
© 2023 American Physical Therapy Association. All rights reserved.
APTA Guide to Physical Therapist Practice
Educator Module
2023

Educator Module
The goal of these slides is to assist and enhance student
learning using the Guide to Physical Therapy Practice. It
touches on the main points within the Guide and includes
activities for students to work on to increase their understanding
of physical therapy.

Chapter 1: Introduction to the APTA Guide to
Physical Therapist Practice

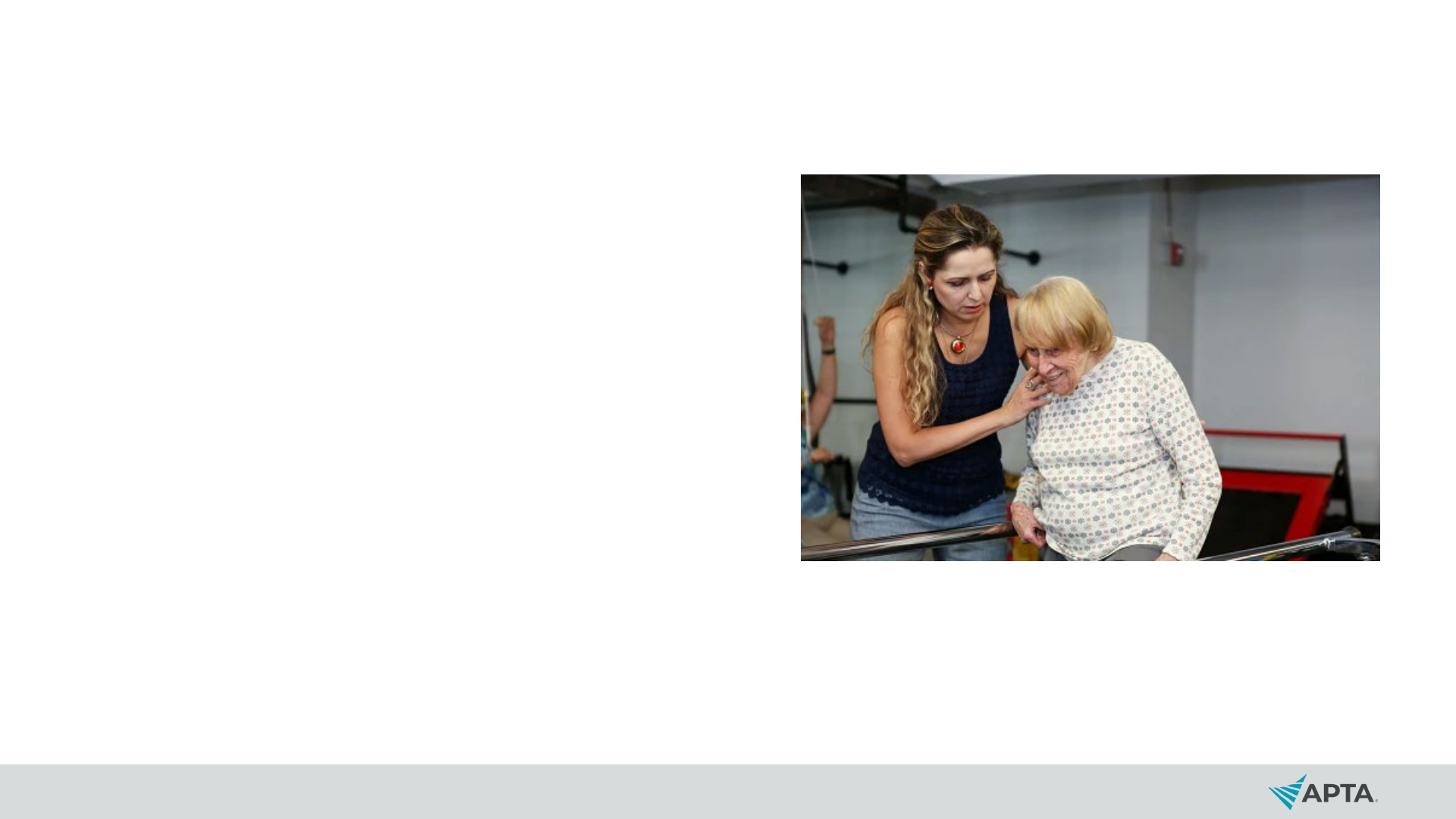
Who Are Physical Therapists?
Physical therapists are health
professionals who diagnose and manage
movement dysfunction as it relates to the
restoration, maintenance, and promotion
of optimal physical function and the
health and well-being of individuals,
families, and communities.
Physical therapists possess a distinct
body of knowledge that provides a unique
perspective on purposeful, precise, and
efficient movement across the life span.

