Colonization by S. aureus
Another potential difficulty arises from the fact that S. aureus, the main causative agent of
osteomyelitis, found in healthy oral and nasal flora has the ability to penetrate endothelial,
epithelial, and osteoblastic cells and thrive in the intracellular environment, where it is less
susceptible to the antibiotic therapy.
436–438
Different but in all cases finite uptake efficiency
and kinetics were observed for different strains of S. aureus, and common to all of them was
the role of fibronectin-binding proteins in intracellular colonization, the blocking of which
completely prevented the latter from occurring.
439
S. aureus internalized by the cells and
shielded from the host immune system is thought to provide a reservoir of bacteria in
recurring osteomyelitis and inhibit the immunological role of osteoblasts in releasing
cytokines and attracting leukocytes to the infection site. Targeting the antibiotic therapy to
Uskoković
Page 23
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

these intracellular colonies may thus prove to be more relevant for treating chronic bone
infection than eliminating only pathogens that colonize the bone matrix.
440
Nanoparticles,
including calcium phosphate ones, have shown great promise in the intracellular delivery of
plasmids,
441–443
and they may similarly prove to be effective carriers of antibiotics inside
the cell where bacterial microcolonies are localized. Correspondingly, a recent study showed
that clindamycin-loaded hydroxyapatite and amorphous calcium phosphate particles are
more effective in reducing the intracellular bacterial population and slowing the growth of S.
aureus cocultured with osteoblastic MC3T3-E1 cells than the pure antibiotic.
444
Figure 10a
shows a schematic description of their uptake by the cell and the delivery of a genetic
material to it, whereas 10b shows the intracellular localization of calcium phosphate
nanoparticles in an immunofluorescent analysis of osteoblastic MC3T3-E1–calcium
phosphate interface. A reduction in the number of intracellular bacteria has already been
demonstrated for nanosized PLGA particles loaded with nafcillin.
445
The rapid degradation
of calcium phosphate carriers in the acidic milieu of a lysosome–endosome complex
following uptake may also increase the osmotic pressure and enable the plasmid or protein
cargo to escape swiftly into the cytoplasm before it is enzymatically hydrolyzed, which
could be considered yet another advantage of calcium phosphates as intracellular delivery
agents.
D. Synergetic and Sensitivity Effects
Immunofluorescent labeling and confocal microscopy, along with other in vitro assays,
including real-time polymerase chain reaction, can provide good insight into the cell–
material interface on which the bone regeneration aspect of therapy ultimately depends
446
(Fig. 11a). Nanoparticles have, however, been notorious in terms of resisting any clear-cut
descriptions of their biological effects, as exemplified by the recently derived inverse, dose-
dependent toxicity relationship for 100-nm silica nanoparticles in the human epithelial
intestinal HT-29 cell line.
447
In a similarly counterintuitive fashion, the uptake efficiency
and the expression of plasmids could occasionally be out of proportion: Efficient uptake
may lead to low gene transfection and vice versa.
449
Synergetic effects resulting from the
minor amounts of impurities left over from synthesis procedures or supposedly inert product
components may prove to be equally important in determining therapeutic outcomes. For
example, the osteogenic effect of calcium phosphate as a drug carrier was able not only to
mitigate but also to fully reverse the unviable effect that the pure antibiotic exerted on
osteoblastic cells, while retaining its antimicrobial potency through a more sustained release
of the antibiotic (Fig. 11b).The addition of calcium hydroxide to tobramycin-containing
PMMA beads similarly had a protective effect on bone against the high concentrations of
the antibiotic.
450
A related problem occurring in parallel with the sophistication of the carrier particle is the
difficulty transferring the synthesis methods from the laboratory to the clinic or any large-
scale fabrication setting. Namely, the more intricate the particle, the greater the range of
experimental variables to which its preparation is sensitive.
451
The case of Abbott Labs
losing hundreds of millions of dollars trying to restore the polymorph of their proprietary
AIDS drug, Ritonavir, after a new polymorph had begun to appear in their synthesis batches
and before being forced to withdraw the drug from the market and lose another half a billion
Uskoković
Page 24
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

dollars,
452
can thus be instructive, if not ominous, in its foreshadowing the trend of a
pervasive irreproducibility toward which the science of synthesis of fine particles streams.
Startups in organic photovoltaics have, for instance, failed to make profit mainly because of
the unsurpassable variability in processing outcomes. A systematic analysis of two donor
materials synthesized by the same manufacturer resulted in confirmation of the same
crystallinity, side-chain variation, interface composition, and domain morphology, yet their
performance was radically different because of a difference in the nano scale that was too
fine to be probed by state-of-the-art instrumentation.
454
Note also that the purity of solvents
and compounds used as precursors for the synthesis of nanostructured powders has had a
drastic effect on their morphology,
455
whereas cell detachment or excellent spreading result
depending on whether cultured cells are grown on ordinary or tissue culture–grade
polystyrene.
456
Alongside the chemical effects exemplified by different reaction outcomes
when reactants produced by different manufacturers are used, there exist examples of the
following physical effects on synthesis reactions: stirring rate
457,458
; the Earth’s magnetic
field
459,460
; gravity,
461,462
whose intensity appears to be directly proportional to the
osteogenic potency of mesenchymal stem cells and boney tissues
463–465
; the seasonal
variations in (1) humidity,
466
(2) barometric pressure, and (3) temperature; micrometric
differences in the positioning of samples in furnaces during annealing
467;
experimental
animal behavior; and circadian rhythm, on which the expression of almost 50% of genes in
certain cell types has been shown to depend
468
; and the reaction vessel composition,
469
texture,
470
and dimensions,
471,472
one of the most critical parameters in the transfer of
synthesis methods from a small-scale setup in a laboratory to a large-scale fabrication setting
in an industrial milieu. For example, overly tall reaction volumes increased the probability
of the formation of aragonite or vaterite, two of the less thermodynamically stable calcium
carbonate phases during the precipitation of this compound from a solution in the presence
of an organic matrix, whereas flattened volumes were more prone to yield calcite, the least
soluble calcium carbonate phase.
473
Agitation, a traditional means for dispersing particles,
has occasionally had the opposite effect, inducing the aggregation of both polymeric and
inorganic nanoparticles,
474
which may explain cases in which the efficiency of drug loading
via adsorption is inversely proportional to the stirring rate.
475
Similarly antagonistic effects
of specific physicochemical synthesis parameters present more of a rule than an exception in
the field of nanoscience.
476
Assessments of biological responses are particularly prone to
exhibit such antagonistic intricacies, as exemplified by the case in which doubling the dose
of calcium phosphate nanoparticles transformed the response of human bronchial epithelial
cells from unviable to viable.
477
Biological systems in general are, in fact, notorious for
their sensitivity to the slightest change in their homeostatic equilibria, as demonstrated by
the long-familiar finding that bone reaches its maximum toughness in compositions that
leave behind 66.5 wt% of ash, twice higher than the value at 65 and 68 wt% of ash
content.
478,479
On the characterization side, this sensitivity results in ever more difficult
separation of the effects of the measurement system from the properties of the measured
objects, and this will increasingly apply to all 3 essential characterization aspects toward
which materials science progresses: single-particle spectroscopic microscopy, high-
throughput analysis, and in situ analyses. Of course, each of these problems conceals a
gateway to an exciting opportunity, as exemplified by the fact that ultrafine microscopic
methods do regularly create or remove single vacancies
480
or shift adatoms
481,482
on the
Uskoković
Page 25
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

surfaces of analyzed materials, but measuring the energy required for these local
transformations to take place has allowed for the construction of atomic-scale images of
local phase properties,
483,484
which is state-of-the-art in the field of materials imaging.
In view of this one thing is certain: the design of a new generation of biomaterials will need
to cope with the very same issues pertaining to the extraordinary sensitivity of function to
the finest structural and compositional variations if its products are to match perfectly the
properties of the natural tissues they are meant to replace. Yet, as common wisdom has it, a
path without risks, perplexities, and challenges is not worth taking, and difficulties arising
from attempts to design nanoscale platforms for the ultrasensitive delivery of pharmaceutics
can certainly be seen as signs that those involved in these endeavors are heading in the right
direction.
VI. SUMMARY
We approach a time of a prolific confluence of materials science and medicine. It is
anticipated that materials science will provide the foundations for the design and
development of advanced diagnostic and therapeutic methods. Within the frame of its
objective, this review has provided a critical view of the current state of affairs in the
development of nanoparticulate and other solid-state carriers for the local delivery of
antibiotics in the treatment of osteomyelitis. In a broader picture extending outside of this
narrow frame, however, is a view of ongoing progress in the way a relatively modest field of
medicine, in terms of the complexity of therapeutic materials used, is being revolutionized
by recent advancements in materials science and engineering. The surgical implantation of
PMMA beads or, occasionally, plaster of Paris still presents the most popular method for the
local and sustained delivery of antibiotics in the treatment of osteomyelitis, but this is about
to change as more sophisticated materials, nanostructured in essence, are being developed
on laboratory benches and sent down the translational path toward the direction of the
bedside.
The two principal downsides of the traditional means of treating bone infection are systemic
and long-term administration of antibiotics and the necessity for surgical debridement. The
new generation of carriers for the delivery of antimicrobials envisaged during this discourse
is expected to tackle these issues by first promoting the sustained release of antibiotics
limited to the target site. Another vital feature of advanced carriers for the controlled release
of antibiotics is their ability to contribute to the osteogenesis of the adjacent tissue in parallel
with their degradation and replacement with regenerated bone. Thus antibiotic delivery and
tissue regeneration are two central aspects of therapies for osteomyelitis in which milestone
improvements are to be expected using the new generation of nanostructured carriers. Next
steps in their development would be tuning their structure to an environmentally responsive
and spatiotemporally targeted performance, as well as integrating them with alternatives to
traditional antibiotics, whose ineffectiveness against increasingly resistant opportunistic
pathogens is approaching critical scales. If we look at this trend in the development of drug
delivery carriers for treating a particular disease from a broader angle, outside of the frame
once again, we might conclude that structurally complex, multifunctional, theranostic
composite nanoparticles present an object of interest toward which scientific efforts
Uskoković
Page 26
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

colliding at this multidisciplinary junction of medical significance will be converging in the
years and perhaps decades to come.
For a long time the degradation of polymeric biomaterials had been considered an
unfavorable process, a cause of the deterioration of their properties and performance in the
body. It took a fresh, new look at them to turn these demerits into advantages and present
their degradation as a colossal value and untapped potential for the biomedical community.
Using their degradation as a pathway to controlled drug release and tuning it to the rate of
new tissue in growth nowadays presents the basic approach to tissue engineering and
regenerative medicine. It goes without saying, of course, that the time for the reversal of this
paradigm and inauguration of equally legitimate strivings to create bionic tissue-engineered
materials—whose purpose would be not only to restore the lost functionality in a segment of
the body or the body as a whole but also to augment and raise it far beyond the levels of
ordinariness via lasting assimilation of the new interfaces—has yet to come. Be that as it
may, potential problems faced by even the hypothetically perfect antibiotic delivery vehicles
mentioned toward the end of this discourse include (1) the propensity of S. aureus, the main
causative agent of osteomyelitis, to form intracellular colonies involved in recurrent, chronic
osteomyelitis; (2) the need for the mechanical and release properties of a carrier to be
adjusted to the target area of surgical implantation or injection; (3) the disparity between
environments in which in vitro and in vivo drug–carrier composite testing is carried out; (4)
unpredictable synergetic effects of the delivery system components or foreign agents; and
(5) experimental sensitivity issues posed in parallel with the increasing subtleness of
nanoplatforms designed for the controlled delivery of therapeutics. Inspired by the parable
of biodegradable polymers, we could conclude that all of these problems, were they
considered from a fresh, new angle, might either stimulate the development of
bioengineered systems that will solve them and many other problems at the same time or,
even more amazingly, be glimpsed as solutions per se to problems existing in a different
domain. For if a new, multidisciplinary model for a prolific lifetime in science teaches us
something, it is that two gaps in knowledge, when combined, can create a bridge to much
greater knowledge lying far beyond the horizon.
Acknowledgments
Writing of this review was supported by the National Institutes of Health grant R00-DE021416: Osteogenic
calcium phosphate nanoparticles with designable drug release kinetics. The confocal optical micrographs presented
herein were acquired by the author at the Nikon Imaging Center at the University of California, San Francisco.
References
1. Lew DP, Waldvogel FA. Osteomyelitis. Lancet. 2004; 364(9431):369–79. [PubMed: 15276398]
2. DeWald, RL. Spinal deformities. New York: Thieme Medical Publishers, Inc; 2003. p. 222
3. Ikpeme IA, Ngim NE, Ikpeme AA. Diagnosis and treatment of pyogenic bone infections. Afr Health
Sci. 2010; 10(1):82–8. [PubMed: 20811530]
4. Office of the Surgeon General. Bone health and osteoporosis: a report of the Surgeon General.
Rockville: US Department of Health and Human Services; 2004.
5. Paluska SA. Osteomyelitis. Clin Fam Practice. 2004; 6(1):127–56.
Uskoković
Page 27
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

6. King, RW.; Johnson, DL. Stearns, DA.; Talavera, F.; Weiss, EL.; Halamka, JD.; Kulkarni, R.,
editors. Osteomyelitis. eMedicine Medscape Reference. 2011. retrieved from http://
emedicine.medscape.com/article/785020-overview#a0101
7. Bisland SK, Chien C, Wilson BC, Burch S. Pre-clinical in vitro and in vivo studies to examine the
potential use of photodynamic therapy in the treatment of osteomyelitis. Photochem Photobio Sci.
2006; 5:31–8.
8. Khan, AN.; Macdonald, S. Gentili, A.; Coombs, BD.; Beltran, J.; Krasny, RM.; Chew, FS., editors.
Osteomyelitis, chronic. eMedicine Medscape Reference. 2011. retrieved from http://
emedicine.medscape.com/article/393345-overview
9. Vanarsdale WW II. On the present state of knowledge in bacterial science in its surgical relations
(continued): osteomyelitis. Ann Surg. 1886; 3:221–6.
10. Qureshi AT, Terrell L, Monroe WT, Dasa V, Janes ME, Gimble JM, Hayes DJ. Antimicrobial
biocompatible bioscaffolds for orthopaedic implants. J Tissue Eng Regen Med. 2014; 8(5):386–95.
[PubMed: 22700366]
11. Waldvogel FA, Medoff G, Swartz MN. Osteomyelitis: a review of clinical features, therapeutic
considerations and unusual aspects. N Engl J Med. 1970; 282:198–206. [PubMed: 4902833]
12. Del Pozo JL, Patel R. Infection associated with prosthetic joints. N Engl J Med. 2009; 361:787–94.
[PubMed: 19692690]
13. Blyth CC, Gomes L, Sorrell TC, da Cruz M, Sud A, Chen SC. Skull-base osteomyelitis: fungal vs.
bacterial infection. Clin Microbiol Infect. 2011; 17(2):306–11. [PubMed: 20384699]
14. Slenker AK, Keith SW, Horn DL. Two hundred and eleven cases of Candida osteomyelitis: 17
case reports and a review of the literature. Diagn Microbiol Infect Dis. 2012; 73(1):89–93.
[PubMed: 22578942]
15. Dotis J, Roilides E. Osteomyelitis due to Aspergillus species in chronic granulomatous disease: an
update of the literature. Mycoses. 2011; 54(6):e686–9. [PubMed: 21615532]
16. Fowler TP, Keener J, Buckwalter JA. Brucella osteomyelitis of the proximal tibia: a case report.
Iowa Orthop J. 2004; 24:30–2. [PubMed: 15296202]
17. Pääkkönen M, Kallio PE, Kallio MJ, Peltola H. Management of osteoarticular infections caused by
Staphylococcus aureus is similar to that of other etiologies: analysis of 199 staphylococcal bone
and joint infections. Pediatr Infect Dis J. 2012; 31(5):436–8. [PubMed: 22189524]
18. Saifudheen K, Anoop TM, Mini PN, Ramachandran M, Jabbar PK, Jayaprakash R. Primary
tubercular osteomyelitis of the sternum. Int J Infect Dis. 2010; 14(2):e164–6. [PubMed: 19524467]
19. Walsh DS, Portaels F, Meyers WM. Buruli ulcer (Mycobacterium ulcerans infection). Trans R Soc
Trop Med Hyg. 2008; 102(10):969–78. [PubMed: 18657836]
20. Balaji D. Osteomyelitis variolosa: a case report. J Orthop Surg (Hong Kong). 2011; 19:120–2.
[PubMed: 21519093]
21. Lentz MW, Noyes FR. Osseous deformity from osteomyelitis variolosa. A case report. Clin Orthop
Relat Res. 1979; 143:155–7. [PubMed: 509817]
22. Al-Jassir FF, Aldeeri RA, Alsiddiky AM, Zamzam MM. Osteomyelitis following Bacille
Calmette-Guerin vaccination. Saudi Med J. 2012; 33(1):87–90. [PubMed: 22273655]
23. Singhai RK. Osteo-articular complications of smallpox vaccination. J Indian Med Assoc. 1970;
55:20–2. [PubMed: 5474321]
24. Mruk AL, Record KE. Antimicrobial options in the treatment of adult staphylococcal bone and
joint infections in an era of drug shortages. Orthopedics. 2012; 35(5):401–7. [PubMed: 22588396]
25. Montanaro L, Testoni F, Poggi A, Visai L, Speziale P, Arciola CR. Emerging pathogenetic
mechanisms of the implant-related osteomyelitis by Staphylococcus aureus. Int J Artif Organs.
2011; 34(9):781–8. [PubMed: 22094557]
26. Conlon HA. Human bites in the classroom: incidence, treatment, and complications. J Sch Nurs.
2007; 23:197–201. [PubMed: 17676966]
27. Waldvogel, FA.; Medoff, G.; Swartz, MN. Osteomyelitis: Clinical features, therapeutic
considerations, and unusual aspects. Springfield: Charles C. Thomas; 1971.
28. Salgado CJ, Jamali AA, Mardini S. A model for chronic osteomyelitis using Staphylococcus
aureus in goats. Clin Orthop Relat Res. 2005; 436:246–50. [PubMed: 15995448]
Uskoković
Page 28
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

