CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 1 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
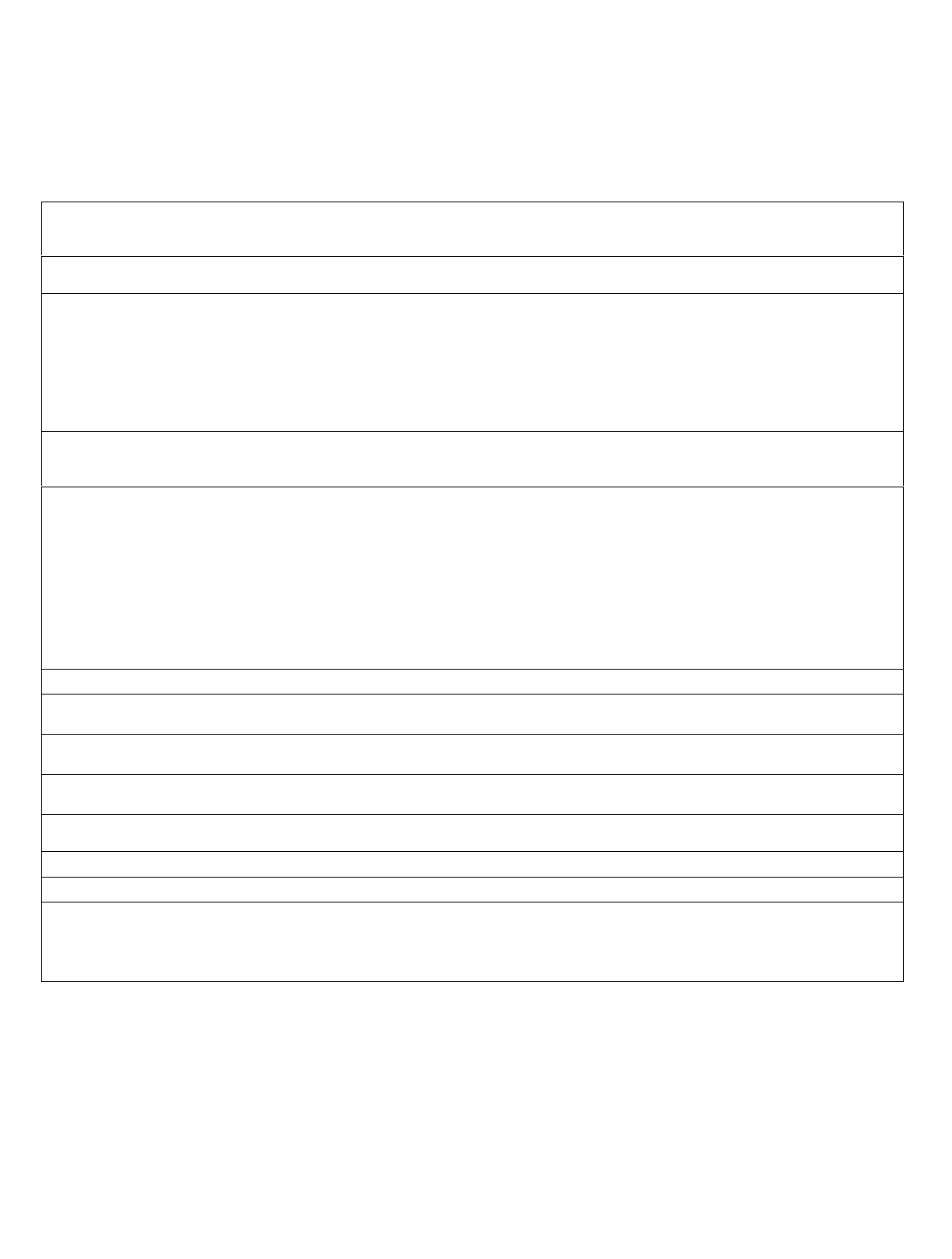
COMMON TOXICITY CRITERIA (CTC)
Grade
Adverse Event 0 1 2 3 4
ALLERGY/IMMUNOLOGY
Allergic reaction/
hypersensitivity
(including drug fever)
none
transient rash, drug
fever <38°C (<100.4°F)
urticaria, drug fever
≥38°C (≥100.4°F),
and/or asymptomatic
bronchospasm
symptomatic
bronchospasm,
requiring parenteral
medication(s), with or
without urticaria;
allergy-related
edema/angioedema
anaphylaxis
Note: Isolated urticaria, in the absence of other manifestations of an allergic or hypersensitivity reaction, is graded in the DERMATOLOGY/SKIN category.
Allergic rhinitis
(including sneezing, nasal
stuffiness, postnasal drip)
none mild, not requiring
treatment
moderate, requiring
treatment
--
Autoimmune reaction none serologic or other
evidence of
autoimmune reaction
but patient is
asymptomatic (e.g.,
vitiligo), all organ
function is normal and
no treatment is required
evidence of
autoimmune reaction
involving a non-
essential organ or
function (e.g.,
hypothyroidism),
requiring treatment
other than
immunosuppressive
drugs
reversible autoimmune
reaction involving
function of a major
organ or other adverse
event (e.g., transient
colitis or anemia),
requiring short-term
immunosuppressive
treatment
autoimmune reaction
causing major grade 4
organ dysfunction;
progressive and
irreversible reaction;
long-term
administration of high-
dose immuno-
suppressive therapy
required
Also consider Hypothyroidism, Colitis, Hemoglobin, Hemolysis.