What Do Physical Therapists Do?
Based on the person’s diagnosis,
prognosis, and goals, physical
therapists design and implement a
customized and integrated plan of care
in collaboration with the individual to
achieve the individual’s goal-directed
outcomes.
Physical therapists work towards
maximizing an individual’s ability to
engage with and respond to their
environment, emphasizing movement-
related interventions to optimize
functional capabilities and
performance.

Activity
• In your own terms, describe physical therapist practice.

Biopsychosocial Model
• In this model, a person’s
health status is determined
by the interplay of the
biological, psychological,
and social domains.

Social Determinants of Health
SDOH are the measure of all the exposures of an
individual in a lifetime and how those exposures relate
to health.
SDOH influence the environmental context of
movement and health.
Social risk factors are the adverse social conditions
that may lead to poor health.

Social Determinants of Health
Social determinants of health
include items such as
economic stability, age,
gender, social status, access
to health services, quality
education, healthy
environments, social and
community context and
support, and healthy
environments.

Activity
• Find a photo that demonstrates a social determinant of health.
Write a caption that describes a current goal to address this.

Physical Therapist Practice Core Concepts
Evidence-based practice
Quality assessment and outcomes
Professional values
Evidence-based practice
includes:
Commitment to
professional practice
includes:

Quality Measurement and Outcomes
It is important that physical therapists measure the quality and impact of
their services. Physical therapists use quality measures to help record or
quantify health service delivery processes, outcomes, and perceptions,
and to assess the effectiveness and efficiency of organizational structures
and/or health systems.

Core Values: Accountability
Active acceptance of the
responsibility for the diverse roles,
obligations, and actions of the
physical therapist and physical
therapist assistant including
self‐regulation and other behaviors
that positively influence patient and
client outcomes, the profession, and
the health needs of society.

Core Values: Altruism
The primary regard for or devotion to
the interest of patients and clients,
thus assuming the responsibility of
placing the needs of patients and
clients ahead of the physical
therapist’s or physical therapist
assistant’s self‐interest.

Core Values: Collaboration
Working together with patients and
clients, families, communities, and
professionals in health and other
fields to achieve shared goals.
Collaboration within the physical
therapist‐physical therapist assistant
team is working together, within each
partner’s respective role, to achieve
optimal physical therapist services
and outcomes for patients and
clients.

Core Values: Compassion and Caring
Compassion is the desire to identify with
or sense something of another’s
experience, a precursor of caring.
Caring is the concern, empathy, and
consideration for the needs and values
of others.
Core Values: Duty
• The commitment to meeting
one’s obligations to provide
effective physical therapist
services to patients and clients,
to serve the profession, and to
positively influence the health of
society.

Core Values: Excellence
The provision of physical therapist
services occurs when the physical
therapist and physical therapist
assistant consistently use current
knowledge and skills while
understanding personal limits,
integrate the patient or client
perspective, embrace advancement,
and challenge mediocrity.