29. Baltensperger, MM.; Eyrich, GK. Osteomyelitis of the jaws. Berlin: Springer-Verlag; 2009.
30. Krakowiak PA. Alveolar osteitis and osteomyelitis of the jaws. Oral Maxillofac Surg Clin North
Am. 2011; 23(3):401–13. [PubMed: 21798440]
31. Humber CC, Albilia JB, Rottenberg B. Chronic osteomyelitis following an uncomplicated dental
extraction. J Can Dent Assoc. 2011; 77:b98. [PubMed: 21810374]
32. Yenson A, de Fries HO, Deeb ZE. Actinomycotic osteomyelitis of the facial bones and mandible.
Otolaryngol Head Neck Surg. 1983; 91(2):173–6. [PubMed: 6408574]
33. Hatzenbuehler J, Pulling TJ. Diagnosis and management of osteomyelitis. Am Fam Physician.
2011; 84(9):1027–33. [PubMed: 22046943]
34. Buchholz HW, Engelbrecht H. Depot effects of various antibiotics mixed with Palacos resins.
Chirurg. 1970; 41:511–15. [PubMed: 5487941]
35. Dingeldein, E.; Wahlig, H. Gentamycin-konzentration in korperflussigkeit von patienten nach
implantation von gentamycin-PMMA-kugeln. In: Contzen, H., editor. Unfallchirurgie, Symposium
Munchen. Vol. 1. Erlangen: Verlag; 1976. p. 8
36. McLaren AC. Alternative materials to acrylic bone cement for delivery of depot antibiotics in
orthopaedic infections. Clin Orthop Relat Res. 2004; 427:101–6. [PubMed: 15552144]
37. Klemm K. The use of antibiotic-containing bead chains in the treatment of chronic bone infections.
Clin Microbiol Infect. 2001; 7(1):28–31. [PubMed: 11284941]
38. Alonge TO, Ogunlade SO, Omololu AB, Fashina AN, Oluwatosin A. Management of chronic
osteomyelitis in a developing country using ceftriaxone-PMMA beads: an initial study. Int J Clin
Pract. 2002; 56(3):181–3. [PubMed: 12018822]
39. Giavaresi G, Borsari V, Fini M, Giardino R, Sambri V, Gaibani P, Soffiatti R. Preliminary
investigations on a new gentamicin and vancomycin-coated PMMA nail for the treatment of bone
and intra-medullary infections: An experimental study in the rabbit. J Orthop Res. 2008; 26(6):
785–92. [PubMed: 18186130]
40. Roeder B, Van Gils CC, Maling S. Antibiotic beads in the treatment of diabetic pedal
osteomyelitis. J Foot Ankle Surg. 2000; 39(2):124–30. [PubMed: 10789104]
41. Nelson CL, Hickmon SG, Harrison BH. Elution characteristics of gentamicin-PMMA beads after
implantation in humans. Orthopedics. 1994; 17(5):415–6. [PubMed: 8036185]
42. Moojen DJ, Hentenaar B, Charles Vogely H, Verbout AJ, Castelein RM, Dhert WJ. In vitro release
of antibiotics from commercial PMMA beads and articulating hip spacers. J Arthroplasty. 2008;
23(8):1152–6. [PubMed: 18534493]
43. Wong MW, Hui M. Development of gentamicin resistance after gentamicin-PMMA beads for
treatment of foot osteomyelitis: report of two cases. Foot Ankle Int. 2005; 26(12):1093–5.
[PubMed: 16390644]
44. Shinsako K, Okui Y, Matsuda Y, Kunimasa J, Otsuka M. Effects of bead size and polymerization
in PMMA bone cement on vancomycin release. Biomed Mater Eng. 2008; 8(6):377–85. [PubMed:
19197114]
45. Greene N, Holtom PD, Warren CA, Ressler RL, Shepherd L, McPherson EJ, Patzakis MJ. In vitro
elution of tobramycin and vancomycin polymethylmethacrylate beads and spacers from Simplex
and Palacos. Am J Orthop (Belle Mead NJ). 1998; 27(3):201–5. [PubMed: 9544361]
46. Adams K, Couch L, Cierny G, Calhoun J, Mader JT. In vitro and in vivo evaluation of antibiotic
diffusion from antibiotic-impregnated polymethylmethacrylate beads. Clin Orthop Relat Res.
1992; 278:244–52. [PubMed: 1563160]
47. Bereznowski Z. In vivo assessment of methyl methacrylate metabolism and toxicity. Int J Biochem
Cell Biol. 1995; 27(12):1311–6. [PubMed: 8581827]
48. Mainwaring G, Foster JR, Lund V, Green T. Methyl methacrylate toxicity in rat nasal epithelium:
studies of the mechanism of action and comparisons between species. Toxicology. 2001; 158(3):
109–18. [PubMed: 11275353]
49. Anagnostakos K, Hitzler P, Pape D, Kohn D, Kelm J. Persistence of bacterial growth on antibiotic-
loaded beads: Is it actually a problem? Acta Orthopaedica. 2008; 79:302–7. [PubMed: 18484259]
50. El-Husseiny M, Patel S, MacFarlane RJ, Haddad FS. Biodegradable antibiotic delivery systems. J
Bone Joint Surg Br. 2011; 93(2):151–7. [PubMed: 21282751]
Uskoković
Page 29
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

51. Gogia JS, Meehan JP, Di Cesare PD, Jamali AA. Local antibiotic therapy in osteomyelitis.
Seminar Plastic Surgery. 2009; 23(2):100–7.
52. Nelson CL, Griffin FM, Harrison BH, Cooper RE. In vitro elution characteristics of commercially
and noncommercially prepared antibiotic PMMA beads. Clin Orthop Relat Res. 1992; 284:303–9.
[PubMed: 1395310]
53. Schnettler, R.; Steinau, HU. Septic bone and joint surgery. Stuttgart: Thieme; 2010.
54. Barth RE, Vogely HC, Hoepelman AI, Peters EJ. ’To bead or not to bead? ’ Treatment of
osteomyelitis and prosthetic joint-associated infections with gentamicin bead chains. Int J
Antimicrob Agents. 2011; 38(5):371–5. [PubMed: 21549570]
55. Evans RP, Nelson CL. Gentamicin-impregnated polymethylmethacrylate beads compared with
systemic antibiotic therapy in the treatment of chronic osteomyelitis. Clin Orthop Relat Res. 1993;
295:37–42. [PubMed: 8403668]
56. Blaha JD, Calhoun JH, Nelson CL, Henry SL, Seligson D, Esterhai JL Jr, Heppenstall RB, Mader
J, Evans RP, Wilkins J. Comparison of the clinical efficacy and tolerance of gentamicin PMMA
beads on surgical wire versus combined and systemic therapy for osteomyelitis. Clin Orthop Relat
Res. 1993; 295:8–12. [PubMed: 8403674]
57. Thomas MV, Puleo DA. Calcium sulfate: Properties and clinical applications. J Biomed Mater Res
B Appl Biomater. 2009; 88(2):597–610. [PubMed: 19025981]
58. Jaeblon T. Polymethylmethacrylate: properties and contemporary uses in orthopaedics. J Am Acad
Orthop Surg. 2010; 18(5):297–305. [PubMed: 20435880]
59. Kanellakopoulou K, Galanopoulos I, Soranoglou V, Tsaganos T, Tziortzioti V, Maris I, Papalois
A, Giamarellou H, Giamarellos-Bourboulis EJ. Treatment of experimental osteomyelitis caused by
methicillin-resistant Staphylococcus aureus with a synthetic carrier of calcium sulphate (Stimulan)
releasing moxifloxacin. Int J Antimicrob Agents. 2009; 33(4):354–9. [PubMed: 19097865]
60. Jia WT, Luo SH, Zhang CQ, Wang JQ. In vitro and in vivo efficacies of teicoplanin-loaded
calcium sulfate for treatment of chronic methicillin-resistant Staphylococcus aureus osteomyelitis.
Antimicrob Agents Chemother. 2010; 54(1):170–6. [PubMed: 19917757]
61. Dreesmann H. Ueber knochenplombierung. Beitr Klin Chir. 1892; 9:804–10.
62. Dasmah A, Hallman M, Sennerby L, Rasmusson L. A clinical and histological case series study on
calcium sulfate for maxillary sinus flooraugmentation and delayed placement of dental implants.
Clin Implant Dent Relat Res. 2012; 14(2):259–65. [PubMed: 19843103]
63. Andreana S. A combined approach for treatment of developmental groove associated periodontal
defect. A case report. J Periodontol. 1998; 69:601–7. [PubMed: 9623905]
64. Mittal M, Chandra S, Chandra S. An evaluation of plaster of Paris barriers used under various
materials to repair furcation perforations (in vitro study). J Endod. 1999; 25:385–8. [PubMed:
10530267]
65. Jepegnanam TS, von Schroeder HP. Rapid resorption of calcium sulfate and hardware failure
following corrective radius osteotomy: 2 case reports. J Hand Surg Am. 2012; 37(3):477–80.
[PubMed: 22305728]
66. Ziran BH, Smith WR, Morgan SJ. Use of calcium-based demineralized bone matrix/allograft for
nonunions and posttraumatic reconstruction of the appendicular skeleton: preliminary results and
complications. J Trauma. 2007; 63(6):1324–8. [PubMed: 18212656]
67. Greish YE, Brown PW. Phase evolution during the formation of stoichiometric hydroxyapatite at
37. 4 degrees C. J Biomed Mater Res B Appl Biomater. 2003; 67:632–7. [PubMed: 14528461]
68. Combes C, Miao B, Bareille R, Rey C. Preparation, physical-chemical characterisation and
cytocompatibility of calcium carbonate cements. Biomaterials. 2006; 27(9):1945–54. [PubMed:
16219345]
69. Kurkcu M, Benlidayi ME, Cam B, Sertdemir Y. Anorganic bovine-derived hydroxyapatite vs β-
tricalcium phosphate in sinus augmentation: a comparative histomorphometric study. J Oral
Implantol. 2012; 38(Spec No):519–26. [PubMed: 23072285]
70. Ikenaga M, Hardouin P, Lemaitre J, Andrianjatovo H, Flautre B. Biomechanical characterization
of a biodegradable calcium phosphate hydraulic cement: a comparison with porous biphasic
calcium phosphate ceramics. J Biomed Mater Res. 1998; 40:139–44. [PubMed: 9511108]
Uskoković
Page 30
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

71. Kuemmerle JM, Oberle A, Oechslin C, Bohner M, Frei C, Boecken I, von Rechenberg B.
Assessment of the suitability of a new brushite calcium phosphate cement for cranioplasty - an
experimental study in sheep. J Craniomaxillofac Surg. 2005; 33(1):37–44. [PubMed: 15694148]
72. Heybeli N, Oktar FN, Ozyazgan S, Akkan G, Ozsoy S. Low-cost antibiotic loaded systems for
developing countries. Technol Health Care. 2003; 11(3):207–16. [PubMed: 12775937]
73. McKee MD, Li-Bland EA, Wild LM, Schemitsch EH. A prospective, randomized clinical trial
comparing an antibiotic-impregnated bioabsorbable bone substitute with standard antibiotic-
impregnated cement beads in the treatment of chronic osteomyelitis and infected nonunion. J
Orthop Trauma. 2010; 24(8):483–90. [PubMed: 20657257]
74. Beuerlein MJ, McKee MD. Calcium sulfates: what is the evidence? J Orthop Trauma. 2010; 24
(Suppl 1):S46–51. [PubMed: 20182236]
75. de Klaver PA, Hendriks JG, van Onzenoort HA, Schreurs BW, Touw DJ, Derijks LJ. Gentamicin
serum concentrations in patients with gentamicin-PMMA beads for infected hip joints: a
prospective observational cohort study. Ther Drug Monit. 2012; 34(1):67–71. [PubMed:
22249345]
76. Melamed EA, Peled E. Antibiotic impregnated cement spacer for salvage of diabetic osteomyelitis.
Foot Ankle Int. 2012; 33(3):213–9. [PubMed: 22734283]
77. Fargues PC, Bailly M, Grevillot G. Adsorption of BSA and hemoglobin on hydroxyapatite support:
equilibria and multicomponent dynamic adsorption. Adsorption J Int Adsorption Soc. 1998; 4(1):
5–16.
78. Gagnon P. Improved antibody aggregate removal by hydroxyapatite chromatography in the
presence of polyethylene glycol. J Immun Meth. 2008; 336(2):222–8.
79. Jungbauer A, Hahn R, Deinhofer K, Luo P. Performance and characterization of a nanophased
porous hydroxyapatite for proten chromatography. Biotechnol Bioeng. 2004; 87:364–75.
[PubMed: 15281111]
80. Giovannini R, Freitag R. Comparison of different types of ceramic hydroxyapatite for the
chromatographic separation of plasmid DNA and a recombinant anti-Rhesus D antibody.
Bioseparation. 2001; 9:359–68. [PubMed: 11518239]
81. Yu S, Geng J, Zhou P, Wang J, Chen X, Hu J. New hydroxyapatite monolithic column for DNA
extraction and its application in the purification of Bacillus subtilis crude lysate. J
Chromatography A. 2008; 1183:29–37.
82. Gagnon P, Ng P, Zhen J, Aberin C, He J, Mekosh H, Cummings L, Zaidi S, Richieri R. A ceramic
hydroxyapatite-based purification platform. Simultaneous removal of leached Protein A,
aggregates, DNA, and endotoxins from MABs. BioProcess Int. 2006; 4:50–60.
83. Saito M, Kurosawa Y, Okuyama T. Scanning electron microscopy-based approach to understand
the mechanism underlying the adhesion of dengue viruses on ceramic hydroxyapatite columns.
PLoS One. 2013; 8(1):e53893. [PubMed: 23326529]
84. Hilbrig, F.; Freitag, R. Hydroxyapatite in bioprocessing. In: Subramanian, G., editor.
Biopharmaceutical production technology. Vol. 1. Weinheim: Wiley-VCH; 2012. p. 283-331.
85. Kawasaki T, Niikura M, Kobayashi Y. Fundamental study of hydroxyapatite high-performance
liquid chromatography: II. Experimental analysis on the basis of the general theory of gradient
chromatography. J Chromatography. 1990; 515:91–123.
86. Midy V, Rey C, Bres E, Dard M. Basic fibroblast growth factor adsorption and release properties
of calcium phosphate. J Biomed Mater Res. 1998; 41(3):405–11. [PubMed: 9659610]
87. Zhu XD, Zhang HJ, Fan HS, Li W, Zhang XD. Effect of phase composition and microstructure of
calcium phosphate ceramic particles on protein adsorption. Acta Biomater. 2010; 6(4):1536–41.
[PubMed: 19857608]
88. Chen YL, Zhang XF, Gong YD, Zhao NM, Zeng TY, Song XQ. Conformational changes of
fibrinogen adsorption onto hydroxyapatite and titanium oxide nanoparticles. J Colloid Interface
Sci. 1999; 214(1):38–45. [PubMed: 10328894]
89. Fujii S, Okada M, Sawa H, Furuzono T, Nakamura Y. Hydroxyapatite nanoparticles as particulate
emulsifier: fabrication of hydroxyapatite-coated biodegradable microspheres. Langmuir. 2009;
25(17):9759–66. [PubMed: 19514753]
Uskoković
Page 31
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

90. Uskoković V, Desai TA. Phase composition control of calcium phosphate nanoparticles for tunable
drug delivery kinetics and treatment of osteomyelitis. Part 1: Preparation and drug release. J
Biomed Mat Res A. 2013; 101:1416–26.
91. Uskoković V, Uskoković DP. Nanosized hydroxyapatite and other calcium phosphates: Chemistry
of formation and application as drug and gene delivery agents. J Biomed Mat Res B Appl Biomat.
2011; 96B(1):152–91.
92. Ignjatović NL, Ajduković ZR, Savić VP, Uskoković DP. Size effect of calcium phosphate coated
with poly-DL-lactide- co-glycolide on healing processes in bone reconstruction. J Biomed Mat
Res B Appl Biomat. 2010; 94B:108–17.
93. Boskey AL, Myers ER. Is bone mineral crystalsize significant contributor to “bone quality”? IBMS
BoneKEy-Osteovision. 2004; 1:4–7.
94. Eppell SJ, Tong W, Katz JL, Kuhn L, Glimcher MJ. Shape and size of isolated bone mineralites
measured using atomic force microscopy. J Orthop Res. 2001; 19:1027–34. [PubMed: 11781001]
95. Ishikawa K, Asaoka K. Estimation of ideal mechanical strength and critical porosity of calcium
phosphate cement. J Biomed Mater Res. 1995; 29:1537–43. [PubMed: 8600144]
96. Linhart W, Briem D, Amling M, Rueger JM, Windolf J. Mechanical failure of porous
hydroxyapatite ceramics 7. 5 years after implantation in the proximal tibial. Unfallchirurg. 2004;
107(2):154–7. [PubMed: 14999381]
97. Hofmann MP, Mohammed AR, Perrie Y, Gbureck U, Barralet JE. High-strength resorbable
brushite bone cement with controlled drug-releasing capabilities. Acta Biomater. 2009; 5:43–9.
[PubMed: 18799378]
98. Bohner M, Baumgart F. Theoretical model to determine the effects of geometrical factors on the
resorption of calcium phosphate bone substitutes. Biomaterials. 2004; 25(17):3569–82. [PubMed:
15020131]
99. Liu C, Shen W, Chen J. Solution property of calcium phosphate cement hardening body. Mat
Chem Phys. 1999; 58:78–82.
100. Takagi S, Frukhtbeyn S, Chow LC, Sugawara A, Fujikawa K, Ogata H, Hayashi M, Ogiso B. In
vitro and in vivo characteristics of fluorapatite-forming calcium phosphate cements. J Res Natl
Inst Stand Technol. 2010; 115(4):267–76. [PubMed: 21479080]
101. Bohner M, Brunner TJ, Stark WJ. Controlling the reactivity of calcium phosphate cements. J
Mater Chem. 2008; 18:5669–75.
102. Ambard AJ, Mueninghoff L. Calcium phosphate cement: review of mechanical and biological
properties. J Prosthodont. 2006; 15:321–8. [PubMed: 16958734]
103. Dorozhkin SV. Calcium orthophosphates in nature, biology and medicine. Materials. 2009; 2(2):
399–498.
104. Combes C, Rey C. Amorphous calcium phosphates: synthesis, properties and uses in
biomaterials. Acta Biomat. 2010; 6:3362–78.
105. Magalhaes, MCF.; Marques, PAAP.; Correia, RN. Calcium and magnesium phosphates: normal
and pathological mineralization. In: Königsberger, E.; Königsberger, LC., editors.
Biomineralization – medical aspects of solubility. Chichester: John Wiley & Sons; 2006. p.
71-124.
106. Webb NC. The crystal structure of β-Ca2P2O7. Acta Cryst. 1966; 21:942–8.
107. Bennett RM, Lehr JR, McCarty DJ. Factors affecting the solubility of calcium pyrophosphate
dihydrate crystals. J Clin Invest. 1975; 56(6):1571–9. [PubMed: 423]
108. Dorozhkin S. Self-setting calcium orthophosphate formulations. J Funct Biomat. 2013; 4:209–
311.
109. Confavreux CB. Bone: from a reservoir of minerals to a regulator of energy metabolism. Kidney
Int Suppl. 2011; 121:S14–9. [PubMed: 21346725]
110. Park EK, Lee YE, Choi JY, Oh SH, Shin HI, Kim KH, Kim SY, Kim S. Cellular biocompatibility
and stimulatory effects of calcium metaphosphate on osteoblastic differentiation of human bone
marrow-derived stromal cells. Biomaterials. 2004; 25:3403–11. [PubMed: 15020113]
111. Liu YK, Lu QZ, Pei R, Ji HJ, Zhou GS, Zhao XL, Tang RK, Zhang M. The effect of extracellular
calcium and inorganic phosphate on the growth and osteogenic differentiation of mesenchymal
Uskoković
Page 32
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

