Mental Cognitive Subcommittee
Content Model and Classification Recommendations
APPENDIX C
Report of the
Metal-Cognitive Subcommittee
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
This page is left intentionally blank.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
REPORT OF THE MENTAL COGNITIVE SUBCOMMITTEE OF THE
OCCUPATIONAL INFORMATION DEVELOPMENT ADVISORY PANEL
Subcommittee Chair
David J. Schretlen, Ph.D.
Subcommittee Members
Robert T. Fraser, Ph.D.
Sylvia E. Karman, Project Director
September 1, 2009
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
This page left intentionally blank.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-i
TABLE OF CONTENTS
Executive Summary ........................................................................................................ 1
Introduction ..................................................................................................................... 3
Methodology, Procedures, and Findings ......................................................................... 5
Mental Cognitive Subcommittee Recommendations..................................................... 19
Core Mental Residual Functional Capacities ............................................................. 21
Suggested Studies ........................................................................................................ 27
References.................................................................................................................... 31
Appendices ................................................................................................................... 45
Appendix A.................................................................................................................... 47
Appendix B.................................................................................................................... 51
Appendix C – 1.............................................................................................................. 57
Appendix C – 2.............................................................................................................. 59
Appendix C – 3.............................................................................................................. 61
Appendix C – 4.............................................................................................................. 65
Appendix C – 5.............................................................................................................. 67
Appendix C – 6.............................................................................................................. 81
Appendix C – 7............................................................................................................ 101
Appendix C – 8............................................................................................................ 111
Appendix D.................................................................................................................. 174
Appendix E.................................................................................................................. 179
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-ii
This page left intentionally blank.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-1
Executive Summary
The Mental Cognitive Subcommittee was assembled to advise the OIDAP about what
psychological abilities of disability applicants should be included in the Content Model
and Classification Recommendations made to the Social Security Administration.
The Subcommittee reviewed relevant scientific literature, consulted experts in the fields
of psychiatric disability and vocational outcomes research, heard presentations by
academic experts, staff members of the Social Security Administration (SSA), and
Disability Determination Services (DDS), and interviewed medical consultants and
disability claims examiners for the Maryland State DDS office. The Subcommittee
convened a Roundtable Meeting in Chicago in June 2009 that was attended by
participants representing a broad range of expertise. Roundtable participants were
asked to nominate human abilities they regarded as essential for work, and to discuss
their rationale for including each element. The Subcommittee met both in person and
via telephone conference to synthesize the data obtained from these activities and
sources. Finally, other OIDAP members and Roundtable participants were asked to
comment on the provisional synthesis of essential human abilities that the
Subcommittee recommends for inclusion in the Content Model. The essential
recommendations of this Subcommittee are as follows:
1. The conceptual model of psychological abilities required to do work should be
revised. The aims are to redress shortcomings of the current model, base a
revised model on scientific evidence, identify specific abilities that can be reliably
assessed and tested for predictive validity, and retain elements of the current
mental residual functional capacity (MRFC) model that meet these criteria in
order to maintain continuity where possible.
2. Psychological abilities that are deemed essential to do work are conceptualized
as falling into four core categories: (A) neurocognitive functioning, (B) initiative &
persistence, (C) interpersonal functioning, and (D) self-management.
3. The Subcommittee recommends that SSA adopt 15 abilities that represent
specific aspects of the four general categories listed above. These abilities and
the rationale for including each are described in the report.
4. The Subcommittee recommends that it provide ongoing consultation to the OIS
Project’s psychometrician as the SSA develops items for data collection. The
SSA should consider using different methods and scales, depending on the
psychological ability being assessed.
5. The Subcommittee recommends a series of studies to determine the reliability
and predictive validity of any instruments developed to assess residual functional
capacities and occupational demands as part of the OIS Project.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-2
This page left intentionally blank.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-3
Introduction
The Mental Cognitive Subcommittee was convened by the OIDAP Chair. The members
initially included David J. Schretlen, PhD (Chair), Robert T. Fraser, PhD, Sylvia E. Karman,
and Mary Barros-Bailey, PhD. However, Dr. Barros-Bailey subsequently withdrew from
membership. A biographical sketch of each member appears in Appendix A of this report.
In a working paper entitled “What is a Content Model?” the SSA concluded that the
Occupational Information System it plans to develop must describe the personal abilities
and characteristics that individuals must possess in order to be able to perform each
occupation. Further, these abilities and characteristics must be defined in ways that are
maximally useful for assessing the residual functional capacity (RFC) of claimants. In
response, the OIDAP Chair appointed a Mental Cognitive Subcommittee to review mental
abilities that can be impaired by illness or injury, and thereby impede a person’s ability to
do work. The aim of this subcommittee was to make recommendations about how to
conceptualize the mental and interpersonal characteristics required to do work. The
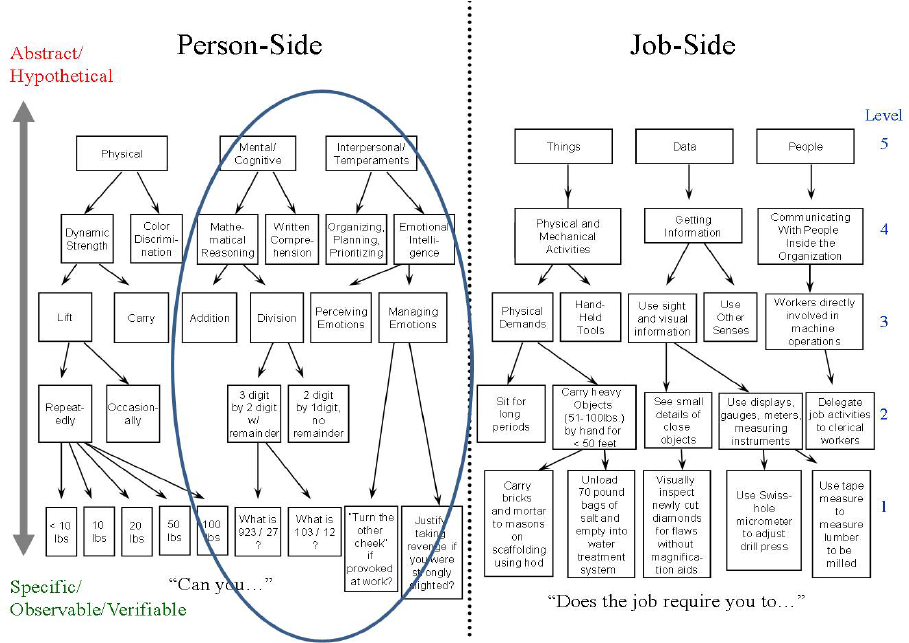
characteristics of interest are circled in Figure 1 below, with a primary emphasis on
intermediate levels of abstraction.
Figure 1. Cartoon depicts the person-side and job-side characteristics to be considered for
inclusion in an occupational information system. The Mental Cognitive Subcommittee was asked to
help OIDAP conceptualize the essential psychological abilities at intermediate levels of abstraction
that should be included in such a model.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-4
This page left intentionally blank.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-5
Methodology, Procedures, and Findings
Mental Cognitive Subcommittee discussions and activities: The subcommittee’s
approach to data gathering and analysis consisted of multiple activities. These included
break-out meetings at the second quarterly OIDAP meeting in Atlanta, Georgia, and the
third quarterly OIDAP meeting in Chicago, Illinois. In addition, the subcommittee met by
telephone conference calls seven times between March 17, 2009, and August 12, 2009.
In the first telephone conference, subcommittee members agreed to review the MRFC
assessment (SSA-4734-F4-SUP) currently used for disability determination purposes,
and to discuss its elements at the next meeting. Subcommittee members agreed to
consider what psychological variables should be included in the content model for an
ideal OIS, how they should be measured, and what existing sources of empirical data
linking specific aspects of cognitive, emotional, and behavioral functioning to job
performance are available for review. At the second telephone conference, Dr. Fraser
proposed that an ideal behavioral assessment would include measures of processing
speed, divided attention, incidental memory, executive abilities, and verbal fluency. He
noted that depression and anxiety are important to assess because they are known to
impede job maintenance. He also cited research showing that variables that predict
return to work can differ from those that predict job maintenance, and that optimal
predictors vary by medical condition (e.g., traumatic brain injury versus multiple
sclerosis). Dr. Barros-Bailey emphasized the importance of assessing an individual’s
capacity to initiate tasks and inhibit behavioral outbursts, as well as the importance of
determining the validity of any assessment instruments developed. Dr. Schretlen asked
whether the SSA might be willing to consider funding or conducting research designed
to empirically determine the cognitive and other “person-side” abilities and
characteristics required to successfully meet the demands of selected occupations.
As a result of these telephone conferences and a discussion at the second quarterly
meeting of the OIDAP, the subcommittee decided to convene a Roundtable Meeting on
June 8, 2009. The meeting agenda and which experts to invite were discussed via email
correspondence and during telephone conference calls on May 8 and 19, 2009. Results
of the June Roundtable Meeting were discussed by the subcommittee on July 21, 2009
and August 5, 2009. These discussions focused on synthesizing feedback obtained
from participants both during and after the June Roundtable Meeting. Subcommittee
members debated the merits and limitations of various conceptualizations of both the
overarching categories or dimensions of psychological and interpersonal abilities that
are required to perform work, as well as the specific exemplars of these categories.
These discussions informed recommendations made in the subcommittee’s final report
to the OIDAP.
Presentations to the OIDAP and Mental Cognitive Subcommittee
: Information derived
from presentations made to and by the subcommittee also was considered for inclusion
in the subcommittee’s report to the OIDAP. Points of greatest relevance to the
subcommittee’s charge are summarized below.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-6
First Mental Cognitive Subcommittee Presentation: At the OIDAP quarterly meeting on
April 29, 2009, Dr. Schretlen gave a presentation entitled “Cognitive Assessment for the
Determination of Mental Residual Functional Capacity.” In this presentation, he
explained that individual differences in cognitive performance strongly predict
occupational attainment in healthy adults, and often predict work outcomes
(employment, disability, job placement, work performance) better than symptom or
injury severity in many psychiatric conditions, such as schizophrenia, traumatic brain
injury, and multiple sclerosis. He suggested that this makes cognitive impairment a sort
of “final common pathway” to work disability. However, he pointed out that most
research on the relationship between cognitive functioning and work is based on
performance-based measures, such as individually administered tests of IQ, attention,
and memory. Consequently, if SSA elects to rely on ratings derived from medical
records or other informants to assess cognitive abilities, it will be essential to validate
such ratings against performance-based measures of residual cognitive abilities.
Dr. Schretlen next pointed out that the universe of cognitive processes can be parsed
into smaller “factors” many different ways. He described and contrasted the statistical
methods of exploratory and confirmatory factor analysis. He then reviewed the results of
19 studies that investigated the underlying or latent structure of cognitive functioning
among healthy adults and patients with neuropsychiatric disorders. This showed that
there is scientific evidence for varied factor structures. Dr. Schretlen discussed the
advantages and disadvantages of adopting a parsimonious model of cognitive
functioning (just one or two factors) versus a more complex model (three or more
factors). A single summary measure of residual cognitive capacity (such as “g”) has the
advantages of being easily understood, reliably measured, and strongly predictive of
work outcomes. The main disadvantage is that relying solely on g might mask more
specific cognitive impairments that could preclude the ability to work. Dr. Schretlen then
showed a table from the Wonderlic Personnel Test (WPT) manual depicting the WPT
scores of several thousand adults in 70+ occupations. The WPT reliably measures g in
12 minutes, and the table clearly demonstrates that scores on this test vary by
occupation, likely due to differences in occupational complexity. Further, nearly half of
the 100 most widespread occupational groups overlapped with jobs for which
incumbents’ WPT scores were reported in the test manual, and their scores spanned a
very broad range. Dr. Schretlen then presented the findings of two studies conducted at
Johns Hopkins. One showed that a very brief test that measures two cognitive factors
(the Mental Status Exam −Telephone Version or MSE−TV) distinguished SSI/SSDI
beneficiaries who were found disabled due to a mental disorder from healthy adults with
very large effect sizes. The other study involved a confirmatory factor analysis of
15 cognitive measures in 576 adults. It showed that a six-factor model of cognitive
architecture applied equally well to healthy adults and patients with schizophrenia or
bipolar disorder despite large group differences in overall levels of performance on the
cognitive tests. Dr. Schretlen concluded the presentation by reiterating the point that the
SSA will have to decide whether to use performance-based measures (like IQ tests) or
informant ratings (as currently used for MRFC assessment) to measure psychological
abilities that are essential to work. He emphasized that validating any new instruments

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-7
to assess psychological abilities also will require the SSA to determine what level of
impairment shall define a disability “threshold.” Finally, he urged the SSA to develop
proprietary measures, rather than rely on previously published psychological tests, and
to conduct the necessary research to validate measures that are adopted. Slides and
references for this presentation are shown in Appendix D.
Second Mental Cognitive Subcommittee Presentation: At the OIDAP quarterly meeting
on June 10, 2009, Dr. Schretlen presented a talk entitled “Clinical Inference in the
Assessment of Mental Residual Functional Capacity.” In this presentation, he outlined
three major approaches that the SSA might use to draw inferences about whether an
individual claimant has sufficient residual psychological (or physical) capacities to do
work. The aim of this talk was to discuss the underlying logic and threats to the validity
of each method of inference. The first method involves reliance on pathognomonic
signs, such as a positive Babinski reflex that signifies the presence of an upper motor
neuron lesion. Dr. Schretlen explained that the major limitations of this method are that
the reliability with which such pathognomonic signs can be elicited and the frequency of
their appearance in normal (i.e., non-pathological) populations are rarely assessed. He
presented data showing that many so-called pathognomonic signs occur quite
frequently in healthy adults. The implication of these limitations is that the SSA should
not assume that successful job incumbents are free of such signs. For example, if an
occupation requires frequent lifting of 25 pounds from the ground, it would be prudent to
study a random selection of persons who successfully work in that occupation to
determine how many of them are unable to frequently lift 25 pounds from the ground.
The SSA should not assume that all successful job incumbents in that occupational
category can do so.
The second approach to inference involves pattern analysis, or the identification of a
clinically recognizable gestalt of signs, symptoms, and laboratory findings, to diagnose a
disease or condition. This approach to inference probably mirrors the logical task of
matching an individual claimant’s RFC to specific occupational demands. A great deal
of empirical evidence supports the validity of this approach to inference, but it has two
limitations: First, it works best for individuals whose clinical presentations are typical of a
given disease or condition. It is more difficult to diagnose a disease or condition when
the patient’s presentation is atypical, or when the clinical presentation is obscured by
the presence of co-occurring conditions or treatment side-effects. The second limitation
is that normal intra-individual variability can be misinterpreted as meaningful. For
example, Dr. Schretlen showed that in one study, 197 normal healthy adults showed an
average discrepancy of more than 3 standard deviations (i.e., the equivalent of >50 IQ
points) between their best and worst score on a battery of cognitive tests. Dr. Schretlen
concluded that the logic of this approach closely mirrors the process of matching RFC
with job demands, but he cautioned that empirical study of populations of individuals
with and without disabilities is needed to validate the approach.
The third method of clinical inference involves deficit measurement. Dr. Schretlen
pointed out that this is the most widely used and accepted approach to diagnosing
impairment. An IQ of 70 falls 2 standard deviations below the mean and places one

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-8
among the lowest 2% of the population in overall intelligence. Scores below this are
widely considered abnormal. Likewise, laboratory blood values or measures of physical
strength that place one among the lowest 2% of the population are also usually
interpreted as abnormal. However, some diseases or injuries might cause a decrement
in some ability, even though the person’s residual capacity remains within the normal
range for the population as a whole. For example, an attorney who sustains a severe
traumatic brain injury might lose 25 IQ points as a result. However, if her IQ was 120
before the accident, it would still fall within the average range after the accident. Thus,
impairment can be defined by an ability that is very low compared to the population as a
whole, or by a decline from a person’s own pre-morbid level of functioning.
Dr. Schretlen pointed out that these observations have important implications. One is
that these two scenarios suggest that we need to establish different types of cutoffs to
define “impairment.” He also presented data which show that normal adults frequently
produce one or two abnormal scores using any cutoff when enough tests are
administered. Dr. Schretlen concluded the talk by pointing out that a study of successful
job incumbents would probably show that many, and perhaps even most, people fall
short of meeting one or more of their usual job demands. He noted that whatever cutoff
the SSA uses to define insufficient RFC to meet a job demand will directly affect the
percentage of applicants who will be found disabled. He asked whether a claimant
whose upper extremity strength exceeds that of the weakest 10% of successful
incumbents in a given occupation should be deemed able to do that job. Obviously, the
claimant can meet that job’s strength demands to some degree because 10% of
successful job incumbents are weaker than he. However, maybe the 10% of successful
job incumbents who are weaker were stronger when they were hired, and would not be
hired if they applied for the same job today. The point is that the SSA will have to decide
what cutoff defines insufficient RFC if disability determination is ever based on empirical
evidence. Finally, Dr. Schretlen also discussed the issue of “effort” and how suboptimal
effort can uncouple the linkage between ability and performance on tests of
psychological functioning, strength, etc. Slides and references for this presentation are
shown in Appendix E.
Mental Cognitive Roundtable: On June 8, 2009, the Subcommittee held a Roundtable
meeting in Chicago, Illinois, to solicit opinions from and facilitate discussion by experts
in the field about mental impairments that cause work disability. In a series of
discussions, the Mental Cognitive Subcommittee identified and invited a panel of
experts to participate in a one-day meeting for this purpose. Participants were provided
with background materials ahead of the meeting (see Appendix C). The first document
explained the purpose and scope of the Roundtable. It asked each participant to review
the current MRFC assessment (SSA-4734-SUP), and then write a brief response to
each of four questions before the meeting. The four questions were as follows:
1. If you think the current MRFC Assessment does not need revision, or that
improving it is not feasible, explain why.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-9
2. If you think the existing MRFC Assessment could be improved, then nominate up
to 10 dimensions of psychological and interpersonal functioning that, when
impaired by disease or injury, impede one’s ability to work.
1
3. Do you know of any well-designed empirical studies that have identified
psychological or interpersonal deficits that decrease the likelihood an affected
individual will be able to do competitive work?
4. While the goal of this Roundtable is not to devise measures of the person
characteristics you nominate in response to Question 2, please comment on
what you deem to be the best approach (informant-rating, self-rating, direct
observation, testing) to assess the characteristics you enumerated. (These might
vary across functions.)
The Roundtable participants, their affiliations, and areas of expertise are shown in the
table below. Each participant’s biographic sketch appears in Appendix B.
Name Affiliation Expertise
David J. Schretlen,
PhD, ABPP
OIDAP Mental Cognitive Subcommittee
(chair); Johns Hopkins University
Clinical neuropsychology; cognitive &
neuroimaging correlates of disability
Robert T. Fraser,
PhD
OIDAP Mental Cognitive Subcommittee;
University of Washington
Rehabilitation psychology; TBI;
epilepsy; multiple sclerosis
Marry Barros-
Bailey, PhD, CRC
OIDAP (chair); Mental Cognitive
Subcommittee; Private Practice
Rehabilitation counseling; life care
planning; vocational expert
Sylvia E. Karman,
BA
SSA; Director, Occupational Information
Dev. Project; Mental Cognitive Subcom.
SSA disability programs; use of the
DOT for disability adjudication
Mark Wilson, PhD
OIDAP Work Taxonomy Subcommittee
(chair); North Carolina State University
Industrial and organizational
psychology; occupational analysis
Shannon Gwaltney-
Gibson, PhD
OIDAP Work Taxonomy Subcommittee;
East Carolina University
Industrial and organizational
psychology; occupational analysis
E. Sally Rogers,
ScD
Director of Research, Center for Psychiatric
Rehabilitation, Boston University
Psychiatric rehabilitation outcomes
research; vocational recovery
Gary R. Bond, PhD
Professor, Department of Psychiatry,
Dartmouth University School of Medicine
Psychiatric rehabilitation outcomes
research; supported employment
Susanne Bruyère,
PhD
Director, Employment and Disability
Institute, ILR School, Cornell University
Disability policy and discrimination;
rehabilitation outcomes research
Lynda Payne, PhD
Maryland Disability Determination Services,
Consulting Psychologist
Developmental psychology, psychiatric
disability
Pamela A. Warren,
PhD
Departments of Psychology and Psychiatry,
University of Illinois
Occupational and health psychology;
psychological disability management
1
For purposes of calibrating the level of specificity that we are looking for, a capacity such as “the ability to
reason” is too global and nonspecific. Conversely, a capacity such as “the ability to tolerate occasional brusque
remarks from co-workers without losing one’s temper” might be too specific. Because our aim is to develop a
list of candidate abilities that is comprehensive but parsimonious, we ask that you limit your list to about
10 functional capacities. Based on SSA requirements, these dimensions or factors must be observable and
measurable.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-10
In addition to the Roundtable participants, 16 representatives of SSA and other
stakeholder associations observed the proceedings and asked questions of the
panelists. These included:
Aliza Gordon, SSA Deborah Harkin, SSA
Debra Tidwell-Peters, SSA Elaina Wise, SSA
Elizabeth A. Kennedy, SSA George D. Harris, SSA
John E. Owen, III, SSA Michele Schaefer, SSA
Nancy Torkas, SSA Paul Kryglik, SSA
Robert J. Harvey, SSA Robert Pfaff, SSA
Shirleen B. Roth, SSA Susan J. Swansiger, SSA
Thomas A. Hardy, OIDAP Tom Johns, SSA
Elizabeth Rasch, NIH
Ms. Karman opened the Roundtable by providing a brief overview of the OIDAP. Then,
following brief remarks by Dr. Fraser, Dr. Schretlen opened the Roundtable discussion
by asking participants to address Question 1 from the Purpose and Scope invitation.
Participants uniformly agreed that the current MRFC assessment could be improved.
Dr. Rogers noted that the form is oriented toward lower level occupations and that some
items assess two abilities, making it difficult to rate an individual who shows no limitation
in one respect but some limitation in the other. Dr. Warren and others noted that the
ratings are cross-sectional but illness-related impairments wax and wane over time.
Dr. Bond noted that impairments are often situation-specific, and Dr. Rogers
emphasized that observer ratings based on situational assessments have generally
been found to be more predictive of work outcomes in mental illness than
pencil-and-paper tests or ratings of an individual’s personal characteristics. Dr. Payne
observed that the current rating scheme is too coarse (not significantly limited;
moderately limited; markedly limited), lacks sensitivity to fluctuations over time, and
does not mirror occupational demands. Drs. Wilson, Gwaltney-Gibson, and others
concurred that the inferential leap between residual abilities and job demands is too
large. Dr. Fraser noted that the items are not evenly distributed across cognitive
domains (e.g., eight concern attention/concentration, whereas only three concern
memory and reasoning). Dr. Payne also noted that the items probably are not weighted
equally in terms of how disabling they are.
Most of the Roundtable discussion focused on Question 2, which asked participants to
nominate dimensions of psychological and interpersonal functioning that, when impaired
by disease or injury, impede one’s ability to work. Responses to the 20 individual items

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-11
that inform the current MRFC assessment (SSA-4734-SUP) included the following
comments:
1. The ability to remember locations and work-like procedures. The locations queried
by this item are unclear. Also, why ask about “work-like” procedures?
2. The ability to understand and remember very short and simple instructions. What
defines very short and simple instructions is unclear. If someone understands
instructions but cannot remember them, how is this rated?
3. The ability to understand and remember detailed instructions. These abilities
could be assessed with a single item that rates information complexity (e.g., the
person can understand and remember simple but not complex instructions).
4. The ability to carry out very short and simple instructions. Since it is highly unlikely
that someone can carry out short and simple instructions without understanding
them, these items are redundant.
5. The ability to carry out detailed instructions. Again, 4 and 5 could be combined in
a single item that rates complexity.
6. The ability to maintain attention and concentration for extended periods. The
qualifier “extended” lacks specificity. Item does not capture differences in kinds or
intensity of attention required by different jobs.
7. The ability to perform activities within a schedule, maintain regular attendance,
and be punctual within customary tolerances. There was widespread agreement
that an item like this should be retained.
8. The ability to sustain an ordinary routine without special supervision. Despite lively
debate, several participants argued that an item rating one’s ability to work in a
reasonably independent fashion is useful. In response to question of whether job
descriptions can reference level of supervision they entail, Dr. Wilson said “yes.”
9. The ability to work in coordination with or proximity to others without being
distracted by them. Equally disabling is whether is person is distracting to others.
It was suggested that we could assess distractibility to and by others in an item
about problems working with other people. Also, it was noted that many people
are more distracted by technology (surfing the Internet, text messaging) than by
other people.
10. The ability to make simple work-related decisions. Several participants felt that
this item is unnecessary as it is too low-level. However, degree of decision making
is a fundamental dimension by which jobs vary, so some assessment of this
should be retained.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-12
11. The ability to complete a normal workday and workweek without interruptions by
psychological symptoms. Although this item is multi-faceted, it is the only item that
rates functioning over a week and it maps onto actual work demands.
12. The ability to interact appropriately with the general public. While several
participants felt that this is an important ability, it also was noted that there is no
disease or injury that selectively impairs one’s ability to interact with the general
public but not coworkers or supervisors.
13. The ability to ask simple questions or request assistance. Concern about this item
centered on the qualifier “simple.” In general, rating assertiveness was endorsed.
14. The ability to accept instruction and respond appropriately to criticism from
supervisors. Despite differences of opinion about whether to assess reactions to
“criticism,” “feedback,” or “direction,” there was broad agreement that the ability to
deal with authority and supervision at work is important to assess.
15. The ability to get along with coworkers or peers without distracting them or
exhibiting behavioral extremes. Concern was expressed about the complexity of
this item and use of the term “behavioral extremes.”
16. The ability to maintain socially appropriate behavior and to adhere to basic
standards of neatness and cleanliness. Participants favored separating hygiene
and socially appropriate behavior, as these often do not correlate and they have
different implications in terms of meeting the demands of different jobs.
17. The ability to respond appropriately to changes in the work setting. There was
broad agreement that it is important to assess flexibility in response to changing
demands.
18. The ability to be aware of normal hazards and take appropriate precautions. This
item is set so low that it does not discriminate among applicants or the ability to
meet different job demands. Essentially, lacking awareness of normal hazards or
the ability to take needed precautions probably precludes any form of
employment.
19. The ability to travel in unfamiliar places or use public transportation. Several
participants expressed doubt that this item is necessary.
20. The ability to set realistic goals or make plans independently of others. Several
participants suggested that an item assessing executive functioning would be
useful.
In response to Question 3
, all of the Roundtable participants indicated that they were
not aware of any large scale studies or research databases linking MRFC to the
performance of specific work demands in any normal, psychiatric, or neurological
population. Many small studies and some large scale studies that examined
demographic, clinical, and cognitive predictors of work outcomes have been reported,

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-13
but none of these offers the level of specificity required by SSA to link MRFC to work.
Drs. Fraser, Rogers, Bond, and Bruyère all provided references and/or PDF files of
articles of potential interest. These articles have been reviewed by the Mental Cognitive
Subcommittee and cited in the reference section of this report.
This research is chiefly found within the psychiatric vocational rehabilitation literature. A
number of these studies support social or interpersonal skills as consistently related to
job success (Becker et al., 1998; MacDonald-Wilson, Rogers, & Anthony, 2001;
Tsang et al., 2000). A fifteen-year review of the psychiatric rehabilitation literature
indicated mixed results related to psychiatric symptoms or diagnoses, but confirmed
social skills as a consistent predictor of work outcome for people with psychiatric
disabilities. MacDonald-Wilson, Rogers, and Anthony (2001) conclude that although
psychiatric diagnoses and symptoms tend to be related to poorer vocational outcomes,
there is not a high correlation as supported by the research to date.
In terms of cognitive functioning and vocational status, there are some limited studies
that indicate a relationship. Gold et al. (1999), using the Repeatable Battery for the
Assessment of Neuropsychological Status (RBANS), established significant differences
between employed and unemployed participants on the total battery score and four
index scores (immediate memory, delayed memory, attention, and language). In a later
study, Gold et al. (2002), using a full neuropsychological battery, established that
measures of IQ, attention, working memory, and problem solving were related to job
tenure as assessed over 24 months. In summarizing the existing literature, although
there are some established findings, further study is needed in relation to these
domains of interpersonal, emotional, and cognitive functioning and vocational status
(MacDonald-Wilson, Rogers, & Anthony, 2001). This research needs to be extended
outside the bounds of psychiatric rehabilitation and involve larger mainstream samples
with more discrete and standardized measures of functioning as related to successful
job tenure.
Finally, in response to Question 4
, the Roundtable participants briefly discussed their
thoughts about the most useful approaches to measurement of MRFC. Several themes
emerged from this discussion. First, it was universally recognized that any assessment
of MRFC must incorporate a longitudinal component because most mental disorders
involve some degree of functional variability over time, and some disorders, such as
recurrent major depression or bipolar disorder, are usually characterized by episodes of
impairment separated by periods of more intact functioning. One potential approach to
this would be to include ratings of frequency of impairment over time (e.g., interpersonal
conflicts could be rated in terms of frequency over time).
Another criticism was that the current ratings (not significantly limited, moderately
limited, and markedly limited) are too coarse and lack clear definitions. One approach to
improving this would be to use behaviorally anchored rating scales (BARS). Another
would be to specify intensity or complexity in quantitative terms.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-14
In the context of this discussion, Dr. Elizabeth Rasch asked for a description of
situational assessments. Dr. Rogers explained that they typically involve having a
trained rater observe while a person engages in work-related tasks. The observer then
rates the person’s engagement in work activities using rating scales, often with
behavioral anchors. The examination can take up to six hours, and it enables the
examiner to make very realistic observations of a person’s pace, persistence, self-
direction, rate of on-task behavior, etc. Dr. Bond added that a limitation of work sample
observation is that assigned tasks might bear little resemblance to the kind of work that
a given patient wants or intends to do.
Finally, there was some discussion of the need to consider additive and interaction
effects. This would require an empirical study involving relatively large samples of
workers with and without disabilities in order to test higher-order relationships among
predictors of work outcomes.
Following the Roundtable, participants were asked to revise their pre-meeting
responses to the four questions based on the discussions held in Chicago.
Dr. Schretlen took the post-meeting responses to Question 2 (or pre-meeting responses
of those who did not submit revisions), and created a matrix of psychological abilities
nominated by each participant for inclusion in an MRFC assessment. These are shown
in the table on the next two pages.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-15
Core Psychological Abilities Nominated by Roundtable Participants as Essential for Work
David Schretlen Bob Fraser Lynda Payne E. Sally Rogers Gary Bond Pamela Warren Susanne Bruyere
Information Processing and Decision Making
1
General cognitive
ability
Reasoning & problem-
solving (verbal, visual)
Cognitive ability
Capacity to learn to
new skills
Information
processing ability
2
Communication &
language
Ability to communicate (with
co-workers, supervisors &
public)
Written and oral
expression
Communication
skills
Language abilities
3 Verbal memory ability
Ability to understand &
remember verbal instructions
& work-relevant material
Memory
Memory, short and
long-term
Recall information
4 Visual memory ability
Ability to understand &
remember visual instructions
& work-relevant material
Memory
Visual-spatial
processing
5 Psychomotor speed
Ability to process information
efficiently
Speed of
processing
Motor skills &
dexterity
Speed of
information
processing
6
Attention &
distractibility
Ability to attend &
concentrate
Attention Attention; focus Avoid distractibility
7 Executive functioning
Ability to initiate, perform,
and regulate task sequences
Flexibility, executive
functioning
planning, emotional
regulation
Organizational
capacity
Adapt to ambiguity
Flexibility in
response to
competing and
changing demands
8 Other candidates
Independent
decision-making
ability
Exercise good
judgment
Judgment; Ability to
follow instructions
Ability to comply
with instructions
Interpret and
execute info;
Sequence tasks
Initiative & Persistence
1
Attendance &
punctuality
Ability to initiate & persist in
work activities
Leave the house Initiate work tasks
2
Ability to complete
tasks independently
Ability to complete
tasks independently
Motivation and work
identity
3
Persistence
(hours/day)
Persistence

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-16
David Schretlen Bob Fraser Lynda Payne E. Sally Rogers Gary Bond Pamela Warren Susanne Bruyere
4
Persistence
(days/week)
Ability to perform simple
tasks at an acceptable
quality level within
reasonable timelines
Stamina &
persistence to
consistently work 40
hrs/week
Interpersonal Functioning
1 Interpersonal friction
Ability to interact
cooperatively and flexibly (w/
supervisor, coworkers,
public)
Ability to interact
with others (co-
workers,
supervisors &
public)
The ability to work
with others on tasks
2 Response to criticism
Ability to respond to
feedback/criticism (from
supervisor, coworkers,
public)
Ability to accept
supervisory
guidance
The ability to
respond to
supervision
Effort at work
Deal with stressful
interactions
3 Assertiveness
Ability to assert positive and
negative perceptions and
feelings relative to work (w/
supervisor, coworkers,
public)
Ability to express
oneself when
needed
4 Other candidates
Ability to understand
& interpret social
cues
Social cognition
Ability to interpret
social cues
Self-Management & Self-Monitoring
1 Personal hygiene
Ability to maintain level of
personal hygiene appropriate
to workplace
Ability to maintain
acceptable hygiene
2 Disturbing behaviors
Ability to maintain organized
and socially appropriate
thinking, speech, and
behavior over the work week
Ability to control
symptoms
3 Self-monitoring
Ability to maintain an
acceptable level of personal
and social awareness

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-17
David Schretlen Bob Fraser Lynda Payne E. Sally Rogers Gary Bond Pamela Warren Susanne Bruyere
4 Other candidates
Ability to manage mood and
emotions as appropriate on
the job
emotional regulation
Affect regulation;
Stress tolerance
Affective status;
modulate mood
Ability to control
and express
emotional states
Note about method:
Need situational
assessment