Core Values: Inclusion
Occurs when the physical
therapist and physical therapist
assistant create a welcoming and
equitable environment for all.
Physical therapists and physical
therapist assistants are inclusive
when they commit to providing a
safe space, elevating diverse and
minority voices, acknowledging
personal biases that may impact
patient care, and taking a position
of anti-discrimination.
Core Values: Integrity
Steadfast adherence to high
ethical principles or standards,
being truthful, ensuring fairness,
following through on
commitments, and verbalizing to
others the rationale for actions.

Core Values: Social Responsibility
The promotion of a mutual trust
between the profession and the
larger public that necessitates
responding to societal needs for
health and wellness.

Activity
• What is an example of a physical therapist core value you
have seen thus far in your education or career?

Code of Ethics for the Physical Therapist
• Delineates the ethical obligations of all physical therapists and
defines the ethical principles that form the foundation of
practice, consultation, education, research, and
administration.

Code of Ethics Purposes
1. Define the ethical principles that form the foundation of physical therapist
practice in patient and client management, consultation, education, research,
and administration.
2. Provide standards of behavior and performance that form the basis of
professional accountability to the public.
3. Provide guidance for physical therapists facing ethical challenges, regardless
of their professional roles and responsibilities.
4. Educate physical therapists, students, other health care professionals,
regulators, and the public regarding the core values, ethical principles, and
standards that guide the professional conduct of the physical therapist.
5. Establish the standards by which APTA can determine if a physical therapist
has engaged in unethical conduct.

Code of Ethics for the Physical Therapist
• Physical therapists shall
provide:
• safe,
• accessible,
• cost-effective, and
• evidence-based services.

Standards of Practice for Physical Therapy
The Standards of Practice for Physical Therapy is the
profession’s statement of conditions and performances that are
essential for provision of high-quality professional service to
society, and it provides a foundation for assessment of physical
therapist practice expected across all settings.

Educational Opportunities for PTs and PTAs
• Fellowship
• Residency
• Board Certification
• Advanced Proficiency Pathways
Physical Therapists Physical Therapist Assistants

For expanded information regarding PT
and PTA professional development
opportunities, see Chapter 5.

Physical Therapist Roles Across the Continuum and
Through the Life Span
• Access to services for health
conditions.
• Direct access and primary care.
• Administration of tests.
• Habilitation and rehabilitation.
• Performance enhancement.
• Prevention and risk-reduction
services.
• Direct-to-employer physical
therapist services.

Activity
Choose a diagnosis and describe the related roles and
activities of the physical therapist.
Example: A patient comes in with an ACL rupture. Identify the roles a
physical therapist could play and describe the activities in each role.
• Direct access
• Primary care
• Administration of tests
• Habilitation and rehabilitation
• Performance enhancement
• Prevention and risk-reduction
• Direct-to-employer services

Professional Functions
• Consultant
• Educator
• Researcher
• Administrator/business owner
and entrepreneur

Activity
• Divide into small groups. For each professional role, identify
job titles and settings that a PT and PTA might hold. Share in
the larger group for a comprehensive review:
• Educator
• Researcher
• Consultant
• Administrator/business owner
• Entrepreneur

