
1
Facilitators Guide for Training
on Kangaroo Mother Care

This facilitator’s guide was prepared by Tedbabe D. Hailegebriel UNICEF HQ.
Christabel Nyange as part of consultancy with UNICEF HQ (New York) with
support from the Bill and Melinda Gates Foundation developed the lesson plan.
Dr. Julieta Villenga Rosales reviewed and provided input. Overall guidance and
direction provided by Nabila Zaka (UNICEF HQ), Kimberly Harding (Nutrition
International) and Stella Abwao for reviewing/providing comments and project
support by Seun Oyedele (UNICEF HQ).
This publication has used training materials, technical presentations, inpatient
record forms, and monitoring tools from the American Academy of Pediatrics
and South African Medical Research Council Unit for Maternal and Infant
Health Care Strategies at the University of Pretoria, University of Pretoria,
WHO and Save the Children. The Do No Harm Technical Series was prepared
by a team led by Jim Litch and Judith Robb-McCord (Every Preemie–SCALE)
and Lily Kak (USAID).
Find all presentations and key documents here.
ACKNOWLEDGEMENTS
Cover Photo: © UNICEF/UN0135391/Selaam

1
Background: . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2
Planning and Organizing . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4
Facilitators’ Preparation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8
Your Role as Facilitator . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9
Training plan by each day (agenda) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10
Introduction to key resources . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12
Lesson Plan . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18
Knowledge Check (Pre-and post-test) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 26
Answer to Knowledge Check (Pre and post-test) . . . . . . . . . . . . . . . . . . . . . . 33
Skill Assesment Tool . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 34
Discussion guides for group works/templates . . . . . . . . . . . . . . . . . . . . . . . . . 36
Template for SWOT ANALYSIS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 36
Template for Follow-up monitoring and national scale-up plan . . . . . . . . . . . 37
Template for Prioritising Actions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 37
Tips for facilitators for Crinkle-Free Workshop . . . . . . . . . . . . . . . . . . . . . . . . . 38
Administrative note . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 38
Introduction to workshop participants . . . . . . . . . . . . . . . . . . . . . . . . . . . . 38
Team building at the beginning and introductions . . . . . . . . . . . . . . . . . . . 38
Ice breakers . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 38
Facilitator meetings: . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 40
Sample Budget for the KMC training . . . . . . . . . . . . . . . . . . . . . . . . . . . . 40
Workshop Evaluation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 41
CONTENTS

2
The global neonatal mortality rate fell from 37 (36, 38) deaths per 1,000 live births in
1990 to 19 (18, 20) in 2016, and 2.6 (2.5, 2.8) million children died in the first month of
life in 2016 – approximately 7,000 newborn deaths every day – most of which occurred
in the first week, with about 1 million dying on the first day and close to 1 million dying
within the next six days
1
. Complication related to preterm births is the leading cause
of death among children under five. Three-quarters of all neonatal deaths occur during
the first week of life, 25–45% in the first 24 hours
2,3
globally, nearly 1 million babies die
each year from complications of premature birth and preterm birth is one of the leading
causes of newborn morbidity and mortality globally.
Low coverage of proven interventions and large disparities in coverage across population,
particularly in the postnatal and childhood periods, result in millions of preventable deaths
of newborns. Despite strong evidence regarding the improved health outcomes among
preterm or low birth weight infants receiving KMC, including a recent recommendation
by the World Health Organization that KMC should be routine care for newborns
weighing less than 2000 g
4
, only modest KMC coverage has been achieved globally.
Millions of LBW babies still do not have access to KMC and other essential neonatal care
interventions, such as those to prevent and cure infections and ensure adequate nutrition.
A previous systematic review identified barriers to health system adoption of KMC and
noted that families play an important role in KMC adoption
5
. Further, the review noted
that family interactions with the health system were critical to KMC adoption. Caregivers
(e.g. mothers, fathers, and families) are key implementers and beneficiaries of KMC.
Health system and social barriers for KMC implementation includes lack of awareness
on the benefits of KMC, expectation that KMC could be done with no or little instruction,
lack of social support, caregivers’ medical concern including the clinical conditions of the
mother and the baby, lack of space for privacy and KMC resources and lack of money
for transportation
6
. Studies have shown that strategies that can improve the presence
of staff, supplies, and space for KMC is a prerequisite for quality implementation of
KMC as well as the qualityof key components of KMC—skin–to–skin care, exclusive
breastfeeding and discharge and outpatient follow-up care—is also needed to achieve
meaningful process evaluation and scale–up of this life–saving intervention
7
.
1 UNICEF UN Inter-agency Group for Child Mortality Estimation. Levels and Trends in Child Mortality.
New York: UNICEF, 2017 report
2 Lawn JE, Cousens S, Zupan J. 4 million neonatal deaths: when? Where? Why? Lancet, 2005, 365:891–900.
3 Born Too Soon: The Global Action Report on Preterm Birth. World Health Organization. Geneva: World Health.
Organization Geneva, 2012. Available: www.who.int/pmnch/media/news/2012/preterm_birth_report/en/.
4 WHO. WHO recommendations on interventions to improve preterm birth outcomes. In. Geneva:
World Health Organization. (2015).
5 Chan GJ, Labar AS, Wall S, Atun R. Kangaroo mother care: a systematic review of barriers and enablers.
Bull World Health Organ. 2016; 94(2):130–41J.
6 Emily R. Smith, Ilana Bergelson, Stacie Constantian, Bina Valsangkar and Grace J. Chan. Barriers and enablers of health
system adoption of kangaroo mother care: a systematic review of caregiver perspectives. BMC Pediatrics 2017 17:35
DOI: 10.1186/s12887-016-0769-5
7 Kondwani Chavula , Dyson Likomwa, Bina Valsangkar, Richard Luhanga, Lydia Chimtembo, Queen Dube, Wasihun
Andualem Gobezie, Tanya Guenther. Readiness of hospitals to provide Kangaroo Mother Care (KMC) and documentation
of KMC service delivery: Analysis of Malawi 2014 Emergency Obstetric and Newborn Care (EmONC) survey data.
www.jogh.org • doi: 10.7189/jogh.07.020802
BACKGROUND

3
This Facilitator’s Manual originally designed for a five-day training course on Kangaroo
Mother Care (KMC) clinical skills and program planning, monitoring and evaluation,
maternal, perinatal death audits and surveillance (MPDSR) and Infection Prevention
and Control(IPC). It was pretested in four trainings in Beirut for MENA region, in Nepal
and Pakistan for ROSA and South Africa for ESARO and WCAR. Participants in these
trainings pointed out that time was not sufficient to adequately cover the MPDSR and
IPC components and the need to include health workers who are responsible for these
activities who may not be represented by participants selected for the KMC training.
The current revision includes three and half day training on KMC while two modules on
IPC and MPDSR are developed and will soon be pretested. By applying the knowledge
and skills acquired at the workshop; participants are expected to change their facilities’
ability to address newborn health issues specifically the provision of quality care for
management of LBW/preterm infants and ensure better outcomes.
How should this document be used?
The workshop intends to equip participants with knowledge and skill to manage Low
Birth Weight/preterm baby and provide essential newborn care, train health workers, plan
and implement KMC at scale, monitor and analyze data related to ENC, LBW/preterm
and KMC, and follow-up at home while caring for the LBW/preterm infants. This capacity
building workshop is designed to support the roll-out of the 2015 WHO recommendations
on Interventions to Improve Preterm Birth Outcomes. If you have comments or
suggestion for improving this document contact Dr. Tedbabe at thailegebriel@unicef.org
What is to be taught and how?
• There is a need to have a training schedule or agenda
• The agenda should contain date, time, and sessions/topics to be covered
and responsible persons, tea/coffee and lunch breaks
• The agenda should also include the objectives of the training program,
introduction of participants and of the training program, and methods of evaluation
Who is responsible for what?
• A training program needs a course coordinator, five facilitators with relevant
skills and experience, administrative and support staff
• Facilitators should divide tasks among themselves before hand and be well
prepared on the tasks they are going perform
• The course coordinator organizes the training program and coordinates activities
• Facilitators provide information, organize learning tasks, demonstrate and
supervise skill practice, evaluate the progress of participants and provide feedback
• Administrative and support staff provide administrative, secretarial, logistics
and other services for the training
Powerpoint slides for lectures.
The facilitators can use all the slides or select based on the need and capacity
of the participants. There are video demonstrations of key clinical skills. Show
each video demonstrations of skills in plenary, let facilitators demonstrate on
each table followed by practice among pair of participants.
D

4
A successful training needs good planning and preparation ahead of time.
The concept note for the training should include these three points
1) Background information that highlights why topic is important to prospective
audience; 2) What the attendee can expect to happen? How will the learning
objectives be achieved? and 3) What the attendee can expect to take away?
-knowledge and/or skills as well as tangibles (resource material, handouts).
It is important to stress the interactive portions of the workshop. In planning
a training course, the facilitator needs to answer the following questions:
Aim
This facilitators guide was developed as a reference to guide health workers
responsible for the training of health care providers at primary and district level
health facilities. The aim is to standardize the knowledge of health professionals
in the management of preterm and/or low birth weight infants through essential
newborn care, to train health professionals in the implementation of two
components of KMC; kangaroo position and nutrition and feeding strategies
for preterm and low birth infants, and to sensitize health care providers on the
importance of early discharge with outpatient follow-up and the relevance and
impact of prematurity and low birth weight on newborn mortality.
Who is the intended audience?
The organization that is planning the
training need to identify the skills level
of the learner/participant, and since
health workers have different training
backgrounds and functions, it is best
to establish aims and tailor the training
accordingly. This workshop is intended
for doctors, nurses and midwives who
provide care for preterm and low birth
weight infants and who are responsible
for planning and managing newborn
health programs in health facilities and
the Ministry of Health. Trainees should
possess basic competences in maternal
and newborn care. Their knowledge and
basic experience in caring for preterm
and low birth weight infants can be
strengthened under the concepts of
Kangaroo Mother Care, as expressed
through its three components: kangaroo
position, kangaroo nutrition and early
discharge with outpatient follow-up.
PLANNING AND ORGANIZING
What skills will be acquired?
• Providing essential newborn care for
preterm and low birth weight babies
• Routinely assessing the baby and mother
• To counsel and support mother initiate
breast feeding
• To identify, prevent and mange
hypothermia
• To use interpersonal communication to
counsel and support mother to put baby
in KMC position in the facility and at
home after discharge
• To teach mothers to express breast
milk, to cup, syringe or dropper feed
the baby, to feed baby through naso
gastric tube
• To teach and support mothers in home
care for the baby and to recognize
danger signs and ask her to promptly
seek care when concerned
• To provide follow-up care
• To mobilize institutional support, plan,
implement and monitor KMC program
5
How many participants will be in the training course?
The training requires extensive practical skills and should accommodate a
number that is easy to manage. The number should not exceed 25 to 30
participants per class.
What is to be taught and how?
• There is a need to have a training schedule or agenda
• The agenda should contain date, time, and sessions/topics to be covered
and responsible persons, tea/coffee and lunch breaks
• The agenda should also include the objectives of the training
program, introduction of participants and of the training program,
and methods of evaluation
• A training program needs a course coordinator, five facilitators with
relevant skills and experience, administrative and support staff with
following clear delineation of responsibilities:
• Facilitators should divide tasks among themselves before hand
and be well prepared on the tasks to be performed
• The course coordinator organizes the training program
and coordinates activities
• Facilitators provide information, organize learning tasks, supervise skill
practice, evaluate the progress of participants and provide feedback
• Administrative and support staff provide administrative, secretarial, logistics
and other services for the training
How many facilitators are needed and what
qualifications should they have?
• The number of facilitators should be determined based on the number of
staff and trained facilitators available. It is good to have up to 5 facilitators
conducting a training program. Ensuring that facilitators have relevant
skills and experience is key, maximum facilitator to trainee ratio
should be 1:6
• Facilitators should know the content of the training modules and be
skilled in the aspects they teach
• Facilitators should be well versed in pedagogical techniques and
imparting skills as stipulated in the training guides
• Facilitators should be KMC experts. A KMC expert is a health
professional with practical (i.e. has worked in a certified Kangaroo
Mother Care Program) and theoretical expertise in all three components
of Kangaroo Mother Care, and is able to train and show others how to
properly apply the Kangaroo Mother Care Method and has the capacity
to evaluate the functioning of a Kangaroo Mother Care Program.