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-18
In addition to the activities described above, the Mental Cognitive Subcommittee
Chairman visited the Maryland State Disability Determination Services (Maryland DDS)
office in Timonium, Maryland, on August 7, 2009. There, Dr. Schretlen interviewed
Ms. Sue Page, Director, and two medical consultants, Carla Sarno, MD (chief
psychiatrist) and Kenneth Wessell, EdD (chief psychologist). He also interviewed
Ms. Rachel Watts and Mr. Bash Kamara, both claims examiners who have worked for
Maryland DDS for 6 and 2 years, respectively. Ms. Page explained that the
Maryland DDS expects to receive between 66,000 and 72,000 new applications for
disability benefits during the current year, representing close to a 20% increase in
applications over the previous year. She explained that the Maryland DDS has
3 psychiatrists and 13 psychologists as consultants who evaluate the medical evidence
regarding mental impairments and MRFC.
In interviews, Dr. Sarno, Ms. Watts, and Mr. Kamara all reiterated the inadequate
representation of longitudinal fluctuations in all aspects of psychological functioning
taken into account by the current MRFC assessment. Dr. Sarno indicated that she relies
primarily on the Psychiatric Technique Review Form (PRTF) to capture longitudinal
aspects of psychiatric disability. All three agreed that obtaining more quantitative,
specific, and behaviorally concrete measures of psychological and interpersonal abilities
could greatly facilitate their work, but only if linkages between these abilities and job
demands are more transparent than they are under the current system. Dr. Wessel,
who has worked for 23 years as a consulting psychologist for DDS, said that he finds
the current MRFC assessment adequate to adjudicate claims, and that the larger
problem is obtaining the medical evidence needed to rate items and write a narrative
using the MRFC form.
The Subcommittee also reviewed working papers prepared by the SSA, input from end
users (comments, questions, and suggestions) based on surveys, and input from
several professional organizations. Discussion of the information received from these
sources will be presented in the OIDAP report.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-19
Mental Cognitive Subcommittee Recommendations
Based on a review of the scientific literature, presentations by staff members from the
SSA, DDS, and various professional organizations to the Subcommittee and OIDAP,
presentations by OIDAP Subcommittee panelists, input from experts who participated in
the Chicago Roundtable, interviews of DDS staff, and internal discussions, the Mental
Cognitive Subcommittee reached several conclusions that it deems relevant to the
development of a new Occupational Information System. These conclusions and the
recommendations to which they lead are outlined below.
Recommendation 1: The conceptual model of psychological abilities required to do
work, as reflected by the current MRFC assessment, should be revised. The revised
model should: (i) redress shortcomings of SSA’s current conceptual model of the
psychological abilities required to do work, (ii) be based on sound scientific evidence
where possible, (iii) lead logically to elements that can be reliably assessed and
empirically tested for predictive validity, and (iv) retain elements of the current MRFC
assessment that are consistent with scientific evidence, reliably measurable, and valid
predictors of the ability to work, as this will provide continuity with the existing system.
As documented in previous sections, it is widely recognized both within and outside of
the SSA that the current MRFC assessment is based on a simplistic conceptual model
of the psychological abilities that are required to do work. Much of the language that
appears in Form SSA-4734-F4-SUP was drawn directly from the Dictionary of
Occupational Titles (DOT) in response to the need for an instrument to complement the
physical RFC assessment. However, the MRFC was never subjected to rigorous study
to verify its reliability and predictive validity of the elements that comprise it.
Recommendation 1a: Any revision of the current MRFC assessment should redress the
following shortcomings: (1) the underrepresentation of neurocognitive abilities, (2) the
reliance on coarse and underspecified categories to rate residual abilities, (3) the failure
to account for longitudinal fluctuations in mental abilities, (4) the inclusion of elements
that combine disparate abilities, (5) the failure to recognize differences in the predictive
power of various abilities, and (6) the large inferential leaps required to match residual
abilities with job demands.
Studies of work outcome among persons with mental disorders typically regress work
outcomes (e.g., employment, work performance, job loss) on multiple predictors, such
as demographic variables, clinical characteristics, and measures of cognitive or social
functioning. While hundreds of such studies have been published, the Subcommittee
found none that examined the accuracy with which a broad set of psychological abilities
predicts whether individuals with mental disorders can work and what occupational
demands they can meet, independent of their demographic background and clinical
symptoms. These are the questions that the SSA must answer to adjudicate disability
claims. However, research has shown that neurocognitive test performance strongly
predicts whether persons with many different mental disorders, neurological conditions,
and medical diseases can work.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-20
Given evidence that neurocognitive functioning predicts work outcomes among persons
with mental and physical disorders, the Subcommittee reviewed factor analytic studies
that have examined the underlying, latent structure of cognition. The aim was to develop
a parsimonious list of abilities that the SSA might use to link with occupational demands
that will be described by the new OIS. Many different factor structures have been found
by previous studies involving healthy and mentally disordered samples. Consequently,
previous research has not yielded a single, broadly replicated factor structure to guide
the Subcommittee’s recommendations. On the other hand, the same research provides
scientific support for several alternate models of cognitive architecture. This affords the
Subcommittee and the SSA some latitude in deciding how to balance parsimony with
specificity in choosing the conceptual model that will drive instrument development.
Recommendation 1b
: The SSA should include aspects of neurocognitive functioning in
a revised conceptual model of MRFC. This recommendation responds to the perceived
failure of the current MRFC assessment to account for impairments of specific cognitive
abilities. These can result from traumatic brain injury, other acquired brain disorders,
developmental disorders that cause cognitive deficits without mental retardation, and
various psychiatric and medical conditions in which other symptoms are primary but that
also involve cognitive morbidity, such as schizophrenia. Inadequate assessment of
neurocognitive impairments was noted as a shortcoming of the current MRFC
assessment by every group from which the Subcommittee obtained input. Including
neurocognitive abilities in a revised MRFC assessment could greatly improve SSA’s
ability to identify under-recognized impairment-related limitations that preclude the
ability to do work.
The most parsimonious approach would be to assess general cognitive ability (“g”),
which can be reliably measured and expressed with a single number. Numerous studies
show that g predicts the ability to do work. Further, when job incumbents are compared,
they show sizable differences on tests of g corresponding to differences in job
complexity. However, tests of g are less sensitive to the deleterious effects of mental
disorders than tests of some other cognitive abilities whose impairment can also limit a
person’s ability to work. Also, empirical research might show that another aspect of
cognitive functioning predicts the ability to do work better than g. For these reasons, the
Subcommittee recommends that the SSA adopt a multi-dimensional model of cognitive
functioning for a revised MRFC assessment. While the provisional “core mental residual
functional capacities” (see below) incorporate a six-factor model of neurocognitive
functioning, the Subcommittee recognizes that alternate models with fewer or different
factors might provide a more efficient assessment with little loss of predictive validity.
Regardless of the number and specific cognitive abilities that SSA ultimately decides to
include in a revised MRFC assessment, it will be important to empirically study and
eliminate any adverse disparate impact that assessing cognitive functioning could have
on specific subgroups of persons applying for disability benefits, such as women, older
adults, and racial or ethnic minorities.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-21
Because human behavior is multiply-determined, it is impossible to parse psychological
abilities that are essential for work into completely orthogonal dimensions. For example,
the ability to focus on a task likely reflects not only an underlying trait-like attentional
capacity, but also such state-like influences as wakefulness, medication side-effects,
the nature of ambient distractions, the presence of intrusive thoughts, etc. Nevertheless,
the Subcommittee concluded that it is useful to group abilities that are essential for work
into broad categories that are relatively independent. The SSA’s current assessment of
MRFC organizes abilities into four broad categories: (1) understanding and memory,
(2) sustained concentration and persistence, (3) social interaction, and (4) adaptation.
Various users (e.g., DDS medical consultants) and Roundtable participants agreed that
the existing organization is imperfect but workable. The Subcommittee decided to
recommend revising, rather than discarding, this organization, as described below.
Recommendation 2: The Subcommittee recommends that the SSA reorganize the
elements of its MRFC into the following four categories: (1) neurocognitive functioning,
(2) initiative and persistence, (3) interpersonal functioning, and (4) self-management.
This revised conceptualization of MRFC elements provides greater homogeneity of
within-category elements and clearer between-category distinctions of MRFC content
than the organization implied by Form SSA-4734-F4-SUP.
Recommendation 3: The Subcommittee recommends that SSA adopt the psychological
abilities shown under each category in the outline below entitled “Core Mental Residual
Functional Capacities.” The 15 abilities specified in this outline provide a comprehensive
but parsimonious assessment of the four major categories of psychological functioning
required to do work. However, the Subcommittee recognizes that the SSA might choose
to discard or replace some of these 15 abilities, or add others that are not listed below.
Therefore, a brief explanation of why each element of the proposed MRFC assessment
was included and worded as shown is presented below. We also identify other abilities
that the Subcommittee considered but excluded from the proposed outline, and explain
the reasoning that led to each decision.
Core Mental Residual Functional Capacities
Psychological residual functional capacities are conceptualized under four major
categories of functioning. Following each specific ability outlined below is a statement
intended to elaborate its meaning in greater detail.
(A) Neurocognitive functioning
1. General cognitive/intellectual ability
(how well a person can reason, solve
problems, and meet cognitive demands of varied complexity)
2. Language & communication
(how well a person can understand spoken or
written language, communicate his or her thoughts, and follow directions)
3. Memory acquisition (how well a person can learn and remember new
information, such as a list of words, instructions, or procedures)

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-22
4. Attention & distractibility (how well a person can sustain the focus of
attention in a work environment with ordinary distractions)
5. Processing speed (how quickly a person can respond to questions and
process information)
6. Executive functioning (how well a person can plan, prioritize, organize,
sequence, initiate, and execute multi-step procedures)
(B) Initiative & persistence
7. Attendance/Punctuality (how consistently a person can leave his/her
residence and maintain regular attendance and punctuality)
8. Initiative (whether a person can start and perform tasks once they are
explained without an unusual level of supervision)
9. Pace/Persistence (whether a person can continue performing understood
tasks at an acceptable pace for a normal work week without excessive
breaks)
(C) Interpersonal functioning
10. Cooperation (the extent to which a person’s interactions with others are
free of irritability, argumentativeness, sensitivity, or suspiciousness)
11. Response to criticism (how well a person responds to criticism, instruction,
and challenges)
12. Social cognition (whether a person can navigate social interactions well
enough to respond appropriately to social cues, state his or her point of
view, and ask for help when needed)
(D) Self-management
13. Personal hygiene
(how well a person maintains an acceptable level of
personal cleanliness and socially appropriate attire)
14. Symptom control
(how well a person inhibits disturbing behaviors, such as
loud speech, mood swings, or responding to hallucinations)
15. Self-monitoring (how well a person can distinguish between acceptable
and unacceptable work performance)
Under the first category, neurocognitive functioning, the Subcommittee recommends
that the SSA adopt a six-factor model. Each of the constituent abilities has been found
to predict either the ability to work or level of occupational attainment among persons
with various mental disorders and/or healthy adults.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-23
General cognitive/intellectual ability (g) is the most robust predictor of occupational
attainment, and corresponds more closely to job complexity than any other ability. The
wording underscores the closer association of g with “fluid” (reasoning) than
“crystallized” (knowledge) intellectual abilities.
Language & communication refer to receptive and expressive language abilities to the
extent that these can be impaired by disease or injury (as in post-stroke aphasia,
neurodevelopmental language disorder, etc.). The Subcommittee recognizes that this
construct overlaps language “skills,” such as literacy, fluency in English, and mastery of
the rules of grammar. Complicating this overlap is the fact that individuals who develop
aphasia usually suffer some loss of these skills as manifestations of the underlying
primary language disorder. It also should be noted that language ability differs from
speech production.
Memory acquisition refers to the ability to encode, store, and retrieve new information.
Impairment of this ability is referred to as anterograde amnesia. The Subcommittee
excluded the loss of remote autobiographical memories or over-learned skills (i.e.,
retrograde amnesia) from this ability for two reasons. The first is that it is extremely rare
for a person to develop retrograde amnesia in the absence of anterograde amnesia as a
result of a brain disease or injury. The second is that claimed retrograde amnesia in the
absence of anterograde amnesia is a common presentation of feigned memory
impairment. Consequently, the Subcommittee intended to emphasize anterograde
memory impairment in the definition of this ability.
Attention & distractibility refer primarily to the ability to focus attention and resist
distraction. The Subcommittee recognizes that this partially overlaps the ability to
persist in working at a task, but construed the latter as placing greater demands on the
ability to stay engaged over days to weeks. The description of this ability is intended to
emphasize the capacity to focus attention despite environmental or internal distractions.
Processing speed
refers to how quickly a person can process simple information, such
as judging whether two numbers are the same. Simple processing speed has been
found to account for variability in how well people perform many everyday activities,
including untimed tasks. Individual differences in processing speed can be measured
quickly and reliably with pencil-and-paper or computerized tests, but they generally are
not observable at the behavioral level. Consequently, the Subcommittee notes that it
would be particularly important to determine how reliably this ability can be rated from
medical records, and whether such ratings have predictive validity.
Executive functioning
probably does not represent a unitary ability, as is apparent in its
description. Because of this, it might be impossible to assess executive functioning with
a single measure. The Subcommittee recommends including it because measures of
executive functioning predict work outcomes among persons with mental disorders.
Clinical performance-based tests of executive functioning, such as the Trail Making
Test, Tower of London, and Stroop Color-Word Test, frequently are timed and thereby
conflate the assessment of executive functions with processing speed and attentional

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-24
demands. In addition, it should be noted that behavioral ratings and performance-based
tests of executive functioning rarely show significant statistical correlation in studies that
administer both types of measures to the same participants.
Attendance/Punctuality refers to the ability to leave one’s residence, attend work
regularly, and be punctual within customary tolerances. This corresponds to Item 7 on
Form SSA-4734-F4-SUP. As noted above, there was widespread agreement among the
Roundtable participants that this item be retained.
Initiative refers to the ability to start and perform tasks once they are explained without
an unusual level of supervision. The wording of this item’s description was intended to
emphasize both the ability to initiate tasks once they are understood, and the extent to
which a person is capable for working independently. While the ability to initiate work is
not represented on the existing MRFC assessment, the ability to perform understood
tasks without special supervision corresponds to Item 8 on Form SSA-4734-F4-SUP.
Pace/Persistence involves the ability to perform understood tasks at an acceptable pace
for a week without excessive breaks. This corresponds to Item 11 on Form
SSA-4734-F4-SUP. Again, despite the fact that this ability clearly is multiply-determined
and therefore susceptible to impairment by many different factors, there was
widespread agreement that this ability should remain in a revised MRFC assessment
because it is sensitive to longitudinal fluctuations in everyday functional competence.
Cooperation refers to freedom from interpersonal friction. Impairments of this ability can
take the form of argumentativeness, excessive sensitivity, suspiciousness, hostility, etc.
The current MRFC includes several items (12, 14, & 15) that aim to separately assess
interpersonal difficulties with supervisors, coworkers, and the general public. While the
Subcommittee realizes that occupations differ in the nature, frequency, and closeness
of interpersonal contact they entail, there is little reason to believe that mental disorders
or injuries impair a person’s ability to cooperate with specific classes of people
(e.g., only coworkers).
Response to criticism refers to the ability to accept instruction, directions, and criticism
from others. This corresponds to Item 14 on Form SSA-4734-F4-SUP, which frames the
ability solely in relation to instruction or criticism by supervisors. The Subcommittee
again recommends broadening this item to assess one’s ability to accept instruction and
respond appropriately to criticism, regardless of its source.
Social cognition
refers to abilities that enable people to respond appropriately to others.
Closely aligned with the concept of emotional intelligence, social cognition is thought to
depend on a person’s ability to interpret nonverbal communication, empathize with
others, and recognize when another person’s point of view differs from one’s own. The
current MRFC assessment does not capture social cognition, and the Subcommittee
recommends adding it because several mental disorders and injuries can impair social
cognition, and thereby disrupt normal social and emotional reciprocity.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-25
Personal hygiene involves the ability to maintain an acceptable level of personal
cleanliness, grooming, and socially appropriate attire. This largely overlaps Item 16 on
Form SSA-4734-F4-SUP, but adds the element of wearing socially appropriate attire.
The rationale for this addition is that occupations vary not only in what level of personal
hygiene is acceptable, but also in the extent to which employees are expected to
recognize and don attire that is acceptable in the work environment.
Symptom control
refers to a person’s ability to inhibit the expression of disturbing
symptomatic behaviors, such as loud or pressured speech, vocal tics, extreme mood
swings, or responding to hallucinations. The Subcommittee recommends adding this
item because of wide variation in how completely and consistently persons with mental
disorders can control the manifestation of symptomatic behaviors. Likewise, it is
recognized that occupations likely differ in how much disturbing behaviors are tolerated.
Self-monitoring
refers to a person’s ability to monitor and evaluate the quality of his own
task performance. The Subcommittee recommends adding this item because mental
disorders and injuries can impair a person’s ability to perceive the accuracy of his or her
own task performance, especially when tasks require precision.
In addition to these 15 core psychological and interpersonal abilities that are
recommended for assessment in a revised MRFC assessment, several others were
nominated but not included. Because the SSA might later consider adding one or more
of these, a brief discussion of the Subcommittee’s rationale for rejecting these items is
offered next.
Several Roundtable participants and end users suggested that the revised MRFC
should assess Judgment. The major reason this does not appear on the list of abilities
recommended for inclusion is that the underlying construct is difficult to define, and the
Subcommittee doubts that it can be reliably assessed. If the SSA decides to continue
relying primarily on informant ratings (as it does now), isolated incidents that appear to
involve poor judgment are likely to be weighted excessively by some adjudicators and
dismissed by others. Wearing insufficient clothing in cold weather, failing to look both
ways before crossing the street, giving money to a swindler, having an extramarital
affair, driving while intoxicated, spending money excessively, smoking cigarettes
despite having emphysema, driving while using a cellular phone, and criticizing one’s
supervisor could all be construed as failures of judgment. However, (1) they are likely to
have very different consequences, (2) their impact on the ability to work are likely to
vary enormously, and (3) they could all be attributed to factors other than judgment, per
se (e.g., cognitive impairment, addiction, etc.). For these reasons the Subcommittee
decided not to recommend that the revised MRFC attempt to assess judgment.
Others suggested that the ability to modulate mood
or regulate emotion be included in a
revised MRFC assessment. In fact, the Subcommittee did add an item (14) that is
intended to assess a person’s ability to inhibit the expression of symptomatic behavior,
which certainly could include severely depressed, elated, or angry mood states.
However, the reason a separate rating of mood state was not included in the list of

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-26
recommended abilities for MRFC assessment is that feeling sad or depressed does not,
in itself, preclude the ability to work. Many people work despite suffering from sadness,
despair, anxiety, or hopelessness. Rather, it is only when depression causes one to
neglect personal hygiene, not get out of bed, lose focus on tasks, slow down one’s
thinking, or stop avoid required interactions with coworkers that difficulty modulating
one’s mood impairs the ability to work. Thus, this item was not thought to convey useful
incremental information above and beyond those recommended in the core list.
A third ability suggested for inclusion is stress tolerance. After beginning a job, persons
with mental disorders often find work increasingly stressful. Over time they might worry
that coworkers dislike them, develop insomnia, or stop taking prescribed medications. If
the person comes to work late and gets reprimanded, he or she might quit rather than
respond adaptively. While the factors leading to such job failures can vary enormously,
persons with mental disorders often are less able to cope effectively with stressors than
psychologically healthy adults. Although only one Roundtable participant nominated
stress tolerance for inclusion in a revised MRFC assessment, the Subcommittee
recommends that the Panel urge SSA to consider the possibility of adding it to the list of
15 items. However, the Subcommittee was not prepared to make this recommendation
for several reasons. First, because poor stress tolerance usually manifests as a series
of maladaptive responses to stressors, reliable assessment of it almost certainly would
require longitudinal data. Second, poor stress tolerance is very difficult to define in
operational terms. Third, stressors that lead to decompensation among persons with
low stress tolerance due to neuropsychiatric impairment probably have very little to do
with job demands, per se. More often, they have to do with problems outside the work
place, such as family conflicts, or than involve illness-related internal conflicts. For this
reason, while illnesses and injuries can impair a person’s stress tolerance, it is precisely
because the can lead to unexpectedly severe reactions to idiosyncratic stressors and
seemingly trivial events that it may be impossible to establish any correspondence
between this ability and the demands of work.
Recommendation 4
: The Subcommittee recommends that the Panel provide ongoing
consultation to the OIS Project’s psychometrician as the SSA develops items for data
collection. More generally, the Subcommittee recommends that the SSA consider the
possibility that MRFC abilities be assessed using different methods (e.g., informant
ratings for some, performance-based measures for others) and different scales (e.g.,
Likert, behaviorally-anchored ratings, percentiles, etc.) for different categories of
psychological and interpersonal abilities.
Recommendation 5
: Finally, the Subcommittee recommends a series of studies to
examine the reliability and predictive validity of any instruments developed to assess
residual functional capacities and occupational demands as part of the OIS Project. The
recommended studies are described in greater detail below.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-27
Suggested Studies
The Subcommittee recommends that the SSA conduct a series of studies and data
analyses. Before describing these, the Subcommittee notes that the SSA compiled a
document entitled “Data on the top 100 Occupations by Employment for 2008 and
Projected 2016.” One table in this document shows the top 100 occupations by total
persons employed for 2008 based on the Household Data Annual Averages. These
data were drawn from the Current Population Survey, a monthly survey conducted by
the Bureau of Census for the BLS. The top 100 occupations are based on SOC levels.
A few represent occupational titles that encompass more than one detailed occupation.
The occupations are ranked by the total employed (in thousands). Approximately 65%
of persons in the U.S. labor force work in one of these 100 occupations. A reformatted
version of this table appears below.
Occupation
(Standard Occupational Classification)
Total
Employed
(Thousands)
Occupation
(Standard Occupational Classification)
Total
Employed
(Thousands)
Managers, all other (managers not listed
separately)
3,473
Medical assistants and other healthcare
support occupations
831
First-line supervisors/managers of retail
sales workers 3,471 Education administrators 829
Retail sales persons 3,416
Human resources, training, and labor
relations specialists 803
Driver/sales workers and truck drivers 3,388
Hairdressers, hairstylists, and
cosmetologists
773
Secretaries and administrative assistants 3,296 Farmers and ranchers 751
Cashiers 3,031 Other teachers and instructors 751
Elementary and middle school teachers 2,958 Inspectors, testers & sorters 751
Registered nurses 2,778 Management analysts 731
Janitors and building cleaners 2,125 Social workers 729
Waiters and waitresses 2,010 Food preparation workers 724
Cooks 1,997 Miscellaneous agricultural workers 723
Customer service representatives 1,908 Preschool & kindergarten teachers 685
Nursing, psychiatric, and home health
aides
1,889 Counselors 674
Laborers and freight, stock, and material
movers, hand 1,889 Police and sheriff’s patrol officers 674
Accountants and auditors 1,762 Bus drivers 651
Chief executives 1,655 Painters, construction & maint. 647
Construction laborers 1,651
First line supervisors/managers of food
preparation and servers 635
First line supervisors/managers of office
and administrative support workers
1,641
Pipelayers, plumbers, pipefitters, and
steamfitters
606
Carpenters 1,562 Welding, soldering, & brazing workers 598
Stock clerks and order filers 1,481 Insurance sales agents 573
Maids and housekeeping cleaners 1,434 Industrial truck and tractor operators 568
Bookkeeping, accounting & auditing clerks 1,434 Licensed practical/vocational nurses 566
Receptionists and information clerks 1,413 Medical & health services managers 561

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-28
Occupation
(Standard Occupational Classification)
Total
Employed
(Thousands)
Occupation
(Standard Occupational Classification)
Total
Employed
(Thousands)
Sales representatives, wholesale and
manufacturing
1,343
Property, real estate, and community
service managers
558
Child care workers 1,314
Office and administrative support
workers, all other 558
First line supervisors/managers of non-
retails sales workers 1,287 Shipping, receiving, and traffic clerks 543
Grounds maintenance workers 1,262 Computer programmers 534
Construction managers 1,244 Sales representatives & service 521
Postsecondary teachers 1,218
Billing and posting clerks and machine
operators
516
Secondary school teachers 1,210 Computer & info systems managers 475
Office clerks, general 1,176 Tellers 466
Financial managers 1,168 Maintenance & repair workers 461
Miscellaneous assemblers and fabricators 1,050
Health diagnosing and treating
practitioner support technicians 447
Food service managers 1,039 Clergy 441
Computer software engineers 1,034 Industrial machinery mechanics 439
Teacher assistants 1,020 Personal financial advisors 430
Lawyers 1,014 Network systems and data analysts 422
General and operations managers 985 Engineering technicians 416
Real estate brokers and sales agents 962 Data entry keyers 415
Production workers, all other 958 Machinists 409
Marketing and sales managers 922 Bailiffs, correctional officers & jailers 403
Physicians and surgeons 877
Operating engineers and other
construction equipment operators
398
Electricians 874
Heating, air conditioning, and
refrigeration mechanics 397
First line supervisors/managers of
productions and operating workers 874 Loan counselors and officers 392
Personal and home care aids 871 Packers and packagers, hand 391
Security guards & gaming surveillance
officers
867
Securities, commodities, and financial
services agents
388
Automotive service techs & mechanics 852 Special education teachers 387
First line supervisors/managers of
construction trades and extraction workers
844 Computer support specialists 382
Computer scientists and systems analysts 837 Postal service mail carriers 373
Designers 834 Taxi drivers and chauffeurs 373
Although not shown in this report, the manual for the Wonderlic Personnel Test
(WPT; 1992) includes a figure that presents the mean and median scores of persons
employed in 72 occupations. Attorneys, for example, produced the highest mean and
median WPT scores, while packers produced the lowest WPT scores of the
72 occupational groups. Occupations that appear in the top 100 table were cross-
referenced with the WPT figure. This revealed that the most common occupations in the
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-29
United States are filled by individuals who represent a very broad spectrum of general
cognitive ability based their WPT scores. This exercise suggests that occupational
differences in the WPT or some other measure of g among successful job incumbents
might serve as an ideal measure of overall job complexity.
Based on this reasoning, the Subcommittee recommends that the SSA conduct a study
in which all of the revised physical and mental residual functional capacity measures are
administered to a nationally representative sample of persons who have worked for at
least 6 months (i.e., “successful” incumbents) in one of the 150 to 200 most common
occupations in the U.S. economy. If 50 to 75 successful incumbents in each occupation
are assessed, this will require 7,500 to 15,000 study participants.
By characterizing the physical and psychological abilities of a broadly representative
sample of successful job incumbents using the measures developed for the OIS, it will
be possible to arrange all 150−200 occupations hierarchically in terms of each
person-side characteristic. By reflection, each such hierarchy can be interpreted to
reflect the extent to which the underlying ability is required by each job. In this way,
occupational demands for lifting could be arranged from most to least by comparing the
maximum weight incumbents of each occupational group can actually lift when tested.
Likewise, differences in job complexity could be defined by arranging the mean scores
of job incumbents on some measure of g by occupational group. The occupation whose
incumbents earn the highest mean score would be identified as demanding the most
general cognitive ability. The occupation whose incumbents earn the lowest score
would be identified as requiring the least general cognitive ability. By documenting the
distribution of scores on each physical and psychological measure for all 150−200
occupations surveyed in this way, the SSA would be able to specify where any given
disability applicant’s measured abilities fall in the distribution of abilities required by
each occupation. The same principle would apply to every measured person-side
characteristic and every job-side demand.
The results of this study could solve many problems. First, measuring the physical and
psychological abilities of successful job incumbents would provide empirical data about
the actual abilities required to perform each occupation. Second, by studying only the
150−200 most common occupations, residual abilities of claimants will be compared to
the requirements of occupations that are widely available. (Based on the table above, it
is likely that the top 150−200 occupations include at least 65% of all jobs in the U.S.
economy.) Third, by assessing both physical and psychological abilities of successful
job incumbents, the SSA would obtain critical information about the demands of specific
occupations for linking with patterns of residual abilities shown by individual disability
benefits. Fourth, this approach would greatly decrease the “inferential leap” currently
required between residual functional capacities as assessed by the SSA and
occupational demands as described in the DOT. Fifth, comparing the residual physical
and mental abilities of persons who have been adjudicated as unable to work with the
distributions of corresponding abilities among successful job incumbents could provide
crucial scientific data to help the SSA determine what levels of RFC are too low to work
in specific occupations. Finally, recording evidence about medical conditions that
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-30
successful job incumbents have could provide quantitative data about what residual
capacities enable persons with a medical condition to work.
In addition to this normative study, the Subcommittee recommends that a study be
conducted of claimants for disability benefits and SSI/SSDI beneficiaries who have been
adjudicated as unable to work. By administering the revised physical and mental
residual functional capacity instruments along with the current instruments, the SSA will
be able to determine which specific measures best distinguish individuals who are able
to work (with or without medical conditions) and those who file disability claims and/or
are adjudicated as disabled from working under current SSA rules.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-31
References
Becker, D. R., R. E. Drake, et al. (1998). "Job terminations among persons with severe mental illness
participating in supported employment." Community Mental Health Journal
34(1): 71-82.
Bond, G. R. and R. E. Drake (2008). "Predictors of competitive employment among patients with
schizophrenia." Current Opinion in Psychiatry
21(4): 362-369.
Purpose of review: Recently published studies examining predictors of competitive employment
for patients with schizophrenia are reviewed. Recent findings: Researchers continue to examine
predictors of employment among three types of variables: patient characteristics,
environmental factors, and interventions. Provision of supported employment is the strongest
predictor of competitive employment in this population, while patient predictors continue to
show modest associations with outcomes. Environmental factors, including societal and cultural
influence, local economy, labor laws, disability policies, and governmental regulations, are
presumed to have major influences on employment, but these factors have been little studied.
Summary: Given the strong and consistent evidence base for the effectiveness of supported
employment in helping individuals with schizophrenia achieve competitive employment, mental
health planners should make access to this practice a high priority. Barriers to implementation
of supported employment, including finance, organization, integration, training, and
supervision, need to be systematically addressed. The field currently lacks an adequate
understanding of the role of societal, cultural, and regulatory factors in facilitating and hindering
employment outcomes; such research is much needed. (PsycINFO Database Record (c) 2009
APA, all rights reserved) (from the journal abstract)
Bond, G. R. and M. H. Friedmeyer (1987). "Predictive validity of situational assessment at a psychiatric
rehabilitation center." Rehabilitation Psychology
32(2): 99-112.
Used situational assessment to predict employment outcomes for 77 individuals (mean age 24.5
yrs) attending a community psychiatric rehabilitation program. The assessment form was a 22-
item checklist comprised of 4 dimensions: work readiness, work attitudes, interpersonal
relations, and work quality. Ratings were made in 2 work settings: prevocational work crews and
transitional employment. Situational assessment predicted outcome better than did work
history. Staff ratings were significantly higher for Ss working in transitional employment,
although ratings made in both settings were predictive of later employment outcomes. It is
concluded that situational assessment may be a method better suited for screening out
members who have poor work potential than selecting members who will definitely succeed.
(PsycINFO Database Record (c) 2009 APA, all rights reserved)
Bruyere, S. M. (2005). "Using the International Classification of Functioning, Disability and Health (ICF) to
promote employment and community integration in rehabilitation." Rehabilitation Education
19(2): 105-
117.
The current varied definitions of disability and successful outcomes of rehabilitation service
delivery make comparisons across service systems difficult in most cases. The World Health
Organization's International Classification of Functioning, Disability and Health (ICF) has the
potential to assist vocational rehabilitation administrators, policymakers, and practitioners with
creating a transferable conceptual framework for defining indicators of successful outcomes in
the integration of persons with disabilities into the workforce and community. This article
provides a review of selected literature on applications of the ICF to medical rehabilitation,

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-32
employment, and community participation for persons with disabilities. In addition, the next
steps to make better use of this framework in applications to vocational rehabilitation service
delivery, counselor education, and research are discussed. (PsycINFO Database Record (c) 2009
APA, all rights reserved) (from the journal abstract)
Bruyere, S. M., S. A. Van Looy, et al. (2005). "The International Classification of Functioning, Disability
and Health: Contemporary Literature Overview." Rehabilitation Psychology
50(2): 113-121.
This article reviews the literature from the 3 years since the International Classification of
Functioning, Disability and Health's (ICF's) endorsement, focusing on those articles that discuss
(a) what the ICF means and how it can be used; (b) the general utility of the ICF for specific
fields, such as nursing, occupational therapy, speech-language pathology, and audiology; (c)
examples of applications for classification in particular disorders, such as chronic health
conditions, neuromusculoskeletal conditions, cognitive disorders, mental disorders, sensory
disorders, and primary and secondary conditions in children; (d) uses of the ICF to recode prior
work across multiple surveys and across country coding schemes on disability-related national
survey items; and (e) governmental uses of the ICF in the United States and selected countries
abroad. Future directions needed to effectively implement the ICF across rehabilitation policy,
research, and practice are discussed. (PsycINFO Database Record (c) 2009 APA, all rights
reserved) (from the journal abstract)
Burkhauser, R. V., J. S. Butler, et al. (2001). "How policy variables influence the timing of applications for
Social Security Disability Insurance." Social Security Bulletin
64(1): 52-83.
This article analyzes the impact of policy variables--employer accommodations, state Social
Security Disability Insurance (DI) allowance rates, and DI benefits--on the timing of an
application for DI benefits by workers with a work-limiting health condition starting when their
health condition first begins to bother them. The analysis uses a rich mixture of personal and
employer characteristics from the Health and Retirement Study linked to Social Security
administrative records. We find that most workers do not apply immediately for DI benefits
when they are first bothered by a health condition. On the contrary, the median working-age
man with a work-limiting condition waits 7 years after that time before applying, and the
median working-age woman waits 8 years. Although the risk of applying for benefits is greatest
in the year following onset, only 16 percent of men and 13 percent of women in our sample
apply within the first year, and the risk of application falls thereafter. That finding suggests that
institutional factors, in addition to health factors, may play a role in the timing of DI applications.
Using kernel density estimates of the distribution of application and nonapplication ordered by
state allowance rates (the rate of acceptance per DI determination in each state), we find that
both men and women who live in states with high allowance rates are disproportionately more
likely to apply for benefits in the first year after their condition begins to bother them than are
those in states with low allowance rates. Using life-table analysis, we also find that men and
women who are accommodated by their employers are significantly less likely to apply for DI
benefits in each of the first few years after their condition begins to bother them than are those
who are not accommodated. On the basis of this evidence, we include these policy variables in a
model of the timing of DI application that controls for other socioeconomic variables as well as
health. Using a hazard model, we find that workers who live in states with higher allowance
rates apply for DI benefits significantly sooner than those living in states with lower allowance
rates following the onset of a work-limiting health condition. Workers who are accommodated

