Canada’s Health Crisis:
Profiling Opioid Addiction in Alberta & British Columbia
Report for the Stanford Network on Addiction Policy (SNAP) by:
Blair Gibbs
Ryan Workman
Jake Kiefer
Chosen Canlas
March 2023
1
Background
This project was commissioned by Professor Keith Humphreys of Stanford University and was funded through the
Stanford Network on Addiction Policy (SNAP).
Purpose of Study
The purpose of this report is to investigate the current state of the opioid addiction crisis in Canada. The report gives
specific attention to Alberta and British Columbia, the two provinces in Canada with the highest rates of opioid-related
overdose deaths. The report seeks to identify drivers of the crisis and key features of the provincial policies, along with the
makeup of the addicted populations and overdose victims.
Methodology
This report utilized publicly available data at both the federal and provincial level applying both quantitative and qualitative
research methods. All data was retrieved between September 2022 and February 2023. Access to certain datasets was
refused in the absence of an ethics approval.
2
Executive Summary
Canada’s drug addiction crisis has been mounting for two decades, and shares many of the same features as the
well documented experience of the United States. In both countries, the COVID-19 pandemic exacerbated the health
harms, with rates of drug mortality in areas like British Columbia (BC) in 2022 as high as the worst affected parts of the
USA.
There is more political attention on the issue compared to a decade ago, but a situation that warranted a
declaration of a public health emergency in BC in 2016 has not improved since then – in fact the crisis has
escalated. As of December 31, 2022, the rate of illicit drug toxicity deaths in BC has more than doubled since the
emergency was first declared in 2016.
This report explores what is behind this dramatic deterioration and focuses on the characteristics of the crisis in
British Columbia and Alberta – two neighbouring provinces in Western Canada that are home to a disproportionate
share of the harm caused by opioid addiction today.
Key Findings
Canada’s addiction crisis in context
• The scale of drug-related harms in Canada are significant, dramatically outpacing comparator jurisdictions in
places like Europe. The death rate in Canada’s worst affected province – British Columbia – has risen from 5.8 per
100,000 in 2000 to 44.2 per 100,000 in 2021. In Canada, the number of accidental apparent opioid toxicity deaths
(AAOTDs) per 100,000 was 20.2 per 100,000 in 2021. For comparison, in 2019, England and Wales had a drug-
related mortality rate of 7.7 per 100,000.
• BC’s AAOTD rate in 2021 was more than double the national average, and Alberta was not far behind at 36 per
100,000. Ontario had the most total AAOTDs (2,772) but had a lower death rate of 19.4 per 100,000.
• Between them, BC and Alberta accounted for a quarter of Canada’s population but almost half (49%) of drug
deaths (3,804). To put this another way, 1 in every 7 Canadians live in BC and 1 in every 9 live in Alberta, but 1 in
3
every 4 AAOTD in 2021 was a British Columbian and 1 in every 5 was an Albertan. The share of AAOTDs held by
Alberta and BC has actually decreased slightly from 54% in 2016.
• In Canada overall, in 2020 and 2021, opioids caused nearly half as many deaths (13,815) as COVID-19 over the
same period (29,985), and were responsible for five times the number of lost life years. The COVID-19 pandemic
caused approximately 90,000 lost years of life in 2020 and 2021. Over that same period, premature deaths from
opioids caused nearly 450,000 lost years of life. The crisis has gotten so severe that it halted the increase in Canadian
life expectancy between 2016 and 2017, the first time that Canadian life expectancy has decreased in over four
decades.
• Opioid addiction is now at a scale that makes it a general public health concern. Alcohol and tobacco kill more
Canadians than illicit drugs, however those who overdose on opioids are usually far younger than those who die of
alcohol or tobacco. Because the chronic health impacts of alcohol or tobacco consumption manifest over decades of
use, opioids are responsible for more life years lost than tobacco, and nearly as many life years lost as alcohol, despite
not having the same level of general use in the population.
Opioid addiction in Canada
There are many dimensions to opioid-related-harms, but this report focuses on deaths, hospitalizations, lost life years, and
drug-related crime. Key findings regarding opioid-related harms include:
• Although illicit drug use often begins in adolescence or young adulthood, the people most impacted by
AAOTDs in Canada are those aged between 30 and 49. In 2021, middle-aged Canadians aged 30-49 represented
27% of the population and over half (52%) of all AAOTDs. Two other cohorts – 20-29-year-olds and 50-59-year-olds –
together represent 26% of the population and 38% of AAOTDs.
• The impact of opioid addiction is not evenly spread, and the concentration is significant. Geographically, the
harms are concentrated in Alberta and BC, and there is a disproportionate impact according to age and sex. Over half
of those suffering from opioid harms in Canada are 30-59-year-old men, though in BC the most impacted group is 50-
59-year-old-men.
• Indigenous people in Canada are also over-represented in terms of opioid harms. In Alberta, First Nations
individuals were dying at a rate nearly 7 times that of non-first nations in the first six months of 2020. In BC, between
January and June 2021, 14% of overdose deaths were among First Nations peoples despite them representing only
4
3.3% of the population. First Nations people had an illicit drug-related death rate 4.8 times greater than other BC
residents in 2021.
• Low income and lack of employment were also key drivers of opioid harms. The BC Coroners Service found that
only 35% of those who suffered illicit drug toxicity deaths between August 2017 and July 2021 were employed at the
time of their death. Data for BC shows income levels were also correlated with opioid-related mortality and
hospitalization, with those in the lowest quintile being 3.8 times more likely to suffer opioid-related mortality and 4.3
times more likely to be hospitalized for opioid-related reasons.
• Drug addiction often compounds other health issues, with poor mental health a common aggravating factor. In
BC, between August 2017 and July 2021, 62% of people who died of illicit drugs were experiencing mental health
issues. Those who die have often been in contact with the health system. Decedents had a higher number of health
visits, and 30% had had a previous paramedic attended non-fatal illicit drug related event.
Key drivers of drug deaths
Fentanyl is a synthetic opioid that can be up to 50 times stronger than heroin and 100 times stronger than morphine, but it
was not a feature of the drug market even 10 years ago. Fentanyl and its analogues have played an important role in the
opioid crisis because they are significantly cheaper to produce per dose and much harder to detect illicit supply routes.
This makes them more widespread in illicit drug markets and harder for law enforcement to trace and detect, and it is also
more likely that a dose will be too potent and cause people who use these drugs to overdose:
• The single factor that best explained the distribution of drug harms in Canada, based on published data, was
the prevalence of fentanyl. Though the populations of drug users were highest in Alberta and BC, the difference was
not substantial enough to explain why these provinces have approximately double the rate of deaths than Canada as a
whole, and eight times the AAOTD rate compared to jurisdictions such as Quebec and Newfoundland.
• Fentanyl was detected much more frequently in samples seized by law enforcement in Western Canada than in
Eastern Canada. Based on data from Health Canada’s Drug Analysis Service (DAS), this indicates a preponderance
for more toxic drug supply in these provinces, and marked correlations in other parts of Canada.
• In Alberta, in 2021, fentanyl was detected in 81% of all accidental drug poisoning deaths. In BC between 2019 and
2022, fentanyl was detected in 85% of all illicit overdose deaths. Further, fentanyl detection in BC has risen in tandem
with the death rate.
5
• Increased harms are not the result of an increase in the user base for illicit drugs. When considered alongside
survey data on self-reported drug use, it appears the increase in opioid-related harms in Canada is being driven by the
increased toxicity of the supply, rather than an increase in the number of drug users in the general population.
Other possible drivers of the higher rates of drug harm in Alberta and BC not considered in detail for this report include
access to treatment and rates of attrition in recovery services; inward migration of drug users; income and socio-economic
inequality; distribution of ethnicities within provinces; housing access and stability; and prescribing and dispensing
practice.
Drug crime in Canada
Crime associated with illicit drug markets is a further cause of harm to communities. Compared to twenty years ago, the
emphasis in Canada has shifted away from punishing users and sanctioning possession to deter drug use. However, as in
the USA, the fentanyl causing overdoses in Canada are supplied by an illegal market where addicted drug users are
exploited by organised crime and their international suppliers, who are still subject to serious penalties when they are
caught and prosecuted. The current state of this activity is hard to gauge, but our research found:
• Enforcement against drug crime has reduced in recent years. For Canada overall, sentencing volumes for drug-
related crime have dropped by over 50% in the past decade. Convictions for crime overall in Canada have also
dropped, but not to nearly the same extent, indicating a general lessening of criminal justice enforcement against drug
offences in Canada during the escalating health crisis of opioid addiction.
• The majority of reported opioid-related offences occur in BC. In 2021, BC – comprising approximately 13% of
Canada’s population – had nearly half of all police-reported opioid trafficking, production, and distribution (TPD)
incidents in Canada (drug offences that do not encompass personal possession). BC’s rate of opioid-related police
recorded incidents in 2021 was more than four times the recorded incident rate in Alberta.
• Despite the high volume of drug violations in BC, criminal charges for these offences are low, and appear
disconnected from incident rates. By contrast, charges for serious drug-related crimes are much higher in Alberta,
and increases in charges broadly tracked the trend in incidents, with rising rates after 2012 and reductions more
recently.
• In BC, drug possession incidents have increased significantly in the last decade, and TPD incidences have also
increased after 2016, but charge rates for both categories have remained broadly flat or even fallen over the same
period, suggesting a lack of interest by law enforcement in traditional prosecution for these offences.
6
• Crime incident data confirms BC is the epicentre of drug-crime in Canada, reporting 57 opioid-related incidents
per 100,000 population, compared to 13 per 100,000 in Alberta. Vancouver also has much higher numbers of drug-
related violations than anywhere else, and significantly higher than large cities like Calgary or Edmonton.
• In BC, drug users caught in possession have not been routinely charged by police in recent years,
foreshadowing the formal decriminalisation of drug possession in BC that came into effect on 31 January 2023.
However, this does not seem to reflect a law enforcement focus on upstream interdiction instead. When considering
the more serious drug offences involved in supply and profiting from the illicit market, the gap between TPD incidents
and charges in BC, however, is significant (80 per 100,000 incidents vs. 22 per 100,000 charges in 2019). In contrast,
Alberta charges far more people for TPD relative to the incidents detected (46.6 per 100,000 incidents vs. 38 per
100,000 charges).
Provincial comparison
Drug addiction affects every community but there is also a geographic concentration in western Canada. For more than a
decade, Alberta and BC have been Canada’s opioid hotspots, but there are some differences in how the crisis has
presented in the two provinces.
• British Columbia has a much longer history with substance harms than Alberta, and volume of harm is much
higher in BC, measured according to deaths and hospitalisations. However, the rise in AAOTDs in Alberta during
the pandemic has been steeper relative to its pre-pandemic levels.
• BC’s opioid addiction crisis skews older and more male – for reasons that have not been closely studied. On
age, Alberta is similar to the Canadian average, with 30-49-year-olds representing 30% of the population and 54% of
deaths. Those dying in BC, however, tend to be older: 50–59-year-olds represented only 13% of the province’s
population in 2021, but account for 28% of all AAOTD deaths.
• The ratio of male to female deaths in Alberta was in line with national averages, but was more acute in BC,
where 80% of all AAOTDs in 2021 were men. This could indicate that the resident base of drug users in BC – which
itself may explain the elevated number of deaths there - is being supplemented by inward migration from other
provinces.
• The impact on emergency dispatch caseloads from the addiction crisis is much higher in BC. Looking at
ambulance data, Emergency Medical Service (EMS) responses to suspected opioid-related overdoses are highest in
BC (24,152 responses) – three times the volume of such incidents in Alberta (8,215 responses).
7
Policy Responses in Western Canada
Strategies and municipal initiatives have been launched to addressed the crisis, beginning with the landmark ‘Four Pillars’
strategy published by the City of Vancouver in 2000. Major funding commitments have been made by the provincial
governments; however, the addiction crisis continues in both provinces, with 2022 being the second-deadliest year ever
for drug harms in both jurisdictions.
Both Alberta and BC deploy elements of harm reduction along with recovery. This report found that there was a significant
degree of overlap between the policy approaches and services provided by the two provinces, however the policy framing
and direction are not the same:
• Both provinces support harm reduction activity such as Naloxone distribution to emergency services and
community providers. In recent years, there has been a dramatic upswing in naloxone kit distribution in Alberta
where in 2022 there was approximately 135,330 kits distributed compared to only 32,140 in 2017, and 6,181 in 2016.
In BC, over one million naloxone kits were distributed between 2012 and 2021.
• Both provinces also fund and permit syringe exchange programs, and supervised consumption sites (SCS) in
multiple locations, with Vancouver being the location for the first such facility that opened in 2003.
However, there are some notable differences between Alberta and British Columbia:
• The provincial government and health providers in BC have placed a stronger emphasis on harm reduction,
with ‘safe supply’ for users of illicit drugs, and the recent decriminalization of drug possession, approved by the Federal
Government, in order to further reduce stigma and protect drug users from enforcement.
• Alberta has weighted their response more towards investment in rehabilitation beds and spaces, such as
therapeutic communities. Alberta has also not adopted the models of ‘safe supply’ – including proposals for
automated dispensing – that have been setup in BC. In addition to investments in treatment and new community
dispensing of licensed medicines like Sublocade, the province has also committed capital to building new recovery
communities.
• Published data implies that there is more residential recovery bed provision in Alberta than BC today, but
comparisons are hampered by a lack of consistent recording. It is currently not possible to compare the two provinces
on the politically salient issue of treatment and recovery outcomes based on the available data.
8
• The most apparent difference in policy between the provinces is BC’s recent decriminalisation of substance
possession. Alberta, while, bolstering funding and support around its recovery model, is maintaining current
approaches to law enforcement around illicit drugs.
• Enforcement appears to be a more integral part of the response in Alberta, although the province has also seen a
reduction in its incident caseload. The ratio of serious drug incidents to charges was nearly 1:1 in Alberta, compared to
BC where the ratio of incidents to charges was about 4:1.
There is a lack of policy innovation in BC on the issue of drug addiction, although a growing political interest in finding
sustainable solutions. Alberta’s nascent ‘Recovery-oriented System of Care’ model has new investment and political
leadership but has not yet had time to fully deliver results, with recovery communities still being constructed.
As the implementation of these neighbouring strategies advances, ongoing scrutiny of their impacts and effectiveness is
required to inform policymakers across Canada and other jurisdictions. Close engagement between policymakers and
service leads in both provinces will be important to allow sharing of learnings, especially in those areas where provincial
practices begin to diverge.
Headline conclusions
Despite the urgency of this crisis, and the many years to make the necessary investments, some basic information
architecture is still not in place to support policymakers or to guide those practitioners on the ground working to help
users suffering from drug addiction. This means that the impact of many policies in Canada to reduce harms and to aid
recovery cannot be properly evaluated.
Canada’s experience could provide lessons to other countries like the USA, but only if governments at all levels
commit to a consistent suite of reporting measures that accurately describes the progress being made, and one that
counts more than caseloads, inputs, or a series of ‘harm’ metrics.
Given the significant public funds that continue to be spent, it is time for provincial and federal policymakers to
urgently agree upon what success looks like and how it will be measured. In the absence of robust metrics around
treatment and pathways for recovery, the ‘harm’ metrics around deaths and hospitalisation become the only marker of
policy progress.
9
Of the two provinces studied for this report, Alberta is currently experiencing a reduction in key addiction-related
harms; however, it is based on two quarters of data, and would need to be sustained through 2023 to represent an
established trend. Our research indicates that Canada overall, and BC in particular, is not yet showing the progress that
the public and those impacted by drug addiction deserve.
Widespread public concern about this challenge is likely to continue and as death rates remain high, more
transparency, innovation and new policy responses are therefore needed. The current political attention on how two
provinces are choosing to respond to the opioid addiction crisis provides a window of opportunity to embrace new
solutions with focused political leadership in order to finally see Canada’s harmful trends around opioid addiction
reversed.
10
Contents
Background ......................................................................................................................................................................... 1
Executive Summary ............................................................................................................................................................. 2
Contents ............................................................................................................................................................................. 10
Foreword ............................................................................................................................................................................ 14
Introduction ....................................................................................................................................................................... 17
CHAPTER 1: Defining the Problem ................................................................................................................................... 21
Opioids: their function and role ....................................................................................................................................................... 21
Benefits and Harms........................................................................................................................................................................... 22
Risk and Context ............................................................................................................................................................................... 23
CHAPTER 2: History of Canada’s health crisis ................................................................................................................ 26
Overview ............................................................................................................................................................................................. 26
Wave 1 (1980s – 2010) .................................................................................................................................................................... 27
Wave 2 (2010 – 2014) ...................................................................................................................................................................... 27
Wave 3 (2014-2019) ......................................................................................................................................................................... 28
Wave 4 (2020 – Present) .................................................................................................................................................................. 29
What Comes Next? ........................................................................................................................................................................... 29
CHAPTER 3: Data ............................................................................................................................................................... 30
Deaths, Hospitalizations and EMS .................................................................................................................................................. 30
Population of People who Use Illegal Substances in Canada .................................................................................................... 31
Fentanyl and Overdose Deaths ....................................................................................................................................................... 33
Policing and Criminal Justice .......................................................................................................................................................... 34
11
Multi-Drug Use ................................................................................................................................................................................... 37
Risk Factors........................................................................................................................................................................................ 38
Sex ................................................................................................................................................................................................. 38
Age ................................................................................................................................................................................................. 39
Age and Sex ................................................................................................................................................................................. 40
Ethnicity ......................................................................................................................................................................................... 40
Employment and Socio-Economic Status ................................................................................................................................ 42
Location of Death and Household Characteristics ................................................................................................................. 43
Marital Status ................................................................................................................................................................................ 44
Area-Level Characteristics ......................................................................................................................................................... 44
Mental Health and Contact with Healthcare System .............................................................................................................. 44
Education ...................................................................................................................................................................................... 45
Summary: Canada, Alberta, BC ...................................................................................................................................................... 45
CHAPTER 4: Policies and Services in Alberta and British Columbia ............................................................................. 47
Provincial Contrast? .......................................................................................................................................................................... 47
Enforcement and Decriminalization ................................................................................................................................................ 47
‘Safer Supply’ and Harm Reduction ............................................................................................................................................... 48
Recovery ............................................................................................................................................................................................ 50
Services .............................................................................................................................................................................................. 50
Supervised Consumption Sites ................................................................................................................................................. 50
Rehabilitation ..................................................................................................................................................................................... 52
Naloxone ............................................................................................................................................................................................. 54
12
Opioid Agonist Treatment ................................................................................................................................................................ 55
Technology ........................................................................................................................................................................................ 56
Summary ............................................................................................................................................................................................ 57
CONCLUSIONS .................................................................................................................................................................. 58
Alberta and BC .................................................................................................................................................................................. 58
Policy Recommendations................................................................................................................................................................. 61
Bibliography ...................................................................................................................................................................... 63
Appendix A: Calculations for COVID-19 and Opioid Life Years Lost, 2020-2021 .......................................................... 72
COVID-19 ........................................................................................................................................................................................... 72
Opioids ................................................................................................................................................................................................ 73
Appendix B: Estimating Drug User Population based on CADs data ............................................................................. 74
Appendix C: Terminology for Different Indigenous Groups in Canada ......................................................................... 75
Appendix D: Drivers of the Opioid Crisis ......................................................................................................................... 76
Increased Toxicity ............................................................................................................................................................................. 78
Improved Product ............................................................................................................................................................................. 79
Policing and Enforcement ................................................................................................................................................................ 80
Prescribing and Dispensation ......................................................................................................................................................... 82
Technology ........................................................................................................................................................................................ 83
Point of Entry ..................................................................................................................................................................................... 84
Criminal Networks ............................................................................................................................................................................. 85
Immigration ........................................................................................................................................................................................ 86
Gender/Age ........................................................................................................................................................................................ 87
13
Income and Inequality ...................................................................................................................................................................... 88
Housing and Homelessness ............................................................................................................................................................ 89
Ethnicity .............................................................................................................................................................................................. 90
Marriage Rates .................................................................................................................................................................................. 91
Drug Culture and Stigma ................................................................................................................................................................. 92
Physical and Mental Health ............................................................................................................................................................. 93
Driver Summary ................................................................................................................................................................................ 94
14
Foreword
The United States and Canada continue to experience high rates of opioid-related mortality and other harms associated
with opioid and drug misuse. As neighbouring jurisdictions, these two countries have faced similar challenges in respect of
over-prescribing of opioids, and the problematic impact of new illicit substances in the community, such as fentanyl.
Canada’s opioid addiction crisis has been mounting for two decades, and the COVID-19 pandemic has exacerbated the
health harms, with rates of drug mortality in areas like Greater Vancouver in 2022 as high as the worst affected parts of the
USA. Despite very different healthcare models, both countries have endured a level of adverse population impact from
drug addiction that has not been experienced in other developed nations.
Two decades ago, the City of Vancouver in British Columbia set out their four-pillar strategy (harm reduction, prevention,
treatment and enforcement) to address drug addiction and associated challenges, and the province has attempted to be a
leader in how it innovates to respond to the evolving crisis ever since. It was outside the scope of this project to evaluate
the efficacy of interventions over that period, but nonetheless a clear conclusion is that the collective impact of drug harms
has significantly increased since that comprehensive strategy was announced.
More recently, opioid addiction was declared a ‘public health emergency’ in BC in 2016, and although the nature of the
problem remains essentially unchanged, interventions since that time to address the challenge have not reduced the
societal impact in communities. Judged only by one key metric, the scale of the harms to individuals in BC has actually
grown significantly – with the number of deaths doubling by 2022 compared to when the emergency was first declared.
Drug policy failure doesn’t just harm people who use drugs. The collateral consequences are myriad, and include crime,
family violence and divorce, community disorder, degraded public spaces, lost business investment, and depressed tax
revenue. As such, the wider public is entitled to challenge public health and safety approaches that policymakers have
adopted if they appear to be limited in impact, or potentially exacerbating the problem.
A generalised commitment to ‘harm reduction’ predominates in Canada, and as such, key metrics are viewed more
narrowly as a collection of statistics referring to negative outcomes and harms experienced by individuals who use drugs.
This makes the wider societal impact of drug addiction and the harm reduction policies adopted in response to it, much
harder to track.
15
For example, the evidence base in criminology is clear that addiction drives much offending behaviour, and that a minority
of offenders are responsible for a disproportionate amount of crime, but rarely does research attempt to quantify the
public impact and cost of elevated crime levels associated with drug-addicted offenders or the continuation of addiction in
these populations.
A narrow focus on ‘harm’ to the individual user also provides no framework for measuring success in line with what the
relatives or friends of those suffering from drug addiction might want as an outcome for their own loved one – that is, to
escape addiction and to desist from behaviour that may lead to premature death.
There is an emerging perception in the media and public debate that the strategies adopted in Canada to address the
problem have not yielded sustained improvements across a range of key metrics. The result has been an increase in
public concern and political attention on the issue, and there is a renewed debate about the merits of different policy
responses in Canada.
In recent months, the salience of this issue has increased, with both BC and Alberta seeking to justify and promote their
respective approaches and their record to date. There is however an ongoing lack of good data on key outcomes and
even a consensus on what success would look like in this policy arena.
There is a general acceptance that the harms inflicted by drug misuse, combined with mental health and homelessness,
are ‘wicked’ problems requiring complex and multi-layered responses. In this respect, drug addiction and its
consequences are re-emerging as a key test of the effectiveness of evidence-based urban policymaking in cities across
North America. What can the situation in two of Canada’s worst affected provinces teach us?
The concentration of this crisis in Western Canada is clear, with BC and Alberta comprising half (49%) of all opioid-
overdose deaths in 2022. Below the provincial level, there is a further geographic concentration in major urban areas,
even if victims of opioid overdoses can be found in small towns and rural communities all across Canada. There is also a
strong perception that BC’s crisis is highly concentrated not just in one city (Vancouver), but in one neighbourhood of that
one city centre – the Downtown Eastside.
In Canada more generally, attention of politicians has tended to be dominated by a range of policy and legislative
responses focused on drug users – rather than drug markets or suppliers – that are intended to reduce infectious disease
acquisition, accidental deaths and overdoses. In addition, there has been new steps taken in recent months to further
16
reduce ‘stigma’, including the enactment of decriminalisation of drug possession in British Columbia. This is the first time
that anywhere in Canada has adopted an approach pioneered in just a few other jurisdictions, most famously by Portugal.
This research project, commissioned in Fall 2022, is designed to give an overview of the current drug addiction crisis in
Canada, with a special focus on two neighbouring provinces – British Columbia and Alberta – and to describe its key
features. The goal of the project was to outline the scale and nature of the drug harms affecting these two provinces, to
outline the policy approaches adopted by both provincial governments, and to explore the most likely drivers of the high
death and hospitalisation rates.
It was outside the scope of this report to evaluate the efficacy of different policy responses adopted by each province, or
to make recommendations for how policymakers in both places might respond. Our recommendations – outlined in the
Conclusion – are restricted to those that arise from the research undertaken and relate to how the response to the
challenge might be understood and evaluated more effectively in future.
In terms of years of productive life lost, the sheer scale of the drug addiction challenge makes it the most critical health
crisis for Canada. It demands a sober, non-ideological assessment of what policy responses are working, which
interventions are worth trialing, and how we should judge success when it comes to public policy around drug addiction.
This report provides a summary of where we begin in pursuing answers to those critical questions.

