
1
2023 Cook County
Employee Benets Overview
Department of Risk Management Employee Benets Division
2
TABLE OF CONTENTS
WELCOME 3
KNOW YOUR BENEFITS 4
THE BASICS
Who Is Eligible To Enroll 5
When You Can Enroll 6
How To Enroll In Benets During Annual Open Enrollment 6
Change Your Benets - Permitted During Qualifying Life Events 7
Enrollment Procedure 8
Required Documents For Dependents 8
Eective Date of Benets Coverage 10
Coordination With Other Coverage 10
Dual Coverage 10
Cost And Funding 10
Calculating Your Coverage 11
Leave Of Absence 11
Termination/COBRA 11
GUIDE TO BENEFITS
Medical Plan 12
Prescription Drug Program 14
Dental Program 15
Vision Program 17
Flexible Spending Accounts (FSAs) 19
Health Care FSA 19
Using Your FSA Funds 19
Dependent Day Care FSA 20
Commuter Benet 21
Income Protection/Life Insurance 22
Voluntary Benets 23
Deferred Compensation Retirement Plan 24
Employee Assistance Program 25
Benets Connect/Well-Being 25
HEALTH AND BENEFITS LITERACY
Denitions 26
REMINDERS AND NOTICES
Reminders 27
Notices 27
Important Benets Contact Information 28
3
E
mployees have unique needs when it comes to benets,
and Cook County oers a comprehensive program so you
can choose what is important to protect the health and
well-being of you and your family.
1
Cook County oers a competitive employee benets package and
remains committed to oering benets at the most aordable cost to
employees. The County provides some benets at no cost to you, some
you pay for, and other benet costs are shared between Cook County
and you.
The information in this guide highlights Cook County’s Employee
Benets and well-being programs, as well as important information
about your rights and responsibilities under the plans. Please take the
time to review this guide carefully. You may only make changes to your
benet elections during the annual Open Enrollment period or if you
experience a Qualifying Life Event such as a marriage, divorce or the
birth/adoption of a child.
This guide, the Employee Benets website www.cookcountyrisk.com,
and the Employee Benets team in the Department of Risk Management
are your resources to educate yourself and choose the options best
for you.
Contact Risk Management by phone at 312-603-6385 or email
at risk.mgmt@cookcountyil.gov if you have questions or need
additional assistance.
1
Every eort is made to ensure the information in this guide is accurate. In the event of a
discrepancy between the information in this guide and the ocial Plan Certicates, the
ocial Plan Certicates govern.
WELCOME
4
KNOW YOUR BENEFITS
Review your benets annually in Employee Self Service (ESS). Medical,
dental and vision enrollments are in eect unless you make changes
during the annual Open Enrollment period each year. You must enroll
in health care and dependent day care exible spending accounts
(FSAs) each year to participate–elections do not carry over from one
year to the next.
Check ESS to make sure your personal information is correct for you and
your dependents.
Name
Date of Birth
Social Security Number
Home Address
Check ESS to make sure your benets enrollment is as expected.
Medical Insurance
Dental Insurance
Vision Insurance
Health Care FSA
Dependent Day Care FSA
Group Basic Term Life
Check the Voluntary Benets webpage on
www.cookcountyvoluntarybenets.com to make sure your
enrollment is as expected.
Group Accident Insurance
Group Critical Illness Insurance
Group Hospital Indemnity Insurance
Short-Term Disability Insurance
Universal Life Insurance
Identity Theft Protection
Legal Service Plan
Check the benets plan site to manage your Group Supplemental Life
and Commuter Benets.
Group Supplemental Life (www.metlife.com/mybenets)
Commuter Benets (www.optumnancial.com)
5
WHO IS ELIGIBLE TO ENROLL
You are eligible to participate in Cook County’s group benet plans if you are:
• An employee working at least 30 hours per week on a regular, year-round basis
• Eligible for participation in Cook County’s group benet plans pursuant to the Board
of Commissioners’ Budget Resolution, a collective bargaining agreement or an
employment agreement
Dependent benets are extended to spouse, domestic partners and civil union partners. If both
the employee and spouse or partner are Cook County employees, all family members must be
covered under one enrollment. Children up to age 26 are eligible for health benets coverage as
dependents. Military veterans may be covered up to the age of 30.
Dependent Verication
When you enroll dependents in the County’s benets, you will be asked to provide information about
each of your eligible dependents, such as name, date of birth, Social Security number (SSN), and gender.
You will also be required to submit documentation of the dependent’s relationship to you. Requested
proof includes a government-issued birth certicate or marriage certicate.
You are required to provide the SSN of each of your dependents. However, if your dependent
does not have a SSN when you enroll, you should continue the enrollment and return to ESS
once you have received the SSN and enter the information.
By enrolling your dependents, you are arming that each dependent you are enrolling meets
all eligibility requirements. If at any time your covered dependent no longer meets eligibility
requirements, you agree to promptly remove that dependent from your coverage.
Coverage Tiers
If you choose to participate in a medical, dental and/or vision plan, you also must choose a
Coverage Tier. The County oers four tiers of coverage in the medical plan:
• Employee Only: Coverage for you only
• Employee Plus Spouse/Partner: Coverage for you and your spouse/partner only
• Employee Plus Child(ren): Coverage for you and your eligible child(ren), including the
eligible child(ren) of your spouse/partner
• Employee Plus Family: Coverage for you, your spouse/partner, your eligible child(ren) and
your spouse’s/partner’s eligible child(ren)
Tiers for the dental and vision plans are Employee Only, Employee +1, and Family.
You can choose a dierent coverage tier for medical, dental and vision. For example, you
might enroll in “Employee Only” coverage for medical if your spouse/partner has medical
coverage from his or her employer and “Employee Plus Spouse/Partner” for dental coverage
if your spouse’s/partner’s employer does not oer dental coverage. If enrolled, you and your
dependents must elect the same plan.
THE BASICS