6
What facilities/preparations are needed?
Administrative Notes for the training event.
Administrative note should include essential information on dates, visa,
venue, security, etc is sent at least 4-6 week ahead of the workshop date.
Similarly, the lead facilitator need to inform participants about necessary
preparations, documents or data they need to bringso participants come
prepared. It is crucial to follow-up and compile list of participants with
their responsibility, past training experience on the topic and current role in
newborn care.
Venue
When selecting a venue consider a place that allows the intended number
of patcipants to attend and is suitable for the educational objectives.
A large room with chairs and tables) is required in which all participants
can sit comfortably. The room also needs to have provisions for video
demonstration in plenary.
Participants will be organized in
groups of 6 per facilitator. Each
group will need to refer to an
Action Plan and a Facilitator Flip
Chart. Each participant will need
a Provider Guide and recording
sheets for the Knowledge Check
(multiple choice questions)
and Objective Structured
Clinical Evaluations (OSCE A
and B). Each pair or group of
3 participants will work with a
small baby simulator, manikin or
doll and additional equipment.
A premature newborn simulator is available for insertion of a nasogastric
tube, and a breast model can be used for training manual expression of milk.
Visit to KMC Facilities
A visit to a functioning KMC service should be a mandatory component
of this training. The course coordinator should write an official paper to
the health facility. It is necessary to assign a focal person who selects
and keeps sick children for the participants according to a given schedule.
Encourage participants to observe and learn from the visit, adhere to the
facilities SOP and share their learning which they could use in their facility.
Powerpoint slides for lectures.
The faciltators can use all the slides or selct based on the need and
capacity of the partcipants.
A
B
C
D

7
Essential Equipment and Materials
No Description Quantity
1. Action Plan one for six participants
2. Flip Chart one for six participants
3. Provider Guide one for each participant
4. Parent Guide one for each participant
5. Small baby simulator, manikin or doll in which a
nasogastric tube can be placed
one for two participants
6. Breast model (if available) one for two participants
7. Alcohol-based hand rub or soap and water one for six participants
8. Bag/mask device, small and premature masks (if available) one for two participants
9. Head covering, diaper and socks one for two participants
10. Extra blankets one for two participants
11. Scale (if available) one for six participants
12. Support binder for skin-to-skin care one for each participant
13. Thermometer one for two participants
14. Stethoscope one for two participants
15. Weighing scale, measuring tape and torch one of each per table
16. Water to simulate breast milk one for two participants
17. Cup, or paladai for feeding one for two participants
18.
Measuring container for collecting breast milk one for two participants
19. Clean nasogastric tube (5 or 6 French) one for two participants
20. 20 mL syringe one for two participants
21. Tape to secure nasogastric tube one for two participants
22.
Table to calculate collected breast milk one for two participants
23. Growth chart (optional) one for two participants
24. Mother’s Observation Form (in Provider Guide) one for each participant
25. Newborn Assessment Form (in Provider Guide) one for each participant
26. Newborn Referral Form (in Provider Guide) one for each participant
27. Pen, and paper one for each participant
28. Course Registration Form 1 per room
29. ICD forms
30. Stickit notes (two to three colors) 1 per table
E

8
Facilitators need to review the five sections of each Flip Chart page
1. Explain and demonstrate – Emphasize key points and be practical.
2. Invite discussions – Suggest questions that will provoke discussion
among the providers about the local context of care. These questions will
also help participants identify changes to improve care.
3. Facilitate practice – guidance about how providers should practice skills
required for each action.
4. Background – a summary of details about the action which will help you
answer questions.
5. Educational advice – advice that will assist you in creating the ideal
learning experience. You will need to collect and familiarize yourself with
national and facility guidelines for such practices as eye care, cord care,
and immunizations.
There are four exercises that combine a series of actions to help the learner
integrate the steps of aspect of care. They also focus on how to communicate
with the mother and teach her some of the skills. Familiarize yourself with
exercises and evaluations in the Flip Chart
1. The Knowledge Check can be given as both a pre- and post-course
evaluation if desired.
2. OSCE A and B evaluate knowledge, skills, and decision-making.
3. Review the four sections of each Provider Guide page
4. Review Key Knowledge – a summary of important facts.
Review and prepare for the “Practice Key Skills” section. It is a section to guide
practice during and after the workshop and includes what to monitor - some
key indicators that can be used for data collection as part of efforts to improve
quality of care as well as quality improvement. Conduct demonstration using
videos from the global health media at the indicates session timing in the
lesson plan. (https://globalhealthmedia.org/videos/smallbaby/). The videos on
follow up can be downloaded from www.fundacioncanguro.co after registering
and creating an account. To avoid connection issues; it is recommended to
download the videos ahead of the session.
FACILITATORS’ PREPARATION

9
Explain to participants that, as facilitator your role throughout this course will
be to guide them through the course activities, answer questions as they arise
or find the answer if you do not know, clarify information they find confusing,
give individual feedback on exercises where indicated lead group discussions,
demonstrations on mannequins, video demonstration and role plays, help them
learn skills.
Remember adults learn what they need or want to learn – unlike children who
like to learn almost everything. As facilitator; you should continually relate
course content to the “real world” of the adult learner. Due to the many
pressures adults face whether family, business, or social etc. Adults must feel
that attending and participating in a course gives them information they can
use. Establish relevance for learners by asking them to list their expectations
for the course and paste the expectations on a flipchart. At end of the course,
review the list of the participants’ objectives. Determine if each has been
met by the workshop. Explain how to resolve any issues that have not been
addressed in class.
The adult learner comes to class with a wide variety of experiences, both
personal and professional. The facilitator should respect the learner’s life
experiences and relate the learning topics to those experiences. You can show
respect by asking participants’ opinions, allowing participants to answer, and
offering positive responses when the learner shares experiences. A component
of respect is inclusion. Adults need to feel included as an equal in the group.
You can accomplish this by drawing each learner into discussions, rotating
volunteers and attempting to give each participant equal attention. Consider that
students generally remember:
• 50% of what they hear and see;
• 70% of what they say and
• 90% of what they do and talk about.
Active participation in the learning process ensures that participants gain and
retain the most information from class.
YOUR ROLE AS FACILITATOR

10
This agenda is illustrative for four and half to five days training. When you
organize the training, you can adapt the time based on partcipants experience
and available time. For daily recap session, select and inform one or two
participants in advance. Encourage them to use participatory methods.
Type of Activity Time
Day One
Section 1: Introduction 8:30-9:55am
Ac tivit y 1.1 Registration of participants 10 mins
Activity 1.2 Introduction of participants 15 mins
Activity 1.3 Lay ground rules and announce any administrative arrangements 10 mins
Activity 1.4 Pre-test assessment 30 mins
Activity 1.5 Expectations 20 mins
Activity 1.6 Presentation on workshop rationale, leaning objective and methods 15 mins
Section 2: KMC Clinical Knowledge and Skills 9:55am-1:00pm
Ac tivit y 2 .1 Presentation on essential newborn care 30 mins
TEA BREAK at 9.55am 15 mins
Activity 2.2
Preparing for the birth ofLBW/preterm and essential care
for small babies
40 mins
Activity 2.3 Classify the LBW/preterm 30 mins
Activity 2.4 Presentation on KMC physiologic mechanism of effect 40 mins
LUNCH BREAK at 12.20-3:00 pm 60 mins
Activity 2.5 Maintaining thermal care for the LBW/preterm 90 mins
Day Two 8:30am-5:00pm
Activity 2.6 Recap of day two and administrative announcements 30 mins
Activity 2.7 Feeding the LBW/preterm babies-support breast feeding 80 mins
TEA BREAK at 10:00am 10 mins
Activity 2.8
Support feeding the LBW/preterm-feeding by cup, inserting NGT
and feeding NGT
145 mins
LUNCH BREAK at 1:00pm
60 mins
Activity 2.9
Explain and demonstrate assessing sings of readiness of
breastfeeding when using alternative feeding methods
50 mins
Ac tivit y 2 .10
Routine assessment of LBW/preterm babies for change of
care or referral
60 mins
TRAINING PLAN BY EACH DAY (AGENDA)

11
Type of Activity Time
Day Two 8:30am-5:00pm (cont’d)
TEA BREAK at 3:00pm 10 mins
Ac tivit y 2 .11 Routine assessment of LBW/preterm babies 120 mins
Day Three 8:30am-5:00pm
Ac tivit y 2 .12 Recap of day two and administrative announcements 30 mins
Ac tivit y 2 .13 Prompt referral and stabilization 60 mins
Ac tivit y 2 .14 Planning for successful discharge and home care 20 mins
TEA BREAK at 10:00am 10 mins
Ac tivit y 2 .15 Practice on counseling the mother and other caregivers for home care 60 mins
Ac tivit y 2 .16 Proper hygiene and preventing infection 90 mins
Ac tivit y 2 .17 Conduct OSCE B 60 mins
LUNCH BREAK at 1:00pm 45 mins
Section 3: KMC Implementation Experiences, Challenges and Possible Solutions
Ac tivit y 3.1
Introduction to KMC implementation and scale-up
Learners start to think about what they will include in their action plans
40 mins
Activity 3.2
Quality of care and supportive supervision
Learners work in country or facility teams to document ideas to
include in country/facility action plans
30 mins
TEA BREAK at 3:00pm 10 mins
Activity 3.3 Multidisciplinary care and teamwork in KMC
30 mins
Activity 3.4
Mobilizing support for KMC
(national level, health facilities and community)
40 mins
Day Four 8:30am-5:00pm
Activity 3.6 Recap of day three and administrative announcements 30 mins
Activity 3.7 Documentation for monitoring and evaluation 60 mins
TEA BREAK at 10am 15 mins
Activity 3.8 Action planning for KMC implementation and scale-up 180 mins
Activity 5.5 Orientation to resource materials 30 mins
Activity 5.6 Post-sessions self-assessment and Course Evaluation and closing 60 min

12
This resource package is compiled from different sources and this brief
description is intended to aid the user to smoothly navigate and use as needed
for clinical care as well as to plan and execute trainings.
1. Helping Babies Survive, Essential Care for Every Baby:
Helping Babies Survive (HBS) is an
initiative of the American Academy
of Paediatrics (AAP), developed
in collaboration with WHO, and
supported by the US Agency for
International Development (USAID),
Save the Children, Latter-day Saint
Charities, Laerdal Global Health,
Johnson & Johnson, and a number
of other global health partners. The
Neo-Natalie mannequin in a size
of preterm infant has a “stomach”
that allows skills practice for Naso- Gastric Tube (NGT) insertion, feedings
and NGT removal. The breast Mama Breast Simulator is used for hands on
practice on expressing breast milk. Laerdal is the provider of these materials
and AAP has the copy right. Prior approval is needed for translation and
adaption of the materials in the event you can not have the mannequins;
locally develop dolls/models can be used to practice skills.
2. Early Childhood Devlopment(ECD): includes an article on A
Guide for Monitoring Child Development in Low and Middle-Income
Countries, glossary of terms use in ECD, UNICEF document on
standards for ECD programming. The aim of this document is to guide
practitioners interested in early childhood development through a set of
recommended standards for parenting programmes. The standards cover
a range of good practices that
programmes could offer to
parents and key caregivers.
These standards provide
statements of expectations
of what programmes should
offer to parents and, in doing
so, support them in raising
their children. The poster on
recomndation for care for
child devlopment covers from
for first two years of child’s
live and could be translated
and adapted to local context.
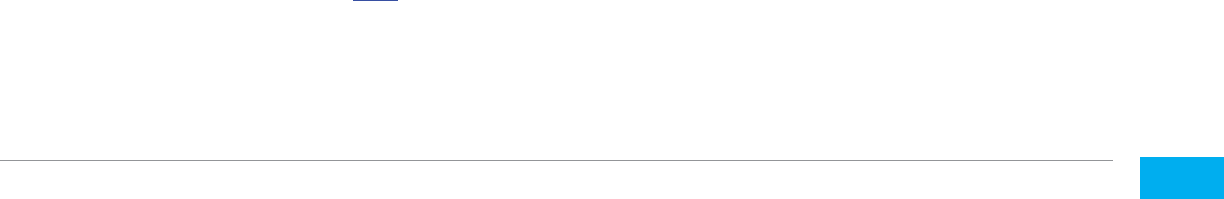
Contents of ECSB Training Materials
• PremieNatalie newborn simulator
• MamaBreast
• Nifty feeding cup
• HBS ECSB Facilitator Set that
includes: 1 action plan wall poster,
flip chart, OSCEs, provider and
parent guide
•
Give your child aection and show your love
•
Be aware of your child’s interests and respond to them
•
Praise your child for trying to learn new skills
Your baby learns
from birth
PLAY Provide ways for
your baby to see, hear, move
arms and legs freely, and
touch you. Gently soothe,
stroke and hold your child.
Skin to skin is good.
COMMUNICATE
Look into baby’s eyes and
talk to your baby. When you
are breastfeeding is a good
time. Even a newborn baby
sees your face and hears
your voice.
PLAY Provide ways for
your child to see, hear, feel,
move freely, and touch
you. Slowly move colourful
things for your child to see
and reach for. Sample toys:
shaker rattle, big ring on a
string.
COMMUNICATE
Smile and laugh with your
child. Talk to your child. Get
a conversation going by
copying your child’s sounds
or gestures.
PLAY Give your child
clean, safe household
things to handle, bang,
and drop. Sample toys:
containers with lids, metal
pot and spoon.
COMMUNICATE
Respond to your child’s
sounds and interests. Call
the child’s name, and see
your child respond.
PLAY Hide a child’s
favourite toy under a cloth
or box. See if the child can
find it. Play peek-a-boo.
COMMUNICATE
Tell your child the names
of things and people.
Show your child how to
say things with hands, like
“bye bye”. Sample toy: doll
with face.
PLAY Give your child
things to stack up, and to put
into containers and take
out. Sample toys: Nesting and
stacking objects, container and
clothes clips.
COMMUNICATE
Ask your child simple
questions. Respond to your
child’s attempts to talk.
Show and talk about nature,
pictures and things.
PLAY Help your child
count, name and compare
things. Make simple toys
for your child. Sample toys:
Objects of dierent colours
and shapes to sort, stick or
chalk board, puzzle.
COMMUNICATE
Encourage your child to
talk and answer your child’s
questions. Teach your
child stories, songs and
games. Talk about pictures
or books. Sample toy: book
with pictures
NEWBORN,
BIRTH UP TO 1 WEEK
1 WEEK UP
TO 6 MONTHS
6 MONTHS
UP TO 9 MONTHS
9 MONTHS
UP TO 12 MONTHS
12 MONTHS
UP TO 2 YEARS
2 YEARS
AND OLDER
Recommendations for
Care for Child Development
INTRODUCTION TO KEY RESOURCES
13
3. Lessons Plan: Executing competency based training session’s entails
a clear plan, expected skill acquisitions, how they are measured and
evaluated. This becomes even more important when the capacity
building activity is expected to be delivered at scale, concurrently by
different trainers than as a small-scale initiative. The competency based
training on care of small babies is run by five facilitators in one session
for 30 participants. Having one lessons plan allows coherent session
flow for facilitators. In addition, the plan guides facilitators in the
preparation required for each session. The lesson plan guide facilitators
in step by step process and indicates the pages in the flip chart for the
specific session. The videos are meant to enhance skill demonstration
and are best delivered in plenary. If the venue does not allow for video
demonstration in plenary session, this could be done in each of the five
small groups. For organising and executing such a training for the first
time; the lesson plan helps organisers in determining the number of
facilitators, supplies and venue required.
4. Technical Presentations: The training is competency based and there
is a minimal number of presentations or theoretical discussions. The
selected few presentations provide important background information
on history of kangaroo mother care, its immediate and long-term
benefit, physiologic mechanism of skin to skin contact, importance of
infection prevention and control and KMC program implementation.
Faciltators are adviced to select the relevant slides for their audience.
a. On history, mechanism of action, immediate and long term benefit
of kangaroo mother care: This presentation provides background
information on the beginning of KMC in Colombia and its start in South
Africa. The presentation has a break point to allow delivering of the
presentation a brief 15-20 minutes’ presentation. Indicative grouping of
the slides is included in the session plan. You as a faciliator can determine
which slides to include and number in each presentation. For example, if
particpants are aware of the information; you can skip this presentation.
The physiologic mechanisms of skin to skin contact in maintaining baby’s
temperature include stimulating breathing, neurophysiologic outcomes
fostering bonding of mother and infant, physiological stress, effects on
stress, nosocomial infections and mortality reduction, brain development
and epigenetics, early intervention and developmental outcomes. This up-
to-date information with current evidence provides learner the knowledge
they need to understand the importance of KMC in the care of preterm
and low birth weight infants. The current evidence on brain development
provides knowledge on the importance of early childhood development
and KMC’s role in the early stimulation, nurturing care and follow-up to
prevent, promptly identify and provide care for disabilities associated with
preterm birth. All presentations and different tools and templates can be
accessed here.