Serum sickness none - - present -
Urticaria is graded in the DERMATOLOGY/SKIN category if it occurs as an isolated symptom. If it occurs with other manifestations of allergic or
hypersensitivity reaction, grade as Allergic reaction/hypersensitivity above.
Vasculitis none mild, not requiring
treatment
symptomatic, requiring
medication
requiring steroids ischemic changes or
requiring amputation
Allergy/Immunology - Other
(Specify, __________)
none mild moderate severe
life-threatening or
disabling
AUDITORY/HEARING
Conductive hearing loss is graded as Middle ear/hearing in the AUDITORY/HEARING category.
Earache is graded in the PAIN category.
External auditory canal normal
external otitis with
erythema or dry
desquamation
external otitis with
moist desquamation
external otitis with
discharge, mastoiditis
necrosis of the canal
soft tissue or bone
Note: Changes associated with radiation to external ear (pinnae) are graded under Radiation dermatitis in the DERMATOLOGY/SKIN category.

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 2 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Grade
Adverse Event 0 1 2 3 4
Inner ear/hearing normal hearing loss on
audiometry only
tinnitus or hearing loss,
not requiring hearing
aid or treatment
tinnitus or hearing loss,
correctable with hearing
aid or treatment
severe unilateral or
bilateral hearing loss
(deafness), not
correctable
Middle ear/hearing normal serous otitis without
subjective decrease in
hearing
serous otitis or infection
requiring medical
intervention; subjective
decrease in hearing;
rupture of tympanic
membrane with
discharge
otitis with discharge,
mastoiditis or
conductive hearing loss
necrosis of the canal
soft tissue or bone
Auditory/Hearing - Other
(Specify, __________)
normal mild moderate severe
life-threatening or
disabling
BLOOD/BONE MARROW
Bone marrow cellularity normal for age
mildly hypocellular or
≤25% reduction from
normal cellularity for
age
moderately hypocellular
or >25 - ≤50%
reduction from normal
cellularity for age or >2
but <4 weeks to
recovery of normal
bone marrow cellularity
severely hypocellular or
>50 - ≤75% reduction
in cellularity for age or
4 - 6 weeks to recovery
of normal bone marrow
cellularity
aplasia or >6 weeks to
recovery of normal
bone marrow cellularity
Normal ranges:
children (
≤
18 years)
90% cellularity
average
younger adults (19-59)
60 - 70%
cellularity average
older adults (≥60 years)
50% cellularity
average
Note: Grade Bone marrow cellularity only for changes related to treatment not disease.
CD4 count WNL <LLN - 500/mm
3
200 - <500/mm
3
50 - <200/mm
3
<50/mm
3
Haptoglobin normal decreased - absent -
Hemoglobin (Hgb) WNL <LLN - 10.0 g/dL
<LLN - 100 g/L
<LLN - 6.2 mmol/L
8.0 - <10.0 g/dL
80 - <100 g/L
4.9 - <6.2 mmol/L
6.5 - <8.0 g/dL
65 - <80 g/L
4.0 - <4.9 mmol/L
<6.5 g/dL
<65 g/L
<4.0 mmol/L
For leukemia studies or bone
marrow infiltrative/
myelophthisic processes, if
specified in the protocol.
WNL 10 - <25% decrease
from pretreatment
25 - <50% decrease
from pretreatment
50 - <75% decrease
from pretreatment
≥75% decrease from
pretreatment
Hemolysis (e.g., immune
hemolytic anemia, drug-
related hemolysis, other)
none only laboratory
evidence of hemolysis
[e.g., direct antiglobulin
test (DAT, Coombs’)
schistocytes]
evidence of red cell
destruction and ≥2gm
decrease in hemoglobin,
no transfusion
requiring transfusion
and/or medical
intervention (e.g.,
steroids)
catastrophic
consequences of
hemolysis (e.g., renal
failure, hypotension,
bronchospasm,
emergency
splenectomy)
Also consider Haptoglobin, Hemoglobin.

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 3 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Grade
Adverse Event 0 1 2 3 4
Leukocytes (total WBC) WNL <LLN - 3.0 x 10
9
/L
<LLN - 3000/mm
3
≥2.0 - <3.0 x 10
9
/L
≥2000 - <3000/mm
3
≥1.0 - <2.0 x 10
9
/L
≥1000 - <2000/mm
3
<1.0 x 10
9
/L
<1000/mm
3
For BMT studies, if
specified in the protocol.