17
Introduction
Canada is in the midst of an opioid overdose crisis.
Though there is not reliable country-wide data on
overdose harms dating back further than 2016, British
Columbia’s death rate due to illicit drugs rose from 5.8
per 100,000 in 2000 to 44.2 per 100,000 in 2021.
1
This is
comparable to some of the worst affected states in the
US. In Canada, the number of accidental apparent opioid
toxicity deaths (AAOTDs) per 100,000 was 20.2 per
100,000 in 2021.
2
For comparison, in 2019, England and
Wales had a drug-related mortality rate of 7.7 per
100,000,
3
and in 2020 the European Union had a drug-
induced mortality rate of 1.5 per 100,000.
4
1
Illicit Drug Toxicity Deaths in BC: January 1, 2012—December 31,
2022. (2022). British Columbia Coroners Service.
2
Opioid- and stimulant-related harms. (2022). Government of
Canada.
* All countries other than Canada measure total drug-related mortality
Fig. 1. Data sourced from the BC Centers for Disease Control (2023), Office
of National Statistics (2020), Government of Canada (2022) and European
Monitoring Centre for Drugs and Drug Addiction (2022).
3
Deaths related to drug poisoning in England and Wales. (2020).
Office for National Statistics.
4
Frequently asked questions (FAQ): Drug overdose deaths in
Europe. (2022). European Monitoring Centre for Drugs and Drug
Addiction.
0
5
10
15
20
25
30
2000
2002
2004
2006
2008
2010
2012
2014
2016
2018
2020
Deaths per 100,000
Opioid Overdose Deaths* in Canada
compared to select jurisdictions
USA Canada European Union England and Wales
18
The only G7 country that has a similar rate of overdose
deaths is the United which had 25.4 drug overdose
deaths per 100,000 in 2020 (age-adjusted rate).
5
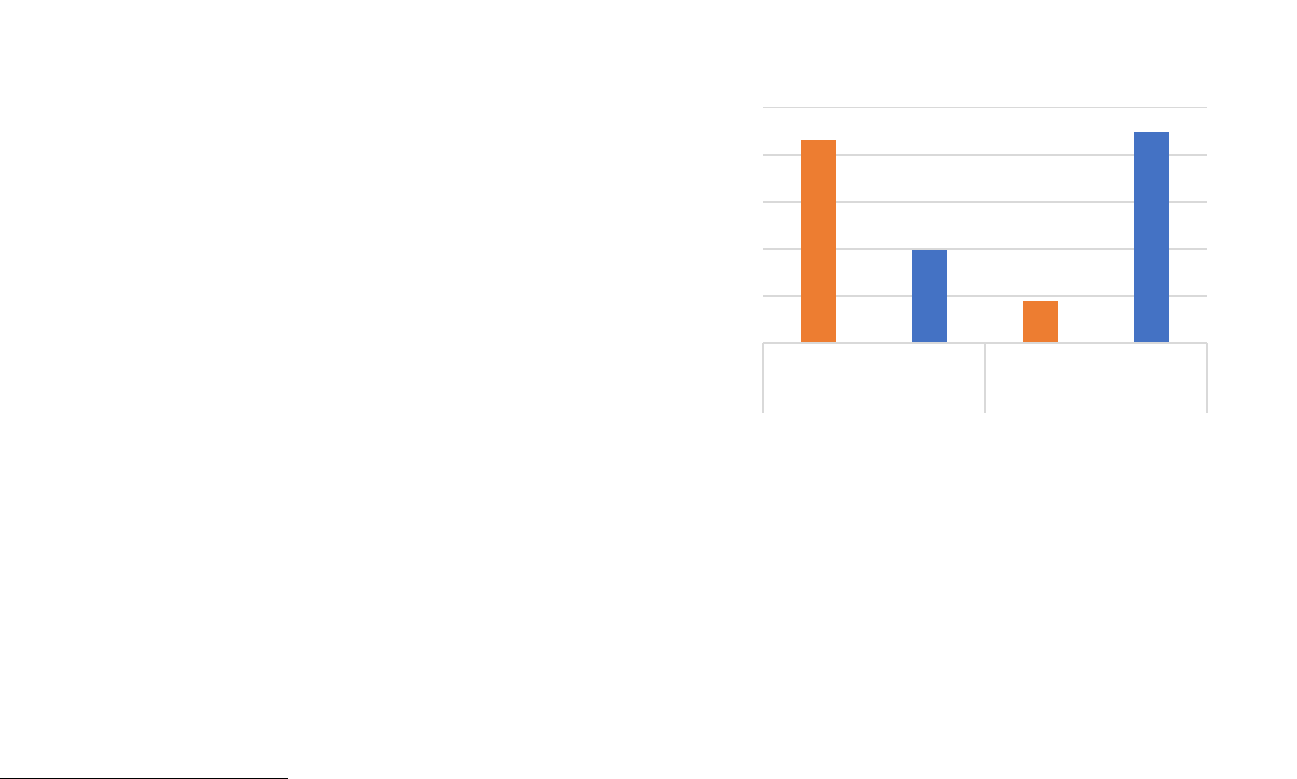
In 2020 and 2021, there were 13,815 deaths attributed to
accidental opioid poisoning in Canada.
6
This is almost half
the death toll that COVID-19 had over the same period
(29,985).
7
Considering the relative ages of those killed,
however, the opioid crisis has caused a far greater loss in
years of life. COVID-19 caused approximately 90,000 lost
years of life in 2020 and 2021.
8
Over that same period,
opioids caused nearly 450,000 lost years of life (see
appendix A).
9
5
CDC Wonder. (2023). CDC Centers for Disease Control and
Prevention.
6
Opioid- and stimulant-related harms. (2022). Government of
Canada.
7
COVID-19 daily epidemiology update. (2020). Public Health Agency
of Canada.
Fig. 2. Data sourced from Government of Canada (2022) and Public Health
Agency of Canada (2022).
The crisis has gotten so severe that it halted the increase
in Canadian life expectancy between 2016 and 2017, the
first time that Canadian life expectancy has decreased in
over four decades.
10
8
COVID-19 daily epidemiology update. (2020). Public Health Agency
of Canada.
9
Opioid- and stimulant-related harms. (2022). Government of
Canada.
10
Changes in life expectancy by selected causes of death, 2017.
(2019).
0
100,000
200,000
300,000
400,000
500,000
0
7,000
14,000
21,000
28,000
35,000
COVID-19 Opioids COVID-19 Opioids
Deaths Life Years Lost
Life-years lost - COVID-19 vs.
Accidental Opioid-Related Overdoses

19
32%
22%
46%
28%
21%
51%
Alberta and BC's Share of Canada's
AAOTDs, 2016 and 2021
BC Alberta Other Provinces and Territories
Addressing opioid addiction in BC and Alberta
Though opioid overdose deaths have been increasing
across the country, they have been most concentrated in
BC, Alberta, and Ontario. BC’s AAOTD rate in 2021 was
more than double the national average, and Alberta was
not far behind at 36 per 100,000. Ontario had the most
total AAOTDs (2,772) but had a lower death rate of 19.4
per 100,000. Between them, BC and Alberta accounted
for only 25% of the population but 49% of AATODs
(3,804). To put this another way, 1 in very 7 Canadians
live in BC and 1 in every 9 live in Alberta, but 1 in every 4
AAOTD in 2021 was a British Columbian and 1 in every 5
is an Albertan. The share of AAOTDs held by Alberta and
BC has actually decreased slightly from 54% in 2016.
11
In response to the crisis, both BC and Alberta have made
new investments in addiction services. BC’s 2021 budget
earmarked $0.5 billion for mental health and addiction
services over the next three years
12
and its 2023 budget
marked over a billion
13
, while Alberta’s 2022 budget
included $1 billion for addiction and mental health care
with an additional $60 million over three years to build a
recovery-oriented system of care.
14
11
Opioid- and stimulant-related harms. (2022). Government of
Canada.
12
Grochowski, S. (2021). B.C. announces historic half-billion-dollar
funding for overdose crisis, mental health. Maple Ridge - Pitt
Meadows News.
Fig. 3. Data sourced from Government of Canada (2022).
In recent months, certain policy differences between
Alberta and BC have become politically salient in Canada.
This report found there to be similarities between the two
provinces’ strategies, but also significant differences.
Both provinces support harm reduction activity such as
Naloxone distribution to emergency services and
community providers, syringe exchange programs, and
licenced overdose prevention provision (SCS) in multiple
locations to provide drug users with a safer, regulated
environment to consume. Each province has also shifted
away from police enforcement against drug possession
13
More than $1B announced for mental health, addictions support in
2023. (2023). CBC.
14
Toward an Alberta model of wellness. (2022). Government of
Alberta.
2016
2021

20
and towards diversion to treatment and education for
drug users.
BC’s approach places a stronger emphasis on stigma
reduction and decimalization, with a greater policy focus
on harm reduction, conceptualised as overdose
prevention and access to safer supply (i.e., prescribed
medical alternatives to toxic illegal drugs) including
through automated dispensing. In addition, BC has with
federal consent – as of 31 January 2023 – removed
criminal penalties for possession of illicit drugs.
15
Alberta,
in contrast is pursuing a ‘recovery-oriented system of
care’
16
and has emphasized the importance of community
support, treatment pathways, and more regulation over
and higher standards for SCS.
17
There also appears to be
a generally higher rate of enforcement against drug
trafficking, production, and distribution in Alberta,
although arrest rates for possession have dropped in both
provinces in the last decade.
Alberta and BC are relatively similar geographically and
culturally, are approximately equal in population, and the
factors driving their respective opioid crises seem
comparable. This makes them interesting neighbours for
a jurisdictional comparison; however, the difference in
policy approach is still developing. In time, the outcomes
achieved in AB and BC will provide an important
15
Judd, A., & Zussman, R. (2022, May 31). B.C. becomes first
province to remove criminal penalties for possession of some hard
drugs. Global News.
dimension to the political debate over the right response
to the problem Canada-wide. For now, it is too soon to
analyse the relative progress of each province as it
attempts to address opioid harms; nevertheless, this
report will draw attention to some key differences that
should be monitored going forward.
16
Toward an Alberta model of wellness. (2022). Government of
Alberta.
17
Impact: A Socio-Economic Review of Supervised Consumption
Sites in Alberta. (2020). Government of Alberta.

21
CHAPTER 1: Defining the Problem
In considering the current state of Canada’s opioid crisis,
for this chapter we summarise the role of opioids in
society, and how they may cause harms, either in
isolation, or in conjunction with other addictive
substances.
Opioids: their function and role
Opioids are a group of analgesic (pain relieving) drugs
commonly used in clinical practice. In addition to
providing pain relief, opioids trigger the release of
endorphins, reducing an individual’s perception of pain
and creating feelings of pleasure. Importantly, opioids
also slow multiple biological functions, including
breathing, which is why they can be fatal.
Opioids are used in both legal and illegal contexts. Legal
opioid use is restricted to medical contexts in Canada, as
it is in most countries, and a range of licensed medical
products contain opioids. Individuals may also use
opioids illegally for purposes of managing physical or
psychological pain or for the pleasurable affects of the
drug itself. People can also combine their use of
18
Felbab-Brown, V. (2020). Fentanyl and Geopolitics. Brookings
Institution.
19
Fentanyl Facts. (2022, February 23). Centers for Disease Control
and Prevention.
prescription opioids with other addictive substances or
opioids sourced from the illicit market.
Though certain opioids are primarily used in an illegal
context (e.g., heroin), for many types there is no chemical
difference between the substance being used in legal and
illegal contexts (e.g., fentanyl). Sometimes drugs may
even be sourced from the same production facilities.
18
Some types of opioids are more potent than others.
Fentanyl is a synthetic opioid that can be up to 50 times
stronger than heroin and 100 times stronger than
morphine.
19
Fentanyl and its analogues have played an
important role in the opioid crisis because they are
significantly cheaper to produce per dose. This makes
them more widespread in illicit drug markets, but it is also
more likely that a dose will be too potent and cause
people who use these drugs to overdose.
There are drugs in Canada that kill more people per year
than opioids. Purely in terms of deaths, the two most
lethal substances in the country are alcohol and
tobacco.
20
20
Canadian Substance Use Costs and Harms. (2020). Canadian
Centre on Substance Use and Addiction.

22
Fig. 4. Data sourced from Canadian Centre on Substance Use and Addiction
(2020).
Nonetheless, those who overdose on opioids are usually
far younger than those who die of alcohol or tobacco,
because the chronic health impacts of alcohol or tobacco
consumption manifest over decades of use. Opioids are
responsible for more life years lost than tobacco, and
nearly as many life years lost as alcohol, despite not
having the same level of general use in the population.
21
21
Canadian Substance Use Costs and Harms. (2020). Canadian
Centre on Substance Use and Addiction.
* Productive Life Years lost defined as years lost before the age of 65
Fig. 5. Data sourced from Canadian Centre on Substance Use and Addiction
(2020).
Benefits and Harms
Like many other drugs in modern society, opioids can be
both beneficial and harmful. They are a valuable tool for
the management of acute and chronic pain, and have
clear clinical efficacy and well-established prescribing
guidelines for use. At the same time, opioids are an
addictive substance, and rapid expansion of prescribing
by the medical profession occurred before some of the
0
10,000
20,000
30,000
40,000
50,000
60,000
2015 2016 2017 2015 2016 2017 2015 2016 2017
Alcohol Tobacco Opioids
Deaths by Substance Type, 2015-2017
0
20,000
40,000
60,000
80,000
100,000
120,000
2015 2016 2017 2015 2016 2017 2015 2016 2017
Alcohol Tobacco Opioids
Productive Life Years* Lost by
Substance Type, 2015-2017

23
risks of addiction were properly understood. When
someone takes opioids, their body can become
dependent, making it more challenging to desist, or to
reduce their use of the drug over time. Taking too strong
a dose can have immediate, negative health
consequences, up to and including death.
The policy debate about addiction is complicated by the
nature of the behaviour. Unlike most other illnesses or
adverse health conditions (e.g., cancer), opioid addiction
makes users complicit in their own injury, and unlike most
diseases, subjects do derive some enjoyment from the
use of opioids, which acts as a strong incentive to
continue using.
22
The debate over how to address drug addiction of all
kinds is a legitimate matter of public policy because of the
harms suffered by users, but also because of the wider
societal impact of the behaviour. Opioid use may not only
be harmful to the person themselves – impacting their
employability, housing, and relationships with dependents
– but can also cause harm to those around them. Friends
and family may struggle to help users manage their
addiction, addicts may resort to theft or fraud to sustain
their addiction, children may suffer neglect or separation,
and the broader public may suffer from the crime and
disorder impact of drug addicted populations, including
degradation of the public realm and drug paraphernalia
22
Humphreys, K. (2022). Testimony to the Oregon Senate
Committee on Judiciary and Ballot Measure 100 Implementation.
proliferating in parks or other public spaces. These
broader societal impacts can be exacerbated if drug
using populations are concentrated in certain urban
neighbourhoods where their behaviour is highly visible
and especially when combined with open drug markets
and street dealing of illicit drugs.
Risk and Context
Risk of harm from opioids is highly dependent on why
and how opioids are acquired. The safest context for
mitigating the risks associated with opioids is when they
are used for medical purposes for in-hospital treatment.
The patient does not have unsupervised access to
opioids, the opioids are unlikely to be diverted to an
unintended recipient, and the treatment is closely
monitored and is usually time-limited.

24
Risk contexts for opioid use
Fig. 6. Risk is an interaction between Why and How.

25
Despite being one of the largest consumers of opioids in
the world, Germany has relatively low overdose rates,
and this has been attributed to the fact that opioids are
primarily prescribed in-hospital and in other 24-hour care
settings.
23
Opioids prescribed by medical practitioners are also
relatively low risk. The majority of people who are
prescribed opioids use them for their intended purpose,
and benefit from the resulting pain relief; however, the
opioid crisis in the USA and Canada had its origins in the
over-prescribing of regulated opioid treatments. The
lower the threshold for opioid prescriptions, the greater
the risk for the recipient and those around them.
It is significantly riskier to use opioids for pleasure, even if
the opioids being used are prescription opioids. Like
many other substances (alcohol, cannabis, nicotine),
opioid use carries a number of potential health
implications, such as addiction, liver damage, and
overdoses. The risk of using opioids for pleasure goes up
considerably if the opioids are diverted from an intended
recipient or otherwise acquired via the illicit market or
other unregulated source, where dosage and purity are
not controlled or guaranteed. Self-medicating, either with
diverted prescriptions or illegally sourced substances, is
risky for these same reasons.
23
Felbab-Brown, K. H., Jonathan P. Caulkins, and Vanda. (2020).
What the US and Canada can learn from other countries to combat
the opioid crisis [Brookings].