14
b. Implementation, monitoring and evaluation of kangaroo mother
care program There are six sessions on the agenda devoted to the
implementation of a KMC program. Much of the materials that are provided
serve as hints and reminders for facilitators and are not necessarily
presentations that you can repeat as is with workshop participants. All the
handouts serve as examples of activities that can be included in working
sessions for brainstorming and compiling plans of action.
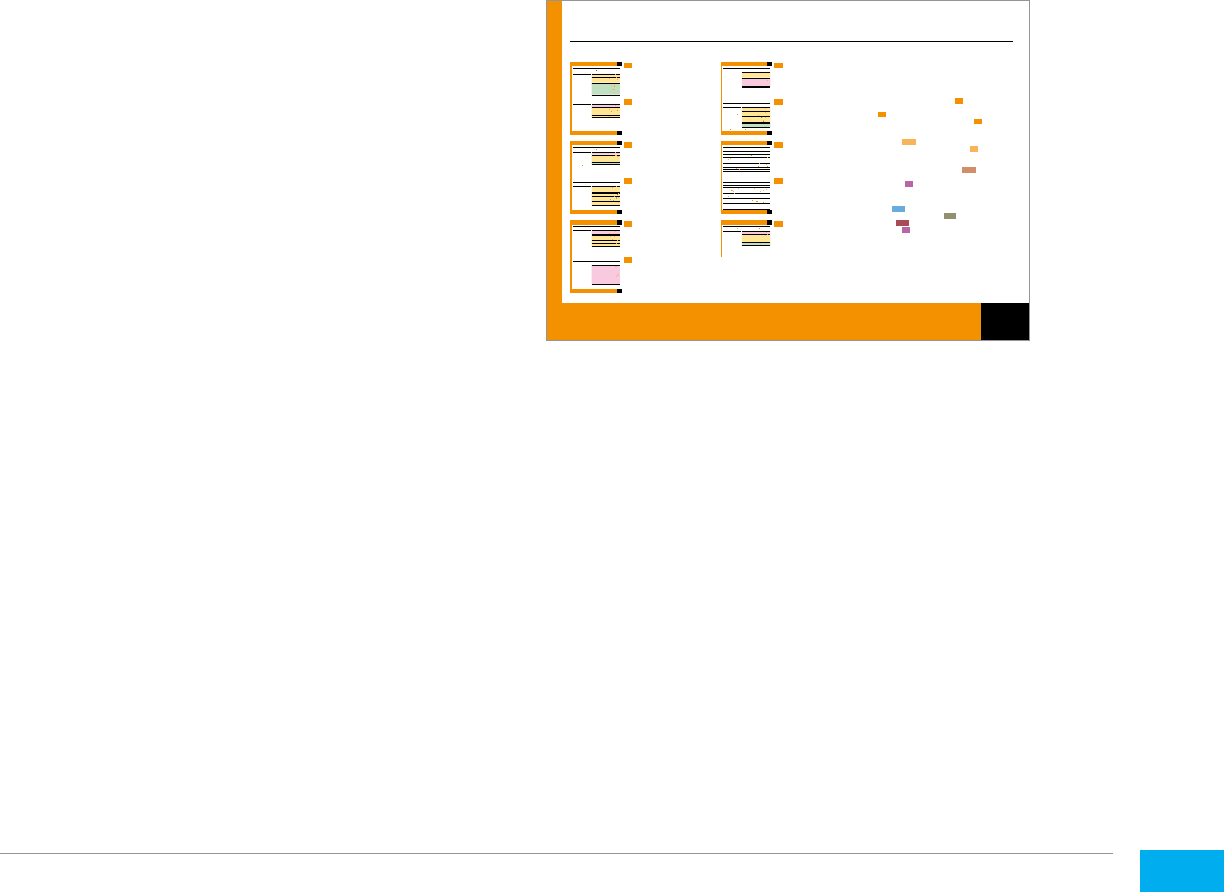
5. Technical Briefs: The technical briefs
by Every Preemie-SCALE highlights
the safe and effective use of specific
inpatient newborn care interventions.
Central to this series of technical
briefs is the guiding principle of “Do
No Harm”. The briefs are designed to
provide stakeholders with evidence-
based information regarding safe and
effective inpatient care in low resource
settings as an important step to avoid
harm and improve health outcomes for
newborns. The series covers:
• Current evidence based
recommendations on safe
and effective use of oxygen,
• Infection prevention,
• Thermal protection and
• Human milk for inpatient newborn care.
They can be translated to local language if needed and can be accessed
www.everypreemie.org/resources/
6. Guidelines: The clinical guidelines are from Kalafong Hospital KMC unit
in South Africa. The guidelines are standard operating procedures of the
KMC unit. To provide guidelines and compliance requirements regarding
admission, transfer and discharge procedures. They are intended to serve
as an example and each health facility may adapt them to the specific
situation and need.
a. Feeding: infant feeding policy of the hospital is clearly defined to be breast
milk. The policy indicated the choice and volume of feeds, caloric requirement
of premature infants, and use of breast milk fortifiers, method of feeding and
management of breast milk bank. The resource also includes a guide to daily
feeding requirements by weight and age, cup feeding procedures and protocol
and method of use of breast milk fortifier.
DO NO HARM TECHNICAL BRIEF
Safe and Effective Oxygen Use for
Inpatient Care of Newborns
How can unsafe oxygen use cause
harm?
Oxygen is fundamental for sustaining life, but it is also toxic.
Unique developmental vulnerabilities of newborns put them at a
greater risk of injury from oxygen use than adults. Injury may occur
from high levels of oxygen in the blood, regardless of the
administered oxygen concentration, and from exposure of the lungs
to high concentrations of oxygen. The two main complications of
oxygen use with newborns are retinopathy of prematurity (ROP) and
lung injury. The historical success of improving survival of
premature infants was tempered by blindness in some survivors
that was caused by low, but unmonitored, oxygen exposure. Even
with low concentrations of administered oxygen, levels in the blood
can rise far above normal. ROP is the abnormal development of
blood vessels in the retina of the eye. In its most severe form, ROP
can result in blindness. Exposure to supplemental oxygen also
produces complications from direct oxygen toxicity to lung tissue.
Chronic lung disease (also known as bronchopulmonary dysplasia)
is a serious consequence in extremely preterm infants, but
cumulative oxygen exposure also leads to lung problems in infancy
among moderately preterm babies.
5
There are multiple ways in which inadequately regulated oxygen
use can cause harm. In the special care of newborns the most
common include:
• 100% oxygen administration
• Unmonitored oxygen saturation during any supplemental oxygen
administration
• “Prophylactic” administration of oxygen to sick or at-risk
newborns without clinical indication
• Environmental enrichment with oxygen (i.e. oxygen in
incubator)
• Use of non-rebreathing mask or funnel to deliver oxygen
• Interrupted oxygen administration (rotating allocation of
available oxygen)
What are current WHO
recommendations for oxygen
therapy?
Current WHO recommendations and clinical guidelines address
several aspects of oxygen therapy (Table 1).
Clinical indications for oxygen use include resuscitation of preterm
infants and advanced resuscitation of term infants as well as the
full spectrum of respiratory illness from mild hypoxemia to
moderate/severe respiratory distress and respiratory failure.
Routine resuscitation of term and moderate-to-late preterm infants
begins with bag-and-mask ventilation using room air. However,
preterm infants < 32 weeks should receive ventilation beginning
with 30% oxygen or air if blended oxygen is not available (rather
than 100% oxygen). Oxygen concentration should be guided by
blood oxygen saturation levels. Titrating the concentration of
oxygen to meet time-specific saturation targets (Table 2). The
adjustment of the concentration of oxygen levels should be by 10%
(FiO2=0.1) per 30 seconds and must be guided by oxygen
saturation levels reached.
6
Oxygen is important in the care of newborn infants because many conditions that affect babies in the first days of life
can result in low levels of oxygen in the body. Hypoxemia, or low level of oxygen in the blood, is a life-threatening
condition that results in increased mortality and morbidity. Prematurity and respiratory distress syndrome (surfactant
deficiency), pneumonia and other severe infections, asphyxia and difficulties in the transition from fetal to neonatal
life can all result in hypoxemia. Supplemental oxygen is an essential lifesaving treatment.
Why is Safe Oxygen Use Important?
Access to appropriate oxygen therapy has been demonstrated to reduce death from childhood pneumonia and neonatal
respiratory distress. Improved detection of hypoxemia and the safe administration of oxygen has resulted in a 35%
reduction in the risk of death from childhood pneumonia in high-burden settings.
1
Historically, the administration and
delivery of oxygen with pressure that helps maintain lung inflation has resulted in a dramatic improvement in survival
of premature infants.
2
Oxygen therapy remains an essential element in the treatment of newborn respiratory distress,
with specialized delivery methods being increasingly used in low and middle-income countries.
3;4
15
b. For doctors: Clinical guideline for doctors include neonatal jaundice
management flow chart, admission and discharge criteria that includes
clinical conditions of both the infant and the mother as well as the social
circumstances of as well. Similarly, the ward protocol describes detailed
roles and responsibilities of doctors, work organization and allocation among
different teams, discharge arrangements and procedures, and routine care and
clinical rounds in the unit.
c. For nurses: includes standard operating procedures of the unit,
clear instruction for weighing the infant and recoding it regularly and
clearly, KMC unit checklist that describes admission producers, routine
investigation and treatment, discharge procedure and documentation.
7. Ward documents: are useful guides in using different equipment and tools
in the care of the premature infants. It includes how to care and correctly
use electronic or mechanical baby scales to maintain their precision,
postnatal daily checklist, admission book, information brochure for mothers
and monthly statistics from. Recommended standards for described
essential care, environmental design, infection prevention, levels of newborn
care in the facility and human resource requirements.
8. Key WHO Guidelines:
Pregnancy, Childbirth,
Postpartum and Newborn
Care: A guide for essential
practice’ (PCPNC) has
been updated to include
recommendations from
recently approved WHO
guidelines relevant to
maternal and perinatal
health. These include pre-
eclampsia & eclampsia;
postpartum haemorrhage;
postnatal care for the mother and baby; newborn resuscitation;
prevention of mother-to- child transmission of HIV; HIV and infant
feeding; malaria in pregnancy, tobacco use and second-hand exposure
in pregnancy, post-partum depression, post-partum family planning and
post abortion care. This revised guide brings a full range of updated
evidence – based norms and standards that enable health care providers
at the first health care level to provide high-quality, integrated care during
pregnancy and childbirth and after birth, both for mothers and babies.
All recommendations are for skilled attendants working at the primary
level of health care, either at the facility or in the community. WHO
recommendations on interventions to improve preterm birth outcomes
NEWBORN CARE
EXAMINE THE NEWBORN
Use this chart to assess the newborn after birth, classify and treat, possibly around an hour; for discharge (not before 24 hours); and during the first week of life at
routine, follow-up, or sick newborn visit. Record the findings on the postnatal record
N6
and home-based record.
Always examine the baby in the presence of the mother.
ASK, CHECK RECORD LOOK, LISTEN, FEEL SIGNS CLASSIFY TREAT AND ADVISE
Check maternal and newborn record
or ask the mother:
How old is the baby?
Preterm (less than 37 weeks
or 1 month or more early)?
Breech birth?
Difficult birth?
Resuscitated at birth?
Has baby had convulsions?
Ask the mother:
Do you have concerns?
How is the baby feeding?
Is the mother very ill or transferred?
Assess breathing (baby must
be calm)
→listen for grunting
→count breaths: are they 30-60
per minute? Repeat the count
if elevated
→look at the chest
for in-drawing.
Look at the movements: are they
normal and symmetrical?
Look at the presenting part —
is there swelling and bruises?
Look at abdomen for pallor.
Look for malformations.
Feel the tone: is it normal?
Feel for warmth. If cold, or
very warm, measure temperature.
Weigh the baby.
Body temperature
35.5ºC-36.4ºC.
MILD
HYPOTHERMIA
Re-warm the baby skin-to-skin
K9
.
If temperature not rising after 2 hours, reassess
the baby.
Mother not able to breastfeed
due to receiving special
treatment.
Mother transferred.
MOTHER NOT ABLE
TO TAKE CARE FOR BABY
Help the mother express breast milk
K5
.
Consider alternative feeding methods until mother is
well
K5-K6
.
Provide care for the baby, ensure warmth
K9
.
Ensure mother can see the baby regularly.
Transfer the baby with the mother if possible.
Ensure care for the baby at home.
Normal temperature:
36.5ºC-37.5ºC.
Normal weight baby
(2500 g or more).
Feeding well — suckling effectively
8 times in 24 hours,
day and night.
No danger signs.
No special treatment needs or
treatment completed.
Small baby, feeding well and
gaining weight adequately.
WELL BABY If first examination:
Breastfeeding counseling
K2-K3
.
Give vitamin K
K12
.
Ensure care for the newborn
J10
.
Examine again for discharge.
If pre-discharge examination:
Immunize if due
K13
.
Advise on baby care
K2
,
K9-K10
.
Advise on routine postnatal contacts at age
3-7days
K14
.
Advise on when to return if danger signs
K14
.
Breastfeeding counselling
K2-K3
.
Record in home-based record.
If further visits, repeat advices.
t
Next: If preterm, birth weight <2500 g or twin
NEWBORN CARE
J2
Examine the newborn
J2
EXAMINE THE NEWBORN
IF PRETERM, BIRTH WEIGHT <2500-G OR TWIN
ASK, CHECK RECORD LOOK, LISTEN, FEEL SIGNS CLASSIFY TREAT AND ADVISE
Baby just born.
Birth weight
→<1500 g
→1500 g to <2500 g.
Preterm
→<32 weeks
→33-36 weeks.
Twin.
If this is repeated visit,
assess weight gain
Birth weight <1500 g.
Very preterm <32 weeks
or >2 months early).
VERY SMALL BABY
Refer baby urgently to hospital
K14
.
Ensure extra warmth during referral.
Birth weight 1500 g-<2500 g.
Preterm baby (32-36 weeks
or 1-2 months early).
Several days old and
weight gain inadequate.
Feeding difficulty.
SMALL BABY
Provide as close to continuous Kangaroo mother
care as possible.
Give special support to breastfeed the small
baby
K4
.
Ensure additional care for a small baby
J11
.
Reassess daily
J11
.
Do not discharge before feeding well, gaining weight
and body temperature stable.
If feeding difficulties persist for 3 days and
otherwise well, refer for breastfeeding counselling.
Twin TWIN
Give special support to the mother to breastfeed
twins
K4
.
Do not discharge until both twins can go home.
t
Next: Assess breastfeeding
NEWBORN CARE
J3
If preterm, birth weight <2500‑g or twin
J3
IF PRETERM,
BIRTH WEIGHT <2500 G OR TWIN
ASSESS BREASTFEEDING
Assess breastfeeding in every baby as part of the examination.
If mother is complaining of nipple or breast pain, also assess the mother’s breasts
J9
.
ASK, CHECK RECORD LOOK, LISTEN, FEEL SIGNS CLASSIFY TREAT AND ADVISE
Ask the mother
How is the breastfeeding going?
Has your baby fed in the
previous hour?
Is there any difficulty?
Is your baby satisfied with the feed?
Have you fed your baby any other
foods or drinks?
How do your breasts feel?
Do you have any concerns?
If baby more than one day old:
How many times has your baby fed
in 24 hours?
Observe a breastfeed.
If the baby has not fed in the
previous hour, ask the mother to put
the baby on her breasts and observe
breastfeeding for about 5 minutes.
Look
Is the baby able to
attach correctly?
Is the baby well-positioned?
Is the baby suckling effectively?
If mother has fed in the last hour,
ask her to tell you when her baby is
willing to feed again.
Not suckling (after 6 hours
of age).
Stopped feeding.
NOT ABLE TO FEED
Refer baby urgently to hospital
K14
.
Not yet breastfed (first hours
of life).
Not well attached.
Not suckling effectively.
Breastfeeding less than 8 times
per 24 hours.
Receiving other foods or drinks.
Several days old and inadequate
weight gain.
FEEDING DIFFICULTY
Support exclusive breastfeeding
K2-K3
.
Help the mother to initiate breastfeeding
K3-K4
.
Teach correct positioning and attachment
K3-K4
.
Advise to feed more frequently, day and night.
Reassure her that she has enough milk.
Advise the mother to stop feeding the baby other
foods or drinks.
Reassess at the next feed or follow-up visit in
2 days.
Suckling effectively.
Breastfeeding 8 times in 24 hours
on demand day and night
FEEDING WELL
Encourage the mother to continue breastfeeding on
demand
K3
.
To assess replacement feeding see
J12
.
t
Next:
Check for special treatment needs
NEWBORN CARE
J4
Assess breastfeeding
J4
ASSESS BREASTFEEDING
CHECK FOR SPECIAL TREATMENT NEEDS
ASK, CHECK RECORD LOOK, LISTEN, FEEL SIGNS CLASSIFY TREAT AND ADVISE
Check record for
special treatment needs
Has the mother had
within 2 days of delivery:
→fever >38ºC?
→infection treated with antibiotics?
Membranes ruptured >18 hours
before delivery?
Mother tested RPR-positive?
Mother tested HIV-infected?
→is or has been on ARV
→has she received
infant feeding counselling?
Is the mother receiving TB treatment
which began <2 months ago?
Baby <1 day old and
membranes ruptured >18 hours
before delivery,
or
Mother being treated with
antibiotics for infection,
or
Mother has fever >38ºC.
RISK OF
BACTERIAL INFECTION
Give baby 2 IM antibiotics for 5 days
K12
.
Assess baby daily
J2-J7
.
Mother tested RPR-positive. RISK OF
CONGENITAL SYPHILIS
Give baby single dose of benzathine penicillin
K12
.
Ensure mother and partner are treated
F6
.
Follow up in 2 weeks.
Mother known to be HIV-infected.
Mother has not been
counselled on infant feeding.
Mother chose breastfeeding.
Mother chose
replacement feeding.
RISK OF HIV TRANSMISSION
Give ARV to the newborn
G12
.
Teach mother to give ARV to her baby
G12
,
K13
.
Counsel on infant feeding options
G7
.
Give special counselling to mother who is breast
feeding
G7
.
Teach the mother safe replacement feeding.
Follow up in 2 weeks
G8
.
Mother started TB treatment
<2 months before delivery.
RISK OF TUBERCULOSIS
Give baby isoniazid propylaxis for 6 months
K13
.
Give BCG vaccination to the baby only when baby’s
treatment completed.
Follow up in 2 weeks.
t
Next: Look for signs of jaundice and local infection
NEWBORN CARE
J5
Check for special treatment needs
J5
CHECK FOR SPECIAL
TREATMENT NEEDS
LOOK FOR SIGNS OF JAUNDICE AND LOCAL INFECTION
ASK, CHECK RECORD LOOK, LISTEN, FEEL SIGNS CLASSIFY TREAT AND ADVISE
What has been applied to
the umbilicus?
Look at the skin, is it yellow?
→if baby is less than 24 hours
old, look at skin on the face
→if baby is 24 hours old or
more, look at palms and soles.
Look at the eyes. Are they swollen
and draining pus?
Look at the skin, especially
around the neck, armpits,
inguinal area:
→Are there skin pustules?
→Is there swelling, hardness or
large bullae?
Look at the umbilicus:
→Is it red?
→Draining pus?
→Does redness extend to
the skin?
Yellow skin on face and
only <24 hours old.
Yellow palms and soles and
≥24 hours old.
SEVERE JAUNDICE
Refer baby urgently to hospital
K14
.
Encourage breastfeeding on the way.
If feeding difficulty, give expressed breast milk by
cup
K6
.
Eyes swollen and draining pus. GONOCOCCAL
EYE INFECTION
Give single dose of appropriate antibiotic for eye
infection
K12
.
Teach mother to treat eyes
K13
.
Follow up in 2 days. If no improvement or worse,
refer urgently to hospital.
Assess and treat mother and her partner for
possible gonorrhea
E8
.
Red umbilicus or skin around it. LOCAL
UMBILICAL INFECTION
Teach mother to treat umbilical infection
K13
.
If no improvement in 2 days, or if worse, refer
urgently to hospital.
Less than 10 pustules. LOCAL SKIN INFECTION
Teach mother to treat skin infection
K13
.
Follow up in 2 days.
If no improvement of pustules in 2 days or more,
refer urgently to hospital.
t
Next: If danger signs
NEWBORN CARE
J6
Look for signs of jaundice and local infection
J6
LOOK FOR SIGNS OF JAUNDICE
AND LOCAL INFECTION
IF DANGER SIGNS
SIGNS CLASSIFY TREAT AND ADVISE
Any of the following signs:
Fast breathing
(more than 60 breaths
per minute).
Slow breathing or gasping
(less than 30 breaths
per minute).
Severe chest in-drawing.
Not feeding well.
Grunting.
Convulsions.
Floppy or stiff.
No spontaneous movement,
floppy or stiff.
Temperature>37.5ºC.
Temperature <35.5ºC or not
rising after rewarming.
Umbilicus draining pus or
umbilical redness and swelling
extending to skin.
More than 10 skin pustules
or bullae, or swelling, redness,
hardness of skin.
Bleeding from stump or cut.
Pallor.
POSSIBLE
SERIOUS ILLNESS
Give first dose of 2 IM antibiotics
K12
.
Refer baby urgently to hospital
K14
.
In addition:
Re-warm and keep warm during referral
K9
.
Treat local umbilical infection before referral
K13
.
Treat skin infection before referral
K13
.
Stop the bleeding.
t
Next: If swelling, bruises or malformation
NEWBORN CARE
J7
If danger signs
J7
IF DANGER SIGNS
IF SWELLING, BRUISES OR MALFORMATION
SIGNS CLASSIFY TREAT AND ADVISE
Bruises, swelling on buttocks.
Swollen head — bump on
one or both sides.
Abnormal position of legs
(after breech presentation).
Asymmetrical arm movement,
arm does not move.
BIRTH INJURY
Explain to parents that it does not hurt the baby,
it will disappear in a week or two and no special
treatment is needed.
DO NOT force legs into a different position.
Gently handle the limb that is not moving,
do not pull.
Club foot
Cleft palate or lip
Odd looking, unusual appearance
Open tissue on head,
abdomen or back
MALFORMATION
Refer for special treatment if available.
Help mother to breastfeed. If not successful,
teach her alternative feeding methods
K5-K6
.
Plan to follow up.
Advise on surgical correction at age of
several months.
Refer for special evaluation.
Cover with sterile tissues soaked with
sterile saline solution before referral.
Refer for special treatment if available.
Other abnormal appearance. SEVERE MALFORMATION
Manage according to national guidelines.
t
Next: Assess the mother’s breasts if complaining of nipple or breast pain
NEWBORN CARE
J8
If swelling, bruises or malformation
J8
IF SWELLING, BRUISES
OR MALFORMATION
ASSESS THE MOTHER’S BREASTS IF COMPLAINING OF NIPPLE OR BREAST PAIN
ASK, CHECK RECORD LOOK, LISTEN, FEEL SIGNS CLASSIFY TREAT AND ADVISE
How do your breasts feel?
Look at the nipple for fissure
Look at the breasts for:
→swelling
→shininess
→redness.
Feel gently for painful part of
the breast.
Measure temperature.
Observe a breastfeed
if not yet done
J4
.
Nipple sore or fissured.
Baby not well attached.
NIPPLE SORENESS
OR FISSURE
Encourage the mother to continue breastfeeding.
Teach correct positioning and attachment
K3
.
Reassess after 2 feeds (or 1 day). If not better, teach the mother
how to express breast milk from the affected breast and feed
baby by cup, and continue breastfeeding on the healthy side.
Both breasts are swollen,
shiny and patchy red.
Temperature <38ºC.
Baby not well attached.
Not yet breastfeeding.
BREAST
ENGORGEMENT
Encourage the mother to continue breastfeeding.
Teach correct positioning and attachment
K3
.
Advise to feed more frequently.
Reassess after 2 feeds (1 day). If not better, teach mother
how to express enough breast milk before the feed to relieve
discomfort
K5
.
Part of breast is painful,
swollen and red.
Temperature >38ºC.
Feels ill.
MASTITIS
Encourage mother to continue breastfeeding.
Teach correct positioning and attachment
K3
.
Give cloxacillin for 10 days
F5
.
Reassess in 2 days. If no improvement or worse, refer to hospital.
If mother is HIV-infected let her breastfeed on the healthy breast.
Express milk from the affected
breast and discard until no fever
K5
.
If severe pain, give paracetamol
F4
.
No swelling, redness
or tenderness.
Normal body temperature.
Nipple not sore and no
fissure visible.
Baby well attached.
BREASTS HEALTHY
Reassure the mother.
t
Next: Return to
J2
and complete the classification, then go to
J10
NEWBORN CARE
J9
Assess the mother’s breasts if complaining of nipple or breast pain
J9
ASSESS THE MOTHER’S BREASTS
IF COMPLAINING OF NIPPLE OR
BREAST PAIN
CARE OF THE NEWBORN
Use this chart for care of all babies until discharge.
CARE AND MONITORING RESPOND TO ABNORMAL FINDINGS
Ensure the room is warm (not less than 25ºC and no draught).
Keep the baby in the room with the mother, in her bed or within easy reach.
Let the mother and baby sleep under a bednet.
If the baby is in a cot, ensure baby is dressed or wrapped and covered by a blanket.
Cover the head with a hat.
Support exclusive breastfeeding on demand day and night.
Ask the mother to alert you if breastfeeding difficulty.
Assess breastfeeding in every baby before planning for discharge.
DO NOT discharge if baby is not yet feeding well.
If mother reports breastfeeding difficulty, assess breastfeeding and help the mother with positioning
and attachment
J3
.
Teach the mother how to care for the baby.
→Keep the baby warm
K9
.
→Give cord care
K10
.
→Ensure hygiene
K10
.
DO NOT expose the baby in direct sun.
DO NOT put the baby on any cold surface.
DO NOT bath the baby before 6 hours.
If the mother is unable to take care of the baby, provide care or teach the companion
K9-K10
.
Wash hands before and after handling the baby.
Ask the mother and companion to watch the baby and alert you if
→Feet cold.
→Breathing difficulty: grunting, fast or slow breathing, chest in-drawing.
→Any bleeding.
If feet are cold:
→Teach the mother to put the baby skin-to-skin
K13
.
→Reassess in 1 hour; if feet still cold, measure temperature and re-warm the baby
K9
.
If bleeding from cord, check if tie is loose and retie the cord.
If other bleeding, assess the baby immediately
J2-J7
.
If breathing difficulty or mother reports any other abnormality, examine the baby as on
J2-J7
.
Give prescribed treatments according to the schedule
K12
.
Examine every baby before planning to discharge mother and baby
J2-J9
.
DO NOT discharge before baby is 24 hours old.
t
Next:
Additional care of a small baby (or twin)
NEWBORN CARE
J10
Care of the newborn
J10
CARE OF THE NEWBORN
ADDITIONAL CARE OF A SMALL BABY (OR TWIN)
Use this chart for additional care of a small baby: preterm, 1-2 months early or weighing 1500 g-<2500 g. Refer to hospital a very small baby: >2 months early, weighing <1500 g
CARE AND MONITORING RESPOND TO ABNORMAL FINDINGS
Plan to keep the small baby longer before discharging.
Allow visits to the mother and baby.
Give special support for breastfeeding the small baby (or twins)
K4
:
→Encourage the mother to breastfeed every 2-3 hours.
→Assess breastfeeding daily: attachment, suckling, duration and frequency of feeds, and baby
satisfaction with the feed
J4
K6
.
→If alternative feeding method is used, assess the total daily amount of milk given.
→Weigh daily and assess weight gain
K7
.
If the small baby is not suckling effectively and does not have other danger signs, consider
alternative feeding methods
K5-K6
.
→Teach the mother how to hand express breast milk directly into the baby’s mouth
K5
→Teach the mother to express breast milk and cup feed the baby
K5-K6
→Determine appropriate amount for daily feeds by age
K6
.
If feeding difficulty persists for 3 days, or weight loss greater than 10% of birth weight and
no other problems, refer for breastfeeding counselling and management.
Ensure additional warmth for the small baby
K9
:
→Ensure the room is very warm (25º–28ºC).
→Teach the mother how to keep the small baby warm in skin-to-skin contact.
→Provide extra blankets for mother and baby.
Ensure hygiene
K10
.
DO NOT bath the small baby. Wash as needed.
Assess the small baby daily:
→Measure temperature
→Assess breathing (baby must be quiet, not crying): listen for grunting; count breaths per minute,
repeat the count if >60 or <30; look for chest in-drawing
→Look for jaundice (first 10 days of life): first 24 hours on the abdomen, then on palms and soles.
If difficult to keep body temperature within the normal range (36.5ºC to 37.5ºC):
→Keep the baby in skin-to-skin contact with the mother as much as possible
→If body temperature below 36.5ºC persists for 2 hours despite skin-to-skin contact with mother,
assess the baby
J2-J8
.
If breathing difficulty, assess the baby
J2-J8
.
If jaundice, refer the baby for phototherapy.
If any maternal concern, assess the baby and respond to the mother
J2-J8
.
Plan to discharge when:
→Breastfeeding well
→Gaining weight adequately on 3 consecutive days
→Body temperature between 36.5º and 37.5ºC on 3 consecutive days
→Mother able and confident in caring for the baby
→No maternal concerns.
Assess the baby for discharge.
If the mother and baby are not able to stay, ensure daily (home) visits or send to hospital.
NEWBORN CARE
J11
Additional care of a small baby (or twin)
J11
ADDITIONAL CARE OF A
SMALL BABY (OR TWIN)
ASSESS REPLACEMENT FEEDING
If mother chose replacement feeding assess the feeding in every baby as part of the examination.
Advise the mother on how to relieve engorgement
K8
. If mother is complaining of breast pain, also assess the mother’s breasts
J9
.
ASK, CHECK RECORD LOOK, LISTEN, FEEL SIGNS CLASSIFY TREAT AND ADVISE
Ask the mother
What are you feeding the baby?
How are you feeding your baby?
Has your baby fed in the
previous hour?
Is there any difficulty?
How much milk is baby taking
per feed?
Is your baby satisfied with the feed?
Have you fed your baby any other
foods or drinks?
Do you have any concerns?
If baby more than one day old:
How many times has your baby fed
in 24 hours?
How much milk is baby taking
per day?
How do your breasts feel?
Observe a feed
If the baby has not fed in the
previous hour, ask the mother
to feed the baby and observe
feeding for about 5 minutes.
Ask her to prepare the feed.
Look
Is she holding the cup to the
baby’s lips?
Is the baby alert, opens eyes
and mouth?
Is the baby sucking and
swallowing the milk effectively,
spilling little?
If mother has fed in the last hour,
ask her to tell you when her baby is
willing to feed again.
Not sucking (after 6 hours
of age).
Stopped feeding.
NOT ABLE TO FEED
Refer baby urgently to hospital
K14
.
Not yet fed (first 6 hours of life).
Not fed by cup.
Not sucking and swallowing
effectively, spilling
Not feeding adequate amount
per day.
Feeding less than 8 times per
24 hours.
Receiving other foods or drinks.
Several days old and inadequate
weight gain.
FEEDING DIFFICULTY
Teach the mother replacement feeding
G8
.
Teach the mother cup feeding
K6
.
Advise to feed more frequently, on demand,
day and night.
Advise the mother to stop feeding the baby other
foods or drinks or by bottle.
Reassess at the next feed or follow-up visit in
2 days.
Sucking and swallowing adequate
amount of milk, spilling little.
Feeding 8 times in 24 hours on
demand day and night.
FEEDING WELL
Encourage the mother to continue feeding by cup on
demand
K6
.
NEWBORN CARE
J12
Assess replacement feeding
J12
ASSESS REPLACEMENT FEEDING
Examinine routinely all babies around an hour of birth,
for discharge, at routine and follow-up postnatal visits in the
first weeks of life, and when the provider or mother observes
danger signs.
Use the chart Assess the mother’s breasts if the mother is
complaining of nipple or breast pain
J9
.
During the stay at the facility, use the Care of the newborn chart
J10
. If the baby is small but does not need referral, also use the
Additional care for a small baby or twin chart
J11
.
Use the Breastfeeding, care, preventive measures and treatment
for the newborn sections for details of care, resuscitation and
treatments
K1-K13
.
Use Advise on when to return with the baby
K14
for advising the
mother when to return with the baby for routine and follow-up
visits and to seek care or return if baby has danger signs.
Use information and counselling sheets
M5-M6
.
For care at birth and during the first hours of life, use Labour
and delivery
D19
.
ALSO SEE:
Counsel on choices of infant feeding and HIV-related
issues
G7-G8
.
Equipment, supplies and drugs
L1-L5
.
Records
N1-N7
.
Baby dead
D24
.
NEWBORN CARE
J1
Newborn care