WNL
≥2.0 - <3.0 X 10
9
/L
≥2000 - <3000/mm
3
≥1.0 - <2.0 x 10
9
/L
≥1000 - <2000/mm
3
≥0.5 - <1.0 x 10
9
/L
≥500 - <1000/mm
3
<0.5 x 10
9
/L
<500/mm
3
For pediatric BMT studies
(using age, race and sex
normal values), if specified
in the protocol.
≥
75 - <100% LLN
≥
50 - <75% LLN
≥
25 - 50% LLN
<25% LLN
Lymphopenia WNL
<LLN - 1.0 x 10
9
/L
<LLN - 1000/mm
3
≥0.5 - <1.0 x 10
9
/L
≥500 - <1000/mm
3
<0.5 x 10
9
/L
<500/mm
3
-
For pediatric BMT studies
(using age, race and sex
normal values), if specified
in the protocol.
≥
75 - <100%LLN
≥
50 - <75%LLN
≥
25 - <50%LLN
<25%LLN
Neutrophils/granulocytes
(ANC/AGC)
WNL
≥1.5 - <2.0 x 10
9
/L
≥1500 - <2000/mm
3
≥1.0 - <1.5 x 10
9
/L
≥1000 - <1500/mm
3
≥0.5 - <1.0 x 10
9
/L
≥500 - <1000/mm
3
<0.5 x 10
9
/L
<500/mm
3
For BMT studies, if
specified in the protocol.
WNL
≥1.0 - <1.5 x 10
9
/L
≥1000 - <1500/mm
3
≥0.5 - <1.0 x 10
9
/L
≥500 - <1000/mm
3
≥0.1 - <0.5 x 10
9
/L
≥100 - <500/mm
3
<0.1 x 10
9
/L
<100/mm
3
For leukemia studies or bone
marrow infiltrative/
myelophthisic process, if
specified in the protocol.
WNL 10 - <25% decrease
from baseline
25 - <50% decrease
from baseline
50 - <75% decrease
from baseline
≥75% decrease from
baseline
Platelets WNL
<LLN - 75.0 x 10
9
/L
<LLN - 75,000/mm
3
≥50.0 - <75.0 x 10
9
/L
≥50,000 - <75,000/mm
3
≥10.0 - <50.0 x 10
9
/L
≥10,000 - <50,000/mm
3
<10.0 x 10
9
/L
<10,000/mm
3
For BMT studies, if
specified in the protocol.
WNL
≥50.0 - <75.0 x 10
9
/L
≥50,000 - <75,000/mm
3
≥20.0 - <50.0 x 10
9
/L
≥20,000 - <50,000/mm
3
≥10.0 - <20.0 x 10
9
/L
≥10,000 - <20,000/mm
3
<10.0 x 10
9
/L
<10,000/mm
3
For leukemia studies or bone
marrow infiltrative/
myelophthisic process, if
specified in the protocol.
WNL 10 - <25% decrease
from baseline
25 - <50% decrease
from baseline
50 - <75% decrease
from baseline
≥75% decrease from
baseline
Transfusion: Platelets none - - yes platelet transfusions and
other measures required
to improve platelet
increment; platelet
transfusion
refractoriness associated
with life-threatening
bleeding. (e.g., HLA or
cross matched platelet
transfusions)
For BMT studies, if
specified in the protocol.
none
1 platelet transfusion in
24 hours
2 platelet transfusions in
24 hours
≥3 platelet transfusions
in 24 hours
platelet transfusions and
other measures required
to improve platelet
increment; platelet
transfusion
refractoriness associated
with life-threatening
bleeding. (e.g., HLA or
cross matched platelet
transfusions)
Also consider Platelets.

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 4 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Grade
Adverse Event 0 1 2 3 4
Transfusion: pRBCs none - - yes -
For BMT studies, if
specified in the protocol.
none
≤2 u pRBC in 24 hours
elective or planned
3 u pRBC in 24 hours
elective or planned
≥4 u pRBC in 24 hours
hemorrhage or
hemolysis associated
with life-threatening
anemia; medical
intervention required to
improve hemoglobin
For pediatric BMT studies, if
specified in the protocol.
none
≤
15mL/kg in 24 hours
elective or planned
>15 -
≤
30mL/kg in 24
hours elective or
planned
>30mL/kg in 24 hours hemorrhage or
hemolysis associated
with life-threatening
anemia; medical
intervention required to
improve hemoglobin
Also consider Hemoglobin.
Blood/Bone Marrow - Other
(Specify, __________)
none mild moderate severe
life-threatening or
disabling
CARDIOVASCULAR (ARRHYTHMIA)
Conduction abnormality/
Atrioventricular heart block
none
asymptomatic, not
requiring treatment
(e.g., Mobitz type I
second-degree AV
block, Wenckebach)
symptomatic, but not
requiring treatment
symptomatic and
requiring treatment
(e.g., Mobitz type II
second-degree AV
block, third-degree AV
block)
life-threatening (e.g.,
arrhythmia associated
with CHF, hypotension,
syncope, shock)
Nodal/junctional
arrhythmia/dysrhythmia
none
asymptomatic, not
requiring treatment
symptomatic, but not
requiring treatment
symptomatic and
requiring treatment
life-threatening (e.g.,
arrhythmia associated
with CHF, hypotension,
syncope, shock)
Palpitations none present - - -
Note: Grade palpitations only in the absence of a documented arrhythmia.