26
CHAPTER 2: History of Canada’s Health Crisis
Overview
Canada’s opioid addiction crisis can be traced back two decades, and divides into four successive waves, each
representing a significant transition or evolution with an escalation of harms each time. The opioid crisis in the United
States has followed a similar trajectory, and has been included in the below table for comparison. Note that these phases
are a useful heuristic, rather than definitive and discrete categories.
Fig. 7. Data sourced from CDC Centers for Disease Control (2023), Government of Canada (2022), and BC Coroners Service (2022).

27
Wave 1 (1980s – 2010)
The reason that Canada and the USA have such
significant levels of opioid harms compared to other
countries has its origins in their relatively high
consumption of prescription opioids. Though
consumption has decreased in recent years, Canada was
once the second-largest consumer of opioids in the
world.
24
Currently, Canada is the fourth largest per-capita
consumer of controlled opioids, behind only Germany,
Iceland, and the USA.
25
This disproportionate consumption of opioids began as
far back as the 1980s, when opioid manufacturers began
campaigning for the increased utilization of opioids in
healthcare.
26
Since the 1980s, the volume of opioids sold
to hospitals and to pharmacies for prescription increased
by more than 3,000%.
27
As controlled opioid consumption
increased, so did the misuse of opioids. Patients either
used prescriptions for non-medical purposes, or
prescriptions were diverted from their intended
24
Lisa, B., & Jessica, H. (2018). Evidence synthesis - The opioid crisis
in Canada: A national perspective. Health Promotion and Chronic
Disease Prevention in Canada : Research, Policy and Practice, 38(6),
224–233.
25
Richards, G. C., Aronson, J. K., Mahtani, K. R., & Heneghan, C.
(2022). Global, regional, and national consumption of controlled
opioids: A cross-sectional study of 214 countries and non-
metropolitan territories. British Journal of Pain, 16(1), 34–40.
recipients. This was the first wave of the opioid crisis in
Canada and the USA.
It was during this period, in 2001, that Vancouver
implemented its four-pillar drug strategy of Prevention,
Treatment, Enforcement, and Harm Reduction, which
guided the approach in the early stages of what would
later become a much more serious public health crisis.
28
Wave 2 (2010 – 2014)
The first wave resulted in a large base of opioid users in
the general population, even if the majority were not
suffering from addiction or abusing other substances. The
second wave was characterized by the rise of
unregulated opioids from the illicit market, as dealers
responded to the demand for cheap and potent opioids
such as heroin and began to expand distribution.
This trend may have been encouraged by measures
taken by health authorities in Canada and the USA to limit
the supply of medical opioids and tackle over-prescribing
by some clinicians in an effort to reduce the number of
26
Meldrum, M. L. (2016). The Ongoing Opioid Prescription Epidemic:
Historical Context. American Journal of Public Health, 106(8), 1365–
1366.
27
Lisa, B., & Jessica, H. (2018). Evidence synthesis - The opioid crisis
in Canada: A national perspective. Health Promotion and Chronic
Disease Prevention in Canada : Research, Policy and Practice, 38(6),
224–233.
28
Framework for Action: A Four Pillar Approach to Vancouver’s Drug
Problems. (2001). City of Vancouver.
28
people becoming addicted. According to one source,
medical opioid consumption in Canada declined by
36.8% between 2009 and 2019.
29
Though this drop in
medical opioid consumption may have reduced the
number of people suffering addiction for the first time, it
may also have pushed existing dependent users to seek
out riskier alternatives. This likely consequence was
acknowledged at the time and became part of the policy
response to over-prescribing.
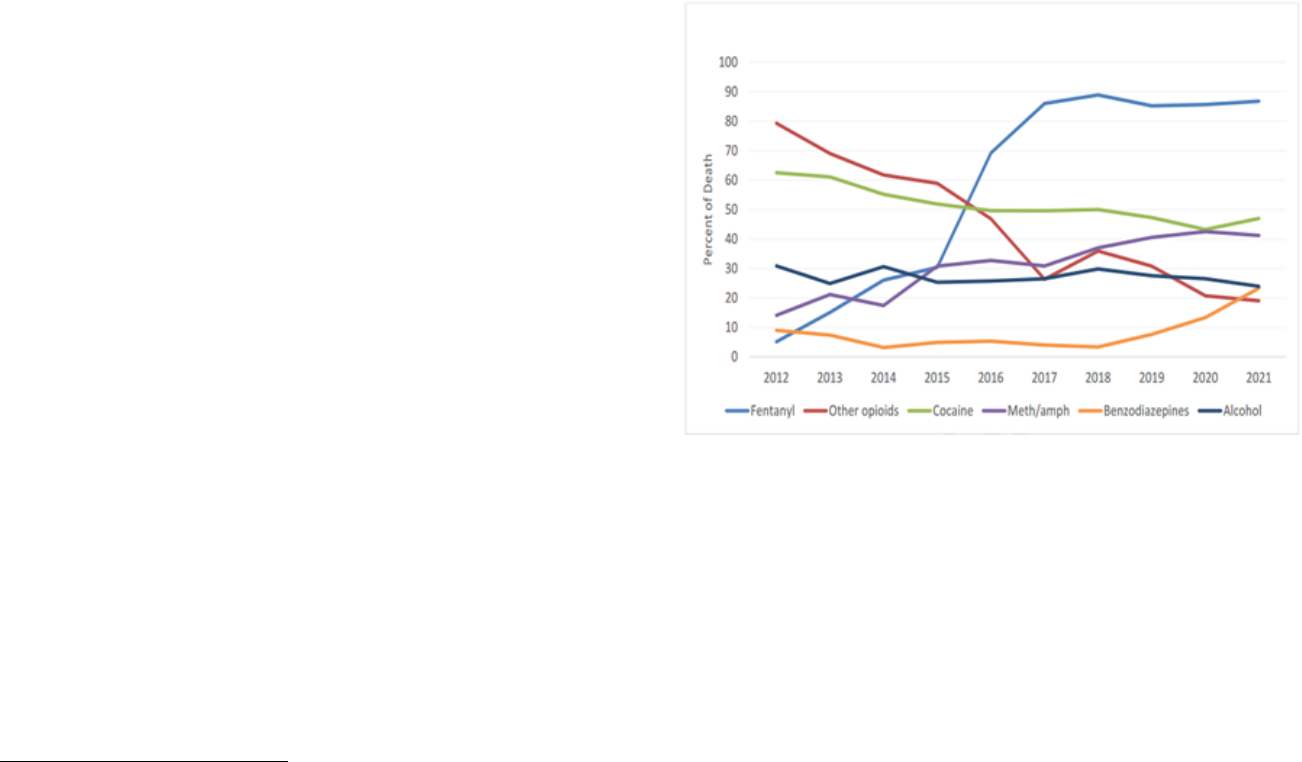
Wave 3 (2014-2019)
The second wave began transitioning into the third wave
as the toxicity of the drugs in the illegal market began to
increase, with deaths rising accordingly. In BC, in 2012,
fentanyl – at that time, the most potent opioid in
circulation – was detected in about 5% of all illicit drug
toxicity deaths. BC Coroners’ Service data shows the
rapid increase in subsequent years, with a sustained rise
in fentanyl detection among deaths over the past
decade).
30
When considered in tandem with the rise of deaths in BC
(see below) it is difficult to dispute that the increased
availability of fentanyl has resulted in a significant
increase in fentanyl consumption and fentanyl-related
29
Jayawardana, S., Forman, R., Johnston-Webber, C., Campbell, A.,
Berterame, S., Joncheere, C. de, Aitken, M., & Mossialos, E. (2021).
Global consumption of prescription opioid analgesics between 2009-
2019: A country-level observational study. EClinicalMedicine, 42.
deaths. More evidence regarding the role of fentanyl is
reviewed in section 4.
Fig. 8. Drug Types Relevant to Death, 2012-2021. From Illicit Drug Toxicity
Deaths in BC: January 1, 2012—October 31, 2022. (2022). British Columbia
Coroners Service.
It is unclear why deaths dropped between 2018 and
2019. One possibility is that use declined because supply
was restricted due to regulatory changes in China that
banned the production and sale of some types of fentanyl
without a license.
31
However, the decline in deaths would
soon reverse.
30
Illicit Drug Toxicity Deaths in BC: January 1, 2012—October 31,
2022. (2022). British Columbia Coroners Service.
31
Felbab-Brown, V. (2020). Fentanyl and Geopolitics. Brookings
Institution.
Drug Types Relevant to Death in BC, 2012-2021

29
It was in 2016 that the provincial government in BC
declared a state of medical emergency regarding drug
toxicity deaths, and greater political attention on the issue
and government funding began.
32
Wave 4 (2020 – Present)
With the onset of the COVID-19 pandemic, the number of
AAOTDs in Canada began to increase again, reaching
their highest levels ever in 2021. The rise in AAOTDs
would have been caused by a confluence of factors, but
three of what are likely the most prominent drivers are
listed below.
First, social distancing and isolation would facilitate a
riskier environment for drug use. As will be discussed in
section 4, most AAOTDs happen while someone is alone
in a private residence.
Second, the stress of the pandemic caused increase drug
use. Surveys conducted by the Canadian Centre on
Substance Use found that drug users, particularly those
with a history of substance use disorder, reported
32
Provincial health officer declares public health emergency. (2016).
Government of British Columbia.
33
Mental Health and Substance Use During COVID-19. (2023).
Canadian Centre on Substance Use and Addiction.
34
Moallef, S., DeBeck, K., Fairbairn, N., Cui, Z., Brar, R., Wilson, D.,
Johnson, C., Milloy, M.-J., & Hayashi, K. (2022). Inability to contact
increased stress and substance use with the onset of the
COVID-19 pandemic.
33
Third, some health and treatment services were more
difficult to access throughout the pandemic. For example,
one study found that many users had difficulty accessing
their prescriber to access Opioid Agonist Therapy (OAT)
medication.
34
What Comes Next?
Across Canada, AAOTDs have fallen from their record
2021 high, but not by much. Both BC and Alberta are
now making significant investments in tackling the crisis.
In the next section, we will review data on the current
state of the crisis in Canada overall, and then the two
worst affected provinces of Alberta and British Columbia.
opioid agonist therapy prescribers during the COVID-19 pandemic in
a Canadian setting: A cross-sectional analysis among people on
opioid agonist therapy. Addiction Science & Clinical Practice, 17(1),
73.
Illicit Drug Toxicity Deaths by Year in BC
2012
2013
2014
2015
2016
2017
2018
2019
2020
2021
270
334
369
529
994
1495
1562
987
1774
2306

30
CHAPTER 3: Data
This project describes the current state of Canada’s
opioid crisis based on quantitative analysis of official
(federal and provincial) data sources. Some municipal
data sources also exist, but they are not widespread and
are not recorded with standardised definitions or to the
same level of assurance.
Deaths, Hospitalizations and EMS
Canada-wide data regarding opioid-related deaths and
hospitalization only begins in 2016. British Columbia does
publish data regarding illicit drug toxicity deaths going as
far back as 1996, but there is not comparable historical
data from other provinces (see fig. 7, pg. 26). To facilitate
comparisons between Canada-wide and BC data, this
report will primarily refer to accidental apparent opioid
toxicity deaths (AAOTDs), which excludes suicides. This
does not significantly impact the analysis because
intentional opioid toxicity deaths represent only a small
portion of all opioid toxicity deaths. In 2021, only 3% (268
out of 7993) of all apparent opioid toxicity deaths were
identified as non-accidental.
35
35
Opioid- and stimulant-related harms. (2022). Government of
Canada.
36
Opioid- and stimulant-related harms. (2022). Government of
Canada.
37
Population and dwelling counts: Canada, provinces and territories.
(2022). Statistics Canada.
The health crisis of drug addiction in Canada is
concentrated in BC, Alberta and Ontario. In 2021, there
were 7,725 AAOTDs in Canada. 49% of those deaths
(3,804)
36
occurred in Alberta and BC, despite the two
provinces representing only 25% of Canada’s
population.
37
Ontario had the highest number of AAOTDs
(2,772), but had a comparably low death rate of 19.4 per
100,000 compared to Alberta’s 36.2 and BC’s 41.9.
38
The
Yukon technically had the highest AAOTD rate at 53.2
per 100,000, but due to its low population this
represented a total of only 23 deaths.
39
38
Opioid- and stimulant-related harms. (2022). Government of
Canada.
39
Opioid- and stimulant-related harms. (2022). Government of
Canada.

31
Fig. 9. Data sourced from Government of Canada (2022)
Hospitalization and EMS rates followed a similar trend. Of
the 4,433-accidental opioid-related poisoning
hospitalizations (AOPHs) in Canada, 2,351 (53%) of them
occurred in Alberta and BC.
40
Looking at ambulance data, the impact on emergency
dispatch caseloads from the addiction crisis is much
higher in BC. Emergency Medical Service (EMS)
responses to suspected opioid-related overdoses are
highest in BC (24,152 responses) – three times the
volume of such incidents in Alberta (8,215 responses),
41
40
Opioid- and stimulant-related harms. (2022). Government of
Canada.
Fig. 10. Data sourced from Government of Canada (2022).
though not all provinces shared EMS data and EMS
responses will be highly impacted by provincial
infrastructure.
Population of People who Use Illegal
Substances in Canada
It is important to assess opioid harms against the
estimated population of people who use substances. The
best source of data to estimate such figures in Canada is
the Canadian Alcohol and Drugs Survey (CADS), a
biennial general population survey of alcohol and drug
use amongst Canadians 15 and older. The CADS breaks
down drug use in several ways. For the purposes of this
41
Opioid- and stimulant-related harms. (2022). Government of
Canada.

32
report, population estimates are based on the ‘illegal drug
use, any of 5 drugs’
42
category for 2013, 2015 and 2017
data, and the ‘any of 6 drugs’
43
category for 2019 data
(see appendix B for details).
Any of 5 drugs:
2013, 2015, 2017
Cocaine/crack, speed/methamphetamine/crystal
meth ecstasy, hallucinogens (excluding salvia), and
heroin
Any of 6 drugs:
2019
Cocaine/crack, speed/methamphetamine, ecstasy,
hallucinogens, heroin, salvia
Based on the CADS figures, in 2019 16.1% of Canadians
(c.5 million people) had used at least one of the 6 select
drugs in their lifetime, while 3.5% had used at least one in
the past year (c.1 million). Prevalence of use was highest
in Alberta and BC, the two provinces who had the highest
percentage of past-year users, with 4.8% (170,800) of
Albertans and 3.8% (157,300) of British Columbians
having used at least one of the drugs in the past year.
44
45
Use of at least one of six illegal drugs, 2019
Canada
Alberta
BC
Past year
3.5%
4.8%
3.8%
Lifetime
16.1%
18.0%
17.8%
* Any of 6 drugs in 2019
42
Cocaine/crack, speed/methamphetamine/crystal meth, ecstasy,
hallucinogens (excluding salvia), and heroin
43
Cocaine/crack, speed/methamphetamine, ecstasy, hallucinogens,
heroin, salvia
44
Canadian Alcohol and Drugs Survey (CADS): 2019 detailed tables.
(2021). Government of Canada.
** No data was available for BC in 2017
Fig. 11. Data sourced from Government of Canada (2021).
Past year drug use appeared to increase between 2013
and 2019 in Canada and Alberta. The number of lifetime
users appeared to drop between 2017 and 2019 in
Canada, Alberta, and BC,
46
but this may be attributable to
changes in the survey.
45
Due to sample size, it cannot confidently be said that past year
drug use was higher in Alberta and lower in BC in 2019 (the only
year for which confidence intervals were provided).
46
Canadian Alcohol and Drugs Survey (CADS): 2019 detailed tables.
(2021). Government of Canada.
0
2
4
6
2013 2015 2017 2019*
Percentage of past year users,
any of 5* drugs
Canada Alberta British Columbia

33
* Any of 6 drugs in 2019.
Fig. 12. Data sourced from Government of Canada (2021).
Fentanyl and Overdose Deaths
The single most significant factor that seems to affect the
number of people dying due to drug overdoses across
Canada’s provinces is the degree to which fentanyl is
present in the drug supply. Based on data from Health
Canada’s Drug Analysis Service (DAS), which identifies
substances contained in samples seized by law
enforcement, fentanyl was detected much more
47
Adulterants, Contaminants and Co-occurring Substances in Drugs
on the Illegal Market in Canada. (2020). Canadian Centre on
Substance Use and Addiction.
48
Substance use surveillance data. (2023). Government of Alberta.
frequently in Western Canada than in Eastern Canada.
47
The table below compares the rate of fentanyl detected in
seized samples in different regions and their respective
AAOTD death rate.
In Alberta, in 2021, fentanyl was detected in 81% of all
accidental drug poisoning deaths.
48
In BC, between 2019
and 2022, fentanyl was detected in 85% of all illicit
overdose deaths.
49
Further, fentanyl detection in BC has
risen in tandem with the death rate (see fig. 8, pg. 28).
50
When considered with the previously reviewed CADS
data, it appears the increase in opioid-related harms in
Canada are driven by the increased toxicity of the supply,
rather than an increase in the number of drug users in the
general population.
49
Illicit Drug Toxicity Deaths in BC: January 1, 2012—October 31,
2022. (2022). British Columbia Coroners Service.
50
Illicit Drug Toxicity Deaths in BC: January 1, 2012—October 31,
2022. (2022). British Columbia Coroners Service.
0
5
10
15
20
25
30
2013 2015 2017 2019*
Percentage of lifetime users, any of 5*
drugs
Canada Alberta British Columbia
Region (2021)
Canada
BC
Ontario
Quebec
Fentanyl
detection
69%
91%
55%
14%
Deaths per
100,000
20.2
42.2
18.7
5.2

34
Policing and Criminal Justice
Illicit drug markets are a key aspect of the addiction crisis
in Canada, being responsible for the supply of
unregulated opioids into communities and with criminals
based in Canada and those overseas exploiting users
suffering addiction. Organised crime understands that
addiction makes their ‘customers’ desperate to maintain
access to drugs, even if this means buying them illegally
from street dealers, or becoming indebted to them. As
the opioid crisis has unfolded, enforcement by the police
and prosecutors has continued, but the true picture of
how drug markets are addressed by law enforcement
agencies is difficult to determine.
Canadian criminal justice and policing statistics are not
sufficiently granular to make comparisons between
municipalities on how cases are processed. Data at the
51
Greg Moreau. (2022). Police-reported crime statistics in Canada,
2021. Canadian Centre for Justice and Community Safety Statistics.
provincial level and reported to StatsCan provides a high-
level summary of drug crime across the country, and
incident data is also available for larger census areas.
Police department data (where such city police
departments exist) is not consistent or comparable.
The majority of reported opioid-related offences occur in
BC. In 2021, BC – comprising approximately 13% of
Canada’s population – had nearly half of all police-
reported opioid possession, trafficking, production, and
important/exportation incidents in Canada. BC’s rate of
opioid-related police reported incidents was more than
four times the recorded incident rate in Alberta.
51
Fig. 13. Data sourced from Statistics Canada (2022).
Glossary of Criminal Justice Terminology and Acronyms:
Incident: a set of connected events usually constituting an
occurrence report. An incident may involve
multiple perpetrators and victims.
Charge: When a person is charged, they are formally
accused of committing an offence. Charges are
made on an individual basis.
Convictions: Guilty outcomes in court.
TPD: Trafficking, production, and distribution
586
2,970
5,996
13
57
16
0
10
20
30
40
50
60
0
1,000
2,000
3,000
4,000
5,000
6,000
7,000
Number Rate Number Rate Number Rate
Alberta British Columbia Canada
Rate per 100,000
Number
Police-Reported Opioid-Related Incidents,
Number and Rate per 100,000, 2021

35
Fig. 14. Data sourced from Statistics Canada (2022).
For all drug violations, Vancouver reported 374 incidents
per 100,000 compared to 99 in Edmonton and 162 in
Canada.
52
Enforcement to suppress illicit drug markets and to
address unregulated supply requires police incidents to
result in charges and convictions. Given the high volume
of drug violations in BC, it is noteworthy that charges are
low, and are disconnected from charge rates. Meanwhile
charges for drug-related crimes are much higher in
52
Incident-based crime statistics, by detailed violations, Canada,
provinces, territories, Census Metropolitan Areas and Canadian
Forces Military Police. (2022). Statistics Canada.
Alberta for TPD and increases in charges broadly tracked
the trend in incidents, with rising rates after 2012 and
reductions more recently.
Fig. 15. Data sourced from Statistics Canada (2022).
In BC, drug possession incidents have increased
significantly in the last decade, and TPD incidences have
also spiked after 2016, but charge rates for both
categories have remained broadly flat or even fallen over
the same period.
0
100
200
300
400
500
600
700
800
0
1,500
3,000
4,500
6,000
7,500
9,000
10,500
12,000
Number
Per 100,000
Total
Per 100,000
Total
Per 100,000
Total
Per 100,000
Total
Per 100,000
Vancouver Kelowna Edmonton Calgary Lethbridge
Rate per 100,000
Number
All Drug Incidents,
Select Albertan and BC Cities,
Number and Rate per 100,000, 2021
0
30
60
90
120
2000
2002
2004
2006
2008
2010
2012
2014
2016
2018
2020
Alberta drug incidences vs. charges
(excl. cocaine)
Drug possession, incidences Drug possession, charges
Drug TPD, incidences Drug TPD, charges