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-33
following the onset of a work-limiting health condition, however, are significantly slower to
apply for DI benefits. Using the mean values of all explanatory variables, we estimate the
relative importance of changes in these policy variables on the speed with which workers apply
for benefits after onset. We find that the mean time until application for men is 10.22 years.
Universal accommodations following onset would delay application by 4.36 years. In contrast, a
20 percent decrease in state allowance rates would delay application by only 0.88 years. For
working-age women, the average expected time until application once a condition begins to
bother them is 10.58 years. Universal accommodations would delay that by 3.76 years, and a 20
percent decrease in allowance rates would delay it by 1.47 years. A complication in this analysis
is that the policy variables are to some degree endogenous. Accommodation is probably offered
more often to workers who want to continue working. Allowance rates are chosen by states on
the basis of federal policy and local choices and probably in part on the health condition of
workers in the state. Therefore, our estimates are upper bounds of these policy effects. Still, we
believe we provide evidence that the social environment faced by workers with work-limiting
health conditions can significantly influence their decision to apply for DI benefits, holding their
specific health conditions constant.
Desmarais, L. B. and P. R. Sackett (1993). "Investigating a cognitive complexity hierarchy of jobs." Journal
of Vocational Behavior 43(3): 279-297.
Investigated the construct validity of the Occupational Aptitude Patterns (OAP) Map, an
occupational classification system based on ability requirements, by placing the positions held
by a large, nationally representative sample of full-time employed, young, civilian adults into the
classification system. Results largely supported the OAP Map structure. The OAP Map captured
differences across jobs in their requirements for general cognitive ability, although the overlap
across job clusters was large. The Map differentiated jobs also on the basis of their
requirements for specific abilities (e.g., scientific/mechanical ability), once the effects for
general cognitive ability requirements were taken into account. (PsycINFO Database Record (c)
2009 APA, all rights reserved)
Dickinson, D., A. S. Bellack, et al. (2007). "Social/communication skills, cognition, and vocational
functioning in schizophrenia." Schizophrenia Bulletin
33(5): 1213-20.
Deficits in social/communications skills have been documented in schizophrenia, but it is unclear
how these deficits relate to cognitive deficits and to everyday functioning. In the current study,
social/communication skills performance was measured in 29 schizophrenia patients with a
history of good vocational functioning (GVF) and 26 with a history of poor vocational functioning
(PVF) using a role-play-based social skills assessment, the Maryland Assessment of Social
Competence (MASC). A battery of standard cognitive tasks was also administered. MASC-
indexed social skills were significantly impaired in PVF relative to GVF patients (odds ratio = 3.61,
P < .001). Although MASC social skills performance was significantly associated with cognitive
performance in domains of verbal ability, processing speed, and memory, the MASC
nevertheless remained an independent predictor of vocational functioning even after
controlling for cognitive performance. Social/communications skills predict vocational
functioning history independently of cognitive performance, and social skills measures should be
considered for inclusion in test batteries designed to predict everyday functioning in
schizophrenia.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-34
Fraser, R. T. and D. C. Clemmons (2000). Traumatic brain injury rehabilitation: Practical vocational,
neuropsychological, and psychotherapy interventions. Boca Raton, FL US, CRC Press.
This book presents innovative guidelines for allied health members of the traumatic brain-injury
rehabilitation team with information to help achieve more successful vocational and
psychosocial outcomes. It provides a clear overview of critical components of
neuropsychological information and the use of this information in vocational planning; examples
of functional areas of cognition and neuropsychological assessment; the linkages between
cognitive and behavioral impairments; the different categories of assistive technology;
psychotherapy and behavioral interventions as well as successful vocational interventions; and
models of work access, including methods of supported employment, the development of a
tailored job coaching program, and the specifics of utilizing natural supports. This book is useful
to anyone involved in neurorehabilitation, vocational rehabilitation, rehab psychology,
neuropsychology, and students in counseling programs or studying medical aspects of disability.
(PsycINFO Database Record (c) 2009 APA, all rights reserved) (from the cover)
Fraser, R. T., E. Johnson, et al. (In press). Using neuropsychological information in vocational planning:
perspective for clinical practice. A practical guide to neuropsychological testing for patients,
practitioners and other professionals. E. Arzubi and E. Mambrino. New York, Springer Publishing
Company.
This chapter provides a practical overview of the benefits of using neuropsychological testing in vocational
rehabilitation planning. A major emphasis of the chapter is on the interplay between neuropsychologists
and vocational rehabilitation staff in optimizing the utility of the neuropsychological report in the work
planning effort.
Fraser, R. T., D. Vandergoot, et al. (2004). "Employment outcomes research in vocational rehabilitation:
Implications for Rehabilitation Counselor (RC) training." Journal of Vocational Rehabilitation
20(2): 135-
142.
This paper reviews salient categories of rehabilitation programs' employment outcomes
research, as recently presented by the authors at the May 2002 "Bridging Gaps" conference,
sponsored by the National Institute of Disability and Rehabilitation Research (NIDRR) and the
Office of Special Education and Rehabilitation Services (OSERS), US Department of Education
and several co-sponsors (e.g., the American Psychological Association/Rehabilitation
Psychology, Division 22, etc.). The purpose of this paper is to review these findings and draw the
most relevant implications for rehabilitation counselor training programs' curricula. The paper
begins with a review of the contextual changes affecting vocational rehabilitation (VR) services
delivery today and then presents employment outcomes research findings as related to the
vocational rehabilitation participant, the rehabilitation counselor in the placement process, and
the actual services provided. Implications for rehabilitation counseling curricula are presented
not only in relation to job placement coursework, but also coursework relating to counseling
strategies, vocational assessment, and medical aspects of disability. Modifications to
coursework in the above areas (and potentially others) should have impact in preparing more of
an "employment outcomes skilled and oriented" RC program graduate. (PsycINFO Database
Record (c) 2009 APA, all rights reserved) (from the journal abstract)
Frey, W. D., S. T. Azrin, et al. (2008). "The Mental Health Treatment Study." Psychiatric Rehabilitation
Journal 31(4): 306-312.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-35
Social Security Disability Insurance (SSDl) beneficiaries with primary psychiatric impairments
comprise the largest, fastest growing, and most costly population in the SSDl program. The
Mental Health Treatment Study provides a comprehensive test of the hypothesis that access to
evidence-based employment services and behavioral health treatments, along with insurance
coverage, can enable SSDl beneficiaries with psychiatric impairments to return to competitive
employment It will also examine which beneficiaries choose to enter an employment study
under such conditions. Currently in the field in 22 cities across the U.S., the MHTS aims to recruit
3,000 SSDl beneficiaries with psychiatric impairments into a randomized controlled trial. This
paper describes the MHTS, its background, and its process and outcome assessments. (PsycINFO
Database Record (c) 2009 APA, all rights reserved) (from the journal abstract)
Gold, J. M., R. W. Goldberg, et al. (2002). "Cognitive correlates of job tenure among patients with severe
mental illness." American Journal of Psychiatry
159(8): 1395-402.
OBJECTIVE: There is clear evidence that cognitive performance is a correlate of functional
outcome among patients with schizophrenia. However, few studies have specifically examined
the cognitive correlates of competitive employment performance or the longer-term outcomes
of vocational rehabilitation. The objective of the present study was to examine the cognitive
predictors of vocational functioning in the context of a controlled clinical trial by comparing two
approaches to vocational rehabilitation. METHOD: A broad neuropsychological battery was
administered to 150 patients upon entry into the vocational rehabilitation trial. Vocational
performance was assessed over a 24-month follow-up interval. RESULTS: There were no
differences in baseline cognitive performance between the 40 patients who obtained
competitive employment and the 110 patients who remained unemployed over the follow-up
interval. In contrast, multiple cognitive measures were significantly correlated with the total
number of hours that patients were employed. The cognition-job tenure relationship appears to
be fairly general, involving measures of IQ, attention, working memory, and problem solving.
CONCLUSIONS: Cognitive performance was a significant predictor of job tenure but not job
attainment in the context of a clinical trial of two vocational rehabilitation approaches. It
appears that many persistently unemployed patients are capable of obtaining competitive
employment with effective vocational services. Longer-term employment success, however,
may be related to multiple aspects of baseline cognitive performance.
Gold, J. M., C. Queern, et al. (1999). "Repeatable battery for the assessment of neuropsychological
status as a screening test in schizophrenia I: sensitivity, reliability, and validity." American Journal of
Psychiatry 156(12): 1944-50.
OBJECTIVE: Cognitive impairment is an important feature of schizophrenia and is correlated with
functional outcome. However, psychiatry lacks a screening instrument that can reliably assess
the types of cognitive impairment often seen in schizophrenia. The authors assessed the
sensitivity, convergent validity, and reliability of the Repeatable Battery for the Assessment of
Neuropsychological Status (RBANS) as well as the relationship of the RBANS to symptoms and
employment status. This newly published test takes 25 minutes to administer and was
standardized on a U.S.-Census-matched adult population. The test provides a total score and
five index scores, each with a mean value of 100 (SD = 15). METHOD: RBANS data were obtained
from 129 patients with schizophrenia in the outpatient and inpatient programs of the Maryland
Psychiatric Research Center. RBANS data were correlated with WAIS-III and Wechsler Memory
Scale, 3rd ed. performance in 38 patients. Reliability data for alternate forms of the RBANS were

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-36
obtained from 53 patients; symptom ratings were obtained from 48 patients; and employment
status was examined in 77 patients. RESULTS: The patients with schizophrenia demonstrated
marked impairment on the RBANS (their mean total score was 71.4). The patients' index scores
suggested that they had relatively less impairment of language and visual functions than of
memory and attention. The RBANS demonstrated high correlations with full-scale IQ and
memory measures. The total score demonstrated good reliability. RBANS performance
minimally correlated with Brief Psychiatric Rating Scale ratings but was strongly related to
employment outcome. CONCLUSIONS: The RBANS appears to be a useful cognitive screening
instrument in schizophrenia. The instrument may be a useful prognostic indicator and offers a
means of assessing cognitive status.
Gottfredson, L. S. (1986). "Occupational Aptitude Patterns Map: Development and implications for a
theory of job aptitude requirements." Journal of Vocational Behavior
29(2): 254-291.
Used US Employment Service data on the cognitive and noncognitive aptitude requirements of
different occupations to create an occupational classification, ”the Occupational Aptitude
Patterns Map (OAPM),”of 13 job clusters arrayed according to major differences in overall
intellectual difficulty level and in functional focus (field) of work activities. The OAPM was
compared with an alternative, aptitude-based classification; with J. L. Holland's (1985) typology
of work environments; and with ratings for complexity of involvement with data, people, and
things. Those comparisons supported the construct validity of different aspects of the OAPM
and helped clarify uses for which it is most appropriate. It is concluded that when combined
with previous evidence about patterns of job aptitude demands, the OAPM provides the basis
for a theory of job aptitude requirements. The OAPM and accompanying analyses support the
following hypotheses: (1) General intelligence is the major gradient by which aptitude demands
have become organized across jobs in the US economy; (2) within broad levels of work, the
aptitude demands of different fields of work differ primarily in the shape of their cognitive
profiles; and (3) different aptitude demand patterns arise in a large part from broad differences
in the tasks workers actually perform on the job. (45 ref) (PsycINFO Database Record (c) 2009
APA, all rights reserved)
Gottfredson, L. S. (2002). "Where and why g matters: Not a mystery." Human Performance
15(1): 25-46.
Explains g as being the highly general capability for processing complex information of any type,
explaining its value in predicting job performance. And, as complexity is the major distinction
among jobs, g is more important further up the occupational hierarchy. The author discusses the
generalizability and stability of the g factor, its meaning as a construct, and the complexity
factor among jobs. (PsycINFO Database Record (c) 2008 APA, all rights reserved)
Harding, B., S. Torres-Harding, et al. (2008). "Factors associated with early attrition from psychosocial
rehabilitation programs." Community Mental Health Journal
44(4): 283-288.
This study aimed to identify characteristics associated with early dropout from a vocationally
oriented psychosocial rehabilitation (PSR) program for clients with severe mental illness. The
sample consisted of 194 individuals who participated in a study comparing a supported
employment program to a stepwise vocational program. Study participants who dropped out of
the PSR program within 6 months of study entry were compared to those who continued for at
least 6 months. Dropouts had poorer competitive employment outcomes than those who
continued. Participants with at least a high school diploma, never married, with a schizophrenia-

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-37
spectrum diagnosis, and those assigned to a stepwise model of vocational rehabilitation were
more likely to dropout. The implications of these findings are discussed. (PsycINFO Database
Record (c) 2009 APA, all rights reserved) (from the journal abstract)
Heitzman, A. M., J. M. Meltzer, et al. (2009). "A call to update the DOT: Findings of the IARP
Occupational Database Committee." The Rehabilitation Professional
17(2): 63-84.
Lerner, D., B. C. Amick, III, et al. (2003). "Relationship of employee-reported work limitations to work
productivity." Medical Care
41(5): 649-659.
Work limitation rates are crucial indicators of the health status of working people. If related to
work productivity, work limitation rates may also supply important information about the
economic burden of illness. Our objective was to assess the productivity impact of on-the-job
work limitations due to employees' physical or mental health problems. Subjects were asked to
complete a self-administered survey on the job during 3 consecutive months. Using robust
regression analysis, we tested the relationship of objectively-measured work productivity to
employee-reported work limitations. Each survey included a validated self-report instrument,
the Work Limitations Questionnaire (WLQ). The firm provided objective, employee-level work
productivity data. In adjusted regression analyses (n=1,827), employee work productivity
(measured as the log of units produced/hour) was significantly associated with 3 dimensions of
work limitations: limitations handling the job's time and scheduling demands, physical job
demands, and output demands. For every 10% increase in on-the-job work limitations reported
on each of the 3 WLQ scales, work productivity declined approximately 4 to 5%. Employee work
limitations have a negative impact on work productivity. (PsycINFO Database Record (c) 2009
APA, all rights reserved)
Lerner, D., B. C. Amick, III, et al. (2001). "The Work Limitations Questionnaire." Medical Care
39(1): 72-
85.
Developed and assessed psychometric properties of a questionnaire for measuring on-the-job
impact of chronic health problems and/or treatment (work limitations). Three pilot studies
(focus groups, cognitive interviews, and an alternate forms test) generated candidate items,
dimensions, and response scales. Two field trials (Studies 1 and 2) tested test recall error and
construct validity of the questionnaire. Ss were employed individuals (aged 18-64 yrs) from
several chronic condition (e.g., arthritis, headache, epilepsy) groups (48 in Study 1, 121 in Study
2) and 14 healthy controls (Study 1). With 25 items, 4 dimensions (limitations handling time,
physical, mental-interpersonal, and output demands), and a 2-wk reporting period, the Work
Limitations Questionnaire demonstrated high reliability and validity. (PsycINFO Database Record
(c) 2009 APA, all rights reserved)
MacDonald-Wilson, K., E. S. Rogers, et al. (2001). "Unique issues in assessing work function among
individuals with psychiatric disabilities." Journal of Occupational Rehabilitation
11(3): 217-232.
With the admission of people who experience psychiatric disabilities in the state-federal
vocational rehabilitation system and the Social Security disability rolls in the 1960s, assessment
of their capacity to work has been a major concern. Given the rising rates of claims for
psychiatric disability in both the public and the private sectors, and the disappointing
employment outcomes of people with psychiatric disabilities compared to those with other
disabilities, there have been numerous initiatives to accurately assess their employment
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-38
potential. Historically, such assessment within the Social Security Administration has relied upon
evaluation of a person's medical impairment, but numerous studies suggest a weak relationship
between measures of psychiatric diagnosis or symptoms and work outcome. Efforts have been
undertaken to identify valid and reliable methods of assessing the ability of people with
psychiatric disabilities to work. The authors review (a) methods of assessing work function for
this population, and (b) the literature on predictors of work functioning and the nature of
psychiatric disability, and suggest implications for disability determination policies and for future
research. (PsycINFO Database Record (c) 2009 APA, all rights reserved) (from the journal
abstract)
MacDonald-Wilson, K. L., E. S. Rogers, et al. (2003). "Identifying relationships between functional
limitations, job accommodations, and demographic characteristics of persons with psychiatric
disabilities." Journal of Vocational Rehabilitation
18(1): 15-24.
Years after the passage of the Americans with Disabilities Act, little empirical information exists
about the relationship between the functional limitations experienced by individuals with
psychiatric disabilities, and related reasonable accommodations provided on the job. A multi-
site, longitudinal study was conducted with 191 employees in 22 supported employment
programs across 3 states during a 1-year study period. Data were gathered prospectively in a
structured, narrative form designed to describe both the functional limitations and
accommodations of participants. The most frequent functional limitations among this group of
employed persons with psychiatric disabilities were cognitive in nature, followed by social,
physical, and emotional/other. There was a significant relationship between the type of
functional limitation and the number and type of accommodations received. There was a
marginally significant relationship between type of functional limitation and a diagnosis of
schizophrenia. There were no significant relationships between any other clinical or
demographic factors, functional limitations or reasonable accommodations. Cognitive
limitations were the most prevalent in this sample and the best predictor of the number of
accommodations provided. (PsycINFO Database Record (c) 2009 APA, all rights reserved)
MacDonald-Wilson, K. L., E. S. Rogers, et al. (2002). "An investigation of reasonable workplace
accommodations for people with psychiatric disabilities: quantitative findings from a multi-site study."
Community Mental Health Journal
38(1): 35-50.
Despite the requirement of many employers to provide accommodations in the workplace for
individuals with disabilities under Section 504 of the Rehabilitation Act of 1973, the
preponderance of accommodations that have been described in the literature concern physical
rather than psychiatric disabilities. This study was an exploratory, descriptive, longitudinal,
multi-site investigation of reasonable workplace accommodations for individuals with
psychiatric disabilities involved in supported employment programs. We discuss the functional
limitations and reasonable accommodations provided to 191 participants and the characteristics
of 204 employers and 22 service provider organizations participating in the study. Implications
for service providers and administrators in supported employment programs are discussed.
Mak, D. C. S., H. W. H. Tsang, et al. (2006). "Job Termination Among Individuals with Severe Mental
Illness Participating in a Supported Employment Program." Psychiatry: Interpersonal and Biological
Processes 69(3): 239-248.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-39
This study, which explored job terminations among 60 individuals with severe mental illness
participating in a supported employment program in Hong Kong, used the Chinese Job
Termination Interview that was validated and translated from the Job Termination Interview
(JTI; Becker, Drake, Bond et al., 1988). More than half of the job terminations (53%) were
unsatisfactory which included dissatisfaction with job (44%) and lack of interest (22%).
Modification of work schedules and provision of adequate supervision and coaching at the
workplace were identified as necessary job accommodations. Similarities and differences of
findings were compared with overseas studies. Possible improvement of current supported
employment program was discussed. (PsycINFO Database Record (c) 2009 APA, all rights
reserved) (from the journal abstract)
Massel, H. K., R. P. Liberman, et al. (1990). "Evaluating the capacity to work of the mentally ill."
Psychiatry: Journal for the Study of Interpersonal Processes
53(1): 31-43.
Ss were grouped into categories of psychotic (n = 79) or nonpsychotic (n = 64), and disabled or
nondisabled, in regard to adjudication for mental impairment from the Social Security
Administration (SSA). Ss were evaluated for their work capacity in either a 3- or 15-day
vocational assessment. There were significant relationships between disability status and work
capacity, in the direction of better performance for nondisabled Ss. Ss who were adjudicated
appeared to be more work incapacitated than Ss who were not so adjudicated. Findings
reflected concordance between the evaluation procedure and the SSA's disability determination
process. (PsycINFO Database Record (c) 2009 APA, all rights reserved)
Matheson, L. N. (2001). "Disability methodology redesign: considerations for a new approach to
disability determination." J Occup Rehabil
11(3): 135-42.
Disability determination meets important societal needs, involving billions of dollars and millions
of people every year. However, disability determination decisions often are incorrect, and the
high proportion of decision appeals and reversals creates additional administrative expense and
difficulty for the people that the disability determination system is intended to support. Projects
funded by the United States Social Security Administration explored these issues and developed
new conceptual models and tools to improve the accuracy and fairness of disability
determination. This paper provides an introduction to the projects and the papers in this special
issue of the Journal of Occupational Rehabilitation.
Matheson, L. N., M. Kane, et al. (2001). "Development of new methods to determine work disability in
the United States." J Occup Rehabil
11(3): 143-54.
The development of new methods to determine work disability for the United States Social
Security Administration is described, including the fiscal and administrative background to the
current and proposed methods. An introduction to the current disability determination process
and description of its status is followed by a description of the original proposed plan for
redesign of the process. In response to this plan, the authors participated in several research
projects. An overview of some of the key research projects performed to improve the Social
Security Administration disability determination process is provided.
Matheson, L. N., V. Kaskutas, et al. (2001). "Development of a database of Functional Assessment
Measures related to work disability." Journal of Occupational Rehabilitation
11(3): 177-199.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-40
The development of the Functional Assessment Measures Database is described. The database
provides a method to organize and search for measures that are used to assess the functional
abilities of people with medical impairments to determine work disability. Although there are
several large collections of information about tests, questionnaires, structured interviews, and
other measures used in medicine, psychology, and education, there is no central repository of
information about the functional assessment measures that are used in rehabilitation. A team of
experts in functional assessment, psychology, medicine, occupational therapy, and physical
therapy was composed. The project identified 4,200 different measures that are used in the
functional assessment of persons with disability across the life span, 812 of which are used to
evaluate adults in terms of work disability. The database has 3,033 scales that are found in 633
measures. In the database, each measure is described and is linked to at least one functional
assessment construct. The use of the database in the Social Security Administration Redesign
Project is described. Other possible uses for the database are presented. (PsycINFO Database
Record (c) 2009 APA, all rights reserved)
McGuire, A. B., G. R. Bond, et al. (2007). "Situational assessment in psychiatric rehabilitation: A
reappraisal." Journal of Vocational Rehabilitation
27(1): 49-55.
Background: One widely-used approach in the vocational rehabilitation field is the situational
work assessment, in which staff rate general worker behaviors relevant to any employment
setting. The Work Behavioral Inventory (WBI) is a standardized situational assessment
developed specifically for individuals with severe mental illness (SMI). Originally developed in a
sheltered workshop environment, its application in community settings has not been studied.
We examined the predictive validity for the WBI in a range of community and agency settings.
Methods: Using a prospective longitudinal study, we assessed 52 clients with schizophrenia
spectrum disorders newly enrolled in a vocational program at a psychiatric rehabilitation
agency. Participants were followed for nine months and assessed every two months on the WBI.
Findings: WBI ratings were unrelated to employment outcomes in the full sample at nine
months. However, among participants who obtained paid employment at some time during
follow-up, WBI ratings were positively associated with total wages earned, weeks worked, and
paid hours worked. Conclusions: Situational assessment is a useful method for predicting
employment outcomes for individuals with schizophrenia who obtain work. However, its utility
in predicting initial job acquisition is uncertain. In addition, the limitations in the use of situation
assessments in community employment settings raise questions about how it would be best
adapted in programs implementing evidence-based supported employment. (PsycINFO
Database Record (c) 2009 APA, all rights reserved) (from the journal abstract)
McGurk, S. R. and H. Y. Meltzer (2000). "The role of cognition in vocational functioning in
schizophrenia." Schizophr Res
45(3): 175-84.
Schizophrenia is associated with long-term unemployment. Cognitive dysfunction, rather than
clinical symptoms, may be the most important factor in the ability to work for patients with this
disorder. To evaluate the relationship of clinical symptoms and cognitive functioning to work
status, thirty patients with schizophrenia, who were participants in a vocational rehabilitation
program, were evaluated with a comprehensive neuropsychological battery and assessment of
psychopathology. Subjects were classified as being in stable full-time, part-time or unemployed
work status for at least a year. Univariate analysis indicated that patients who were working full-
time were significantly better educated, more likely to be treatment-resistant, more likely to be

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-41
treated with an atypical antipsychotic medication, had more positive symptoms, and were
engaged in work tasks which were more cognitively complex than the part-time employed and
unemployed work groups. An ANCOVA controlling for education demonstrated that the full-time
employed group performed significantly better than the unemployed group on measures of
executive functioning, working memory and vigilance; and significantly better than the part-time
group on measures of vigilance and executive functioning. Although negative symptoms did not
significantly relate to work status in the univariate analysis, a multiple regression indicated that
negative symptoms, level of education, and executive functioning differentiated the work
groups. These results suggest that poor premorbid function, negative symptoms and cognitive
dysfunction are significantly associated with unemployment in schizophrenia.
McGurk, S. R. and K. i. T. Mueser (2006). "Strategies for coping with cognitive impairments of clients in
supported employment." Psychiatric Services
57(10): 1421-1429.
Objective: This study evaluated the strategies used by employment specialists to help clients in
supported employment programs manage cognitive impairments that interfered with obtaining
and keeping jobs. Methods: Twenty-five supported employment specialists were surveyed to
identify strategies they used to help their clients cope with cognitive problems in the domains of
attention, psychomotor speed, memory, and problem solving. Then, 50 employment specialists
were surveyed to determine whether they used each of the different coping strategies
generated in the first part of the study. For each strategy used, they rated how effective it was.
Results: Employment specialists reported using a total of 76 different strategies for helping their
clients cope with cognitive difficulties. The specialists reported using an average of 48 different
coping strategies, which they rated on average as just below effective. Strategies for dealing
with attention problems were rated as more effective than strategies used in the other three
domains. The number of coping strategies that they reported using was significantly correlated
with the perceived effectiveness of the strategies and the proportion of clients in their caseload
who were working. Conclusions: Supported employment specialists were actively involved in
helping clients cope with their cognitive impairments. Use of more strategies was correlated
with specialists' greater perceived effectiveness of the strategies and with higher rates of
working clients on their caseloads, although the reasons for these associations are unclear.
Further research is needed to evaluate whether employment specialists' use of more strategies
to help clients cope with cognitive problems contributes to better work outcomes. (PsycINFO
Database Record (c) 2009 APA, all rights reserved) (from the journal abstract)
McGurk, S. R. and K. T. Mueser (2004). "Cognitive functioning, symptoms, and work in supported
employment: a review and heuristic model." Schizophr Res
70(2-3): 147-73.
OBJECTIVE: Supported employment has been shown to improve the employment outcomes of
clients with severe mental illness (SMI), but many clients who receive this service still fail to
achieve their vocational goals. There is a need to better understand how illness-related
impairments interfere with work, and how supported employment services deal with those
impairments in order to improve the employment outcomes of clients with SMI. METHOD: We
conducted a review of research on the relationship between cognitive functioning, symptoms,
and competitive employment in clients with SMI. Based on this review, we developed a heuristic
model of supported employment that proposes specific interactions between cognitive factors,
symptoms, vocational services, and employment outcomes. RESULTS: The review indicated that
cognitive functioning and symptoms were strongly related to work in studies of general

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-42
psychiatric samples. In studies of clients participating in vocational rehabilitation programs,
associations between cognitive functioning, symptoms, and work were also present, but were
attenuated, suggesting that vocational rehabilitation compensates for the effects of some
cognitive impairments and symptoms on work. We describe a heuristic model of supported
employment that posits specific and testable effects of cognitive domains and symptoms on
vocational services and employment outcomes. CONCLUSIONS: Supported employment appears
to work by compensating for the effects of cognitive impairment and symptoms on work. The
model may serve as a guide for research aimed at understanding how supported employment
works, and for developing supplementary strategies designed to improve the effectiveness and
cost-effectiveness of supported employment services.
McGurk, S. R. and K. T. Mueser (2006). "Cognitive and clinical predictors of work outcomes in clients
with schizophrenia receiving supported employment services: 4-year follow-up." Adm Policy Ment
Health 33(5): 598-606.
In a prior study we showed that cognitive functioning was a modest predictor of work and
supported employment services over 2-years in 30 clients with schizophrenia, whereas
symptoms were not (McGurk et al. (2003). Psychiatric Services, 58, 1129-1135). In order to
evaluate whether the long-term provision of supported employment services reduced the
impact of cognitive functioning on work, we examined the relationships between cognitive
functioning and symptoms assessed after the initial 2 years of the program, and work and
vocational services over the following 2 years (3-4 years after joining the program). Cognitive
functioning was more predictive of work during the latter 2 years of the study than the first 2
years, and a similar but weaker pattern was present for the prediction of employment services.
Symptoms remained weak predictors for both time periods. In addition, learning and memory
and executive functions were strongly correlated with job task complexity during the 3-4 year
follow-up, but not the 1-2 year follow-up, suggesting that employment specialists were able to
improve their ability to match clients to jobs based on their cognitive skills. Furthermore, the
specific associations between cognitive functioning, services, and work outcomes changed from
years 1-2 to years 3-4, suggesting a dynamic interplay between these factors over the long-term,
rather than static and unchanging relationships. The findings indicate that rather than supported
employment services reducing the impact of cognitive functioning on long-term competitive
work, the impact actually increases over time, suggesting that efforts to improve cognitive
functioning (e.g., cognitive rehabilitation) may optimize employment outcomes in
schizophrenia.
Penn, D. L., L. J. Sanna, et al. (2008). "Social cognition in schizophrenia: An overview." Schizophrenia
Bulletin 34(3): 408-411.
The purpose of this column is to provide an overview of social cognition in schizophrenia. The
column begins with a short introduction to social cognition. Then, we describe the application of
social cognition to the study of schizophrenia, with an emphasis on key domains (i.e., emotion
perception, Theory of Mind, and attributional style). We conclude the column by discussing the
relationship of social cognition to neurocognition, negative symptoms, and functioning, with an
eye toward strategies for improving social cognition in schizophrenia. (PsycINFO Database
Record (c) 2009 APA, all rights reserved) (from the journal abstract)

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-43
Rogers, E. S., K. Sciarappa, et al. (1991). "Development and evaluation of situational assessment
instruments and procedures for persons with psychiatric disability." Vocational Evaluation & Work
Adjustment Bulletin 24(2): 61-67.
Developed 2 instruments, a work adjustment skills scale and an interpersonal skills scale. Staff in
2 psychosocial programs were trained in the situational assessment procedures and in
observation techniques. 50-63 yr old clients (with schizophrenia, schizo-affective, or depressive
disorder) were selected to examine the psychometric properties of the instruments. Interrater
reliability, test-retest reliability, internal consistency, and split-half reliability statistics were
computed from the data collected. Results suggest high levels of reliability for the 2
instruments. Predictive validity and concurrent validity of the instruments were examined by
following the clients for 1 yr postassessment. A discriminant analysis was performed to
determine if the situational assessment predicted vocational outcome. Concurrent validity was
determined by correlating Ss' scores on the 2 scales with the Griffiths' Work Behavior Scale.
(PsycINFO Database Record (c) 2009 APA, all rights reserved)
Salyers, M. P., A. B. McGuire, et al. (2008). "What makes the difference? Practitioner views of success
and failure in two effective psychiatric rehabilitation approaches." Journal of Vocational Rehabilitation
28(2): 105-114.
The current study examined success in two vocational programs by interviewing practitioners in
two philosophically different employment programs at a psychosocial rehabilitation agency.
Practitioners' views of what constitutes success and factors facilitating success were analyzed
using both qualitative and quantitative means. In general, practitioners viewed success as more
than just obtaining a job, but maintaining employment over time and making life changes.
Success was most often attributed to consumer motivation, and lack of success was attributed
to mental health symptoms. Furthermore, practitioners from each program tended to view
success in a manner consistent with their program's philosophy. (PsycINFO Database Record (c)
2009 APA, all rights reserved) (from the journal abstract)
Schultheis, A. M. and G. R. Bond (1993). "Situational assessment ratings of work behaviors: Changes
across time and between settings." Psychosocial Rehabilitation Journal
17(2): 107-119.
Evaluated staff ratings of work behaviors for 52 clients with serious mental illness participating
in a community mental health center vocational program. There were 2 sites for job training: in-
house work crews and a "handyman work crew" providing temporary, paid employment in the
community. Contrary to expectations, clients declined significantly in their work performance
over a 3-mo period. Moreover, when observed in the community work crews, clients were rated
significantly higher than when observed in in-house crews. Findings are interpreted as reflecting
a "demoralization effect" among clients working in the in-house setting after previously working
in a paid community placement. (PsycINFO Database Record (c) 2009 APA, all rights reserved)
Tsang, H., B. Ng, et al. (2000). "Predictors of post-hospital employment status for psychiatric patients in
Hong Kong: From perceptions of rehabilitation professionals to empirical evidence." International
Journal of Social Psychiatry 46(4): 306-312.
Compared the social vocational competence and psychosocial support of employed and
unemployed psychiatric patients following discharge. 50 mental hospital patients (aged 17-55
yrs) were assessed concerning social vocational competence and psychosocial support. Results
show that 3 mo following discharge employed Ss exhibited better psychosocial support and
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-44
social vocational competence than did unemployed Ss. Employed and unemployed Ss did not
differ in their medical history, work history, or demographic variables. (PsycINFO Database
Record (c) 2009 APA, all rights reserved)
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-45
Appendices
Appendix A—Biographic Sketches of Subcommittee Members .................................. 47
Appendix B—Biographic Sketches of Mental Cognitive Roundtable
Participants............................................................................................................. 51
Appendix C—Mental Cognitive Roundtable Background Materials............................. 57
Appendix D—First Mental Cognitive Subcommittee Presentation............................. 127
Appendix E—Second Mental Cognitive Subcommittee Presentation........................ 151
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-46
This page left intentionally blank.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-47
Appendix A
Biographic Sketches of Subcommittee Members
David J. Schretlen, Ph.D., Chair
David J. Schretlen, Ph.D. is as an Associate Professor of Psychiatry and Behavioral
Sciences, as well as an Associate Professor of Radiology at the Johns Hopkins
University School of Medicine. He is board-certified in clinical neuropsychology, and
works at the Johns Hopkins Hospital, where he sees patients, teaches, and conducts
research.
Dr. Schretlen completed his doctorate in clinical psychology at the University of Arizona
in 1986, an internship at McLean Hospital, Harvard Medical School, and a post-doctoral
residency in neuropsychology and rehabilitation at the UCLA Neuropsychiatric Institute.
While at UCLA, Dr. Schretlen was awarded a Mary E. Switzer fellowship by the National
Institute of Disability and Rehabilitation Research.
Dr. Schretlen has served as a grant reviewer for the National Institutes of Health and
the Veterans Administration Medical Center. He serves on the editorial boards of
several scientific journals. A prolific researcher, he has authored over 175 articles,
monographs, book chapters, and abstracts. His research interests include the use of
quantitative brain imaging to investigate cognitive and emotional aspects of human
behavior. He has received federal and private research funding to study determinants of
work disability in traumatic brain injury and bipolar disorder. He currently is analyzing
predictors of functional disability in schizophrenia and bipolar disorder. Related to this is
another program of research in which Dr. Schretlen is investigating strategies to
increase the diagnostic sensitivity and specificity of neurocognitive measures for
persons of diverse socioeconomic background.
In addition to research and teaching, Dr. Schretlen is actively engaged in clinical work
that primarily involves neuropsychological assessment. He consults to physicians about
treatment planning and attorneys about matters involving such matters as vocational
aptitude and work disability resulting from brain injuries.
Mary Barros-Bailey, Ph.D.
Mary Barros-Bailey, PhD, CRC, NCC is a bilingual rehabilitation counselor, vocational
expert, and life care planner in Boise, Idaho. She is the immediate past Chair
(2007-2008) of the Commission on Rehabilitation Counselor Certification (CRCC) and
served as the Ethics Committee Chair from 2005-2007. Mary was one of the founding
members of the Inter-organizational O*NET Task Force (IOTF) that in the early 2000s
collaborated with the US Social Security Administration and the US Department of
Labor on the use of occupational data within the disability context. She is a reviewer or
on the Editorial Boards of several peer-review journals such as the Journal of
Counseling & Development (American Counseling Association), the Journal of Forensic