Prolonged QTc interval
(QTc >0.48 seconds)
none
asymptomatic, not
requiring treatment
symptomatic, but not
requiring treatment
symptomatic and
requiring treatment
life-threatening (e.g.,
arrhythmia associated
with CHF, hypotension,
syncope, shock)
Sinus bradycardia none asymptomatic, not
requiring treatment
symptomatic, but not
requiring treatment
symptomatic and
requiring treatment
life-threatening (e.g.,
arrhythmia associated
with CHF, hypotension,
syncope, shock)
Sinus tachycardia none
asymptomatic, not
requiring treatment
symptomatic, but not
requiring treatment
symptomatic and
requiring treatment of
underlying cause
-
Supraventricular arrhythmias
(SVT/atrial fibrillation/
flutter)
none
asymptomatic, not
requiring treatment
symptomatic, but not
requiring treatment
symptomatic and
requiring treatment
life-threatening (e.g.,
arrhythmia associated
with CHF, hypotension,
syncope, shock)
Syncope (fainting) is graded in the NEUROLOGY category.
Vasovagal episode none -
present without loss of
consciousness
present with loss of
consciousness
-

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 5 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Grade
Adverse Event 0 1 2 3 4
Ventricular arrhythmia
(PVCs/bigeminy/trigeminy/
ventricular tachycardia)
none asymptomatic, not
requiring treatment
symptomatic, but not
requiring treatment
symptomatic and
requiring treatment
life-threatening (e.g.,
arrhythmia associated
with CHF, hypotension,
syncope, shock)
Cardiovascular/
Arrhythmia - Other
(Specify, ___________)
none asymptomatic, not
requiring treatment
symptomatic, but not
requiring treatment
symptomatic, and
requiring treatment of
underlying cause
life-threatening (e.g.,
arrhythmia associated
with CHF, hypotension,
syncope, shock)
CARDIOVASCULAR (GENERAL)
Acute vascular leak
syndrome
absent -
symptomatic, but not
requiring fluid support
respiratory compromise
or requiring fluids
life-threatening;
requiring pressor
support and/or
ventilatory support
Cardiac-ischemia/infarction none non-specific T - wave
flattening or changes
asymptomatic, ST - and
T - wave changes
suggesting ischemia
angina without evidence
of infarction
acute myocardial
infarction
Cardiac left ventricular
function
normal asymptomatic decline
of resting ejection
fraction of ≥10% but
<20% of baseline value;
shortening fraction
≥24% but <30%
asymptomatic but
resting ejection fraction
below LLN for
laboratory or decline of
resting ejection fraction
≥20% of baseline value;
<24% shortening
fraction
CHF responsive to
treatment
severe or refractory
CHF or requiring
intubation
CNS cerebrovascular ischemia is graded in the NEUROLOGY category.
Cardiac troponin I (cTnI) normal - - levels consistent with
unstable angina as
defined by the
manufacturer
levels consistent with
myocardial infarction as
defined by the
manufacturer
Cardiac troponin T (cTnT) normal
≥0.03 - <0.05 ng/mL ≥0.05 - <0.1 ng/mL ≥0.1 - <0.2 ng/mL ≥0.2 ng/mL
Edema none asymptomatic, not
requiring therapy
symptomatic, requiring
therapy
symptomatic edema
limiting function and
unresponsive to therapy
or requiring drug
discontinuation
anasarca (severe
generalized edema)
Hypertension none asymptomatic, transient
increase by >20 mmHg
(diastolic) or to
>150/100* if previously
WNL; not requiring
treatment
recurrent or persistent
or symptomatic increase
by >20 mmHg
(diastolic) or to
>150/100* if previously
WNL; not requiring
treatment
requiring therapy or
more intensive therapy
than previously
hypertensive crisis
*Note: For pediatric patients, use age and sex appropriate normal values >95th percentile ULN.

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 6 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Grade
Adverse Event 0 1 2 3 4
Hypotension none changes, but not
requiring therapy
(including transient
orthostatic hypotension)
requiring brief fluid
replacement or other
therapy but not
hospitalization; no
physiologic
consequences
requiring therapy and
sustained medical
attention, but resolves
without persisting
physiologic
consequences
shock (associated with
acidemia and impairing
vital organ function due
to tissue hypoperfusion)
Also consider Syncope (fainting).
Notes: Angina or MI is graded as Cardiac-ischemia/infarction in the CARDIOVASCULAR (GENERAL) category.
For pediatric patients, systolic BP 65 mmHg or less in infants up to 1 year old and 70 mmHg or less in children older than 1 year of age, use two successive
or three measurements in 24 hours.