36
Fig. 16. Data sourced from Statistics Canada (2022).
For Canada overall, sentencing volumes for drug-related
crime have dropped by over 50% in the past decade.
53
53
Adult criminal courts, guilty cases by type of sentence. (2012).
Statistics Canada.
Fig. 17. Data sourced from Statistics Canada (2022).
Convictions for crime overall in Canada have also
dropped, but not to the same extent, indicating a general
lessening of criminal justice enforcement against drug
offences in Canada during the escalating health crisis of
opioid addiction.
0
30
60
90
120
150
180
2000
2001
2002
2003
2004
2005
2006
2007
2008
2009
2010
2011
2012
2013
2014
2015
2016
2017
2018
2019
2020
2021
BC drug incidences vs. charges (excl.
cocaine)
Drug possession, incidences Drug possession, charges
Drug TPD, incidences Drug TPD, charges
0
2,000
4,000
6,000
8,000
10,000
2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
Guilty Drug Cases in Canada,
Possession and Other
Drug, Possession Drug, Other

37
Fig. 18. Data sourced from Statistics Canada (2022).
Multi-Drug Use
Though fentanyl now dominates drug toxicity deaths in
BC and Alberta, many drug samples were found to
contain other substances, and many of those who died of
overdoses were found to have other substances in their
system.
In their national review of submitted opioid samples,
Health Canada’s Drug Analysis Service found that only
31% contained only opioids. 13% contained other
psychoactive substances, and most samples contained
cutting agents (non-psychoactive adulterants or co-
54
Adulterants, Contaminants and Co-occurring Substances in Drugs
on the Illegal Market in Canada. (2020). Canadian Centre on
Substance Use and Addiction.
occurring substances). In BC, 15% of submitted samples
contained other psychoactive substances, the highest in
the country.
54
In both BC and Alberta, it appeared that drugs other than
fentanyl frequently contributed to the deaths of drug
users. As can be seen in the below table, a significant
proportion of all fentanyl deaths would have involved
another substance.
Percentage of deaths involving specific substances
55
56
Substance
Alberta (2021)
BC (2019-22)
Fentanyl
81%
86%
Methamphetamine
57%
42%
Cocaine
24%
45%
Alcohol
23%
26%
55
Substance use surveillance data. (2023) Government of Alberta.
56
Illicit Drug Toxicity Deaths in BC: January 1, 2012—October 31,
2022. (2022). British Columbia Coroners Service.
0
50,000
100,000
150,000
200,000
250,000
300,000
2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
Guilty Cases in Canada for all crime,
Total Offences

38
Risk Factors
Opioid harms are not distributed evenly across different
groups in Canada. Some are far more likely to suffer
opioid-related harms than others.
Sex
Men are significantly more likely to suffer opioid-related
harms in Canada than women.
Fig. 19. Data sourced from Government of Canada (2022).
In 2021, three quarters (74%) of all AAOTDs and 65% of
all accidental opioid-related poisoning hospitalizations
(AOPHs) were men. The ratio of male to female deaths in
Alberta was in line with national averages, but was more
57
Opioid- and stimulant-related harms. (2022). Government of
Canada.
acute in BC, where 80% of all AAOTDs in 2021 were
men. Though the proportion of men to women dying of
AAOTDs has remained relatively stable in the past few
years (2017-2021), the proportion of men to women
being hospitalized for AOPHs has been rising steadily.
57
CADs data did not break down responses by both
province and gender, so it is not possible to evaluate
whether the ratio of men to women in BC’s drug using
population differs from other provinces.
Fig, 20. Data sourced from Government of Canada (2022).
0%
20%
40%
60%
80%
100%
Deaths Hosp. Deaths Hosp. Deaths Hosp.
Canada Alberta BC
Male vs. Female Proportion of Opioid-
Related Deaths and Hospitalizations, 2021
Male Female
0%
10%
20%
30%
40%
50%
60%
70%
80%
Canada Alberta BC
Percentage of Men Hospitalized for
Accidental Opioid-Related Poisonings
2017 2018 2019 2020 2021

39
Age
Drug use often begins in adolescence or young
adulthood. However, the ages most impacted by AAOTDs
in Canada are those between 30 and 49. In 2021 30-49-
year-olds represented 27% of the population and over
half (52%) of all AAOTDs. 20-29-year-olds and 50-59-
year-olds together then represent 26% of the population
and 38% of AAOTDs.
Alberta is similar to the Canadian average, with 30-49-
year-olds representing 30% of the population and 54% of
deaths. Those dying in BC, however, tend to be older.
50–59-year-olds represented only 13% of the population
in 2021 but account for 28% of all AAOTD deaths.
Fig. 21. Data sourced from Government of Canada (2022).
58
Population estimates on July 1st, by age and sex. (2022). Statistics
Canada.
Those in middle age – 30-49-year-olds – then represent
42% of deaths (and 27% of the population).
58
59
Similar to gender, AOPH rates for different age groups do
not entirely align with AAOTD rates. Most notably, those
who are over 60 are hospitalized at a much greater rate
than the rate at which they are dying, while those 50-59
are dying at a greater rate than they are hospitalized.
Fig. 22. Data sourced from Government of Canada (2022).
59
Opioid- and stimulant-related harms. (2022). Government of
Canada.
0
5
10
15
20
25
30
35
<19 20 to 29 30 to 39 40 to 49 50 to 59 60+
Percentage of Accidental Apparent Opioid
Toxicity Deaths by Age Group, 2021
Canada Alberta BC
0%
20%
40%
60%
80%
100%
Deaths Hosp. Deaths Hosp. Deaths Hosp.
Canada Alberta BC
Proportion of Opioid-Related Deaths
and Hospitalizations by age, 2021
0-19 20-29 30-39 40-49 50-59 60+

40
As with sex, however, the age of those being hospitalized
has increasingly come to resemble the age of those dying
of opioid overdoses.
Fig. 23. Data sourced from Government of Canada (2022).
Age and Sex
Taken together, age and sex are major determinants of
AAOTDs. In Canada 30-59-year-old men represent 54%
of all AAOTDs but only make up 20% of the total
population (2021). The next two most significant
categories are 20–29-year-old men (12% of deaths, 7% of
the population) and 30-39-year-old women (8% of deaths,
60
Alberta Opioid Response Surveillance Report: First Nations People
in Alberta. (2021). The Alberta First Nations Information Governance
Centre.
7% of the population). Taken together, these groups
represent 74% of all AAOTDs but only 34% of the
population.
Ethnicity
There is a lack of data regarding ethnicity and opioid
harms in Canada. Four sources of data were identified.
Reports were published in both BC and Alberta analyzing
the impact of the opioid crisis on First Nations
populations (note that this does not encompass all
indigenous peoples in Canada, see Appendix C), and the
BC Coroners Service analyzed the representation of
indigenous peoples in illicit overdose deaths.
In Alberta, First Nations individuals were dying at a rate
nearly 7 times that of non-first nations in the first six
months of 2020.
60
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Hosp.
Deaths
Hosp.
Deaths
Hosp.
Deaths
Hosp.
Deaths
Hosp.
Deaths
Hosp.
Deaths
2016 2017 2018 2019 2020 2021
Age Ratios of AAOTDs and
AOPHs over time
0-19 20-29 30-39 40-49 50-59 60+

41
Fig. 24. Data sourced from The Alberta First Nations Information Governance
Centre (2021).
In BC, between January and June 2021, 14% of overdose
deaths were among First Nations peoples despite them
representing only 3.3% of the population, resulting in a
death rate 4.8 times greater than for other BC residents.
61
The third identified source was a report analyzing the
demographic characteristics of people hospitalized
across Canada (excluding Quebec) due to opioid
poisonings between 2011 and 2016.
62
The report found
that those who self-identified as visible minorities had a
hospitalization rate of only 2.6 per 100,000, compared to
people who did not identify as a member of a visible
minority who had a hospitalization rate of 13.2 per
100,000. Self-identified indigenous peoples were found to
have significantly higher rates of hospitalization due to
opioid poisoning.
Rates of Hospitalization Due to Opioid Poisoning by Self-Identified Ethnicity, 2011-2016
Group
Not visible
minority
Visible
minority
First Nations
On Reserve
(First Nations)
Off reserve
(First Nations)
Métis
Inuit
Crude Rate
per 100,000
13.2
2.6
34.1
47.6
26.4
24.8
22.7
61
BC Coroners Service Death Review Panel: A Review of Illicit Drug
Toxicity Deaths. (2022). BC Coroners Service.
62
Gisèle Carrière, Rochelle Garner, & Claudia Sanmartin. (2018).
Social and economic characteristics of those experiencing
hospitalizations due to opioid poisonings. Statistics Canada.
0
20
40
60
80
100
120
2016 2017 2018 2019 01-06/2020
Alberta First Nations Mortality Rates
per 100,000
First Nations Non-First Nations

42
Employment and Socio-Economic Status
Though there was not Canada-wide data available on
employment status and opioid-related deaths, the BC
Coroners Service found that only 35% of those who
suffered illicit drug toxicity deaths between August 2017
and July 2021 were employed at the time of their death.
Of those employed, over half worked in the trades, in
transportation, or as equipment operators.
63
When it comes to hospitalization, research found that
unemployment correlated with opioid-related incidents.
Those under 65 who were not in the labour force were
most likely to be hospitalized (30.8 per 100,000), while
those who were employed were least likely to be
hospitalized (6.5 per 100,000).
64
Other research also found that income levels were also
correlated with opioid-related mortality and
hospitalization.
65
Those in the lowest quintile were 3.8
times more likely to suffer opioid-related mortality
66
and
63
BC Coroners Service Death Review Panel: A Review of Illicit Drug
Toxicity Deaths. (2022). BC Coroners Service.
https://www2.gov.bc.ca/assets/gov/birth-adoption-death-marriage-
and-divorce/deaths/coroners-service/death-review-
panel/review_of_illicit_drug_toxicity_deaths_2022.pdf
64
Gisèle Carrière, Rochelle Garner, & Claudia Sanmartin. (2018).
Social and economic characteristics of those experiencing
hospitalizations due to opioid poisonings. Statistics Canada.
https://www150.statcan.gc.ca/n1/pub/82-003-
x/2018010/article/00002-eng.htm
65
Wasem Alsabbagh, Martin Cooke, Susan J. Elliott, Feng Chang,
Noor-Ul-Huda Shah, & Marco Ghobrial. (2022). Stepping up to the
4.3 times more likely to be hospitalized for opioid-related
reasons.
67
Average Opioid-related mortality
by income quintile, 2000-2017
Income
Quintile
Death
Cases
Population
Adjusted
rate
Rate Ratio
1 (highest)
1,585
4,923,280
18.9
1.0 (reference)
2
2,325
5,115,515
26.4
1.4
3
4,035
6,070,270
38.5
2.0
4
4,960
6,086,520
48.2
2.6
5 (lowest)
5,955
4,792,290
72.1
3.8
The death rate ratio between the highest and lowest
quintile has been decreasing over time (having gone from
4.33 in 2000 to 2.15 in 2017), but the hospitalization ratio
has not changed significantly.
Canadian opioid crisis: A longitudinal analysis of the correlation
between socioeconomic status and population rates of opioid-related
mortality, hospitalization and emergency department visits (2000–
2017). Government of Canada. https://www.canada.ca/en/public-
health/services/reports-publications/health-promotion-chronic-
disease-prevention-canada-research-policy-practice/vol-42-no-6-
2022/canadian-opioid-crisis-longitudinal-analysis-correlation-
socioeconomic-status-population-rates-mortality-hospitalization-
emergency-department-visits-2000-2017.html
66
2000-2017
67
2000-2013, age- and sex- adjusted rate.

43
Average Opioid-related hospitalization
by income quintile, 2000/01-2012/13
Income
Quintile
Hosp.
cases
Population
Adjusted
rate
Rate Ratio
1 (highest)
4,520
4,923,280
96.5
1.0 (reference)
2
5,835
5,115,515
138.9
1.4
3
9,020
6,070,270
203.8
2.1
4
15,785
6,086,520
284.7
3.0
5 (lowest)
21,855
4,792,290
413.2
4.3
Location of Death and Household Characteristics
There is no Canada-wide data on location of death, and
there is no published geographic mapping of deaths
below provincial level, however both BC and Alberta have
category data.
In both BC and Alberta, the majority of drug overdose
deaths occurred in private residences. In BC, between
August 2017 and July 2021, 65% of all illicit drug toxicity
deaths occurred in private non-subsidized residences,
and a further 19% occurred in subsidized housing, hotels
or shelters.
68
In 2021, in Alberta the average quarterly
death rate in private residences where the decedent lived
long-term was 68% of all deaths.
69
Research found that the most common living
arrangements of those being hospitalized were those
68
BC Coroners Service Death Review Panel: A Review of Illicit Drug
Toxicity Deaths. (2022). BC Coroners Service.
69
Substance use surveillance data. (2023) Government of Alberta.
living alone (25.1 per 100,000) and single parents (25.5
per 100,000). They were also far more likely to be in band
housing (53.8 per 100,000) or renting (21.3 per
100,000).
70
Though Canada-wide data was not available on the
relationship between opioid harms and homelessness,
the BC Coroners Service found that 12% of those who
died of illicit drug toxicity between 2017 and 2021 were
homeless.
71
70
Gisèle Carrière, Rochelle Garner, & Claudia Sanmartin. (2018).
Social and economic characteristics of those experiencing
hospitalizations due to opioid poisonings. Statistics Canada.
71
BC Coroners Service Death Review Panel: A Review of Illicit Drug
Toxicity Deaths. (2022). BC Coroners Service.

44
Marital Status
Data from BC found that, in 2016 and 2017, 65% of those
who died had never been married, and 18% were
separated or divorced.
72
Comparable data was not
available elsewhere in Canada, but is mirrored by
statistics from the United States.
73
Fig. 25. Data sourced from BC Coroners Service (2022).
Area-Level Characteristics
A study found that in 2016-2017, the majority of deaths
occurred in major population centres (30% of all deaths
occurred in metropolitan zones with 1,500,000+
residents), but the highest rate of deaths occurred in
72
Illicit Drug Overdose Deaths in BC. (2018). BC Coroners Service.
73
The Numbers Behind the Opioid Crisis. (2017). Social Capital
Project.
smaller centres (15.9 deaths per 100,000 occurred in
zones with 100,000-499,999 residents. 1,500,000+ zones
only had a death rate of 10.7).
74
Mental Health and Contact with Healthcare System
Though there is not Canada-wide data on the intersection
between opioid harms and contact with the healthcare
system, both Alberta and BC report on whether those
who suffer from AAOTDs had contact with the healthcare
system prior to their death.
In Alberta, January to June 2022, 56% of those who
suffered a non-pharmaceutical opioid-related death had
received at least one health service within 30 days of
death, 34% had been dispensed an antidepressant, 18%
had had a mental health visit, and 16% had a visit related
to chronic pain.
75
In BC, between August 2017 and July 2021, 62% of
people who died of illicit drugs were experiencing mental
health issues. 50% had a mental health diagnosis, while
12% and anecdotal evidence of a mental health disorder.
43% had a health visit related to mental health in the year
prior to their death, compared to 14% of the B.C.
population. 72% of those who died had a visit with a
health professional less than three months before their
death, and 87% had a visit within one year of their death.
74
Canadian area-level characteristics of substance-related acute
toxicity deaths, 2016 to 2017. (2022). Government of Canada.
75
Substance use surveillance data. (2023) Government of Alberta.
0% 10% 20% 30% 40% 50% 60% 70%
Unknown
Widowed
Separated/divorced
Married (incl. common law)
Never Married
Marital Status of Those Suffering from Illicit
Drug Overdose Deaths in BC, 2016-2017

45
Decedents had a higher number of health visits, and 30%
had had a previous paramedic attended non-fatal illicit
drug related event.
76
A prior BC report looking at 2016
and 2017 data found that 45% of decedents had sought
assistance for pain-related issues in the year prior to their
death.
77
Education
Education was highly predictive of risk of hospitalization
due to opioid poisoning. Those with no credentials were
hospitalized at a rate of 23 per 100,000, while those with
a university degree were hospitalized at a rate of 5.5 per
100,00.
78
Rate of hospitalization due to opioids by education level,
2011-2016
Highest level of education
attainment
Crude rate per
100,000
No certificate, diploma, or degree
23.0
High school diploma and/or trade
certificate
14.3
College Diploma or university
below bachelor
12.7
University degree
5.5
76
BC Coroners Service Death Review Panel: A Review of Illicit Drug
Toxicity Deaths. (2022). BC Coroners Service.
77
Illicit Drug Overdose Deaths in BC. (2018). BC Coroners Service.
Summary: Canada, Alberta, BC
The published data enables a summary of differences
between Alberta and BC, Canada’s two opioid hotspots.
Over half the people suffering AAOTDs in Canada are
30–59-year-old men, and the majority of deaths have
occurred in Alberta and BC. Though there appear to be a
higher prevalence of drug use, and more drug users in
the two provinces than in other Canadian provinces, this
factor is insufficient for explaining why deaths are so
concentrated in the two provinces. Instead, deaths seem
concentrated in Alberta and BC because of the relative
toxicity of the drugs being supplied and consumed there.
Those dying were generally poorer, unemployed,
unmarried, and less educated. For those that were
employed, they were most commonly working in the
trades, transportation, or as equipment operators. They
often would have had recent contact with the healthcare
system, mental health issues, and/or have sought
assistance for chronic pain.
First Nations peoples suffer disproportionally high levels
of opioid harms. Other visible minorities are significantly
less likely to suffer opioid-related harms than the general
population.
78
Gisèle Carrière, Rochelle Garner, & Claudia Sanmartin. (2018).
Social and economic characteristics of those experiencing
hospitalizations due to opioid poisonings. Statistics Canada.

46
The majority of deaths occurred in large population
centres with populations over 1.5 million, but the highest
rate of deaths occurred in smaller population centres.
Alberta and BC are Canada’s opioid hotspots, but there
are some differences in how the crisis has presented in
the two provinces. First, BC has a much longer history
with substance harms with Alberta, and volume of harm is
much higher in BC, measured according to deaths and
hospitalisations. However, the rise in AAOTDs in Alberta
during the pandemic has been steeper relative to its pre-
pandemic levels.
Fig. 26. Data sourced from Government of Canada (2022).
Those dying of AAOTDs in BC are notably older than
those dying in Alberta and the rest of the country. They
are also the most likely to be male, with 80% of all deaths
being men (vs. 74 % in Canada and 73% in Alberta).
Finally, police incident data confirms BC is the epicentre
of drug-crime in Canada, reporting 57 opioid-related
incidents per 100,000 vs. 13 in Alberta. In terms of the
major cities, Vancouver also has significantly higher
numbers of drug-related violations than either Calgary or
Edmonton, which could be a reflection of police activity,
as opposed to underlying prevalence. Despite this, there
are significantly fewer arrests for drug-related crime in
the BC, and a low charge rate despite rising rates of
incidents.
Considering the recent decriminalisation of possession in
BC it is perhaps unsurprising that drug users have not
been routinely charged by police when caught in
possession in recent years; however, this does not seem
to reflect a law enforcement focus on upstream
interdiction against dealers and traffickers instead. When
considering the more serious drug offences involved in
supply and profiting from the illicit market – namely
importing and trafficking – the gap between TPD
incidents and charges, however, is significant (80 per
100,000 incidents vs. 22 per 100,000 charges in 2019). In
contrast, Alberta charges far more people for TPD
relative to the incidents detected (46.6 per 100,000
incidents vs. 38 per 100,000 charges).
0
10
20
30
40
50
2017 2018 2019 2020 2021 2022 (Jan-
Jun)
Deaths per 100,000
Alberta and BC AAOTDs
Canada Alberta British Columbia

47
CHAPTER 4: Policies and Services
in Alberta and British Columbia
This chapter summarises the respective programs that
Alberta and BC have implemented to address the
addiction crisis. The backdrop is stark: BC in 2022
experienced its second worst year of overdose deaths
ever (2,272), just behind the 2021 total (2,306).
79
Alberta
too went through its second worst year of overdoses
(1,346) in 2022, compared to its worst total the preceding
year (1,621).
80
Nevertheless, the recent annualised
decline in deaths of 17% in Alberta – if sustained in 2023
– would be the start of a positive trend.
Provincial Contrast?
The two broad policy approaches explored in this section
include both harm reduction, which dominates the
approach in BC, and recovery-oriented care, which is the
model being pursued in Alberta since 2019.
Some observers have suggested that Alberta’s emphasis
on recovery (inspired by ‘Towards an Alberta Model of
Wellness’) represents a new model of care in Canada and
a departure from the harm reduction policies embraced
in British Columbia.
81
This is an oversimplification as it
79
Wells, V. S. (2023, January 31). 2022 was second deadliest year
for toxic drug deaths ever. The Georgia Straight.
80
Substance use surveillance data. (2023). Government of Alberta.
presupposes that Alberta’s current service approach is
wholly distinct from British Columbia’s, which it is not. For
example, harm reduction efforts are also undertaken in
Alberta, and BC funds residential recovery provision.
Nevertheless, there is a distinct contrast in the strategic
emphasis that is placed on recovery in Alberta, compared
to what is currently guiding all policy in BC, and as of
January 2023, both provinces take different policing
responses to drug possession.
Enforcement and Decriminalization
In an attempt to further reduce the potential for drug
users to be subject to enforcement, the BC Government
has advocated decriminalisation of drug possession in the
province. As of 31 January 2023, and following approval
from the federal government in November 2022, BC has
now adopted a decriminalization policy that prevents law
enforcement from arresting individuals aged 18 or above
for possessing minor quantities (2.5g) of illicit
substances.
82
Given that charges for possession were
already low, this could also be viewed as the formalization
and codification of current practices. Possessing drugs
for the purpose of trafficking, possessing drugs at
schools, child-care facilities and airports remains illegal
and several municipalities have local bylaws prohibiting
81
Alberta, B.C., and two different approaches to fight Canada’s
epidemic of drug deaths. (2022, October 11). The Globe and Mail.
82
Kulkarni, A. (2023, January 31). What you need to know about the
decriminalization of possessing illicit drugs in B.C. CBC.