Chapter 2: Accessing Physical Therapist Services and
the Elements of Patient and Client Management
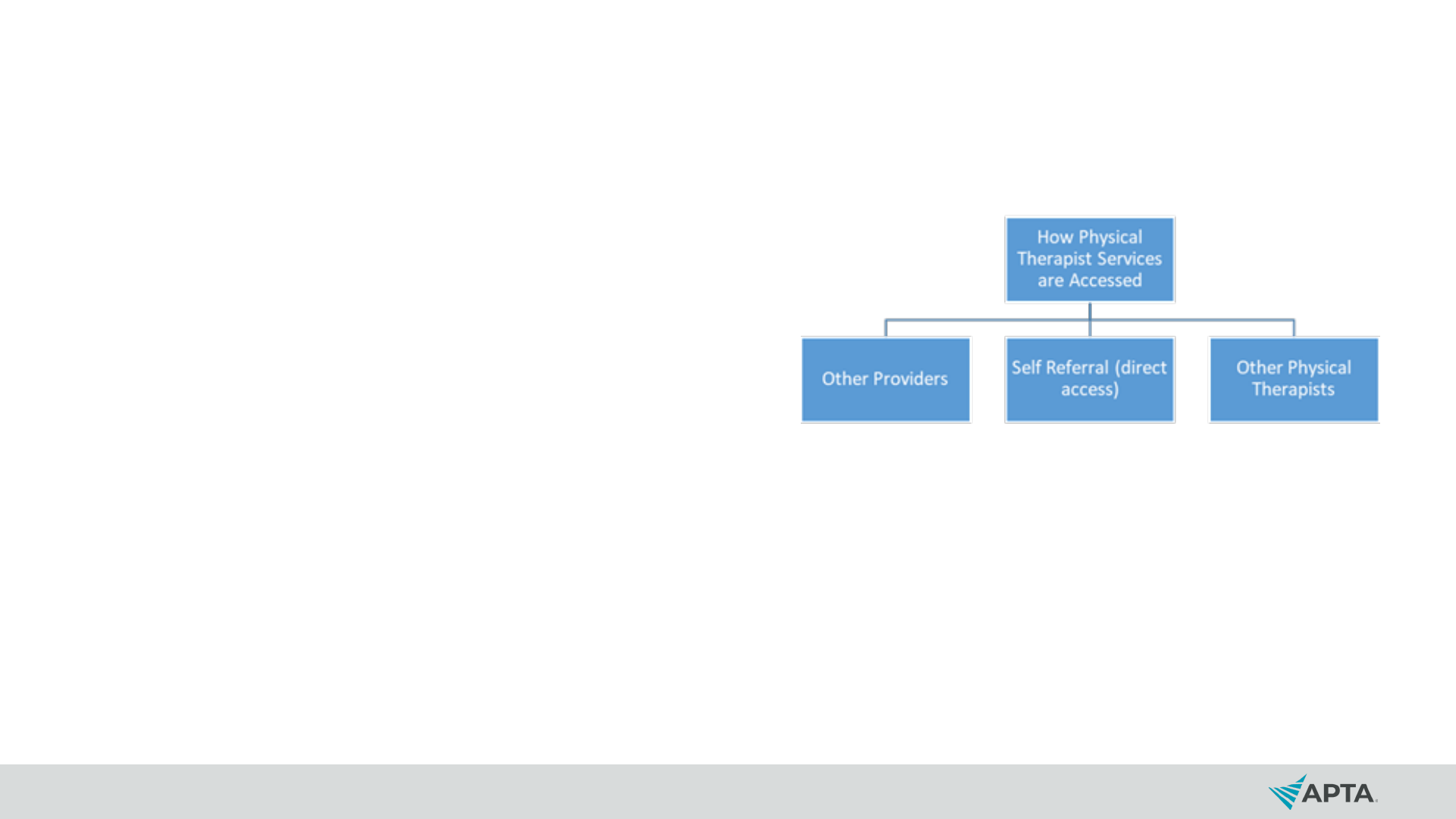
How Do Individuals Access Physical Therapist Services?
• Self-referral (sometimes
termed “direct access”)
• State practice acts vary on
allowances for self-
referral/direct access
• Provider
• Other provider type
• Another physical therapist
• Intervention for a particular
condition

Decision Making
• The physical therapist
decides whether to provide
interventions for the
individual or refer them to
another provider or multiple
providers for management,
co-management, or
consultation.

The Physical Therapist May:
Co-manage: Collaborate with other professionals to direct or coordinate an individual’s
management.
Consult: Render or receive professional expert opinion or advice concerning
specialized knowledge and skills to identify problems, recommend solutions, or
produce a specified outcome or product on behalf of an individual.
Manage: Manage and remain accountable for the services provided when the physical
therapist's management plan involves the use of other recognized assistive personnel.
Refer: Refer an individual to another provider when the individual requires services
that are outside of the PT’s personal, jurisdictional, or professional scope of practice.
Similarly, the PT may choose to refer an individual for specific testing that the therapist
deems necessary for the development of a working diagnosis or management plan.