6
WHEN YOU CAN ENROLL
You can enroll in County coverage within 31 days of the date you rst become eligible, during
the annual Open Enrollment period or within 31 days of a Qualifying Life Event (QLE). Benets
are eective the rst day of the month following the date you became benets eligible, except
for Group Term Life Insurance, which is eective your rst day of employment.
New Hire or Newly Eligible for Benets
As a newly hired benets-eligible employee, or if you are newly eligible for benets, you have
31 days from your date of eligibility to enroll in the County’s benet plans. Enrollment is not
mandatory. The monetary penalty for not having health coverage under the Aordable Care Act
is no longer applicable.
Enrollment in Group Term Basic Life Insurance is automatic. You are not required to enroll in this
benet. If you wish to be enrolled in other benets, you are required to act. You are required to
enroll in the coverages listed below because enrollment is not automatic, and you will not be
defaulted into any plan. All coverage continues each year unless you make changes; however,
you must enroll each year to participate in the Health Care Flexible Spending Account (HCFSA)
and Dependent Day Care Flexible Spending Account (DCAP).
HOW TO ENROLL IN BENEFITS DURING ANNUAL OPEN ENROLLMENT
Choose your benets carefully and understand all your benet options so you can make an
informed decision for the upcoming year.
If you want to enroll in County coverage; drop County coverage; change to a dierent
medical, dental or vision option; enroll in a exible spending account; or change your
coverage tier, for example, from single to family or vice versa, you must do so during
the annual Open Enrollment period. All changes are binding from December 1 through
November 30, unless you experience a QLE. If you experience a QLE, you may add, change
or cancel coverage within 31 days of the event. Benet changes must be made within 31
days of the QLE.
See the Qualifying Life Events section for more information.
Medical, Dental and/or Vision Coverage
If you previously enrolled in coverage and do not change benet elections during a subsequent
annual Open Enrollment period, you will be assigned the same coverage for the following year.
Plan enrollment changes are eective December 1.
*You must enroll in HCFSA and DCAP each year to have coverage.
YOU MUST ENROLL WITHIN 31 DAYS*
TO HAVE COVERAGE:
YOU MAY ENROLL AT ANY TIME
THROUGHOUT THE YEAR:
• Medical coverage
• Dental coverage
• Vision coverage
• Group Supplemental Life
• Health Care and Dependent Day Care
Spending Accounts*
• Voluntary Benets
• Commuter Benets
• Deferred Compensation

7
Health Care Flexible Spending Account (HCFSA) and/or Dependent Day Care Spending Account (DCAP)
FSA enrollments do not carry over so you must re-enroll each year to participate. FSA elections
are eective January 1.
Voluntary Benet Plans
You can enroll each year during annual Open Enrollment (or as a new hire) or within 31 days
of a QLE.
Once you are enrolled, your participation will continue as long as you maintain eligibility requirements
unless you elect to drop coverage during a subsequent annual Open Enrollment period.
After You Enroll or Waive Conrmation of Enrollment
Once you submit your enrollment elections in ESS, you will be able to view your benets elections.
Review your benets elections carefully to conrm they are accurate. You can review your elections
or make changes to your benets until the deadline. All enrollments are nal as of 11:59 p.m. CST on
October 31. A conrmation of your enrollment can be printed from ESS.
CHANGE YOUR BENEFITS – PERMITTED DURING QUALIFYING LIFE EVENTS
Open Enrollment is the annual period available to make changes to your
benets. A Qualifying Life Event (QLE) is required for you to request changes
to your benets outside of the Open Enrollment period. You can enroll, add
or remove dependents; change plans; or enroll in/make changes to a exible
spending account within 31 days of any of the following events:
• Employment
• Marriage, establishment of a partnership (with government-issued
domestic partner certicate or civil union certicate)
• Birth, adoption, or obtaining legal guardianship of a child
• Loss of other coverage for you or your dependent(s) for reasons such as
legal separation, divorce, death, termination of employment or moving outside
of the service area
• A change in employment status signicantly impacting the employee
contribution rate
Changes must be completed through Employee Self Service (ESS) within 31 days of
the QLE. Appropriate dependent documentation must also be uploaded within 31
days. Government-issued newborn birth certicates must be uploaded within 45 days.
Please note: QLE additions are eective on the event date (e.g., due to marriage, birth).
A QLE that terminates participation, such as waived coverage or the removal of a
dependent from coverage (e.g., a divorce, death of a dependent, or aging out),
is eective the last day of the month in which the event occurs.
Enrollments not completed within the designated time frame will not be accepted.
The next opportunity to enroll will be the following annual Open Enrollment period
or within days of another QLE.
If you are not currently enrolled and your QLE does not include a dependent change,
please send an email to risk.mgmt@cookcountyil.gov to set up your eligibility to enroll
in ESS. Enrollments entered more than 31 days after the QLE will not be processed.
Dependent children who reach the age of 26 (30 for military veterans) are
automatically terminated from benet coverage on the last day of the month of the
26th birthday. Special rules apply to disabled dependents.
BE AWARE!
THERE’S ONLY
A 31-DAY
WINDOW TO
MAKE CHANGES!
You must make
changes to your
benets within
31 days of your
life event, or you
will have to wait
until the next
Open Enrollment
period.
Coverage begins
on the date of
the event.

8
ENROLLMENT PROCEDURE
STEP 1: Log in to Employee Self Service (ESS).
To access ESS from within the County’s network, click on the Oracle EBS icon on your
desktop or use www.ccgprod.ccounty.com and then click on the applicable button.
You may also log in to ESS from home at: www.ccgprod.cookcountyil.gov
For assistance with logging into ESS, contact your agency’s technology desk.
STEP 2: Complete your enrollment within 31 days of a QLE or during annual Open
Enrollment using ESS.
Your dependents will not have medical, vision, or dental coverage unless you SUBMIT THE
REQUIRED DOCUMENTATION BY THE DEADLINE.
STEP 3: Upload copies of documents to prove they are your legal dependents.
STEP 4: Print and retain your conrmation statement for your records. This is the only
conrmation of your enrollment.
STEP 5: Monitor your Cook County email. Risk Management will contact you via email
to notify you of any problems with your dependent enrollment or documentation.
Note: You are encouraged to submit documents right away to avoid delays in processing.
REQUIRED DOCUMENTS FOR DEPENDENTS
If you include dependents in your Cook County coverage, you must submit proof of eligibility
for each dependent. Required documents must be scanned and uploaded through ESS.