48
drug use at public facilities and in private spaces like
shopping malls.
83
Meanwhile, Alberta is maintaining conventional
enforcement pertaining to possession of illicit substances.
The Alberta Association of Chiefs of Police has stated that
it is too soon to look at decriminalization in Alberta
because the necessary levels of support, including
addiction treatment services, are unavailable.
84
Despite
this position, as recently as last year the city of Edmonton
passed a motion to develop its own decriminalization
strategy to reduce future harm from toxic drugs.
85
Along with the rest of Canada, with the exception of BC,
drug possession remains illegal in Alberta without a
prescription. Alberta police officers can now offer
diversion to treatment to individuals caught with illicit
substances; however, drug possession is not
decriminalised and individuals can still be arrested,
charged, and processed for possession. Overall incident
rates for possession in Alberta have reduced in recent
years, though this is probably best attributed to the
COVID-19 pandemic.
83
Kulkarni, A. (2023, January 31). What you need to know about the
decriminalization of possessing illicit drugs in B.C. CBC.
84
Graveland, B. (2022, January). It’s too soon to support drug
decriminalization: Alberta police chiefs. Global News.
85
Amato, S. (2022, April 11). Edmonton moves forward on
decriminalizing ‘simple personal possession’ of drugs. CTV News.
86
Hyshka, E., Anderson-Baron, J., Karekezi, K., Belle-Isle, L., Elliott,
R., Pauly, B., Strike, C., Asbridge, M., Dell, C., McBride, K., Hathaway,
The next section will explore elements of harm reduction
and recovery-oriented models of care.
‘Safer Supply’ and Harm Reduction
The origins of harm reduction in British Columbia can be
traced to the first needle exchange and distribution
programs in 1988 and 1989 aiming to limit the reuse and
sharing of needles to help address the AIDS epidemic.
86
The federal government then adapted harm reduction as
part of its drug policy and introduced further measures
such as attempts to decriminalize cannabis possession
and providing for exemptions to criminal prosecution to
open Insite in 2003 in BC, which was the first supervised
injection facility to exist in North America.
87
Since this time BC embraced more elements of harm
reduction, including investments in naloxone distribution,
Opioid Agonist Therapy (OAT), supervised drug
consumption services, overdose prevention technology,
‘safer supply’ distribution and most recently,
decriminalization of illicit substances.
A., & Wild, T. C. (2017). Harm reduction in name, but not substance:
A comparative analysis of current Canadian provincial and territorial
policy frameworks. Harm Reduction Journal, 14(1), 50.
87
Hyshka, E., Anderson-Baron, J., Karekezi, K., Belle-Isle, L., Elliott,
R., Pauly, B., Strike, C., Asbridge, M., Dell, C., McBride, K., Hathaway,
A., & Wild, T. C. (2017). Harm reduction in name, but not substance:
A comparative analysis of current Canadian provincial and territorial
policy frameworks. Harm Reduction Journal, 14(1), 50.

49
In March 2020, BC rolled out the first ‘safer supply’ pilot
program to residents.
88
According to Dr. Thomas Kerr, a
senior scientist at BC’s Centre on Substance Use, safe
supply is defined as a legal supply of drugs that enables
individuals to use regulated substances as opposed to
toxic supplies from the illicit market.
89
As part of its 2021
budget, BC increased funding to expand the program and
as of February 2022, at least 12,000 citizens have
accessed prescribed safer supply.
90
There is no way of
tracking who is in receipt of drugs via these channels,
what proportion of these drugs are given or sold to others
not enrolled in the program. Note also that drug users
enrolled in ‘safer supply’ may choose to continue to
source drugs from the illicit market.
The many dimensions of harm reduction in BC have
become a defining strategy for how the province
addresses the addiction crisis. Below, BC lists specific
examples of harm reduction measures currently
practiced in the province.
91
This represents an overview
of how BC is defining harm reduction and what types of
service provisions the province has adopted in response
to the opioid crisis.
88
Grochowski, S. (2022, February). What is safe supply? A look at
what B.C. drug users, advocates are demanding. Vancouver Sun.
89
Grochowski, S. (2022, February). What is safe supply? A look at
what B.C. drug users, advocates are demanding. Vancouver Sun.
Components of Harm Reduction in BC
▪ Supply distribution and needle recovery programs
▪ Options for opioid substitution (agonist) therapies
such as methadone or suboxone
▪ Take home naloxone kits. The kits include
medication to reverse an opioid overdose
▪ Supervised consumption/injection services and
overdose prevention services
▪ Mental wellness and healing support programs
and centres
▪ Outreach and support programs
▪ Information and resources on safer ways to use
substances
▪ Public awareness campaigns to support de-
stigmatisation of drug use
▪ Peer support programs run and attended by
people with experience using substances
Alberta also has elements of harm reduction present in its
public policy approach to substance use and addiction.
The province distributes naloxone, offers OATs –
including the rapid deployment of new therapies like
Sublocade since late 2021 – and hosts SCS across the
province.
90
B.C. introduces new prescribed safer supply policy, a Canadian
first. (2021, July 15). BC Gov News.
91
Understanding Harm Reduction: Substance Use. (2020).
HealthLinkBC.

50
Recovery
The origins of the recovery-orientated model in Alberta
can be tracked back to 2019 when the United
Conservative Party (UPC), under Jason Kenney, entered
office. The party’s election platform at the time promised
to prioritizing investments in rehabilitation beds and
spaces that could help expand treatment capacity and
support more drug users to recover, as a key strategy to
reverse the opioid crisis in Alberta.
92
According to Alberta Health Services, recovery-oriented
care providers work with individuals in their current state,
respect autonomy and dignity and place an emphasis on
individual safety and providing support for harm
reduction, positive risk taking and continual personal
growth.
93
Moreover, recovery seeks to transcend
symptom management and cravings and instead aims to
support the development of a return to social,
psychological, cultural, sexual, and spiritual aspects of
life.
94
The following reflects some of the key features of the
recovery-oriented model of care in Alberta.
95
92
How Alberta is tackling its toxic drug crisis. (2022). The Drug and
Alcohol Testing Association of Canada.
93
Recovery Oriented Care. (2020). Alberta Health Services.
Components of Recovery Oriented Care in
Alberta
▪ Individual, family, or group therapies
▪ Professional/clinician-led or peer-led therapies
▪ Privately or publicly managed
▪ Formal or informal settings
▪ Wellness-focused or treatment-focused
▪ Prevention-focused or action-focused
▪ Cultural interventions
Alberta Health Services includes harm reduction
references within its definition of recovery-oriented care,
and drug users can still access many services that are
also available in BC.
Services
The following section aims to investigate what services
are available to citizens within the scope of each
province’s overarching policy model.
Supervised Consumption Sites
Currently, both Alberta and BC deploy SCS in each
province as reflected in the table below. Each province
hosts sites that offer a variety of services to visitors, but
data on capacity or current service caseload is not
published:
94
Recovery Oriented Care. (2020). Alberta Health Services.
95
Recovery Oriented Care. (2020). Alberta Health Services.

51
Supervised Consumption Sites in Alberta and BC
Province
City
Location
Authorized services
Alberta
Calgary
Sheldon M. Chumir Health Centre (Alberta Health Services)
1213 4
th
St SW
Injection
Intranasal
Oral
Alberta
Edmonton
Boyle McCauley Health Centre (Boyle McCauley Health Centre) 10628
96th St
Injection
Intranasal
Oral
Peer assistance
Alberta
Edmonton
George Spady Centre Society (George Spady Centre Society) 10015
105A Ave NW
Injection
Intranasal
Oral
Peer assistance
Alberta
Edmonton
Royal Alexandra Hospital
(Alberta Health Services)
10240 Kingsway Ave
Injection
Intranasal
Oral
Alberta
Grande Prairie
Northreach Mobile Supervised Consumption Service (Northreach
Society) 10101 97A St
Injection
Intranasal
Oral
British
Columbia
Vancouver
Dr. Peter Centre (Dr. Peter AIDS Foundation)
96
1110 Comox St
Injection
British
Columbia
Vancouver
Hope 2 Health
(BC Centre for Excellence in HIV/AIDS)
611 Powell St
Drug content checking
Injection
Intranasal
Oral
British
Columbia
Vancouver
Insite (Vancouver Coastal Health)
139 East Hastings St
Drug content checking
Injection
Intranasal
Oral
Safer supply prescription fulfillment
British
Columbia
Victoria
The Harbour Supervised Consumption Service (Island Health) 941A
Pandora Ave
Drug content checking
Injection
Intranasal
Oral
Peer assistance
96
No representative could be reached from the Dr. Peter Center who would confirm whether they fulfilled safer supply prescriptions.

52
Insite, being North America’s first legal SCS, still operates
in Vancouver’s Downtown Eastside. Since its inception in
2003, funding has been expanded to other sites
throughout the province. These sites provide hygienic
environments to consume drugs without fear of arrest for
possession and to help improve the integration of care for
individuals who use substances.
97
In Alberta, the first permanent SCS in Calgary began
operations in 2018 and rapidly expanded services to
additional sites in Edmonton, Lethbridge, and Grand
Prairie. Currently, Alberta has five sites in operation that
are authorized by the same valid exemption from the
federal government under section 56.1 of the Controlled
Drugs and Substances Act.
Alberta previously hosted an additional site in Lethbridge
which saw the highest volume of visitors in North
America
98
but this site has subsequently closed.
99
According to a government audit, the site closed due to
the discovery of misappropriated funds.
100
It is not possible to determine the number of clients that
the network of consumption sites supports in each
province, although given their longer history, it is likely
that the four sites in BC have a higher caseload. What is
97
Supervised Consumption Services: Operational Guidance. (2017).
British Columbia Centre on Substance Use.
98
Lethbridge supervised consumption site shutting down at month’s
end. (2020, August). Calgary Herald.
99
Lethbridge supervised consumption site shutting down at month’s
end. (2020, August). Calgary Herald.
apparent is that the only services unique to BC are drug
checking and safer supply prescription fulfillment. All
other authorized services are available in each province
depending on the site.
It is argued by advocates that there have not been fatal
overdoses at drug consumption sites in BC and this is
proof that the model is working. However, there is no
published operating criteria for these sites and no means
to hold providers accountable, and the expansion of drug
consumption sites has occurred in parallel to continued
increases in drug deaths in the community. There is also
a lack of evidence that supervised consumption sites
reduce mortality.
101
Data is not publicly available that demonstrates the
impacts of SCS on drug harms. It is possible that while
these sites were initially effective for their intended
purpose to limit the spread of HIV and other
communicable diseases, they are not generating the
same success in reducing overdose deaths.
Rehabilitation
In 2019, the Government of Alberta, in support of the
recovery model, announced $140 million of spending
100
Lethbridge supervised consumption site shutting down at month’s
end. (2020, August). Calgary Herald.
101
Panagiotoglou, D. (2022). Evaluating the population-level effects of
overdose prevention sites and supervised consumption sites in
British Columbia, Canada: Controlled interrupted time series. PLoS
ONE, 17(3), e0265665.

53
over four years with an additional $20 million investment
in 2022, including 8,560 new treatment and recovery
spaces, which would reportedly increase available spaces
to over 27,000 from 19,000 spaces in 2019.
102
As part of
this they are the first province to eliminate fees for
addiction recovery programs.
103
Part of this investment is directed towards creating
communal settings for care that are defined as
‘rehabilitation/therapeutic communities.’ These
communities enable individuals to receive treatment that
focuses on many facets of the individual and their overall
lifestyle changes that prepare them for a return to normal
life.
104
The treatment is funded by the provincial
government and is a gradual recovery program that
assists individuals returning to full community living on
their own.
BC points to treatment and supportive recovery services
as either live-in or bed-based substance use services
offering a variety of programs that can be shorter or
longer depending on individual need. The amalgam of
102
Johnson, L. (2022, March). Toxi-City (Part 3): Deadly drugs in
Edmonton — How is the Alberta government tackling the problem?
Edmonton Journal.
103
French, J. (2020, November 7). Financial hurdle gone: Alberta first
province to eliminate fees for addiction recovery programs. CBC.
104
Recovery Community Operations Competitive Grant. (n.d.).
Government of Alberta.
services and models of care differ depending on the
individual as well.
In 2016, in BC, the number of rehabilitation beds totaled
approximately 2,547.
105
Currently, the province has a total
of 3,261.
106
In 2022, the government announced the
investment of $164 million to build more complex-care
housing.
107
Making accurate inter-provincial comparisons on
treatment beds and spaces is not possible because
Alberta and BC do not use common definitions. It
appears that Alberta has significantly more spaces
dedicated to rehabilitation than BC, but its numbers
encompass both ‘live in’ and ‘communal’ settings.
Additionally, it appears BC does not currently offer any
therapeutic community settings as defined in Alberta.
When it comes to wait times to access rehabilitation
spaces and beds, while provincial health authorities like
Island Health suggest waitlists for existing rehabilitation
beds in BC is typically about five weeks,
108
Albertans face
105
McElroy, J., & Clancy, N. (2016, September). Are there enough
beds for drug treatment in B.C.? CBC.
106
Russ, G. (2022, September 27). A tale of two provinces: Assessing
the opioid crises in BC and Alberta. Macdonald-Laurier Institute.
107
Cowie, A. (2022, May 21). Powell River and Bella Coola to receive
funding for complex-care housing. CityNews.
108
Dickson, L. (2022, August 28). People seeking detox treatment
face weeks-long waits. Times Colonist.

54
a waitlist to access beds that can range between six
weeks and twelve months depending upon location.
109
Moreover, the definition of rehabilitation beds in each
province is not uniform. This is particularly important
because Alberta is charting a comparatively new path
when it comes to creating rehabilitation communities,
which encompass rehabilitation beds in a manner that
does not appear to exist in BC.
Ultimately, despite funding announcements around
creating new rehabilitation spaces and beds in Alberta,
demand is still exceeding supply and it is therefore too
early to conclude whether the expansion in rehabilitation
beds is impacting the opioid crisis.
Naloxone
Naloxone provision is another service that is offered in
both Alberta and BC. Naloxone is an opioid antagonist
medication that can temporarily reverse the effects of an
overdose and allow time for help to arrive by blocking the
effects of opioids and restoring normal breathing.
110
Antagonist medications bind to the same brain receptors
as opioids, which stops the receptor from producing the
suppressed respiratory response.
109
Bhatti, A. (2017, October 16). Waitlists Are Growing in Alberta for
Treatment Centres. Andy Bhatti.
110
Naloxone. (n.d.). CAMH.
111
Get Naloxone. (n.d.). Alberta Health Services.
In Alberta, there are currently over 2000 sites that
provide naloxone kits free of charge for individuals to take
home.
111
In BC, there are approximately 1800 currently
on record.
112
In recent years there has been a dramatic
upswing in naloxone kit distribution in Alberta where in
2022 there was approximately 135,330 kits distributed
compared to only 32,140 in 2017, and 6,181 in 2016.
113
In
BC, over one million naloxone kits were distributed
between 2012 and 2021.
114
With clear efficacy, both
provinces continue to increase the number of naloxone
kits distributed in recent years. However, the increase in
distribution in Alberta has been particularly rapid.
*2022 Q4 data not yet available. Chart uses average of prior three quarters.
Fig. 27. Data sourced from Government of Alberta (2023).
112
Take Home Naloxone. (n.d.). Towards the Heart. Retrieved 6
March 2023, from https://towardtheheart.com/naloxone
113
Substance use surveillance data. (2023). Government of Alberta.
114
More than one million naloxone kits shipped in B.C. as overdose
crisis continues. (2021, June). BC Centre for Disease Control.
0
50000
100000
150000
200000
2016 2017 2018 2019 2020 2021 2022*
Naloxone Kit Distribution in Alberta by year

55
Opioid Agonist Treatment
OATs are defined as agonist medications, which are
drugs that produce a similar response to illicit opioids, but
in a safer and more stable fashion.
115
Agonist
medications bind to the same brain receptors as illicit
opioids, reducing withdrawal symptoms and creating
biological and emotional stability for the patient.
116
This is
different from naloxone, which is an antagonist drug
designed to rapidly reverse the effects of opioid
overdoses.
The process for engaging in an opioid agonist treatment
plan in BC does not involve a referral and most OATs are
covered for all provincial residents who have sought
treatment from a doctor to explore their options.
117
The
Island Health Authority in BC is careful to point out that
these treatments often require a combination of individual
and group counselling.
Similarly, the Government of Alberta defines opioid
agonist therapy as taking medications to treat opioid use
disorder by reducing cravings and helping to manage
withdrawal symptoms.
118
These types of medications are
prescribed to be taken daily and treatment plans exist
within a long-term or short-term context depending on
each individual.
115
Opioid Agonist Therapy. (n.d.). Island Health.
116
Pharmacological Treatment. (n.d.). Indian Health Services.
117
Opioid Agonist Therapy. (n.d.). Island Health.
The process for engaging in an opioid agonist treatment
plan in Alberta requires the acquisition of a prescription
and dispensation by a pharmacist. The associated
dispensing fees can provide a barrier to individuals
without health benefits coverage.
119
However, the OAT
coverage program offered by the Government of Alberta
aims to eliminate the gap in coverage by offering OAT to
individuals for up to 120 days free of charge for those
with a valid prescription and a current provincial health
card identification number.
Clearly, the role OATs play in reducing or eliminating
cravings is significant. Nonetheless, it does not appear as
though it is more difficult to gain access to this type of
treatment. In Alberta, there has been a rapid deployment
of Sublocade – an injection that can satiate cravings for
30 days – and which was licensed in Canada in 2018.
118
Opioid Agonist Therapy Gap Coverage Program. (n.d.).
Government of Alberta.
119
Opioid Agonist Therapy Gap Coverage Program. (n.d.).
Government of Alberta.

56
*2022 Q4 data not yet available. Chart uses average of prior three quarters.
Fig. 28. Data sourced from Government of Alberta (2023)
Technology
Alberta has recently emerged as a leader on the
technology front when it comes to addressing the opioid
crisis.
In 2017, the government introduced the virtual opioid
dependency treatment program (VODP), utilizing
telehealth infrastructure to support the provision of OATs
to Albertans.
120
120
The Virtual Opioid Dependency Program (VODP). (n.d.). Health
Standards Organization.
121
Digital Overdose Response System. (n.d.). DORSAPP.
122
Digital Overdose Response System. (n.d.). DORSAPP.
Additionally, the Digital Overdose Response System
(DORS) app allows Albertans using opioids or other
substances to rely on automated alerts to summon
emergency response to their location if they become
unconscious.
121
The DORS app also provides information on national and
provincial addiction recovery supports and services, such
as the Addiction Helpline, to ensure a range of support is
available to individuals using the app.
122
Another
supporting piece of technology deployed in Alberta is an
online too called My Recovery Plan, which offers
assessment tools, generates recovery goals, monitors
progress, and helps with challenge management.
123
This
platform, developed in partnership with the treatment
provider Last Door, and derived from their own in-take
assessment system, is geared around tracking not just
interventions, but the drug users ‘recovery capital’, as a
individualised metric of their place on a recovery journey.
The tool has become the basis for tracking policy impact
beyond ‘harm’ metrics, and the expansion of MRP is
underway.
BC, on the other hand, has technology available such as
Lifeguard.
124
This is a smartphone app, like DORS in
Alberta, which alerts first responders by automatically
dialing 911 during a suspected overdose event. Another
123
My Recovery Plan. (n.d.). Government of Alberta.
124
Two years later, Lifeguard App continues to save lives. (2022,
May). BC Emergency Health Services.
0
500
1000
1500
2000
2500
3000
2016 2017 2018 2019 2020 2021 2022*
Unique Individuals Prescribed
Sublocade in Alberta by year

57
smartphone app that exists in BC is the Brave App, which
acts as a panic button for individuals using substances
and at risk for overdose.
125
In an effort to prevent
overdoses in the first place, a piece of technology
currently being tested is a portable drug checking
machine called a Fournier-Transform Infrared
Spectrometer, which would be the first piece of
technology of its kind in Canada.
126
Though both provinces are investing in and deploying
technology to support users, Alberta has married the
investment in this area with a plan to track and eventually
publish more data on the whole addiction journey,
including the progress being made towards recovery.
With technology in Alberta integrated into this coherent
structure of services, in years to come it will be possible
for policy-makers to evaluate the province’s impact on
improving recovery capital as well as addressing drug
harms – a first of its kind in the developed world.
Summary
Both Alberta and BC deploy elements of recovery and
harm reduction. The most apparent difference in policy
between the provinces is BC’s recent decriminalization of
substance possession. Alberta, while, bolstering funding
and support around its recovery model, is maintaining
current approaches to law enforcement around illicit
125
Overdose Detection Saves Lives. (n.d.). Brave.
drugs. Alberta continues to invest in rehabilitation beds
and spaces, such as therapeutic communities and has
not adopted the models of ‘safer supply’ – including
proposals for automated dispensing – that have been
setup in BC.
New policy innovation in BC is not currently apparent on
the issue of drug addiction, whereas Alberta’s nascent
model has not yet had time to fully deliver results, with
recovery communities still being constructed for example.
In a similar way, though BC has emphasized harm
reduction for two decades, its safer supply strategy only
reached the implementation phase 2021.
As the implementation of these strategies advances,
ongoing scrutiny of their impacts and effectiveness is
required to inform policy-makers in Canada and other
jurisdictions. Close engagement between policy-makers
and service leads in both provinces will be important to
allow sharing of learnings and best practice, especially in
those areas where provincial practices diverge.
126
Overdose prevention. (n.d.). Government of BC; Province of
British Columbia.