stem cells in vitro: implication for bone tissue engineering. Biomed Mater. 2009; 4(2):025004.
[PubMed: 19208939]
112. Mailland M, Waelchli R, Ruat M, Boddeke HG, Seuwen K. Stimulation of cell proliferation by
calcium and a calcimimetic compound. Endocrinology. 1997; 138:3601–5. [PubMed: 9275041]
113. Rainer A, Centola M, Spadaccio C, Gherardi G, Genovese JA, Licoccia S, Trombetta M.
Comparative study of different techniques for the sterilization of poly-L-lactide electrospun
microfibers: effectiveness vs. material degradation. Int J Artif Organs. 2010; 33(2):76–85.
[PubMed: 20306434]
114. Báez LA, Langston C, Givaruangsawat S, McLaughlin R. Evaluation of in vitro serial antibiotic
elution from meropenem-impregnated polymethylmethacrylate beads after ethylene oxide gas
and autoclave sterilization. Vet Comp Orthop Traumatol. 2011; 24(1):39–44. [PubMed:
21103653]
115. França R, Mbeh DA, Samani TD, Le Tien C, Mateescu MA, Yahia L, Sacher E. The effect of
ethylene oxide sterilization on the surface chemistry and in vitro cytotoxicity of several kinds of
chitosan. J Biomed Mater Res B Appl Biomater. 2013; 101(8):1444–55. [PubMed: 24591223]
116. Cottam E, Hukins DWL, Lee K, Hewitt C, Jenkins MJ. Effect of sterilisation by gamma
irradiation on the ability of polycaprolactone (PCL) to act as a scaffold material. Med Eng Phys.
2009; 31:221–6. [PubMed: 18760952]
117. Wang P, Li C, Gong H, Jiang X, Wang H, Li K. Effects of synthesis conditions on the
morphology of hydroxyapatite nanoparticles produced by wet chemical process. Powder Tech.
2010; 203:315–21.
118. Grandjean-Laquerriere A, Laquerriere P, Guenounou M, Laurent-Maquin D, Phillips TM.
Importance of the surface area ratio on cytokines production by human monocytes in vitro
induced by various hydroxyapatite particles. Biomaterials. 2005; 26(15):2361–9. [PubMed:
15585239]
119. Xu Z, Liu C, Wei J, Sun J. Effects of four types of hydroxyapatite nanoparticles with different
nanocrystal morphologies and sizes on apoptosis in rat osteoblasts. J Appl Toxicol. 2012; 32(6):
429–35. [PubMed: 22162110]
120. Huang LCL, Chang HC. Adsorption and immobilization of cytochrome c on nanodiamonds.
Langmuir. 2004; 20(14):5879–84. [PubMed: 16459604]
121. Uskoković V, Batarni SS, Schweicher J, King A, Desai TA. The effect of morphology of calcium
phosphate nanoparticles for sustained release of antibiotics on their antibacterial and osteogenic
performance. ACS Appl Mat Interfaces. 2013; 5(7):2422–31.
122. Webster TJ, Ergun C, Doremus RH, Siegel RW, Bizios R. Enhanced functions of osteoblasts on
nanophase ceramics. Biomaterials. 2000; 21(17):1803–10. [PubMed: 10905463]
123. Webster TJ, Ergun C, Doremus RH, Siegel RW, Bizios R. Enhanced osteoclast-like cell functions
on nanophase ceramics. Biomaterials. 2001; 22(11):1327–33. [PubMed: 11336305]
124. Ziv V, Weiner S. Bone crystal sizes: A comparison of transmission electron microscopic and X-
ray diffraction line width broadening techniques. Connect Tissue Res. 1993; 29:1–11. [PubMed:
8339541]
125. Singh N, Manshian B, Jenkins GJS, Griffiths SM, Williams PM, Maffeis TGG, Wright CJ, Doak
SH. Nanogenotoxicology: the DNA damaging potential of engineered nanomaterials.
Biomaterials. 2009; 30:3891–914. [PubMed: 19427031]
126. Itokazu M, Yang W, Aoki T, Ohara A, Kato N. Synthesis of antibiotic-loaded interporous
hydroxyapatite blocks by vacuum method and in vitro drug release testing. Biomaterials. 1998;
19(7–9):817–9. [PubMed: 9663758]
127. Petrone C, Hall G, Langman M, Filiaggi MJ. Compaction strategies for modifying the drug
delivery capabilities of gelled calcium polyphosphate matrices. Acta Biomater. 2008; 4(2):403–
13. [PubMed: 17997374]
128. Rauschmann MA, Wichelhaus TA, Stirnal V, Dingeldein E, Zichner L, Schnettler R, Alt V.
Nanocrystalline hydroxyapatite and calcium sulphate as biodegradable composite carrier material
for local delivery of antibiotics in bone infections. Biomaterials. 2005; 26(15):2677–84.
[PubMed: 15585271]
Uskoković
Page 33
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

129. Rouahi M, Champion E, Gallet O, Jada A, Anselme K. Physico-chemical characteristics and
protein adsorption potential of hydroxyapatite particles: Influence on in vitro biocompatibility of
ceramics after sintering. Coll Surf B: Biointerfaces. 2006; 47(1):10–9.
130. Kim HM, Himeno T, Kokubo T, Nakamura T. Process and kinetics of bonelike apatite formation
on sintered hydroxyapatite in a simulated body fluid. Biomaterials. 2005; 26(21):4366–73.
[PubMed: 15701365]
131. Vukomanović M, Škapin S, Jančar B, Maksin T, Ignjatović N, Uskoković V, Uskoković D.
Poly(D,L-lactide-co-glycolide)/hydroxyapatite core-shell nanospheres. Part 1: A multifunctional
system for controlled drug delivery. Coll Surf B: Biointerfaces. 2011; 82(2):404–13.
132. Calvente JJ, López-Pérez G, Jurado JM, Andreu R, Molero M, Roldán E. Reorientation of thiols
during 2D self-assembly: interplay between steric and energetic factors. Langmuir. 2010; 26(4):
2914–23. [PubMed: 19764782]
133. Lu X, Jin T, Jin Y, Wu L, Hu B, Tian Y, Fan X. Toxicogenomic analysis of the particle dose- and
size-response relationship of silica particles-induced toxicity in mice. Nanotechnology. 2013;
24(1):015106. [PubMed: 23221170]
134. Downs TR, Crosby ME, Hu T, Kumar S, Sullivan A, Sarlo K, Reeder B, Lynch M, Wagner M,
Mills T, Pfuhler S. Silica nanoparticles administered at the maximum tolerated dose induce
genotoxic effects through an inflammatory reaction while gold nanoparticles do not. Mutat Res.
2012; 14;745(1–2):38–50.
135. Yazdi AS, Guarda G, Riteau N, Drexler SK, Tardivel A, Couillin I, Tschopp J. Nanoparticles
activate the NLR pyrin domain containing 3 (Nlrp3) inflammasome and cause pulmonary
inflammation through release of IL-1α and IL-1β. Proc Natl Acad Sci U S A. 2010; 107(45):
19449–54. [PubMed: 20974980]
136. Bohner, M. Designing ceramics for injectable bone graft substitutes. In: Vernon, B., editor.
Injectable biomaterials: science and applications. Cambridge: Woodhead Publishing; 2011. p.
24-45.
137. Neuendorf RE, Saiz E, Tomsia AP, Ritchie RO. Adhesion between biodegradable polymers and
hydroxyapatite: Relevance to synthetic bone-like materials and tissue engineering scaffolds. Acta
Biomater. 2008; 4(5):1288–96. [PubMed: 18485842]
138. Okada M, Furuzono T. Hydroxylapatite nanoparticles: fabrication methods and medical
applications. Sci Technol Adv Mater. 2012; 13:06413.
139. Jiang JL, Li YF, Fang TL, Zhou J, Li XL, Wang YC, Dong J. Vancomycin-loaded nano-
hydroxyapatite pellets to treat MRSA-induced chronic osteomyelitis with bone defect in rabbits.
Inflamm. 2012; 61(3):207–15.
140. Joosten U, Joist A, Gosheger G, Liljenqvist U, Brandt B, von Eiff C. Effectiveness of
hydroxyapatite-vancomycin bone cement in the treatment of Staphylococcus aureus induced
chronic osteomyelitis. Biomaterials. 2005; 26(25):5251–8. [PubMed: 15792552]
141. Nayak AK, Laha B, Sen KK. Development of hydroxyapatite-ciprofloxacin bone-implants using
“Quality by design”. Acta Pharm. 2011; 61(1):25–36. [PubMed: 21406341]
142. Hamanishi C, Kitamoto K, Tanaka S, Otsuka M, Doi Y, Kitahashi T. A self-setting TTCP-DCPD
apatite cement for release of vancomycin. J Biomed Mater Res. 1996; 33(3):139–43. [PubMed:
8864885]
143. Itokazu M, Matsunaga T, Kumazawa S, Oka M. Treatment of osteomyelitis by antibiotic
impregnated porous hydroxyapatite block. Clin Mater. 1994; 17(4):173–9. [PubMed: 10155678]
144. Tan Y, Wang G, Fan H, Wang X, Lu J, Zhang X. Expression of core binding factor 1 and
osteoblastic markers in C2C12 cells induced by calcium phosphate ceramics in vitro. J Biomed
Mater Res A. 2007; 82(1):152–9. [PubMed: 17269146]
145. Rupani A, Hidalgo-Bastida LA, Rutten F, Dent A, Turner I, Cartmell S. Osteoblast activity on
carbonated hydroxyapatite. J Biomed Mater Res A. 2012; 100(4):1089–96. [PubMed: 22318934]
146. Song JH, Kim JH, Park S, Kang W, Kim HW, Kim HE, Jang JH. Signaling responses of
osteoblast cells to hydroxyapatite: the activation of ERK and SOX9. J Bone Miner Metab. 2008;
26(2):138–42. [PubMed: 18301969]
Uskoković
Page 34
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

147. Zhang W, Tsurushima H, Oyane A, Yazaki Y, Sogo Y, Ito A, Matsumura A. BMP-2 gene-
fibronectin-apatite composite layer enhances bone formation. J Biomed Sci. 2011; 18:62.
[PubMed: 21859498]
148. Bae SE, Choi J, Joung YK, Park K, Han DK. Controlled release of bone morphogenetic protein
(BMP)-2 from nanocomplex incorporated on hydroxyapatite-formed titanium surface. J Control
Release. 2012; 160(3):676–84. [PubMed: 22543042]
149. Lock J, Liu H. Nanomaterials enhance osteogenic differentiation of human mesenchymal stem
cells similar to a short peptide of BMP-7. Int J Nanomedicine. 2011; 6:2769–77. [PubMed:
22114505]
150. Matsushita N, Terai H, Okada T, Nozaki K, Inoue H, Miyamoto S, Takaoka K. A new bone-
inducing biodegradable porous beta-tricalcium phosphate. J Biomed Mater Res A. 2004; 70:450–
8. [PubMed: 15293319]
151. Matsushita N, Terai H, Okada T, Nozaki K, Inoue H, Miyamoto S, Takaoka K. Accelerated repair
of a bone defect with a synthetic biodegradable bone-inducing implant. J Orthop Sci. 2006;
11:505–11. [PubMed: 17013740]
152. Suto M, Nemoto E, Kanaya S, Suzuki R, Tsuchiya M, Shimauchi H. Nanohydroxyapatite
increases BMP-2 expression via a p38 MAP kinase dependent pathway in periodontal ligament
cells. Arch Oral Biol. 2013; 58(8):1021–8. [PubMed: 23518236]
153. Dalby MJ, Gadegaard N, Tare R, Andar A, Riehle MO, Herzyk P, Wilkinson CDW, Oreffo ROC.
The control of human mesenchymal cell differentiation using nanoscale symmetry and disorder.
Nature Materials. 2007; 6:997–1003.
154. Carragee EJ, Hurwitz EL, Weiner BK. A critical review of recombinant human bone
morphogenetic protein-2 trials in spinal surgery: emerging safety concerns and lessons learned.
Spine J. 2011; 11(6):471–91. [PubMed: 21729796]
155. Carragee EJ, Mitsunaga KA, Hurwitz EL, Scuderi GJ. Retrograde ejaculation after anterior
lumbar interbody fusion using rhBMP-2: a cohort controlled study. Spine J. 2011; 11(6):511–6.
[PubMed: 21612985]
156. Woo EJ. Adverse events after recombinant human BMP2 in nonspinal orthopaedic procedures.
Clin Orthop Relat Res. 2013; 471(5):1707–11. [PubMed: 23132207]
157. Majid K, Tseng MD, Baker KC, Reyes-Trocchia A, Herkowitz HN. Biomimetic calcium
phosphate coatings as bone morphogenetic protein delivery systems in spinal fusion. Spine J.
2011; 11(6):560–7. [PubMed: 20097616]
158. Hu YY, Rawal A, Schmidt-Rohr K. Strongly bound citrate stabilizes the apatite nanocrystals in
bone. Proc Natl Acad Sci U S A. 2010; 107(52):22425–9. [PubMed: 21127269]
159. Costello LC, Franklin RB, Reynolds MA, Chellaiah M. The important role of osteoblasts and
citrate production in bone formation: “osteoblast citration” as a new concept for an old
relationship. Open Bone J. 2012; 410.2174/1876525401204010027
160. Gyawali D, Nair P, Kim HKW, Yang J. Citrate-based biodegradable injectable hydrogel
composites for orthopedic applications. Biomat Sci. 2013; 1:52–64.
161. Tencer AF, Woodard PL, Swenson J, Brown KL. Mechanical and bone ingrowth properties of a
polymer-coated, porous, synthetic, coralline hydroxyapatite bone-graft material. Ann N Y Acad
Sci. 1988; 523:157–72. [PubMed: 2898222]
162. Porter AE, Buckland T, Hing K, Best SM, Bonfield W. The structure of the bond between bone
and porous silicon-substituted hydroxyapatite bioceramic implants. J Biomed Mater Res A. 2006;
78(1):25–33. [PubMed: 16596583]
163. del Valle S, Mino N, Munoz F, Gonzalez A, Planell JA, Ginebra MP. In vivo evaluation of an
injectable macroporous calcium phosphate cement. J Mater Sci Mater Med. 2007; 18:353–61.
[PubMed: 17323169]
164. Takagi S, Chow LC. Formation of macropores in calcium phosphate cement implants. J Mater Sci
Mater Med. 2001; 12:3395–404.
165. Wepener I, Richter W, van Papendorp D, Joubert AM. In vitro osteoclast-like and osteoblast
cells’ response to electrospun calcium phosphate biphasic candidate scaffolds for bone tissue
engineering. J Mater Sci: Mater Med. 2012; 23:3029–40. [PubMed: 22965382]
Uskoković
Page 35
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

166. Paris O, Fritz-Popovski G, Van Opdenbosch D, Zollfrank C. Recent progress in the replication of
hierarchical biological tissues. Adv Funct Mat. 2013; 23:4408–22.
167. Marković M, Takagi S, Chow LC. Formation of macropores in calcium phosphate cements
through the use of mannitol crystals. Key Eng Mater. 2001; 192–195:773–6.
168. Xu HHK, Weir MD, Burguera EF, Fraser AM. Injectable and macroporous calcium phosphate
cement scaffold. Biomaterials. 2006; 27:4279–87. [PubMed: 16650891]
169. Fullana SG, Ternet H, Freche M, Lacout JL, Rodriguez F. Controlled release properties and final
macroporosity of a pectin microspheres-calcium phosphate composite bone cement. Acta
Biomater. 2010; 6:2294–300. [PubMed: 19931655]
170. Almirall A, Larrecq G, Delgado JA, Martínez S, Planell JA, Ginebra MP. Fabrication of low
temperature macroporous hydroxyapatite scaffolds by foaming and hydrolysis of an α-TCP
paste. Biomaterials. 2004; 25:3671–80. [PubMed: 15020142]
171. Tas AC. Preparation of porous apatite granules from calcium phosphate cement. J Mater Sci
Mater Med. 2008; 19:2231–9. [PubMed: 18049869]
172. Sarda S, Nilsson M, Balcells M, Fernández E. Influence of surfactant molecules as air-entraining
agent for bone cement macroporosity. J Biomed Mater Res A. 2003; 65A:215–21. [PubMed:
12734815]
173. Wang XP, Ye JD, Li X, Dong H. Production of in-situ macropores in an injectable calcium
phosphate cement by introduction of cetyltrimethyl ammonium bromide. J Mater Sci Mater Med.
2008; 19:3221–5. [PubMed: 18452031]
174. Lopez-Heredia MA, Sariibrahimoglu K, Yang W, Bohner M, Yamashita D, Kunstar A, van
Apeldoorn AA, Bronkhorst EM, Lanao RPF, Leeuwenburgh SCG, Itatani K, Yang F, Salmon P,
Wolke JGC, Jansen JA. Influence of the pore generator on the evolution of the mechanical
properties and the porosity and interconnectivity of a calcium phosphate cement. Acta Biomater.
2012; 8:404–14. [PubMed: 21884833]
175. Lanao RPF, Leeuwenburgh SC, Wolke JG, Jansen JA. In vitro degradation rate of apatitic
calcium phosphate cement with incorporated PLGA microspheres. Acta Biomater. 2011; 7:3459–
68. [PubMed: 21689794]
176. Bohner M. Calcium phosphate emulsions: possible applications. Key Eng Mater. 2011; 192–
195:765–8.
177. Pathi SP, Lin DDW, Dorvee JR, Estroff LA, Fischbach-Teschl C. Hydroxyapatite Nanoparticle-
containing scaffolds for study of breast cancer bone metastasis. Biomaterials. 2011; 32:5112–22.
[PubMed: 21507478]
178. Sionkowska A, Kozłowska J. Properties and modification of porous 3-D collagen/hydroxyapatite
composites. Int J Biol Macromol. 2013; 52:250–9. [PubMed: 23063427]
179. van der Zande M, Walboomers XF, Brännvall M, Olalde B, Jurado MJ, Alava JI, Jansen JA.
Genetic profiling of osteoblast-like cells cultured on a novel bone reconstructive material,
consisting of poly-L-lactide, carbon nanotubes and microhydroxyapatite, in the presence of bone
morphogenetic protein-2. Acta Biomater. 2010; 6(11):4352–60. [PubMed: 20601234]
180. Liao H, Walboomers XF, Habraken WJ, Zhang Z, Li Y, Grijpma DW, Mikos AG, Wolke JG,
Jansen JA. Injectable calcium phosphate cement with PLGA, gelatin and PTMC microspheres in
a rabbit femoral defect. Acta Biomater. 2011; 7(4):1752–9. [PubMed: 21185953]
181. Okazaki M, Sato M, Takahashi J. Space-cutting model of hydroxyapatite. Biomaterials. 1995;
16(1):45–9. [PubMed: 7718692]
182. Gibson IR, Best SM, Bonfield W. Chemical characterization of silicon-substituted
hydroxyapatite. J Biomed Mater Res. 1999; 44(4):422–8. [PubMed: 10397946]
183. Yao F, LeGeros JP, LeGeros RZ. Simultaneous incorporation of carbonate and fluoride in
synthetic apatites: Effect on crystallographic and physico-chemical properties. Acta Biomater.
2009; 5(6):2169–77. [PubMed: 19269268]
184. Wopenka B, Pasteris JD. A mineralogical perspective on the apatite in bone. Mat Sci Eng C.
2005; 25:131–43.
185. Young RA. Biological apatite vs. hydroxyapatite at the atomic level. Clin Orthop Relat Res.
1975; 113:249–62. [PubMed: 1192672]
Uskoković
Page 36
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