9
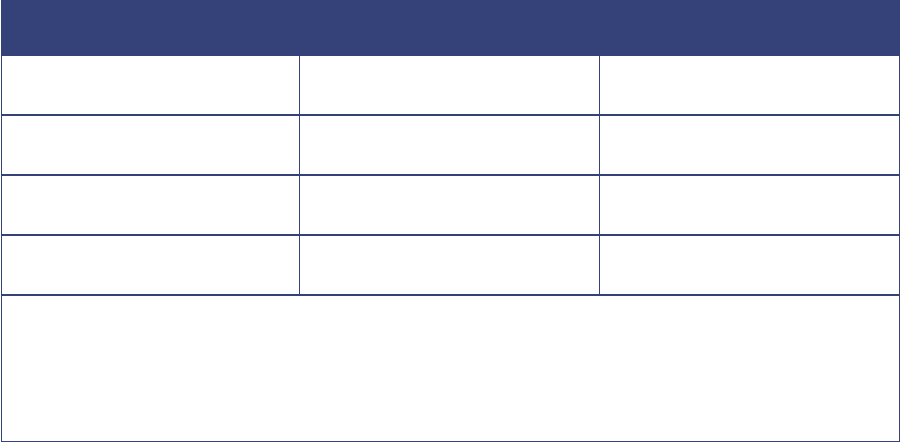
DEPENDENT BEING ENROLLED DOCUMENT(S) REQUIRED
Spouse Government-issued marriage certicate
Child (0-25yrs.) Government-issued birth certicate with
employee’s name listed as parent
Adult Military Dependent Child (Age 26-30)
Illinois Resident
Government-issued certied birth
certicate, proof of Illinois residency, DD
Form 214 indicating discharge other than
dishonorable discharge
Adopted Child At time of placement:
A copy of legal adoption documentation
showing placement in employee’s home
prior to adoption, or one of the following:
• Interim order with judge’s signature and
the circuit court le stamp
• Petition for adoption with the circuit
court le stamp
• Pre-adoptive notarized placement
agreement establishing the employee’s
obligation to provide support for the
child in anticipation of adoption
• Placement papers signed by the court
Within 31 days of nalized adoption:
• Final order of adoption issued
through court, or
• Final adoption certicate issued
through court
Legal Guardianship of Dependent
(Court Appointed)
Certied guardianship documents signed by
judge and stamped by circuit court placing
the child in the home (date of placement)
Civil Union Partner Government-issued civil union certicate
Domestic Partner Government-issued domestic
partnership certicate
What Happens If I Do Not Enroll?
If you do not enroll within 31 days following your hire date or the date you become
eligible for benets, you will not have medical, dental and/or vision coverage through
the County. Additionally, you will not be able to contribute to exible spending accounts.
You will have to wait until the next Open Enrollment or until you experience a QLE.

10
EFFECTIVE DATE OF BENEFITS COVERAGE
New Hire: 1st day of the month following date of hire
Qualifying Life Event:
• Event date when adding coverage (e.g., due to marriage, birth)
• Last day of the month in which the event date occurs when removing coverage
or dependents from coverage
Open Enrollment: December 1 (FSA OE changes begin January 1)
COORDINATION WITH OTHER COVERAGE
If you are eligible for benets coverage elsewhere, for example, through a spouse’s/partner’s
or other employer’s plan, you should compare the County’s coverage and costs to the other
coverage. You may decide to enroll in some plans oered through the County and some from
the other source.
However, if you are enrolling in coverage from two sources, be sure you understand how
benets are paid when you are covered by two group medical plans or group dental plans.
In many instances, you may pay for coverage from two group plans, but you will not receive
double benets or even be reimbursed for 100% of your costs as a result of what is called
“coordination of benets.”
DUAL COVERAGE
Dual coverage is prohibited on all County benet plans for employees and dependents if both
individuals work for Cook County in a benet-eligible position. If a dual-coverage enrollment is
made, the Employee Benets Division will update the enrollment based on a pre-dened order
of benets determination so that each individual is only enrolled in coverage under one record.
Both parties involved in the dual-coverage enrollment will be notied of the change.
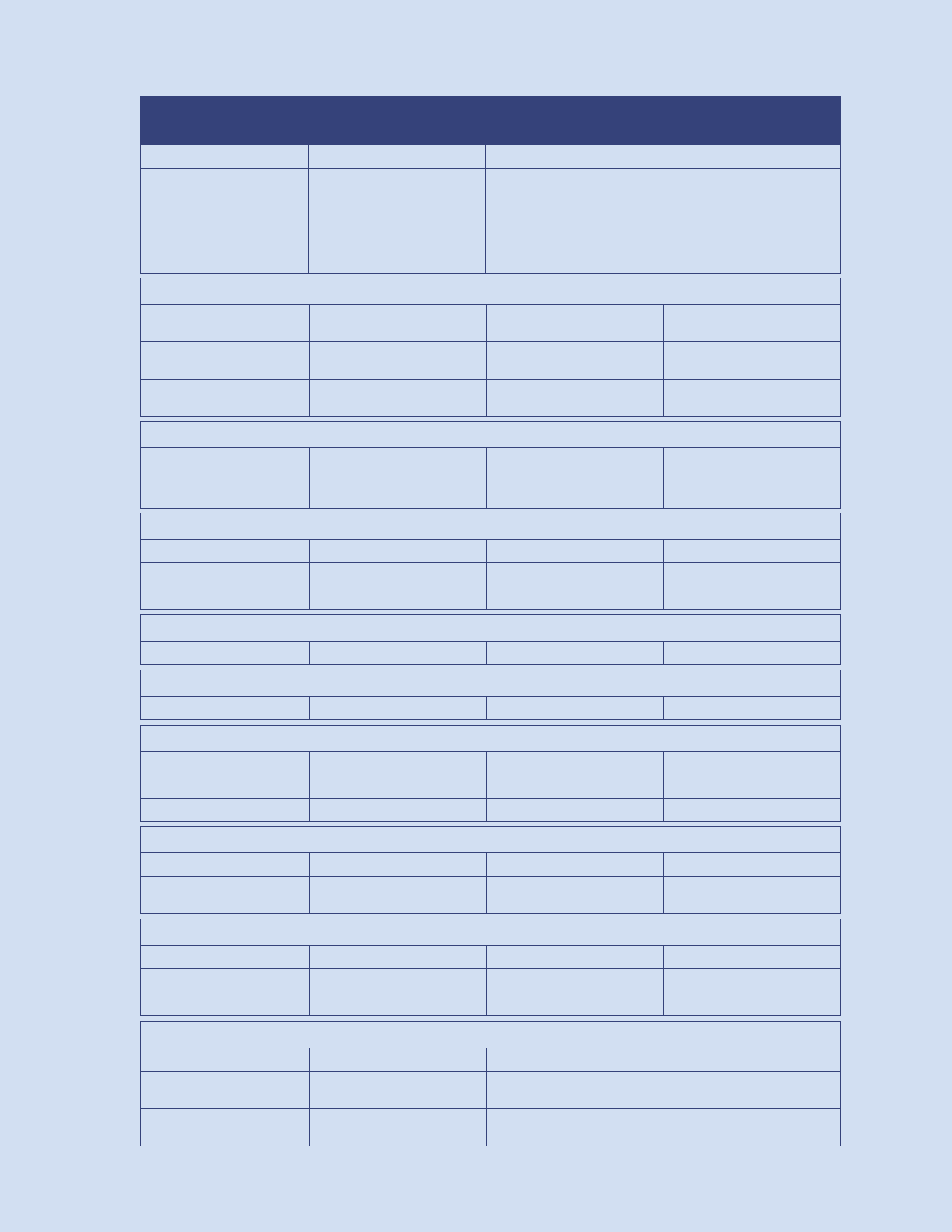
COST AND FUNDING
Contributing to Your Plans
You and the County share the cost for medical coverage, with the County paying the majority of
the costs as shown in the chart below.
For full time employees, your cost is based on the plan and coverage tier you choose and your
annual salary (based on 1.0 FTE) as shown in the chart on the following page:
Cook County pays the
full cost…
• Basic Life Insurance
• Dental Insurance
• Vision Insurance
You pay the full cost…
• Commuter Benets
• Deferred
Compensation
• Flexible Spending
Accounts
• Supplemental Life
Insurance
• Voluntary Benets
You and Cook County
share the cost…
• Medical (including
prescription drug)
11
CALCULATING YOUR COVERAGE
This chart shows your cost as a percentage of pre-tax standard salary based on plan selected
and family members you elect to cover.
HMO PPO
Employee Only 1.75% 2.75%
Employee + Spouse 2.50% 3.50%
Employee + Children 2.25% 3.25%
Employee + Family 3.00% 4.00%
Employees working less than 30 hours/week may contribute at a dierent rate.
Employees on an approved leave of absence remain responsible for their regular payroll
contributions when billed.
Employees on a personal leave of absence are responsible for paying the full County cost for
continued coverage.
LEAVE OF ABSENCE
Part-time Employees and Employees on a Personal Leave of Absence
Part-time employees and employees on a Personal Leave of Absence (PLOA) are required to
notify Risk Management in writing that they wish to enroll in benets or continue coverage
within 31 days of the status change. Once the enrollment or PLOA continuation is processed, Risk
Management will issue and mail a monthly invoice to the employee for payment of insurance.
These employees are required to pay the full County cost of coverage.
Health Insurance Statements
The Department of Revenue issues and mails statements to employees for the payment of
health insurance deductions when they are not able to be deducted from a regular paycheck or
if no paycheck is issued.
Employees on an unpaid leave status must pay their account balances in full or return to work by
the date provided or coverage will be terminated. Employees back at work whose balances are
not paid in full will have their accounts turned over to a collection agency.
TERMINATION / COBRA
Coverage for employee health benets ends on the last day of the month following the
employment termination date.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) allows employees and/or their
dependents to continue certain insurance benets after termination of employment or when a
dependent’s status changes, resulting in loss of coverage. Medical, dental and vision plans can
be continued for up to 18 months under COBRA, or longer in certain circumstances.
Once the COBRA enrollment is processed, Risk Management will issue and mail a monthly
invoice to the employee for the full County cost plus an administrative fee. Employees have 60
days to apply for coverage retroactive to the benets termination date.