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-48
Vocational Analysis (American Board of Vocational Experts), and the Journal of Mixed
Methods Research (SAGE Publications). Mary has a doctorate in Counseling with a
cognate in Rehabilitation Counseling from the University of Idaho. Her research and
presentation interests include professional issues in rehabilitation counseling (ethics,
methodological, aging, multicultural, and international). She has presented and
published nationally and internationally.
Robert T. Fraser, Ph.D.
Robert T. Fraser, Ph.D. is a professor in the University of Washington's Department of
Rehabilitation Medicine, jointly with the Departments of Neurological Surgery and
Neurology and consultant with Associates in Rehabilitation and Neuropsychology. He is
an active counseling and rehabilitation psychologist, a certified rehabilitation counselor
and a certified life care planner who directs Neurological Vocational Services within
Rehabilitation Medicine. Within neurological rehabilitation, he has specialized in
epilepsy, brain injury, and multiple sclerosis.
Dr. Fraser is author or co-author of more than one hundred publications and co-editor
on four texts to include Traumatic Brain Injury Rehabilitation (CRC Press,1999), Multiple
Sclerosis Workbook (New Harbinger, 2006), and Comprehensive Care in Epilepsy
(John Libbey, 2001). He has been awarded numerous Federal grants by the
Department of Education (NIDRR and RSA) - four of which have been specific to
traumatic brain injury rehabilitation, and, more recently, in epilepsy self-management by
the Center for Disease Control (CDC). He was awarded two World Rehabilitation Fund
fellowships to review, respectively, the post-acute traumatic brain injury programs in
Israel and epilepsy rehabilitation advances in Scandinavia and Holland. He lectures
nationally on TBI rehabilitation. Research emphases have included evaluation of
innovative psychosocial rehabilitation strategies and prediction of vocational
rehabilitation outcome across different neurological disabilities. He is the recipient of two
American Rehabilitation Counseling Association Research Awards, and an Epilepsy
Foundation of America Career Achievement Award. Dr. Fraser is a past-president of
Rehabilitation Psychology, Div. 22 of the American Psychological Association and a
Fellow in the Division, a former Board member of the Epilepsy Foundation of America
(EFA), a current board member of the Epilepsy Foundation Northwest, and was recently
elected to the Board of Governors for the International Consortium of Multiple Sclerosis
Centers.
Dr. Fraser has received master’s degrees in rehabilitation counseling (University of
Southern California) and public administration (Seattle University). His doctorate is in
rehabilitation psychology from the University of Wisconsin–Madison, with a dissertation
focused on the use of task analysis in the national classification and utilization of state
agency vocational rehabilitation personnel.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-49
Sylvia E. Karman
As Director for Social Security Administration’s (SSA’s) Occupational Information
Development Project in the Office of Program Development and Research,
Sylvia E. Karman oversees the research and development of occupational information
tailored to SSA’s disability programs. She directs the investigations and developmental
work to replace the Dictionary of Occupational Titles, as well as studies to inform
disability policy development. She also chairs the SSA Occupational Information
System Development Workgroup.
Ms. Karman serves as an expert for SSA executive management and for numerous
private and public sector entities on medical-vocational assessment and occupational
information issues critical to disability evaluation. As the former Chief of the Vocational
Policy Branch in SSA’s Office of Disability Programs and, before that, the lead senior
policy analyst and project manager for occupational information analysis and policy
issues related to SSA’s use of the Dictionary, she has long held a leadership role for the
agency in these subject areas.
Ms. Karman began her career with SSA in 1979 as a college intern. After graduating in
1982 with a bachelors of arts degree from Towson University in Maryland, her work
involved policy and legislative development and program evaluation for the
Supplemental Security Income program under title XVI and for the agency’s disability
programs under both titles II and XVI. Ms. Karman has presented and published papers
in the areas of SSA’s use of the Dictionary of Occupational Titles for disability
adjudication, medical-vocational assessment, and the role of vocational factors and
occupational information in disability evaluation, including transferable skills analysis.
She is a frequent speaker at conferences and seminars throughout the US and Canada.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-50
This page left intentionally blank.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-51
Appendix B
Biographic Sketches of Mental Cognitive Roundtable Participants
David J. Schretlen, PhD, ABPP
See Appendix A
Mary Barros-Bailey, PhD, CRC
See Appendix A
Robert T. Fraser, PhD
See Appendix A
Sylvia E. Karman, BA
See Appendix A
Shannon Gwaltney-Gibson, PhD
Education
B.A., Liberal Arts, magna cum laude, Armstrong Atlantic State University
M.S., Industrial and Organizational Psychology, Virginia Polytechnic Institute & State
University
Ph.D., Industrial and Organizational Psychology, Virginia Polytechnic Institute & State
University
Areas of Expertise
Professor Gibson’s expertise is in issues related to human resources management &
organizational behavior in organizations. Her research includes more than 35 published
conference proceedings and 19 peer-reviewed journal articles on topics relevant to
human resources and organizational development including job analysis, technology
acceptance in organizations, and entrepreneurship. Her research can be seen in the
Journal of Small Business Strategy, Business Education Forum, Small Business
Institute Forum, and Management Research News, among others.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-52
Professional Activities
Professor Gibson is an Associate Professor of Management at East Carolina University,
where she has been a member of the College of Business since 2003. She has
extensive experience teaching issues related to occupational analysis; in addition to
currently teaching graduate level Human Resources, she previously spent two years
teaching Industrial and Organizational Psychology at ECU, as well as courses at
Radford University and Texas A&M Corpus Christi. She was awarded the 2009 Robert
L. Jones University Alumni Award for Outstanding Teaching and the 2009 Max Ray
Joyner Award for Faculty Service Through Continuing Education. In addition to her
university responsibilities, she currently acts as a consultant to State Farm Insurance on
issues related to human resources management and leadership development. She is a
member of The Academy of Management, the Society for the Advancement of
Management, the Society for Industrial & Organizational Psychology, the Southeast
Decision Sciences Institute, and the Southeast Institute for Operations Research and
the Management Sciences.
Mark Wilson, PhD
Dr. Mark A. Wilson, Associate Professor of Psychology, NC State University, joined the
faculty in 1992. He received a B.A. in Psychology from Wartburg College (1975), an
M.A. in Experimental Psychology from the University of Missouri-Kansas City (1978),
and a Ph.D. in Industrial/ Organizational Psychology from Ohio State University (1983).
While completing the Ph.D., he served as Project Coordinator, Technical Director, and
Senior Research Associate for Organizational Research and Development Inc. on a
comprehensive human-resource research project involving human-resource planning,
job analysis, selection (managerial assessment centers), performance appraisal, and
compensation for a market-leading insurance company. The experience drastically
altered his view of the field and his research interests. It was while working on the
project that he developed his interest in the integration of human-resource systems,
comprehensive job analysis, his dedication to the scientist-practitioner model and the
problems of practitioners, and his love for fieldwork.
He has always been interested in work measurement issues, models of human job
performance in organizations, and research methods. He has consulted and conducted
research extensively with numerous large organizations in both the private and public
sectors. He has taught graduate and undergraduate management courses as an
Assistant Professor at both Texas Tech University (1981-1985) and Iowa State
University of Science and Technology (1985-1992). In 1999, he was made an honorary
member of the United States Army Special Forces. In 2006, he was appointed editor of
Ergometrika (The Journal of Work Measurement Research).

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-53
Gary R. Bond, PhD
Education
B.S., Mathematics, Michigan State University
M.A., Psychology, University of Chicago
Ph.D., Psychology, University of Chicago
Areas of Expertise
Professor Bond is an expert in effective rehabilitation approaches for people with severe
mental illness. His research has focused on two particular areas: assertive community
treatment, which is a comprehensive, intensive case management approach for people
with severe mental illness who also have other challenging problems, and supported
employment, which is an individualized approach to helping people attain competitive
employment. He has published 139 peer-reviewed journal articles, 32 book chapters,
and has taken part in 20 international presentations.
Professional Activities
Professor Bond is the Chancellor’s Professor of Psychology at Indiana University
Purdue University, Indianapolis. He served as the Director of the Clinical Rehabilitation
Psychology Program at IUPUI for 14 years and also served as the Director of the Illinois
Psychiatric Rehabilitation Training Institute from 2002-2003. Professor Bond has twice
held the Research Scientist Development Award from the National Institute of Mental
Health (1989-1994, 1996-2001) and has received national awards from the American
Psychological Association, the American Rehabilitation Counseling Association, the
International Association of Psychosocial Rehabilitation Services, and the National
Association of Case Management. He is currently involved as a co-investigator or
consultant on five grants.
Susanne Bruyère, PhD
Education
B.A., Psychology and Special Education, D’Youville College
M.S. Ed., Rehabilitation Counseling, University of Southern California
M.A., Adult Education, Seattle University
M.P.A, Public Administration, Seattle University
Ph.D, Rehabilitation Counseling, University of Wisconsin, Madison

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-54
Areas of Expertise
Professor Bruyère is an expert in the fields of disability, disability and rehabilitation,
disability and law, and diversity and inclusion. She has focused on other relevant topics
including: primary and secondary prevention of workplace disability, disability
management, non-discrimination for persons with disabilities in employment, the
Americans with Disabilities ACT (ADA), and the interplay between the ADA, human
resource practices, and labor relations. She has contributed to 13 publications and her
work can be found in journals such as the Journal of Rehabilitation Psychology and
American Rehabilitation.
Professional Activities
Professor Bruyère is the Associate Dean of Outreach and the Director of the
Employment and Disability Institute at Cornell University in the School of Industrial and
Labor Relations – Extension Division. A fellow in the American Psychological
Association, she has served as the past President of the Division of Rehabilitation
Psychology of the American Psychological Association and the National Council on
Rehabilitation Education. She currently serves on the boards of the National Association
of Rehabilitation Research and Training Centers and of CARF (the Rehabilitation
Accreditation Commission). She is currently the Project Director and Principal
Investigator of numerous research efforts. Three are funded by the U.S. Department of
Education, National Institute on Disability and Rehabilitation Research (NIDRR). One of
the projects she is currently working on is a four-year research and demonstration
project in collaboration with the Society for Human Resource Management, the
Washington Business Group on Health, and the Lewin Group to address ways to
improve the employment practices covered under the Americans with Disabilities Act
(ADA).
Lynda Payne, PhD
Education
A.A., Nursing, Middle Tennessee State University, Murfreesboro, TN
B.S., Psychology, Idaho State University, Pocatello, ID
M.S., Marriage & Family Therapy, University of Maryland, College Park, MD
Ph.D., Applied Developmental Psychology, University of Maryland, Baltimore County,
MD
Personal Activities and Interests
Lynda Payne, PhD, is a Consulting Psychologist for the State of Maryland’s Disability
Determination Services. In addition to her role as a consulting psychologist, she works

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-55
as a Psychometrician for the Kennedy Krieger Institute in Baltimore, Maryland. From
1995-2004, she was involved in a research study for the Department of the Environment
/ HUD in which she investigated the treatment of lead-exposed children through a
multi-site, clinical trial of an oral chelating agent. From 2001-2005, she examined the
target capacity for expansion for adolescent outpatient substance abuse treatment.
She has presented at the International Conference on Infant Studies and has been
published in the American Journal of Mental Retardation and the Encyclopedia of
Human Behavior.
E. Sally Rogers, ScD
Education
B.A., Temple University
M.A., Seton Hall University
ScD, Boston University
Personal Activities and Interests
Professor Rogers is an Associate Professor of Occupational Therapy at the Sargent
College of Health and Rehabilitation Sciences, Boston University. She also serves as
the Director of Research at the Center for Psychiatric Rehabilitations. Her interests
include the evaluating the effectiveness and cost effectiveness of psychiatric
rehabilitations, measuring outcomes, and assisting psychological rehabilitation
programs to evaluate the effectiveness of their services. She has contributed to 24
publications and is currently the principle investigator on three grants, two of which are
funded by the National Institute on Disability and Rehabilitation Research (NIDRR).
Pamela A. Warren, PhD
Education
B.A., Psychology, Southern Illinois University, Carbondale, Illinois
M.A., Behavior Analysis and Therapy, Southern Illinois University, Carbondale, Illinois
Ph.D., Psychology, Southern Illinois University, Carbondale, Illinois
Professional Activities
Dr. Warren is a faculty member in the Department of Counseling as well as the
Department of Psychiatry at the University of Illinois, Urbana, Illinois. She has worked
as a Clinical Psychologist for the Carle Clinic Association in Urbana, Illinois since 1991.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-56
She continues to be an advisor for the American College of Occupational and
Environmental Medicine’s (ACOEM) Practice Guidelines newsletter, and is a
psychological disability evaluator for the Illinois State Universities Retirement System.
She conducts independent psychological evaluations and complete file & peer reviews
for several national insurance companies and employers, such as Blue Cross Blue
Shield, Claim Care, CountryWide, CompCare, American Airlines, Behavioral Medical
Interventions, and Army Corp of Engineers, and others. She is a psychological
consultant to Health Care Services Corporation and served as a consultant to the Social
Security Administration’s Ticket To Work program. She has served on a number of
expert panels, such as the expert panels for ACOEM’s Chronic Pain Practice Guidelines
and Psychiatric Guidelines revision as well as the Social Security Administration’s
Functional and Vocational Expertise Panel. She has been co-investigator on a number
of studies, including research on the evaluation of psychological concerns that occur in
women with breast cancer and the EUMASS (European Union of Medicine in
Assurance and Social Security) study of the Psychosocial Aspects of Disability and
Healthcare. She has served as a reviewer for the American Medical Association Guide
to the Evaluation of Permanent Impairment, 6th edition as well as for PsyBar, Inc. She
has served on a number of committees and boards, including the Disability Research
Institute Advisory Board Reed Group Medical Disability Advisory (MDA) Board, the
International Board of Directors for the International Association of Rehabilitation
Professionals Case Management Division, the Disability Management Employers
Coalition Conference Selection Committee, and the Health Services Council, American
Psychological Association, Division 38 (Health Psychology). She has conducted over
300 professional seminars on psychological issues related to disability, identification of
psychological issues in the workplace, evidence-based treatments of psychological
concerns in the workplace, chronic pain, illness issues, and appropriate forensic
psychological evaluation to public and professional groups. These presentations have
been conducted both locally and nationally. In addition to these presentations, Dr.
Warren has written five publications.
Professional Associations
Dr. Warren is a member of the American Psychological Association (Clinical, Health,
Occupational Health, and Consulting Psychology Divisions), the American College of
Occupational & Environmental Medicine, the Association for Applied Psychophysiology
and Biofeedback, the Prescribing Psychologists Register, the International Association
for Rehabilitation Professionals, the Disability Management Employers Coalition, and
the Association for the Scientific Advancement of Psychological Injury and Law.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-57
Appendix C – 1
Mental Cognitive Roundtable – Instructions to Participants
General Meeting Information
The meeting will be held at the Hyatt Regency McCormick Place, 2233 South Martin L.
King Drive, Chicago, Illinois, USA 60616-9985, in Conference Center Room CC22C on
Monday, June 8, 2009, from 8:30 am to 4:30 pm (CDT).
For Roundtable participants, your travel arrangements will be handled by A-S-K
Associates, as you were notified in an email from Debra Tidwell-Peters.
For Panel members, if you have any questions about travel, please contact Elaina Wise
at 410-965-9863.
If you need directions or information from the hotel, please see the hotel website at
http://www.mccormickplace.hyatt.com/hyatt/hotels/index.jsp or contact the hotel at
(312) 567-1234.
Roundtable Discussion Materials and Assignments
The attached document, “Purpose and Scope of Roundtable,” will provide you with
detailed information on the research questions that we are investigating, as well as
background information on Social Security’s disability programs. The latter will provide
the context for this discussion.
Before the Roundtable, we ask that you:
1. Read the “Purpose and Scope” document and any pertinent sections of the
Appendices,
2. Complete the brief (two pages or less) writing assignment described in the
“Purpose and Scope” document, bringing this with you to the Roundtable, and
3. Send a brief (one page or less) biography to Shirleen Roth, SSA staff, at
.
After the Roundtable, we will ask you to send us your original writing assignment,
described in bullet 2 above. In addition, we will ask you to revise your responses (or
not) in light of the Roundtable discussion and send that to us as well. Your “pre” and
“post” meeting responses will be used to document the outcome of the Roundtable.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-58
This page left intentionally blank.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-59
Appendix C – 2
SOCIAL SECURITY ADMINISTRATION
Occupational Information Development Advisory Panel
Mental Cognitive Subcommittee Roundtable
Agenda - Monday, June 8, 2009
8:30 am to 8:45 am OPENING COMMENTS AND INTRODUCTIONS
Sylvia E. Karman
Project Director, Occupational Information System
Project, Social Security Administration
Panel Member, Occupational Information
Development Advisory Panel
8:45 am to 9:00 am OPENING COMMENTS
David J. Schretlen, Ph.D.
Panel Member, Occupational Information
Development Advisory Panel
Chair, Mental Cognitive Subcommittee
9:00 am to 10:00 am DISCUSSION
Discuss the existing categories of psychological and
interpersonal functioning on SSA’s Mental Residual
Functional Capacity (MRFC) Assessment form.
10:00 am to 10:15 am BREAK
10:15 am to 11:30 pm DISCUSSION
Discuss categories of psychological and interpersonal
functioning which, if impaired by disease or injury,
might impede an individual’s ability to work.
11:30 am to 12:45 pm LUNCH ON YOUR OWN
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-60
12:45 pm to 1:45 pm DISCUSSION (continued from morning session)
Discuss categories of psychological and interpersonal
functioning which, if impaired by disease or injury,
might impede an individual’s ability to work.
1:45 pm to 2:00 pm BREAK
2:00 pm to 3:00 pm DISCUSSION
Discuss the empirical studies that identify the
psychological or interpersonal deficits that decrease
the likelihood that an affected individual would be able
to do competitive work.
3:00 pm to 3:15 pm BREAK
3:15 pm to 4:15 pm DISCUSSION
Discuss the best approach(es) for assessing the
categories of psychological and interpersonal
functioning described earlier in the day.
4:15 pm to 4:30 pm REVIEW OF DISCUSSION AND ACTION ITEMS
David J. Schretlen, Ph.D., Chair
4:30 pm ADJOURN

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-61
Appendix C – 3
Mental Cognitive Roundtable – Purpose and Scope of the Roundtable
Occupational Information Development Advisory Panel
Mental/Cognitive Subcommittee
On June 8, 2009, the Mental/Cognitive Subcommittee (the Subcommittee) of the
Occupational Information Development Advisory Panel (the Panel) will be conducting a
Roundtable to obtain the opinions and facilitate a discussion by experts in the field of
mental and cognitive functional limitations resulting from impairments. The information
gathered at this Roundtable will assist the Subcommittee in making recommendations
to the Panel on the mental, cognitive, and psychosocial requirements of work.
The task of this subcommittee is to identify the most important dimensions of
psychological and interpersonal functioning that are impaired by diseases or medical
conditions and, as a result, disable a person from working. The task is not to identify
diseases or injuries that cause the functional deficits, nor is it to determine how best to
assess or remediate the deficits. Rather, the task is to develop a parsimonious list of
essential psychological and interpersonal capacities that, when disrupted by illness or
injury, prevent affected individuals from engaging in substantial gainful activity (i.e.,
competitive work).
We ask each participant to write a brief response to each of the following questions,
after considering SSA’s current Mental Residual Functional Capacity (MRFC)
Assessment, and be prepared to discuss your views of each at the Roundtable. Please
try to limit your response to these questions to two pages or less (total).
5. If you think the current MRFC Assessment does not need revision, or that
improving it is not feasible, explain why.
6. If you think the existing MRFC Assessment could be improved, then nominate up
to 10 dimensions of psychological and interpersonal functioning that, when
impaired by disease or injury, impede one’s ability to work.
2
7. Do you know of any well-designed empirical studies that have identified
psychological or interpersonal deficits that decrease the likelihood an affected
individual will be able to do competitive work?
8. While the goal of this Roundtable is not to devise measures of the person
characteristics you nominate in response to Question 2, please comment on
2
For purposes of calibrating the level of specificity that we are looking for, a capacity such as “the ability
to reason” is too global and nonspecific. Conversely, a capacity such as “the ability to tolerate occasional
brusque remarks from co-workers without losing one’s temper” might be too specific. Because our aim is
to develop a list of candidate abilities that is comprehensive but parsimonious, we ask that you limit your
list to about 10 functional capacities. Based on SSA requirements, these dimensions or factors must be
observable and measurable.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-62
what you deem to be the best approach (informant-rating, self-rating, direct
observation, testing) to assess the characteristics you enumerated. (These might
vary across functions.)
We have attached background materials to assist participants in preparing for the
Roundtable and in becoming familiar with the legal framework within which the Social
Security Administration (SSA) adjudicates disability claims. We do not intend that
participants will become experts on SSA’s disability programs or policy but, rather, that
participants will understand the context in which we ask these questions and the
necessary limitations to the scope of the Roundtable discussion. To some extent, this
scope will also be described in this paper.
While we have provided policy statements as context for the discussion, the discussion
will focus on the four research questions cited above, not SSA policy.
The Social Security Act (the Act) and the Definition of Disability
The Act defines disability as an inability to do substantial gainful work because of a
“medically determinable physical or mental impairment.” A physical or mental
impairment (impairment) is “an impairment that results from anatomical, physiological,
or psychological abnormalities which are demonstrable by medically acceptable clinical
and laboratory diagnostic techniques.” The Act stipulates that “an individual shall not be
considered to be disabled … if alcoholism or drug addiction would … be a contributing
factor material to the … determination that the individual is disabled.” (See Appendix
A.)
Appendix A is provided as a reference and is not required reading.
Use of the Dictionary of Occupational Titles in SSA’s Disability Programs
The background paper by this title, located in Appendix B, provides an overview of the
history of SSA’s disability programs and SSA’s occupational information needs. It
explains, in particular, the three criteria that any occupational reference used by SSA (or
created by SSA) must meet (pages 3 – 4). We ask that all participants read this
background paper.
Listed Impairments
Some impairments are so severe that, based on medical considerations only, SSA will
determine that an individual with one of these listed impairments is unable to work and
therefore disabled, without comparing his or her functioning to the requirements of the
world of work. To adjudicate these claims, SSA does not need occupational
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-63
information. For your information, we have included, in Appendix C, a copy of the listed
impairments for mental disorders.
Appendix C is provided as a reference and is not required reading. However, we
believe that it would be helpful for all participants to have an understanding of the level
of severity reflected in these listed impairments. In the Roundtable discussion, you do
not need to consider requirements of work that reflect mental impairments so severe
that an individual with that impairment would be considered disabled without
considering the world of work.
Residual Functional Capacity
Because of the definition of disability contained in the Act and similar language in the
Regulations, SSA considers only the physically or mentally limiting effects of an
impairment(s) when assessing the functional capacity that the individual retains. That
is, SSA does not consider, for example, the individual’s age, body habitus, level of
conditioning or deconditioning, personality, aptitudes, basic talents and abilities, and so
on, when it assesses an individual’s functional capacity. It considers only the limiting
effects of the impairment(s). (See 20 CFR 404.1545 in Appendix D.)
For your reference, we have attached the form that SSA uses to document its
assessment of a claimant’s “mental residual functional capacity” (the last Appendix) and
SSA instructions to adjudicators on how to complete this form (Appendix E). As you will
see, SSA currently identifies four categories, or domains, of functioning:
Understanding and Memory,
Sustained Concentration and Persistence,
Social Interaction, and
Adaptation.
Other potential categories of functioning that might be considered include, for example,
Applying Information, Interacting with Others, Maintaining Pace, and Managing Oneself.
These categories of functioning are the focus of this Roundtable. As such, we ask that
all participants read 20 CFR 404.1545 (“Residual Functional Capacity” only) in
Appendix D and the form, “Mental Residual Functional Capacity Assessment” (SSA-
4734-SUP), in the last Appendix. Appendix E is intended to answer any questions you
may have about completion of the form, “Mental Residual Functional Assessment,” for
example, questions about the definition of the term “moderately limited,” so that these
questions do not distract from the Roundtable discussion. Reading of Appendix E is not
otherwise required.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-64
Evaluation of the Claimant’s Ability to do Past Work or Other Work
When comparing an individual’s functional capacity with the jobs that exist in the
national economy and the demands of those jobs, SSA currently uses the Dictionary of
Occupational Titles as a primary reference of how work is performed in the national
economy. In making this comparison, SSA does not consider whether work exists in
the immediate area in which the claimant lives, whether a specific job vacancy exists for
him or her, or whether the claimant would be hired if he or she applied for work. (See
20 CFR 404.1566(a) in Appendix D). In addition, if an individual is able to do work,
given his or her functional capacity and vocational profile, SSA does not consider if he
or she remains unemployed because of:
His or her inability to get work;
Lack of work in his or her local area;
The hiring practices of employers;
Technological changes in the industry in which he or she has worked;
Cyclical economic conditions;
No job openings for him or her;
The claimant would not actually be hired to do work he or she could otherwise
do; or
The claimant does not wish to do a particular type of work.
(See 20 CFR 404.1566(c) in Appendix D.)
Lastly, the Act and Regulations proscribe consideration of any element other than that
mentioned in the citations. As a result, in determining disability, SSA does not consider
elements that vocational rehabilitation specialists might consider in developing an
intervention for a client. For example, SSA does not consider placement and
employability issues, the potential for supported employment, accommodations (other
than those actually provided by a previous employer), and increased vocational
potential through training.
For “Residual Functional Capacity,” we asked that you read 20 CFR 404.1545
(“Residual Functional Capacity” only) in Appendix D. The remaining sections of
Appendix D are provided as a reference and are not required reading.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-65
Appendix C – 4
EXCERPT FROM THE SOCIAL SECURITY ACT, AS AMENDED,
AND RELATED ENACTMENTS THROUGH JANUARY 1, 2009
Disability Insurance Benefits
Sec. 223. [42 U.S.C. 423]
Definition of Disability
(d)(1) The term “disability” means … inability to engage in any substantial gainful activity by
reason of any medically determinable physical or mental impairment which can be expected to
result in death or which has lasted or can be expected to last for a continuous period of not less
than 12 months …
(2) … (A) An individual shall be determined to be under a disability only if his physical or mental
impairment or impairments are of such severity that he is not only unable to do his previous
work but cannot, considering his age, education, and work experience, engage in any other kind
of substantial gainful work which exists in the national economy, regardless of whether such
work exists in the immediate area in which he lives, or whether a specific job vacancy exists for
him, or whether he would be hired if he applied for work. For purposes of the preceding
sentence (with respect to any individual), “work which exists in the national economy” means
work which exists in significant numbers either in the region where such individual lives or in
several regions of the country.
(B) ***
(C) An individual shall not be considered to be disabled for purposes of this title if alcoholism or
drug addiction would (but for this subparagraph) be a contributing factor material to the
Commissioner's determination that the individual is disabled.
(3) For purposes of this subsection, a “physical or mental impairment” is an impairment that
results from anatomical, physiological, or psychological abnormalities which are demonstrable
by medically acceptable clinical and laboratory diagnostic techniques.
*****
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-66
This page left intentionally blank.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-67
Appendix C – 5
Mental Cognitive Roundtable – Background Paper:
Use of the Dictionary of Occupational Titles
in SSA’s Disability Program
Background
How SSA Came to Consider Vocational Factors to Evaluate Disability
When Social Security was established in 1935, the Social Security Board discussed the
prospects of creating a national program designed to protect workers in the event of
disability. Even early discussions among Social Security Board members in the mid-
1930s acknowledged that an assessment of disability would require the consideration of
vocational aspects in addition to medical factors.
3
Still, when the Social Security
Administration’s (SSA’s) disability insurance program for cash benefits was enacted in
1956, the law did not specifically require consideration of the factors of age, education,
and work experience. The Social Security Act defined disability as the “inability to
engage in any substantial gainful activity by reason of any medically determinable
physical or mental impairment which can be expected to result in death or be of long-
continued and indefinite duration”.
4
However, it soon became apparent that disability could not always be decided on
medical facts alone. In 1957, Arthur E. Hess, Assistant Director for the Division of
Disability Operations, met with staff to give them guidance about borderline cases, that
is, those cases that could not be decided on medical facts alone. He told them that they
need to view the whole person, medically and vocationally.
5
At that time, SSA used
vocational factors to rebut or overcome the presumption that the individual is not
disabled. By the late 1950s and early 1960s, SSA encountered numerous judicial and
Congressional challenges involving cases in which SSA was unable to make a disability
decision on medical facts alone and had denied disability on the basis that an individual
was able to work despite his impairment.
6
Congress investigated the new disability
3
Hess, Arthur E. (1993). The Disability Program: Its Origin, Our Heritage, Its Future, Our Challenge.
Presented at the Social Security Administration Disability Symposium in Atlanta, GA on January 21.
Baltimore: Social Security Administration.
4
Social Security Advisory Board (October 2003). The Social Security Definition of Disability, p. 3.
5
Hess, A.E. (1957) Staff paper: Adjudicative Climate in Evaluation of Borderline Cases. Presented at
Bureau of Old-Age and Survivors Insurance, Division of Disability Operations staff meeting on March 29.
6
See, for example, Kerner v. Fleming (2
nd
Circuit, 1960) and Rinaldi v. Ribicoff (2
nd
Circuit, 1962).