186. Knabe C, Houshmand A, Berger G, Ducheyne P, Gildenhaar R, Kranz I, Stiller M. Effect of
rapidly resorbable bone substitute materials on the temporal expression of the osteoblastic
phenotype in vitro. J Biomed Mater Res A. 2008; 15;84(4):856–68.
187. Mann, S. Biomineralization. Oxford: Oxford University Press; 2001. p. 50
188. Okazaki M, LeGeros RZ. Properties of heterogeneous apatites containing magnesium, fluoride,
and carbonate. Adv Dent Res. 1996; 10(2):252–9. [PubMed: 9206345]
189. Abrams SA, Chen Z, Hawthorne KM. Magnesium metabolism in 4 to 8 year old children. J Bone
Miner Res. 2013; 29(1):118–22. [PubMed: 23787702]
190. Landi E, Logroscino G, Proietti L, Tampieri A, Sandri M, Sprio S. Biomimetic Mg-substituted
hydroxyapatite: from synthesis to in vivo behavior. J Mater Sci Mater Med. 2008; 19(1):239–47.
[PubMed: 17597369]
191. Roy M, Bose S. Osteoclastogenesis and osteoclastic resorption of tricalcium phosphate: effect of
strontium and magnesium doping. J Biomed Mater Res A. 2012; 100(9):2450–61. [PubMed:
22566212]
192. Odabasi E, Turan M, Aydin A, Kutlu M. Magnesium, zinc, copper, manganese, and selenium
levels in postmenopausal women with osteoporosis. Can magnesium play a key role in
osteoporosis? Ann Acad Med Singapore. 2008; 37:564–7. [PubMed: 18695768]
193. Aaseth J, Boivin G, Andersen O. Osteoporosis and trace elements - an overview. J Trace Elem
Med Biol. 2012; 26(2–3):149–52. [PubMed: 22575536]
194. Peng Y, Shi K, Wang L, Lu J, Li H, Pan S, Ma C. Characterization of Osterix protein stability and
physiological role in osteoblast differentiation. PLoS One. 2013; 8(2):e56451. [PubMed:
23457570]
195. Brown ED, Chan W, Smith JC Jr. Bone mineralization during a developing zinc deficiency. Proc
Soc Exp Biol Med. 1978; 157:211–4. [PubMed: 622387]
196. Thian ES, Konishi T, Kawanobe Y, Lim PN, Choong C, Ho B, Aizawa M. Zinc-substituted
hydroxyapatite: a biomaterial with enhanced bioactivity and antibacterial properties. J Mater Sci
Mater Med. 2013; 24(2):437–45. [PubMed: 23160913]
197. Rodríguez-Valencia C, López-Álvarez M, Cochón-Cores B, Pereiro I, Serra J, González P. Novel
selenium-doped hydroxyapatite coatings for biomedical applications. J Biomed Mater Res A.
2013; 101(3):853–61. [PubMed: 22968925]
198. Carlisle EM. Proceedings: Silicon as an essential element. Fed Proc. 1974; 33(6):1758–66.
[PubMed: 4275098]
199. Porter AE, Botelho CM, Lopes MA, Santos JD, Best SM, Bonfield W. Ultrastructural comparison
of dissolution and apatite precipitation on hydroxyapatite and silicon-substituted hydroxyapatite
in vitro and in vivo. J Biomed Mater Res A. 2004; 69(4):670–9. [PubMed: 15162409]
200. Li Y, Li Q, Zhu S, Luo E, Li J, Feng G, Liao Y, Hu J. The effect of strontium-substituted
hydroxyapatite coating on implant fixation in ovariectomized rats. Biomaterials. 2010; 31(34):
9006–14. [PubMed: 20800275]
201. Lin K, Xia L, Li H, Jiang X, Pan H, Xu Y, Lu WW, Zhang Z, Chang J. Enhanced osteoporotic
bone regeneration by strontium-substituted calcium silicate bioactive ceramics. Biomaterials.
2013; 34(38):1028–42.
202. Fielding G, Bose S. SiO2 and ZnO dopants in three-dimensionally printed tricalcium phosphate
bone tissue engineering scaffolds enhance osteogenesis and angiogenesis in vivo. Acta Biomater.
2013; 9(11):9137–48. [PubMed: 23871941]
203. Saidak Z, Marie PJ. Strontium signaling: molecular mechanisms and therapeutic implications in
osteoporosis. Pharmacol Ther. 2012; 136(2):216–26. [PubMed: 22820094]
204. Hayakawa S, Kanaya T, Tsuru K, Shirosaki Y, Osaka A, Fujii E, Kawabata K, Gasqueres G,
Bonhomme C, Babonneau F, Jäger C, Kleebe HJ. Heterogeneous structure and in vitro
degradation behavior of wet-chemically derived nanocrystalline silicon-containing
hydroxyapatite particles. Acta Biomater. 2013; 9(1):4856–67. [PubMed: 22922250]
205. Pan HB, Li ZY, Lam WM, Wong JC, Darvell BW, Luk KD, Lu WW. Solubility of strontium-
substituted apatite by solid titration. Acta Biomater. 2009; 5(5):1678–85. [PubMed: 19135423]
Uskoković
Page 37
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

206. Barrio DA, Cattaneo ER, Apezteguia MC, Etcheverry SB. Vanadyl(IV) complexes with
saccharides. Bioactivity in osteoblast-like cells in culture. Can J Physiol Pharmacol. 2006;
84:765–75. [PubMed: 16998540]
207. Pizzala H, Caldarelli S, Eon JG, Rossi AM, San Gil RA, Laurencin D, Smith ME. A solid-state
NMR study of lead and vanadium substitution into hydroxyapatite. J Am Chem Soc. 2009;
131(14):5145–52. [PubMed: 19317471]
208. Hodson ME, Valsami-Jones E, Cotter-Howells JD. Bonemeal additions as a remediation
treatment for metal contaminated soil. Environ Sci Technol. 2000; 34:3501–7.
209. Yang PP, Quan ZW, Li CX, Kang XJ, Lian HZ, Lin J. Bioactive, luminescent and mesoporous
europium-doped hydroxyapatite as a drug carrier. Biomaterials. 2008; 29(32):4341–7. [PubMed:
18715638]
210. Graeve OA, Kanakala R, Madadi A, Williams BC, Glass KC. Luminescence variations in
hydroxyapatites doped with Eu2+ and Eu3+ ions. Biomaterials. 2010; 31:4259–67. [PubMed:
20188413]
211. Albernaz MD, Ospina CA, Rossi AM, Santos-Oliveira R. Radiolabelled nanohydroxyapatite with
99mTc: perspectives to nanoradiopharmaceuticals construction. Artif Cells Nanomed Biotechnol.
2014; 42(2):88–91. [PubMed: 23586417]
212. Sun J, Xie G. Tissue distribution of intravenously administrated hydroxyapatite nanoparticles
labeled with 125I. J Nanosci Nanotechnol. 2011; 11(12):10996–1000. [PubMed: 22409042]
213. Thomas S, Mendes JD, Souza SA, Lorenzato CS, Assi PE, Pacheco LR, Gabriel MB, Bordim A,
Gutfilen B, da Fonseca LM. Radioactive synovectomy with (90) yttrium and (153) samarium
hydroxyapatite in haemophilic joints: preliminary study on radiation safety. Haemophilia. 2013;
19(4):632–6. [PubMed: 23534894]
214. Ignjatović N, Ajduković Z, Savić V, Najman S, Mihailović D, Vasiljević P, Stojanović Z,
Uskoković V, Uskoković D. Nanoparticles of cobalt-substituted hydroxyapatite in regeneration
of mandibular osteoporotic bones. J Mat Sci: Mat Med. 2013; 24(2):343–54.
215. Gloria A, Russo T, D’Amora U, Zeppetelli S, D’Alessandro T, Sandri M, Bañobre-López M,
Piñeiro-Redondo Y, Uhlarz M, Tampieri A, Rivas J, Herrmannsdörfer T, Dediu VA, Ambrosio
L, De Santis R. Magnetic poly(ε-caprolactone)/iron-doped hydroxyapatite nanocomposite
substrates for advanced bone tissue engineering. J R Soc Interface. 2013; 10(80):20120833.
[PubMed: 23303218]
216. Panseri S, Cunha C, D’Alessandro T, Sandri M, Giavaresi G, Marcacci M, Hung CT, Tampieri A.
Intrinsically superparamagnetic Fe-hydroxyapatite nanoparticles positively influence osteoblast-
like cell behavior. J Nanobiotechnology. 2012; 10:32. [PubMed: 22828388]
217. Chandra VS, Baskar G, Suganthi RV, Elayaraja K, Joshy MI, Beaula WS, Mythili R,
Venkatraman G, Kalkura SN. Blood compatibility of iron-doped nanosize hydroxyapatite and its
drug release. ACS Appl Mater Interfaces. 2012; 4(3):1200–10. [PubMed: 22316071]
218. Canullo L, Heinemann F, Gedrange T, Biffar R, Kunert-Keil C. Histological evaluation at
different times after augmentation of extraction sites grafted with a magnesium-enriched
hydroxyapatite: double-blinded randomized controlled trial. Clin Oral Implants Res. 2013; 24(4):
398–406. [PubMed: 22998494]
219. Aina V, Lusvardi G, Annaz B, Gibson IR, Imrie FE, Malavasi G, Menabue L, Cerrato G, Martra
G. Magnesium- and strontium-co-substituted hydroxyapatite: the effects of doped-ions on the
structure and chemico-physical properties. J Mater Sci Mater Med. 2012; 23(12):2867–79.
[PubMed: 23053798]
220. Bock N, Riminucci A, Dionigi C, Russo A, Tampieri A, Landi E, Goranov VA. A novel route in
bone tissue engineering: magnetic biomimetic scaffolds. Acta Biomaterialia. 2010; 6(3):786–96.
[PubMed: 19788946]
221. Tampieri A, D’Alessandro T, Sandri M, Sprio S, Landi E, Bertinetti L, Panseri S, Pepponi G,
Goettlicher J, Bañobre-López M, Rivas J. Intrinsic magnetism and hyperthermia in bioactive Fe-
doped hydroxyapatite. Acta Biomater. 2012; 8(2):843–51. [PubMed: 22005331]
222. Yamamoto H, Shibata Y, Tachikawa T, Miyazaki T. In vivo performance of two different
hydroxyapatite coatings on titanium prepared by discharging in electrolytes. J Biomed Mater Res
B Appl Biomater. 2006; 78(1):211–4. [PubMed: 16362960]
Uskoković
Page 38
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

223. Ohashi N, Nakamura M, Nagai A, Tanaka Y, Sekijima Y, Yamashita K. Comparison of
hydroxyapatite with carbonate apatite in osteoclastic cell resorptive activity. Key Eng Mat. 2007;
361–363:1039–42.
224. Ramchandani M, Robinson D. In vitro and in vivo release of ciprofloxacin from PLGA 50:50
implants. J Control Release. 1998; 54(2):167–75. [PubMed: 9724903]
225. Orhan Z, Cevher E, Yildiz A, Ahiskali R, Sensoy D, Mülazimoğlu L. Biodegradable
microspherical implants containing teicoplanin for the treatment of methicillin-resistant
Staphylococcus aureus osteomyelitis. Arch Orthop Trauma Surg. 2010; 130(1):135–42.
[PubMed: 19434413]
226. Koort JK, Makinen TJ, Suokas E, Veiranto M, Jalava J, Tormala P, Aro HT. Sustained release of
ciprofloxacin from an osteoconductive poly(DL)-lactide implant. Acta Orthop. 2008; 79(2):295–
301. [PubMed: 18484258]
227. Sayin B, Caliş S, Atilla B, Marangoz S, Hincal AA. Implantation of vancomycin microspheres in
blend with human/rabbit bone grafts to infected bone defects. J Microencapsul. 2006; 23(5):553–
66. [PubMed: 16980276]
228. Le Ray AM, Gautier H, Laty MK, Daculsi G, Merle C, Jacqueline C, Hamel A, Caillon J. In vitro
and in vivo bactericidal activities of vancomycin dispersed in porous biodegradable poly(epsilon-
caprolactone) microparticles. Antimicrob Agents Chemother. 2005; 49(7):3025–7. [PubMed:
15980391]
229. Xiong MH, Bao Y, Yang XZ, Zhu YH, Wang J. Delivery of antibiotics with polymeric particles.
Adv Drug Deliv Rev. 2014 Feb 16. pii:S0169–409X(14)00024–6. 10.1016/j.addr.2014.02.002
230. Vilar G, Tulla-Puche J, Albericio F. Polymers and drug delivery systems. Curr Drug Deliv. 2012;
9(4):367–94. [PubMed: 22640038]
231. Sabir MI, Xu X. A review of biodegradable polymeric materials for bone tissue engineering
applications. J Mater Sci. 2009; 44:5713–24.
232. Cameron, RE.; Kamvari-Moghaddam, A. Synthetic bioresorbable polymers. In: Buchanan, F.,
editor. Degradation rate of bioresorbable materials. Cambridge: Woodhead; 2008. p. 43-66.
233. Deepa G, Thulasidasan AK, Anto RJ, Pillai JJ, Kumar GS. Cross-linked acrylic hydrogel for the
controlled delivery of hydrophobic drugs in cancer therapy. Int J Nanomedicine. 2012; 7:4077–
88. [PubMed: 22888244]
234. Kluin OS, van der Mei HC, Busscher HJ, Neut D. Biodegradable vs non-biodegradable antibiotic
delivery devices in the treatment of osteomyelitis. Expert Opin Drug Deliv. 2013; 10(3):341–51.
[PubMed: 23289645]
235. Neut D, Kluin OS, Crielaard BJ, van der Mei HC, Busscher HJ, Grijpma DW. A biodegradable
antibiotic delivery system based on poly-(trimethylene carbonate) for the treatment of
osteomyelitis. Acta Orthop. 2009; 80(5):514–9. [PubMed: 19916681]
236. Lang W. A new method for the removal of chronic bone suppuration. Report on the removal of
osteomyelitic and multi-infected tuberculous fistulae by filling the bone cavity with polyamide
fibers. Z Orthop Ihre Grenzgeb. 1969; 106(2):393–413. [PubMed: 4240700]
237. Gurselt I, Yagmurlu F, Korkusuz F, Hasirci V. In vitro antibiotic release from poly(3-
hydroxybutyrate-co-3-hydroxyvalerate) rods. J Microencapsul. 2002; 19(2):153–64. [PubMed:
11837970]
238. Chen L, Wang H, Wang J, Chen M, Shang L. Ofloxacin-delivery system of a polyanhydride and
polylactide blend used in the treatment of bone infection. J Biomed Mater Res B Appl Biomater.
2007; 83(2):589–95. [PubMed: 17410574]
239. Brin YS, Nyska A, Domb AJ, Golenser J, Mizrahi B, Nyska M. Biocompatibility of a polymeric
implant for the treatment of osteomyelitis. J Biomater Sci Polym Ed. 2009; 20(7–8):1081–90.
[PubMed: 19454170]
240. Li LC, Deng J, Stephens D. Polyanhydride implant for antibiotic delivery - from the bench to the
clinic. Adv Drug Deliv Rev. 2002; 54(7):963–86. [PubMed: 12384317]
241. Moskowitz JS, Blaisse MR, Samuel RE, Hsu HP, Harris MB, Martin SD, Lee JC, Spector M,
Hammond PT. The effectiveness of the controlled release of gentamicin from polyelectrolyte
multilayers in the treatment of Staphylococcus aureus infection in a rabbit bone model.
Biomaterials. 2010; 31(23):6019–30. [PubMed: 20488534]
Uskoković
Page 39
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