16
useful to those directly providing care to pregnant women and
preterm infants, such as obstetricians, paediatricians, midwives,
nurses and general practitioners. The information in this guideline
will be useful for developing job aids and tools for pre- and in-
service training of health workers to enhance their delivery of
maternal and neonatal care relating to preterm birth. In includes list
of the nine-evidence based maternal and newborn interventions
to improve health outcomes for the preterm infants. The file also
includes the new WHO IPC guideline. It is the core components
of IPC programmes form a key part of WHO strategies to prevent
current and future threats, strengthen health service resilience and
help combat antimicrobial resistance (AMR). The guide is useful
to develop protocols for IPC and AMR action plans and to support
health care facilities as they develop or strengthen their own
approaches to IPC.
9. Training Supplies: The list contains essential supplies required
to organise in- services capacity building and training on Kangaroo
Mother Care (KMC). The list assumes that participants have skills
on essential newborn care and helping babies breathe/resuscitation.
The supply is for one session for 30 participants and five facilitators.
10. Articles: Born Too Soon, the Global Action Report on Preterm
Birth, published in 2012. It reports the magnitude of the problem,
evidence based interventions and delivery platforms, global action
agenda for research and advocates for increased resource and
accelerated progress. The 2010 Plos article describes new strategies
that can prevent, diagnose, and treat neonates with sepsis are
needed in both low- and high-income settings. The review of
neonatal sepsis gives an overview of the burden of bacterial sepsis
and meningitis in the newborn population in developing countries.
It is focused on the pathogens mostly implicated, their antibiotic
susceptibility patterns, and management. The 2005 Lancet paper
on hospital acquired neonatal infection in developing countries
reviewed the burden of hospital-acquired bacterial infections, the
range of neonatal pathogens and antimicrobial resistance, potentially
modifiable intrapartum and postnatal risk factors for infection,
and low-cost quality improvement, infection prevention strategies
for resource constrained settings and further research needs. In
Journal of Hospital Infection, 2008, authors describe strategies for
the prevention of nosocomial infections to include hand hygiene
practices, prevention of central venous catheter (CVC)-related
bloodstream infections (CRBSIs), judicious use of antimicrobials for
therapy and chemoprophylaxis, enhancement of host defenses, skin
care and early enteral feeding with human milk.