Activity
Review each definition:
• Co-manage
• Consult
• Manage
• Refer
• Describe patient conditions or presentations that would
necessitate a PT perform each of the actions.

Episode of Care/Services
• An episode of care/service
consists of all physical
therapist services that are:
• provided by a physical
therapist,
• provided in an unbroken
sequence, and
• related to management for a
given condition or problem.
• A visit consists of a physical
therapist encounter or
session.

Consumers of Physical Therapist Services
• Patients are individuals who
receive physical therapist
services for a disease,
disorder, condition,
impairment, activity limitation,
or participation restriction.
• Clients engage the services of
a physical therapist and who
can benefit from the physical
therapist's consultation,
interventions, professional
advice, or health promotion,
fitness, wellness, or prevention
services. Clients may include
businesses, school systems,
and others to whom physical
therapists provide services.

Consumers of Physical Therapist Services
• Communities are groups of
people that may or may not
be spatially connected but
who share common
interests, concerns, or
identities.
• Populations are groups of
people connected by their
demographics and other
factors; examples are
ethnicity, socioeconomic
status, and population
density.

Activity: Group Discussion
• How would your management plan/approach for a population
differ from that of a patient?
• How would it differ between a patient and a client?
• How would your preparation and documentation for a patient
differ from that of a client?
• Which services would you envision to be beneficial for
communities?

Patient and Client Management Model

Elements of Patient and Client Management
Examination
Evaluation
Diagnosis
Prognosis
Intervention
Outcomes
Referral/
consultation

Activity
• During the initial evaluation, the physical therapist has
determined that the score collected on the Generalized
Anxiety Disorder-7 screen (GAD-7) for the patient was 10/21,
exceeding the screening threshold for risk of an anxiety
disorder. Further evaluation and testing is recommended.
What should the PT do?

Activity Continued
• During the history, the PT finds that the individual lives alone
and has difficulty in buying food. This finding could impact the
person’s well-being and the prognosis. What should the PT
do?

Chapter 3: Physical Therapist Examination and
Evaluation

Examination
• The physical therapist
conducts an examination
that includes:
• History.
• Physical examination.
• Tests and measures.

Reexamination
• Reexamination includes the application of selected items from
the history and physical examination and comparing them
with the initial examination findings.
• Reexamination may be indicated more than once during a
single episode of care/services and often is performed over
the course of a disease, disorder, or condition.

Activity
• Compare the concepts of examination and reexamination.
• Give an example of when a formal reexamination may be
indicated.

Subjective History
• Systematic gathering of
subjective data obtained
(through a comprehensive
questioning process or
completion of a patient self-
administered questionnaire)
from the individual and/or
caregiver and other
members of the health care
team, and through a review
of available health records.

Red Flags
• Signs and symptoms found in
the patient history and physical
examination that suggest the
presence of a serious
pathology.
• Example: Red Flags for Stroke
(“Act F.A.S.T.”)
• Face: Smile and see if one side of the
face droops.
• Arms: Raise both arms. Does one arm
drop down?
• Speech: Say a short phrase and check
for slurred or strange speech.
• Time: If the answer to any of these is
yes, call 911 right away and write down
the time when symptoms started.
Source: Centers for Disease Control and Prevention.

Activity
• Provide a primary hypothesis that would require further, in-
depth examination during a more detailed portion of the
physical examination.
• A 78-year-old woman has a diagnosis of Parkinson disease and lives
alone. Upon further questioning, you discover that she has challenges
with communication (due to decreased respiratory function), cognitive
decline (based on her son sitting with her during the appointment),
limited physical activity, history of falls, and complaints of stiffness. A
home health aide helps her with IADL, but she still has to cook and
clean her home, which she says is difficult for her. She also notes
several falls when attempting to cook in the kitchen for a long period of
time, noting she has started bringing a chair to sit on for rest breaks.