58
CONCLUSIONS
Canada has been grappling with a worsening opioid crisis
for over two decades. The harms caused by the crisis are
substantial, causing half as many deaths in 2020 and
2021 as COVID-19 and five times as many life years lost.
The problem is particularly acute in Alberta and BC,
which together account for 50% of all AAOTDs in Canada
despite representing only 25% of the population.
The data reviewed for this project gives a broad picture of
why drug harms are so high in Alberta and BC and who is
bearing the brunt of these harms. Harms are highest in
Alberta and BC principally because in these two
provinces the drug supply is most toxic. Though there are
likely more drug users in these two provinces, the
difference in self-reported drug use is insufficient to
explain the concentration of harms on the west coast.
Though a number of other factors may contribute to the
crisis (e.g., innovation in the illicit market, inward
migration of drug users
127
, and access to housing), their
impact is likely to not be as significant as the toxicity of
the drug supply itself.
127
Somers, J. M., Moniruzzaman, A., & Rezansoff, S. N. (2016).
Migration to the Downtown Eastside neighbourhood of Vancouver
and changes in service use in a cohort of mentally ill homeless
adults: A 10-year retrospective study. BMJ Open, 6(1), e009043.
128
Substance use surveillance data. (2023). Government of Alberta.
129
Illicit Drug Toxicity Deaths in BC: January 1, 2012—December 31,
2022. (2022). British Columbia Coroners Service.
Alberta and BC
As the opioid crisis in Alberta and BC have intensified, so
have comparisons of their respective policy platforms. In
particular, a number of commentators have held up
Alberta’s recovery-oriented system of care as a new
alternative for BC’s harm-reduction oriented approach.
This report makes three observations on this subject.
First, though there was a greater decline in Alberta’s
overdose-related deaths compared to British Columbia’s
between 2021 and 2022 (17%
128
vs. 1.4%
129
respectively)
it is still Alberta’s second most deadly year on record with
regards to drug-related harms.
130
Sustained reductions in
the opioid mortality rate in 2023 would be needed to
confirm a positive trend in Alberta. Also of course,
overdoses are not the only indicator of success of drug
policy.
Second, however much differences are emphasized
between the provinces, both utilize harm-reduction and
recovery-oriented interventions. Alberta, for example,
distributes more naloxone than BC.
130
Substance use surveillance data. (2023). Government of Alberta.
59
Third, data gaps and differences in definitions in certain
key areas makes effective comparisons across the two
provinces harder. For example, different definitions
prevent comparisons of recovery beds and spaces
available in the two provinces.
It is too soon to determine if Alberta’s recovery-oriented
system of care is delivering better results than BC’s more
harm-reduction centred approach, however BC’s
longstanding approach has been the subject of the most
intense criticism, given the scale of drug harms there.
The rate of drug deaths in the province has been
increasing for two decades, and 2022 only saw a very
modest decline, so it is unclear whether further
investment in the same harm-reduction efforts will
improve this state of affairs.
The differences between Alberta and BC’s policies are
real, but in terms of provincial approaches, their service
offerings are more similar than they are different. As
Alberta’s recovery-orientated model is implemented, it is
possible that the differences in approach will become
clearer.
The two provinces studied for this project have made
some progress in becoming more transparent, and have
also pioneered new prescription treatment programs.
Compared to a decade ago, there is more information in
the public domain, and more system-wide performance
data being published. In recent months, Alberta has
launched a detailed online data dashboard that allows the
addiction crisis and other interventions there to be
tracked, with an innovative ‘recovery capital’ scoring
matrix to track more than harmful episodes or agency
demand.
However, key metrics are still difficult to evaluate given
gaps in reporting and the lack of data collection. Alberta
has the more comprehensive dataset to report on current
performance, although some of British Columbia’s data –
though harder to access and compare – is more granular
and has a longer time series. The two provinces are
suffering the same public health crisis, and as
neighbouring jurisdictions, their respective approaches
warrant further investigation. Primary research, supported
by comprehensive government data, is required to
extract identifiable best practices from comparisons
between the two, and this is the type of activity that a
Federal Government study could seek to evaluate.
Where Next?
There is an ongoing public health emergency of drug
addiction in Canada. The Covid-19 pandemic and its
consequences exacerbated the harms associated with
the pre-existing challenges around poly-drug use
combined with mental illness, and homelessness among
a cohort of individuals suffering from low levels of social
capital.
Our research indicates that current approaches in both
provinces, based on the available data, are not yet
60
showing the progress that the public and those impacted
by drug addiction deserve. Of the two provinces, Alberta
is currently experiencing a reduction in key addiction-
related harms, however it is based on two quarters of
data, and would need to be sustained through 2023 in
order to represent an established trend.
Politicians, the public and practitioners working in the
field across both provinces want to see better progress to
mitigate the health harms from addiction. And although
the pandemic was an accelerant to some negative trends,
and despite major investments in services, the Federal
Government has not undertaken an intervention to
properly score the impact of provincial and municipal
responses in Western Canada. Given the scale of the
crisis and the number of lives lost, and set against the
assertive role played by Health Canada and other national
agencies in responding to the pandemic, this reticence is
hard to explain.
In both provinces, and in Canada overall, the biggest
impediment to an informed public policy debate is the
lack of data around long-term treatment outcomes,
desistence, and recovery. This is one area where a set of
nationally agreed definitions and counting rules would
benefit everyone. Overdoses are relatively easy to count
but cannot be the only metric by which drug policy is
judged.
The lack of good data on the downstream interventions
and the addiction recovery journey may be the symptom
of a wider problem in that public health practitioners and
provincial and federal policy-makers do not share a single
view on the evidence base around intervention efficacy,
nor the best pathways towards, effective recovery from
drug addiction.
Public concern about this challenge is likely to continue
and as death rates remain high, more transparency,
innovation and new policy responses are therefore
needed. Alberta Government’s development of a
‘recovery-orientated system of care’ provides an
important example of how political leadership and a
comprehensive strategy are necessary conditions for
success. Combined with new technology and data
tracking that captures a drug user’s recovery potential, it
may provide a collective impetus to widen the policy
agenda across Canada as a whole from a narrow goal of
reducing fatal overdoses.
Whatever new policy responses take hold in either BC or
Alberta, it is not constructive for the wider debate in
Canada for the media and researchers to be hampered
by a lack of coherence around policy goals combined
with inadequate data collection and publication.
Drug addiction and its consequences are problems
shared across many jurisdictions, but provinces like BC
and Alberta, and Canadian policy-makers in general,
should be well placed to develop an evidence-based
policy framework that is comprehensive for the whole
addiction journey, and supported by the best data. Such
61
a robust policy framework would encompass prevention,
enforcement and interventions, through to treatment and
recovery.
Canada’s experience could provide lessons to other
countries like the USA, but only if governments at all
levels commit to a consistent reporting measure that
accurately describes the progress being made, and one
that counts more than caseloads, inputs, or a series of
‘harm’ metrics. Despite the urgency of this crisis, that
basic information architecture is still not fully in place and
as a result, the impact of many policies in Canada to
reduce harms and to aid recovery cannot be properly
evaluated.
With COVID-19 we have recently seen the kind of
mobilization that both the Federal and Provincial
governments are capable of when they actively
cooperate. The scale of opioid-related harms in Canada
warrants major coordinated action of this kind, led by
Ottawa, with much more focus on how progress at all
levels will be measured, and much greater transparency
around what outcomes are being pursued.
Policy Recommendations
Agree what success looks like.
• Given the significant public funds that continue to be
spent, provincial and federal policy-makers should
now urgently agree what success looks like and how it
will be measured.
• The Federal government should agree with Canadian
provinces a core set of performance metrics that will
be routinely collated and published, and fund a full
evaluation of the provincial policy framework in British
Columbia, where the crisis is most acute;
• Health Canada should publish a comprehensive policy
briefing that summarises the international evidence-
base for all currently funded addiction services,
including innovative models like ‘safer supply’;
• Key national metrics must be developed
collaboratively and in a way that covers all provinces
and encompasses the full spectrum from prevention,
through enforcement and other interventions, to
treatment and recovery, with a balance between
positive and negative outcomes where possible.
• Alberta and British Columbia should work together to
share learnings as new approaches are adopted in
each province, such as recovery communities in
Alberta, the use of treatment interventions using
Sublocade, or the impact of decriminalisation in BC.
62
Collate and publish more, better data.
• All public authorities and those service providers
funded by the government, should be obliged to
monitor and report on the full set of outputs at every
stage and in a standardised format. Better data that is
published in a more accessible way will aid the media
and public to understand trends and to gauge whether
current approaches are working.
• Existing data that relates to harms should be
augmented with new data relating to benefits, such as
long-term recovery rates and first-time entrants. BC
would benefit from adopting a platform similar to MRP
in Alberta where recovery capital is scored and
tracked.
• Standardised counts are needed for intra-provincial
comparisons, especially of activity-based measures
like safer supply prescribing behaviour, attendance at
overdose prevention sites, and capacity and utilisation
of treatment spaces.
• Data that is not currently published, but which would
enhance public debate, such as the geographic
concentration of drug deaths below the provincial
level, or the costs associated with treatment
programmes, should be released.
• Local population and user surveys that would inform
public understanding of areas like Vancouver’s
Downtown East Side should be commissioned,
including documenting the residency history of drug
users in that area to determine the level of inward
migration.
• Collect and publish more federal and provincial data
on enforcement and criminal justice caseloads related
to drug crime. This would enhance the policy debate,
especially in the context of decriminalisation now
underway in BC, which is affecting possession but is
not meant to lead to a reduction in enforcement
against drug traffickers and those detected and
charged at a local level with more serious offences
like importation or distribution of illicit drugs.

63
Bibliography
2020 Homeless Count in Metro Vancouver. (2020). BC Non-Profit Housing Association.
https://www.vancitycommunityfoundation.ca/sites/default/files/uploads/HC2020_FinalReport.pdf
Adult criminal courts, guilty cases by type of sentence. (2012). Statistics Canada.
https://www150.statcan.gc.ca/t1/tbl1/en/cv.action?pid=3510003001
Adulterants, Contaminants and Co-occurring Substances in Drugs on the Illegal Market in Canada. (2020). Canadian Centre on
Substance Use and Addiction. https://www.ccsa.ca/sites/default/files/2020-04/CCSA-CCENDU-Adulterants-Contaminants-
Co-occurring-Substances-in-Drugs-Canada-Report-2020-en.pdf
Alberta, B.C., and two different approaches to fight Canada’s epidemic of drug deaths. (2022, October 11). The Globe and
Mail. https://www.theglobeandmail.com/opinion/editorials/article-alberta-bc-and-two-different-approaches-to-fight-
canadas-epidemic-of/
Alberta Opioid Response Surveillance Report: First Nations People in Alberta. (2021). The Alberta First Nations Information
Governance Centre. https://open.alberta.ca/dataset/ef2d3579-499d-4fac-8cc5-94da088e3b73/resource/1d3c4477-7a5b-
40a8-90f0-a802dbfd7748/download/health-alberta-opioid-response-surveillance-report-first-nations-people-2021-06.pdf
Ali, F., Russell, C., Nafeh, F., Rehm, J., LeBlanc, S., & Elton-Marshall, T. (2021). Changes in substance supply and use
characteristics among people who use drugs (PWUD) during the COVID-19 global pandemic: A national qualitative
assessment in Canada. International Journal of Drug Policy, 93, 103237. https://doi.org/10.1016/j.drugpo.2021.103237
Amato, S. (2022, April 11). Edmonton moves forward on decriminalizing ‘simple personal possession’ of drugs. CTV News.
https://edmonton.ctvnews.ca/edmonton-moves-forward-on-decriminalizing-simple-personal-possession-of-drugs-
1.5857543
BC Coroners Service Death Review Panel: A Review of Illicit Drug Toxicity Deaths. (2022). BC Coroners Service.
https://www2.gov.bc.ca/assets/gov/birth-adoption-death-marriage-and-divorce/deaths/coroners-service/death-review-
panel/review_of_illicit_drug_toxicity_deaths_2022.pdf
B.C. introduces new prescribed safer supply policy, a Canadian first. (2021, July 15). BC Gov News.
https://news.gov.bc.ca/releases/2021MMHA0035-001375

64
Bhatti, A. (2017, October 16). Waitlists Are Growing in Alberta for Treatment Centres. Andy Bhatti.
https://andybhatti.com/insights/waitlists-growing-alberta-treatment-centres/
Canadian Alcohol and Drugs Survey (CADS): 2019 detailed tables. (2021). [Surveys]. Government of Canada.
https://www.canada.ca/en/health-canada/services/canadian-alcohol-drugs-survey/2019-summary/detailed-tables.html
Canadian area-level characteristics of substance-related acute toxicity deaths, 2016 to 2017. (2022). Government of Canada.
https://www.canada.ca/en/health-canada/services/opioids/data-surveillance-research/area-level-characteristics-substance-
related-acute-toxicity-deaths-analysis-coroner-medical-examiner-data.html
Canadian Substance Use Costs and Harms. (2020). Canadian Centre on Substance Use and Addiction.
https://csuch.ca/publications/CSUCH-Canadian-Substance-Use-Costs-Harms-Report-2020-en.pdf
Cassie, R., Hayashi, K., DeBeck, K., Milloy, M.-J., Cui, Z., Strike, C., West, J., & Kennedy, M. C. (2022). Difficulty accessing
supervised consumption services during the COVID-19 pandemic among people who use drugs in Vancouver, Canada.
Harm Reduction Journal, 19(1), 126. https://doi.org/10.1186/s12954-022-00712-7
CDC Wonder. (2023). CDC Centers for Disease Control and Prevention.
https://wonder.cdc.gov/controller/datarequest/D76;jsessionid=84DD69593B4BE7EF99009F793AEA
Changes in life expectancy by selected causes of death, 2017. (2019). Statistics Canada.
https://www150.statcan.gc.ca/n1/daily-quotidien/190530/dq190530d-eng.htm
COVID-19 daily epidemiology update. (2020). [Datasets;statistics;education and awareness]. Public Health Agency of Canada.
https://www.canada.ca/en.html
Cowie, A. (2022, May 21). Powell River and Bella Coola to receive funding for complex-care housing. CityNews.
https://vancouver.citynews.ca/2022/05/21/bc-complex-care-housing/
Deaths related to drug poisoning in England and Wales. (2020). Office for National Statistics.
https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsrelatedtodrugp
oisoninginenglandandwales/2019registrations
Dickson, L. (2022, August 28). People seeking detox treatment face weeks-long waits. Times Colonist.
https://www.timescolonist.com/local-news/people-seeking-detox-treatment-face-weeks-long-waits-5749399
Digital Overdose Response System. (n.d.). DORSAPP. Retrieved 6 March 2023, from https://www.dorsapp.ca

65
Drug Overdose Deaths: Death Rate Maps & Graphs. (2022). Centers for Disease Control and Prevention.
https://www.cdc.gov/drugoverdose/deaths/index.html
Felbab-Brown, K. H., Jonathan P. Caulkins, and Vanda. (2020, January 13). What the US and Canada can learn from other
countries to combat the opioid crisis [Brookings]. https://www.brookings.edu/blog/order-from-chaos/2020/01/13/what-the-
us-and-canada-can-learn-from-other-countries-to-combat-the-opioid-crisis/
Felbab-Brown, V. (2020). Fentanyl and Geopolitics. Brookings Institution. https://www.brookings.edu/wp-
content/uploads/2020/07/8_Felbab-Brown_China_final.pdf
Fentanyl Facts. (2022, February 23). Centers for Disease Control and Prevention.
https://www.cdc.gov/stopoverdose/fentanyl/index.html
Framework for Action: A Four Pillar Approach to Vancouver’s Drug Problems. (2001). City of Vancouver.
https://council.vancouver.ca/010430/rr1.htm
French, J. (2020, November 7). Financial hurdle gone: Alberta first province to eliminate fees for addiction recovery programs.
CBC. https://www.cbc.ca/news/canada/edmonton/financial-hurdle-gone-alberta-first-province-to-eliminate-fees-for-
addiction-recovery-programs-1.5793854
Frequently asked questions (FAQ): Drug overdose deaths in Europe. (2022). European Monitoring Centre for Drugs and Drug
Addiction. https://www.emcdda.europa.eu/publications/topic-overviews/content/faq-drug-overdose-deaths-in-
europe_en#question4
Get Naloxone. (n.d.). Alberta Health Services. Retrieved 6 March 2023, from
https://www.albertahealthservices.ca/info/page15586.aspx#:~:text=There%20are%20over%202%2C000%20sites,a%20kit
%20free%20of%20charge
Gisèle Carrière, Claudia Sanmartin, & Rochelle Garner. (2021). Understanding the socioeconomic profile of people who
experienced opioid overdoses in British Columbia, 2014 to 2016. Statistics Canada.
https://www150.statcan.gc.ca/n1/pub/82-003-x/2021002/article/00003-eng.htm
Gisèle Carrière, Rochelle Garner, & Claudia Sanmartin. (2018). Social and economic characteristics of those experiencing
hospitalizations due to opioid poisonings. Statistics Canada. https://www150.statcan.gc.ca/n1/pub/82-003-
x/2018010/article/00002-eng.htm
Government Communications and Public. (n.d.). Reducing stigma—Province of British Columbia. Government of BC; Province
of British Columbia. Retrieved 8 March 2023, from https://www2.gov.bc.ca/gov/content/overdose/reducing-stigma

66
Graveland, B. (2022, January). It’s too soon to support drug decriminalization: Alberta police chiefs. Global News.
https://globalnews.ca/news/8527587/alberta-police-chiefs-drug-decriminalization/
Greg Moreau. (2022). Police-reported crime statistics in Canada, 2021. Canadian Centre for Justice and Community Safety
Statistics. https://www150.statcan.gc.ca/n1/pub/85-002-x/2022001/article/00013-eng.htm
Grochowski, S. (2021, April 20). B.C. announces historic half-billion-dollar funding for overdose crisis, mental health. Maple
Ridge - Pitt Meadows News. https://www.mapleridgenews.com/news/b-c-announces-historic-half-billion-dollar-funding-for-
overdose-crisis-mental-health/
Grochowski, S. (2022, February). What is safe supply? A look at what B.C. drug users, advocates are demanding. Vancouver
Sun. https://vancouversun.com/news/local-news/safe-supply
Harm Reduction—Reducing Stigma. (2019). Government of Alberta. https://www.albertahealthservices.ca/assets/info/hrs/if-hrs-
reducing-stigma.pdf
Health characteristics, annual estimates. (2022). Statistics Canada.
https://www150.statcan.gc.ca/t1/tbl1/en/cv.action?pid=1310009601
Homeless shelter capacity, bed and shelter counts for emergency shelters, transitional housing and domestic violence shelters
for Canada and provinces, Infrastructure Canada. (2022). Statistics Canada.
https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1410035301
How Alberta is tackling its toxic drug crisis. (2022). The Drug and Alcohol Testing Association of Canada. https://datac.ca/how-
alberta-is-tackling-its-toxic-drug-crisis/?locale=en
Humphreys, K. (2022). Testimony to the Oregon Senate Committee on Judiciary and Ballot Measure 100 Implementation.
https://addictionpolicy.stanford.edu/sites/g/files/sbiybj25011/files/media/file/keith_humphreys_testimony.pdf
Humphreys, K., Shover, C. L., Andrews, C. M., Bohnert, A. S. B., Brandeau, M. L., Caulkins, J. P., Chen, J. H., Cuéllar, M.-F.,
Hurd, Y. L., Juurlink, D. N., Koh, H. K., Krebs, E. E., Lembke, A., Mackey, S. C., Ouellette, L. L., Suffoletto, B., & Timko, C.
(2022). Responding to the opioid crisis in North America and beyond: Recommendations of the Stanford–Lancet
Commission. The Lancet, 399(10324), 555–604. https://doi.org/10.1016/S0140-6736(21)02252-2
Hyshka, E., Anderson-Baron, J., Karekezi, K., Belle-Isle, L., Elliott, R., Pauly, B., Strike, C., Asbridge, M., Dell, C., McBride, K.,
Hathaway, A., & Wild, T. C. (2017). Harm reduction in name, but not substance: A comparative analysis of current
Canadian provincial and territorial policy frameworks. Harm Reduction Journal, 14(1), 50. https://doi.org/10.1186/s12954-
017-0177-7