17
Facilitators
Learning Objectives
At the end of the sessions, participants will be able to acquire knowledge and skills
to manage LBW/preterm babies and counsel and support mothers and caregivers with
LBW/preterm babies
• Preparation and/or anticipating for birth of LBW/preterm newborns
and Essential newborn care
• Maintaining thermal care for the LBW/preterm and KMC positioning
• Feeding LBW/preterm babies
• Routine assessment of LBW/preterm babies for change of care or referral
• Referral, discharge, re-admission and follow-up of LBW/preterm babies
• KMC Implementation Experiences, challenges and Possible Solutions
• Increasing KMC support, and Action Planning for Implementation and Scale-up
• Perinatal Death Reviews using WHO guidelines
• IPC (Infection Prevention & Control) in Health Care Facilities (HCF)
Sitting arrangement/ Resources/Preparation required
Sitting arrangement
One facilitator per table
3 pairs of two Participants per table
Resources
• Facilitator Agenda
• ECSB Action Plan (on wall, or easel)
• ECSB Flipchart
• ECSB Kit
• PowerPoint presentation
• Videos
• Participant Agenda (1 per person)
• ECSB Provider Guide (1 per person)
• ECSB Parent Guide (1 per person)
• PremieNatalie (1 per pair)
• MamaBreast (1 per pair)
Other resources per table
• Alcohol handrub for hand washing
• Thermometers (type used locally)
• Vials of antibiotics
• Vial to simulate eye drops
• Vial to simulate Vitamin K
• 1.0 mL Syringe for Vitamin K
• 1.0 mL Syringe for antibiotics
• Cloth binder for skin-to skin care
• Baby blanket, cap, socks and nappy
• Measuring container for breast milk
• Cup, spoon, for feeding baby
• Clean nasogastric tube (5 or 6 French)
• Clean 20ml syringe
• Weighing scale, measuring tape and torch
Preparation required
• Organise venue for PowerPoint presentation
• Translate to local language if needed
LESSON PLAN
WORKSHOP TITLE: Kangaroo Mother Care (KMC)

18
Timing Facilitator/ Participant Activities Resources/tools required
DAY 1
Objective 1: Preparation for birth of LBW newborns & essential care– 100 mins
30
mins
• Explain, counsel and demonstrate essential care for
small babies (ECSB flip chart 1/1b)
• Explain on preparation for birth of LBW, and
coordination and collaboration among different teams
(ECSB flip chart 2/2b)
• Explain and demonstrate essential newborn
care - show video (7 mins)
• Explain and demonstrate essential care of the
small baby at birth (ECSB flip chart 3/3b) - show video
(7 mins)
• ECSB flip chart
• Videos
• PremieNatalie
• Vitamin K vial
and syringe
• Antibiotics vial
and syringe
• Baby blanket
40
mins
• Participants practice preparing for birth of a small baby,
and communicating with the family
• Participants practice on identifying steps that keep a
small baby well and support breathing, warmth, feeding,
and preventing infection
• Using a manikin, participants practice on essential care
of the small baby at birth
15
mins
• Explain and demonstrate classifying LBW babies (ECSB
flip chart 4/4b, 5/5b) –show video (6 mins)
15
mins
• Participants practice classifying the small baby
Objective 2: Maintaining thermal care for the LBW and KMC positioning – 90 mins
40
mins
• Explain and demonstrate assisting mothers to
provide skin-to-skin care for small babies in the first
24 hours, checking the temperature, and wrapping the
baby when no longer using skin-to-skin care (ECSB flip
chart 6/6b)
• Facilitator demonstrate interpersonal counseling skills
• Explain, counsel and demonstrate assessing a baby
during continuous skin-to-skin care for activity, breathing,
color and temperature (ECSB flip chart 7/7b, 8/8b)
• PowerPoint presentation
(slides 1-28)
• ECSB flip chart
• Videos
• PremieNatalie
• Cloth binder
• Thermometers
• Baby blanket
7
mins
• Show video (7 mins)
23
mins
• Using the manikin, participants practice continuous skin-
to-skin care, and assessing activity, breathing, color and
temperature (ECSB flip chart 9/9b)
20
mins
• Participants practice recording feedings and wet or dirty
diapers on a simple form

19
Timing Facilitator/ Participant Activities Resources/tools required
DAY 2
Objective 3: Feeding LBW babies – 300 mins
30
mins
• Q & A session for Day 1 lessons
Participants get a chance to ask questions on day 1
sessions and clarify any issues
• Videos
• ECSB flip chart
• PremieNatalie
• MamaBreast
• Measuring container for
breast milk
• Cup, spoon, for
feeding baby
• Clean NGT (5 or 6 French)
• Soap & water/Alcohol
hand rub
• Water to simulate milk
20
mins
• Explain, counsel and demonstrate supporting
breastfeeding and evaluating the baby’s effectiveness
at breastfeeding (ECSB flip chart 10/10b)
20
mins
• Working in pairs, participants practice evaluating baby’s
effectiveness at breastfeeding using case scenario
(ECSB flip chart 10b)
20
mins
• Explain, counsel and demonstrate expressing breastmilk,
and storing expressed milk (ECSB flip chart 11/11b)
show video (7 mins)
20
mins
• Using MamaBreast, participants practice on expressing
breastmilk and correctly storing breast milk
20
mins
• Explain, counsel and demonstrate cup feeding (ECSB
flip chart 12/12b)- show video (8.43 mins)
20
mins
• Participants practice feeding by cup, including proper/
thorough cleaning of cup/spoon before each feeding, and
assessing the baby’s ability to take cup or spoon feedings
25
mins
• Explain, counsel and demonstrate inserting and removing
a nasogastric tube (ECSB 13/13b)–show video (7 mins)
• Explain, counsel and demonstrate feeding with NGT
(ECSB flip chart 15/15b)–show video (6.15 mins)
20
mins
• Using a manikin, participants practice inserting NGT,
feeding with a NGT, and safely removing NGT
10
mins
• Explain feeding options for babies with HIV+ mothers
15
mins
• Explain and demonstrate determining appropriate
volume of breastmilk (ECSB flip chart 14/14b)
30
mins
• Participants discuss determining appropriate volume of
breastmilk using case scenarios (ECSB flip chart 14b)
20
mins
• Explain and demonstrate assessing signs of readiness
for breastfeeding (ECSB flip chart 16/16b)
https://globalhealthmedia.org/portfolio-items/
breastfeeding-the-small-baby/?portfolioID=5623(9)
(10.35 mins)
30
mins
• Participants discuss assessing breastfeeding readiness
using case scenarios (ECSB flip chart 16b)