Review of Systems
Physical therapists seek information relevant to major body systems
through observation and questioning to help determine whether there are
symptoms that suggest the need for referral for additional medical
evaluation.
• Cardiovascular system.
• Pulmonary system.
• Endocrine system.
• Eyes, ears, nose, and throat.
• Gastrointestinal system.
• Genitourinary/reproductive systems.
• Hematologic/lymphatic systems.
• Immune system.
• Integumentary system.
• Nervous system.
• Musculoskeletal system.
• Overall physical and psychological
condition, such as unexplained weight
change, fatigue, lethargy, and malaise;
cognitive well-being; and emotional well-
being, such as anxiety and feelings of
hopelessness.

Physical Examination
• Begins with the systems review:
• Cardiovascular and pulmonary systems.
• Integumentary system.
• Musculoskeletal system.
• Neuromuscular system.
• Neurologic system.
• Communication ability, affect, cognition, language, ability to
read, and learning style.
• Movement.

Activity
• Explain the difference between the review of systems and the
physical examination/systems review.
• The PT sees in the history that the patient has smoked two
packs per day for 10 years, so the PT auscultates the lungs
and finds crackles in the right and left lower lobes. (Review of
systems or physical exam/systems review?)
• The patient self-referred to physical therapy for generalized
joint pain and fear of falling. The PT scans the patient for joint
deformities and asks questions about recent falls or loss of
balance. (Review of systems or physical exam/systems
review?)

Tests and Measures
Physical therapists use
measurements (including
outcome measures):
• To identify impairments
and potential causes of
impairments in body
structures and functions,
activity limitations, and
participation restrictions.
The results of tests and
measures:
• Inform risk identification and
prevention and health
promotion activities.
• Contribute to outcome
assessment.
• Help the PT determine change
in the individual’s status.

Tests and Measures
Tests and measures are a component of the physical
examination used to:
• Confirm or reject a clinical hypothesis regarding the factors
that contribute to making the individual’s current level of
function less than optimal.
• Support the physical therapist’s clinical judgments about the
diagnosis, prognosis, and development of an effective
management plan.

26 Categories of Tests and Measures
• Aerobic capacity/endurance.
• Anthropometric characteristics.
• Adaptive and assistive technology.
• Balance.
• Circulation (arterial, venous, lymphatic).
• Cognitive and mental function.
• Community, social, and civic life.
• Cranial and peripheral nerve integrity.
• Education life.
• Environmental factors.
• Gait.
• Integumentary integrity.
• Joint integrity and mobility.
• Mobility (e.g., Locomotion).
• Motor function.
• Muscle performance (strength, power,
endurance, and length).
• Neuromotor development and sensory
processing.
• Pain.
• Posture.
• Range of motion.
• Reflex integrity.
• Self-care and domestic life.
• Sensory integrity.
• Skeletal integrity.
• Ventilation and respiration.
• Work/community integration.

Types of Measures
Properties of Tests and Measures
Reliability: Consistent time after
time, with as little variation as
possible.
Validity: The degree to which a useful
(meaningful) interpretation can be
inferred from a measurement.
Self-report measures provide information about the individual's
perception of how their impaired body function or structure is limiting
activities and participation.
Performance-based measures involve observing the individual
performing an activity.

Measuring Outcomes
When standardized tests and measures are used to determine
change in outcome status during and at the end of an episode
of care, they may be referred to as outcome measures.
These tests may measure:
• Functional status (activity limitations and participation restrictions),
including changes in health, wellness, and fitness.
• Impairments of body functions and structures.
• Adverse outcomes and complications.
• Morbidity and mortality.
• The individual’s self-reported outcomes.
• The individual’s satisfaction with the care/services received.