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-68
insurance program and its medical-vocational decision process in 1959.
7
A number of
the court cases in the early 1960s cases also focused attention on SSA’s medical-
vocational decisions. These cases involved a concept regarding “substantial evidence,”
in that once the claimant had proven that he was unable to do his previous work
because of his impairment and that he did not have the skills and functioning to do other
work, the burden of proof fell to SSA to show that he was “actually—not theoretically—
capable of doing some type of work.”
8
SSA addressed these challenges through
statutory changes and routine consultation of government occupational resources. SSA
introduced a legislative proposal to include, among other changes, the consideration of
vocational factors. Congress incorporated SSA’s proposal and passed the 1967
Amendments which added the consideration of vocational factors to SSA’s definition of
disability. Since 1967, SSA and others interpret the definition of disability in section
223(d) of the Social Security Act to require SSA to look to the world of work to
determine if an adult’s impairment(s) is disabling when the individual’s claim cannot be
decided by medical facts alone. The following language was added to the law in 1967
and remains in effect today:
“An individual shall be determined to be under a disability only if his physical or mental
impairment or impairments are of such severity that he is not only unable to do his
previous work but cannot, considering his age, education, and work experience, engage
in any other kind of substantial gainful activity which exists in the national economy,
regardless of whether such work exists in the immediate area in which he lives, or
whether he would be hired if he applied for work. For purposes of the preceding
sentence (with respect to any individual), ‘work which exists in the national economy’
means work which exists in significant numbers either in the region where such
individual lives or in several regions of the country.”
9
Consequently, SSA has referred to government labor market and occupational data
since the court challenges of the early 1960s. SSA needed the data to arrive at and
support its decisions regarding whether an individual’s impairment is of such severity
that it prevents him/her from doing not only his or her past work, but any other work in
the U.S. economy.
7
See Harrison Subcommittee Report, Preliminary Report to the Committee on Ways and Means (U.S.
House of Representatives, 1960).
8
U.S. House of Representatives, Committee on Ways and Means (1974), Subcommittee Staff Report on
the Disability Insurance Program. Washington, D.C.: U.S. Government Printing Office, p. 46.
9
See Social Security Act, Section 223(d)(2)(A)

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-69
What is the Dictionary of Occupational Titles?
Over the years, SSA has come to rely on the Department of Labor’s (DOL’s) Dictionary
of Occupational Titles (DOT) as its main occupational resource to evaluate disability
claims when the decision cannot be made based on medical facts alone. The DOT is an
occupational classification system of jobs in the U.S. economy. The DOL first developed
the classification in 1939, and it produced several updates throughout the decades.
Following its last major revision in 1977, and minor revisions in 1991, the DOT contains
over 12,000 occupations. Arranged by industry, the DOT occupation descriptions reflect
the main tasks, strength level requirements, and skill level of the occupation. In the
1970s, SSA contracted with DOL to produce a companion volume to the DOT entitled
the Selected Characteristics of Occupations (SCO) that provides measures for
additional physical demands of work for DOT occupations, such as climbing, balancing,
reaching, handling, special senses requirements (visual acuity, hearing, etc.), and
environmental requirements (noise levels, exposure to cold, etc.). The DOL last updated
the SCO in 1993.
The DOT and SCO provide measurable ratings for physical demands of work for each
of the 12,000+ occupations. These ratings have been crucial to SSA’s evaluation of how
much an individual can do despite his impairment (residual functional capacity or RFC)
and whether this level of functioning enables the individual to do his past work or any
other work.
What Compels SSA to Use the Dictionary of Occupational Titles?
Any occupational resource that SSA uses must meet at least three criteria. To date, the
DOT is the only occupational resource produced publicly or privately that accomplishes
this. The three criteria are as follows:
1. Must Reflect Work Requirements
The need for an occupational resource to enable SSA to compare human function with
work requirements is by far the largest hurdle SSA must overcome regarding its reliance
on the DOT. This criterion involves the need to assess an individual’s RFC in terms
of the ability to work. The need for demands of work that can be walked back to an
individual’s medical evidence to assess functioning is crucial because work is the
yardstick used in the statutory definition of disability. Despite active research on the
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-70
subject,
10
SSA has not been successful in finding an effective alternative that is also
operationally feasible to an RFC assessment and comparison with job demands. The
Social Security Act states…
That disability is defined as the “inability to engage in substantial gainful activity
by reason of a medically determinable physical or mental impairment…” (Section
223(d)(1)(A).
That SSA shall find an individual to be disabled only if his/her impairment(s) is so
severe that he/she “is not only unable to do…previous work, but cannot
considering age, education, and work experience, engage in any other substantial
gainful activity” (Section 223(d)(2)(A)).
It does not matter “whether such work exists in the immediate area in which [the
claimant] lives, whether a specific job vacancy exists…or whether [the claimant]
would be hired if [he/she] applied for work” (Section 223(d)(2)(A)).
Therefore, an occupational resource must enable SSA to evaluate the claimant’s ability
to perform work (residual functional capacity) rather than to obtain work (employability).
As such, the resource must reflect information that is aggregated, described, and rated
in a manner that enables SSA adjudicators to compare an individual’s RFC to work
requirements to determine the individual’s ability to perform work despite a severe
impairment(s).
So far, the DOT is the only resource of occupations existing nationwide that provides
the measures needed to assess function in terms of ability to work.
11
2. Must Reflect National Existence and Incidence of Work
The Act states…
That SSA must consider the claimant’s age, education, and work experience to
determine if he/she can “engage in any other substantial gainful activity” that “exists
in the national economy.”(Section 223(d)(2)(A)).
10
Institute of Medicine (1999). Measuring Functional Capacity and Work Requirements: Summary of a
Workshop;
American Institutes for Research (1999). Synthesis, Integration, and Completion of Research into a New
Disability Decision Making Process and Development of Initial Prototype of that Process; Disability
Research Institute (2002). Job Demands Project.
11
While at least one private sector update of DOT data exists, it only updates DOT data and does not
represent a new or different classification system.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-71
That “‘work which exists in the national economy’ means work which exists in
significant numbers either in the region where the individual lives or in several other
regions of the country.” (Section 223(d)(2)(A)).
Therefore, any occupational resource that SSA uses must reflect work that actually
exists in “significant numbers” throughout the nation (or throughout at least several
regions of the nation). To meet this requirement of the law, SSA regulations take
administrative notice of the reliable job information from various government sources,
including the DOT.
12
More information about SSA vocational rules is discussed below.
3. Must Meet the Burden of Proof in a Legally Defensible Way
Section 223(d)(2)(A) was added to the Social Security Act in 1967 to address judicial
13
and legislative
14
concerns regarding SSA’s burden of proof and consistency in making
disability determinations or decisions in cases for which both medical and non-medical
factors must be considered. This section of the Act has long been construed to mean
that SSA has a burden of proof regarding its determination or decision that a claimant
has the ability to work despite a severe medical impairment. SSA must show “what the
claimant can do”
15
and that the claimant is “actually—not theoretically—capable of doing
some kind of work.”
16
Therefore, any alternative occupational resource SSA uses must be legally defensible
for SSA to meet its burden of proof.
17
This means that the alternative resource should
be validated by an objective third party for use in SSA’s disability process. While the
DOT is imperfect, SSA’s use of it has been upheld in the Supreme Court.
18
It has face
validity that has been tested judicially.
12
20 CFR 404.1566(d) and 416.966(d)
13
See Kerner v. Fleming (2
nd
Circuit, 1960) and Rinaldi v. Ribicoff (2
nd
Circuit, 1962).
14
See Harrison Subcommittee Report, Preliminary Report to the Committee on Ways and Means (U.S.
House of Representatives, 1960), pp. 17-20.
15
SSA’s need to show “what the claimant can do” is one of the main points of the Kerner Doctrine that
formed the basis for SSA’s vocational policy in the early 1960’s and led to the 1967 Amendments’
addition of vocational factors to the Statute. See Kerner v. Fleming (2
nd
Circuit, 1960).
16
Committee on the Ways and Means, Staff Report on the Disability Insurance Program (U.S. House of
Representatives, 1974), p. 45.
17
Courts require expert testimony (and the data and methods used) to meet specific standards. Daubert
v. Merrell Dow Pharmaceuticals, Inc., 509 U.S. 579 (1993), and Kuomo Tire Co. v. Carmichael, ___ U.S.
___, No. 97-1709, Slip op. at 11, 67 USLW 4179, 4183 (March 23, 1999).
18
See Taylor v. Schweiker (SSR 82-47c) and Campbell vs. Heckler (SSR 83-46c).

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-72
Use of the Dictionary of Occupational Titles for SSA Disability Evaluation
As outlined above, the Social Security Act defines disability as follows:
“inability to engage in any substantial gainful activity by reason of a medically
determinable physical or mental impairment which can be expected to result in death or
which has lasted or can be expected to last for a continuous period of not less than 12
months..[a]n individual shall be determined to be under a disability only if his physical or
mental impairment or impairments are of such severity that he is not only unable to do
his previous work but cannot, considering his age, education, and work experience,
engage in any other kind of substantial gainful activity which exists in the national
economy
19
An important point is that SSA’s definition of disability embodies a medical-vocational
concept. It requires a medical cause (i.e., a “medically determinable physical or mental
impairment”) and a directly related vocational consequence (i.e., the “inability to engage
in any substantial gainful activity”). So, SSA’s disability evaluation process relies,
fundamentally, on a comparison between what a person can do and what jobs require.
Sequential Evaluation Process
To decide whether an individual is disabled under this definition, SSA has established
an evaluation process that all adjudicators at all levels must follow.
20
We consider the
following questions, sequentially, and stop as soon we reach a decision:
Step 1: Is the individual currently working and performing “substantial gainful
activity” (SGA)? If yes, the person is not disabled. Otherwise, go to step
2.
Step 2: Does the individual have an impairment that is severe and meets duration
requirements? If no, the person is not disabled. Otherwise, go to step 3.
Step 3: Does the individual’s impairment(s) meet (or equal) the criteria in the
Listing of Impairments? If yes, the person is disabled. Otherwise, go to
step 4.
19
§223(d)(1)(A) and 223(d)(2)(A) of the Social Security Act. The Statute provides a different definition of
disability for children under the age of 18 applying for benefits under Title XVI.
20
See 20 CFR 404.1520 and 416.920. If an individual already qualifies for benefits and SSA must
determine whether his/her disability continues, SSA uses a different sequential evaluation process that
includes a medical improvement review standard. See §§404.1594 and 416.994 of our regulations.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-73
Step 4: Is the individual still able to perform past work? If yes, the person is not
disabled. Otherwise, go to step 5.
Step 5: Is the individual able to do other work, given his/her residual functional
capacity, age, education, and work experience? If yes, the person is not
disabled. If no, he/she is disabled.
The First Three Steps
While the first three steps of the five-step sequential evaluation process do not require
adjudicators to consult an occupational reference, each of the three steps has a
connection to the world of work. At step 1, we determine whether the individual is
working (doing “substantial gainful activity”). At step 2, we consider the medical severity
and duration of the individual’s impairment(s). Regarding severity, we determine
whether the impairment(s) prevents the individual from doing basic work activities. SSA
regulations define these activities as “abilities and aptitudes necessary to do most jobs,”
and the regulations provide examples:
Physical functions such as walking, standing, sitting, lifting, carrying, reaching, handling,
etc.
Capacities for seeing, hearing, and speaking.
Understanding, carrying out, and remembering simple instructions.
Use of judgment.
Responding appropriately to supervision, co-workers, etc.
Dealing with changes in a routine work setting.
21
At step 3, we consider whether the individual’s impairment(s) meets or equals the
criteria cited in the Listing of Impairments.
22
SSA does not consider the vocational
factors of age, education, and work experience at this step. The Listing of Impairments
describes impairments that SSA considers to be severe enough to prevent an individual
from doing any gainful activity, a stricter standard than “substantial gainful activity” that
is applied at steps 1, 4 and 5.
21
See §§ 404.1520 and 416.920.
22
See §§ 404.1520 (d) and 416.920(d). For the purpose of the Listing of Impairments, see §§
404.1525(a) and 416.925(a). Listing of Impairments can be found in Appendix 1, Part 404, Subpart P.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-74
Assessment of Residual Functional Capacity
If we cannot determine at step 3 whether an individual is disabled, we must proceed to
step 4. But before we go to step 4, we must assess the individual’s RFC. The RFC is
the most an individual can do despite the limitations of his or her impairment(s). We
assess RFC based on all relevant medical and other evidence that is in the individual’s
case record.
Assessment of human function is one side of the disability evaluation equation, and the
assessment of what is required to do work forms the other side of the equation. The
DOT and the SCO classify what is physically required, including ratings and measures,
for over 12,000 occupations nationwide. To be able to make use of the DOT’s
descriptions of work as proxies for the ability to function, SSA’s RFC assessment
process is based on DOT/SCO definitions, ratings, and measures. As such, the form
SSA uses to assess physical RFC (SSA-4734-BK) describes a person’s ability to do
work-related physical activity in terms of the rating categories cited in the DOT and
SCO, e.g., physical demands related to strength (walking, standing, lifting, carrying,
etc.) or other physical functions, including postural and manipulative functions (stooping,
crouching, reaching, handling, etc.).
23
Connections between the DOT definitions, ratings, and measures of physical demands
of work and SSA’s RFC are evident in how SSA assesses physical function, such as
strength. For example, the DOT classifies work into five strength levels, with
“sedentary” being the lowest and “very heavy” being the highest. SSA’s physical RFC
enables SSA adjudicators and medical consultants to rate the most the individual can
do in terms of strength (e.g., lifting, carrying, standing, walking) and other physical
functions so that the individual’s RFC can be compared to his or her past work or other
work as defined in the DOT. Figure 1 on the next page displays an example of case
information and how the RFC and DOT definitions mesh to enable an adjudicator to
evaluate the individual’s RFC, and ability to do past or other work.
23
See §§ 404.1545 and 416.945. For individuals with mental disorders, we also rate their ability to meet
other job demands that are not captured in the DOT, such as the ability to understand, remember and
carry out instructions, and the ability to respond appropriately to supervision, co-workers, and work
pressures in a work setting. See §§ 404.1545(c) and 416.945(c).

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-75
Figure 1: Illustration of How DOT Definitions are Reflected in Evaluation of RFC and
Steps 4 and 5.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-76
Figure 1 shows how evidence from the individual’s (Joe Smith’s) case record is used to
evaluate his RFC. Also, Figure 1 illustrates that the RFC questions are based on
definitions, measures, and ratings from the DOT. Figure 1 indicates that Joe Smith has
an RFC that limits him to work involving the lowest strength level, sedentary work. That
means that Joe cannot do his past work as a Street Light Wirer, either as he did it or as
it is done in the economy generally, because the limitations of his back impairment
prevent him from doing key tasks. Also, we see that the job requires a higher strength
level (light) than his RFC permits. Furthermore, given his age (55), education (11
th
grade), work experience (semi-skilled and cannot be transferred to other work), and
RFC (sedentary), we would find he is disabled as directed by rule 201.02. Figure 1
features a portion of Table 1 of the Grid, which includes rules for cases in which the
individual in limited to sedentary work, and the relevant rule and vocational factors are
circled.
Step 4
At step 4, we compare the individual’s RFC to the demands of his or her past work. If
the individual cannot do his/her past work as the individual describes it, then we must
determine if he or she has the RFC to do his or her past work as it is done generally in
the economy. When we do this, we often rely on the DOT/SCO for information about the
job demands that are relevant to the individual’s RFC.
Step 5
If the individual cannot do his/her past work, we move on to step 5. At this point, we
use the same RFC assessment to decide whether there are other jobs the individual
can do, considering his/her age, education and work experience. To make this
judgment, we use the DOT and SCO for information about other jobs that may be within
the person’s abilities and to help assess the potential vocational
advantages/disadvantages of the person’s education and work experience (i.e.,
acquired skills). We use the DOT to cite jobs in certain situations when we determine
that an individual can do other work. SSA’s regulations also permit the use of vocational
experts or other specialists,
24
and these experts frequently rely on occupational
resources that are also tied to the DOT.
Using the Grid at Step 5
SSA’s regulations take administrative notice of “reliable job information available from
various governmental and other publications,” including the DOT.
25
At step 5, SSA
24
See 20 CFR 404.1566(e) and 416.966(e)
25
See 20 CFR 404.1566(d) and 416.966(d)

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-77
adjudicators must consult a set of tables in Appendix 2 of Part 404, Subpart P, known
as the vocational rules or the Grid, to arrive at a decision. The Grid combines certain
medical-vocational fact patterns into “rules” that direct a decisional outcome (i.e., either
“disabled” or “not disabled”). The four basic factors that are combined in the Grid involve
strength level (based on RFC assessment and DOT ratings), age, education, and work
experience (no work, unskilled, semi-skilled, or skilled). The existence of jobs in the
national economy is reflected in the “Decisions” shown in the vocational rules.
26
Below are excerpts of the Grid displaying a few rules in each of the tables. Note that
each table reflects a distinct strength level: sedentary, light, medium:
Table No. 1—Residual Functional Capacity: Maximum Sustained Work Capability
Limited to Sedentary Work as a Result of Severe Medically Determinable Impairment(s)
Rule Age Education Previous work experience Decision
201.01 Advanced age Limited or less Unskilled or none Disabled
201.02 ......do ......do
Skilled or semiskilled—skills not
transferable
Do.
*Table 1 contains 29 rules: 201.01-201.29
Table No. 2—Residual Functional Capacity: Maximum Sustained Work Capability
Limited to Light Work as a Result of Severe Medically Determinable Impairment(s)
Rule Age Education
Previous work
experience Decision
202.0
1
Advanced
age
Limited or less Unskilled or none Disabled.
202.0
5
......do
High school graduate or more—
provides for direct entry into skilled
work
[2]
......do
Not
disabled.
*Table 2 contains 22 rules: 202.01 through 202.22.
26
See Part 404, Subpart P, Appendix 2, Section 200.00(b).