Myocarditis none - - CHF responsive to
treatment
severe or refractory
CHF
Operative injury of
vein/artery
none primary suture repair
for injury, but not
requiring transfusion
primary suture repair
for injury, requiring
transfusion
vascular occlusion
requiring surgery or
bypass for injury
myocardial infarction;
resection of organ (e.g.,
bowel, limb)
Pericardial effusion/
pericarditis
none asymptomatic effusion,
not requiring treatment
pericarditis (rub, ECG
changes, and/or chest
pain)
with physiologic
consequences
tamponade (drainage or
pericardial window
required)
Peripheral arterial ischemia none - brief episode of
ischemia managed non-
surgically and without
permanent deficit
requiring surgical
intervention
life-threatening or with
permanent functional
deficit (e.g.,
amputation)
Phlebitis (superficial) none - present - -
Notes: Injection site reaction is graded in the DERMATOLOGY/SKIN category.
Thrombosis/embolism is graded in the CARDIOVASCULAR (GENERAL) category.
Syncope (fainting) is graded in the NEUROLOGY category.
Thrombosis/embolism none - deep vein thrombosis,
not requiring
anticoagulant
deep vein thrombosis,
requiring anticoagulant
therapy
embolic event including
pulmonary embolism
Vein/artery operative injury is graded as Operative injury of vein/artery in the CARDIOVASCULAR (GENERAL) category.
Visceral arterial ischemia
(non-myocardial)
none -
brief episode of
ischemia managed non-
surgically and without
permanent deficit
requiring surgical
intervention
life-threatening or with
permanent functional
deficit (e.g., resection of
ileum)
Cardiovascular/
General - Other
(Specify, ______________)
none mild moderate severe life-threatening or
disabling

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 7 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Grade
Adverse Event 0 1 2 3 4
COAGULATION
Note: See the HEMORRHAGE category for grading the severity of bleeding events.
DIC
(disseminated intravascular
coagulation)
absent - -
laboratory findings
present with no
bleeding
laboratory findings and
bleeding
Also consider Platelets.
Note: Must have increased fibrin split products or D-dimer in order to grade as DIC.
Fibrinogen WNL
≥0.75 - <1.0 x LLN ≥0.5 - <0.75 x LLN ≥0.25 - <0.5 x LLN
<0.25 x LLN
For leukemia studies or bone
marrow infiltrative/
myelophthisic process, if
specified in the protocol.
WNL <20% decrease from
pretreatment value or
LLN
≥20 - <40% decrease
from pretreatment value
or LLN
≥40 - <70% decrease
from pretreatment value
or LLN
<50 mg
Partial thromboplastin time
(PTT)
WNL
>ULN - ≤1.5 x ULN >1.5 - ≤2 x ULN
>2 x ULN -
Phlebitis is graded in the CARDIOVASCULAR (GENERAL) category.
Prothrombin time (PT) WNL
>ULN - ≤1.5 x ULN >1.5 - ≤2 x ULN
>2 x ULN -
Thrombosis/embolism is graded in the CARDIOVASCULAR (GENERAL) category.
Thrombotic
microangiopathy (e.g.,
thrombotic
thrombocytopenic
purpura/TTP or hemolytic
uremic syndrome/HUS)
absent - - laboratory findings
present without clinical
consequences
laboratory findings and
clinical consequences,
(e.g., CNS hemorrhage/
bleeding or thrombosis/
embolism or renal
failure) requiring
therapeutic intervention
For BMT studies, if
specified in the protocol.
- evidence of RBC
destruction
(schistocytosis) without
clinical consequences
evidence of RBC
destruction with
elevated creatinine (≤3
x ULN)
evidence of RBC
destruction with
creatinine (>3 x ULN)
not requiring dialysis
evidence of RBC
destruction with renal
failure requiring
dialysis and/or
encephalopathy
Also consider Hemoglobin, Platelets, Creatinine.
Note: Must have microangiopathic changes on blood smear (e.g., schistocytes, helmet cells, red cell fragments).
Coagulation - Other
(Specify, __________)
none mild moderate severe
life-threatening or
disabling
CONSTITUTIONAL SYMPTOMS
Fatigue
(lethargy, malaise, asthenia)
none
increased fatigue over
baseline, but not
altering normal
activities
moderate (e.g., decrease
in performance status
by 1 ECOG level or
20% Karnofsky or
Lansky) or causing
difficulty performing
some activities
severe (e.g., decrease in
performance status by
≥2 ECOG levels or 40%
Karnofsky or Lansky) or
loss of ability to
perform some activities
bedridden or disabling
Note: See Appendix III for performance status scales.

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 8 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Grade
Adverse Event 0 1 2 3 4
Fever (in the absence of
neutropenia, where
neutropenia is defined as
AGC <1.0 x 10
9
/L)
none 38.0 - 39.0°C (100.4 -
102.2°F)
39.1 - 40.0°C (102.3 -
104.0°F )
>40.0°C (>104.0°F ) for
<24hrs
>40.0°C (>104.0°F ) for
>24hrs
Also consider Allergic reaction/hypersensitivity.
Note: The temperature measurements listed above are oral or tympanic.