12
GUIDE TO BENEFITS
HMO PPO
No deductibles or coinsurance.
Employees are responsible for copays.
There are deductibles, coinsurance
and copays.
Must select a primary care physician.
There is no out-of-network coverage
except in an emergency.
Covers in-network and out-of-network
doctors. Selection of a primary care
physician is strongly encouraged but
not required.
Oers nancial savings for services
obtained in the Domestic tier of coverage.
Requires a referral from your primary
care physician to see a specialist.
Can visit a specialist without a referral.
Pre-certication is required for
certain services.
MEDICAL PLAN
Cook County oers two medical plan options to choose from when selecting coverage for
you and your family. Each medical plan includes a prescription drug benet. Your medical plan
choices are HMO or PPO.
www.bcbsil.com/cookcounty
BlueAdvantage HMO
Group #B03351
1-800-892-2803
Blue Cross Blue Shield PPO
Group #291116
1-800-960-8809

13
Feature HMO Plan
Cook County
Domestic Tier
PPO Plan
In-Network
PPO Plan
Out-of-Network
Annual deductible $0
$350 individual
$700 family
$700 individual
$1,400 family
Out-of-Pocket (OOP) maximum
$1,600 individual
$3,200 family
$2,000 individual
$4,000 family
$4,000 individual
$8,000 family
NOTE: You are responsible for the full cost of any charges that exceed the Schedule of Maximum Allowances (SMA),
sometimes referred to as “R&C” or “reasonable and customary” amount.
Benets HMO Plan
Cook County
Domestic Tier
PPO Plan
In-Network
PPO Plan
Out-of-Network
Primary Care
Primary care visit to treat an
injury or illness
$15 copay/visit $25 copay+10% coinsurance/visit 40% coinsurance/visit
Specialist visit $20 copay/visit $35 copay+10% coinsurance/visit 40% coinsurance/visit
Other practitioner office visit $15 copay/visit $25 copay+10% coinsurance/visit 40% coinsurance/visit
Preventative care/screening/
immunization
$0 copay/visit $0 $0
Outpatient Services
Diagnostic test (x-ray, blood work)
and imaging (CT/PET scans, MRIs)
$0 0% coinsurance
10%
coinsurance
40% of the maximum allowance
Facility fee (e.g., ambulatory
surgery center)
$100 copay/visit 0% coinsurance
10%
coinsurance
40% of the maximum allowance
Physician/surgeon fees $0 10% coinsurance 40% coinsurance
Maternity prenatal/postnatal care
$15 copay/visit
First prenatal visit only
$25 copay/visit+10% coinsurance
First prenatal visit only
40% coinsurance
Mental/behavioral health
outpatient services
$15 copy/visit $25 copay/visit+10% coinsurance 40% coinsurance
Substance use disorder
outpatient services
$15 copy/visit $25 copay/visit+10% coinsurance 40% coinsurance
Emergency Care
Emergency room services $100 $100
Emergency medical transportation $0 Ground transportation only 10% coinsurance
Urgent care
$15 copay/visit
Must be affiliated with chosen
medical group or referral required
$25 copay/visit+10% coinsurance $25 copay+40% coinsurance
Inpatient Benets
Facility fee (e.g., hospital room) $100 copay/visit 0% coinsurance 10% coinsurance 40% coinsurance
Physician/surgeon fee $0 10% coinsurance 40% coinsurance
Mental/behavioral health
inpatient services
$100 copay/admission 0% coinsurance 10% coinsurance 40% coinsurance
Substance use disorder
inpatient services
$100 copay/admission 0% coinsurance 10% coinsurance 40% coinsurance
Delivery and all maternity
inpatient services
$100 copay/admission 0% coinsurance 10% coinsurance 40% coinsurance
Extended Care
Home health care $0 10% coinsurance 40% coinsurance
Skilled nursing care $100 copay/admission 10% coinsurance 40% coinsurance
Hospice service $0 10% coinsurance 40% coinsurance
NOTE: Effective 12/1/21, The County PPO plan will incorporate a Cook County Health tier (“Domestic Tier”) wherein covered members will have lower
out-of-pocket costs when choosing to access health care within CCH faciities. Facility charges will be 0% after the annual plan deductible is met.
Hospital-based facility services not obtained at CCH will be paid based on their network status (in or out of network rate.)
SUMMARY OF HEALTH BENEFITS