Evaluation
• Evaluation is the interpretation and synthesis of the examination
findings that lead to a diagnosis, prognosis, and management
plan specific to the individual or community.
• Physical therapists interpret and synthesize the history and the
physical examination findings to:
• Establish a diagnosis from which to develop a management plan.
• Determine a prognosis, including goals for physical therapist management.
• Develop a management plan or plan of care if indicated.
• Develop a working diagnosis list as part of the process used to determine
whether a referral to or consultation with another health care provider is
indicated.

Activity
• Give an example of a physical therapist examination and
evaluation. What are the differences?
• Describe a situation in which a red flag might come up and
how you as the clinician will respond.

Chapter 4: Physical Therapist Practice: Diagnosis,
Prognosis, Intervention, and Outcomes
Diagnosis
• A label encompassing a cluster of signs and symptoms
commonly associated with a disorder or syndrome or
category of impairments in body structures and function,
activity limitations, or participation restrictions.
• Physical therapists establish a diagnosis in order to make
appropriate management decisions for an individual and
determine the most appropriate intervention strategy.

Diagnosis
Diagnosis Classifications:
• ICD-10
• ICF
• Movement systems

Prognosis
The physical therapist’s determination of
the predicted optimal level of
improvement in function over a
designated time frame.
Prognosis typically includes a prediction
of levels of improvement during the
episode of physical therapy in
determining goals and outcomes.
Can be influenced by contextual factors.

Activity
• Read the Chapter 4 compendium and define a contextual
factor. How can this influence a patient’s outcome or
recovery?
• What are some other resources a clinician might use to guide
their prognosis?

Management Plan
• A framework of physical therapist services provided to
individuals, groups or populations, based on best available
evidence, clinical expertise and the individual’s wants and
needs.
• May include a plan of care which consists of:
• Individual’s goals.
• Prognosis.
• Interventions to be used including duration and frequency.
• Summary of plans for referral or consultation to other
providers.

Goals
The intended impact on functioning as a result of
implementing the physical therapist management plan.
Measurable, functionally driven, time-limited, and, when
applicable, classified as short term and long term.
Primary criterion for conclusion of physical therapist
services is achievement of individual’s goals.

Goals
• Example: Patient will ambulate for 100 feet with no assistive
device using step-through gait pattern in three weeks in order
to walk to mailbox each day.

Activity
• Create a goal for a patient to be achieved in two weeks and a
goal for a patient to achieve by the conclusion of physical
therapist services.