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-78
Table No. 3—Residual Functional Capacity: Maximum Sustained Work Capability
Limited to Medium Work as a Result of Severe Medically Determinable Impairment(s)
Rule Age Education
Previous work
experience Decision
203.01
Closely approaching
retirement age
Marginal or
none
Unskilled or none Disabled.
203.03 ......do Limited Unskilled
Not
disabled.
203.05 ......do ......do
Skilled or semiskilled—
skills transferable
Do.
*Table 3 contains 31 rules: 203.01 through 203.31
Section 204.00 of Appendix 2, Part 404, Subpart P, represents work that is heavy or
very heavy. There is no table for section 204.00, and it is most often used when the
individual has a severe impairment(s) that affects mental or cognitive functions or other
non-strength physical functions, but there are no strength limitations. Therefore,
adjudicators use this rule when evaluating an impairment that does not preclude heavy
work (or very heavy work), considering also age, education, and skill level of prior work
experience.
All disability decisions made at step 5 are based on the Grid. If the facts of the case
coincide directly with a Grid rule, we use the rule to direct the decision. However, if the
facts of the case do not coincide exactly with the factors of a particular rule, we use the
rule as guidance for decision-making, that is, we use the rule as a “framework.” For
example, if the individual has both strength and non-strength limitations, the adjudicator
must select the Grid rule that comes closest to facts of the case and use this rule as a
framework. This is because the Grid reflects strength-related ratings, and it does not
reflect non-strength physical limitations or mental/cognitive limitations. SSA regulations
and rulings provide adjudicators guidance on how to assess limitations that are not
reflected in the Grid to arrive at “framework” decisions.
27
The Grid matters for two main reasons:
It takes “administrative notice” of the total number of unskilled jobs in the nation
at three physical strength levels as classified in the DOT. This enables SSA to
27
See §§ 404.1545(b) and (c), as well as 416.945(b) and (c). See also Part 404, Subpart P, Appendix 2,
§§ 200.00(a)-(e). See also SSR 83-12, SSR 83-14, SSR 85-15, SSR 96-4p, SSR 96-8p, and SSR 96-9p.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-79
meet its burden of proof at step 5 when an adjudicator finds that an individual is
capable of doing other work, considering the individual’s RFC, age, education,
and work experience (skill level).
It provides consistent “rulemaking” or application of case fact patterns regarding
RFC and vocational factors to ensure that SSA’s decisions are uniform, not
arbitrary and capricious.
28
In summary, the five steps of sequential evaluation described above are derived from
the definition of disability in the Social Security Act. This brief overview describes the
importance of occupational information to SSA’s disability programs. For more than 50
years, SSA has been considering occupational information in disability determinations
after reaching the conclusion that disability eligibility could not always be decided on
medical factors alone. Over the years, SSA has come to rely on the Department of
Labor’s DOT as the main source of this occupational information. Although the DOT
was not designed specifically for SSA’s disability programs, it comes closer to meeting
SSA’s legal and programmatic requirements than any other existing occupational
information resource. Any occupational information system designed for SSA’s
disability programs would need to replace the DOT, and meet three requirements: 1) It
must reflect the requirements of work, 2) It must reflect the national existence and
incidence of work, and 3) It must meet SSA’s “Burden of Proof” in a legally defensible
way.
28
See SSR 83-46c, Heckler v. Campbell.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-80
This page left intentionally blank.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-81
Appendix C – 6
Mental Cognitive Roundtable – Listed Impairments for Mental Disorders
Disability Evaluation under Social Security
(Blue Book- September 2008)
12.00 Mental Disorders
A. Introduction: The evaluation of disability on the basis of mental disorders requires
documentation of a medically determinable impairment(s), consideration of the degree
of limitation such impairment(s) may impose on the individual's ability to work, and
consideration of whether these limitations have lasted or are expected to last for a
continuous period of at least 12 months. The listings for mental disorders are arranged
in nine diagnostic categories: Organic mental disorders (12.02); schizophrenic, paranoid
and other psychotic disorders (12.03); affective disorders (12.04); mental retardation
(12.05); anxiety-related disorders (12.06); somatoform disorders (12.07); personality
disorders (12.08); substance addiction disorders (12.09); and autistic disorder and other
pervasive developmental disorders (12.10). Each listing, except 12.05 and 12.09,
consists of a statement describing the disorder(s) addressed by the listing, paragraph A
criteria (a set of medical findings), and paragraph B criteria (a set of impairment-related
functional limitations). There are additional functional criteria (paragraph C criteria) in
12.02, 12.03, 12.04, and 12.06, discussed herein. We will assess the paragraph B
criteria before we apply the paragraph C criteria. We will assess the paragraph C
criteria only if we find that the paragraph B criteria are not satisfied. We will find that you
have a listed impairment if the diagnostic description in the introductory paragraph and
the criteria of both paragraphs A and B (or A and C, when appropriate) of the listed
impairment are satisfied.
The criteria in paragraph A substantiate medically the presence of a particular mental
disorder. Specific symptoms, signs, and laboratory findings in the paragraph A criteria of
any of the listings in this section cannot be considered in isolation from the description
of the mental disorder contained at the beginning of each listing category. Impairments
should be analyzed or reviewed under the mental category(ies) indicated by the medical
findings. However, we may also consider mental impairments under physical body
system listings, using the concept of medical equivalence, when the mental disorder
results in physical dysfunction. (See, for instance, 12.00D12 regarding the evaluation of
anorexia nervosa and other eating disorders.)
The criteria in paragraphs B and C describe impairment-related functional limitations
that are incompatible with the ability to do any gainful activity. The functional limitations
in paragraphs B and C must be the result of the mental disorder described in the
diagnostic description, that is manifested by the medical findings in paragraph A.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-82
The structure of the listing for mental retardation (12.05) is different from that of the
other mental disorders listings. Listing 12.05 contains an introductory paragraph with the
diagnostic description for mental retardation. It also contains four sets of criteria
(paragraphs A through D). If your impairment satisfies the diagnostic description in the
introductory paragraph and any one of the four sets of criteria, we will find that your
impairment meets the listing. Paragraphs A and B contain criteria that describe
disorders we consider severe enough to prevent your doing any gainful activity without
any additional assessment of functional limitations. For paragraph C, we will assess the
degree of functional limitation the additional impairment(s) imposes to determine if it
significantly limits your physical or mental ability to do basic work activities, i.e., is a
"severe" impairment(s), as defined in §§ 404.1520(c) and 416.920(c). If the additional
impairment(s) does not cause limitations that are "severe" as defined in §§ 404.1520(c)
and 416.920(c), we will not find that the additional impairment(s) imposes "an additional
and significant work-related limitation of function," even if you are unable to do your past
work because of the unique features of that work. Paragraph D contains the same
functional criteria that are required under paragraph B of the other mental disorders
listings.
The structure of the listing for substance addiction disorders, 12.09, is also different
from that for the other mental disorder listings. Listing 12.09 is structured as a reference
listing; that is, it will only serve to indicate which of the other listed mental or physical
impairments must be used to evaluate the behavioral or physical changes resulting from
regular use of addictive substances.
The listings are so constructed that an individual with an impairment(s) that meets or is
equivalent in severity to the criteria of a listing could not reasonably be expected to do
any gainful activity. These listings are only examples of common mental disorders that
are considered severe enough to prevent an individual from doing any gainful activity.
When you have a medically determinable severe mental impairment that does not
satisfy the diagnostic description or the requirements of the paragraph A criteria of the
relevant listing, the assessment of the paragraph B and C criteria is critical to a
determination of equivalence.
If your impairment(s) does not meet or is not equivalent in severity to the criteria of any
listing, you may or may not have the residual functional capacity (RFC) to do substantial
gainful activity (SGA). The determination of mental RFC is crucial to the evaluation of
your capacity to do SGA when your impairment(s) does not meet or equal the criteria of
the listings, but is nevertheless severe.
RFC is a multidimensional description of the work-related abilities you retain in spite of
your medical impairments. An assessment of your RFC complements the functional
evaluation necessary for paragraphs B and C of the listings by requiring consideration
of an expanded list of work-related capacities that may be affected by mental disorders
when your impairment(s) is severe but neither meets nor is equivalent in severity to a
listed mental disorder.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-83
B. Need for medical evidence: We must establish the existence of a medically
determinable impairment(s) of the required duration by medical evidence consisting of
symptoms, signs, and laboratory findings (including psychological test findings).
Symptoms are your own description of your physical or mental impairment(s).
Psychiatric signs are medically demonstrable phenomena that indicate specific
psychological abnormalities, e.g., abnormalities of behavior, mood, thought, memory,
orientation, development, or perception, as described by an appropriate medical source.
Symptoms and signs generally cluster together to constitute recognizable mental
disorders described in the listings. The symptoms and signs may be intermittent or
continuous depending on the nature of the disorder.
C. Assessment of severity: We measure severity according to the functional
limitations imposed by your medically determinable mental impairment(s). We assess
functional limitations using the four criteria in paragraph B of the listings: Activities of
daily living; social functioning; concentration, persistence, or pace; and episodes of
decompensation. Where we use "marked" as a standard for measuring the degree of
limitation, it means more than moderate but less than extreme. A marked limitation may
arise when several activities or functions are impaired, or even when only one is
impaired, as long as the degree of limitation is such as to interfere seriously with your
ability to function independently, appropriately, effectively, and on a sustained basis.
See §§ 404.1520a and 416.920a.
1. Activities of daily living include adaptive activities such as cleaning, shopping,
cooking, taking public transportation, paying bills, maintaining a residence, caring
appropriately for your grooming and hygiene, using telephones and directories, and
using a post office. In the context of your overall situation, we assess the quality of
these activities by their independence, appropriateness, effectiveness, and
sustainability. We will determine the extent to which you are capable of initiating and
participating in activities independent of supervision or direction.
We do not define "marked" by a specific number of activities of daily living in which
functioning is impaired, but by the nature and overall degree of interference with
function. For example, if you do a wide range of activities of daily living, we may still find
that you have a marked limitation in your daily activities if you have serious difficulty
performing them without direct supervision, or in a suitable manner, or on a consistent,
useful, routine basis, or without undue interruptions or distractions.
2. Social functioning refers to your capacity to interact independently, appropriately,
effectively, and on a sustained basis with other individuals. Social functioning includes
the ability to get along with others, such as family members, friends, neighbors, grocery
clerks, landlords, or bus drivers. You may demonstrate impaired social functioning by,
for example, a history of altercations, evictions, firings, fear of strangers, avoidance of
interpersonal relationships, or social isolation. You may exhibit strength in social
functioning by such things as your ability to initiate social contacts with others,
communicate clearly with others, or interact and actively participate in group activities.
We also need to consider cooperative behaviors, consideration for others, awareness of
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-84
others' feelings, and social maturity. Social functioning in work situations may involve
interactions with the public, responding appropriately to persons in authority (e.g.,
supervisors), or cooperative behaviors involving coworkers.
We do not define "marked" by a specific number of different behaviors in which social
functioning is impaired, but by the nature and overall degree of interference with
function. For example, if you are highly antagonistic, uncooperative, or hostile but are
tolerated by local storekeepers, we may nevertheless find that you have a marked
limitation in social functioning because that behavior is not acceptable in other social
contexts.
3. Concentration, persistence or pace refers to the ability to sustain focused attention
and concentration sufficiently long to permit the timely and appropriate completion of
tasks commonly found in work settings. Limitations in concentration, persistence, or
pace are best observed in work settings, but may also be reflected by limitations in
other settings. In addition, major limitations in this area can often be assessed through
clinical examination or psychological testing. Wherever possible, however, a mental
status examination or psychological test data should be supplemented by other
available evidence.
On mental status examinations, concentration is assessed by tasks such as having you
subtract serial sevens or serial threes from 100. In psychological tests of intelligence or
memory, concentration is assessed through tasks requiring short-term memory or
through tasks that must be completed within established time limits.
In work evaluations, concentration, persistence, or pace is assessed by testing your
ability to sustain work using appropriate production standards, in either real or simulated
work tasks (e.g., filing index cards, locating telephone numbers, or disassembling and
reassembling objects). Strengths and weaknesses in areas of concentration and
attention can be discussed in terms of your ability to work at a consistent pace for
acceptable periods of time and until a task is completed, and your ability to repeat
sequences of action to achieve a goal or an objective.
We must exercise great care in reaching conclusions about your ability or inability to
complete tasks under the stresses of employment during a normal workday or
workweek based on a time-limited mental status examination or psychological testing by
a clinician, or based on your ability to complete tasks in other settings that are less
demanding, highly structured, or more supportive. We must assess your ability to
complete tasks by evaluating all the evidence, with an emphasis on how independently,
appropriately, and effectively you are able to complete tasks on a sustained basis.
We do not define "marked" by a specific number of tasks that you are unable to
complete, but by the nature and overall degree of interference with function. You may
be able to sustain attention and persist at simple tasks but may still have difficulty with
complicated tasks. Deficiencies that are apparent only in performing complex
procedures or tasks would not satisfy the intent of this paragraph B criterion. However, if
you can complete many simple tasks, we may nevertheless find that you have a marked
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-85
limitation in concentration, persistence, or pace if you cannot complete these tasks
without extra supervision or assistance, or in accordance with quality and accuracy
standards, or at a consistent pace without an unreasonable number and length of rest
periods, or without undue interruptions or distractions.
4. Episodes of decompensation are exacerbations or temporary increases in symptoms
or signs accompanied by a loss of adaptive functioning, as manifested by difficulties in
performing activities of daily living, maintaining social relationships, or maintaining
concentration, persistence, or pace. Episodes of decompensation may be demonstrated
by an exacerbation in symptoms or signs that would ordinarily require increased
treatment or a less stressful situation (or a combination of the two). Episodes of
decompensation may be inferred from medical records showing significant alteration in
medication; or documentation of the need for a more structured psychological support
system (e.g., hospitalizations, placement in a halfway house, or a highly structured and
directing household); or other relevant information in the record about the existence,
severity, and duration of the episode.
The term repeated episodes of decompensation, each of extended duration in these
listings means three episodes within 1 year, or an average of once every 4 months,
each lasting for at least 2 weeks. If you have experienced more frequent episodes of
shorter duration or less frequent episodes of longer duration, we must use judgment to
determine if the duration and functional effects of the episodes are of equal severity and
may be used to substitute for the listed finding in a determination of equivalence.
D. Documentation: The evaluation of disability on the basis of a mental disorder
requires sufficient evidence to (1) establish the presence of a medically determinable
mental impairment(s), (2) assess the degree of functional limitation the impairment(s)
imposes, and (3) project the probable duration of the impairment(s). See §§ 404.1512
and 416.912 for a discussion of what we mean by "evidence" and how we will assist you
in developing your claim. Medical evidence must be sufficiently complete and detailed
as to symptoms, signs, and laboratory findings to permit an independent determination.
In addition, we will consider information from other sources when we determine how the
established impairment(s) affects your ability to function. We will consider all relevant
evidence in your case record.
1. Sources of evidence.
a. Medical evidence. There must be evidence from an acceptable medical source
showing that you have a medically determinable mental impairment. See §§ 404.1508,
404.1513, 416.908, and 416.913. We will make every reasonable effort to obtain all
relevant and available medical evidence about your mental impairment(s), including its
history, and any records of mental status examination, psychological testing, and
hospitalizations and treatment. Whenever possible, and appropriate, medical source
evidence should reflect the medical source's considerations of information from you and
other concerned persons who are aware of your activities of daily living; social
functioning; concentration, persistence, or pace; or episodes of decompensation. Also,
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-86
in accordance with standard clinical practice, any medical source assessment of your
mental functioning should take into account any sensory, motor, or communication
abnormalities, as well as your cultural and ethnic background.
b. Information from the individual. Individuals with mental impairments can often provide
accurate descriptions of their limitations. The presence of a mental impairment does not
automatically rule you out as a reliable source of information about your own functional
limitations. When you have a mental impairment and are willing and able to describe
your limitations, we will try to obtain such information from you. However, you may not
be willing or able to fully or accurately describe the limitations resulting from your
impairment(s). Thus, we will carefully examine the statements you provide to determine
if they are consistent with the information about, or general pattern of, the impairment as
described by the medical and other evidence, and to determine whether additional
information about your functioning is needed from you or other sources.
c. Other information. Other professional health care providers (e.g., psychiatric nurse,
psychiatric social worker) can normally provide valuable functional information, which
should be obtained when available and needed. If necessary, information should also
be obtained from nonmedical sources, such as family members and others who know
you, to supplement the record of your functioning in order to establish the consistency of
the medical evidence and longitudinality of impairment severity, as discussed in
12.00D2. Other sources of information about functioning include, but are not limited to,
records from work evaluations and rehabilitation progress notes.
2. Need for longitudinal evidence. Your level of functioning may vary considerably over
time. The level of your functioning at a specific time may seem relatively adequate or,
conversely, rather poor. Proper evaluation of your impairment(s) must take into account
any variations in the level of your functioning in arriving at a determination of severity
over time. Thus, it is vital to obtain evidence from relevant sources over a sufficiently
long period prior to the date of adjudication to establish your impairment severity.
3. Work attempts. You may have attempted to work or may actually have worked during
the period of time pertinent to the determination of disability. This may have been an
independent attempt at work or it may have been in conjunction with a community
mental health or sheltered program, and it may have been of either short or long
duration. Information concerning your behavior during any attempt to work and the
circumstances surrounding termination of your work effort are particularly useful in
determining your ability or inability to function in a work setting. In addition, we should
also examine the degree to which you require special supports (such as those provided
through supported employment or transitional employment programs) in order to work.
4. Mental status examination. The mental status examination is performed in the course
of a clinical interview and is often partly assessed while the history is being obtained. A
comprehensive mental status examination generally includes a narrative description of
your appearance, behavior, and speech; thought process (e.g., loosening of
associations); thought content (e.g., delusions); perceptual abnormalities (e.g.,
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-87
hallucinations); mood and affect (e.g., depression, mania); sensorium and cognition
(e.g., orientation, recall, memory, concentration, fund of information, and intelligence);
and judgment and insight. The individual case facts determine the specific areas of
mental status that need to be emphasized during the examination.
5. Psychological testing.
a. Reference to a "standardized psychological test" indicates the use of a psychological
test measure that has appropriate validity, reliability, and norms, and is individually
administered by a qualified specialist. By "qualified," we mean the specialist must be
currently licensed or certified in the State to administer, score, and interpret
psychological tests and have the training and experience to perform the test.
b. Psychological tests are best considered as standardized sets of tasks or questions
designed to elicit a range of responses. Psychological testing can also provide other
useful data, such as the specialist's observations regarding your ability to sustain
attention and concentration, relate appropriately to the specialist, and perform tasks
independently (without prompts or reminders). Therefore, a report of test results should
include both the objective data and any clinical observations.
c. The salient characteristics of a good test are: (1) Validity, i.e., the test measures what
it is supposed to measure; (2) reliability, i.e., the consistency of results obtained over
time with the same test and the same individual; (3) appropriate normative data, i.e.,
individual test scores can be compared to test data from other individuals or groups of a
similar nature, representative of that population; and (4) wide scope of measurement,
i.e., the test should measure a broad range of facets/aspects of the domain being
assessed. In considering the validity of a test result, we should note and resolve any
discrepancies between formal test results and the individual's customary behavior and
daily activities.
6. Intelligence tests.
a. The results of standardized intelligence tests may provide data that help verify the
presence of mental retardation or organic mental disorder, as well as the extent of any
compromise in cognitive functioning. However, since the results of intelligence tests are
only part of the overall assessment, the narrative report that accompanies the test
results should comment on whether the IQ scores are considered valid and consistent
with the developmental history and the degree of functional limitation.
b. Standardized intelligence test results are essential to the adjudication of all cases of
mental retardation that are not covered under the provisions of 12.05A. Listing 12.05A
may be the basis for adjudicating cases where the results of standardized intelligence
tests are unavailable, e.g., where your condition precludes formal standardized testing.
c. Due to such factors as differing means and standard deviations, identical IQ scores
obtained from different tests do not always reflect a similar degree of intellectual
functioning. The IQ scores in 12.05 reflect values from tests of general intelligence that
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-88
have a mean of 100 and a standard deviation of 15; e.g., the Wechsler series. IQs
obtained from standardized tests that deviate from a mean of 100 and a standard
deviation of 15 require conversion to a percentile rank so that we can determine the
actual degree of limitation reflected by the IQ scores. In cases where more than one IQ
is customarily derived from the test administered, e.g., where verbal, performance, and
full scale IQs are provided in the Wechsler series, we use the lowest of these in
conjunction with 12.05.
d. Generally, it is preferable to use IQ measures that are wide in scope and include
items that test both verbal and performance abilities. However, in special
circumstances, such as the assessment of individuals with sensory, motor, or
communication abnormalities, or those whose culture and background are not
principally English-speaking, measures such as the Test of Nonverbal Intelligence,
Third Edition (TONI-3), Leiter International Performance Scale-Revised (Leiter-R), or
Peabody Picture Vocabulary Test-Third Edition (PPVT-III) may be used.
e. We may consider exceptions to formal standardized psychological testing when an
individual qualified by training and experience to perform such an evaluation is not
available, or in cases where appropriate standardized measures for your social,
linguistic, and cultural background are not available. In these cases, the best indicator of
severity is often the level of adaptive functioning and how you perform activities of daily
living and social functioning.
7. Personality measures and projective testing techniques. Results from standardized
personality measures, such as the Minnesota Multiphasic Personality Inventory-Revised
(MMPI-II), or from projective types of techniques, such as the Rorschach and the
Thematic Apperception Test (TAT), may provide useful data for evaluating several types
of mental disorders. Such test results may be useful for disability evaluation when
corroborated by other evidence, including results from other psychological tests and
information obtained in the course of the clinical evaluation, from treating and other
medical sources, other professional health care providers, and nonmedical sources.
Any inconsistency between test results and clinical history and observation should be
explained in the narrative description.
8. Neuropsychological assessments. Comprehensive neuropsychological examinations
may be used to establish the existence and extent of compromise of brain function,
particularly in cases involving organic mental disorders. Normally, these examinations
include assessment of cerebral dominance, basic sensation and perception, motor
speed and coordination, attention and concentration, visual-motor function, memory
across verbal and visual modalities, receptive and expressive speech, higher-order
linguistic operations, problem-solving, abstraction ability, and general intelligence. In
addition, there should be a clinical interview geared toward evaluating pathological
features known to occur frequently in neurological disease and trauma; e.g., emotional
lability, abnormality of mood, impaired impulse control, passivity and apathy, or
inappropriate social behavior. The specialist performing the examination may administer
one of the commercially available comprehensive neuropsychological batteries, such as
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-89
the Luria-Nebraska or the Halstead-Reitan, or a battery of tests selected as relevant to
the suspected brain dysfunction. The specialist performing the examination must be
properly trained in this area of neuroscience.
9. Screening tests. In conjunction with clinical examinations, sources may report the
results of screening tests; i.e., tests used for gross determination of level of functioning.
Screening instruments may be useful in uncovering potentially serious impairments, but
often must be supplemented by other data. However, in some cases the results of
screening tests may show such obvious abnormalities that further testing will clearly be
unnecessary.
10. Traumatic brain injury (TBI). In cases involving TBI, follow the documentation and
evaluation guidelines in 11.00F.
11. Anxiety disorders. In cases involving agoraphobia and other phobic disorders, panic
disorders, and posttraumatic stress disorders, documentation of the anxiety reaction is
essential. At least one detailed description of your typical reaction is required. The
description should include the nature, frequency, and duration of any panic attacks or
other reactions, the precipitating and exacerbating factors, and the functional effects. If
the description is provided by a medical source, the reporting physician or psychologist
should indicate the extent to which the description reflects his or her own observations
and the source of any ancillary information. Statements of other persons who have
observed you may be used for this description if professional observation is not
available.
12. Eating disorders. In cases involving anorexia nervosa and other eating disorders,
the primary manifestations may be mental or physical, depending upon the nature and
extent of the disorder. When the primary functional limitation is physical; e.g., when
severe weight loss and associated clinical findings are the chief cause of inability to
work, we may evaluate the impairment under the appropriate physical body system
listing. Of course, we must also consider any mental aspects of the impairment, unless
we can make a fully favorable determination or decision based on the physical
impairment(s) alone.
E. Chronic mental impairments. Particular problems are often involved in evaluating
mental impairments in individuals who have long histories of repeated hospitalizations
or prolonged outpatient care with supportive therapy and medication. For instance, if
you have chronic organic, psychotic, and affective disorders, you may commonly have
your life structured in such a way as to minimize your stress and reduce your symptoms
and signs. In such a case, you may be much more impaired for work than your
symptoms and signs would indicate. The results of a single examination may not
adequately describe your sustained ability to function. It is, therefore, vital that we
review all pertinent information relative to your condition, especially at times of
increased stress. We will attempt to obtain adequate descriptive information from all
sources that have treated you in the time period relevant to the determination or
decision.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-90
F. Effects of structured settings. Particularly in cases involving chronic mental
disorders, overt symptomatology may be controlled or attenuated by psychosocial
factors such as placement in a hospital, halfway house, board and care facility, or other
environment that provides similar structure. Highly structured and supportive settings
may also be found your home. Such settings may greatly reduce the mental demands
placed on you. With lowered mental demands, overt symptoms and signs of the
underlying mental disorder may be minimized. At the same time, however, your ability to
function outside of such a structured or supportive setting may not have changed. If
your symptomatology is controlled or attenuated by psychosocial factors, we must
consider your ability to function outside of such highly structured settings. For these
reasons, identical paragraph C criteria are included in 12.02, 12.03, and 12.04. The
paragraph C criterion of 12.06 reflects the uniqueness of agoraphobia, an anxiety
disorder manifested by an overwhelming fear of leaving the home.
G. Effects of medication. We must give attention to the effects of medication on your
symptoms, signs, and ability to function. While drugs used to modify psychological
functions and mental states may control certain primary manifestations of a mental
disorder, e.g., hallucinations, impaired attention, restlessness, or hyperactivity, such
treatment may not affect all functional limitations imposed by the mental disorder. In
cases where overt symptomatology is attenuated by the use of such drugs, particular
attention must be focused on the functional limitations that may persist. We will consider
these functional limitations in assessing impairment severity. See the paragraph C
criteria in 12.02, 12.03, 12.04, and 12.06.
Drugs used in the treatment of some mental illnesses may cause drowsiness, blunted
affect, or other side effects involving other body systems. We will consider such side
effects when we evaluate the overall severity of your impairment. Where adverse effects
of medications contribute to the impairment severity and the impairment(s) neither
meets nor is equivalent in severity to any listing but is nonetheless severe, we will
consider such adverse effects in the RFC assessment.
H. Effects of treatment. With adequate treatment some individuals with chronic mental
disorders not only have their symptoms and signs ameliorated, but they also return to a
level of function close to the level of function they had before they developed symptoms
or signs of their mental disorders. Treatment may or may not assist in the achievement
of a level of adaptation adequate to perform sustained SGA. See the paragraph C
criteria in 12.02, 12.03, 12.04, and 12.06.
I. Technique for reviewing evidence in mental disorders claims to determine the
level of impairment severity. We have developed a special technique to ensure that
we obtain, consider, and properly evaluate all the evidence we need to evaluate
impairment severity in claims involving mental impairment(s). We explain this technique
in §§ 404.1520a and 416.920a.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-91
12.01 Category of Impairments, Mental
12.02 Organic mental disorders: Psychological or behavioral abnormalities associated
with a dysfunction of the brain. History and physical examination or laboratory tests
demonstrate the presence of a specific organic factor judged to be etiologically related
to the abnormal mental state and loss of previously acquired functional abilities.
The required level of severity for these disorders is met when the requirements in both
A and B are satisfied, or when the requirements in C are satisfied.
A. Demonstration of a loss of specific cognitive abilities or affective changes and the
medically documented persistence of at least one of the following:
1. Disorientation to time and place; or
2. Memory impairment, either short-term (inability to learn new information),
intermediate, or long-term (inability to remember information that was known sometime
in the past); or
3. Perceptual or thinking disturbances (e.g., hallucinations, delusions); or
4. Change in personality; or
5. Disturbance in mood; or
6. Emotional lability (e.g., explosive temper outbursts, sudden crying, etc.) and
impairment in impulse control; or
7. Loss of measured intellectual ability of at least 15 I.Q. points from premorbid levels or
overall impairment index clearly within the severely impaired range on
neuropsychological testing, e.g., Luria-Nebraska, Halstead-Reitan, etc;
AND
B. Resulting in at least two of the following:
1. Marked restriction of activities of daily living; or
2. Marked difficulties in maintaining social functioning; or
3. Marked difficulties in maintaining concentration, persistence, or pace; or
4. Repeated episodes of decompensation, each of extended duration;
OR
C. Medically documented history of a chronic organic mental disorder of at least 2 years'
duration that has caused more than a minimal limitation of ability to do basic work
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-92
activities, with symptoms or signs currently attenuated by medication or psychosocial
support, and one of the following:
1. Repeated episodes of decompensation, each of extended duration; or
2. A residual disease process that has resulted in such marginal adjustment that even a
minimal increase in mental demands or change in the environment would be predicted
to cause the individual to decompensate; or
3. Current history of 1 or more years' inability to function outside a highly supportive
living arrangement, with an indication of continued need for such an arrangement.
12.03 Schizophrenic, paranoid and other psychotic disorders: Characterized by the
onset of psychotic features with deterioration from a previous level of functioning.
The required level of severity for these disorders is met when the requirements in both
A and B are satisfied, or when the requirements in C are satisfied.
A. Medically documented persistence, either continuous or intermittent, of one or more
of the following:
1. Delusions or hallucinations; or
2. Catatonic or other grossly disorganized behavior; or
3. Incoherence, loosening of associations, illogical thinking, or poverty of content of
speech if associated with one of the following:
a. Blunt affect; or
b. Flat affect; or
c. Inappropriate affect;
or
4. Emotional withdrawal and/or isolation;
AND
B. Resulting in at least two of the following:
1. Marked restriction of activities of daily living; or
2. Marked difficulties in maintaining social functioning; or
3. Marked difficulties in maintaining concentration, persistence, or pace; or
4. Repeated episodes of decompensation, each of extended duration;
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-93
OR
C. Medically documented history of a chronic schizophrenic, paranoid, or other
psychotic disorder of at least 2 years' duration that has caused more than a minimal
limitation of ability to do basic work activities, with symptoms or signs currently
attenuated by medication or psychosocial support, and one of the following:
1. Repeated episodes of decompensation, each of extended duration; or
2. A residual disease process that has resulted in such marginal adjustment that even a
minimal increase in mental demands or change in the environment would be predicted
to cause the individual to decompensate; or
3. Current history of 1 or more years' inability to function outside a highly supportive
living arrangement, with an indication of continued need for such an arrangement.
12.04 Affective disorders: Characterized by a disturbance of mood, accompanied by a
full or partial manic or depressive syndrome. Mood refers to a prolonged emotion that
colors the whole psychic life; it generally involves either depression or elation.
The required level of severity for these disorders is met when the requirements in both
A and B are satisfied, or when the requirements in C are satisfied.
A. Medically documented persistence, either continuous or intermittent, of one of the
following:
1. Depressive syndrome characterized by at least four of the following:
a. Anhedonia or pervasive loss of interest in almost all activities; or
b. Appetite disturbance with change in weight; or
c. Sleep disturbance; or
d. Psychomotor agitation or retardation; or
e. Decreased energy; or
f. Feelings of guilt or worthlessness; or
g. Difficulty concentrating or thinking; or
h. Thoughts of suicide; or
i. Hallucinations, delusions, or paranoid thinking; or
2. Manic syndrome characterized by at least three of the following:
a. Hyperactivity; or
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-94
b. Pressure of speech; or
c. Flight of ideas; or
d. Inflated self-esteem; or
e. Decreased need for sleep; or
f. Easy distractibility; or
g. Involvement in activities that have a high probability of painful consequences which
are not recognized; or
h. Hallucinations, delusions or paranoid thinking; or
3. Bipolar syndrome with a history of episodic periods manifested by the full
symptomatic picture of both manic and depressive syndromes (and currently
characterized by either or both syndromes);
AND
B. Resulting in at least two of the following:
1. Marked restriction of activities of daily living; or
2. Marked difficulties in maintaining social functioning; or
3. Marked difficulties in maintaining concentration, persistence, or pace; or
4. Repeated episodes of decompensation, each of extended duration;
OR
C. Medically documented history of a chronic affective disorder of at least 2 years'
duration that has caused more than a minimal limitation of ability to do basic work
activities, with symptoms or signs currently attenuated by medication or psychosocial
support, and one of the following:
1. Repeated episodes of decompensation, each of extended duration; or
2. A residual disease process that has resulted in such marginal adjustment that even a
minimal increase in mental demands or change in the environment would be predicted
to cause the individual to decompensate; or
3. Current history of 1 or more years' inability to function outside a highly supportive
living arrangement, with an indication of continued need for such an arrangement.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-95
12.05 Mental retardation: Mental retardation refers to significantly subaverage general
intellectual functioning with deficits in adaptive functioning initially manifested during the
developmental period; i.e., the evidence demonstrates or supports onset of the
impairment before age 22.
The required level of severity for this disorder is met when the requirements in A, B, C,
or D are satisfied.
A. Mental incapacity evidenced by dependence upon others for personal needs (e.g.,
toileting, eating, dressing, or bathing) and inability to follow directions, such that the use
of standardized measures of intellectual functioning is precluded;
OR
B. A valid verbal, performance, or full scale IQ of 59 or less;
OR
C. A valid verbal, performance, or full scale IQ of 60 through 70 and a physical or other
mental impairment imposing an additional and significant work-related limitation of
function;
OR
D. A valid verbal, performance, or full scale IQ of 60 through 70, resulting in at least two
of the following:
1. Marked restriction of activities of daily living; or
2. Marked difficulties in maintaining social functioning; or
3. Marked difficulties in maintaining concentration, persistence, or pace; or
4. Repeated episodes of decompensation, each of extended duration.
12.06 Anxiety-related disorders: In these disorders anxiety is either the predominant
disturbance or it is experienced if the individual attempts to master symptoms; for
example, confronting the dreaded object or situation in a phobic disorder or resisting the
obsessions or compulsions in obsessive compulsive disorders.
The required level of severity for these disorders is met when the requirements in both
A and B are satisfied, or when the requirements in both A and C are satisfied.
A. Medically documented findings of at least one of the following:
1. Generalized persistent anxiety accompanied by three out of four of the following
signs or symptoms:
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-96
a. Motor tension; or
b. Autonomic hyperactivity; or
c. Apprehensive expectation; or
d. Vigilance and scanning; or
2. A persistent irrational fear of a specific object, activity, or situation which results in a
compelling desire to avoid the dreaded object, activity, or situation; or
3. Recurrent severe panic attacks manifested by a sudden unpredictable onset of
intense apprehension, fear, terror and sense of impending doom occurring on the
average of at least once a week; or
4. Recurrent obsessions or compulsions which are a source of marked distress; or
5. Recurrent and intrusive recollections of a traumatic experience, which are a source of
marked distress;
AND
B. Resulting in at least two of the following:
1. Marked restriction of activities of daily living; or
2. Marked difficulties in maintaining social functioning; or
3. Marked difficulties in maintaining concentration, persistence, or pace; or
4. Repeated episodes of decompensation, each of extended duration.
OR
C. Resulting in complete inability to function independently outside the area of one's
home.
12.07 Somatoform disorders: Physical symptoms for which there are no demonstrable
organic findings or known physiological mechanisms.
The required level of severity for these disorders is met when the requirements in both
A and B are satisfied.
A. Medically documented by evidence of one of the following:
1. A history of multiple physical symptoms of several years duration, beginning before
age 30, that have caused the individual to take medicine frequently, see a physician
often and alter life patterns significantly; or
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-97
2. Persistent nonorganic disturbance of one of the following:
a. Vision, or
b. Speech; or
c. Hearing; or
d. Use of a limb; or
e. Movement and its control (e.g., coordination disturbance, psychogenic seizures,
akinesia, dyskinesia; or
f. Sensation (e.g., diminished or heightened).
3. Unrealistic interpretation of physical signs or sensations associated with the
preoccupation or belief that one has a serious disease or injury;
AND
B. Resulting in at least two of the following:
1. Marked restriction of activities of daily living; or
2. Marked difficulties in maintaining social functioning; or
3. Marked difficulties in maintaining concentration, persistence, or pace; or
4. Repeated episodes of decompensation, each of extended duration.
12.08 Personality disorders: A personality disorder exists when personality traits are
inflexible and maladaptive and cause either significant impairment in social or
occupational functioning or subjective distress. Characteristic features are typical of the
individual's long-term functioning and are not limited to discrete episodes of illness.
The required level of severity for these disorders is met when the requirements in both
A and B are satisfied.
A. Deeply ingrained, maladaptive patterns of behavior associated with one of the
following:
1. Seclusiveness or autistic thinking; or
2. Pathologically inappropriate suspiciousness or hostility; or
3. Oddities of thought, perception, speech and behavior; or
4. Persistent disturbances of mood or affect; or
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-98
5. Pathological dependence, passivity, or aggressivity; or
6. Intense and unstable interpersonal relationships and impulsive and damaging
behavior;
AND
B. Resulting in at least two of the following:
1. Marked restriction of activities of daily living; or
2. Marked difficulties in maintaining social functioning; or
3. Marked difficulties in maintaining concentration, persistence, or pace; or
4. Repeated episodes of decompensation, each of extended duration.
12.09 Substance addiction disorders: Behavioral changes or physical changes
associated with the regular use of substances that affect the central nervous system.
The required level of severity for these disorders is met when the requirements in any of
the following (A through I) are satisfied.
A. Organic mental disorders. Evaluate under 12.02.
B. Depressive syndrome. Evaluate under 12.04.
C. Anxiety disorders. Evaluate under 12.06.
D. Personality disorders. Evaluate under 12.08.
E. Peripheral neuropathies. Evaluate under 11.14.
F. Liver damage. Evaluate under 5.05.
G. Gastritis. Evaluate under 5.00.
H. Pancreatitis. Evaluate under 5.08.
I. Seizures. Evaluate under 11.02 or 11.03.
12.10 Autistic disorder and other pervasive developmental disorders:
Characterized by qualitative deficits in the development of reciprocal social interaction,
in the development of verbal and nonverbal communication skills, and in imaginative
activity. Often, there is a markedly restricted repertoire of activities and interests, which
frequently are stereotyped and repetitive.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-99
The required level of severity for these disorders is met when the requirements in both
A and B are satisfied.
A. Medically documented findings of the following:
1. For autistic disorder, all of the following:
a. Qualitative deficits in reciprocal social interaction; and
b. Qualitative deficits in verbal and nonverbal communication and in imaginative activity;
and
c. Markedly restricted repertoire of activities and interests;
OR
2. For other pervasive developmental disorders, both of the following:
a. Qualitative deficits in reciprocal social interaction; and
b. Qualitative deficits in verbal and nonverbal communication and in imaginative activity;
AND
B. Resulting in at least two of the following:
1. Marked restriction of activities of daily living; or
2. Marked difficulties in maintaining social functioning; or
3. Marked difficulties in maintaining concentration, persistence, or pace; or
4. Repeated episodes of decompensation, each of extended duration.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-100
This page left intentionally blank.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-101
Appendix C – 7
Mental Cognitive Roundtable –
Excerpts from the Code of Federal Regulations (CFR)
Residual Functional Capacity
§404.1545 [and 416.945] Your residual functional capacity.
(a) General—(1) Residual functional capacity assessment. Your impairment(s), and any
related symptoms, such as pain, may cause physical and mental limitations that affect
what you can do in a work setting. Your residual functional capacity is the most you can
still do despite your limitations. We will assess your residual functional capacity based
on all the relevant evidence in your case record. (See §404.1546.)
(2) If you have more than one impairment. We will consider all of your medically
determinable impairments of which we are aware, including your medically determinable
impairments that are not "severe," as explained in §§404.1520(c), 404.1521, and
404.1523, when we assess your residual functional capacity. (See paragraph (e) of this
section.)
(3) Evidence we use to assess your residual functional capacity. We will assess your
residual functional capacity based on all of the relevant medical and other evidence. In
general, you are responsible for providing the evidence we will use to make a finding
about your residual functional capacity. (See §404.1512(c).) However, before we make
a determination that you are not disabled, we are responsible for developing your
complete medical history, including arranging for a consultative examination(s) if
necessary, and making every reasonable effort to help you get medical reports from
your own medical sources. (See §§404.1512(d) through (f).) We will consider any
statements about what you can still do that have been provided by medical sources,
whether or not they are based on formal medical examinations. (See §404.1513.) We
will also consider descriptions and observations of your limitations from your
impairment(s), including limitations that result from your symptoms, such as pain,
provided by you, your family, neighbors, friends, or other persons. (See paragraph (e) of
this section and §404.1529.)
(4) What we will consider in assessing residual functional capacity. When we assess
your residual functional capacity, we will consider your ability to meet the physical,
mental, sensory, and other requirements of work, as described in paragraphs (b), (c),
and (d) of this section.
(5) How we will use our residual functional capacity assessment. (i) We will first use our
residual functional capacity assessment at step four of the sequential evaluation
process to decide if you can do your past relevant work. (See §§404.1520(f) and
404.1560(b).)
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-102
(ii) If we find that you cannot do your past relevant work (or you do not have any past
relevant work), we will use the same assessment of your residual functional capacity at
step five of the sequential evaluation process to decide if you can make an adjustment
to any other work that exists in the national economy. (See §§404.1520(g) and
404.1566.) At this step, we will not use our assessment of your residual functional
capacity alone to decide if you are disabled. We will use the guidelines in §§404.1560
through 404.1569a, and consider our residual functional capacity assessment together
with the information about your vocational background to make our disability
determination or decision. For our rules on residual functional capacity assessment in
deciding whether your disability continues or ends, see §404.1594.
(b) Physical abilities. When we assess your physical abilities, we first assess the nature
and extent of your physical limitations and then determine your residual functional
capacity for work activity on a regular and continuing basis. A limited ability to perform
certain physical demands of work activity, such as sitting, standing, walking, lifting,
carrying, pushing, pulling, or other physical functions (including manipulative or postural
functions, such as reaching, handling, stooping or crouching), may reduce your ability to
do past work and other work.
(c) Mental abilities. When we assess your mental abilities, we first assess the nature
and extent of your mental limitations and restrictions and then determine your residual
functional capacity for work activity on a regular and continuing basis. A limited ability to
carry out certain mental activities, such as limitations in understanding, remembering,
and carrying out instructions, and in responding appropriately to supervision, co-
workers, and work pressures in a work setting, may reduce your ability to do past work
and other work.
(d) Other abilities affected by impairment(s). Some medically determinable
impairment(s), such as skin impairment(s), epilepsy, impairment(s) of vision, hearing or
other senses, and impairment(s) which impose environmental restrictions, may cause
limitations and restrictions which affect other work-related abilities. If you have this type
of impairment(s), we consider any resulting limitations and restrictions which may
reduce your ability to do past work and other work in deciding your residual functional
capacity.
(e) Total limiting effects. When you have a severe impairment(s), but your symptoms,
signs, and laboratory findings do not meet or equal those of a listed impairment in
appendix 1 of this subpart, we will consider the limiting effects of all your impairment(s),
even those that are not severe, in determining your residual functional capacity. Pain or
other symptoms may cause a limitation of function beyond that which can be
determined on the basis of the anatomical, physiological or psychological abnormalities
considered alone; e.g., someone with a low back disorder may be fully capable of the
physical demands consistent with those of sustained medium work activity, but another
person with the same disorder, because of pain, may not be capable of more than the
physical demands consistent with those of light work activity on a sustained basis. In
assessing the total limiting effects of your impairment(s) and any related symptoms, we
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-103
will consider all of the medical and nonmedical evidence, including the information
described in §404.1529(c).
Vocational Considerations
§404.1560 When we will consider your vocational background.
(a) General. If you are applying for a period of disability, or disability insurance benefits
as a disabled worker, or child's insurance benefits based on disability which began
before age 22, or widow's or widower's benefits based on disability for months after
December 1990, and we cannot decide whether you are disabled at one of the first
three steps of the sequential evaluation process (see §404.1520), we will consider your
residual functional capacity together with your vocational background, as discussed in
paragraphs (b) and (c) of this section.
(b) Past relevant work. We will first compare our assessment of your residual functional
capacity with the physical and mental demands of your past relevant work.
(1) Definition of past relevant work. Past relevant work is work that you have done within
the past 15 years, that was substantial gainful activity, and that lasted long enough for
you to learn to do it. (See §404.1565(a).)
(2) Determining whether you can do your past relevant work. We will ask you for
information about work you have done in the past. We may also ask other people who
know about your work. (See §404.1565(b).) We may use the services of vocational
experts or vocational specialists, or other resources, such as the "Dictionary of
Occupational Titles" and its companion volumes and supplements, published by the
Department of Labor, to obtain evidence we need to help us determine whether you can
do your past relevant work, given your residual functional capacity. A vocational expert
or specialist may offer relevant evidence within his or her expertise or knowledge
concerning the physical and mental demands of a claimant's past relevant work, either
as the claimant actually performed it or as generally performed in the national economy.
Such evidence may be helpful in supplementing or evaluating the accuracy of the
claimant's description of his past work. In addition, a vocational expert or specialist may
offer expert opinion testimony in response to a hypothetical question about whether a
person with the physical and mental limitations imposed by the claimant's medical
impairment(s) can meet the demands of the claimant's previous work, either as the
claimant actually performed it or as generally performed in the national economy.
(3) If you can do your past relevant work. If we find that you have the residual functional
capacity to do your past relevant work, we will determine that you can still do your past
work and are not disabled. We will not consider your vocational factors of age,
education, and work experience or whether your past relevant work exists in significant
numbers in the national economy.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-104
(c) Other work. (1) If we find that your residual functional capacity is not enough to
enable you to do any of your past relevant work, we will use the same residual
functional capacity assessment we used to decide if you could do your past relevant
work when we decide if you can adjust to any other work. We will look at your ability to
adjust to other work by considering your residual functional capacity and your vocational
factors of age, education, and work experience. Any other work (jobs) that you can
adjust to must exist in significant numbers in the national economy (either in the region
where you live or in several regions in the country).
(2) In order to support a finding that you are not disabled at this fifth step of the
sequential evaluation process, we are responsible for providing evidence that
demonstrates that other work exists in significant numbers in the national economy that
you can do, given your residual functional capacity and vocational factors. We are not
responsible for providing additional evidence about your residual functional capacity
because we will use the same residual functional capacity assessment that we used to
determine if you can do your past relevant work.
§404.1563 Your age as a vocational factor.
(a) General. "Age" means your chronological age. When we decide whether you are
disabled under §404.1520(g)(1), we will consider your chronological age in combination
with your residual functional capacity, education, and work experience. We will not
consider your ability to adjust to other work on the basis of your age alone. In
determining the extent to which age affects a person's ability to adjust to other work, we
consider advancing age to be an increasingly limiting factor in the person's ability to
make such an adjustment, as we explain in paragraphs (c) through (e) of this section. If
you are unemployed but you still have the ability to adjust to other work, we will find that
you are not disabled. In paragraphs (b) through (e) of this section and in appendix 2 to
this subpart, we explain in more detail how we consider your age as a vocational factor.
(b) How we apply the age categories. When we make a finding about your ability to do
other work under §404.1520(f)(1), we will use the age categories in paragraphs (c)
through (e) of this section. We will use each of the age categories that applies to you
during the period for which we must determine if you are disabled. We will not apply the
age categories mechanically in a borderline situation. If you are within a few days to a
few months of reaching an older age category, and using the older age category would
result in a determination or decision that you are disabled, we will consider whether to
use the older age category after evaluating the overall impact of all the factors of your
case.
(c) Younger person. If you are a younger person (under age 50), we generally do not
consider that your age will seriously affect your ability to adjust to other work. However,
in some circumstances, we consider that persons age 45-49 are more limited in their
ability to adjust to other work than persons who have not attained age 45. See Rule
201.17 in appendix 2.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-105
(d) Person closely approaching advanced age. If you are closely approaching advanced
age (age 50-54), we will consider that your age along with a severe impairment(s) and
limited work experience may seriously affect your ability to adjust to other work.
(e) Person of advanced age. We consider that at advanced age (age 55 or older) age
significantly affects a person's ability to adjust to other work. We have special rules for
persons of advanced age and for persons in this category who are closely approaching
retirement age (age 60-64). See §404.1568(d)(4).
(f) Information about your age. We will usually not ask you to prove your age. However,
if we need to know your exact age to determine whether you get disability benefits or if
the amount of your benefit will be affected, we will ask you for evidence of your age.
§404.1564 Your education as a vocational factor.
(a) General. Education is primarily used to mean formal schooling or other training
which contributes to your ability to meet vocational requirements, for example,
reasoning ability, communication skills, and arithmetical ability. However, if you do not
have formal schooling, this does not necessarily mean that you are uneducated or lack
these abilities. Past work experience and the kinds of responsibilities you had when you
were working may show that you have intellectual abilities, although you may have little
formal education. Your daily activities, hobbies, or the results of testing may also show
that you have significant intellectual ability that can be used to work.
(b) How we evaluate your education. The importance of your educational background
may depend upon how much time has passed between the completion of your formal
education and the beginning of your physical or mental impairment(s) and by what you
have done with your education in a work or other setting. Formal education that you
completed many years before your impairment began, or unused skills and knowledge
that were a part of your formal education, may no longer be useful or meaningful in
terms of your ability to work. Therefore, the numerical grade level that you completed in
school may not represent your actual educational abilities. These may be higher or
lower. However, if there is no other evidence to contradict it, we will use your numerical
grade level to determine your educational abilities. The term education also includes
how well you are able to communicate in English since this ability is often acquired or
improved by education. In evaluating your educational level, we use the following
categories:
(1) Illiteracy. Illiteracy means the inability to read or write. We consider someone
illiterate if the person cannot read or write a simple message such as instructions or
inventory lists even though the person can sign his or her name. Generally, an illiterate
person has had little or no formal schooling.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-106
(2) Marginal education. Marginal education means ability in reasoning, arithmetic, and
language skills which are needed to do simple, unskilled types of jobs. We generally
consider that formal schooling at a 6th grade level or less is a marginal education.
(3) Limited education. Limited education means ability in reasoning, arithmetic, and
language skills, but not enough to allow a person with these educational qualifications to
do most of the more complex job duties needed in semi-skilled or skilled jobs. We
generally consider that a 7th grade through the 11th grade level of formal education is a
limited education.
(4) High school education and above. High school education and above means abilities
in reasoning, arithmetic, and language skills acquired through formal schooling at a 12th
grade level or above. We generally consider that someone with these educational
abilities can do semi-skilled through skilled work.
(5) Inability to communicate in English. Since the ability to speak, read and understand
English is generally learned or increased at school, we may consider this an educational
factor. Because English is the dominant language of the country, it may be difficult for
someone who doesn't speak and understand English to do a job, regardless of the
amount of education the person may have in another language. Therefore, we consider
a person's ability to communicate in English when we evaluate what work, if any, he or
she can do. It generally doesn't matter what other language a person may be fluent in.
(6) Information about your education. We will ask you how long you attended school
and whether you are able to speak, understand, read and write in English and do at
least simple calculations in arithmetic. We will also consider other information about
how much formal or informal education you may have had through your previous work,
community projects, hobbies, and any other activities which might help you to work.
§404.1565 Your work experience as a vocational factor.
(a) General. Work experience means skills and abilities you have acquired through work
you have done which show the type of work you may be expected to do. Work you have
already been able to do shows the kind of work that you may be expected to do. We
consider that your work experience applies when it was done within the last 15 years,
lasted long enough for you to learn to do it, and was substantial gainful activity. We do
not usually consider that work you did 15 years or more before the time we are deciding
whether you are disabled (or when the disability insured status requirement was last
met, if earlier) applies. A gradual change occurs in most jobs so that after 15 years it is
no longer realistic to expect that skills and abilities acquired in a job done then continue
to apply. The 15-year guide is intended to insure that remote work experience is not
currently applied. If you have no work experience or worked only "off-and-on" or for brief
periods of time during the 15-year period, we generally consider that these do not apply.
If you have acquired skills through your past work, we consider you to have these work
skills unless you cannot use them in other skilled or semi-skilled work that you can now
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-107
do. If you cannot use your skills in other skilled or semi-skilled work, we will consider
your work background the same as unskilled. However, even if you have no work
experience, we may consider that you are able to do unskilled work because it requires
little or no judgment and can be learned in a short period of time.
(b) Information about your work. Under certain circumstances, we will ask you about the
work you have done in the past. If you cannot give us all of the information we need, we
will try, with your permission, to get it from your employer or other person who knows
about your work, such as a member of your family or a co-worker. When we need to
consider your work experience to decide whether you are able to do work that is
different from what you have done in the past, we will ask you to tell us about all of the
jobs you have had in the last 15 years. You must tell us the dates you worked, all of the
duties you did, and any tools, machinery, and equipment you used. We will need to
know about the amount of walking, standing, sitting, lifting and carrying you did during
the work day, as well as any other physical or mental duties of your job. If all of your
work in the past 15 years has been arduous and unskilled, and you have very little
education, we will ask you to tell us about all of your work from the time you first began
working. This information could help you to get disability benefits.
§404.1566 Work which exists in the national economy.
(a) General. We consider that work exists in the national economy when it exists in
significant numbers either in the region where you live or in several other regions of the
country. It does not matter whether—
(1) Work exists in the immediate area in which you live;
(2) A specific job vacancy exists for you; or
(3) You would be hired if you applied for work.
(b) How we determine the existence of work. Work exists in the national economy when
there is a significant number of jobs (in one or more occupations) having requirements
which you are able to meet with your physical or mental abilities and vocational
qualifications. Isolated jobs that exist only in very limited numbers in relatively few
locations outside of the region where you live are not considered "work which exists in
the national economy". We will not deny you disability benefits on the basis of the
existence of these kinds of jobs. If work that you can do does not exist in the national
economy, we will determine that you are disabled. However, if work that you can do
does exist in the national economy, we will determine that you are not disabled.
(c) Inability to obtain work. We will determine that you are not disabled if your residual
functional capacity and vocational abilities make it possible for you to do work which
exists in the national economy, but you remain unemployed because of—
(1) Your inability to get work;
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-108
(2) Lack of work in your local area;
(3) The hiring practices of employers;
(4) Technological changes in the industry in which you have worked;
(5) Cyclical economic conditions;
(6) No job openings for you;
(7) You would not actually be hired to do work you could otherwise do; or
(8) You do not wish to do a particular type of work.
(d) Administrative notice of job data. When we determine that unskilled, sedentary, light,
and medium jobs exist in the national economy (in significant numbers either in the
region where you live or in several regions of the country), we will take administrative
notice of reliable job information available from various governmental and other
publications. For example, we will take notice of—
(1) Dictionary of Occupational Titles, published by the Department of Labor;
(2) County Business Patterns, published by the Bureau of the Census;
(3) Census Reports, also published by the Bureau of the Census;
(4) Occupational Analyses, prepared for the Social Security Administration by various
State employment agencies; and
(5) Occupational Outlook Handbook, published by the Bureau of Labor Statistics.
(e) Use of vocational experts and other specialists. If the issue in determining whether
you are disabled is whether your work skills can be used in other work and the specific
occupations in which they can be used, or there is a similarly complex issue, we may
use the services of a vocational expert or other specialist. We will decide whether to use
a vocational expert or other specialist.
§404.1568 Skill requirements.
In order to evaluate your skills and to help determine the existence in the national
economy of work you are able to do, occupations are classified as unskilled, semi-
skilled, and skilled. In classifying these occupations, we use materials published by the
Department of Labor. When we make disability determinations under this subpart, we
use the following definitions:
(a) Unskilled work. Unskilled work is work which needs little or no judgment to do simple
duties that can be learned on the job in a short period of time. The job may or may not
require considerable strength. For example, we consider jobs unskilled if the primary
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-109
work duties are handling, feeding and offbearing (that is, placing or removing materials
from machines which are automatic or operated by others), or machine tending, and a
person can usually learn to do the job in 30 days, and little specific vocational
preparation and judgment are needed. A person does not gain work skills by doing
unskilled jobs.
(b) Semi-skilled work. Semi-skilled work is work which needs some skills but does not
require doing the more complex work duties. Semi-skilled jobs may require alertness
and close attention to watching machine processes; or inspecting, testing or otherwise
looking for irregularities; or tending or guarding equipment, property, materials, or
persons against loss, damage or injury; or other types of activities which are similarly
less complex than skilled work, but more complex than unskilled work. A job may be
classified as semi-skilled where coordination and dexterity are necessary, as when
hands or feet must be moved quickly to do repetitive tasks.
(c) Skilled work. Skilled work requires qualifications in which a person uses judgment to
determine the machine and manual operations to be performed in order to obtain the
proper form, quality, or quantity of material to be produced. Skilled work may require
laying out work, estimating quality, determining the suitability and needed quantities of
materials, making precise measurements, reading blueprints or other specifications, or
making necessary computations or mechanical adjustments to control or regulate the
work. Other skilled jobs may require dealing with people, facts, or figures or abstract
ideas at a high level of complexity.
(d) Skills that can be used in other work (transferability)—(1) What we mean by
transferable skills. We consider you to have skills that can be used in other jobs, when
the skilled or semi-skilled work activities you did in past work can be used to meet the
requirements of skilled or semi-skilled work activities of other jobs or kinds of work. This
depends largely on the similarity of occupationally significant work activities among
different jobs.
(2) How we determine skills that can be transferred to other jobs. Transferability is most
probable and meaningful among jobs in which—
(i) The same or a lesser degree of skill is required;
(ii) The same or similar tools and machines are used; and
(iii) The same or similar raw materials, products, processes, or services are involved.
(3) Degrees of transferability. There are degrees of transferability of skills ranging from
very close similarities to remote and incidental similarities among jobs. A complete
similarity of all three factors is not necessary for transferability. However, when skills are
so specialized or have been acquired in such an isolated vocational setting (like many
jobs in mining, agriculture, or fishing) that they are not readily usable in other industries,
jobs, and work settings, we consider that they are not transferable.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-110
(4) Transferability of skills for individuals of advanced age. If you are of advanced age
(age 55 or older), and you have a severe impairment(s) that limits you to sedentary or
light work, we will find that you cannot make an adjustment to other work unless you
have skills that you can transfer to other skilled or semiskilled work (or you have
recently completed education which provides for direct entry into skilled work) that you
can do despite your impairment(s). We will decide if you have transferable skills as
follows. If you are of advanced age and you have a severe impairment(s) that limits you
to no more than sedentary work, we will find that you have skills that are transferable to
skilled or semiskilled sedentary work only if the sedentary work is so similar to your
previous work that you would need to make very little, if any, vocational adjustment in
terms of tools, work processes, work settings, or the industry. (See §404.1567(a) and
§201.00(f) of appendix 2.) If you are of advanced age but have not attained age 60, and
you have a severe impairment(s) that limits you to no more than light work, we will apply
the rules in paragraphs (d)(1) through (d)(3) of this section to decide if you have skills
that are transferable to skilled or semiskilled light work (see §404.1567(b)). If you are
closely approaching retirement age (age 60-64) and you have a severe impairment(s)
that limits you to no more than light work, we will find that you have skills that are
transferable to skilled or semiskilled light work only if the light work is so similar to your
previous work that you would need to make very little, if any, vocational adjustment in
terms of tools, work processes, work settings, or the industry. (See §404.1567(b) and
Rule 202.00(f) of appendix 2 to this subpart.)
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-111
Appendix C – 8
Mental Cognitive Roundtable – Agency Instructions
for Completing the Mental Residual Functional Capacity Assessment (MRFC)
Relevant Program Operating Manual System (POMS) Instructions for
Completion of the Mental Residual Functional Assessment Form
DI 24510.060 Mental Residual Functional Capacity Assessment
A. Operating Policy
1. SPECIAL FORM
Because of the complexity of mental disorder evaluation, a special Form
SSA-4734-F4-SUP is to be used to document the mental residual functional capacity
(RFC) decision, i.e., what an individual can do despite his /her impairment.
2. MEDICAL CONSULTANT COMPLETION
a. Unfavorable and Partially Favorable Decisions
In decisions that are not fully favorable, only a psychiatrist or psychologist is to perform
the analysis and decide the mental functional capacity.
b. Fully Favorable Decisions
In fully favorable determinations, the medical consultant (MC) who completes the
mental RFC assessment, to the extent possible, should be a psychiatrist or
psychologist.
c. When Physical Impairment Involved
Refer the claim to a physician of the appropriate medical specialty after all mental RFC
considerations have been accomplished.
B. Description of Form SSA-4734-F4-SUP
Form SSA-4734-F4-SUP is divided into four sections:
Heading,
Section I, Summary Conclusions,
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-112
Section II, Remarks,
Section III, Functional Capacity Assessment and MC signature.
1. HEADING
The Heading provides space to record claimant and claim identification data.
2. SECTION I
Section I—Summary Conclusions is designed to record the MC's analysis of the
evidence and his/her conclusions about:
The presence and degree of specific functional limitations, and the adequacy
of documentation.
a. Section I is merely a worksheet to aid in deciding the presence and
degree of functional limitations and the adequacy of documentation
and does not constitute the RFC assessment.
b. Twenty mental function items are grouped under four main
categories:
Understanding and Memory,
Sustained Concentration and Persistence,
Social Interaction, and
Adaptation
c. To the right of each of the items is a series of decision
checkblocks under the headings:
Not Significantly Limited
Moderately Limited
Markedly Limited
No Evidence of Limitation in This Category, and
Not Ratable on Available Evidence
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-113
3. SECTION II
Section II – Remarks provides for discussion of evidence needed to rate particular
items in section I.
4. SECTION III
a. Section III—Functional Capacity Assessment is for recording the mental RFC
determination. It is in this section that the actual mental RFC assessment is
recorded, explaining the conclusions indicated in section I, in terms of the extent
to which these mental capacities or functions could or could not be performed in
work settings.
b. The discussion of all mental capacities and limitations in this section must be in
narrative format.
The MC must also include any other information that he/she believes is
necessary to present a complete picture of mental RFC.
c. The Narrative must not present estimates of capacities for mental functions that
could not be rated because of insufficient evidence. Such would represent
speculation.
d. The completed SSA-4734-F4-SUP must be signed by the MC who conducted the
analysis and prepared the mental RFC assessment.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-114
DI 24510.061 Summary Conclusions and Narrative Statement of Mental RFC
A. Introduction
To assure a comprehensive assessment of mental RFC, the SSA-4734-F4-SUP
requires the MC first to record preliminary conclusions about the effect of the
impairment(s) on each of four general areas of mental function (described in B.1-4
below), then to prepare a narrative statement of mental RFC.
B. Operating Policy
The MC is to analyze each of the mental activities within the following four general
mental functional areas and to indicate on the SSA-4734-F4-SUP:
Whether the evidence is sufficient to permit assessment or, if not, the evidence
needed.
The extent to which the individual can still perform and sustain specific mental
activities and mental functions.
1. UNDERSTANDING AND MEMORY
a. Understanding and memory can be evaluated through evidence from the
mental status examination(s) or from elements of standardized psychological
tests (such as IQ tests) that assess the ability to understand and remember, as
well as evidence available from other medical and nonmedical sources, e.g.,
reports of prior work attempts or work evaluations.
b. The ability to understand and remember may be at least partially assessed
through answers to some of the following questions:
o Is the individual able to complete forms, respond to two or three-step
instructions for filling out applications, or follow instructions given by
someone?
o Did the individual have difficulty in the process of filing for disability, going
for examinations, or remembering appointments?
o Is there any history of work or school failures due to inability to
remember and understand?
o Was the individual involved in special education or training programs?
(These might indicate some impairment of the ability to understand and
remember.)
o Is there any evidence that the claimant requires supervision or
assistance to perform activities of daily living because of problems with
understanding or remembering?