14
30-DAY SUPPLY AT RETAIL 90 -DAY SUPPLY *
Generic $15 $30
Formulary brand on the drug list $30 $60
Non-formulary brand not on
the drug list
$50 $100
PRESCRIPTION DRUG PROGRAM
When you enroll in a medical plan, you automatically receive prescription drug coverage
through CVS Health. Prescriptions can be purchased through your local pharmacy or mail order.
CVS Health pharmacy is included in all Target stores that oer pharmacy services. Prescription
copays range from $15 to $100 depending on your prescription.
You will save money by purchasing generic drugs rather than brand-name drugs.
Maintenance Choice Program
The Maintenance Choice Program is mandatory. After two lls, all maintenance medications
must be lled in a 90-day supply through mail order or at a CVS Pharmacy.
*If you choose to buy a formulary brand (on the drug list) or non-formulary brand (not on the drug
list) when a generic substitute is available, you will pay the generic copay, plus the dierence in
cost between the generic and the full retail formulary brand or non-formulary brand drug cost.
You must ask your doctor to write a 90-day supply prescription and get it lled at your
CVS Pharmacy.
Generic Step Therapy Program
The Generic Step Therapy Program requires members to use up to two generic alternatives in
certain drug classes before a brand will be covered.
www.caremark.com
1-866-409-8522

15
DENTAL PROGRAM
Dental coverage is provided to employees and enrolled dependents at no charge. Regular
visits to the dentist can do more than just brighten your smile; they can also be important to
your overall health.
County employees have a choice of two dental plans:
• Guardian Dental HMO provides access to services performed at participating dental
HMO practices
• Guardian Dental PPO allows you to seek dental care from dentists who are in or out of
the PPO network, with greater coverage in-network
www.guardiananytime.com/cookcounty
Dental HMO: 1-866-494-4542
Dental PPO: 1-866-302-4542
See the Summary of Dental Plans on page 16
16
Item/Procedure
Dental HMO Copayment
(Member Pays)
Dental PPO
In-Network Out-of-Network
Benefit Period Maximum None $1,500
Deductible None
$25 per Individual
$100 per Family
(4 individual maximums)
Deductible does not apply to
preventive and orthodontic
services
$50 per Individual
$200 per Family
(4 individual maximums)
Deductible does not apply to
preventive and orthodontic
services
Preventative
Dental Exams
(2 exams per benefit period)
$0 100% of the maximum allowance 80% of the maximum allowance
Profylaxis
(2 exams per benefit period)
$0 100% of the maximum allowance 80% of the maximum allowance
Fluoride Treatment
(2 exams per benefit period)
Once every 24 months 100% of the maximum allowance 80% of the maximum allowance
Primary Services
Dental X-Rays $0 80% of the maximum allowance 60% of the maximum allowance
Space Maintainers
(eligible members up to age 19)
$63-$96 80% of the maximum allowance 60% of the maximum allowance
Oral Surgery
Routine Extractions $18-$20 80% of the maximum allowance 60% of the maximum allowance
Removal of Impacted Teeth
(soft tissue and partial bone)
$$50-$65 80% of the maximum allowance 60% of the maximum allowance
Restorative
Amalgams and Anterior Resins $17-$44 80% of the maximum allowance 60% of the maximum allowance
Posterior Resins $53-$105 80% of the maximum allowance 60% of the maximum allowance
Crowns and Fixed Bridges $256-$300 per unit 50% of the maximum allowance 50% of the maximum allowance
Periodontics
Scaling and Root Planing $37/quadrant 80% of the maximum allowance 60% of the maximum allowance
Gingivectomy $111/quadrant 80% of the maximum allowance 60% of the maximum allowance
Osseous Surgery $206/quadrant 80% of the maximum allowance 60% of the maximum allowance
Prosthetics
Full or Partial Dentures $383-$396 50% of the maximum allowance 50% of the maximum allowance
Denture Reline $40-$72 50% of the maximum allowance 50% of the maximum allowance
Endosseous Implants Not covered 50% of the maximum allowance 50% of the maximum allowance
Emergency Services
Palliative Emergency Treatment $0 80% of the maximum allowance 80% of the maximum allowance
Endodontics
Root Canal Therapy $109-$162 80% of the maximum allowance 60% of the maximum allowance
Orthodontics
Adults (19 or older) Not covered 50% of the maximum allowance
Dependent Children (up to age 19)
$3,233-$3,356 not including
x-rays or orthodontic records
50% of the maximum allowance
Lifetime Maximum
One full course of treatment for
dependent children under age 19
$1,250
SUMMARY OF DENTAL PLANS

17
See the Summary of Vision Plans on page 18
VISION PROGRAM
Vision coverage is provided at no charge to employees and enrolled dependents. Eye exams
are an important part of your overall health.
The vision plan is administered by Davis Vision and covers routine eye exams, as well as
prescription eyeglasses and contact lenses. The amount you pay for your vision care depends on
the type of services or eyewear you choose.
Coverage is only available if you use an in-network provider. To locate a Davis Vision
provider, visit:
www.davisvision.com
1-800-381-6420