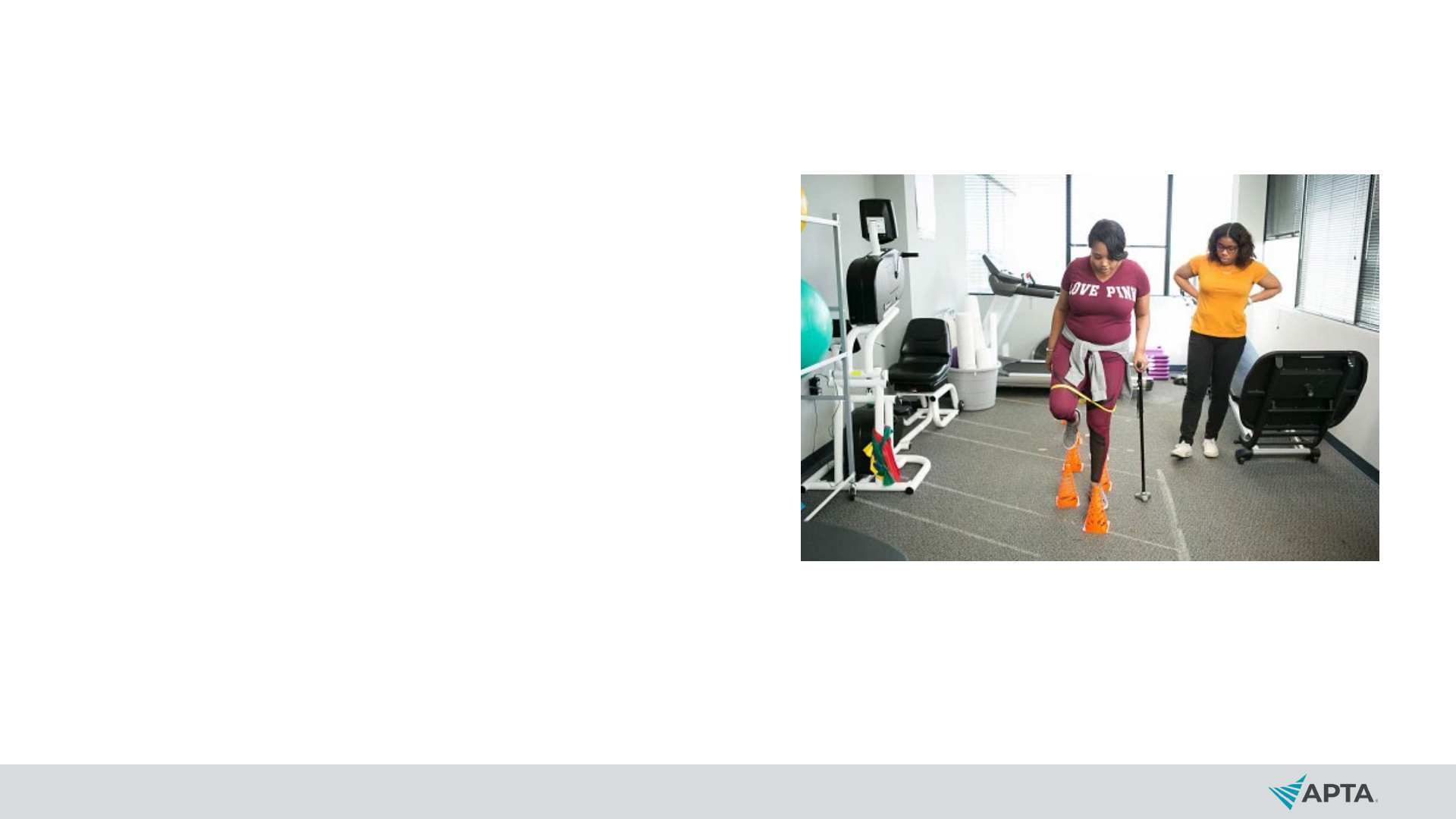
Interventions
• Physical therapists use interventions to remediate impairments in all
major body systems, improve functional performance, and promote
improved health and wellness that lead to optimized activity,
participation, and quality of life.
• Interventions are based on the PT’s examination findings, diagnosis, and
the accompanying goals established as part of the management plan
and plan of care.
• Factors that influence complexity, frequency, and duration of the
intervention and the decision-making process may include:
• Psychosocial and economic factors.
• Patient’s overall health status.
• Adherence to the intervention program.

Procedural Interventions
Adaptive and
assistive
technology
Biophysical agents Functional training
Integumentary
repair and
protection
techniques
Manual therapy
Motor
function/movement
training
Respiratory and
ventilatory
techniques
Therapeutic
exercise

Physical Therapist Prevention Services
• Primary prevention services
by physical therapists is
centered around a health
and wellness program to
reduce future injury or
disease in an otherwise
healthy population.

Activity
• Think of an example of primary prevention services in
physical therapist practice.

Outcomes
• Outcomes are the actual results of implementing the
management plan that indicate the impact on
functioning.
• Physical therapists report outcomes to demonstrate
progress, for payment purposes, and to know whether
goals have been met.

Activity
• Identify the use of clinical outcomes that are measured and
reported by physical therapists to describe the patient’s
condition and progress.

Using the Compendium
• Enhance learning.
• Dive deeper into a topic.
• Access references.
To open or close the
Compendium, click on the + or –
sign.