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-115
o Did the individual come to appointments without supervision, finding
his/her own way without unusual supervision?
2. SUSTAINED CONCENTRATION AND PERSISTENCE
a. The individual's ability to sustain ongoing mental performance for a full workday
is essential. These may be evaluated through:
o Medical history and reports, and
o Reports of performance at past work, recent work attempts, recreational or
volunteer activities, or vocational evaluations.
b. Limitations in these areas may be demonstrated in typically less demanding
settings, such as sheltered work, vocational training, or school (i.e., in any
situation demanding performance of tasks requiring concentration or task
persistence).
c. Use care in inferring an individual's ability to sustain the mental demands of
work in a competitive setting from his/her performance in a less demanding
setting, such as sheltered work.
NOTE: Discussion with the disability examiner of the performance required in
competitive work environments may clarify this distinction.
3. SOCIAL INTERACTION
The items in this subsection deal with socially acceptable behavior and the individual's
capacity to relate to others in a work setting. To assess these factors, important
considerations are:
Historical information about interpersonal interactions with others, particularly in
an employment or work-like setting.
Indications, on mental status examinations or psychological testing, of
withdrawal, bizarre or unusual behavior, emotional lability, paranoid ideas, or
faulty insight and judgment.
Observed behavior, in terms of how the individual relates to various interviewers
or behaves when exposed to a stressful circumstance or situation.
4. ADAPTATION
Adaptive functions reflect the individual's ability to integrate other areas of functioning.
a. The items in this section pertain to the individual's ability to:
o plan,
o respond to changes,

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-116
o deal appropriately with mental demands (stress),
o avoid hazards and maintain safe behavior,
o follow rules,
o adhere to schedules and to time constraints, and
o travel.
b. The area of mental demands of work(“stress”) is difficult to assess. Some
mentally impaired individuals may be unusually sensitive to changes in their
environment and may become anxious, depressed, confused, or even psychotic
when confronted with seemingly slight mental demands.
“Stress” is a highly individualized phenomenon and can only be assessed
with regard to each individual's experiences and limitations. Even work
activities usually considered to entail low stress may produce adverse responses
in some individuals.
c. Data in the medical file may demonstrate sensitivity to change, e.g.,
resistance to try a new activity, treatment or medication, or exacerbation of
symptoms when a therapist leaves, changes schedule, or goes on vacation.
d. Most health care settings have rules, schedules, and hazards. Limitations in
conforming to acceptable behavior may sometimes emerge in the reports from
hospital, or clinics.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-117
DI 24510.063 Completion of Section I of SSA-4734-F4-SUP
A. Operating Policy
For each of the items under the four headings, A through D, one of the five boxes to
the right of each item must be checked.
B. Operating Procedure
Complete Section I by checking the appropriate boxes.
1. CHECK BOX 1
“Not Significantly Limited,” when the effects of the mental disorder do not prevent
the individual from consistently and usefully performing the activity.
2. CHECK BOX 2
“Moderately Limited,” when the evidence supports the conclusion that the individual's
capacity to perform the activity is impaired.
NOTE: The degree and extent of the capacity or limitation must be described in
narrative format in Section III.
3. CHECK BOX 3
“Markedly Limited,” when the evidence supports the conclusion that the individual
cannot usefully perform or sustain the activity.
4. CHECK BOX 4
When there is no allegation of limitation of this activity, or the medical evidence
does not indicate limitations in a particular area and no limitation would be expected,
based on the nature of the illness and the rater's clinical experience.
5. CHECK BOX 5
When there is insufficient evidence and either a problem in this aspect of work
function has been alleged, the evidence suggests a problem, or the MC's clinical
judgment suggests the likelihood of a problem.
NOTE: Absence of a rating (i.e., checking blocks 1, 2, or 3) for one or more items in a
subsection in section I does not automatically preclude a narrative RFC statement for
that subsection. Other items in the subsection may be ratable and may indicate such a
level of functional loss that the disability examiner can conclude that the individual's
capacity for work is severely compromised, in spite of the absence of a rating for other
items.
Discussion with the disability examiner will resolve whether additional information about a
subsection is necessary for a useful assessment of mental RFC.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-118
DI 24510.064 Completion of Section II of SSA-4734-F4-SUP - Remarks
A. Introduction
This section is for the identification of any deficiencies of evidence, the type of
evidence needed, and any recommendations of the source(s) from which the evidence
is to be obtained.
B. Operating Procedure
1. BOX 5 IS CHECKED
a. When box 5 is checked for several items within a subsection, consider the
possibility that the record is inadequate to permit an RFC statement for that
subsection.
b. When this is the case, do not write a functional assessment for that
subsection in section III. Instead, write a rationale in section II , explaining why
the narrative assessment is missing for that subsection.
2. ADDITIONAL MEDICAL DEVELOPMENT
a. Current evidence is insufficient.
When the evidence in file is insufficient to permit the MC to make
assessments of critical mental functional capacities, the MC will record the
medical development to be undertaken in section II of the SSA-4734-F4-SUP.
NOTE: In addition to permitting new judgments on items that were not initially
ratable, the new evidence may cause the MC to reconsider judgments on
other items.
b. Additional evidence Obtained.
o When additional medical evidence is obtained, a new SSA-4734-F4-
SUP must be prepared to replace the preliminary SSA-4734-F4-SUP.
o The new, signed SSA-4734-F4-SUP is to be filed on the left side of the
folder.
o Clearly mark the preliminary SSA-4734-F4-SUP “PRELIMINARY ONLY”
on the first page, then file on the right side of the folder.
o Do not file preliminary SSA-4734-F4-SUP's on the left side of the folder.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-119
DI 24510.065 Section III of SSA-4734-F4-SUP - Functional Capacity Assessment
A. INTRODUCTION
Section III is for recording the formal narrative mental RFC assessment and provides
for the MC to prepare a narrative statement for each of the subsections (A through D)
in section I.
B. OPERATING PROCEDURE
In preparing the formal narrative statement, the MC is to address each of the four
mental categories (Understanding and Memory, Concentration and Persistence, Social
Interaction, and Adaptation) by:
Identifying each mental category in turn; and
Providing a narrative discussion of the individual's capacities and limitations.
1. Writing the Narrative Statement
a. Identify the subsection (e.g., Understanding and Memory), then discuss the
functions that the individual has demonstrated that he/she can do, as well as
any limitations of those functions.
o Describe, in detail, the mental capacities, limitations, and any other
information that is important in the comprehensive expression of mental
RFC.
o Indicate the extent to which the individual could be expected to perform
and sustain the activity.
o Include any additional information or consideration that is necessary to
give a clear description of the individual's mental functional capacity.
Examples:
o The claimant can understand, remember, and carry out a two-step
command involving simple instructions.
o The claimant can understand complex instructions but can only recall at a
span of two-step commands. The claimant, therefore, would be limited to
this span.
o The claimant can understand and remember a four-step command, but
the disruption of executive functions is such that he can carry out only a
single step before confusing the order.
b. Record conclusions of functional capacity provided by examining physicians
that are appropriate and consistent with the documented medical and

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-120
nonmedical evidence, along with the supporting findings. (See DI
24510.030C(III).)
c. Confine discussion to the effects of the impairment(s) on function.
d. Include no severity ratings or nonspecific qualifying terms (e.g., moderate,
moderately severe) to describe limitations. Such terms do not describe function
and do not usefully convey the extent of capacity limitation.
e. Offer no opinion as to whether the individual is disabled or whether the
individual can or might perform or qualify for levels of work (e.g., unskilled) or
specific jobs (e.g., truck driver).
2. Signature and Date
a. After completing the narrative statement in section III, sign and date the SSA-
4734-F4-SUP in the spaces provided.
b. The MC's name is to be typed or stamped below the signature.
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-121
Appendix C – 9
Mental Cognitive Roundtable –
Mental Residual Functional Capacity Assessment Form

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-122

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-123

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-124

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-125
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-126
This page is intentionally blank.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-127
Appendix D
First Mental Cognitive Subcommittee Presentation
Cognitive Asessment for the
Determination of Mental
Residual Functional Capacity
David J. Schretlen, PhD
OIDAP Meeting
April 29, 2009
Abstract/
Hypothetical
Specific/
Observable/Verifiable
Use Swiss-
hole
micrometer
to adjust
drill press
Use
Swiss-
hole
micrometer
to
adjust
bottling
machine
Carry heavy
Objects
(51-100lbs.)
by hand for
< 50 feet
Hand-
Held
Tools
Carry
bricks
and mortar
to masons
on
scaffolding
using hod
Sit for
long
periods
Use tape
measure
to
measure
lumber
to be
milled
Mechanical
Activities
Things
Carry
Lift
Physical
What is
923 / 27
?
What is
103 / 12
?
< 10
lbs
Managing
Emotions
“Turn the
other
cheek”
if
provoked
at work?
Data People
“Can you…”
“Does the job require you to…”
Use displays,
gauges, meters,
measuring
instruments
Physical and
Mechanical
Activities
Use sight
and visual
information
Getting
Information
Workers directly
involved in
machine
operations
Communicating
With People
Inside the
Organization
Delegate
job activities
to clerical
workers
Mathe-
matical
Reasoning
Dynamic
Strength
Organizing,
Planning,
Prioritizing
Addition
10
lbs
20
lbs
50
lbs
100
lbs
Division
Perceiving
Emotions
Justify
taking
revenge if
you were
strongly
slighted?
See small
details of
close
objects
Unload
70 pound
bags of
salt and
empty into
water
treatment
system
Visually
inspect
newly cut
diamonds
for flaws
without
magnifica-
tion aids
Mental/
Cognitive
Interpersonal/
Temperaments
Color
Discrimi-
nation
Written
Compre-
hension
Emotional
Intelli-
gence
Person-Side Job-Side
1
2
3
4
5
3 digit
by 2 digit
w/
remainder
2 digit
by 1digit,
no
remainder
Repeat-
edly
Occasion-
ally
Physical
Demands
Level
Use
Other
Senses

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-128
Abstract/
Hypothetical
Specific/
Observable/Verifiable
Use Swiss-
hole
micrometer
to adjust
drill press
Use
Swiss-
hole
micrometer
to
adjust
bottling
machine
Carry heavy
Objects
(51-100lbs.)
by hand for
< 50 feet
Hand-
Held
Tools
Carry
bricks
and mortar
to masons
on
scaffolding
using hod
Sit for
long
periods
Use tape
measure
to
measure
lumber
to be
milled
Mechanical
Activities
Things
Carry
Lift
Physical
What is
923 / 27
?
What is
103 / 12
?
< 10
lbs
Managing
Emotions
“Turn the
other
cheek”
if
provoked
at work?
Data People
“Can you…”
“Does the job require you to…”
Use displays,
gauges, meters,
measuring
instruments
Physical and
Mechanical
Activities
Use sight
and visual
information
Getting
Information
Workers directly
involved in
machine
operations
Communicating
With People
Inside the
Organization
Delegate
job activities
to clerical
workers
Mathe-
matical
Reasoning
Dynamic
Strength
Organizing,
Planning,
Prioritizing
Addition
10
lbs
20
lbs
50
lbs
100
lbs
Division
Perceiving
Emotions
Justify
taking
revenge if
you were
strongly
slighted?
See small
details of
close
objects
Unload
70 pound
bags of
salt and
empty into
water
treatment
system
Visually
inspect
newly cut
diamonds
for flaws
without
magnifica-
tion aids
Mental/
Cognitive
Interpersonal/
Temperaments
Color
Discrimi-
nation
Written
Compre-
hension
Emotional
Intelli-
gence
Person-Side Job-Side
1
2
3
4
5
3 digit
by 2 digit
w/
remainder
2 digit
by 1digit,
no
remainder
Repeat-
edly
Occasion-
ally
Physical
Demands
Level
Use
Other
Senses

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-129
Mental/Cognitive
• Individual differences in cognitive test performance predict
occupational attainment in healthy and clinical populations
• Often predicts work outcome better than primary symptom
severity (eg, TBI, MS, Schizophrenia, etc.)
• This makes cognitive function a “final common pathway” of
work disability in many diseases and conditions
• Thus, it is essential to include cognition in mental RFC
• Two ways to approach this
– Performance-based measures (IQ, memory, attention testing)
– Ratings (self- or informant-repot)
We must first decide what
abilities to assess before we
decide how to assess them
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-130
Clinical approach: A view from the
the perspective of what goes wrong
Domain affected Disease/condition Manifestation
Intelligence Fragile X Intellectual disability
Language Stroke Aphasia
Attention Traumatic brain injury Distractibility/ADD
Learning/memory Korsakoff Amnesia
Processing speed Parkinson Bradyphrenia/bradykinesia
Visual-spatial abilities Lewy body Agnosia
Executive functioning Schizophrenia Dysexecutive & abulia
Arithmetical abilities Developmental Acalculia
Skilled movement Brain tumor Apraxia
Wakefulness Narcolepsy Drowsiness
Psychometric approach: A view from the
perspective of factor analyses
• EFA (exploratory factor analysis) is used to elucidate an
underlying factor structure
• CFA (confirmatory factor analysis) is used to test a priori
hypotheses
– Based on a conceptual model or previous findings
– Evaluate a model and compare it to specific alternatives
– Test how well hypothesized models fit the observed data
• Compare “nested” models (in which some models combine factors from
preceding ones)

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-131
FACTOR ANALYSES
CFA: Confirmatory Factor Analysis, EFA: Exploratory factor analysis, BCPA: block principal component analysis, RCA: Reliable
Components Analysis, PCA: Prin Components Analysis; SCFA: Single Confirmatory Factor Analysis, PAF: Prin Axis Factoring
HEALTHY SAMPLES Sample / Tests in Domain Analysis # Vars # Factors
Gomez et al., 2006
521 Spanish-speaking Normal Control EFA 27 6
1. Attentional-executive category formation test, visual search, semantic verbal fluency, phonological verbal fluency, design fluency
2. Contextual-exec memory LMI, LMD, Verbal paired associates Immediate, & Delayed, motor functions
3. Verbal memory word list encoding, free recall, cued recall, recognition
4. Sustained attention time orientation, digit detection, mental control, faces immediate, faces delayed recall
5. Atten - working memory digit span forward, & backward, spatial span forward, & backward
6. Orientation place orientation, person orientation
Tulsky et al., 2003
1,250 Normal Control (healthy adults aged 16 - 89) CFA 26 6
1. Verbal comprehension Vocabulary, Information, Similarities, Comprehension (Verbal Comp of WAIS-III)
2. Perceptual organization Matrix Reasoning, Block Design, Picture Completion (WAIS-III) Picture Arrangement (WMS-III)
3. Auditory memory Logical Mem I, Logical Mem II, Verbal Paired I, Verbal Paired II, Word List I, Word List II
4. Visual memory Faces I, Faces II, Family Picture I, Family Pictures II, Visual Reproduction I, Visual Reproduction II
5. Working memory Letter Number Sequencing, Digit Span, Arithmetic, Spatial Span
6. Processing speed Symbol Search, Digit Symbol
Rowe et al., 2007
1,316 Normal Controls (mean age = 33, range 6-16) PCA 19 7
1. Info processing & speed Verbal Interference Test Part I, and II, Switching of Attention Test Parts I, and II, Choice Reaction Time test
2. Verbal memory Verbal Learning and Recall Test: delayed, recognition, immediate recall
3. Viligance/sustained atten CPT Reaction Time, CPT Errors
4. Working memory Digit Span forward, Digit Span backward, Span of Visual Memory Test
5. Sensori-motor function average pause between taps on tapping test for dominant and non-dominant hands
6. Verbal processing Letter Fluency, Category Fluency
7. Executive function Maze complettion time, Maze overrun errors, Span of Visual Memory Test
Salthouse, 1998
Three healthy groups: children (age 5-17) n = 3,155 ; college students (age 18-22) n = 735; nonstudents (age 18-94) n = 1580
1. General higher-order factor
concept formation, calculation, app probs, science, social studies, humanities, incomplete words, visual closure, sound blending,
memory for names, Visual-Auditory learning, memory for sentances, memory for words, visual matching, cross out SCFA 16 1
Colom et al., 2009
1. g (General Intelligence) Adv Progressive Matrices (APM), Induct reason (PMA-R), abs reason (DAT-AR), vocab (PMA-V), verbal reason (DAT-VR)
1. Gf (fluid intelligence) Advanced Progressive Matrices (APM), Inductive reasoning subtest (PMA-R), abstract reasoning (DAT-AR)
2. Gc (crystallized intelligence) vocabulary (PMA-V), verbal reasoning (DAT-VR), numerical reasoning (DAT-NR)
3. Gv (verbal intelligence) Solid Figures, mental rotation (PMA-S), spatial relations (DAT-SR)
Visser et al., 2006
200 Normal Controls (age range = 17-66, M = 22.7 (6.1))
1. g (General intelligence) Nec Arith Operations, Diagramming Relationships, Opposites, Paper Folding, Social Translations, Vocab, Map Planning, PAF 15 1
Subtraction and Multiplication, Consistency, Cartoon Predictions, Stork Stand, Mark Making, Tonal Accuracy
MIXED/MULTIPLE GRPS
Dickinson et al., 2004
97 Schizophrenia & 87 Normal Conrols
1. Common Factor Vocab, Sim, Info, PC, BD, MR, LNS, Spatial Span, DSym, Sym Search, LM I, LM II, VP I, VP II, Fac Rec I, II, Famly Pict I, II SCFA 18 1
Dickinson et al., 2006
157 Normal Control CFA 17 6
148 Schizophrenia CFA 17 6
1. Verbal comprehension Vocab (WAIS-R), Visual Naming (MAE)
2. Perceptual organization Block Design (WAIS-R), Line Orientation (Benton)
3. Verbal learning/memory Trials 1-5 & Delayed Free Recall (CVLT), Logical Mem immediate & delayed (WMS-R)
4. Visual learning/memory Figural Memory immediate & delayed (WMS-R)
5. Info processing speed Symbol Cancellation Test, Trls A, Animal Naming (BDAE)
6. Exec/Working memory Digit Span (WAIS-R), Trls B, Categories & Persev. Erros (WCST)
Genderson et al., 2007
125 NC (-5 due to kurtosis) CFA* 21 7
162 probands (-5 due to kurtosis) CFA* 21 7
94 SZ (-5 due to kurtosis) CFA* 21 7
382 full sample (-15 due to kurtosis) CFA* 21 7
1. Speed Trls A, Trls B, Let. Fluency, Cat. Fluency
2. Target detection CPT distraction, CPT viligance, Zero-back
3. N back updating/ exec One Back, Two Back, Three Back
4. Verbal episodic memory CVLT Trails 1-5, WM Log Memory, WM Pair Assoc I, Pair Assoc II
5. Visual processing/memory WM Visual Reprod I, Visual Reprod II, Benton Line,
6. WCST executive function WCST Persev Errors, WCST Categories
7. Digit span WMSR Forward, WMSR Backward

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-132
Gladsjo et al., 2004
209 Psychotic Disorder CFA 21 6
131 Normal Control CFA 21 6
1. Verbal crystalized WAIS-R Vocab, Info, Similarities; Boston Naming
2. Attention/working mem WAIS-R Arith, Digit Span
3. Verbal episodic CVLT Monday Total, Story Learning, CVLT Long-Deay Free Recall
4. Speed of info processing WAIS-R Digit Symbol, Trls A, Trls B, GPB, Digit Viligance, Let. Fluency
5. Visual episodic Figure Learning, Figure Delay
6. Reasoning/problem solving Block Design, Category, WCST
Johnson et al., 2009
191 Normal Controls ( mean age = 75) CFA 12 4
115 autopsy confirmed AD (mean age = 80) CFA 12 4
1. General (all measures) ** all of the tests are included in this factor
2. Verbal memory Information, Paired Associates Learning, BNT, Logical Memory
3. Visuospatial BVRT (Benton Visual Rec. Test), Digit Symbol, Trls A, Block Design
4. Working memory Word Fluency, Mental Control, Digit Span Backward, Digit Span Forward
Schretlen et al., 2009
340 Normal Control CFA 15 6
126 Bipolar Disorder CFA 15 6
110 Schizophrenia CFA 15 6
1. Attention BTA-L, BTA-N, CPT-II
2. Speed TMT-A, TMT-B, GPT
3. Fluency Letter, Category, Design
4. Visual memory BVMT 1-3, BVMT Del
5. Verbal memory HVLT 1-3, HVLT Del
6. Executive function WCST Cat, WCST Err
Siedlecki et al., 2008
322 Normal Control CFA 15 5
878 Questionable Dementia CFA 15 5
639 Alzheimer Disease CFA 15 5
1. Processing speed Shape Time (shapes) and TMX Time (letters) of Cancellation Task
2. Memory SRT (Selective Reminding Task) Total Recall, Delayed Recall, Delayed Recog, BVRT (Benton Visual) Recog
3. Language Naming (BNT), Repitition, Comprehension, Letter Fluency, Category Fluency
4. Reasoning visual/spatial WAIS Similarities, Identities/Oddities (MDRS), Rosen (drawing test), BVRT Matching (Benton Visual)
5. Attention TMX Omits (Letters)& Shape Omits of Cancellation Test,
CLINICAL SAMPLES
Frazier et al., 2004
1,364 mixed patient sample RCA 21 4
1. Memory WMS-III Auditory Immediate, Visual Immediate, Auditory Delayed, Visual Delayed, Auditory Recognition
2. Visual motor Trls A, Trls B, WAIS-III PSI, WAIS-III POI, Finger Tapping Dominant, Finger Tapping Non-Dominant, GBP Dom, GPB Ndom
3. Language WAIS-III VCI, WAIS-III POI, WRAT-3 Reading, BNT, Verbal Fluency
4. Executive WCST Perseverative Errors, WCST Categories
Friis et al., 2002
219 Schizophrenia EFA 17 5
1. Working memory
Controlled Oral Word Association Task (COWA), Digit Span w/distractor, Digit Span w/out distractor (Digit Span
Distractability Test), CPT hits
2. Executive function WCST Categories, WCST Perseverative Responses, WCST # attempts to first category
3. Verbal learning CVLT immediate recall, CVLT delayed free recall, CVLT errors
4. Impulsivity CPT false alarms (comissions), CPT Reation Time
5. Motor speed Finger Tapping
Jaeger et al., 2003
156 Schizophrenia BPCA 44 6
1. Attention Concen Endurance (Letters -Errors), Stroop-Words, Stroop-Colors, Trls A, WMS-R Visual Mem, WAIS-R Digit Symbol
2. Working memory
Concentration Endurance Test (Fluctuation), WAIS-R DS Forward, Letter Number Span # Correct, Longest, WAIS-R Arith,
WAIS-R DS Backward, LMI
3. Ideational fluency + WCST persev. Ruff Fugural Fluency- Unique Designs, COWAT, Animal Naming, WCST Per Errors
4. Learning WMS-R LM I, LM II, WMS-R Verbal Paired I, Verbal Paired II, WMS-R VR I, VR II, WMS-R Visual Paired I, Visual Paired II
5. Verbal knowledge WAIS-R Vocab, Info, Comp, Similarities
6. Non-Verbal function WMS-R VR I, VR II, WAIS-R Block Design, Object Assembly, Pict Comp, Pict Arrangement

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-133
Czobor et al., 2007
185 Schizophrenia, 65 Schizoaffective EFA 29 6
155 Bipolar Disorder EFA, CFA 29 6
1. Attention Concentration Endurance Test (Letters -Errors), Stroop-Words, Stroop-Colors, Trls A, WAIS-R Digit Symbol
2. Working memory Concen Endurance (Fluctuation), WMS-R DS Forward, Letter Number Span , WAIS-R Arith, WAIS-R DS Backward, LMI
3. Ideational fluency + WCST persev. Ruff Fugural Fluency- Unique Designs, COWAT, Animal Naming
4. Learning WMS-R Verbal Paired I, Verbal Paired II, WMS-R Visual Paired I, Visual Paired II
5. Verbal knowledge WAIS-R Vocab, Info, Comp, Similarities
6. Non-Verbal function WAIS-R Block Design, Pict Comp, Pict Arrangement
Keefe et al., 2006
1,493 Schizophrenia (includes medical and substance abuse comorbidities) PCA 24 5
1. Processing speed COWAT, Category instance, GPB, WAIS-R Digit Symbol
2. Reasoning WCST (Perseverative errors & categories)
3. Verbal memory HVLT (total recall)
4. Working memory Computerized test of visuospatial working memory, letter-number sequencing (# correct)
5. Viligance CPT (d-prime)
Williams et al., 2008
*verified factor structure found in Rowe et al. (2007)
56 First Episode Schizophrenia (mean age = 20) PCA 19 7
1. Information processing & speed Verbal Interference Test Part I, and II, Switching of Attention Test Parts I, and II, Choice Reaction Time test
2. Verbal memory Verbal Learning and Recall Test: delayed, recognition, immediate recall
3. Viligance/sustained attention CPT Reaction Time, CPT Errors
4. Working memory capacity Digit Span forward, Digit Span backward, Span of Visual Memory Test
5. Sensori-motor function average pause between taps on tapping test for dominant and non-dominant hands
6. Verbal processing Letter Fluency, Category Fluency
7. Executive function Maze complettion time, Maze overrun errors, Span of Visual Memory Test
General Findings
• Several models of latent cognitive structure have found
empirical support in one or more population
– A few have been replicated in multiple samples
– And a few have been confirmed by CFA
• The measures included in an assessment strongly affect the
nature of the latent cognitive model that is found
• Three “levels” of model complexity deserve particular
attention
– Single factor model: General cognitive ability (g)
– Two-factor models: Crystallized and fluid abilities (Gc & Gf)
– Multiple-factor models: Multiple cognitive domains

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-134
Lumping vs. splitting
• A single summary measure of impairment or cognitive RFC
ability has advantages
– It is easily understood
– More reliably measured than specific cognitive domains
– Separate factors share common variance anyway
– Summary measures correlate best with most outcomes
• Multiple factors have advantages too
– No theoretical cognitive construct maps onto a summary
impairment index
– Summary scores might mask specific impairments or aspects of
RFC that preclude or support employability
– Scores for multiple measures are no harder to understand than a
single summary score
One-Factor Model: g
• Hundreds of studies document the existence of a single
general mental ability, g, on which individuals differ
• g is a construct
– That is not directly observable
– Determined by genetic and environmental factors
• Arises from fact that performances on all cognitive tasks are
positively correlated
– All cognitive tests measure g (to varying degrees)
– Thus, g is not tied to any specific test content such as words,
numbers, or geometric patterns
– Nor is g bound to any sex, age, or cultural group
• The g component of tests accounts for most of their
predictive power

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-135

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-136
Some Implications & Questions
• 25% of workers fall below 1
st
quartile
• What point in the distribution of
incumbents’ scores defines insufficient
RFC to meet job demands?
– 25
th
%ile, 2
nd
%ile
• How “well” must a disability applicant be
able to perform a job in order to be not
disabled?
– Poor employees are the first laid off
– Job placement vs. job maintenance
• What is “fair” to non-disabled workers?