Hot flashes/flushes are graded in the ENDOCRINE category.
Rigors, chills none
mild, requiring
symptomatic treatment
(e.g., blanket) or non-
narcotic medication
severe and/or
prolonged, requiring
narcotic medication
not responsive to
narcotic medication
-
Sweating
(diaphoresis)
normal mild and occasional frequent or drenching - -
Weight gain <5% 5 - <10% 10 - <20%
≥20%
-
Also consider Ascites, Edema, Pleural effusion (non-malignant).
Weight gain associated with
Veno-Occlusive Disease
(VOD) for BMT studies, if
specified in the protocol.
<2%
≥2 - <5% ≥5 - <10% ≥10% or as ascites ≥10% or fluid retention
resulting in pulmonary
failure
Also consider Ascites, Edema, Pleural effusion (non-malignant).
Weight loss <5% 5 - <10% 10 - <20%
≥20%
-
Also consider Vomiting, Dehydration, Diarrhea.
Constitutional Symptoms -
Other
(Specify, __________)
none mild moderate severe
life-threatening or
disabling
DERMATOLOGY/SKIN
Alopecia normal mild hair loss pronounced hair loss - -
Bruising
(in absence of grade 3 or 4
thrombocytopenia)
none localized or in
dependent area
generalized - -
Note: Bruising resulting from grade 3 or 4 thrombocytopenia is graded as Petechiae/purpura and Hemorrhage/bleeding with grade 3 or 4 thrombocytopenia in the
HEMORRHAGE category, not in the DERMATOLOGY/SKIN category.
Dry skin normal controlled with
emollients
not controlled with
emollients
--
Erythema multiforme (e.g.,
Stevens-Johnson syndrome,
toxic epidermal necrolysis)
absent -
scattered, but not
generalized eruption
severe or requiring IV
fluids (e.g., generalized
rash or painful
stomatitis)
life-threatening (e.g.,
exfoliative or ulcerating
dermatitis or requiring
enteral or parenteral
nutritional support)
Flushing absent present - - -
Hand-foot skin reaction none skin changes or
dermatitis without pain
(e.g., erythema, peeling)
skin changes with pain,
not interfering with
function
skin changes with pain,
interfering with
function
-
Injection site reaction none pain or itching or
erythema
pain or swelling, with
inflammation or
phlebitis
ulceration or necrosis
that is severe or
prolonged, or requiring
surgery
-

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 9 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Grade
Adverse Event 0 1 2 3 4
Nail changes normal discoloration or ridging
(koilonychia) or pitting
partial or complete loss
of nail(s) or pain in
nailbeds
--
Petechiae is graded in the HEMORRHAGE category.
Photosensitivity none painless erythema painful erythema
erythema with
desquamation
-
Pigmentation changes (e.g.,
vitiligo)
none localized pigmentation
changes
generalized
pigmentation changes
--
Pruritus none mild or localized,
relieved spontaneously
or by local measures
intense or widespread,
relieved spontaneously
or by systemic measures
intense or widespread
and poorly controlled
despite treatment
-
Purpura is graded in the HEMORRHAGE category.
Radiation dermatitis none
faint erythema or dry
desquamation
moderate to brisk
erythema or a patchy
moist desquamation,
mostly confined to skin
folds and creases;
moderate edema
confluent moist
desquamation ≥1.5 cm
diameter and not
confined to skin folds;
pitting edema
skin necrosis or
ulceration of full
thickness dermis; may
include bleeding not
induced by minor
trauma or abrasion
Note: Pain associated with radiation dermatitis is graded separately in the PAIN category as Pain due to radiation.
Radiation recall reaction
(reaction following
chemotherapy in the absence
of additional radiation
therapy that occurs in a
previous radiation port)
none
faint erythema or dry
desquamation
moderate to brisk
erythema or a patchy
moist desquamation,
mostly confined to skin
folds and creases;
moderate edema
confluent moist
desquamation ≥1.5 cm
diameter and not
confined to skin folds;
pitting edema
skin necrosis or
ulceration of full
thickness dermis; may
include bleeding not
induced by minor
trauma or abrasion
Rash/desquamation none
macular or papular
eruption or erythema
without associated
symptoms
macular or papular
eruption or erythema
with pruritus or other
associated symptoms
covering <50% of body
surface or localized
desquamation or other
lesions covering <50%
of body surface area
symptomatic
generalized
erythroderma or
macular, papular or
vesicular eruption or
desquamation covering
≥50% of body surface
area
generalized exfoliative
dermatitis or ulcerative
dermatitis
Also consider Allergic reaction/hypersensitivity.
Note: Stevens-Johnson syndrome is graded separately as Erythema multiforme in the DERMATOLOGY/SKIN category.
Rash/dermatitis associated
with high-dose
chemotherapy or BMT
studies.
none
faint erythema or dry
desquamation
moderate to brisk
erythema or a patchy
moist desquamation,
mostly confined to skin
folds and creases;
moderate edema
confluent moist
desquamation ≥1.5 cm
diameter and not
confined to skin folds;
pitting edema
skin necrosis or ulcera-
tion of full thickness
dermis; may include
spontaneous bleeding
not induced by minor
trauma or abrasion
Rash/desquamation
associated with graft versus
host disease (GVHD) for
BMT studies, if specified in
the protocol.