18
Vision Care
Services
In-Network
Member Cost
Out-of-Network
Reimbursement
Exam with dilation as necessary $0 copay N/A
Frames
$0 copay; $100 allowance, plus 20% discount on balance
N/A
Benefits specific to Davis Vision, $150 allowance at Visionworks,
or Davis Vision “Exclusive Collection” covered in full
Standard Plastic Lenses
Single Vision $0 copay N/A
Bifocal $0 copay N/A
Trifocal $0 copay N/A
Lenticular $0 copay N/A
Contact Lens Fit & Follow-up (contact lens fit and follow-up visits are available once a comprehensive eye exam has been completed)
Standard Contact Lens Fit & Follow-up $0 copay, covered in full N/A
Specialty Contact Lens Fit & Follow-up $0 copay, up to $50 allowance plus 15% discount on any overage N/A
Frequency
Examination Once every 12 months
Lenses or Contact Lenses Once every 12 months
Frames Once every 24 months
Contact Lens Fit (contact lens allowance includes materials only)
Conventional and Disposable $0 copay, $100 allowance, 15% of balance over $100 N/A
Medically Necessary $0 copay, covered in full (prior approval required) N/A
Laser Vision Correction
Laser Vision Coverage 40-50% off the national average price of tradional LASIK N/A
Lens Options (paid by the member in addition to the price of the lenses)
Standard Progressive Lenses $0 N/A
Premium Progressive Lenses $40 N/A
Ultra-Progressive Lenses $90 N/A
High-Index Lenses $60 N/A
Plastic Photosensitive Lenses (Transitions) $70 N/A
Scratch Protection Plan:
Single Vision/Multifocal Lenses
$20/$40 N/A
UV Treatment $12 N/A
Tint (Solid and Gradient) $0 N/A
Standard Polycarbonate–Adults $35 N/A
Standard Polycarbonate–Kids Under 19 $0 N/A
Standard Anti-Reflective Coating $40 N/A
Premium Anti-Reflective Coating $55 N/A
Ultra-Anti-Reflective Coating $69 N/A
Polarized $75 N/A
Other Add-Ons and Services
$20 discount (where applicable) balance from insured frame
purchase: 30% discount on additional pairs of eyeglasses
N/A
VISION PLAN SUMMARY

19
FLEXIBLE SPENDING ACCOUNTS (FSAs)
Health Care and Dependent Day Care Flexible Spending Accounts are administered
by Optum Financial.
You can save money when you use pre-tax dollars from a Health Care Flexible Spending Account
(HCFSA) or Dependent Day Care Flexible Spending Account (DCAP) to pay eligible health care
expenses and dependent day care expenses. Your decision to participate in these voluntary
accounts should be based on your needs and personal situation.
What is a Flexible Spending Account?
A Flexible Spending Account (FSA) is a tax-advantaged account that allows you to use pre-tax
dollars to pay for qualied medical or dependent day care expenses.
When you contribute to an FSA:
• You decide how much to contribute. You elect an annual contribution in which deductions
are taken in equal amounts for the number of remaining pay periods in the plan year
• These contributions can be used for eligible expenses incurred in the calendar year
(January 1 through December 31), as well as eligible expenses incurred January 1 through
March 15 of the following calendar year. Although the plan year ends December 31, there
is a grace period until March 15 to incur claims with any unused funds, and you must
submit outstanding claims for reimbursement by March 31
• You save on taxes since your contributions are deducted from your pay before federal
income tax, state income tax, and Social Security taxes are calculated. You are not taxed on
the money you use from your account for eligible expenses
• You cannot change your elections after your enrollment period unless you experience a QLE
• Any money not used will be forfeited. Therefore, it is important to estimate your
contribution amounts wisely
• You must enroll during the annual Open Enrollment period for FSA participation for
the next year. If you do not enroll, you will not have an account
HEALTH CARE FSA
The Health Care FSA allows an annual contribution of $250 to $2,850 in pre-tax money to pay
for eligible out-of-pocket health care expenses, including physician oce copays, health plan
deductibles, prescription drugs, and dental and vision expenses. You also can use funds for your
spouse or federal tax dependents. For a complete list of eligible expenses, visit:
www.optumnancial.com
USING YOUR FSA FUNDS
Debit Card
Optum Financial will provide you with a debit card you can use to pay for eligible expenses
when you incur them.
SAVE YOUR
RECEIPTS!
Supporting
documentation of
the expenses and
payment may be
required for your debit
card transactions:
• Explanation
of Benets
• Itemized receipt
from your provider
Credit card statements
and cancelled
checks do not meet
the requirements
for acceptable
documentation.
By federal law, any
funds remaining
in these accounts
at the end of the
grace period cannot
be rolled over or
refunded.
20
FSA Claim Deadlines
You have until March 15, 2023 to use your remaining FSA balance for plan
year 2022. Any balance remaining after March 15, 2023 will be forfeited.
All claims for 2022 must be submitted by March 31, 2023.
DEPENDENT DAY CARE FSA
The Dependent Day Care Flexible Spending Account allows an annual contribu-
tion of $250 to $5,000 and lets you save pre-tax money for reimbursement of eli-
gible dependent day care or elder care expenses. Note: the Dependent Day Care
FSA is not for the payment of your dependents’ eligible health care expenses.
This is an account for eligible expenses including childcare or certain elder care
expenses if you have children under age 13 who attend a licensed day care center,
before or after school care, or summer day camp; or if you provide care for a
dependent who is mentally or physically incapable of caring for himself or herself.
These plans are governed by IRS regulation. If you are unclear on the eligibility of
an expense, visit the eligible expense list at www.optumnancial.com.
Unlike the Health Care FSA, you may only receive reimbursements for services
already incurred, and only up to the available funds in your account. An expense
is incurred when a service is received—not when a bill is paid. Even though your
service provider may require payment at the beginning of the service period,
you cannot request reimbursement until after the service is provided.
To reimburse yourself from your Dependent Day Care FSA, you must pay for the care
and then submit the appropriate supporting documentation and Reimbursement
Claim Form. All reimbursement requests must include a completed and signed
Provider Certication form.
If you do not have a Provider Certication form, submit an itemized statement
from the provider that includes:
• Start and end dates of service
• Dependent’s name and date of birth
• Itemization of charges
• Provider’s name, address and tax ID or Social Security number
The form can be located at:
www.optumnancial.com
Submit a Claim
You can also submit a claim using a smart phone or online. You can choose to
have eligible reimbursements either deposited directly into your bank account or
a check mailed to your home address.
These plans are governed by IRS regulation. If you are questioning the eligibility
of an expense, visit the eligible expense list at www.optumnancial.com.