20
Timing Facilitator/ Participant Activities Resources/tools required
Objective 4: Routine assessment of LBW babies for change of care or referral – 120 mins
20
mins
• Explain and demonstrate on routine assessment
of LBW babies for change of care or referral
(ECSB flip chart 18/18b)
• PowerPoint presentation
(slides 29-52)
• Daily weight follow-up,
ward observation
• Daily PNC check form
• Ward statistics forms
60
mins
• Participants work in groups of 3 (mother, provider,
colleague assuming care of the baby) practice case
scenario (ECSB flip chart 18b)
40
mins
• Participants practice on filling daily follow-up of vital
signs, adequacy of feeding, weight gain, danger signs
and filling forms and clinical notes
• participants practice interpersonal counseling skills
DAY 3
Objective 5: Referral, discharge and re-admission of LBW babies – 240 mins
30
mins
• Q & A session for Day 2 lessons
Participants get a chance to ask questions on day 2
sessions and clarify any issues
• Power Point presentation
(slides 53-64)
• Referral form (provider
guide, pg 60)
15
mins
• Explain and demonstrate prompt referral, and
stabilization for transport when a baby needs advance
care (ECSB flip chart 19/19b)
45
mins
• Participants work in pairs, discuss case scenarios
(ECSB flip chart 19b)
• Power Point presentation
(slides 6 5 -111)
• Parent Guide or local
materials
• Soap and water/ Alcohol
hand rub
• Bag and mask (optional)
20
mins
• Explain and demonstrate on planning for successful
discharge and home care (ECSB flip chart 20/20b)
40
mins
• Using parent guide or local materials, participants
practice on counselling the mother for home care
(ECSB flip chart 20b)
30
mins
• Explain and demonstrate proper hygiene and preventing
infection (ECSB flip chart 21/21b)
45
mins
• Discharge and outpatient high risk follow-up of preterm
and low birth weight infants
Note: The slides on neurological examination (Amiel Tison and
INFANIB exam) will be used when it is feasible. A pediatrician must
be available to provide mentoring support.
60
mins
• Participants practice on teaching the mother how to
wash hands
• Participants discuss hygiene practices and immunizations
given in the first 6 months (ECSB flip chart 21b)
45
mins
• Administer OSCE B to all participants • OSCE B

21
Timing Facilitator/ Participant Activities Resources/tools required
Objective 6: KMC Implementation Experiences, challenges
and Possible Solutions- 135 mins
40-60
mins
Introduction to KMC implementation and scale-up
• Expectations: what do learners want to be able to do at
the end of the workshop
• Learners share their own experience with KMC
implementation (if any) (a few short presentations or
discussion in group with plenary feedback)
Inform participants to include the following
key information:
• Total number of births (percentage of premature and
low birth weight infants)
• Neonatal mortality (percentage of deaths that are
attributed to prematurity or low birth weight)
• Place of birth (i.e. concentrated cities of the
country, number of births in the community VS.
institutional births)
• Basic description of the health system (i.e. different
levels of care, private institutions VS. public institutions
distribution, number of public hospitals, who pays for
health care in the government; health insurance,
out of pocket)
• Ethnic minorities and geographic distribution
• Current medical care that is being delivered to
premature and low birth weight infants and the cost of
providing such care
• Available data on screening and referral from lower
health facilities and follow-up babies monitored (in both
facility and community level)
• Nutrition profile (TIBF, EBF, wasting, stunting)
• Available policies or guidelines on infant and neonatal
care (i.e. Has the country being sensitized to KMC? is
KMC included in policies and national guidelines?)
• Institutions that offer traditional neonatal care/
institutions that offer neonatal care and KMC
(if any)
• Learners are prepared for further disseminating
knowledge and skills through training, orientation,
on-the-job training, etc. appropriate to the context
• Discussion
• Short presentations by
participants
• PowerPoint presentation
to guide the session
• Use training slide table
as handout
• USAID/MCHIP KMC
implementation guide
30
mins
Quality of care and supportive supervision – short
presentation with group activities in between
• Learners work in country or facility teams to document
ideas to include in country/facility action plans
• Power Point presentation
• Activity handout
• Example supportive
supervision checklists
• USAID/MCHIP KMC
implementation guide

22
Timing Facilitator/ Participant Activities Resources/tools required
40
mins
Multidisciplinary care and teamwork in KMC – short
presentation with group activities in between
• Participants brainstorm on categories of health
services, professionals and other health workers
that should be involved in KMC at different levels
of the health system per what is available in their
country or health facility (Examples: nutritionists/
dieticians, speech-language therapists, psychologists,
occupational therapists, physiotherapists,
ophthalmologists, neurologists, community
health workers)
• Discussion on the need for multidisciplinary care
in KMC and role of KMC for early childhood
development
• PowerPoint presentation
• Activity handouts
40
mins
Mobilizing support for KMC – short presentation with
group activities in between (national level, health
facilities and community)
• Participants brainstorm on KMC sensitization and
mobilization at different levels (Who? What? Where?
When? How?)
• Participants brainstorm how to look beyond barriers
and transform barriers into enablers
• Power Point presentation
• Activity handouts
• USAID/MCHIP KMC
implementation guide
DAY 4
Objective 7: Increasing KMC support, and Action Planning for Implementation
and Scale-up – 180 mins
30
mins
• Q & A session for Day 3 lessons
Participants get a chance to ask questions on day 3
sessions and clarify any issues
60
mins
Documentation for monitoring and evaluation
• Rationale for the monitoring and evaluation of KMC
• Utilization of data for program improvement
and advocacy
• Documentation and record keeping – case scenarios and
learners practice filling or interpreting patient records
and collective registers and and reflect on the use of the
results of the analysis
Power Point presentation
(Presentations: 3.5 and 3.6
and handouts: 3.5)
• Facilitator(s)and
participant(s) share
experiences
• Completed stats form
and KMC register
for discussion and
interpretation

23
Timing Facilitator/ Participant Activities Resources/tools required
30
mins
Action planning for KMC implementation
and scale-up
• Different interpretations of KMC, stages of change, tools
for measuring change, deciding on an approach
for scale-up
• Power Point
presentation
(Presentations: 3.1
and 3.6 and
handouts: 3.6
90
mins
Learners work in country/facility teams to develop
short- and long-term action plans (immediate, 3, 6,
and 12 months) – use available templates or design
own template
• Facility level: implementation or quality improvement
• District or regional level
• National level
Working groups hand in a copy of their action plan to the
lead facilitator – if hand written, the facilitator could make
a photocopy or take a picture so that participants take the
original plan with them
• Design templates for
country brain storming
(action plans [stages
of change/simple/ PPT
template], prioritizing
activities)
40-60
mins
Learners report back to other country/facility teams on
their plans – what will be done immediately, what will
be done immediately, within 1month, within 3 months, 6
months and one year (Could also be done on the next day)
• Power Point
• Electronic copy to lead
facilitator
60
mins
• Participants take a post-test assessment for the course
and do course evaluation
10
mins
• Closing, and post-course remarks
Formative/Summative Assessment
• Q & A
• Making presentations/being able to provide feedback
• Multiple Choice Questions Examination (MCQ): a 30-item examination
pre-and-post training.
• Objective Structured Clinical Exams (OSCEs): two OSCEs.
• OSCE A to evaluate the skills of positioning, counseling and assessment
with skin-to-skin care.
– If time allows.
– If not conduct only B
• OSCE B to evaluate the skills of family counseling, NG placement
and NG feed administration.

24
Essential Care for Small Babies – Knowledge check
Select the best answer to each question or statement Circle the letter of the
correct answer
1. Which of the following statements correctly describes
a well small baby?
Feeds by cup, stays warm with skin-to-skin care, has convulsions
Feeds by cup, stays warm with skin-to-skin care, weighs 1600 grams
Breastfeeds poorly, breathes at 100 times per minute, maintains
temperature in an incubator
Feeds by cup, weighs 1200 grams, maintains temperature in an incubator
2. Which of the following is an important step in the care of
a small baby?
Teaching the mother to give a bath
Giving the small baby lots of time in the sunlight
Preventing infection by washing hands before touching the baby
Weighing the small baby five times a day
3. Which of the following statements describes preparation
for the birth of a small baby?
Identify a skilled helper, provide extra warmth in the area for delivery,
anticipate need to help the baby breathe at birth.
Prepare an area for the baby’s bath, check equipment,
review emergency plan.
Wash hands, prepare herbs for babies first feeding.
Anticipate need to help baby breathe at birth, identify a skilled helper,
prepare an area for the baby’s bath.
a
b
c
d
a
b
c
d
a
b
c
e
KNOWLEDGE CHECK
(PRE-AND POST-TEST)

25
4. A 1700-gram baby has been placed skin-to-skin with the mother after birth.
What other care should be provided in the first 90 minutes after birth?
Showing the baby to the extended family
Feeding the baby with a nasogastric tube
Monitoring breathing and measuring temperature
Bathing the baby
5. At 90 minutes after birth, an 1800-gram baby is placed skin-to-skin
with the mother and has a temperature of 36.7˚ C. What should you
do to help maintain the baby’s temperature?
Bathe the baby in warm water.
Place in direct sunlight.
Assist mother with continuous skin-to-skin care.
Place the baby on an open warmer set for high heat output.
6. Shortly after birth, a small baby is classified based on the temperature,
weight, and physical exam. The baby is 1400 grams, is breathing at 90
breaths per minute, and has a temperature of 35˚C. What should you do?
Put the baby to the breast to assess breastfeeding.
Continue to watch for improvement.
Place a nasogastric tube to administer a feeding.
Arrange a transfer for advanced care.
7. How many feedings should a small baby receive in a day?
Two to four
Five to six
Eight to twelve
Twenty-four
a
b
c
d
a
b
c
d
a
b
c
d
a
b
c
d

26
8. Which of the following techniques can help a mother to support
or improve a small baby’s latch?
Wrapping the breasts in tight clothing between feedings
Supporting the head of the baby so he is positioned to take the nipple
and surrounding area into an open mouth
Putting oils on the breast
Feeding first with a bottle until sucking is strong
9. What is the skin temperature of a well small baby?
35.0-35.5˚C
35.5-36.5˚C
36.5-37.5˚C
37.0-38.0˚C
10. Shortly after birth, the temperature of an 1800-gram baby is 36˚C.
After placing the baby skin-to-skin, the baby’s temperature remains
the same. Which of the following actions should be taken?
Place the baby in direct sunlight.
Place warm stones around the baby.
Bathe the baby in warm water.
Remove wet diaper and cover the mother and the baby with a blanket.
11. A 1600-gram baby has been maintaining temperature with
continuous skin-to-skin care. The baby will not breastfeed or cup feed
and requires nasogastric feeding. What do you advise the mother
about skin-to-skin care?
The mother can continue skin-to-skin care even while the baby
is receiving nasogastric feedings.
The baby will need to be in an incubator while receiving nasogastric feeding.
The baby will need to be on a radiant warmer while receiving
nasogastric feeding.
The mother must stop skin-to-skin care during nasogastric feeding.
a
b
c
d
a
b
c
d
a
b
c
d
a
b
c
d

27
12. When a baby cannot feed directly from the breast after support is
provided, what should you advise a mother to do next?
Give the baby formula.
Keep trying to breastfeed the baby.
Express her breast milk to feed to the baby by a safe,
alternate feeding method.
Wait until the baby can feed directly from the breast.
13. When a mother expresses her breast milk, how can it be stored safely?
In a covered container in a cool place for up to 6 hours
In an open container in a shaded area
In an open container in direct sunlight
In a covered container heated in warm water until used
14. When breastfeeding is not effective, which of the following are safe
and recommended alternate feeding methods for a small baby?
Attempt cup feedings and if not successful, insert a nasogastric tube.
Use a syringe to pour milk directly into the baby’s mouth.
Dip finger or tongue depressor into milk and allow the baby to lick the milk.
Give bottle feedings and insert a nasogastric tube.
15. Which of the following best describes a 3-day-old 1800-gram baby
who needs nasogastric tube feeding?
The baby is breastfeeding 8-12 times per day.
The baby is gaining 15 grams/kilograms per day.
The baby shows feeding readiness cues every 2-4 hours.
The baby takes 5-10 mL by cup per feeding for 4 feedings.
16. What is the proper length for nasogastric tube insertion?
From the tip of the nose to earlobe to half way between the tip of
the breast bone and the umbilicus
From the mouth opening to the nipple to the umbilicus
From the earlobe to the umbilicus
From the tip of the nose to the chin to the bottom of the breast bone
a
b
c
d
a
b
c
d
a
b
c
d
a
b
c
d
a
b
c
d

28
17. You have just inserted a nasogastric tube into a small baby who cannot
breastfeed or receive cup feedings. Which of the following best describes
a method for confirming proper placement of the nasogastric tube?
Measure the tube outside the nose.
Inject 2 mL of air while listening with a stethoscope for the sound of air
entering the stomach.
Administer 5 mL of a feeding and then withdraw it back to see if it is
mixed with gastric contents.
Evaluate the baby’s breathing.
18. What should a mother be taught to do before administering
a nasogastric feeding?
Wash her hands and reinsert the nasogastric tube.
Wash her hands and confirm placement of the nasogastric tube by
checking that the mark on the tube is at the edge of the nose.
Wash her hands and confirm placement of the nasogastric tube by
checking that the mark on the tube is at the sternum.
Wash her hands and inject 10 mL of air into the tube.
19. After initial weight loss, how much weight should a small baby
gain each day?
5 grams per kilogram per day on average
15 grams per kilogram per day on average
25 grams per kilogram per day on average
30 grams per day on average
20. On the day after birth, a 1600-gram baby cannot breastfeed or cup
feed, and will be fed every three hours by a nasogastric tube. What
volume should be administered for the baby’s first feeding?
1 mL
5 mL
12 mL
25 mL
a
b
c
d
a
b
c
d
a
b
c
d
a
b
c
d

29
21. A 1600-gram baby is fed by a nasogastric tube. After the initial day of
feedings, what is the daily increase in the volume of each feeding?
4 mL
5 mL
10 mL
15 mL
22. Which of the following indicates feeding intolerance and the need
for advanced care?
Spitting up small amounts
Tense abdominal distension
Stooling 6-8 times per day
Crying before each feeding
23. In a small baby being fed by an alternative method, how often should
breastfeeding readiness be assessed?
At least once per day
At least once per week
At least once every two weeks
At least once per month
24. A small baby is now 10 days old and has been fed by nasogastric tube
since birth. During the first attempt to breast feed, he sucks actively,
and swallowing sounds are heard. What should be done next to
make the transition to breastfeeding?
Stop nasogastric feeding immediately, pull out the nasogastric tube,
and breastfeed only.
Continue with nasogastric feeding, while gradually increasing the number
of breastfeeding attempts per day.
Stop nasogastric feeding immediately and breastfeed only
throughout the daytime.
Continue with nasogastric feeding, wait two days, and try
breastfeeding again.
a
b
c
d
a
b
c
d
a
b
c
d
a
b
c
d