242. Wei G, Kotoura Y, Oka M, Yamamuro T, Wada R, Hyon SH, Ikada Y. A bioabsorbable delivery
system for antibiotic treatment of osteomyelitis: the use of lactic acid oligomer as a carrier. J
Bone Joint Surg [Br]. 1991; 73-B:246–52.
243. Garvin K, Feschuk C. Polylactide-polyglycolide antibiotic implants. Clin Orthop Relat Res. 2005;
437:105–10. [PubMed: 16056034]
244. Koort JK, Makinen TJ, Suokas E, Veiranto M, Jalava J, Tormala P, Aro HT. Sustained release of
ciprofloxacin from an osteoconductive poly(DL)-lactide implant. Acta Orthop. 2008; 79(2):295–
301. [PubMed: 18484258]
245. Bostman OM. Osteotic changes accompanying degradation of absorbable fracture fixation
implants. J Bone Joint Surg. 1991; 73(4):679–82.
246. Bostman O, Hirvensalo E, Mikinen J, Rokkanen P. Foreign-body reaction to fracture fixation of
biodegradable synthetic polymers. J Bone Joint Surg. 1990; 72(4):592–6.
247. Solheim E, Sudmann B, Bang G, Sudmann E. Biocompatibility and effect on osteogenesis of
poly(ortho ester) compared to poly(DL-lactic acid). J Biomed Mater Res. 2000; 49(2):257–63.
[PubMed: 10571914]
248. Tiainen J, Soini Y, Suokas E, Veiranto M, Törmälä P, Waris T, Ashammakhi N. Tissue reactions
to bioabsorbable ciprofloxacin-releasing polylactide-polyglycolide 80/20 screws in rabbits’
cranial bone. J Mater Sci Mater Med. 2006; 17(12):1315–22. [PubMed: 17143763]
249. Plachokova A, Link D, van den Dolder J, van den Beucken J, Jansen J. Bone regenerative
properties of injectable PGLA-CaP composite with TGF-beta1 in a rat augmentation model. J
Tissue Eng Regen Med. 2007; 1(6):457–64. [PubMed: 18265419]
250. Lemaire S, Van Bambeke F, Pierard D, Appelbaum PC, Tulkens PM. Activity of fusidic acid
against extracellular and intracellular Staphylococcus aureus: influence of pH and comparison
with linezolid and clindamycin. Clin Infect Dis. 2011; 52(Suppl 7):S493–503. [PubMed:
21546626]
251. Middleton JC, Tripton AJ. Synthetic biodegradable polymers as orthopaedic devices.
Biomaterials. 2000; 21:2334–46.
252. Ouédraogo M, Semdé R, Somé IT, Traoré-Ouédraogo R, Guissou IP, Henschel V, Dubois J,
Amighi K, Evrard B. Monoolein-water liquid crystalline gels of gentamicin as bioresorbable
implants for the local treatment of chronic osteomyelitis: in vitro characterization. Drug Dev Ind
Pharm. 2008; 34(7):753–60. [PubMed: 18627115]
253. Xiong MH, Li YJ, Bao Y, Yang XZ, Hu B, Wang J. Bacteria-responsive multifunctional nanogel
for targeted antibiotic delivery. Adv Mater. 2012; 24(46):6175–80. [PubMed: 22961974]
254. Semdé R, Gondi RF, Sombié BC, Yaméogo BG, Ouédraogo M. Effect of hydroxyapatite on the
physicochemical characteristics of a gentamicin-loaded monoolein gel intended to treat chronic
osteomyelitis. J Adv Pharm Technol Res. 2012; 3(2):100–5. [PubMed: 22837957]
255. Zhou J, Fang T, Wang Y, Dong J. The controlled release of vancomycin in gelatin/β-TCP
composite scaffolds. J Biomed Mater Res A. 2012; 100(9):2295–301. [PubMed: 22499502]
256. Hasegawa M, Sudo A, Komlev VS, Barinov SM, Uchida A. High release of antibiotic from a
novel hydroxyapatite with bimodal pore size distribution. J Biomed Mater Res B Appl Biomater.
2004; 15;70(2):332–9.
257. Della Porta G, Adami R, Del Gaudio P, Prota L, Aquino R, Reverchon E. Albumin/gentamicin
microspheres produced by supercritical assisted atomization: optimization of size, drug loading
and release. J Pharm Sci. 2010; 99(11):4720–9. [PubMed: 20845468]
258. Haswani DK, Nettey H, Oettinger C, D’Souza MJ. Formulation, characterization and
pharmacokinetic evaluation of gentamicin sulphate loaded albumin microspheres. J
Microencapsul. 2006; 23(8):875–86. [PubMed: 17390629]
259. Aquino RP, Auriemma G, Mencherini T, Russo P, Porta A, Adami R, Liparoti S, Della Porta G,
Reverchon E, Del Gaudio P. Design and production of gentamicin/dextrans microparticles by
supercritical assisted atomisation for the treatment of wound bacterial infections. Int J Pharm.
2013; 440(2):188–94. [PubMed: 22917746]
260. Weszl M, Skaliczki G, Cselenyák A, Kiss L, Major T, Schandl K, Bognár E, Stadler G,
Peterbauer A, Csönge L, Lacza Z. Freeze-dried human serum albumin improves the adherence
Uskoković
Page 40
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

and proliferation of mesenchymal stem cells on mineralized human bone allografts. J Orthop
Res. 2012; 30(3):489–96. [PubMed: 22371968]
261. Skaliczki G, Schandl K, Weszl M, Major T, Kovács M, Skaliczki J, Szendröi M, Dobó-Nagy C,
Lacza Z. Serum albumin enhances bone healing in a nonunion femoral defect model in rats: a
computer tomography micromorphometry study. Int Orthop. 2013; 37(4):741–5. [PubMed:
23318937]
262. Kuechle DK, Landon GC, Musher DM, Noble PC. Elution of vancomycin, daptomycin, and
amikacin from acrylic bone cement. Clin Orthop Relat Res. 1991; (264):302–8. [PubMed:
1705191]
263. Zhou J, Fang T, Wen J, Shao Z, Dong J. Silk coating on poly(ε-caprolactone) microspheres for
the delayed release of vancomycin. J Microencapsul. 2011; 28(2):99–107. [PubMed: 21265711]
264. Ziv K, Nuhn H, Ben-Haim Y, Sasportas LS, Kempen PJ, Niedringhaus TP, Hrynyk M, Sinclair R,
Barron AE, Gambhir SS. A tunable silk-alginate hydrogel scaffold for stem cell culture and
transplantation. Biomaterials. 2014; 35:3736–43. [PubMed: 24484675]
265. Cevher E, Orhan Z, Mülazimoğlu L, Sensoy D, Alper M, Yildiz A, Ozsoy Y. Characterization of
biodegradable chitosan microspheres containing vancomycin and treatment of experimental
osteomyelitis caused by methicillin-resistant Staphylococcus aureus with prepared microspheres.
Int J Pharm. 2006; 317(2):127–35. [PubMed: 16624509]
266. Aimin C, Chunlin H, Juliang B, Tinyin Z, Zhichao D. Antibiotic loaded chitosan bar. An in vitro,
in vivo study of a possible treatment for osteomyelitis. Clin Orthop Relat Res. 1999; (366):239–
47. [PubMed: 10627741]
267. Uskoković V, Desai TA. In vitro analysis of nanoparticulate hydroxyapatite/chitosan composites
as potential drug delivery platforms for the sustained release of antibiotics in the treatment of
osteomyelitis. J Pharm Sci. 2014; 103(2):567–79. [PubMed: 24382825]
268. Sandolo C, Péchiné S, Le Monnier A, Hoys S, Janoir C, Coviello T, Alhaique F, Collignon A,
Fattal E, Tsapis N. Encapsulation of Cwp84 into pectin beads for oral vaccination against
Clostridium difficile. Eur J Pharm Biopharm. 2011; 79(3):566–73. [PubMed: 21664462]
269. Désévaux C, Lenaerts V, Girard C, Dubreuil P. Characterization of crosslinked high amylose
starch matrix implants. 2. In vivo release of ciprofloxacin. J Control Release. 2002; 82(1):95–
103. [PubMed: 12106980]
270. Ueng SW, Lee MS, Lin SS, Chan EC, Liu SJ. Development of a biodegradable alginate carrier
system for antibiotics and bone cells. J Orthop Res. 2007; 25(1):62–72. [PubMed: 17019681]
271. Matsuno H, Yudoh K, Hashimoto M, Himeda Y, Miyoshi T, Yoshida K, Kano S. A new
antibacterial carrier of hyaluronic acid gel. J Orthop Sci. 2006; 11(5):497–504. [PubMed:
17013739]
272. Orhan Z, Cevher E, Mülazimoglu L, Gürcan D, Alper M, Araman A, Ozsoy Y. The preparation
of ciprofloxacin hydrochloride-loaded chitosan and pectin microspheres: their evaluation in an
animal osteomyelitis model. J Bone Joint Surg Br. 2006; 88(2):270–5. [PubMed: 16434537]
273. Huneault LM, Lussier B, Dubreuil P, Chouinard L, Désévaux C. Prevention and treatment of
experimental osteomyelitis in dogs with ciprofloxacin-loaded crosslinked high amylose starch
implants. J Orthop Res. 2004; 22(6):1351–7. [PubMed: 15475220]
274. Xing J, Hou T, Luobu B, Luo F, Chen Q, Li Z, Jin H, Xu J. Anti-infection tissue engineering
construct treating osteomyelitis in rabbit tibia. Tissue Eng Part A. 2013; 19(1–2):255–63.
[PubMed: 22861191]
275. Knaepler H. Local application of gentamicin-containing collagen implant in the prophylaxis and
treatment of surgical site infection in orthopaedic surgery. Int J Surg. 2012; 10(Suppl 1):S15–20.
[PubMed: 22659311]
276. Mendel V, Simanowski HJ, Scholz HC, Heymann H. Therapy with gentamicin-PMMA beads,
gentamicin-collagen sponge, and cefazolin for experimental osteomyelitis due to Staphylococcus
aureus in rats. Arch Orthop Trauma Surg. 2005; 125(6):363–8. [PubMed: 15864679]
277. Chaudhary S, Sen RK, Saini UC, Soni A, Gahlot N, Singh D. Use of gentamicin-loaded collagen
sponge in internal fixation of open fractures. Chin J Traumatol. 2011; 14(4):209–14. [PubMed:
21801664]
Uskoković
Page 41
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

278. Kanellakopoulou K, Giamarellos-Bourboulis EJ. Carrier systems for the local delivery of
antibiotics in bone infections. Drugs. 2000; 59(6):1223–32. [PubMed: 10882159]
279. Kawalec-Carroll JS, Hetherington VJ, Dockery DS, Shive C, Targoni OS, Lehmann PV, Nadler
D, Prins D. Immunogenicity of unprocessed and photooxidized bovine and human osteochondral
grafts in collagen-sensitive mice. BMC Musculoskelet Disord. 2006; 7:32. [PubMed: 16545115]
280. Browne S, Zeugolis DI, Pandit A. Collagen: finding a solution for the source. Tissue Eng Part A.
2013; 19(13–14):1491–4. [PubMed: 23240852]
281. Patino MG, Neiders ME, Andreana S, Noble B, Cohen RE. Collagen as an implantable material
in medicine and dentistry. J Oral Implantol. 2002; 28(5):220–5. [PubMed: 12498470]
282. Park SN, Kim JK, Suh H. Evaluation of antibiotic-loaded collagen-hyaluronic acid matrix as a
skin substitute. Biomaterials. 2004; 25(17):3689–98. [PubMed: 15020144]
283. Cui F, Li G, Huang J, Zhang J, Lu M, Lu W, Huan J, Huang Q. Development of chitosan-
collagen hydrogel incorporated with lysostaphin (CCHL) burn dressing with anti-methicillin-
resistant Staphylococcus aureus and promotion wound healing properties. Drug Deliv. 2011;
18(3):173–80. [PubMed: 20726806]
284. Lynn AK, Yannas IV, Bonfield W. Antigenicity and immunogenicity of collagen. J Biomed
Mater Res B: Appl Biomater. 2004; 71:343–54. [PubMed: 15386396]
285. Akturk O, Tezcaner A, Bilgili H, Deveci MS, Gecit MR, Keskin D. Evaluation of sericin/collagen
membranes as prospective wound dressing biomaterial. J Biosci Bioeng. 2011; 112(3):279–88.
[PubMed: 21697006]
286. Ipsen T, Jørgensen PS, Damholt V, Tørholm C. Gentamicin-collagen sponge for local
applications. 10 cases of chronic osteomyelitis followed for 1 year. Acta Orthop Scand. 1991;
62(6):592–4. [PubMed: 1767654]
287. Sørensen TS, Sørensen AI, Merser S. Rapid release of gentamicin from collagen sponge. In vitro
comparison with plastic beads. Acta Orthop Scand. 1990; 61(4):353–6. [PubMed: 2402990]
288. Hou J, Wang J, Cao L, Qian Z, Xing W, Lu J, Liu C. Segmental bone regeneration using rhB-
MP-2-loaded collagen/chitosan microspheres composite scaffold in a rabbit model. Biomed Mat.
2012; 7:035002.
289. Kundu B, Nandi SK, Dasgupta S, Datta S, Mukherjee P, Roy S, Singh AK, Mandal TK, Das P,
Bhattacharya R, Basu D. Macro-to-micro porous special bioactive glass and ceftriaxone-
sulbactam composite drug delivery system for treatment of chronic osteomyelitis: an
investigation through in vitro and in vivo animal trial. J Mater Sci Mater Med. 2011; 22(3):705–
20. [PubMed: 21221731]
290. Xie Z, Liu X, Jia W, Zhang C, Huang W, Wang J. Treatment of osteomyelitis and repair of bone
defect by degradable bioactive borate glass releasing vancomycin. J Control Release. 2009;
139:118–26. [PubMed: 19545593]
291. Zhang X, Jia W, Gu Y, Xiao W, Liu X, Wang D, Zhang C, Huang W, Rahaman MN, Day DE,
Zhou N. Teicoplanin-loaded borate bioactive glass implants for treating chronic bone infection in
a rabbit tibia osteomyelitis model. Biomaterials. 2010; 31(22):5865–74. [PubMed: 20434766]
292. Thanyaphoo S, Kaewsrichan J. Synthesis and evaluation of novel glass ceramics as drug delivery
systems in osteomyelitis. J Pharm Sci. 2012; 101(8):2870–82. [PubMed: 22674208]
293. Valappil SP, Pickup DM, Carroll DL, Hope CK, Pratten J, Newport RJ, Smith ME, Wilson M,
Knowles JC. Effect of silver content on the structure and antibacterial activity of silver-doped
phosphate-based glasses. Antimicrob Agents Chemother. 2007; 51(12):4453–61. [PubMed:
17908949]
294. Aughenbaugh W, Radin S, Ducheyne P. Silica sol-gel for the controlled release of antibiotics. II.
The effect of synthesis parameters on the in vitro release kinetics of vanomycin. J Biomed Mater
Res. 2001; 57(3):321–6. [PubMed: 11584809]
295. Pavelić, K.; Hadžija, M. Medical applications of zeolites. In: Auerbach, SM.; Carrado, KA.;
Dutta, PK., editors. Handbook of zeolite science and technology. New York: Marcel Dekker;
2005. p. 1460
296. Rhodes CJ. Properties and applications of zeolites. Sci Prog. 2010; 93(3):223–84. [PubMed:
21047018]
Uskoković
Page 42
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

297. Banu J, Varela E, Guerra JM, Halade G, Williams PJ, Bahadur AN, Hanaoka K, Fernandes G.
Dietary coral calcium and zeolite protects bone in a mouse model for postmenopausal bone loss.
Nutr Res. 2012; 32(12):965–75. [PubMed: 23244542]
298. Schütze N, Oursler MJ, Nolan J, Riggs BL, Spelsberg TC. Zeolite A inhibits osteoclast-mediated
bone resorption in vitro. J Cell Biochem. 1995; 58(1):39–46. [PubMed: 7642721]
299. Harrison RG, Fox OD, Meng MO, Dalley NK, Barbour LJ. Cation control of pore and channel
size in cage-based metal-organic porous materials. Inorg Chem. 2002; 41(4):838–43. [PubMed:
11849084]
300. Chen Y, Lykourinou V, Vetromile C, Hoang T, Ming LJ, Larsen R, Ma S. How can proteins enter
the interior of a MOF? Investigation of cytochrome c translocation into a MOF consisting of
mesoporous cages with microporous windows. J Am Chem Soc. 2012; 134:13188–91. [PubMed:
22862180]
301. Vallet-Regí M, Balas F, Arcos D. Mesoporous materials for drug delivery. Angew Chem Int Ed
Engl. 2007; 46(40):7548–58. [PubMed: 17854012]
302. Hanke M, Arslan HK, Bauer S, Zybaylo O, Christophis C, Gliemann H, Rosenhahn A, Wöll C.
The biocompatibility of metal-organic framework coatings: an investigation on the stability of
SURMOFs with regard to water and selected cell culture media. Langmuir. 2012; 28(17):6877–
84. [PubMed: 22471238]
303. Seil JT, Webster TJ. Antimicrobial applications of nanotechnology: methods and literature. Int J
Nanomedicine. 2012; 7:2767–81. [PubMed: 22745541]
304. Wilkinson LJ, White RJ, Chipman JK. Silver and nanoparticles of silver in wound dressings: a
review of efficacy and safety. J Wound Care. 2011; 20(11):543–9. [PubMed: 22240850]
305. Monteiro DR, Gorup LF, Takamiya AS, Ruvollo-Filho AC, de Camargo ER, Barbosa DB. The
growing importance of materials that prevent microbial adhesion: antimicrobial effect of medical
devices containing silver. Int J Antimicrob Agents. 2009; 34(2):103–10. [PubMed: 19339161]
306. Becker RO. Silver ions in the treatment of local infections. Met Based Drugs. 1999; 6:311–4.
[PubMed: 18475906]
307. Gulati K, Aw MS, Losic D. Drug-eluting Ti wires with titania nanotube arrays for bone fixation
and reduced bone infection. Nanoscale Res Lett. 2011; 6:571. [PubMed: 22039969]
308. Popat KC, Eltgroth M, Latempa TJ, Grimes CA, Desai TA. Decreased Staphylococcus epidermis
adhesion and increased osteoblast functionality on antibiotic-loaded titania nanotubes.
Biomaterials. 2007; 28(32):4880–8. [PubMed: 17697708]
309. Peng L, Mendelsohn AD, LaTempa TJ, Yoriya S, Grimes CA, Desai TA. Long-term small
molecule and protein elution from TiO2 nanotubes. Nano Lett. 2009; 9(5):1932–6. [PubMed:
19323554]
310. Harris LG, Meredith DO, Eschbach L, Richards RG. Staphylococcus aureus adhesion to standard
micro-rough and electropolished implant materials. J Mater Sci Mater Med. 2007; 18(6):1151–6.
[PubMed: 17268867]
311. Gristina AG. Biomaterial-centered infection: microbial adhesion versus tissue integration.
Science. 1987; 237:1588–95. [PubMed: 3629258]
312. Kirkham J, Brookes SJ, Shore RC, Wood SR, Smith DA, Zhang J, Chen H, Robinson C.
Physicochemical properties of crystal surfaces in matrix-mineral interactions during mammalian
biomineralisation. Curr Opin Coll Interface Sci. 2002; 7:124–32.
313. Müller B. Tailoring biocompatibility: benefitting patients. Mat Today. 2010; 13(4):58.
314. Sisti KE, Piattelli A, Guastaldi AC, Queiroz TP, de Rossi R. Nondecalcified histologic study of
bone response to titanium implants topographically modified by laser with and without
hydroxyapatite coating. Int J Periodontics Restorative Dent. 2013; 33(5):689–96. [PubMed:
23998165]
315. Hirota M, Hayakawa T, Yoshinari M, Ametani A, Shima T, Monden Y, Ozawa T, Sato M,
Koyama C, Tamai N, Iwai T, Tohnai I. Hydroxyapatite coating for titanium fibre mesh scaffold
enhances osteoblast activity and bone tissue formation. Int J Oral Maxillofac Surg. 2012; 41(10):
1304–9. [PubMed: 22513355]
Uskoković
Page 43
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