None
macular or papular
eruption or erythema
covering <25% of body
surface area without
associated symptoms
macular or papular
eruption or erythema
with pruritus or other
associated symptoms
covering ≥25 - <50% of
body surface or
localized desquamation
or other lesions
covering ≥25 - <50% of
body surface area
symptomatic
generalized
erythroderma or
symptomatic macular,
papular or vesicular
eruption, with bullous
formation, or
desquamation covering
≥50% of body surface
area
generalized exfoliative
dermatitis or ulcerative
dermatitis or bullous
formation
Also consider Allergic reaction/hypersensitivity.
Note: Stevens-Johnson syndrome is graded separately as Erythema multiforme in the DERMATOLOGY/SKIN category.

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 10 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Grade
Adverse Event 0 1 2 3 4
Urticaria
(hives, welts, wheals)
none requiring no medication requiring PO or topical
treatment or IV
medication or steroids
for <24 hours
requiring IV medication
or steroids for ≥24
hours
-
Wound-infectious none cellulitis superficial infection infection requiring IV
antibiotics
necrotizing fasciitis
Wound-non-infectious none incisional separation incisional hernia fascial disruption
without evisceration
fascial disruption with
evisceration
Dermatology/Skin - Other
(Specify, ________)
none mild moderate severe
life-threatening or
disabling
ENDOCRINE
Cushingoid appearance (e.g.,
moon face, buffalo hump,
centripetal obesity,
cutaneous striae)
absent - present - -
Also consider Hyperglycemia, Hypokalemia.
Feminization of male absent - - present -
Gynecomastia none mild pronounced or painful
pronounced or painful
and requiring surgery
-
Hot flashes/flushes none
mild or no more than 1
per day
moderate and greater
than 1 per day
--
Hypothyroidism absent asymptomatic,TSH
elevated, no therapy
given
symptomatic or thyroid
replacement treatment
given
patient hospitalized for
manifestations of
hypothyroidism
myxedema coma
Masculinization of female absent - - present -
SIADH (syndrome of
inappropriate antidiuretic
hormone)
absent - - present -
Endocrine - Other
(Specify, __________)
none mild moderate severe
life-threatening or
disabling
GASTROINTESTINAL
Amylase is graded in the METABOLIC/LABORATORY category.
Anorexia none loss of appetite oral intake significantly
decreased
requiring IV fluids requiring feeding tube
or parenteral nutrition
Ascites (non-malignant) none asymptomatic
symptomatic, requiring
diuretics
symptomatic, requiring
therapeutic paracentesis
life-threatening
physiologic
consequences
Colitis none - abdominal pain with
mucus and/or blood in
stool
abdominal pain, fever,
change in bowel habits
with ileus or peritoneal
signs, and radiographic
or biopsy
documentation
perforation or requiring
surgery or toxic
megacolon
Also consider Hemorrhage/bleeding with grade 3 or 4 thrombocytopenia, Hemorrhage/bleeding without grade 3 or 4 thrombocytopenia, Melena/GI bleeding,
Rectal bleeding/hematochezia, Hypotension.
Constipation none
requiring stool softener
or dietary modification
requiring laxatives
obstipation requiring
manual evacuation or
enema
obstruction or toxic
megacolon

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 11 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Grade
Adverse Event 0 1 2 3 4
Dehydration none dry mucous membranes
and/or diminished skin
turgor
requiring IV fluid
replacement (brief)
requiring IV fluid
replacement (sustained)
physiologic
consequences requiring
intensive care;
hemodynamic collapse
Also consider Diarrhea, Vomiting, Stomatitis/pharyngitis (oral/pharyngeal mucositis), Hypotension.
Diarrhea
patients without colostomy:
none
increase of <4
stools/day over pre-
treatment
increase of 4-6
stools/day, or nocturnal
stools
increase of ≥7
stools/day or
incontinence; or need
for parenteral support
for dehydration
physiologic
consequences requiring
intensive care; or
hemodynamic collapse
patients with a colostomy: none mild increase in loose,
watery colostomy
output compared with
pretreatment
moderate increase in
loose, watery colostomy
output compared with
pretreatment, but not
interfering with normal
activity
severe increase in loose,
watery colostomy
output compared with
pretreatment, interfering
with normal activity
physiologic
consequences, requiring
intensive care; or
hemodynamic collapse
Diarrhea associated with
graft versus host disease
(GVHD) for BMT studies, if
specified in the protocol.
None
>500 - ≤1000mL of
diarrhea/day
>1000 - ≤1500mL of
diarrhea/day
>1500mL of
diarrhea/day
severe abdominal pain
with or without ileus
For pediatric BMT studies, if
specified in the protocol.