30
25. A 1600-gram baby has been receiving nasogastric feeding for 10 days
and now has started to feed at the breast. Which of the following is an
indication that the baby is ready to receive all the feedings by breast?
Waking and crying in between feedings.
Choking during occasional feedings
Sucking and swallowing audibly for 10 minutes during each feeding
Weight gain of 5 grams per day when no nasogastric feedings
are provided
26. Small babies should be regularly assessed for:
Frequency and success at feeding, temperature, presence of hiccups
Activity, breathing, color, temperature and weight gain
Breathing problems, temperature, and white blood cell count
Frequency and success at feeding, cough, presence of convulsions
27. A 2-day-old 1700-gram baby has a normal examination and breathing
rate. How often should the baby be assessed for temperature,
breathing and feeding tolerance?
Once per day
Every 2 to 3 hours
At least once per shift.
Only if the baby seems ill
28. When should the mother or other providers wash their hands in
order to protect a small baby?
Before touching the baby and before preparing a feeding
Before greeting the family
Before closing a window
Before leaving the hospital at the end of the day
a
b
c
d
a
b
c
d
a
b
c
d
a
b
c
d
31
29. A small baby needs to be referred for advanced care to a hospital
1 hour away. What should you do to prepare the baby for transport?
Place a nasogastric tube so that mother can feed through the tube during
transport.
Continuation of KMC in transit and communicate with health providers at
the receiving facility and the family, and prepare a referral note.
Bathe the baby to prevent infection.
Use a radiant warmer to warm the baby to 38˚C so that the baby will
maintain temperature during transport.
30. Which of the following statements below describes a small baby who
should be considered for discharge from the birth facility?
The mother has not demonstrated competence with infant feeding, the
baby has adequate weight gain documented over 3 consecutive days, and
breathes 40 breaths per minute.
The mother has demonstrated competence with infant feeding, the baby
has adequate weight gain documented over 3 consecutive days, and the
baby breathes 40 breaths per minute.
The mother has demonstrated competence with infant feeding, the baby
has adequate weight gain documented over 3 consecutive days, and the
baby is breathing 80 breaths per minute.
The mother has demonstrated competence with infant feeding, the baby
has adequate weight gain documented over 5 consecutive days, and the
baby is under a radiant warmer.
a
b
c
d
a
b
c
d
Answer to Knowledge Check (Pre and post-test)
1. B
2. C
3. A
4. C
5. C
6. D
7. C
8. B
9. C
10. D
11. A
12. C
13. A
14. A
15. D
16. A
17. B
18. B
19. B
20. C
21. A
22. B
23. A
24. B
25. C
26. B
27. C
28. A
29. B
30. B

32
ID:__________________________
OSCE A – Classify, Provide continuous skin-to-skin care and monitor
“I am going to read a role play case. Please show and tell me what you would do to take care of this small baby.
I will only give indication about the baby’s condition when you ask. No other feedback will be given until the end of the case.”
“A 28-year-old mother has given birth to a 1700 gram baby. You have provided essential care, including cord care, vitamin K,
and eye care. You perform your rst assessment. You nd that the baby is breathing well and the rest of the exam is normal;
the temperature is 36.3˚C. Tell me what information you will use, how you will classify the baby and what thermal care the
baby will need.”
Classify the small baby Done Not Done
Uses the weight, temperature and exam to classify the baby ................................................................................
Recognizes a well small baby ..........................................................................................................................................................
Plans to provide continuous skin-to-skin care ..............................................................................................................
Prompt: This is a well small baby who will need continuous skin-to- skin care.
Describe and show how you will help mother begin continuous skin-to-skin care.
Show the mother how to do skin-to-skin care
Explains to mother the steps and advantages of skin-to-skin care ......................................................................
Dresses baby with diaper, hat and socks (if available) ...............................................................................................
Places the baby upright on mother’s skin between breasts ....................................................................................
Positions baby with arms and legs exed, head turned............................................................................................
Secures snugly with a cloth pulled up to the ear .........................................................................................................
Covers with a garment or closes mother’s shirt ............................................................................................................
Prompt: The baby and mother are comfortable.
Please demonstrate how you will monitor the baby and show the mother about
how to monitor the baby while in skin-to-skin.
Monitors baby’s activity, breathing, color, temperature ...........................................................................................
Advises mother how to monitor activity, breathing, color, temperature ..........................................................
SCORING:
Successful completion requires a total score of 9 of 12. Incompletely done items should be marked as “Not Done.”
SCORE: ______________________________/ 12
ID:__________________________
OSCE B – Feeding with a nasogastric tube and daily assessment
“I am going to read a role play case. Please show and tell me what you would do to take care of this small baby.
I will only give indication about the baby’s condition when you ask. No other feedback will be given until the end of the case.”
“A 1700 gram baby is 8 hours old. The baby has a normal physical exam, and has been maintaining a temperature
of 36.7˚C with continuous skin-to-skin care. The baby did not latch well at the breast and did not tolerate cup feeding.
Mother has successfully expressed 15mL of milk. Describe and show what you will do next to feed this small baby.”
Done Not Done
Insert a nasogastric tube
Communicates with the mother about need for nasogastric feeding ...............................................................
Washes hands .............................................................................................................................................................................
Measures depth tube should be inserted and marks tube ......................................................................................
Lubricates tube with expressed breast milk ...................................................................................................................
Inserts tube ..................................................................................................................................................................................
Conrms proper placement ..................................................................................................................................................
Tapes tube on face ....................................................................................................................................................................
Prompt: Show how you will feed breast milk with the nasogastric tube.
Feed with a nasogastric tube
Determines amount of feeding baby requires (12 mL) .............................................................................................
Measures the amount to be fed ..........................................................................................................................................
Connects syringe and transfers milk with tube pinched ..........................................................................................
Allows milk to slowly enter stomach .................................................................................................................................
Removes syringe, recaps tube .............................................................................................................................................
Prompt: The baby is now ve days old and you are doing your daily assessment.
Tell me what you will assess and I will provide the ndings.
After completing your assessment please tell me your plan.
Describe a daily assessment
Maternal concerns (none) ......................................................................................................................................................
Physical assessment (active, breathing well, pink, warm) ........................................................................................
Temperature (36.7⁰C) ...........................................................................................................................................................................
Weight (1550 grams) ...............................................................................................................................................................
Intake (nasogastric feeds 24 mL every 3 hours, good tolerance) ...........................................................................
Output (7 wet diapers, 3 stools)...........................................................................................................................................
Recognizes that the baby remains well............................................................................................................................
Advance feedings to 28 mL every 3 hours ......................................................................................................................
SCORING:
Successful completion requires a total score of 16 of 20. Incompletely done items should be marked as “Not Done.”
SCORE: _____/20
26b
SKILL ASSESMENT TOOL

33
ID:__________________________
OSCE A – Classify, Provide continuous skin-to-skin care and monitor
“I am going to read a role play case. Please show and tell me what you would do to take care of this small baby.
I will only give indication about the baby’s condition when you ask. No other feedback will be given until the end of the case.”
“A 28-year-old mother has given birth to a 1700 gram baby. You have provided essential care, including cord care, vitamin K,
and eye care. You perform your rst assessment. You nd that the baby is breathing well and the rest of the exam is normal;
the temperature is 36.3˚C. Tell me what information you will use, how you will classify the baby and what thermal care the
baby will need.”
Classify the small baby Done Not Done
Uses the weight, temperature and exam to classify the baby ................................................................................
Recognizes a well small baby ..........................................................................................................................................................
Plans to provide continuous skin-to-skin care ..............................................................................................................
Prompt: This is a well small baby who will need continuous skin-to- skin care.
Describe and show how you will help mother begin continuous skin-to-skin care.
Show the mother how to do skin-to-skin care
Explains to mother the steps and advantages of skin-to-skin care ......................................................................
Dresses baby with diaper, hat and socks (if available) ...............................................................................................
Places the baby upright on mother’s skin between breasts ....................................................................................
Positions baby with arms and legs exed, head turned............................................................................................
Secures snugly with a cloth pulled up to the ear .........................................................................................................
Covers with a garment or closes mother’s shirt ............................................................................................................
Prompt: The baby and mother are comfortable.
Please demonstrate how you will monitor the baby and show the mother about
how to monitor the baby while in skin-to-skin.
Monitors baby’s activity, breathing, color, temperature ...........................................................................................
Advises mother how to monitor activity, breathing, color, temperature ..........................................................
SCORING:
Successful completion requires a total score of 9 of 12. Incompletely done items should be marked as “Not Done.”
SCORE: ______________________________/ 12
ID:__________________________
OSCE B – Feeding with a nasogastric tube and daily assessment
“I am going to read a role play case. Please show and tell me what you would do to take care of this small baby.
I will only give indication about the baby’s condition when you ask. No other feedback will be given until the end of the case.”
“A 1700 gram baby is 8 hours old. The baby has a normal physical exam, and has been maintaining a temperature
of 36.7˚C with continuous skin-to-skin care. The baby did not latch well at the breast and did not tolerate cup feeding.
Mother has successfully expressed 15mL of milk. Describe and show what you will do next to feed this small baby.”
Done Not Done
Insert a nasogastric tube
Communicates with the mother about need for nasogastric feeding ...............................................................
Washes hands .............................................................................................................................................................................
Measures depth tube should be inserted and marks tube ......................................................................................
Lubricates tube with expressed breast milk ...................................................................................................................
Inserts tube ..................................................................................................................................................................................
Conrms proper placement ..................................................................................................................................................
Tapes tube on face ....................................................................................................................................................................
Prompt: Show how you will feed breast milk with the nasogastric tube.
Feed with a nasogastric tube
Determines amount of feeding baby requires (12 mL) .............................................................................................
Measures the amount to be fed ..........................................................................................................................................
Connects syringe and transfers milk with tube pinched ..........................................................................................
Allows milk to slowly enter stomach .................................................................................................................................
Removes syringe, recaps tube .............................................................................................................................................
Prompt: The baby is now ve days old and you are doing your daily assessment.
Tell me what you will assess and I will provide the ndings.
After completing your assessment please tell me your plan.
Describe a daily assessment
Maternal concerns (none) ......................................................................................................................................................
Physical assessment (active, breathing well, pink, warm) ........................................................................................
Temperature (36.7⁰C) ...........................................................................................................................................................................
Weight (1550 grams) ...............................................................................................................................................................
Intake (nasogastric feeds 24 mL every 3 hours, good tolerance) ...........................................................................
Output (7 wet diapers, 3 stools)...........................................................................................................................................
Recognizes that the baby remains well............................................................................................................................
Advance feedings to 28 mL every 3 hours ......................................................................................................................
SCORING:
Successful completion requires a total score of 16 of 20. Incompletely done items should be marked as “Not Done.”
SCORE: _____/20
26b