21
COMMUTER BENEFIT
Regardless of how you get to work, the Commuter Benets Program lets you pay for your
eligible transit expenses and, now eligible on a pilot basis, work-related parking expenses
through automatic, pre-tax payroll deductions. Ordering is handled directly through Optum
Financial either online or over the phone. You can request that funds be deposited into your
Ventra account or onto an EdenRed Commuter card, or that a monthly transit pass to be mailed
to your home.
You can enroll, change your product or funding amount, or cancel at any time. Orders must be
submitted by the 10th of the month for the following month. Just visit www.optumnancial.com
or call 1-844-284-6267. Representatives are available 24 hours per day, seven days per week.
1-844-284-6267
www.optumnancial.com

22
PROTECT YOUR FUTURE INCOME FOR YOU AND YOUR LOVED ONES
The County provides basic term life insurance at no cost to you. You have an opportunity
to buy more coverage through the County’s group insurance policy. You may contact the
insurance providers at any time to learn more.
Group Term Basic Life Insurance: Totally County paid, this coverage is equal to one times
salary rounded to the next highest thousand for a full-time employee. This plan provides a
benet in the event of death of an employee. Coverage can be converted or ported to an
individual policy upon separation from employment. The maximum benet is $750,000.
Supplemental Group Term Life Insurance: You may purchase additional group term
coverage equal to one, two or three times salary, upon employment. During Open
Enrollment periods, current participants can increase their coverage within plan, and new
enrollments require Evidence of Insurability. Enrollment at other times or increases in
amounts require Evidence of Insurability. Payment is made through convenient payroll
deduction at reasonable group rates based on age. Coverage can be converted or ported to
an individual policy upon separation from employment.
Please note: Proof of good health may be required if you are increasing the amount of
insurance to 4X-5X your annual earnings, up to $500,000.
23
VOLUNTARY BENEFITS
Cook County oers voluntary benets options through Mercer, administered by Benet Harbor.
These plans are a benecial tool to help protect your nancial security. Employees are encouraged
to review all plans available prior to making benets selections, considering your family’s needs.
Payment for these voluntary benets is conveniently available through payroll deduction.
The following plans are available:
Group Accident Insurance
• Accident Insurance pays a lump sum benet directly to you
(unless otherwise assigned) for injuries caused by a covered
accident
Group Critical Illness Insurance
• Critical Illness Insurance pays a lump sum benet upon
diagnosis of a covered critical illness, such as a heart attack,
stroke, or internal cancer
Group Hospital Indemnity Insurance
• If you have a covered illness or injury, which results in
hospitalization, Hospital Indemnity Insurance pays out a lump
sum regardless of the cost of care
Short-Term Disability Insurance
• An injury or sickness may slow you down, but it won’t slow
down your monthly bills. Short-Term Disability Insurance
provides a monthly benet if you are disabled from an o-the-
job injury and cannot work
Universal Life Insurance
• A death not only leaves behind loved ones but also potentially
overwhelming nancial obligations. Universal Life Insurance
provides your beneciary a lump-sum cash benet in the
event of your death
Identity Theft Protection
• IDShield provides identity theft protection and identity
restoration services for you and your family
Legal Service Plan
• LegalShield provides you with direct access to a dedicated law
rm who will answer your personal legal questions and help
resolve life’s legal matters
Employees should carefully consider which of the optional products the County oers meet their
needs for life insurance, disability insurance, medical and dental care, and supplemental insurance.
Detailed information about these products is available online at
www.cookcountyvoluntarybenets.com or by calling 1-800-698-2849. The Department
of Risk Management does not provide advice regarding these insurance products.

24
DEFERRED COMPENSATION RETIREMENT PLAN
The 457 Deferred Compensation Plan program is a supplemental retirement plan that can help
boost your retirement income. Added benets to contributing to the deferred compensation plan
include tax-deferred contributions—possible tax-free earnings/gains.** Starting small can have
a great impact on your retirement savings in the long run. Contact your designated Retirement
Specialist today to get started!
Minimum payroll deduction to
start account
$25 per pay period
Contribution limits if you are
under the age of 50
$20,500 for 2023*
Contribution limits if you are
over age 50
Over age 50 catch-up: $6,500 in addition to
the $20,500*
Pre-retirement catch-up provision available
Please contact your local Retirement Specialist
for more information.
Age at which you must begin
taking distributions
70½ is the Required Minimum Distribution age in which
distributions are required in-service or once termed.
Please contact Nationwide for further information.
Penalty for early withdrawals Distributions before 70½ are not permitted.
Taxation All distributions are subject to federal and state
income tax. Please consult your tax preparer for
additional information.
Who can participate? All full-time and part-time Cook County Government
and Forest Preserve District employees.
www.cookcountydc.com
1-855-457-2665
*Contribution limits are subject to change annually due to IRS regulations.
**Please speak to your Retirement Specialists regarding these provisions.

25
EMPLOYEE ASSISTANCE PROGRAM
The Cook County Employee Assistance Program (EAP) is available to help you with balancing the
demands of family, work and personal needs. The EAP is administered by Magellan Health and is
staed by licensed professionals available to help you at no cost, 24 hours/7 days a week.
The EAP program is here to help you and your household members along the journey of life–no
situation is too big or too small. Services include telephonic goal-oriented coaching, counseling,
online programs and digital self-care tools.
Counseling is available for the entire family–individuals, couples and teens (with parental consent
and in accordance with applicable law and clinical appropriateness).
Virtual therapy is available in four modalities: text message exchange over a week, live phone,
live video or live chat. There are ve EAP visits available at no cost–per individual, per issue. If
additional services are needed, the appropriate health benets plan applies.
All services are condential and can be accessed over the phone at 1-800-327-5048 or online
at www.MagellanAscend.com.
WELL-BEING
Wellness Wednesday Email Communications: Based on the ve core elements of well-being:
1) having a sense of purpose, 2) physical health, 3) nancial health, 4) community engagement,
and 5) maintaining social connections, weekly emails help you explore real-world strategies
designed to help you manage your physical, nancial, and mental health.
Employee Benets Quarterly Newsletter: Keeps you up to date on important information about
your benets and upcoming events. Published in the spring, summer, fall and winter.
Blue Cross Blue Shield of Illinois – Well onTarget: Designed to give you the support you need to
make healthy choices. With Well onTarget, you have access to a convenient, secure website with
personalized tools and resources such as digital self-management programs, health and wellness
content, and tools and trackers.
MyHealth Connection Facebook Community: Focuses on providing preventive care tips and
information. Prevention can reduce risk factors that lead to chronic disease or slow the progression of
a disease. It’s a way to help Cook County employees enjoy longer, healthier and more productive lives.
Health Fair: The annual Employee Health Fair includes a combination of on-site and virtual
programs. Flu shots are provided annually at Open Enrollment on-site events and at CVS Health
locations for employees and for enrolled dependents through the health plan.