67
Illicit Drug Overdose Deaths in BC. (2018). BC Coroners Service. https://www2.gov.bc.ca/assets/gov/birth-adoption-death-
marriage-and-divorce/deaths/coroners-service/statistical/illicitdrugoverdosedeathsinbc-findingsofcoronersinvestigations-
final.pdf
Illicit Drug Toxicity Deaths in BC: January 1, 2012—December 31, 2022. (2022). British Columbia Coroners Service.
https://www2.gov.bc.ca/assets/gov/birth-adoption-death-marriage-and-divorce/deaths/coroners-service/statistical/illicit-
drug.pdf
Impact: A Socio-Economic Review of Supervised Consumption Sites in Alberta. (2020). Government of Alberta.
https://open.alberta.ca/dataset/dfd35cf7-9955-4d6b-a9c6-60d353ea87c3/resource/11815009-5243-4fe4-8884-
11ffa1123631/download/health-socioeconomic-review-supervised-consumption-sites.pdf
Incident-based crime statistics, by detailed violations, Canada, provinces, territories, Census Metropolitan Areas and Canadian
Forces Military Police. (2022). Statistics Canada. https://www150.statcan.gc.ca/t1/tbl1/en/cv.action?pid=3510017701
Income inequality statistics across Canada: Canada, provinces and territories, census divisions and census subdivisions.
(2022). Statistics Canada. https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=9810009601
Indigenous population continues to grow and is much younger than the non-Indigenous population, although the pace of
growth has slowed. (2022). Statistics Canada. https://www150.statcan.gc.ca/n1/daily-quotidien/220921/dq220921a-
eng.htm
Jayawardana, S., Forman, R., Johnston-Webber, C., Campbell, A., Berterame, S., Joncheere, C. de, Aitken, M., & Mossialos, E.
(2021). Global consumption of prescription opioid analgesics between 2009-2019: A country-level observational study.
EClinicalMedicine, 42. https://doi.org/10.1016/j.eclinm.2021.101198
Johnson, L. (2022, March). Toxi-City (Part 3): Deadly drugs in Edmonton — How is the Alberta government tackling the
problem? Edmonton Journal. https://edmontonjournal.com/news/politics/toxi-city-part-3-deadly-drugs-in-edmonton-how-is-
the-alberta-government-tackling-the-problem
Johnson, M. (2022, June 14). Let’s face it. Harm reduction has failed. The Hub. https://thehub.ca/2022-06-14/lets-face-it-harm-
reduction-has-failed/
Jones, W., Kurdyak, P., & Fischer, B. (2020). Examining correlations between opioid dispensing and opioid-related
hospitalizations in Canada, 2007–2016. BMC Health Services Research, 20(1), 677. https://doi.org/10.1186/s12913-020-
05530-w

68
Judd, A., & Zussman, R. (2022, May 31). B.C. becomes first province to remove criminal penalties for possession of some hard
drugs. Global News. https://globalnews.ca/news/8882290/bc-overdose-crisis-decriminalize-possession/
Knaak, S., Mantler, E., & Szeto, A. (2017). Mental illness-related stigma in healthcare: Barriers to access and care and
evidence-based solutions. Healthcare Management Forum, 30(2), 111–116. https://doi.org/10.1177/0840470416679413
Kulkarni, A. (2023, January 31). What you need to know about the decriminalization of possessing illicit drugs in B.C. CBC.
https://www.cbc.ca/news/canada/british-columbia/what-you-need-to-know-drugs-british-columbia-1.6727814
Lethbridge supervised consumption site shutting down at month’s end. (2020, August). Calgary Herald.
https://calgaryherald.com/news/local-news/lethbridge-supervised-consumption-site-shutting-down-at-months-end
Lisa, B., & Jessica, H. (2018). Evidence synthesis - The opioid crisis in Canada: A national perspective. Health Promotion and
Chronic Disease Prevention in Canada : Research, Policy and Practice, 38(6), 224–233.
Marital status, age group and gender: Canada, provinces and territories and census metropolitan areas. (n.d.). Statistics
Canada. Retrieved 27 January 2023, from https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=9810012501
McElroy, J., & Clancy, N. (2016, September). Are there enough beds for drug treatment in B.C.? CBC.
https://www.cbc.ca/news/canada/british-columbia/are-there-enough-beds-for-drug-treatment-in-b-c-1.3756420
McGranahan, D. A., & Parker, T. S. (2021). The Opioid Epidemic: A Geography in Two Phases (No. 287; Economics Research
Report). U.S. Department of Agriculture. https://www.ers.usda.gov/webdocs/publications/100833/err-287.pdf?v=1708
Meldrum, M. L. (2016). The Ongoing Opioid Prescription Epidemic: Historical Context. American Journal of Public Health,
106(8), 1365–1366. https://doi.org/10.2105/AJPH.2016.303297
Mental Health and Substance Use During COVID-19. (2023). Canadian Centre on Substance Use and Addiction.
https://www.ccsa.ca/mental-health-and-substance-use-during-covid-19
Moallef, S., DeBeck, K., Fairbairn, N., Cui, Z., Brar, R., Wilson, D., Johnson, C., Milloy, M.-J., & Hayashi, K. (2022). Inability to
contact opioid agonist therapy prescribers during the COVID-19 pandemic in a Canadian setting: A cross-sectional
analysis among people on opioid agonist therapy. Addiction Science & Clinical Practice, 17(1), 73.
https://doi.org/10.1186/s13722-022-00354-x
More than $1B announced for mental health, addictions support in 2023. (2023, March 3). CBC.
https://www.cbc.ca/news/canada/british-columbia/more-than-1b-announced-for-mental-health-addictions-support-in-2023-
1.6763706
69
More than one million naloxone kits shipped in B.C. as overdose crisis continues. (2021, June). BC Centre for Disease Control.
http://www.bccdc.ca/about/news-stories/stories/2021/one-million-naloxone-kits
My Recovery Plan. (n.d.). Government of Alberta. Retrieved 6 March 2023, from https://www.alberta.ca/my-recovery-plan.aspx
Naloxone. (n.d.). CAMH. Retrieved 6 March 2023, from https://www.camh.ca/en/health-info/mental-illness-and-addiction-
index/naloxone
Opioid Agonist Therapy. (n.d.). Island Health. Retrieved 6 March 2023, from https://www.islandhealth.ca/our-services/mental-
health-substance-use-services/opioid-agonist-therapy
Opioid Agonist Therapy Gap Coverage Program. (n.d.). Government of Alberta. Retrieved 6 March 2023, from
https://www.alberta.ca/opioid-agonist-therapy-gap-coverage-program.aspx
Opioid- and stimulant-related harms. (2022). Government of Canada. https://health-infobase.canada.ca/substance-related-
harms/opioids-stimulants/
Overdose Data and First Nations in BC. (2017). First Nations Health Authority.
https://www.fnha.ca/AboutSite/NewsAndEventsSite/NewsSite/Documents/FNHA_OverdoseDataAndFirstNationsInBC_Preli
minaryFindings_FinalWeb_July2017.pdf
Overdose Detection Saves Lives. (n.d.). Brave. Retrieved 6 March 2023, from https://www.brave.coop/
Overdose prevention. (n.d.). Government of BC; Province of British Columbia. Retrieved 6 March 2023, from
https://www2.gov.bc.ca/gov/content/overdose/what-you-need-to-know/overdose-prevention
Panagiotoglou, D. (2022). Evaluating the population-level effects of overdose prevention sites and supervised consumption
sites in British Columbia, Canada: Controlled interrupted time series. PLoS ONE, 17(3), e0265665.
https://doi.org/10.1371/journal.pone.0265665
Pharmacological Treatment. (n.d.). Indian Health Services. Retrieved 6 March 2023, from
https://www.ihs.gov/opioids/recovery/pharmatreatment/
Pierre Poilievre (Director). (2022, November 20). Everything feels broken. https://www.youtube.com/watch?v=UvvMfwUkXrM
Population. (2013). Statistics Canada. https://www150.statcan.gc.ca/n1/pub/12-581-x/2013000/pop-eng.htm#t01
Population and dwelling counts: Canada, provinces and territories. (2022). Statistics Canada.
https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=9810000101

70
Population estimates on July 1st, by age and sex. (2022). Statistics Canada.
https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1710000501
Provincial health officer declares public health emergency. (2016). Government of British Columbia.
https://news.gov.bc.ca/releases/2016HLTH0026-000568
Recovery Community Operations Competitive Grant. (n.d.). Government of Alberta. Retrieved 6 March 2023, from
https://www.alberta.ca/recovery-community-operations-competitive-grant.aspx
Recovery Oriented Care. (2020). Alberta Health Services. https://www.albertahealthservices.ca/assets/info/amh/if-amh-ecc-
recovery-oriented-care.pdf
Richards, G. C., Aronson, J. K., Mahtani, K. R., & Heneghan, C. (2022). Global, regional, and national consumption of controlled
opioids: A cross-sectional study of 214 countries and non-metropolitan territories. British Journal of Pain, 16(1), 34–40.
https://doi.org/10.1177/20494637211013052
Russ, G. (2022, September 27). A tale of two provinces: Assessing the opioid crises in BC and Alberta. Macdonald-Laurier
Institute. https://macdonaldlaurier.ca/a-tale-of-two-provinces-assessing-the-opioid-crises-in-bc-and-alberta-geoff-russ-for-
inside-policy/
Services, A. H. (n.d.). Enhancing Concurrent Capability (ECC) Toolkit. Alberta Health Services. Retrieved 6 March 2023, from
https://www.albertahealthservices.ca/info/Page14889.aspx
Somers, J. M., Moniruzzaman, A., & Rezansoff, S. N. (2016). Migration to the Downtown Eastside neighbourhood of Vancouver
and changes in service use in a cohort of mentally ill homeless adults: A 10-year retrospective study. BMJ Open, 6(1),
e009043. https://doi.org/10.1136/bmjopen-2015-009043
Substance use surveillance data. (2023). Government of Alberta. https://www.alberta.ca/substance-use-surveillance-data.aspx
Supervised Consumption Services: Operational Guidance. (2017). British Columbia Centre on Substance Use.
https://www.bccsu.ca/wp-content/uploads/2017/07/BC-SCS-Operational-Guidance.pdf
Take Home Naloxone. (n.d.). Towards the Heart. Retrieved 6 March 2023, from https://towardtheheart.com/naloxone
Terminology. (n.d.). Indigenous Foundations. Retrieved 30 January 2023, from
https://indigenousfoundations.arts.ubc.ca/terminology/

71
The Daily — To buy or to rent: The housing market continues to be reshaped by several factors as Canadians search for an
affordable place to call home. (2022). Statistics Canada. https://www150.statcan.gc.ca/n1/daily-
quotidien/220921/dq220921b-eng.htm
The Numbers Behind the Opioid Crisis. (2017). Social Capital Project. https://www.lee.senate.gov/services/files/b54a2abb-
978d-4bbb-a868-531cdfaeae7a
The Virtual Opioid Dependency Program (VODP). (n.d.). Health Standards Organization. Retrieved 6 March 2023, from
https://healthstandards.org/leading-practice/virtual-opioid-dependency-program-
vodp/#:~:text=The%20Virtual%20Opioid%20Dependency%20Program%20(VODP)%20is%20a%20service%20delivered,b
uprenorphine%2Fnaloxone%20in%20Central%20Alberta.
Toward an Alberta model of wellness. (2022). Government of Alberta. https://www.alberta.ca/news.aspx
Two years later, Lifeguard App continues to save lives. (2022, May). BC Emergency Health Services.
http://www.bcehs.ca/about/news-stories/stories/two-years-later-lifeguard-app-continues-to-save-lives
Understanding Harm Reduction: Substance Use. (2020). HealthLinkBC. https://www.healthlinkbc.ca/healthlinkbc-
files/understanding-harm-reduction-substance-use
Wasem Alsabbagh, Martin Cooke, Susan J. Elliott, Feng Chang, Noor-Ul-Huda Shah, & Marco Ghobrial. (2022). Stepping up to
the Canadian opioid crisis: A longitudinal analysis of the correlation between socioeconomic status and population rates of
opioid-related mortality, hospitalization and emergency department visits (2000–2017). Government of Canada.
https://www.canada.ca/en/public-health/services/reports-publications/health-promotion-chronic-disease-prevention-
canada-research-policy-practice/vol-42-no-6-2022/canadian-opioid-crisis-longitudinal-analysis-correlation-socioeconomic-
status-population-rates-mortality-hospitalization-emergency-department-visits-2000-2017.html
Wells, V. S. (2023, January 31). 2022 was second deadliest year for toxic drug deaths ever. The Georgia Straight.
https://www.straight.com/news/2022-was-second-deadliest-year-for-toxic-drug-deaths-ever

72
Appendix A: Calculations for COVID-19 and Opioid Life Years Lost, 2020-2021
COVID-19
Age distribution estimates were made based on Canada’s COVID-19 statistics on November 22, 2022.
131
Age
Deaths
Proportion of total
0 to 11
41
0.09%
12 to 19
25
0.05%
20 to 29
144
0.31%
30 to 39
335
0.73%
40 to 49
720
1.56%
50 to 59
2061
4.48%
60 to 69
4889
10.62%
70 to 79
9875
21.45%
80+
27939
60.70%
Total
46029
100.00%
A midpoint was then assigned for each age group (e.g., 20-29 was assigned 25), and subtracted from 75 (e.g., 20-29 that
died of COVID-19 lost an average of 50 life years).
The total number of deaths as of January 1, 2022 (30,145) was assigned the above age distribution and the estimated
number of deaths in each age group multiplied by the midpoint of LYL. The sum of LYL was then taken for the report.
Age
Deaths
LYL by age (75 - midpoint)
Sum of LYL Lost
0 to 11
26.85144148
70
1879.600904
12 to 19
16.37283017
60
982.3698103
20 to 29
94.30750179
50
4715.37509
30 to 39
219.3959243
40
8775.836972
40 to 49
471.537509
30
14146.12527
50 to 59
1349.776119
20
26995.52239
60 to 69
3201.870668
10
32018.70668
70 to 79
6467.267918
0
0
80+
18297.62009
0
0
Total
30145
N/A
89513.53712
131
COVID-19 daily epidemiology update. (2020). Public Health Agency of Canada.

73
Opioids
Statistics were provided for both the number and distribution of accidental-apparent opioid toxicity deaths in 2020 and
2021, and these were combined to determine the number of deaths per age group.
132
A midpoint was assigned for each
age group and subtracted from 75, and the estimated number of deaths in each age group multiplied by the midpoint of
lost life years. The sum of lost life years was then taken for the report.
Distribution by age
2020 deaths:
6090
2021 deaths:
7725
2020, %
2021, %
2020, #
2021, #
Total Deaths
LYL by age (75 -
midpoint)
Estimated LYL by
Category
0 to 19
2%
2%
121.8
154.5
276.3
65
17959.5
20 to 29
18%
18%
1096.2
1390.5
2486.7
50
124335
30 to 39
27%
29%
1644.3
2240.25
3884.55
40
155382
40 to 49
23%
23%
1400.7
1776.75
3177.45
30
95323.5
50 to 59
21%
20%
1278.9
1545
2823.9
20
56478
60 +
10%
9%
609
695.25
1304.25
0
0
Total
101%
101%
6150.9
7802.25
13953.15
N/A
449478
Due to rounding, the total in the chart is slightly higher than the actual number of deaths.
The lost life years for 60+ was set to 0 to make the above figure a more conservative estimate.
132
Opioid- and stimulant-related harms. (2022). Government of Canada.

74
Appendix B: Estimating Drug User Population Based on CADs Data
The Canadian Alcohol and Drugs Survey (CADS), formerly the Canadian Tobacco, Alcohol and Drugs Survey (CTADS)
measures drug use in a number of ways. For this paper, the ‘any of 5 drugs’ category (2013, 2015, and 2017) and the any
of 6 drugs category (2019) was used to estimate the Canadian user population. These categories were chosen because
they were the most continuous across the shift from CTADS to CADS.
133
The main issue is that, prior to legalization in 2018, cannabis significantly inflated the numbers in most categories when it
came to counting illegal drug use in Canada. The ‘any of 5 drugs’ category in the CTADs excluded cannabis. The ‘any of 6
drugs’ category in the CADS did add salvia (a hallucinogenic), but the use of salvia is relatively low in Canada (In 2019
numbers were too low to estimate past-year use, and only 2.9% of the population reported having used Salvia in their
lifetime).
133
Canadian Alcohol and Drugs Survey (CADS): 2019 detailed tables. (2021). Government of Canada.

75
Appendix C: Terminology for Different Indigenous Groups in Canada
There are a number of different terms for indigenous groups in Canada. Some terms have specific legal meaning.
134
Indigenous: Indigenous is a term that refers to a variety of aboriginal or native groups, often in a global context. In the
United Nations, ‘indigenous’ refers to people of long settlement and connection to specific lands who have been adversely
affected by colonialism.
Aboriginal: in a Canadian context aboriginal refers to the first inhabitants of Canada. Section 35 of the Canadian
Constitution recognizes three aboriginal groups (First Nations, Métis and Inuit).
First Nations: refers to Aboriginal peoples in Canada who are ethnically neither Métis nor Inuit. Often used in place of the
legal term ‘Indian.’
Inuit: Refers to specific groups of people generally living in northern Canada.
Métis: Refers to a collection of cultures and identities that resulted from unions between aboriginal and European people.
Indian: Refers to the legal identity of a First Nations person registered under the Indian Act. Outside of a legal context the
term is often considered offensive.
134
Terminology. (n.d.). Indigenous Foundations.

76
Appendix D: Drivers of the Opioid Crisis
Having reviewed the policy differences between Alberta and BC, the final section of this paper will explore possible
explanations for why the opioid crisis has become so acute in western Canada, as well as factors that may differentiate the
crisis in Alberta verses BC. The following chart breaks down all the factors identified that might be driving the crisis.

77
There are, ultimately, two ways in which factors can increase drug harms. They can increase the number of users, or they
can increase the risk of harm to users. Some factors may do both. For any particular level of harm, the number of users
and the risk of harm will be inversely related.
As previously reviewed, the number of users in Alberta and BC appear to be higher than in other provinces; however, this
difference is not a drastic one. As can be seen from the below table, the ratio of users between Alberta, the province with
the largest user population (proportionately) and Newfoundland/PEI, the provinces with the smallest user populations, was
2.18 in 2019 (4.8/2.2). The ratio between their AAOTDs rates, however, were 5.68 and 4.43 respectively. The AAOTD ratio
between Alberta and Saskatchewan was 1.53, and Saskatchewan has only a 0.1% larger user base than Newfoundland
and PEI. In other words, the size of the user population seems to impact opioid-related harms, but the size of a provinces
user population does not consistently predict AATODs.
135
Note that, due to sample size, the figures used here represent
only rough estimates.
Use of at least one of six illegal drugs, 2019
Canada
BC
AB
SK
MB
On
QC
NB
NS
PE
NL
Past year
3.5%
3.8%
4.8%
2.3%
2.6%
3.5%
3.2%
2.2%
3.2%
2.2%
2.2%
Lifetime
16.1%
17.8%
18.0%
13.4%
16.5%
14.2%
17.8%
19.4%
16.9%
12.1%
12.7%
135
Canadian Alcohol and Drugs Survey (CADS): 2019 detailed tables. (2021). [Surveys]. Government of Canada.

78
Legend
Driver
Possible Driver
Not a Driver
Out of Scope
Toxicity
Improved Product
Policing and Enforcement
Prescribing and
Dispensation
Technology
Point of Entry
Criminal Networks
Services
Immigration
Gender/Age
Income and Inequality
Housing and Homelessness
Ethnicity
Marriage Rates
Drug Culture and Stigma
Physical and Mental Health
136
Substance use surveillance data. (2023). Government of Alberta.
Increased Toxicity
As previously discussed, drug toxicity appears to be a major factor in opioid harms in
Canada. Though there is not a significant amount of data available, that which is available
suggests that fentanyl is significantly more prominent in BC than in the rest of the
country. Though data was not provided for Alberta, fentanyl has been detected in the
majority of Alberta’s accidental drug poisonings (93% in 2021).
136
Based on the alignment between AATODs and fentanyl detection as previously identified
in the report and the lack of correlation between the user population and AAOTDs, the
toxicity of the supply seems like the single most significant determinant of opioid-related
harms.
Unfortunately, since there was not data available regarding the prevalence of fentanyl in
Alberta’s illicit drug supply seized by police, it is not possible to compare the significance
of this factor between the two provinces.