316. Murakami A, Arimoto T, Suzuki D, Iwai-Yoshida M, Otsuka F, Shibata Y, Igarashi T, Kamijo R,
Miyazaki T. Antimicrobial and osteogenic properties of a hydrophilic-modified nanoscale
hydroxyapatite coating on titanium. Nanomedicine. 2012; 8(3):374–82. [PubMed: 21782779]
317. Zavgorodniy AV, Borrero-López O, Hoffman M, Legeros RZ, Rohanizadeh R. Characterization
of the chemically deposited hydroxyapatite coating on a titanium substrate. J Mater Sci Mater
Med. 2011; 22(1):1–9. [PubMed: 21052792]
318. Uskoković V, Hoover C, Vukomanović M, Uskoković DP, Desai TA. Osteogenic and
antimicrobial nanoparticulate calcium phosphate and/or poly-lactide-co-glycolide powders for
the treatment of osteomyelitis. Mat Sci Eng C: Mat Bio Appl. 2013; 33(6):3362–73.
319. Tamazawa G, Ito A, Miyai T, Matsuno T, Kitahara K, Sogo Y, Kimishima K, Satoh T.
Gatifloxacine-loaded PLGA and β-tricalcium phosphate composite for treating osteomyelitis.
Dent Mater J. 2011; 30(3):264–73. [PubMed: 21597226]
320. Fang T, Wen J, Zhou J, Shao Z, Dong J. Poly (ε-caprolactone) coating delays vancomycin
delivery from porous chitosan/β-tricalcium phosphate composites. J Biomed Mater Res B Appl
Biomater. 2012; 100B(7):1803–11. [PubMed: 22807376]
321. Sokolova V, Knuschke T, Buer J, Westendorf AM, Epple M. Quantitative determination of the
composition of multi-shell calcium phosphate-oligonucleotide nanoparticles and their application
for the activation of dendritic cells. Acta Biomater. 2011; 7(11):4029–36. [PubMed: 21784177]
322. Cheng J, Teply BA, Sherifi I, Sung J, Luther G, Gu FX, Levy-Nissenbaum E, Radovic-Moreno
AF, Langer R, Farokhzad OC. Formulation of functionalized PLGA PEG nanoparticles for in
vivo targeted drug delivery. Biomaterials. 2007; 28:869–76. [PubMed: 17055572]
323. Wang RE, Costanza F, Niu Y, Wu H, Hu Y, Hang W, Sun Y, Cai J. Development of self-
immolative dendrimers for drug delivery and sensing. J Control Release. 2012; 159(2):154–63.
[PubMed: 22155555]
324. Mochalin VN, Neitzel I, Etzold BJ, Peterson A, Palmese G, Gogotsi Y. Covalent incorporation of
aminated nanodiamond into an epoxy polymer network. ACS Nano. 2011; 5(9):7494–502.
[PubMed: 21830823]
325. Zhang Z, Ma R, Shi L. Cooperative macromolecular self-assembly toward polymeric assemblies
with multiple and bioactive functions. Acc Chem Res. 2014; 47(4):1426–37. [PubMed:
24694280]
326. Naito K, Obayashi O, Mogami A, Itoi A, Kaneko K. Fracture of the calcium phosphate bone
cement which used to enchondroma of the hand, a case report. Eur J Orthop Surg Traumatol.
2008; 18:405–8.
327. Rezwan K, Chen Q, Blaker J, Boccaccini A. Biodegradable and bioactive porous polymer/
inorganic composite scaffolds for bone tissue engineering. Biomaterials. 2006; 27(18):3413–31.
[PubMed: 16504284]
328. Bucholz RW. Nonallograft osteoconductive bone graft substitutes. Clin Orthop Relat Res. 2002;
395:44–52. [PubMed: 11937865]
329. Alge DL, Bennett J, Treasure T, Voytik-Harbin S, Goebel WS, Chu TMG. Poly(propylene
fumarate) reinforced dicalcium phosphate dihydrate cement composites for bone tissue
engineering. J Biomed Mater Res A. 2012; 100A:1792–802. [PubMed: 22489012]
330. Fernández E, Sarda S, Hamcerencu M, Vlad MD, Gel M, Valls S, Torres R, López J. High-
strength apatitic cement by modification with superplasticizers. Biomaterials. 2005; 26:2289–96.
[PubMed: 15585231]
331. Fujishiro Y, Takahashi K, Sato T. Preparation and compressive strength of α-tricalcium
phosphate/gelatin gel composite cement. J Biomed Mater Res. 2001; 54:525–30. [PubMed:
11426597]
332. dos Santos LA, Carrodeguas RG, Boschi AO, de Arruda ACF. Dual-setting calcium phosphate
cement modified with ammonium polyacrylate. Artif Organs. 2003; 27:412–8. [PubMed:
12752199]
333. Mickiewicz RA, Mayes AM, Knaack D. Polymer – calcium phosphate cement composites for
bone substitutes. J Biomed Mater Res. 2002; 61:581–92. [PubMed: 12115448]
334. Miyazaki K, Horibe T, Antonucci JM, Takagi S, Chow LC. Polymeric calcium phosphate
cements: setting reaction modifiers. Dent Mater. 1993; 9:46–50. [PubMed: 8299870]
Uskoković
Page 44
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

335. Komath M, Varma HK. Development of a fully injectable calcium phosphate cement for
orthopedic and dental applications. Bull Mater Sci. 2003; 26:415–22.
336. Ajduković Z, Ignjatović N, Petrović, Uskoković D. Substitution of osteoporotic alveolar bone by
biphasic calcium phosphate/poly-DL-lactide-co-glycolide biomaterials. J Biomaterials Appl.
2007; 21(3):317–28.
337. Ruhé PQ, Hedberg EL, Padron NT, Spauwen PH, Jansen JA, Mikos AG. Biocompatibility and
degradation of poly(DL-lactic-co-glycolic acid)/calcium phosphate cement composites. J Biomed
Mater Res A. 2005; 74(4):533–44. [PubMed: 16041795]
338. Félix Lanao RP, Leeuwenburgh SC, Wolke JG, Jansen JA. Bone response to fast-degrading,
injectable calcium phosphate cements containing PLGA microparticles. Biomaterials. 2011;
32(34):8839–47. [PubMed: 21871661]
339. Link DP, van den Dolder J, Jurgens WJ, Wolke JG, Jansen JA. Mechanical evaluation of
implanted calcium phosphate cement incorporated with PLGA microparticles. Biomaterials.
2006; 27(28):4941–7. [PubMed: 16759694]
340. Shi P, Zuo Y, Li X, Zou Q, Liu H, Zhang L, Li Y, Morsi YS. Gentamicin-impregnated chitosan/
nanohydroxyapatite/ethyl cellulose microspheres granules for chronic osteomyelitis therapy. J
Biomed Mater Res A. 2010; 93(3):1020–31. [PubMed: 19743510]
341. Romeo HE, Fanovich MA. Functionalized bridged silsesquioxane-based nanostructured
microspheres: performance as novel drug-delivery devices in bone tissue-related applications. J
Biomater Appl. 2012; 26(8):987–1012. [PubMed: 21123279]
342. Fang T, Wen J, Zhou J, Shao Z, Dong J. Poly (ε-caprolactone) coating delays vancomycin
delivery from porous chitosan/β-tricalcium phosphate composites. J Biomed Mater Res B Appl
Biomater. 2012; 100B(7):1803–11. [PubMed: 22807376]
343. Miki T, Imai Y. Osteoinductive potential of freeze-dried, biodegradable, poly (glycolic acid-co-
lactic acid) disks incorporated with bone morphogenetic protein in skull defects of rats. Int J Oral
Maxillofac Surg. 1996; 25(5):402–6. [PubMed: 8961028]
344. Jensen T, Baas J, Dolathshahi-Pirouz A, Jacobsen T, Singh G, Nygaard JV, Foss M, Bechtold J,
Bünger C, Besenbacher F, Søballe K. Osteopontin functionalization of hydroxyapatite
nanoparticles in a PDLLA matrix promotes bone formation. J Biomed Mater Res A. 2011; 99(1):
94–101. [PubMed: 21800419]
345. Ji Y, Xu GP, Zhang ZP, Xia JJ, Yan JL, Pan SH. BMP-2/PLGA delayed-release microspheres
composite graft, selection of bone particulate diameters, and prevention of aseptic inflammation
for bone tissue engineering. Ann Biomed Eng. 2010; 38(3):632–9. [PubMed: 20049636]
346. Yoon SJ, Kim SH, Ha HJ, Ko YK, So JW, Kim MS, Yang YI, Khang G, Rhee JM, Lee HB.
Reduction of inflammatory reaction of poly(d,l-lactic-co-glycolic acid) using demineralized bone
particles. Tissue Eng Part A. 2008; 14(4):539–47. [PubMed: 18352826]
347. Gyenes T, Torma V, Gyarmati B, Zrínyi M. Synthesis and swelling properties of novel pH-
sensitive poly(aspartic acid) gels. Acta Biomater. 2008; 4(3):733–44. [PubMed: 18280800]
348. Jeong B, Kim SW, Bae YH. Thermosensitive sol gel reversible hydrogels. Adv Drug Deliv Rev.
2012; 64:154–62.
349. Peng KT, Chen CF, Chu IM, Li YM, Hsu WH, Hsu RW, Chang PJ. Treatment of osteomyelitis
with teicoplanin-encapsulated biodegradable thermosensitive hydrogel nanoparticles.
Biomaterials. 2010; 31(19):5227–36. [PubMed: 20381140]
350. Ma T, Shang BC, Tang H, Zhou TH, Xu GL, Li HL, Chen QH, Xu YQ. Nano-hydroxyapatite/
chitosan/konjac glucomannan scaffolds loaded with cationic liposomal vancomycin: preparation,
in vitro release and activity against Staphylococcus aureus biofilms. J BiomaterSci Polym Ed.
2011; 22(12):1669–81.
351. Zhu CT, Xu YQ, Shi J, Li J, Ding J. Liposome combined porous beta-TCP scaffold: preparation,
characterization, and anti-biofilm activity. Drug Deliv. 17(6):391. [PubMed: 20429845]
352. Pagliari F, Mandoli C, Forte G, Magnani E, Pagliari S, Nardone G, Licoccia S, Minieri M, Di
Nardo P, Traversa E. Cerium oxide nanoparticles protect cardiac progenitor cells from oxidative
stress. ACS Nano. 2012; 6(5):3767–75. [PubMed: 22524692]
Uskoković
Page 45
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

353. Stevanović M, Savić J, Jordović B, Uskoković D. Fabrication, in vitro degradation and the release
behaviours of poly(DL-lactide-co-glycolide) nanospheres containing ascorbic acid. Coll Surf B:
Biointerfaces. 2007; 59:215–23.
354. Schwegmann H, Feitz AJ, Frimmel FH. Influence of the zeta potential on the sorption and
toxicity of iron oxide nanoparticles on S. cerevisiae and E. coli. J Coll Interface Sci. 2010;
347(1):43–8.
355. Uskoković V. Dynamic light scattering and microelectrophoresis: main prospects and limitations.
J Disp Sci Tech. 2012; 33(12):1762–86.
356. Beech JA. Bioelectric potential gradients may initiate cell cycling: ELF and zeta potential
gradients may mimic this effect. Bioelectromagnetics. 1997; 18(5):341–8. [PubMed: 9209715]
357. Uskoković V. Theoretical and practical aspects of colloid science and self-assembly phenomena
revisited. Rev Chem Eng. 2007; 23(5):301–72.
358. Silvestrini MT, Yin D, Coppes VG, Mann P, Martin AJ, Larson PS, Starr PA, Gupta N, Panter
SS, Desai TA, Lim DA. Radially branched deployment for more efficient cell transplantation at
the scale of the human brain. Stereotact Funct Neurosurg. 2013; 91(2):92–103. [PubMed:
23343609]
359. Stepensky D, Kleinberg L, Hoffman A. Bone as an effect compartment: models for uptake and
release of drugs. Clin Pharmacokinet. 2003; 42(10):863–81. [PubMed: 12885262]
360. Bessa PC, Casal M, Reis RL. Bone morphogenetic proteins in tissue engineering: the road from
laboratory to clinic, part II (BMP delivery). J Tissue Eng Regen Med. 2008; 2:81–96. [PubMed:
18383454]
361. Mistry AS, Mikos AG. Tissue engineering strategies for bone regeneration. Adv Biochem Engin/
Biotechnol. 2005; 94:1–22.
362. Ma X, Zhao Y, Liang XJ. Theranostic nanoparticles engineered for clinic and pharmaceutics. Acc
Chem Res. 2011; 44(10):1114–22. [PubMed: 21732606]
363. Mehta M, Schmidt-Bleek K, Duda GN, Mooney DJ. Biomaterial delivery of morphogens to
mimic the natural healing cascade in bone. Adv Drug Deliv Rev. 2012; 64(12):1257–76.
[PubMed: 22626978]
364. Nair SP, Meghji S, Wilson M, Reddi K, White P, Henderson B. Bacterially induced bone
destruction: mechanisms and misconceptions. Infect Immun. 1996; 64(7):2371–80. [PubMed:
8698454]
365. Stallmann HP, Faber C, Nieuw Amerongen AV, Wuisman PI. Antimicrobial peptides: review of
their application in musculoskeletal infections. Injury. 2006; 37(Suppl 2):S34–40. [PubMed:
16651070]
366. Niu Y, Wang RE, Wu H, Cai J. Recent development of small antimicrobial peptidomimetics.
Future Med Chem. 2012; 4(14):1853–62. [PubMed: 23043481]
367. Girard PP, Cavalcanti-Adam EA, Kemkemer R, Spatz JP. Cellular chemomechanics at interfaces:
sensing, integration and response. Soft Matter. 2007; 3:307–26.
368. Panahifar A, Mahmoudi M, Doschak MR. Synthesis and in vitro evaluation of bone-seeking
superparamagnetic iron oxide nanoparticles as contrast agents for imaging bone metabolic
activity. ACS Appl Mater Interfaces. 2013; 5:5219–26. [PubMed: 23672213]
369. Yewle JN, Puleo DA, Bachas LG. Enhanced affinity bifunctional bisphosphonates for targeted
delivery of therapeutic agents to bone. Bioconjug Chem. 2011; 22(12):2496–506. [PubMed:
22073906]
370. Das S, Crockett JC. Safety issues with bisphosphonate therapy for osteoporosis. Drug Des Devel
Ther. 2013; 7:435–48.
371. Verron E, Bouler JM. Is bisphosphonate therapy compromised by the emergence of adverse bone
disorders? Drug Discov Today. 2014; 19(3):312–9. [PubMed: 23974069]
372. Suresh E, Pazianas M, Abrahamsen B. Safety issues with bisphosphonate therapy for
osteoporosis. Rheumatology (Oxford). 2014; 53:19–31. [PubMed: 23838024]
373. Wahlig, H. In: van Rens, TJG.; Kayser, FH., editors. Gentamicin-PMMA beads, a drug delivery
system: basic results; Local antibiotic treatment in osteomyelitis and soft-tissue infections:
Proceedings of a symposium; Amsterdam. October 25, 1980; Amstewrdam: Excerpta Medica;
1981.
Uskoković
Page 46
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

374. Nehilla BJ, Allen PG, Desai TA. Surfactant-free, drug-quantum-dot coloaded poly(lactide-co-
glycolide) nanoparticles: towards multifunctional nanoparticles. ACS Nano. 2008; 2(3):528–44.
375. Guo Y, Shi DL, Lian J, Dong ZY, Wang W, Cho HS, Liu GK, Wang LM, Ewing RC. Quantum
dot conjugated hydroxylapatite nanoparticles for in vivo imaging. Nanotechnology. 2008; 19(17):
175102. [PubMed: 21825660]
376. Wu P, Yan XP. Doped quantum dots for chemo/biosensing and bioimaging. Chem Soc Rev.
2013; 42(12):5489–521. [PubMed: 23525298]
377. Zhang Y, Yang J. Design strategies for fluorescent biodegradable polymeric biomaterials. J Mater
Chem B Mater Biol Med. 2013; 1(2):132–48. [PubMed: 23710326]
378. Yang J, Zhang Y, Gautam S, Liu L, Dey J, Chen W, Mason RP, Serrano CA, Schug KA, Tang L.
Development of aliphatic biodegradable photoluminescent polymers. Proc Natl Acad Sci U S A.
2009; 106(25):10086–91. [PubMed: 19506254]
379. Al-Sokanee ZN, Toabi AA, Al-Assadi MJ, Alassadi EA. The drug release study of ceftriaxone
from porous hydroxyapatite scaffolds. AAPS PharmSciTech. 2009; 10(3):772–9. [PubMed:
19499343]
380. Nilsson M, Fernández E, Sarda S, Lidgren L, Planell JA. Characterization of a novel calcium
phosphate/sulphate bone cement. J Biomed Mater Res. 2002; 61:600–7. [PubMed: 12115450]
381. Constantz BR, Barr BM, Ison IC, Fulmer MT, Baker J, McKinney LA, Goodman SB,
Gunasekaren S, Delaney DC, Ross J, Poser RD. Histological, chemical and crystallographic
analysis of four calcium phosphate cements in different rabbit osseous sites. J Biomed Mater Res
B Appl Biomater. 1998; 43:451–61.
382. Habraken WJEM, de Jonge LT, Wolke JGC, Yubao L, Mikos AG, Jansen JA. Introduction of
gelatin microspheres into an injectable calcium phosphate cement. J Biomed Mater Res A. 2008;
87A:643–55. [PubMed: 18189298]
383. El-Ghannam A, Ahmed K, Omran M. Nanoporous delivery system to treat osteomyelitis and
regenerate bone: gentamicin release kinetics and bactericidal effect. J Biomed Mater Res B Appl
Biomater. 2005; 73(2):277–84. [PubMed: 15674827]
384. Gultepe E, Nagesha D, Sridhar S, Amiji M. Nanoporous inorganic membranes or coatings for
sustained drug delivery in implantable devices. Adv Drug Deliv Rev. 2010; 62(3):305–15.
[PubMed: 19922749]
385. Lindner M, Bergmann C, Telle R, Fischer H. Calcium phosphate scaffolds mimicking the
gradient architecture of native long bones. J Biomed Mater Res A. 2013; 26:1–8.
386. Zhu Y, Wan Y, Zhang J, Yin D, Cheng W. Manufacture of layered collagen/chitosan-
polycaprolactone scaffolds with biomimetic microarchitecture. Coll Surf B: Biointerfaces. 2014;
113:352–60.
387. Andala DM, Shin SH, Lee HY, Bishop KJ. Templated synthesis of amphiphilic nanoparticles at
the liquid-liquid interface. ACS Nano. 2012; 6(2):1044–50. [PubMed: 22214288]
388. Marković S, Uskoković D. Barium titanate stannate functionally graded materials: Choosing of
the Ti/Sn concentration gradient and the influence of the gradient on electrical properties. Ceram
Trans. 2010; 221:3–17.
389. Hou T, Xu J, Li Q, Feng J, Zen L. In vitro evaluation of a fibrin gel antibiotic delivery system
containing mesenchymal stem cells and vancomycin alginate beads for treating bone infections
and facilitating bone formation. Tissue Eng Part A. 2008; 14(7):1173–82. [PubMed: 18593356]
390. Ueng SW, Yuan LJ, Lin SS, Liu SJ, Chan EC, Chen KT, Lee MS. In vitro and in vivo analysis of
a biodegradable poly(lactide-co-glycolide) copolymer capsule and collagen composite system for
antibiotics and bone cells delivery. J Trauma. 2011; 70(6):1503–9. [PubMed: 21336203]
391. Liu J, Tan Y, Zhang H, Zhang Y, Zu P, Chen J, Poh YC, Tang K, Wang N, Huang B. Soft fibrin
gels promote selection and growth of tumorigenic cells. Nature Materials. 2012; 11(8):734–41.
392. Stevanović M, Savanović I, Uskoković V, Škapin SD, Bračko I, Jovanović U, Uskoković D. A
new, simple, green and one-pot four-component synthesis of bare and poly(α, γ, L-glutamic acid)
capped silver nanoparticles. Coll Polym Sci. 2011; 290(3):221–31.
393. Stevanović M, Uskoković V, Filipović M, Škapin SD, Uskoković DP. Composite PLGA/
AgNpPGA/AscH nanospheres with combined osteoinductive, antioxidative and antimicrobial
activities. ACS Appl Mat Interfaces. 2013; 5(18):9034–42.
Uskoković
Page 47
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