34
The template below can be used over time during the implementation and
expansion of kangaroo mother care (KMC) services. Some of the points to
consider relate to higher levels of the health system, some to facilities, and
others to both. These points are the ideal. Also consider how one would go
about getting there within the reality and constraints within the region, districts,
sub districts, health facilities and communities. Concentrate on Stages 1 and
2 and parts of Stage 3 for identifying the initial actions needed to get the ball
rolling for the implementation and expansion of kangaroo mother care in your
district/region/country. Relevant statements and descriptions your country’s
strategic plans and other policy and guideline documents should also inform
the planning. Organise the outcomes of your discussion and actions that will
be initiated according to the following timeline and allocate a specific person or
persons for each action as well as a date, timeline or deadline. Identify at least
five main action points for each time period: 1. immediately; 2. within 3 months;
3. within 6 months, 4. within 1 year and 5. Beyond 1 year
Template for SWOT ANALYSIS
STRENGTHS
How are we going to
use these strengths in
the implementation
of KMC?
WEAKNESSES
How are we going to try
to improve on or avoid
these weaknesses in the
implementation of KMC?
OPPORTUNITIES
How can we use
these opportunities to
provide quality KMC?
THREATS
What can we do to
minimise these threats in
the unit or ward where
KMC is practised?
DISCUSSION GUIDES FOR GROUP
WORKS/TEMPLATES
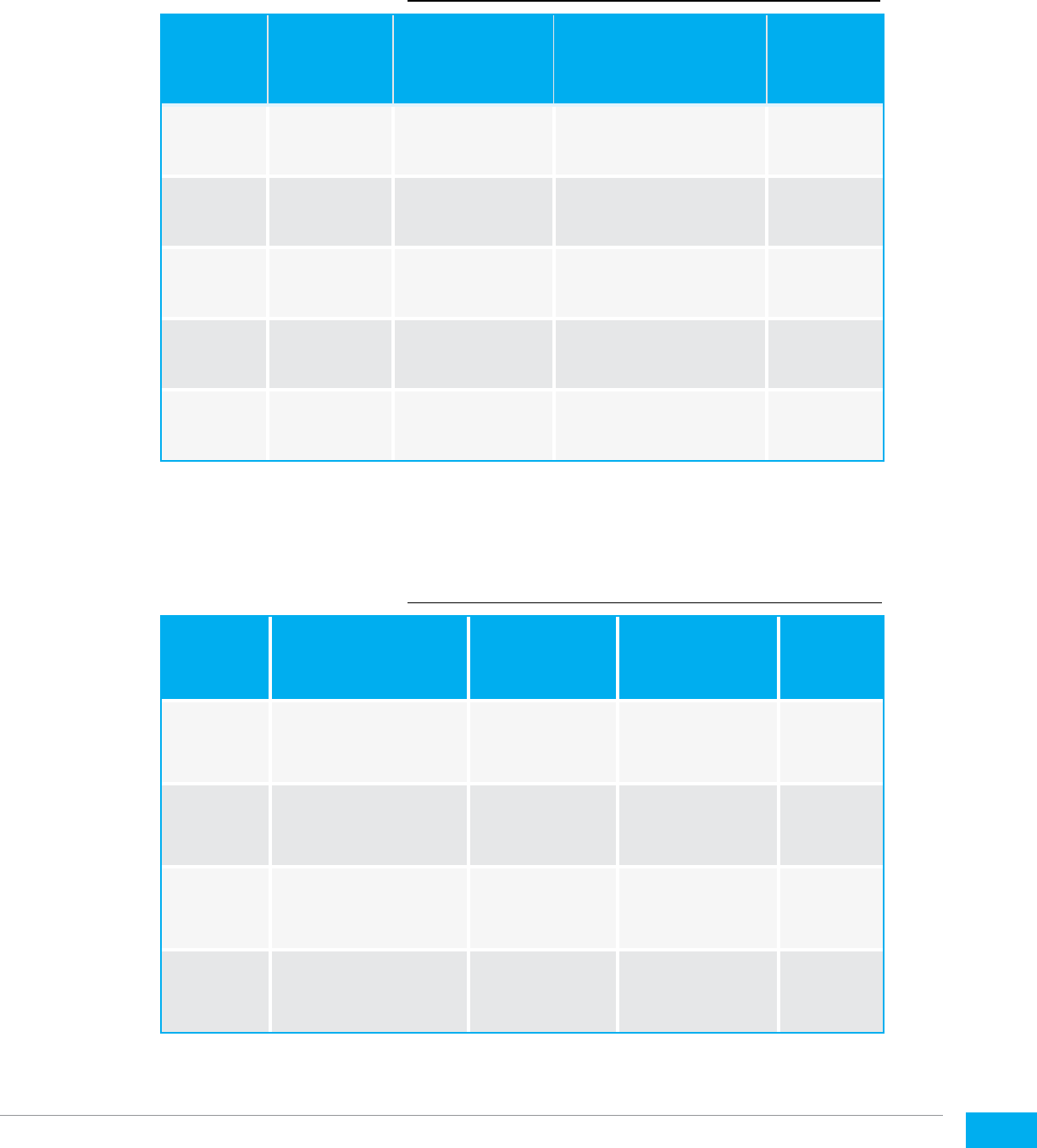
35
Template for Follow-up monitoring
and national scale-up plan
Name of hospital / country:
Action
(key word)
What needs
to be done?
Responsible
person(s)
Deadline for action /
Date for report back
Remarks
Template for Prioritising Actions
Name of hospital / country:
Action
Must do immediately
(within 2 weeks)
Must do within
1 month
Should be
completed
within 3 months
Things to
do later
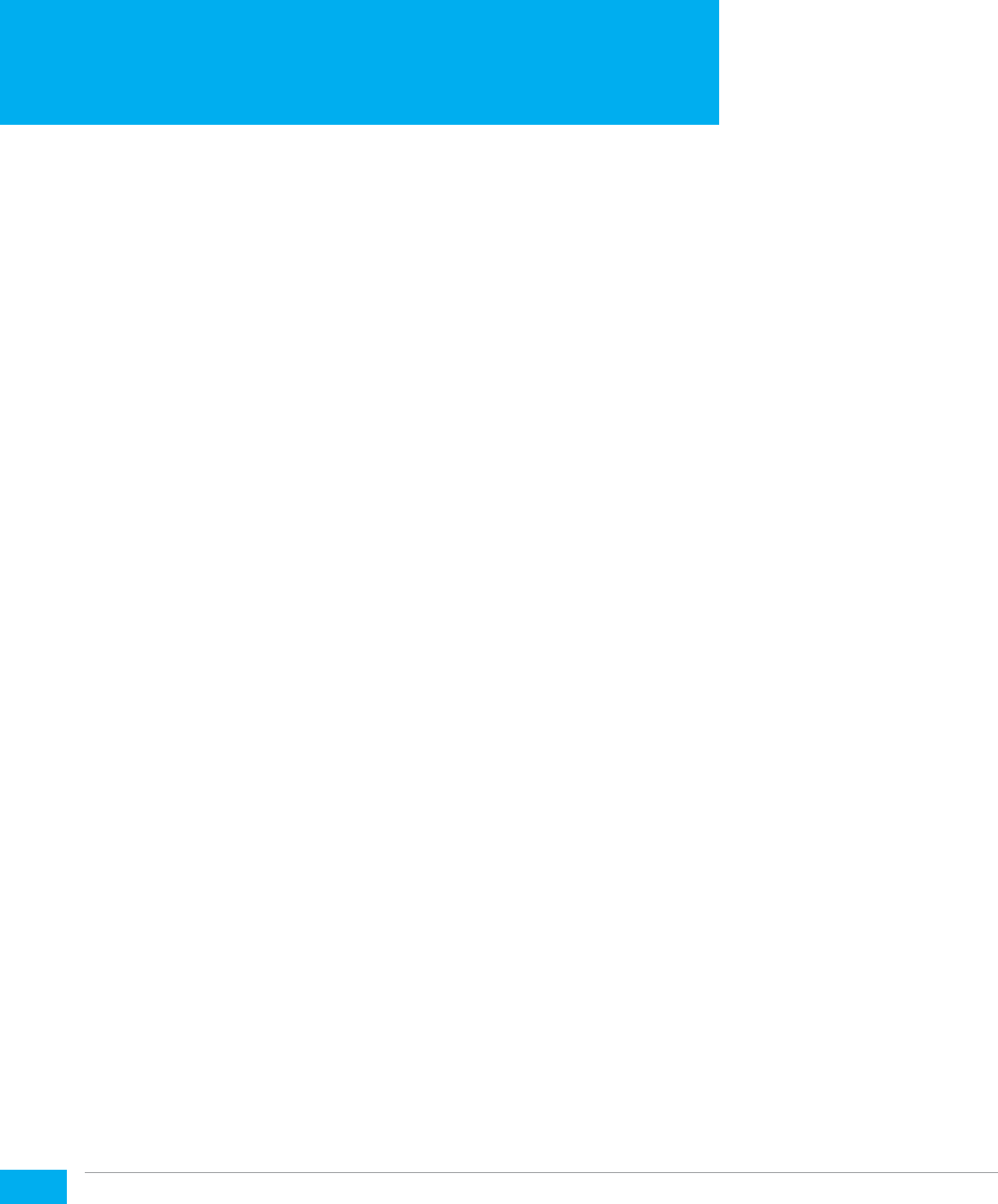
36
Administrative note
Six to eight weeks prior to the workshop send out adminstatrative note to
all partcipants. In the note include key informations such as dates of arrival,
departure and the training, venue and list of possible accomodations, visa
requirments and arrangments, security and weather situation, transportation
arrangement, restaurant and medical facilties and contact information of key
personell. In a seprate e mail is is important to guide on preprations that
partcipants need to make before coming to the traning.
Introduction to workshop participants
Prepare an introduction package with participants’ bios and pictures that
allow better acquaintance. In addition this will allow facilitators to understand
participants’ educational background, experience in newborn care etc. that will
be useful for sitting arrangement and facilitation process.
At least one day prior to the workshop; it is important to arrange the room in
small groups and ensure AV equipment is working properly. On the day of the
workshop arrive early to prepare the room, get to know your audience, do an
icebreaker, assess the range of prior knowledge/experience with the topic,
glean what they hope to accomplish by attending, don’t deviate from the
timeline, designate a time-keeper, utilize effective presentation skills and
group facilitation strategies. Remember to station someone at the exit door
to collect evaluations.
Team building at the beginning and introductions
Ice breakers
Ice breakers can be an effective way of starting a training session or
team-building event. As interactive and often fun sessions run before the
main proceedings, they help people get to know each other and buy into the
purpose of the event.
If such a session is well-designed and well-facilitated, it can really help get
things off to a great start. By getting to know each other, the facilitators,
and learning about the objectives of the event, people can become more
engaged in the proceedings and so contribute more effectively towards a
successful outcome.
TIPS FOR FACILITATORS FOR
CRINKLE-FREE WORKSHOP

37
When to Use Icebreakers
As the name suggests, these sessions are designed to “break the ice” at an
event or meeting. The technique is often used when people who do not
usually work together, or may not know each other at all, meet for a specific,
common purpose.
Consider using an ice breaker when:
• Participants come from different backgrounds.
• People need to bond quickly to work towards a common goal.
• Your team is newly formed.
• The topics you are discussing are new or unfamiliar to
many people involved.
• As facilitator, you need to get to know participants and have them
know you better.
Introductory Ice Breakers
These are used to introduce participants to each other and to facilitate
conversation amongst them.
The Little-Known Fact: ask participants to share their name, department
or role in the organization, length of service, and one little known fact about
themselves. This “little known fact” becomes a humanizing element that can
help break down differences such as grade/status in future interaction.
True or False: ask your participants to introduce themselves and make three or
four statements about themselves, one of which is false. Now get the rest of
the group to vote on which fact is false. As well as getting to know each other
as individuals, this exercise helps to start interaction within the group.
Interviews: ask participants to get into twos. Each person then interviews his
or her partner for a set time while paired up. When the group reconvenes,
each person introduces their interviewee to the rest of the group.
Problem Solvers: ask participants to work in small groups. Create a simple
problem scenario for them to work on in a short time. Once the group have
analyzed the problem and prepared their feedback, ask each group in turn to
present their analysis and solutions to the wider group.

38
Facilitator meetings
Each day, review the teaching activities that completed. Review what worked
well and what needs to be improved in the next day. Identify which participants
need more support. Review what will occur the next day and agree on each
roles and responsibilities. Preprare the venu for next day’s session, print group
work guides, templates, formats, pre-post test and evaluation forms. The
meeting should not be more than an hour and each facilitator could take part in
leading the meeting.
Sample Budget for the KMC training
8
Details
Costs US$
1 Facilitators travel and honorarium (4 facilitators x 6 days) 10,080.00
2 Tentative travel cost of facilitators (direct economy fare and DSA -
rounded off though travel cost would vary for individuals joining from
different countries) : (4x 5000= 20,000)
20,000.00
3 Training materials including manikins 500.00
4 Printing, documentation etc 200.00
4 Training venue including accommodation of participants &
interpretation services
10,685.00
5 Travel and DSA of 30 participants (4 each from 8 countries) 45,504.00
6 Hospital Visit (transport costs)
500.00
7 Follow-up monitoring 10,300.00
Total 97,769.00
8 This is hypothetical budget. Modify to fit the need
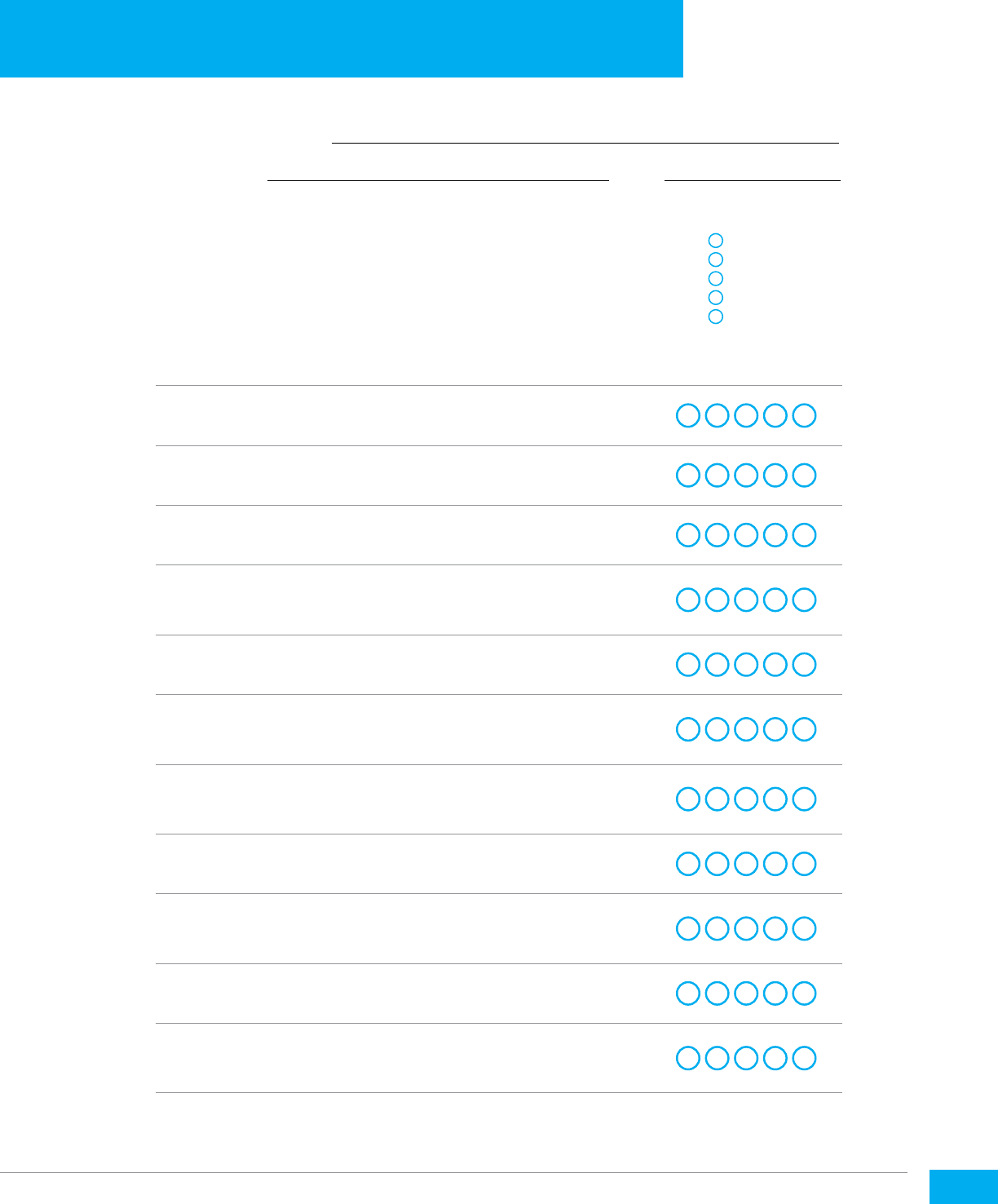
39
Workshop Location:
Facilitator(s): Date:
Your feedback is important for planning future workshops.
Please respond to the following statements by using the 5-point
rating scale to indicate the extent to which you agree or disagree
with each statement. Thank you.
Circle your response
Workshop objectives were stated clearly and met
1
2
3
4
5
The workshop was well organized
1
2
3
4
5
The workshop met my expectations
1
2
3
4
5
The information and/or skills presented were
relevant and useful
1
2
3
4
5
The workshop activities stimulated my learning
1
2
3
4
5
This workshop increased my knowledge/skills
in caring for LBW and small babies
1
2
3
4
5
The facilitator(s) had a good understanding
of the topics
1
2
3
4
5
The handouts were helpful
1
2
3
4
5
The workshop materials and facilities were
adequate and comfortable
1
2
3
4
5
The length of the workshop was appropriate
1
2
3
4
5
I recommend that the workshop be repeated
for other providers
1
2
3
4
5
WORKSHOP EVALUATION
1
= Strongly Disagree
2
= Disagree
3
= Neutral
4
= Agree
5
= Strongly Agree

40
What were the most useful aspects/strengths
of the workshop?
What changes should be made to enhance/improve
this workshop?

41
Additional comments:

© United Nations Children’s Fund (UNICEF)
December 2018