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-137
Comment
• The single-factor g model has advantages
– It is parsimonious
– g is well documented and highly defensible
– We can measure it reliably in many languages
– Individual differences in g are robust, easily assessed, and strongly
predictive of occupational attainment, work performance, and
income in normal, healthy persons
– We can obtain a reasonable estimate of g in a few minutes, using
such instruments as the Wonderlic Personnel Test
• It also has limitations
– Lacks sensitivity to many types of brain dysfunction
– Does not capture more circumscribed cognitive deficits
– Thus, might not measure residual functional capacity very well
Two-Factor Model
• Many studies distinguish between highly over-learned skills or
knowledge (Crystallized abilities or Gc) and current, online
information processing (Fluid abilities or Gf)
– Gc: vocabulary, fund of information, mathematical ability
– Gf: novel problem solving, reasoning, speed of processing
– Gc grows rapidly in childhood, and more slowly in adulthood, and
then declines in very late life
– Gf grows rapidly in childhood, peaks around age 20, and then declines
throughout adulthood
– Gc is more affected than Gf by education
– Gf is more sensitive than Gc to brain dysfunction

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-138
Application of a
Two-Factor Model
MSE-TV in SSDI/SSI Beneficiaries
Variable
ABC Full Sample
(n = 234)
ABC Matched
Sample (n = 139)
SSA Sample
(n = 139)
Age (years) 54 + 17 43 + 13 41 + 11
Sex (M:F%) 44:56 42:58 45:55
Race (W:B:O%) 79:18:2 68:29:3 26:64:5
Educ. (years) 14 + 3 14 + 3 N/A
MMSE 28 + 2 28 + 2 24 + 4

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-139
PCA with Varimax Rotation Factor Loadings for
ABC and SSA Samples
Question
Factor 1
General Ability
Factor 2
Learning/Memory
Factor 3
Orientation
ABC SSA ABC SSA ABC SSA
Orientation
.93 .99
Word recall (1)
.75 .84
Word recall (2)
.83 .86
Serial 7’s
.77 .79
Opposites
.68 .80
Arithmetic
.60 .80
Information
.73 .69
Word recall (3)
.82 .78
Correlations of MSE-TV Scores with Other
Cognitive Measures
Variable
MSE-TV
Total
MMSE
Total
Factor 1
General
Ability
Factor 2
Learning &
Memory
Factor 3
Temporal
Orientation
WAIS-R Sum SS
0.63** 0.53** 0.66** 0.42** 0.02
NART IQ
0.58** 0.37** 0.69** 0.32** 0.03
HVLT Learning
0.48** 0.30** 0.27** 0.50** 0.05
HVLT Delay
0.44** 0.27** 0.27** 0.45** 0.13
BVMT Learning
0.44** 0.33** 0.27** 0.40** 0.06
BVMT Delay
0.35** 0.33** 0.21** 0.40** 0.07

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-140
Group Differences in MSE-TV Scores
MSE-TV
Variable
Healthy
Controls
(N = 139)
Affective
Disorder
(N = 59)
Schizophrenia
Spectrum
(N = 36)
Cognitive
Disorder
(N = 18)
Mental
Retardation
(N = 20)
Total
39.0 + 5.5
a
31.4 + 7.5
b
29.2 + 5.8
b
27.1 + 6.6
b
20.8 + 6.4
c
Factor 1
14.5 + 3.2
a
10.9 + 4.4
b
10.8 + 3.5
b
8.9 + 4.5
b
4.7 + 3.0
c
Factor 2
20.6 + 3.4
a
16.5 + 3.9
b
14.5 + 3.8
b
14.2 + 4.0
b
12.2 + 4.5
c
Factor 3
3.9 + 0.3 4.0 + 0.0 3.9 + 0.4 3.9 + 0.2 4.0 + 0.2

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-141
Comment on Two-Factor Models
• Allow for slightly more fine-grained assessment of cognitive
functioning and impairments
• Gc reflects over-learned “premorbid” verbal abilities that are
relatively in
sensitive to aging and brain dysfunction
• Gf reflects current nonverbal problem solving abilities that
are sensitive to age and brain dysfunction
• These two factors can be combined into one
Multiple-Factor Models
• Several multiple-factor models emerged from our (selective)
review of the literature
• The most robust and well-replicated factors include
– General mental ability (g)
– Verbal learning and memory
– Processing speed
• Somewhat less clear (in terms of independence)
– Working memory
– Attention/concentration
– Executive functioning
– Ideational fluency

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-142
Johns Hopkins Confirmatory Factor
Analysis in Three Populations
• Determine whether the same hypothesized latent factors
would characterize cognitive functioning in three groups
• Test hypothesized model against specific alternatives
• Hypothesized model based on previous study (Schretlen et al,
2007)
Participants and Method
NC
(n = 340)
SZ
(n=110)
BD
(n=126)
Statistic p
Age (years)
54 ± 19 40 ± 11 42 ± 11
F
(2,571)
=44.1 <.001
Sex (male, %) 44 70 40
χ
2
(2)
= 28.2
<.001
Race (w:b:o %) 79:18:3 39:55:6 55:40:5
χ
2
(4)
= 68.9
<.001
Education (years)
14 ± 3 12 ± 2 14 ± 3
F
(2,571)
=19.5 <.001
Est. premorbid IQ
105 ± 10 97 ± 11 103 ± 12
F
(2,,571)
=23.3 <.001
Recruited 576 participants, including 340 reasonably healthy adults
(NC), 110 relatively stable individuals with schizophrenia (SZ), and 126
relatively stable persons with bipolar disorder (BD).
All participants underwent cognitive testing.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-143
Clinical Characteristics of the Patients
SZ
(n=110)
BD
(n=126)
Statistic p
Age at onset , years
23 ± 7 25 ± 9 t
(212)
= −1.8
.064
Illness duration, years
17 ± 11 18 ± 11 t
(212)
= -0.6
.519
# Hospitalizations
5.0 ± 5.6 3.7 ± 5.1 t
(210)
=1.8
.066
SANS (sum)
8.9 ± 5.5 1.8 ± 2.4 t
(193)
=8.6
.001
SAPS (sum)
4.7 ± 3.8 1.0 ± 1.8 t
(191)
= 11.9
.001
Typical antipsychotic (%) 34 5
χ
2
(1)
= 14.7
.001
Atypical antipsychotic (%) 74 47
χ
2
(1)
= 13.9
.001
Antidepressant (%) 23 48
χ
2
(1)
= 12.0
.002
Lithium (%) 4 56
χ
2
(1)
= 58.6
.001
Anticonvulsant (%) 12 44
χ
2
(1)
= 23.7
.001
Competing Models
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-144
Six-Factor Model
Factor Measures
Psychomotor Speed TMT-A, TMT-B, and GPT (mean of both hands)
Attention BTA-L, BTA-N, and CPT Hit RTse
Ideational Fluency Letter, Category, and Design Fluency
Verbal Memory HVLT-R Learning and delayed recall
Visual Memory BVMT-R Learning and delayed recall
Executive Function mWCST category sorts and errors
Six-Factor Model with TMT-B on EF
Factors Measures
Psychomotor Speed TMT-A and GPT (mean of both hands)
Attention BTA-L, BTA-N, and CPT Hit RTse
Ideational Fluency Letter, Category, and Design Fluency
Verbal Memory HVLT-R Learning and delayed recall
Visual Memory BVMT-R Learning and delayed recall
Executive Function TMT-B, mWCST categories and errors

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-145
Five-Factor “Speed” Model
Factors Measures
Psychomotor Speed TMT-A, TMT-B, GPT, Letter, Category, and Design
Attention BTA-L, BTA-N and CPT Hit RTse
Verbal Memory HVLT-R Learning and delayed recall
Visual Memory BVMT-R Learning and delayed recall
Executive Function mWCST category sorts and errors
Five-Factor “Memory” Model
Factors Measures
Psychomotor Speed TMT-A, TMT-B and GPT (mean of both hands)
Attention BTA-L, BTA-N and CPT Hit RTse
Ideational Fluency Letter, Category, and Design Fluency
Memory HVLT-R and BVMT-R learning and delayed recall
Executive Function Wcst categories and Wcst errors
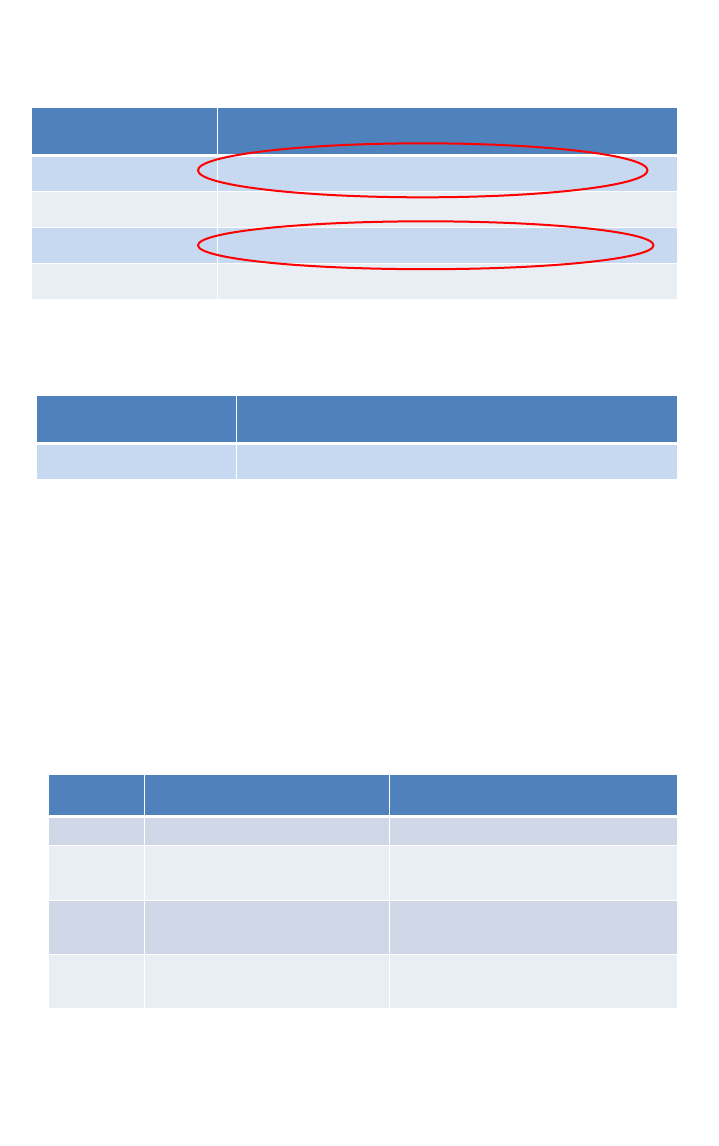
Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-146
Four-Factor Model
Factors Measures
Psychomotor Speed TMT-A, TMT-B, GPT, Letter, Category, and Design
Attention BTA-L, BTA-N and CPT Hit RTse
Memory HVLT-R and BVMT-R learning and delayed recall
Executive Function mWCST category sorts and errors
One-Factor Model
Factors Measures
General Cognition All measures
Evaluating CFA Results
Statistic Name Recommended Values
χ
2
/df Chi-square/df < 3 is a good fit
RMSEA
Root mean square error of
approximation
< 0.05 is a very good fit
< 0.08 is a reasonable fit
NNFI Non-normed fit index
> 0.95 is a close fit
> 0.90 is a good fit
CFI Comparative fit index
> 0.95 is a close fit
> 0.90 is a good fit

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-147
CFA Results: Six-Factor Models
Group χ
2
/df RMSEA NNFI
CFI
Combined 2.50
0.051
0.99 0.99
NC 1.79
0.048
0.98 0.99
BD 1.63
0.071
0.96 0.97
SZ 1.40
0.060
0.98 0.98
Six-Factor Model
Group χ
2
/df RMSEA NNFI
CFI
Combined
4.92 0.083 0.95 0.96
NC
3.44 0.085 0.93 0.95
BD
1.93 0.087 0.94 0.95
SZ
2.03 0.097 0.92 0.94
Six-Factor Model
with TMT-B in EF
CFA Results: Five-Factor Models
Group χ
2
/df RMSEA NNFI
CFI
Combined
4.75 0.081 0.96 0.97
NC
3.38 0.084 0.95 0.96
BD
1.82 0.081 0.95 0.96
SZ
1.54 0.071 0.96 0.97
Five-Factor “Speed”
Model
Group χ
2
/df RMSEA NNFI
CFI
Combined
10.16 0.126 0.89 0.92
NC
4.41 0.100 0.91 0.93
BD
2.59 0.112 0.87 0.90
SZ
2.68 0.124 0.89 0.91
Five-Factor “Memory”
Model

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-148
CFA Results: Remaining Models
Group χ
2
/df RMSEA NNFI
CFI
Combined
11.01 0.132 0.90 0.92
NC
5.69 0.117 0.89 0.91
BD
2.75 0.118 0.87 0.89
SZ
2.76 0.127 0.88 0.91
Four-Factor Model
Group χ
2
/df RMSEA NNFI
CFI
Combined
18.89 0.176 0.76 0.80
NC
12.15 0.181 0.70 0.74
BD
3.95 0.165 0.78 0.81
SZ
4.65 0.171 0.72 0.76
One-Factor (g) Model

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-149
Comment
• In this CFA, the hypothesized six-factor model showed a good
to excellent fit by all evaluative measures
• Other hypothesized models did not fit the data as well
• However, another ensemble of tests almost certainly would
yield a different “optimal” solution
• Therefore, the question of whether to assess mental RFC using
a multi-factor model probably should precede the selection of
which domains to assess
– My personal recommendation is to assess 3–6 domains
Other Big Issues
• Shall we use performance-based measures or informant
rating scales, or both?
– And who should administer them? Change models?
• How shall we validate decision criteria?
– I know of no existing data defining disability “thresholds”
• Shall we use available measures or create a proprietary set
that SSA creates, standardizes, and updates?
– This would be my recommendation for many reasons
– Existing tests become obsolete, raise royalty issues
• There is a theme: The need to design and conduct a couple
studies

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-150
References
Colom R, R.J. H, Alvarez-Linera J, et al.: Gray matter correlates of fluid, crystalized, and spatial
intelligence: Testing the P-FIT model. Intelligence 37:124-135, 2009.
Czobor P, Jaeger J, Berns SM, et al.: Neuropsychological symptom dimensions in bipolar disorder
and schizophrenia. Bipolar Disord 9:71-92, 2007.
Dickinson D, Iannone VN, Wilk CM, et al.: General and specific cognitive deficits in schizophrenia.
Biol Psychiatry 55:826-833, 2004.
Dickinson D, Ragland JD, Calkins ME, et al.: A comparison of cognitive structure in schizophrenia
patients and healthy controls using confirmatory factor analysis. Schizophr Res 85:20-29, 2006.
Frazier TW, Youngstrom EA, Chelune GJ, et al.: Increasing the reliability of ipsative interpretations
in neuropsychology: a comparison of reliable components analysis and other factor analytic
methods. J Int Neuropsychol Soc 10:578-589, 2004.
Friis S, Sundet K, Rund BR, et al.: Neurocognitive dimensions characterising patients with first-
episode psychosis. Br J Psychiatry Suppl 43:s85-90, 2002.
Genderson MR, Dickinson D, Diaz-Asper CM, et al.: Factor analysis of neurocognitive tests in a
large sample of schizophrenic probands, their siblings, and healthy controls. Schizophr Res
94:231-239, 2007.
Gladsjo JA, McAdams LA, Palmer BW, et al.: A six-factor model of cognition in schizophrenia and
related psychotic disorders: relationships with clinical symptoms and functional capacity. Schizophr
Bull 30:739-754, 2004.
Gomez-Perez E, Ostrosky-Solis F: Attention and Memory Evaluation Across the Life Span:
Heterogeneous Effects of Age and Education. Journal of Clinical and Experimental
Neuropsychology 28:477-494, 2006.
Jaeger J, Czobor P, Berns SM: Basic neuropsychological dimensions in schizophrenia.
Schizophr Res 65:105-116, 2003.
Johnson DK, Storandt M, Morris JC, et al.: Cognitive profiles in dementia: Alzheimer disease vs
healthy brain aging. Neurology 71:1783-1789, 2008.
Jones JJS, van Schaik P, Witts P: A factor analysis of the Wechsler Adult Intelligence Scale 3rd
Edition (WAIS-III) in a low IQ sample. British Journal of Clinical Psychology 45:145-152, 2006.
Keefe RS, Bilder RM, Harvey PD, et al.: Baseline neurocognitive deficits in the CATIE
schizophrenia trial. Neuropsychopharmacology 31:2033-2046, 2006.
Rowe DL, Cooper NJ, Liddell BJ, et al.: Brain structure and function correlates of general and
social cognition. J Integr Neurosci 6:35-74, 2007.
Salthouse TA: Independence of age-related influences on cognitive abilities across the life span.
Dev Psychol 34:851-864, 1998.
Siedlecki KL, Honig LS, Stern Y: Exploring the structure of a neuropsychological battery across
healthy elders and those with questionable dementia and Alzheimer's disease. Neuropsychology
22:400-411, 2008.
Tulsky DS, Price LR: The joint WAIS-III and WMS-III factor structure: Development and cross-
validation of a six-factor model of cognitive functioning. Psychological Assessment 15:149-162,
2003.
Visser BA, Ashton MC, Vernon PA: Beyond g: Putting multiple intelligences theory to the test.
Intelligence 34:487-502, 2006.
Williams LM, Whitford TJ, Flynn G, et al.: General and social cognition in first episode
schizophrenia: identification of separable factors and prediction of functional outcome using the
IntegNeuro test battery. Schizophr Res 99:182-191, 2008.

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-151
Appendix E
Second Mental Cognitive Subcommittee Presentation
Clinical Inference in the Assessment of
Mental Residual Functional Capacity
David J Schretlen, PhD, ABPP
OIDAP Panel Meeting
10 June 2009
Methods of Inference
1. Pathognomonic sign approach
2. Pattern analysis
3. Level of performance or deficit measurement

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-152
Pathognomonic Signs
• Characteristic of particular disease or condition
• High specificity
• Present vs. absent
• Often ignored questions
– How frequent are they in healthy individuals?
– How reliable are they?
• 10 physicians (5 neurologists & and 5 others)
• Examined both feet of 10 participants
– 9 w/ upper motor neuron lesions (8 unilateral; 1 bilateral)
– 1 w/ no upper motor neuron lesion
• Babinski present in
– 35 of 100 examinations of foot w/ UMN weakness (sensitivity)
– 23 of 99 examinations of foot w/o UMN weakness (specificity)
Neurology (2005)

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-153
Pathognomonic?
91-year-old Caucasian woman
14 years of educ (AA degree)
Excellent health
Rx: Floxin, vitamins
MMSE = 27/30
WAIS-R MOANS IQ = 109
Benton FRT = 22/27
WMS-R VR Immed. SS = 8
Jan. 2004: 68-year-old retired engineer with
reduced arm swing, bradyphrenia & stooped
posture. Diagnosed with atypical PD.
Apr. 2005: Returns for follow-up testing 2
months after CABG; thinks his memory has
declined slightly but PD is no worse
Jan. 2007: Returns & wife reports
visual hallucinations, thrashing in
sleep, & further memory but his
PD is no worse and he still drives

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-154
Pathognomonic Signs: Limitations & Implications
• Are there any in clinical neuropsychology?
– Unclear if there are any for a specific disease or condition
• Might be more prevalent in normal population than commonly
thought
• Reliability is rarely assessed
• If we recommend that SSA rely on pathognomonic signs of
impairment, we should not assume that successful job
incumbents are free of such signs
Methods of Inference
1. Pathognomonic sign approach
2. Pattern analysis
3. Level of performance or deficit measurement

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-155
Pattern Analysis
• Recognizable gestalt of signs, symptoms, history,
laboratory findings, and test results
• Most elaborate approach to inference
• Best for patients with typical presentations
Empirical Basis of Pattern Analysis
• Considerable empirical support
– But much of it is pieced together from disparate studies
• Studies often involve discriminant function analyses
– Other designs have been used (eg, comparing AD and HD patients
on MMSE after matching for total score)

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-156
Derived 32 z-transformed test scores for 197 healthy Ss
Subtracted each person’s lowest z-score from his or her own
highest z-score to measure the “Maximum Difference” (MD)
Resulting MD scores ranged from 1.6 - 6.1 (M=3.4)
65% produced MD scores >3.0; 20% had MDs >4.0
Eliminating each persons’ single highest and lowest test scores
decreased their MDs, but 27% still produced MS values of 3.0
or greater
Intra-individual variability shown by 197 healthy adults
0
5
10
15
20
25
30
35
<
1
.
5
1
.
5
-
1
.
9
9
2
.
0
-
2
.
4
9
2
.
5
-
2
.
9
9
3
.
0
-
3
.
4
9
3
.
5
-
3
.9
9
4
.
0
-
4
.4
9
4
.
5
-
4
.9
9
>
4
.
9
9
Maxmimum Discrepancy in SD Units
Percent of Cases
All Scores Hi/Lo Scores Excluded

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-157
Pattern Analysis: Limitations & Implications
• Applicability varies with typicality of patient
• Normal variation can be mistaken for meaningful patterns
• This approach probably mirrors the task of linking specific
residual functional capacities to job demands more closely
than the others
• It might be useful to think about linking specific RFCs to job
demands using such statistical methods as cluster analysis or
canonical correlation
Methods of Inference
1. Pathognomonic sign approach
2. Pattern analysis
3. Level of performance or deficit measurement

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-158
Level of Performance
• Often used to detect impairments or deficits
• But
, what is an impairment or deficit?
– Deficient ability compared to normal peers?
– Decline for individual (but normal for peers)?
Level of Performance: Deficit Measurement
• We infer ability from performance
– But factors other than disease (eg, effort) can uncouple them
– There is no one-to-one relationship between brain dysfunction and
abnormal test performance at any level
• But even if other factors do not uncouple them, what is an
abnormal level of performance?
• Thought experiment: Suppose we test the IQs of 1,000,000
perfectly healthy adults

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-159
Would the distribution look like this?
Probably not

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-160
More likely, the distribution would be shifted up
Consequently
• If a distribution of one million IQ test scores is shifted up
10 points, but remains Gaussian, then 4800 people will
still score below 70
• How do we understand normal, healthy people with IQs
below 70?
– Chance?
– Healthy but nonspecifically poor specimens?

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-161
Logical Conclusions
• Some of those who perform in the lowest 2% of the
distribution are normal
• Most of those who perform in the lowest 2% of the
distribution are impaired
• The probability of impairment increases with distance
below the population mean
Cutoff Scores
• Help decide whether performance is abnormal
• Often set at 2 sd below mean, but 1.5 and even 1 sd
below mean have been used
• If test scores are normally distributed, these cutoffs will
include 2.3% to 15.9% of normal individuals on any
single measure

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-162
Multiple Measures
• When a test battery includes multiple measures, the number
of normal healthy individuals who produce abnormal scores
increases
• So does the number of abnormal scores they produce
• Using multiple measures complicates the interpretation of
abnormal performance on test batteries
The binomial distribution can be used to predict how many abnormal
scores healthy persons will produce on batteries of various lengths
Number of Tests Administered
Cut-off 10 20 30
--1.0 SD .50 .84 .95
--1.5 SD .14 .40 .61
--2.0 SD .03 .08 .16
Probability of obtaining 2 or more “impaired” scores based
on selected cut-off criteria & number of tests administered
Ingraham & Aiken (1996)

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-163
• Participants
– 327 reasonably healthy adults without current psychiatric illness
or substance abuse/dependence
• Procedure
– Administered 25 cognitive measures; obtained T-scores
– Classified T-scores as normal or “abnormal” based on three
cutoffs: <40, <35, and <30
– Computed Cognitive Impairment Indices (CII) as the number of
abnormal scores each person produced
– Used both unadjusted and demographically adjusted scores
• We estimated how many individuals would produce 2 or more
abnormal scores using three T-score cutoffs
1. Based on binomial distribution (BN)
2. Based on Monte Carlo simulation (MC) using unadjusted T-scores
3. Based on Monte Carlo simulation (MC
adj
) using adjusted T-scores

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-164
Test/Measure
M ±SD
Mini-Mental State Exam
28.1 ±1.7
Grooved Pegboard Test
Dominant hand
Non-dom hand
80.4 ±28.1
90.5 ±34.7
Perceptual Comparison Test
64.5 ±16.4
Trail Making Test
Part A
Part B
34.9 ±17.0
95.0 ±69.4
Brief Test of Attention
15.4 ±3.7
Modified WCST
Category sorts
Perseverative errors
5.3 ±1.3
2.5 ±3.9
Verbal Fluency
Letters cued
Category cued
28.2 ±9.2
44.8 ±11.4
Boston Naming Test
28.2 ±2.6
Benton Facial Recognition
22.4 ±2.3
Test/Measure
M ±SD
Rey Complex Figure
31.3 ±4.3
Clock Drawing
9.5 ±0.8
Design Fluency Test
14.2 ±7.2
Wechsler Memory Scale
Logical Memory I
Logical Memory II
26.3 ±6.9
22.4 ±7.5
Hopkins Verbal Learning Test
Learning
Delayed recall
Delayed recognition
24.6 ±4.8
8.7 ±2.6
10.4 ±1.6
Brief Visuospatial Memory
Test
Learning
Delayed recall
Delayed recognition
22.2 ±7.5
8.7 ±2.7
5.6 ±0.7
Prospective Memory Test
0.6 ±0.7
25 Measure Battery
Predicted and observed percentages of participants who
produced 2 or more abnormal test scores (y axis) as defined by
three different cutoffs (<40, <35, and <30 T-score points)

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-165
Spearman correlations between Cog Imp Index scores based on unadjusted T-
scores and age, sex, race, years of education and estimated premorbid IQ
No. of
tests
T-score
cutoff
Mean (SD) Age Sex Race Educ. NART IQ
25 < 40 3.6 (4.4) .573** -.029 .215** -.327** -.360**
25 < 35 1.6 (2.7) .528** -.039 .186* -.325** -.354**
25 < 30 0.5 (1.3) .409** -.066 .176 -.312** -.318**
* = p < 0.001; ** = p < 0.0001
This study shows that
• Neurologically normal adults produce abnormal test scores
– Rate varies with battery length & cutoff used to define abnormal
• This is not due purely to chance
– Varies with age, education, sex, race and est. premorbid IQ
– Demographically adjusting scores eliminates the relationship between
these characteristics and abnormal performance
• Findings underscore distinction between “abnormal” test
performance and “impaired” functioning
– Test performance can be abnormal for many reasons: impaired functioning
is but one

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-166
Returning to the question of what cut-off we should
use to define abnormal performance…
• Stringent cut-offs decrease test sensitivity
• Liberal cut-offs decrease test specificity
• Adding tests increases the risk of type I errors
• Excluding tests increases the risk of type II error
• As in most endeavors, we must exercise judgment
Decline from Premorbid Ability
• If we know a person’s “premorbid” ability, then it is
relatively simple to determine decline
– Unfortunately, we rarely know this
– Therefore, we have to estimate it
– So how do we do that?
• Research has focused on estimating premorbid IQ

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-167
Estimating Premorbid IQ
• Demographic prediction
– Barona formula SE
est
= 12 points (95% CI = +24 points)
• Word reading tests are more accurate
– Except for persons with very limited education
– And those with aphasia, reading disorders, or severe dementia
– And persons for whom English is a second language
Stability of NART-R IQ Estimates
NART IQ at Baseline
125120115110105100959085
NART IQ at 5-Year Follow-Up
125
120
115
110
105
100
95
90
85 Rsq = 0.9479

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-168
Correlation of NART-R and WAIS-R
NART IQ
14513512511510595857565
Current Est. FSIQ
145
125
105
85
65 Rsq = 0.5776
Administered 26 cognitive measures to 322 healthy adults
Regressed each on age, saved the residuals, and correlated
these with NART-R scores
Compared the correlation of NART-R and IQ with correlations
of the NART-R and other age-adjusted cognitive measures
But how well does the NART-R predict cognitive
abilities other than
IQ?

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-169
NART-R correlation with
FSIQ = .72
NART-R correlations with
other test scores ranged
from -.53 to .48
(Every one of the latter was
significantly smaller than the
correlation with FSIQ)
Estimating Premorbid Abilities
• An essential and unavoidable aspect of every
neuropsychological examination
• If we don’t do explicitly, then we do it implicitly
• Even the best methods yield ballpark estimates
• We’re better at estimating premorbid IQ than other
premorbid abilities

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-170
Examined 28 scores derived from 16 cognitive tests that were
administered to 221 reasonably healthy adults
Grouped participants by WAIS-R Full Scale IQ into three groups:
N = 37 Below average (BA) FSIQ < 90 Mean = 83
N =106 Average (A) FSIQ 90-109 Mean = 101
N = 78 Above average (AA) FSIQ > 109 Mean = 121
80
85
90
95
100
105
110
115
120
GPT
D
o
m
GP
T
N
-D
o
m
BTA
TMT A
TMT B
mWCST Cat
mWCST P
E
CE
T
D
F
T
PC Spe
e
d
C
PT
H
i
t
R
T
C
P
T
R
T
-SE
CP
T
d'
Le
t
ter VF
C
ate
go
ry
VF
BNT
FRT
Rey CFT
HV
L
T (1-3)
H
V
L
T
(4
)
HV
L
T
D
i
sc
L
M-I
L
M
-
D
B
V
M
T (1
-
3
)
BVMT
(
4)
B
V
M
T
Disc
VR-I
VR-D
Cognitive Test Variable
Age-Adjusted Scaled Scor
e
FSIQ < 90 FSIQ = 90-109 FSIQ>110

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-171
Intelligence and Cognitive Functioning
• Correlations between intelligence and other cognitive abilities
are stronger below than above IQ scores of 110
– It is less likely that smart people will do well on other tests than
it is that dull people will do poorly
• A normal person with an IQ of 85 is likely to produce
“impaired” scores on about 10% of other cognitive tests
Deficit Measurement: Limitations & Implications
• No isomorphic relationship between performance and ability
• Adding tests can increase false positive (type 1) errors
• Setting stringent cut-offs can increase misses (type 2) errors
• NART predicts pre-morbid IQ better than other abilities
• Raising “cut-off” scores for patients of above average IQ can
compound the problem of multiple comparisons

Mental Cognitive Subcommittee
Content Model and Classification Recommendations
C-172
Deficit Measurement: Limitations & Implications
• Many – if not most – successful job incumbents likely fall
short of meeting one or more of their job demands
• What cutoff in the distribution of an ability shown by
successful job incumbents should we use to define sufficient RFC
for someone to do that job? This will directly
affect the
percentage of applicants who will be found disabled
• Factors other than impairment, like effort, can uncouple the
linkage between performance and ability
• Work demands, RFC, and “deficit” vs. “impairment”
References
Axelrod, B. N., & Wall, J. R. (2007). Expectancy of impaired neuropsychological test scores in a non-clinical
sample. International Journal of Neuroscience, 117(11), 1591-1602.
Binder, L. M., Iverson, G. L., & Brooks, B. L. (2009). To err is human: "abnormal" neuropsychological scores
and variability are common in healthy adults. Arch Clin Neuropsychol, 24(1), 31-46.
Brandt, J., Folstein, S. E., & Folstein, M. F. (1988). Differential cognitive impairment in Alzheimer's disease
and Huntington's disease. Annals of Neurology, 23(6), 555-561.
Crawford, J. R., Garthwaite, P. H., & Gault, C. B. (2007). Estimating the percentage of the population with
abnormally low scores (or abnormally large score differences) on standardized neuropsychological test
batteries: A generic method with applications. Neuropsychology, 21(4), 419-430.
Damasceno, A., Delicio, A. M., Mazo, D. F., Zullo, J. F., Scherer, P., Ng, R. T., et al. (2005). Primitive
reflexes and cognitive function. Arquivos de Neuro-Psiquiatria, 63(3A), 577-582.
Diaz-Asper, C. M., Schretlen, D. J., & Pearlson, G. D. (2004). How well does IQ predict neuropsychological
test performance in normal adults? Journal of the International Neuropsychological Society, 10(1), 82-90.
Jacobs, L., & Gossman, M. D. (1980). Three primitive reflexes in normal adults. Neurology, 30(2), 184-188.
Miller, T. M., & Johnston, S. C. (2005). Should the Babinski sign be part of the routine neurologic
examination? Neurology, 65(8), 1165-1168.
Schretlen, D. J., Buffington, A. L., Meyer, S. M., & Pearlson, G. D. (2005). The use of word-reading to
estimate "premorbid" ability in cognitive domains other than intelligence. Journal of the International
Neuropsychological Society, 11(6), 784-787.
Schretlen, D. J., Munro, C. A., Anthony, J. C., & Pearlson, G. D. (2003). Examining the range of normal
intraindividual variability in neuropsychological test performance. Journal of the International
Neuropsychological Society, 9(6), 864-870.
Schretlen, D. J., Testa, S. M., Winicki, J. M., Pearlson, G. D., & Gordon, B. (2008). Frequency and bases of
abnormal performance by healthy adults on neuropsychological testing. J Int Neuropsychol Soc, 14, 436-445
.