394. Monopoli MP, Aberg C, Salvati A, Dawson KA. Biomolecular coronas provide the biological
identity of nanosized materials. Nature Nanotech. 2012; 7:779–86.
395. Prapainop K, Witter DP, Wentworth P Jr. A chemical approach for cell-specific targeting of
nanomaterials: small-molecule-initiated misfolding of nanoparticle corona proteins. J Am Chem
Soc. 2012; 134:4100–3. [PubMed: 22339401]
396. Ignjatović N, Uskoković V, Ajduković Z, Uskoković D. Multifunctional hydroxyapatite and
poly(D,L-lactide-co-glycolide) nanoparticles for the local delivery of cholecalciferol. Mat Sci
Eng C: Bio Appl. 2013; 33(2):943–50.
397. Narducci P, Nicolin V. Differentiation of activated monocytes into osteoclast-like cells on a
hydroxya-patite substrate: an in vitro study. Ann Anatomy. 2009; 191(4):349–55.
398. Buijs PRA, van Eijck CHJ, Hofland LJ, Fouchier RAM, van den Hoogen BG. Different responses
of human pancreatic adenocarcinoma cell lines to oncolytic Newcastle disease virus infection.
Cancer Gene Ther. 2014; 21:24–30. [PubMed: 24384773]
399. Lin HP, Lin CY, Hsiao PH, Wang HD, Sheng Jiang S, Hsu JM, Jim WT, Chen M, Kung HJ,
Chuu CP. Difference in protein expression profile and chemotherapy drugs response of different
progression stages of LNCaP sublines and other human prostate cancer cells. PLoS One. 2013;
8(12):e82625. [PubMed: 24349321]
400. Correia AL, Bissell MJ. The tumor microenvironment is a dominant force in multidrug resistance.
Drug Resist Updat. 2012; 15(1–2):39–49. [PubMed: 22335920]
401. Scheman L, Janota M, Lewin P. The production of experimental osteomyelitis: premilinary
report. J Am Med Assoc. 1941; 177:1525–9.
402. Spagnolo N, Greco F, Rossi A. Chronic Staphylococcal osteomyelitis: a new experimental rat
model. Infect Immun. 1993; 61:5225–30. [PubMed: 8225597]
403. Gracia E, Lacleriga A, Monzon M. Application of a rat osteomyelitis model to compare in vivo
and in vitro the antibiotic efficacy against bacteria with high capacity to form biofilms. J Surg
Res. 1998; 79:146–53. [PubMed: 9758730]
404. Brown KV, Walker JA, Cortez DS, Murray CK, Wenke JC. Earlier debridement and antibiotic
administration decrease infection. J Surg Orthop Adv. 2010; 19:18–22. [PubMed: 20371002]
405. Nair MB, Kretlow JD, Mikos AG, Kasper FK. Infection and tissue engineering in segmental bone
defects - a mini review. Curr Opin Biotechnol. 2011; 22(5):721–5. [PubMed: 21354782]
406. Patel M, Rojavin Y, Jamali AA, Wasielewski SJ, Salgado CJ. Animal models for the study of
osteomyelitis. Semin Plast Surg. 2009; 23(2):148–54. [PubMed: 20567737]
407. Perlroth J, Kuo M, Tan J, Bayer AS, Miller LG. Adjunctive use of rifampin for the treatment of
Staphylococcus aureus infections: a systematic review of the literature. Arch Intern Med. 2008;
168(8):805–19. [PubMed: 18443255]
408. Oh SH, Kang SG, Lee JH. Degradation behaviour of hydrophilized PLGA scaffolds prepared by
melt-moulding particulate-leaching method: comparison with control hydrophobic one. J Mat
Sci: Mat Med. 2006; 17:131–7.
409. Tomlins, P. Influence of porous structure on bioresorbability: tissue engineering scaffolds. In:
Buchanan, F., editor. Degradation rate of bioresorbable materials. Cambridge: Woodhead; 2008.
p. 234-264.
410. Silver IA, Murrills RJ, Etherington DJ. Microelectrode studies on the acid microenvironment
beneath adherent macrophages and osteoclasts. Exp Cell Res. 1988; 175(2):266–76. [PubMed:
3360056]
411. Burg, KJL.; Orr, DE. An overview of bioresorbable materials. In: Buchanan, F., editor.
Degradation rate of bioresorbable materials. Cambridge: Woodhead; 2008. p. 3-18.
412. Driessens FCM. Physiology of hard tissues in comparison with the solubility of synthetic calcium
phosphates. Ann New York Academy Sci. 1988; 523:131–6.
413. Driessens, FCM.; Verbeeck, RMH. Relation between physicochemical solubility and
biodegradability of calcium phosphates. In: de Putter, C.; de Lange, GL.; de Groot, K.; Lee,
AJC., editors. Implant materials in biofunction. Amsterdam: Elsevier; 1988. p. 105-111.
414. Bohner, M. Bioresorbable ceramics. In: Buchanan, F., editor. Degradation rate of bioresorbable
materials. Cambridge: Woodhead; 2008. p. 95-114.
Uskoković
Page 48
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

415. Suzuki O, Nakamura M, Miyasaki Y, Kagayama M, Sakurai M. Bone formation on synthetic
precursors of hydroxyapatite. Tohoku J Exp Med. 1991; 164:37–50. [PubMed: 1926145]
416. Bohner M, Theiss F, Apelt D, Hirsiger W, Houriet R, Rizzoli G, Gnos E, Frei C, Auer JA, von
Rechenberg B. Compositional changes of a dicalcium phosphate dihydrate cement after
implantation in sheep. Biomaterials. 2003; 24:3463–74. [PubMed: 12809775]
417. Penel G, Leroy N, Van Landuyt P, Flautre B, Hardouin P, Lemaître J, Leroy G. Raman
microspectrometry studies of brushite cement: in vivo evolution in a sheep model. Bone. 1999;
25:81S–84S. [PubMed: 10458282]
418. Elliott, JC. Structure and chemistry of the apatites and other calcium orthophosphates.
Amsterdam: Elsevier; 1994.
419. Mabilleau, G.; Sabokbar, A. In vitro biological test methods to evaluate bioresorbability. In:
Buchanan, F., editor. Degradation rate of bioresorbable materials. Cambridge: Woodhead; 2008.
p. 145-160.
420. Wright GD. The origins of antibiotic resistance. Handb Exp Pharmacol. 2012; 211:13–30.
[PubMed: 23090593]
421. Yarboro SR, Baum EJ, Dahners LE. Locally administered antibiotics for prophylaxis against
surgical wound infection. An in vivo study. J Bone Joint Surg Am. 2007; 89(5):929–33.
[PubMed: 17473127]
422. Aarts, HJM.; Guerra, B.; Malorny, B. Molecular methods for detection of antibiotic resistance. In:
Aarestrup, FM., editor. Antimicrobial resistance in bacteria of animal origin. Washington:
American Society for Microbiology Press; 2006. p. 55
423. Bohner M, Lemaître J, van Landuyt P, Zambelli P, Merkle HP, Gander B. Gentamicin- loaded
hydraulic calcium orthophosphate bone cement as antibiotic delivery system. J Pharm Sci. 1997;
86:565–72. [PubMed: 9145380]
424. Chen DW, Hsu YH, Liao JY, Liu SJ, Chen JK, Ueng SW. Sustainable release of vancomycin,
gentamicin and lidocaine from novel electrospun sandwich-structured PLGA/collagen
nanofibrous membranes. Int J Pharm. 2012; 430(1–2):335–41. [PubMed: 22521880]
425. Schnettler, R.; Steinau, HU. Septic bone and joint surgery. Stuttgart: Thieme; 2010.
426. Gbureck U, Vorndran E, Muller FA, Barralet JE. Low temperature direct 3D printed bioceramics
and biocomposites as drug release matrices. J Control Release. 2007; 122:173–80. [PubMed:
17655962]
427. Penner MJ, Masri BA, Duncan CP. Elution characteristics of vancomycin and tobramycin
combined in acrylic bone-cement. J Arthroplasty. 1996; 11(8):939–44. [PubMed: 8986572]
428. Mani G, Torres N, Oh S. Paclitaxel delivery from cobalt-chromium alloy surfaces using self-
assembled monolayers. Biointerphases. 2011; 6:33–42. [PubMed: 21721838]
429. Perry AC, Rouse MS, Khaliq Y, Piper KE, Hanssen AD, Osmon DR, Steckelberg JM, Patel R.
Antimicrobial release kinetics from polymethylmethacrylate in a novel continuous flow chamber.
Clin Orthop Relat Res. 2002; 403:49–53. [PubMed: 12360007]
430. Chan, JCY.; Burugapalli, K.; Kelly, JL.; Pandit, AS. Influence of clinical application on
bioresorbability: host response. In: Buchanan, F., editor. Degradation rate of bioresorbable
materials. Cambridge: Wood-head; 2008. p. 265-318.
431. Beumer GJ, van Blitterswijk CA, Ponec M. Degradative behaviour of polymeric matrices in (sub)
dermal and muscle tissue of the rat: a quantitative study. Biomaterials. 1994; 15:551–9.
[PubMed: 7918908]
432. Bhatia S, Shalaby SW, Powers DL, Lancaster RL, Ferguson RL. The effect of site of implantation
and animal age on properties of polydioxanone pins. J Biomater Sci Poly Ed. 1994; 6:435–46.
433. Claes LE. Mechanical characterization of biodegradable implants. Clin Mater. 1992; 10:41–6.
[PubMed: 10171202]
434. Hu P, Tirelli N. Scavenging ROS: superoxide dismutase/catalase mimetics by the use of an
oxidation-sensitive nanocarrier/enzyme conjugate. Bioconjug Chem. 2012; 23(3):438–49.
[PubMed: 22292618]
435. Parfitt AM. What is the normal rate of bone remodeling? Bone. 2004; 35:1–3. [PubMed:
15207734]
Uskoković
Page 49
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

436. Almeida RA, Matthews KR, Cifrian E, Guidry AJ, Oliver SP. Staphylococcus aureus invasion of
bovine mammary cells. J Dairy Sci. 1996; 79:1021–6. [PubMed: 8827466]
437. Bayles KW, Wesson CA, Liou LW, Fox LK, Bohach GA, Trumble WR. Intracellular
Staphylococcus aureus escapes the endosome and induces apoptosis in epithelial cells. Infect
Immun. 1998; 66:336–42. [PubMed: 9423876]
438. Ellington JK, Harris M, Webb L, Smith B, Smith T, Tan K, Hudson M. Intracellular
Staphylococcus aures: a mechanism for the indolence of osteomyelitis. J Bone Joint Surg. 2003;
85B:918–21.
439. Ahmed S, Meghji S, Williams RJ, Henderson B, Brock JH, Nair SP. Staphylococcus aureus
fibronectin binding proteins are essential for internalization by osteoblasts but do not account for
differences in intracellular levels of bacteria. Infect Immun. 2001; 69(5):2872–7. [PubMed:
11292701]
440. Bost KL, Ramp WK, Nicholson NC, Bento JL, Marriott I, Hudson MC. Staphylococcus aureus
infection of mouse or human osteoblasts induces high levels of interleukin-6 and interleukin-12
production. J Infect Dis. 1999; 180(6):1912–20. [PubMed: 10558948]
441. Hassan MA, Ahmed IS, Campbell P, Kondo T. Enhanced gene transfection using calcium
phosphate co-precipitates and low-intensity pulsed ultrasound. Eur J Pharm Sci. 2012; 47(4):
768–73. [PubMed: 22921720]
442. Cao X, Deng W, Wei Y, Su W, Yang Y, Wei Y, Yu J, Xu X. Encapsulation of plasmid DNA in
calcium phosphate nanoparticles: stem cell uptake and gene transfer efficiency. Int J
Nanomedicine. 2011; 6:3335–49. [PubMed: 22229000]
443. Elangovan S, Jain S, Tsai PC, Margolis HC, Amiji M. Nano-sized calcium phosphate particles for
periodontal gene therapy. J Periodontol. 2013; 84(1):117–25. [PubMed: 22414259]
444. Uskoković V, Desai TA. Simultaneous bactericidal and osteogenic effect of nanoparticulate
calcium phosphate powders loaded with clindamycin on osteoblasts infected with
Staphylococcus aureus. Mat Sci Eng C: Mat Bio Appl. 2014; 37:210–22.
445. Pillai R, Somayaji SN, Rabinovich M, Hudson MC, Gonsalves KE. Nafcillin-loaded PLGA
nanoparticles for treatment of osteomyelitis. Biomed Mater. 2008; 3:034114. [PubMed:
18708713]
446. Dee KC, Bizios R. Mini-review: Proactive biomaterials and bone tissue engineering. Biotechnol
Bioeng. 1996; 50(4):438–42. [PubMed: 18626993]
447. Sergent JA, Paget V, Chevillard S. Toxicity and genotoxicity of nano-SiO2 on human epithelial
intestinal HT-29 cell line. Ann Occup Hyg. 2012; 56(5):622–30. [PubMed: 22378843]
448. Nouri A, Castro R, Santos JL, Fernandes C, Rodrigues J, Tomás H. Calcium phosphate-mediated
gene delivery using simulated body fluid (SBF). Int J Pharm. 2012; 434(1–2):199–208.
[PubMed: 22664458]
449. dos Santos T, Varela J, Lynch I, Salvati A, Dawson KA. Quantitative assessment of the
comparative nanoparticle-uptake efficiency of a range of cell lines. Small. 2011; 7(23):3341–9.
[PubMed: 22009913]
450. Murakami T, Murakami H, Ramp WK, Hudson MC, Nousiainen MT. Calcium hydroxide
ameliorates tobramycin toxicity in cultured chick tibiae. Bone. 1997; 21(5):411–8. [PubMed:
9356734]
451. Uskoković V. Challenges for the modern science in its descend towards nano scale. Current
Nanosci. 2009; 5(3):372–89.
452. Sheldrake, R. Morphic resonance: the nature of formative causation. Rochester: Park Street Press;
2009. p. 96-97.
453. Uskoković V, Desai TA. Phase composition control of calcium phosphate nanoparticles for
tunable drug delivery kinetics and treatment of osteomyelitis. Part 2: antibacterial and
osteoblastic response. J Biomed Mat Res Part A. 2013; 101:1427–36.
454. DeLongchamp, D. Structure measurements for organic photovoltaics manufacturing. Materials
Research Society Conference: Symposium JJ; San Francisco, CA. April 4, 2013;
455. Uskoković V. Insights into morphological nature of precipitation of cholesterol. Steroids. 2008;
73:356–69. [PubMed: 18215404]
Uskoković
Page 50
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