79
Legend
Driver
Possible Driver
Not a Driver
Out of Scope
Toxicity
Improved Product
Policing and Enforcement
Prescribing and Dispensation
Technology
Point of Entry
Criminal Networks
Services
Immigration
Gender/Age
Income and Inequality
Housing and Homelessness
Ethnicity
Marriage Rates
Drug Culture and Stigma
Physical and Mental Health
Improved Product
One way to enhance demand for a product is to make better products. As far as drugs
are concerned, this might entail improved delivery mechanisms, advertising, or providing
‘better’ drugs. Unfortunately, it was not within the scope of this project to conduct the
investigation that exploring this factor would require.

80
Legend
Driver
Possible Driver
Not a Driver
Out of Scope
Toxicity
Improved Product
Policing and Enforcement
Prescribing and Dispensation
Technology
Point of Entry
Criminal Networks
Services
Immigration
Gender/Age
Income and Inequality
Housing and Homelessness
Ethnicity
Marriage Rates
Drug Culture and Stigma
Physical and Mental Health
Policing and Enforcement
The extent to which policing, and enforcement has impacted opioid harms in different
provinces is unclear. Consider the following factors:
- Leading up to 2020 Alberta charged significantly more people for drug crimes
than BC. In 2019, Alberta charged 38 people per 100,000 for TPD-related crimes,
while BC only charged 22.
- As a ratio of charges to incidents, 82% of incidents in Alberta result in a charge,
while only 29% of incidents in BC result in a charge.
- Charges and recorded incidents both dropped with the onset of COVID-19,
suggesting that police backed off enforcement.
- There was a significant drop in opioid-related harms immediately prior to the
pandemic which can most likely be attributed to supply-side interventions in
China.
From these facts, it is difficult to determine how policing impacts opioid-related harms.
Drug markets are also subject to upstream enforcement and interdiction, and to seizures
of illicit drugs entering Canada or being produced domestically. There is no public
declaration of drug volumes seized at provincial level by police and customs in Canada,
however the volume of charges in BC for serious drug offences (i.e. other than
possession cases) is low and has dropped in recent years.
In terms of an enforcement role, they could be a relation between decreased policing
during the pandemic and increased harms, if it enabled illicit market actors to become
more assertive. As the worst affected province, BC seems to do minimal enforcement
around drugs in terms of users, and very low volumes of active charges in the case of
drug supply, importation and trafficking.
Supply-side interventions in markets like China where much fentanyl is produced
seemed to reduce drug harms in 2019 but establishing causality is problematic because
of wider changes occurring at the same time.
81
Set in contrast to BC, higher levels of enforcement in Alberta do not seem to have insulated the province from drug-
related harms. Also, supply-side interventions may have only pushed innovation in the Canadian black market, driving
dealers to find ways to produce opioids and other drugs in Canada rather than importing it, or shifting to new production
areas like Mexico. Ultimately, further investigation is needed into the relation between enforcement and opioid harms, and
the current experiment in decriminalisation of drug possession in BC also warrants thorough, federal evaluation to
determine its impact, including on the illicit market itself.

82
Legend
Driver
Possible Driver
Not a Driver
Out of Scope
Toxicity
Improved Product
Policing and Enforcement
Prescribing and Dispensation
Technology
Point of Entry
Criminal Networks
Policies and Services
Immigration
Gender/Age
Income and Inequality
Housing and Homelessness
Ethnicity
Marriage Rates
Drug Culture and Stigma
Physical and Mental Health
137
Substance use surveillance data. (n.d.). Government of Alberta.
138
Jones, W., Kurdyak, P., & Fischer, B. (2020). Examining
correlations between opioid dispensing and opioid-related
Prescribing and Dispensation
As previously discussed, high levels of historical opioid prescribing played an important
role in the development of Canada’s opioid crisis. Given that Canada is still the fourth-
largest consumer of opioids per capita, it would make sense that prescribing still plays a
role in the crisis.
However, the available evidence suggests that its current impact in Canada’s hotspots is
relatively small compared to illicit opioids. For example, in Alberta there were 1,471
acute accidental drug poisoning deaths related to opioids. Only 5% (78) of these deaths
were attributed to pharmaceutical opioids.
137
One study found that, between 2007 and 2016, dispensing rates were correlated with
opioid-related hospitalization in three provinces, Quebec, New Brunswick, and Nova
Scotia. This suggests that dispensing levels still have an impact on opioid harms in
Canada, but likely has a minimal impact in BC and Alberta given the relative importance
of their illicit markets.
138
hospitalizations in Canada, 2007–2016. BMC Health Services
Research, 20(1), 677.

83
Legend
Driver
Possible Driver
Not a Driver
Out of Scope
Toxicity
Improved Product
Policing and Enforcement
Prescribing and Dispensation
Technology
Point of Entry
Criminal Networks
Policies and Services
Immigration
Gender/Age
Income and Inequality
Housing and Homelessness
Ethnicity
Marriage Rates
Drug Culture and Stigma
Physical and Mental Health
139
Ali, F., Russell, C., Nafeh, F., Rehm, J., LeBlanc, S., & Elton-
Marshall, T. (2021). Changes in substance supply and use
characteristics among people who use drugs (PWUD) during the
Technology
Technological innovation could be playing a role in the availability of opioids in Canada.
Given that supply chains have been disrupted twice in recent years, first by regulatory
change in China and second by the pandemic, it would not be surprising if new
production technology has been developed in the black market. One report found that a
contributing factor to the worsening AAOTD rate during COVID-19 was producers
experimenting with alternative substances and precursors.
139
However, finding specific data on the impacts of technological innovation is beyond the
scope of this project.
COVID-19 global pandemic: A national qualitative assessment in
Canada. International Journal of Drug Policy, 93, 103237.

84
Legend
Driver
Possible Driver
Not a Driver
Out of Scope
Toxicity
Improved Product
Policing and Enforcement
Prescribing and Dispensation
Technology
Point of Entry
Criminal Networks
Policies and Services
Immigration
Gender/Age
Income and Inequality
Housing and Homelessness
Ethnicity
Marriage Rates
Drug Culture and Stigma
Physical and Mental Health
Point of Entry
Given Vancouver’s status as a major port and BC’s relative proximity to China, it makes a
certain amount of sense that illicit opioids would enter Canada on the west coast. This
may partially explain why fentanyl is so much more present in the drug supply in BC and
Alberta (and the Yukon) than in other more eastern regions. However, international illicit
drug trafficking would also have been hindered by the pandemic, and during this period
drug harms increased drastically.
It was ultimately beyond the resources of this project to investigate whether being on the
western side of Canada facilitated drug harms in Alberta and BC. However, it seems
highly unlikely that this factor has not played a role in the proliferation of fentanyl in
western Canada.

85
Legend
Driver
Possible Driver
Not a Driver
Out of Scope
Toxicity
Improved Product
Policing and Enforcement
Prescribing and Dispensation
Technology
Point of Entry
Criminal Networks
Immigration
Gender/Age
Income and Inequality
Housing and Homelessness
Ethnicity
Marriage Rates
Drug Culture and Stigma
Physical and Mental Health
140
RCMP, “2021 Report: Organized Crime in Canada,” Criminal
Intelligence Service Canada (Government of Canada, 2021).
Criminal Networks
It is undoubtedly and increasingly difficult to dispute the role of organized crime in
facilitating the accessibility of illicit drugs to the Canadian populace. In fact, a 2021
RCMP report highlighted that there are well over 2600 active Organized Crime Groups
(OCGs) that continue to contribute to both fentanyl-related deaths and
methamphetamine addiction.
140
Moreover, the same report concludes that there has
been a rapid increase in OCGs involved introducing higher-risk opioids, such as
Isotonitazene, which is even more potent than fentanyl.
141
Therefore, it is difficult to
divorce criminal networks from the opioid crisis.
Nevertheless, while evidence may exist that criminal networks are germane to the
proliferation of toxic drug supplies throughout the country, tracking, investigating, and
analyzing the actions of OCGs and the subsequent impact on the opioid crisis in BC and
Alberta is beyond the scope of this project.
141
RCMP, “2021 Report: Organized Crime in Canada.”

86
Legend
Driver
Possible Driver
Not a Driver
Out of Scope
Toxicity
Improved Product
Policing and Enforcement
Prescribing and Dispensation
Technology
Point of Entry
Criminal Networks
Immigration
Gender/Age
Income and Inequality
Housing and Homelessness
Ethnicity
Marriage Rates
Drug Culture and Stigma
Physical and Mental Health
142
2020 Homeless Count in Metro Vancouver. (2020). BC Non-Profit
Housing Association.
Immigration
The authors explored whether geographic explanations might play a role in the
concentration of drug harms, and considered whether inward migration to BC may be
partially responsible for the scale of drug harms in the province, and in Vancouver in
particular.
Survey data on residency of drug users is not collected routinely. However, those
suffering drug harms in BC are notably older than in the rest of the country. This could
be because older drug users have migrated to BC, attracted by its reputation as a
service centre, or to be among other users. Significant congregation of drug users from
other provinces in BC could partly explain the elevated levels of drug harms there.
Second, a notable portion (15%) of homeless people in Vancouver were found to be
recent arrivals in the city’s 2020 point-in-time homeless count,
142
however, there was not
comparable data from other point-in-time counts. Ultimately it seems plausible that
inward migration impacts drug harms in BC, but there is minimal data to support this as a
key driver and more surveys would be needed to profile the current user population.

87
Legend
Driver
Possible Driver
Not a Driver
Out of Scope
Toxicity
Improved Product
Policing and Enforcement
Prescribing and Dispensation
Technology
Point of Entry
Criminal Networks
Immigration
Gender/Age
Income and Inequality
Housing and Homelessness
Ethnicity
Marriage Rates
Drug Culture and Stigma
Physical and Mental Health
143
Population and dwelling counts: Canada, provinces and territories.
(2022). Statistics Canada.
Gender/Age
Opioid harms are significantly weighted towards 30-to-60-year-old-men. As a proportion
of population, 30-to-60-year-old-men are most concentrated in BC and Alberta,
exempting the Yukon and Northwest Territories.
143
30-60-Year-Old-Men, % of total regional population (2021 data)
Canada
BC
AB
SK
MB
ON
QC
NB
NS
PE
NL
20.09%
20.26%
21.41%
19.72%
19.25%
19.88%
20.11%
19.25%
18.87%
18.27%
19.47%
However, the difference is not significant enough to have much of an impact on harm
statistics. The difference between the province with the most 30-60-year-old-men
(Alberta) and the least (PEI) is 3.14%. In Alberta 3.14% of the population represents
about 140,000 people, which, with a death rate of 36.2
144
, would represent about 50
deaths in 2021 out of 1,608, or about 3%.
144
Opioid- and stimulant-related harms. (2022). Government of
Canada.

88
Legend
Driver
Possible Driver
Not a Driver
Out of Scope
Toxicity
Improved Product
Policing and Enforcement
Prescribing and Dispensation
Technology
Point of Entry
Criminal Networks
Immigration
Gender/Age
Income and Inequality
Housing and Homelessness
Ethnicity
Marriage Rates
Drug Culture and Stigma
Physical and Mental Health
145
The Gini Index is a measure of wealth distribution across a
population. A score of zero means everyone has exactly the same
amount of wealth, and a score of 1 means exactly 1 person owns all
of the wealth.
Income and Inequality
As previously reviewed, opioid-related harms fall more heavily on the poor than on the
wealthy. Further, AAOTDs increase in a relatively linear fashion from the highest income
quintile to the lowest. This suggests that relative wealth, rather than material deprivation,
plays a role in opioid-related harms.
BC and Alberta are two of the most unequal provinces in Canada based on their Gini
index
145
, as can be seen in the below table.
146
Provincial Gini Index based on Adjusted Household After-Tax Income, 2020
Canada
BC
AB
SK
MB
ON
QC
NB
NS
PE
NL
0.302
0.306
0.307
0.293
0.290
0.308
0.280
0.272
0.282
0.271
0.290
The exact impact of this inequality, however, is difficult to determine. Based on available
data and the scope of this project the most that can be said is that inequality may be
impacting levels of opioid-related harms.
146
Income inequality statistics across Canada: Canada, provinces
and territories, census divisions and census subdivisions. (2022).
Statistics Canada.

89
Legend
Driver
Possible Driver
Not a Driver
Out of Scope
Toxicity
Improved Product
Policing and Enforcement
Prescribing and Dispensation
Technology
Point of Entry
Criminal Networks
Immigration
Gender/Age
Income and Inequality
Housing and Homelessness
Ethnicity
Marriage Rates
Drug Culture and Stigma
Physical and Mental Health
147
The Daily — To buy or to rent: The housing market continues to
be reshaped by several factors as Canadians search for an
affordable place to call home. (2022). Statistics Canada.
Housing and Homelessness
There is insufficient evidence to suggest that housing characteristics impact opioid-
related harms.
Those who are renting or who are homeless are notably more likely to suffer drug-
related harms than those who own their own home. Home ownership is lower than
average in BC, and higher than average in Alberta, but neither province stands out
significantly.
147
Homeownership rates by region, 2021
Canada
BC
AB
SK
MB
ON
QC
NB
NS
PE
NL
69.0%
66.8%
70.9%
70.7%
67.4%
59.9%
59.9%
73.0%
66.8%
68.8%
75.7%
Homelessness is, unfortunately, difficult to count. A very rough estimate can be made by
looking at the number of homeless shelter beds across the provinces. However, even
though there are more beds in Alberta and BC, it is unclear whether this is an accurate
proxy for homeless populations in the province.
148
Homeless Beds per 100,000 across all shelter types, 2021
Canada
BC
AB
SK
MB
ON
QC
NB
NS
PE
NL
0.88
1.01
1.00
0.79
0.85
0.66
0.77
0.87
0.71
0.51
0.66
148
Homeless shelter capacity, bed and shelter counts for emergency
shelters, transitional housing and domestic violence shelters for
Canada and provinces, Infrastructure Canada. (2022). Statistics
Canada.

90
Legend
Driver
Possible Driver
Not a Driver
Out of Scope
Toxicity
Improved Product
Policing and Enforcement
Prescribing and Dispensation
Technology
Point of Entry
Criminal Networks
Immigration
Gender/Age
Income and Inequality
Housing and Homelessness
Ethnicity
Marriage Rates
Drug Culture and Stigma
Physical and Mental Health
149
Gisèle Carrière, Rochelle Garner, & Claudia Sanmartin. (2018).
Social and economic characteristics of those experiencing
hospitalizations due to opioid poisonings. Statistics Canada.
Ethnicity
As previously discussed, ethnicity has a notable impact on risk of opioid harms. Visible
minorities were significantly under-represented, with only 2.6 per 100,000 being
hospitalized for accidental opioid poisonings between 2011 and 2016. Those who did not
identify as a member of a visible minority, however, were hospitalized at a much higher
rate of 13.2 per 100,000.
149
First Nations people were significantly over-represented. In Alberta, for example, in
2019, First Nations had an AAOTD rate of 69.5 verses the non-First Nations rate of 11.3.
With that being said, though both Albertan and BC have a higher Indigenous population
than the Canadian average, there are provinces with proportionately higher numbers of
indigenous people. For example, 17% of Saskatchewan’s population identified as
indigenous in 2021, yet the AAOTD rate in the province peaked at 26.3. This suggests
that harms accrue in indigenous communities, but a high indigenous population is not in
itself causal.
Indigenous Population by Region, 2021
Canada
BC
AB
SK
MB
ON
QC
NB
NS
PE
NL
5.0%
5.9%
6.8%
17.0%
4.4%
2.9%
2.5%
4.4%
5.4%
2.2%
9.3%

91
Legend
Driver
Possible Driver
Not a Driver
Out of Scope
Toxicity
Improved Product
Policing and Enforcement
Prescribing and Dispensation
Technology
Point of Entry
Criminal Networks
Immigration
Gender/Age
Income and Inequality
Housing and Homelessness
Ethnicity
Marriage Rates
Drug Culture and Stigma
Physical and Mental Health
150
Marital status, age group and gender: Canada, provinces and
territories and census metropolitan areas. (n.d.). Statistics Canada.
Marriage Rates
As previously discussed, 65% of those who died of illicit toxicity deaths in BC in 2016
and 2017 had never been married, and a further 18% were divorced. This statistic could
represent a proxy for social isolation and low levels of social cohesion.
However, looking at marriage statistics for the provinces, there does not appear to be
any correlation between marriage rates and opioid harms. Alberta and BC do not stand
out when compared with other provinces.
Percentage of Canadians never married or divorced by Province, 2021
150
Canada
BC
AB
SK
MB
ON
QC
NB
NS
PE
NL
35%
34%
34%
34%
35%
35%
37%
32%
34%
33%
31%

92
Legend
Driver
Possible Driver
Not a Driver
Out of Scope
Toxicity
Improved Product
Policing and Enforcement
Prescribing and Dispensation
Technology
Point of Entry
Criminal Networks
Immigration
Gender/Age
Income and Inequality
Housing and Homelessness
Ethnicity
Marriage Rates
Drug Culture and Stigma
Physical and Mental Health
151
Government Communications and Public. (n.d.). Reducing
stigma—Province of British Columbia. Government of BC; Province
of British Columbia.
Drug Culture and Stigma
There is undoubtedly potential for stigma to impact the volume of opioid related deaths.
Moreover, the Government of British Columbia advocates for the reframing of language
when referencing people who use drugs as reducing stigma is believed to improve trust
in government healthcare services and thereby potentially reduce opioid related
deaths.
151
For its part, the Government of Alberta similarly identifies stigma as a barrier to
seeking help for individuals who use substances seeking care, treatment, and recovery
services.
152
While these considerations create a compelling argument for stigma as a
driver, the ability to quantify stigma is beyond the scope of this project.
It is also entirely possible that perceptions of a more pervasive and tolerant drug culture
exist in British Columbia as opposed to Alberta; however, it is difficult to establish
evidence of this reality, or that it would constitute a driver of the opioid crisis in these
provinces, within the scope of this report, due to the limitations around gathering data
from individuals with lived experience.
152
Harm Reduction—Reducing Stigma. (2019). Government of
Alberta.

93
Legend
Driver
Possible Driver
Not a Driver
Out of Scope
Toxicity
Improved Product
Policing and Enforcement
Prescribing and Dispensation
Technology
Point of Entry
Criminal Networks
Immigration
Gender/Age
Income and Inequality
Housing and Homelessness
Ethnicity
Marriage Rates
Drug Culture and Stigma
Physical and Mental Health
153
Health characteristics, annual estimates. (2022). Statistics
Canada.
Physical and Mental Health
It is unclear whether physical and mental health are drivers of the opioid crisis in Alberta
and BC. Perceived mental and physical health varies across the provinces. Health and
mental health in BC is somewhat worse than the Canadian average but Alberta’s is
slightly better, which makes it challenging to draw a causal connection, and it was
beyond the scope of this project to do a more in-depth investigation.
Self-reported perceived health by Province, fair or poor, per 100,000
153
Canada
BC
AB
SK
MB
ON
QC
NB
NS
PE
NL
Health
95.4
126.1
74.8
102.3
91.6
99.6
76.3
132.2
128.8
121.6
126.3
Mental
Health
68.7
84.5
63.4
74.1
67.1
77.1
44.4
78.6
106.7
98.4
67.1
A 2021 USDA study found that physical disability (which was used as a proxy for chronic
pain) tracked opioid harms in the USA between 2000 and 2010.
154
Unfortunately, there is
no comparable data in Canada to draw a similar comparison.
154
McGranahan, D. A., & Parker, T. S. (2021). The Opioid Epidemic:
A Geography in Two Phases (No. 287; Economics Research Report).
U.S. Department of Agriculture.

94
Driver Summary
The primary driver of opioid harms in Alberta and BC appears to be the toxicity of the drug supply. Other factors that the
evidence supports having had an impact are prescribing and dispensation rates and specific gender and age
demographics.
Drivers where the evidence was less definitive include policing and enforcement, immigration, income and socioeconomic
inequality and ethnicity. Relatedly, this project identified several additional issues to consider as potential drivers but were
limited by scope and resources to further investigate. These included improved products, technology, point of entry,
criminal networks and drug culture and stigma, and physical and mental health.
Policies and services, housing and homelessness and marriage rates lacked sufficient evidence to be categorized as
drivers of opioid harms in Alberta and BC. Furthermore, improved product, technology, point of entry, criminal networks,
drug culture and stigma and physical and mental exceeded the scope of this report.
Driver Summary
Drivers
Possible Drivers
Not Drivers
Out of Scope
Toxicity
Policing and
Enforcement
Housing and
Homelessness
Improved Product
Prescribing and
Dispensation
Immigration
Marriage Rates
Technology
Gender/Age
Income and Inequality
Point of Entry
Ethnicity
Criminal Networks
Drug Culture and Stigma
Physical and Mental Health