26
HEALTH AND BENEFITS LITERACY
DEFINITIONS
The language of health insurance can be hard to understand. Yet it is important
to have a basic knowledge of the industry’s terminology. Here are some of the
most common nancial insurance terms to help you make sense of it all–so
you can make smart decisions that will benet you and your family.
Balance Bill – The dierence between the amount charged by an out-of-
network provider for a covered health service and the amount your health
plan (insurance) pays.
Coinsurance – A percentage of the cost of covered health services you pay.
This often starts after the deductible is satised.
Copayment – A xed dollar amount you pay for covered health services
such as a physician visit.
Deductible – A xed, annual amount you pay for covered health services
before the health plan (insurance) starts to pay. For certain services, such
as in-network preventive care, you are not required to rst satisfy
the deductible.
Dual Coverage – The same person is enrolled under more than one of Cook
County’s employee benets. Dual coverage is prohibited for employees and
dependents on all County plans.
In-Network – A group of doctors, hospitals, pharmacies, and other providers
who contract with the health plan and provide services at negotiated rates.
Out-of-Network – A group of doctors, hospitals, pharmacies, and other
providers who do not contract with the health plans and do not provide
services at negotiated rates. You pay more out of pocket and have fewer
protections. Out-of-network providers may balance bill you for these costs.
Out-of-Pocket Maximum – The maximum annual out-of-pocket amount you
pay before the health plan (insurance) pays 100% of covered health services.
For out-of-network services, providers may balance bill even after the out-of-
network, out-of-pocket maximum is reached.
Premium – The amount you pay for health insurance.
Pre-Tax Contributions – Pre-tax contributions include the premium costs
for the medical coverage you elect, as well as any contributions you
choose to make to a Health Care Flexible Spending Account (HCFSA),
Dependent Care Flexible Spending Account (DCAP), Commuter Benet, and
Deferred Compensation Plan up to Federal tax limits. Pre-tax contributions
are deducted from your pay before federal and state income taxes and
Medicare taxes are calculated, reducing your taxable income (and the
current taxes you pay).
USE IN-NETWORK
PROVIDERS TO
SAVE MONEY
While it may be a
personal preference
to use out-of-network
providers, there are
some protections you
lose by doing so.
1. The health plans do
not contract with
out-of-network
providers, which
means they don’t
check into providers’
history such as their
medical license,
education, training,
work history,
malpractice claims,
board certication,
health outcomes, etc.
2. Out-of-network
providers may
balance bill you,
which means
billing you for the
dierence between
the amount they
charge you for a
covered service and
the amount your
insurance pays.
3. Overall, you pay
more out of pocket
for out-of-network
services.
27
REMINDERS
Consequences of Fraudulent Enrollment
Any kind of fraud on the County’s benet plans may result in adverse consequences
to an employee and dependent, for example:
• Failure to notify the Department of Risk Management of an event that would
cause coverage to end, e.g., divorce
• Misrepresentation by the employee or dependent regarding the initial
eligibility, for example, the dependent’s age, or that the dependent is not a legal
dependent of the employee
• Any attempt to assign or transfer coverage to someone else (e.g., letting
another person use your Plan ID card)
The employee may be required to pay for any claims and all administrative costs
that were incurred fraudulently. This may result in coverage being terminated for
the employee and action by the County to collect any money paid. The County may
also discipline the employee, up to and including termination.
NOTICES
Important notices regarding Cook County Employment Benets may be found at:
www.cookcountyil.gov/service/compliance
These notices include:
• Health Insurance Marketplace Coverage
• Cook County’s Group Health Plan Notice of Privacy Practices
• COBRA Election Notices
• Women’s Health and Cancer Rights Act of 1998
• 1095 Tax Reform Request
• Notice to Enrollees of Mental Health Parity and Addiction Equity Act
Exemption for 2021
REMINDERS & NOTICES
IMPORTANT BENEFITS CONTACT INFORMATION
MEDICAL PLANS
Blue Cross Blue Shield
of Illinois
www.bcbsil.com/cookcounty
BlueAdvantage HMO
Group #B03351
1-800-892-2803
Blue Cross Blue Shield PPO
Group #291116
1-800-960-8809
PHARMACY BENEFIT PLAN
CVS Pharmacy
www.caremark.com
1-866-409-8522
GROUP TERM LIFE AND SUPPLEMENTAL
LIFE INSURANCE
MetLife
www.metlife.com/mybenets
Group/Customer #227860
1-866-492-6983
DENTAL PLANS
Guardian
www.guardiananytime.com/cookcounty
Group #397485
Dental HMO: 1-866-494-4542
Dental PPO: 1-866-302-4542
VISION PLAN
Davis Vision
www.davisvision.com/member
1-800-381-6420
FLEXIBLE SPENDING ACCOUNTS AND
COMMUTER BENEFITS
Optum Financial
www.optumnancial.com
1-844-284-6267
COOK COUNTY
VOLUNTARY BENEFITS
Mercer
www.CookCountyVoluntaryBenets.com
1-800-698-2849
DEFERRED COMPENSATION
Nationwide
www.cookcountydc.com
1-855-457-2665
EMPLOYEE ASSISTANCE
PROGRAM
Magellan
www.MagellanAscend.com
1-800-327-5048
JOIN THE FACEBOOK GROUP MYHEALTH CONNECTIONS
MyHealthConnections
www.facebook.com/groups/Myhealthconnections
Cook County Department of Risk Management
Employee Benets Division
118 N. Clark Street, Suite 1072 • Chicago, IL 60602
Phone: (312) 603-6385 • Fax (866) 729-3040
www.cookcountyrisk.com • Email: risk.mgmt@cookcountyil.gov