456. Horbett, TA. Adsorbed proteins on biomaterials. In: Ratner, BD.; Hoffman, AS.; Schoen, FJ.;
Lemons, JE., editors. Biomaterials science. Amsterdam: Academic Press; 2012. p. 394-408.
457. Malaiya A, Vyas SP. Preparation and characterization of indomethacin magnetic nanoparticles. J
Microencapsul. 1998; 5:243–53. [PubMed: 3199309]
458. Debuigne F, Jeunieau L, Wiame M, Nagy JB. Synthesis of organic nanoparticles in different W/O
microemulsions. Langmuir. 2000; 16:7605–11.
459. Madsen HEL. Influence of magnetic field. Growth. 1995; 152:94–100.
460. Reitas AMBF, Andgraf FJGL, Yvlt JN, Iuletti MG. Influence of magnetic field in the kinetics of
crystallization of diamagnetic and paramagnetic inorganic salts. Crystal Res Tech. 1999;
34:1239–44.
461. Baker A, Tóth A, Horváth D, Walkush J, Ali AS, Morgan W, Kukovecz A, Pantaleone JJ,
Maselko J. Precipitation pattern formation in the copper(II) oxalate system with gravity flow and
axial symmetry. J Phys Chem A. 2009; 113(29):8243–8. [PubMed: 19569701]
462. Stiles PJ, Fletcher DF, Morris I. The effect of gravity on the rates of simple liquid-state reactions
in a small, unstirred cylindrical vessel. Part II. Phys Chem Chem Phys. 2001; 3:3651–5.
463. Saxena R, Pan G, McDonald JM. Osteoblast and osteoclast differentiation in modeled
microgravity. Ann N Y Acad Sci. 2007; 1116:494–8. [PubMed: 17656572]
464. Zayzafoon M, Gathings WE, McDonald JM. Modeled microgravity inhibits osteogenic
differentiation of human mesenchymal stem cells and increases adipogenesis. Endocrinology.
2004; 145(5):2421–32. [PubMed: 14749352]
465. Huang Y, Dai ZQ, Ling SK, Zhang HY, Wan YM, Li YH. Gravity, a regulation factor in the
differentiation of rat bone marrow mesenchymal stem cells. J Biomed Sci. 2009; 16:87.
[PubMed: 19772591]
466. Muralithran G, Ramesh S. The effects of sintering temperature on the properties of
hydroxyapatite. Ceram Int. 2000; 26:221–30.
467. Oliver CR, Polsen ES, Meshot ER, Tawfick S, Park SJ, Bedewy M, Hart AJ. Statistical analysis
of variation in laboratory growth of carbon nanotube forests and recommendations for improved
consistency. ACS Nano. 2013; 7(4):3565–80. [PubMed: 23464741]
468. Lacruz RS, Hacia JG, Bromage TG, Boyde A, Lei Y, Xu Y, Miller JD, Paine ML, Snead ML.
The circadian clock modulates enamel development. J Biol Rhythms. 2012; 27(3):237–45.
[PubMed: 22653892]
469. Canham LT, Reeves CL, Loni A, Houlton MR, Newey JP, Simons AJ, Cox TI. Calcium
phosphate nucleation on porous silicon: factors influencing kinetics in acellular simulated body
fluids. Thin Solid Films. 1997; 297:304–7.
470. Kokubo T, Takadama H. How useful is SBF in predicting in vivo bone bioactivity? Biomaterials.
2006; 27:2907–15. [PubMed: 16448693]
471. Uskoković V. Composites comprising cholesterol and carboxymethyl cellulose. Coll Surf B:
Biointerfaces. 2008; 61:250–61.
472. Bunker CE, Harruff BA, Pathak P, Payzant A, Allard LF, Sun YP. Formation of cadmium sulfide
nanoparticles in reverse micelles: extreme sensitivity to preparation procedure. Langmuir. 2004;
20:5642–4. [PubMed: 15986713]
473. Hou WT, Feng QL. Morphologies and growth model of biomimetic fabricated calcite crystals
using amino acids and insoluble matrix membranes of Mytilus edulis. Crystal Growth Design.
2006; 6:1086–90.
474. Li D, Kaner RB. Shape and aggregation control of nanoparticles: not shaken, not stirred. J Am
Chem Soc. 2006; 128:968–75. [PubMed: 16417388]
475. Perumal S, Ramadass SL, Badhan M. Sol-gel processed mupirocin silica microspheres loaded in
collagen scaffold: a synergistic bio-composite for wound healing. Eur J Pharm Sci. 2014; 52:26–
33. [PubMed: 24514452]
476. Uskoković V. Entering the era of nanoscience: time to be so small. J Biomed Nanotech. 2013;
9:1441–70.
477. Fan Q, Wang YE, Zhao X, Loo JS, Zuo YY. Adverse biophysical effects of hydroxyapatite
nanoparticles on natural pulmonary surfactant. ACS Nano. 2011; 5(8):6410–6. [PubMed:
21761867]
Uskoković
Page 51
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

478. Wainwright, SA.; Biggs, WD.; Currey, JD.; Gosline, JM. The mechanical design of organisms.
London: Edward Arnold; 1976.
479. Perry, CC. Biomaterials. In: Interrante, LV.; Hampden-Smith, MJ., editors. Chemistry of
advanced materials: an overview. New York: Wiley-VCH; 1998. p. 499-562.
480. Gai Z, Kalinin SV, Li AP, Shen J, Baddorf AP. In situ observations and tuning of physical and
chemical phenomena on the surfaces of strongly correlated oxides. Adv Funct Mat. 2013;
23:2477–89.
481. Zhang L, Jeon Y, Shim H, Lee G. Direct observation of hopping and merging of single Au
adatoms to form dimers on Si(111)-(7 × 7). J Vac Sci Technol A. 2012; 30:061406.
482. Fuchigami K, Gai Z, Ward TZ, Yin LF, Snijders PC, Plummer EW, Shen J. Tunable metallicity
of the La5/8Ca3/8MnO3 (001) surface by an oxygen overlayer. Phys Rev Lett. 2009;
102:066104. [PubMed: 19257611]
483. Vasudevan RK, Bogle KA, Kumar A, Jesse S, Magaraggia R, Stamps R, Ogale SB, Potdar HS,
Nagarajan V. Ferroelectric and electrical characterization of multiferroic BiFeO3 at the single
nanoparticle level. Appl Phys Lett. 2011; 99:252905.
484. Kim YM, He J, Biegalski MD, Ambaye H, Lauter V, Christen HM, Pantelides ST, Pennycook SJ,
Kalinin SV, Borisevich AY. Probing oxygen vacancy concentration and homogeneity in solid-
oxide fuel-cell cathode materials on the subunit-cell level. Nature Materials. 2012; 11:888–94.
Uskoković Page 52
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

FIG. 1.
(a) Age of patients with osteomyelitis.
11
(b) US population ≥65 years old (bars), along with
a projected increase in the number of patients with bone disease. Sources: US Bureau of the
Census and Office of the Surgeon General.
Uskoković Page 53
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

FIG. 2.
The number of prosthetic joint infections (solid circles and squares), increasing in direct
proportion with the total number of knee (squares) and hip arthroplasties (circles)
performed.
12
Uskoković Page 54
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

FIG. 3.
Radiographs of tibiae displaying a clinical case of acute pyogenic hematogenous
osteomyelitis, also known as Brodie’s abscess (△), along with an area of increased bone
density around the lytic lesion due to periosteal reaction and osteosclerosis (□) (a), and
evidence of chronic osteomyelitis from a goat model, manifesting as a periosteal reaction in
the proximal area of the bone (b).
Uskoković Page 55
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript
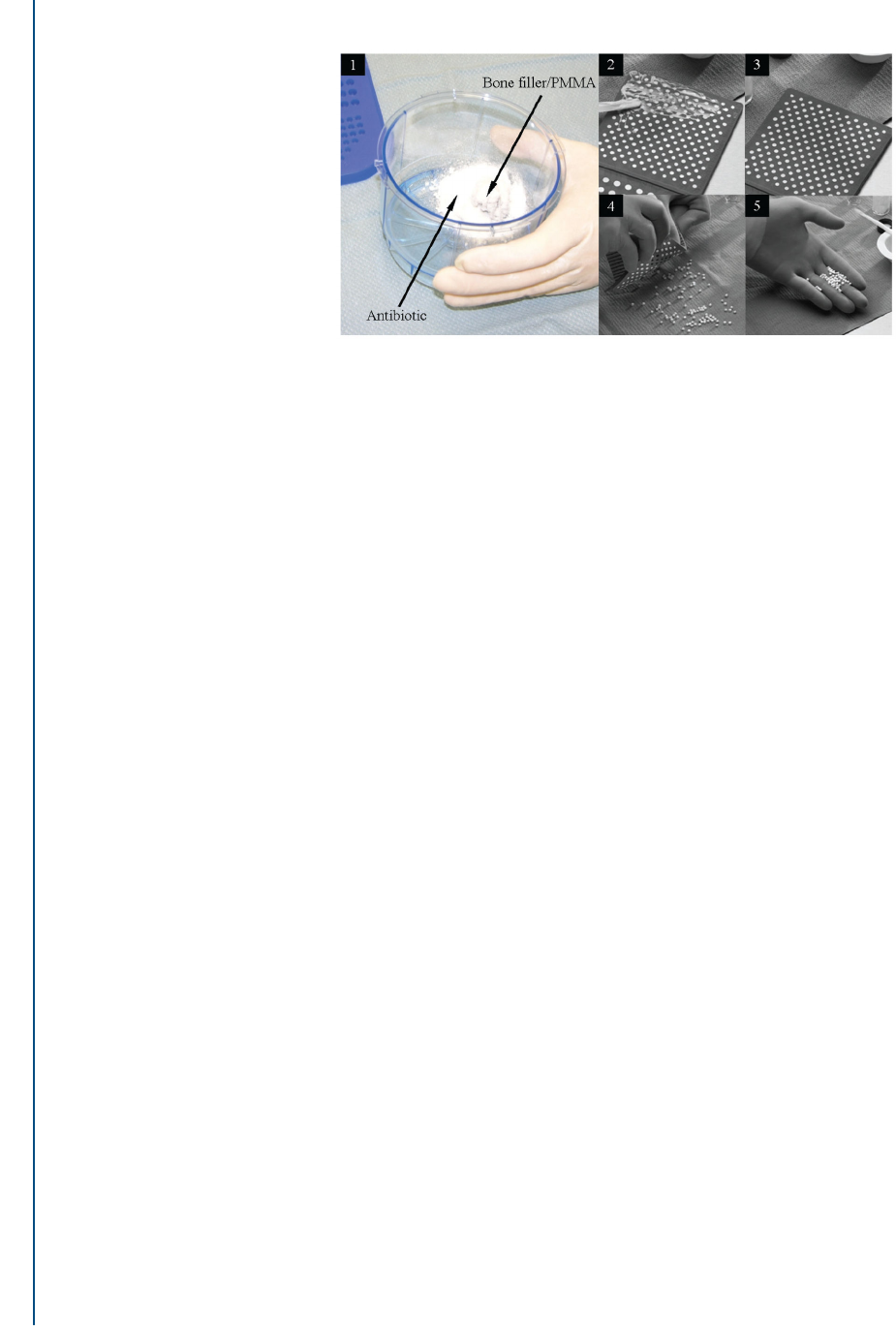
FIG. 4.
A typical preoperative preparation of poly(methyl methacrylate) (PMMA) beads
encapsulating an antibiotic of choice, consisting of (1) manual admixing of the antibiotic
with the bone filler; (2) filling a mold with the solid mixture; (3) hardening; (4) removing
the beads; (5) collecting the beads.
Uskoković Page 56
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

FIG. 5.
(a) Narrowly dispersed calcium phosphate nanoparticles prepared by precipitation form
aggregates upon desiccation at low pressure, capturing the antibiotic clindamycin inside of
the resulting pellet pores, thus ensuring sustained release over prolonged periods of time. (b)
Increased loading efficiency and sustained release from well-dispersed particles could be
obtained by coating calcium phosphate particles with clindamycin adsorbed on them with a
layer of polymer, in this case poly-(D,L-lactide-co-glycolide) (PLGA). High-resolution
transmission electron microscopic images of PLGA-coated hydroxyapatite (c) and
hydroxyapatite nanoparticles (encircled by dashed lines) dispersed in a chitosan matrix
(d).
131
Reprinted with permission from Elsevier (Vukomanović M, Škapin S, Jančar B,
Maksin T, Ignjatović N, Uskoković V, Uskoković D. Poly(D,L-lactide-co-glycolide)/
hydroxyapatite core-shell nanospheres. Part 1: A multifunctional system for controlled drug
delivery. Coll Surf B Biointerfaces. 2011;82(2): 404–13).
Uskoković
Page 57
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

FIG. 6.
An approximate degradation half-life (T
1/2
) for pure poly(lactic acid) (PLA), pure
poly(glycolic acid) (PGA), and their copolymers at various weight ratios (a) and a drastic
difference in the kinetics of drug release from polyethylene glycol diacrylate with 2 different
percentages of cross-linking: 0.5 and 1 (b).
251
Reprinted with permission from Elsevier;
Middleton JC, Tripton AJ. Synthetic biodegradable polymers as orthopaedic devices.
Biomaterials. 2000;21:2334–46.
Uskoković Page 58
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

FIG. 7.
Schematic description of a hypothetical multifunctional composite nanoparticle (a) and the
subdivision of the tissue regeneration process following injury at multiple stages (b). Stages
specific to the bone regeneration process (c) and adverse outcomes of their obviation or
incompletion (d) are shown.
362,363
Reprinted with permission from American Cancer
Society; Ma X, Zhao Y, Liang XJ. Theranostic nanoparticles engineered for clinic and
pharmaceutics. Acc Chem Res 2011;44(10):1114–22, and Elsevier; Mehta M, Schmidt-
Bleek K, Duda GN, Mooney DJ. Biomaterial delivery of morphogens to mimic the natural
healing cascade in bone. Adv Drug Deliv Rev. 2012;64(12):1257–76.
Uskoković
Page 59
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

FIG. 8.
An example of composite monodisperse nanoparticles with simultaneous antioxidative,
antibacterial, and osteoinductive properties. These nanoparticles are formed by coating poly-
(D,L-lactide-co-glycolide) (PLGA) around silver (Ag) poly(glycolic acid) (PGA) core-shell
nanoparticles (Nps) with ascorbic acid dispersed therein. The particles reduced the
concentration of superoxide in human umbilical vein endothelial cells, suppressed the
growth of Escherichia coli and methicillin-resistant Staphylococcus aureus, and upregulated
the expression of 2 osteogenic markers: osteocalcin and protocollagen type I.
392,393
Adapted
and reprinted with permission from Springer (Stevanović M, Savanović I, Uskoković V,
Škapin SD, Bračko I, Jovanović U, Uskoković D. A new, simple, green and one-pot four-
component synthesis of bare and poly(α, γ, L-glutamic acid) capped silver nanoparticles.
Coll Polym Sci. 2012;290(3):221–31) and the American Chemical Society (Stevanović M,
Uskoković V, Filipović M, Škapin SD, Uskoković DP. Composite PLGA/AgNpPGA/AscH
nanospheres with combined osteoinductive, antioxidative and antimicrobial activities. ACS
Appl Mat Interfaces. 2013;5(18):9034–42).
Uskoković Page 60
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

FIG. 9.
Hypothetic release curves for a drug delivery device under two different measurement
regimens: daily replacements of a comparatively small volume of the solvent (circles) and
usage of a considerably larger volume of solvent with no daily replenishments (triangles).
Uskoković Page 61
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

FIG. 10.
(a) A schematic description of the uptake of a calcium phosphate nanoparticle (CaPs) by the
cell and its gene transfection with a DNA plasmid attached to the nanoparticle.
448
(b) A
single-plane confocal optical image of fluorescently stained osteoblastic cell nuclei,
cytoskeletal f-actin, and CaP aggregates containing clindamycin following 48 hours of
incubation. Part A is reprinted with permission from Elsevier (Nouri A, Castro R, Santos JL,
Fernandes C, Rodrigues J, Tomás H. Calcium phosphate-mediated gene delivery using
simulated body fluid (SBF). Int J Pharm. 2012;434(1–2):199–208).
Uskoković Page 62
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

FIG. 11.
(a) A single-plane confocal optical micrograph of a fluorescently stained calcium phosphate
nanoparticle conglomerate loaded with clindamycin and osteoblastic MC3T3-E1 cells (f-
actin; nucleus) following 21 days of incubation in differentiation medium. This image shows
intimate contact between the cells and the material, a direct indication of the
osteoconductivity of the latter. (b) Results of a gene expression study performed using
quantitative reverse transcriptase polymerase chain reaction and showing diminished
expression of three different osteogenic markers BGLAP (left), Col I (middle), and Runx2
(right) in osteoblastic MC3T3-E1 cells incubated with an antibiotic, clindamycin phosphate
(CL). The effect was compensated for when incubation was carried out in the presence of
either hydroxyapatite nanoparticles (HAP) per se or HAP loaded with CL (HAP/CL).
Messenger RNA expression was detected relative to the housekeeping gene ACTB. *Genes
are significantly upregulated (P < 0.05) with respect to the control group. +Genes are
significantly down-regulated (P < 0.05) with respect to the control group.
453
Reprinted with
permission from John Wiley and Sons (Uskoković V, Desai TA. Phase composition control
of calcium phosphate nanoparticles for tunable drug delivery kinetics and treatment of
osteomyelitis. Part 2: antibacterial and osteoblastic response. J Biomed Mat Res Part A.
2013;101:1427–36).
Uskoković Page 63
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
Author Manuscript Author Manuscript Author Manuscript Author Manuscript

Author Manuscript Author Manuscript Author Manuscript Author Manuscript
Uskoković Page 64
Table 1
Main Calcium Phosphate Phases
103–108
Phase Chemical Formula Space Group
pK
sp
at 37°C
Solubility (mg/dm
3
)
MCPA Ca(H
2
PO
4
)
2
Triclinic P
1
̄
1.14
17 · 10
3
MCPM Ca(H
2
PO
4
)
2
·H
2
O
Triclinic P
1
̄
1.14
18 · 10
3
DCPD CaHPO
4
·2H
2
O Monoclinic I
a
6.6 88
DCPA CaHPO
4
Triclinic P
1
̄
7.0 48
β-CPP Ca
2
P
2
O
7
Tetragonal P4
1
18.5 7.6
ACP Ca
3
(PO
4
)
2
·nH
2
O / 25 0.8
α-TCP Ca
3
(PO
4
)
2
Monoclinic P2
1
/a 25.5 2.5
β-TCP Ca
3
(PO
4
)
2
Rhombohedral R3cH 29.5 0.5
TTCP Ca
4
(PO
4
)
2
O Monoclinic P2
1
37.5 0.7
OA Ca
10
(PO
4
)
6
O Pseudo-hexagonal P6
3
/m 69 87
CDHA Ca
10−x
(HPO
4
)
x
(PO
4
)
6−x
(OH)
2−x
(0 < x < 1) Pseudo-hexagonal P6
3
/m 85 9.4
OCP Ca
8
H
2
(PO
4
)
6
·5H
2
O
Triclinic P
1
̄
97.4 8.1
HA Ca
10
(PO
4
)
6
(OH)
2
Pseudo-hexagonal P6
3
/m 117.3 0.3
FA Ca
10
(PO
4
)
6
F
2
Pseudo-hexagonal P6
3
/m 120 0.2
ACP, amorphous calcium phosphate (data pertain to the phase obtainable at pH 9–11); CDHA, calcium-deficient hydroxyapatite; CPP, calcium
pyrophosphate; DCPA, dicalcium phosphate anhydrous, also known as monetite; DCPD, dicalcium phosphate dihydrate, also known as brushite;
FA, fluoroapatite; HA, hydroxyapatite; MCPA, monocalcium phosphate anhydrous; MCPM, monocalcium phosphate monohydrate; OA,
oxyapatite; OCP, octacalcium phosphate; TCP, tricalcium phosphate; TTCP, tetracalcium phosphate.
Crit Rev Ther Drug Carrier Syst. Author manuscript; available in PMC 2015 April 22.