>5 -
≤
10 mL/kg of
diarrhea/day
>10 -
≤
15 mL/kg of
diarrhea/day
>15 mL/kg of
diarrhea/day
-
Also consider Hemorrhage/bleeding with grade 3 or 4 thrombocytopenia, Hemorrhage/bleeding without grade 3 or 4 thrombocytopenia, Pain, Dehydration,
Hypotension.
Duodenal ulcer (requires
radiographic or endoscopic
documentation)
none - requiring medical
management or non-
surgical treatment
uncontrolled by
outpatient medical
management; requiring
hospitalization
perforation or bleeding,
requiring emergency
surgery
Dyspepsia/heartburn none mild moderate severe -
Dysphagia, esophagitis,
odynophagia (painful
swallowing)
none
mild dysphagia, but can
eat regular diet
dysphagia, requiring
predominantly pureed,
soft, or liquid diet
dysphagia, requiring IV
hydration
complete obstruction
(cannot swallow saliva)
requiring enteral or
parenteral nutritional
support, or perforation
Note: If the adverse event is radiation-related, grade either under Dysphagia-esophageal related to radiation or Dysphagia-pharyngeal related to radiation.
Dysphagia-esophageal
related to radiation
none mild dysphagia, but can
eat regular diet
dysphagia, requiring
predominantly pureed,
soft, or liquid diet
Dysphagia, requiring
feeding tube, IV
hydration or
hyperalimentation
complete obstruction
(cannot swallow saliva);
ulceration with bleeding
not induced by minor
trauma or abrasion or
perforation
Also consider Pain due to radiation, Mucositis due to radiation.
Note: Fistula is graded separately as Fistula-esophageal.
Dysphagia-pharyngeal
related to radiation
none
mild dysphagia, but can
eat regular diet
dysphagia, requiring
predominantly pureed,
soft, or liquid diet
dysphagia, requiring
feeding tube, IV
hydration or
hyperalimentation
complete obstruction
(cannot swallow saliva);
ulceration with bleeding
not induced by minor
trauma or abrasion or
perforation
Also consider Pain due to radiation, Mucositis due to radiation.
Note: Fistula is graded separately as Fistula-pharyngeal.
Fistula-esophageal none - - present requiring surgery
Fistula-intestinal none - - present requiring surgery

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 12 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Grade
Adverse Event 0 1 2 3 4
Fistula-pharyngeal none - - present requiring surgery
Fistula-rectal/anal none - - present requiring surgery
Flatulence none mild moderate - -
Gastric ulcer
(requires radiographic or
endoscopic documentation)
none - requiring medical
management or non-
surgical treatment
bleeding without
perforation, uncon-
trolled by outpatient
medical management;
requiring hospitalization
or surgery
perforation or bleeding,
requiring emergency
surgery
Also consider Hemorrhage/bleeding with grade 3 or 4 thrombocytopenia, Hemorrhage/bleeding without grade 3 or 4 thrombocytopenia.
Gastritis none -
requiring medical
management or non-
surgical treatment
uncontrolled by out-
patient medical
management; requiring
hospitalization or
surgery
life-threatening
bleeding, requiring
emergency surgery
Also consider Hemorrhage/bleeding with grade 3 or 4 thrombocytopenia, Hemorrhage/bleeding without grade 3 or 4 thrombocytopenia.
Hematemesis is graded in the HEMORRHAGE category.
Hematochezia is graded in the HEMORRHAGE category as Rectal bleeding/hematochezia.
Ileus (or neuroconstipation) none -
intermittent, not
requiring intervention
requiring non-surgical
intervention
requiring surgery
Mouth dryness normal mild moderate - -
Mucositis
Notes: Mucositis not due to radiation is graded in the GASTROINTESTINAL category for specific sites: Colitis, Esophagitis, Gastritis, Stomatitis/pharyngitis
(oral/pharyngeal mucositis), and Typhlitis; or the RENAL/GENITOURINARY category for Vaginitis.
Radiation-related mucositis is graded as Mucositis due to radiation.
Mucositis due to radiation none erythema of the mucosa patchy pseudomembra-
nous reaction (patches
generally ≤1.5 cm in
diameter and non-
contiguous)
confluent pseudomem-
branous reaction
(contiguous patches
generally >1.5 cm in
diameter)
necrosis or deep
ulceration; may include
bleeding not induced by
minor trauma or
abrasion
Also consider Pain due to radiation.
Notes: Grade radiation mucositis of the larynx here.
Dysphagia related to radiation is also graded as either Dysphagia-esophageal related to radiation or Dysphagia-pharyngeal related to radiation, depending on
the site of treatment.
Nausea none able to eat
oral intake significantly
decreased
no significant intake,
requiring IV fluids
-
Pancreatitis none - - abdominal pain with
pancreatic enzyme
elevation
complicated by shock
(acute circulatory
failure)
Also consider Hypotension.
Note: Amylase is graded in the METABOLIC/LABORATORY category.
Pharyngitis is graded in the GASTROINTESTINAL category as Stomatitis/pharyngitis (oral/pharyngeal mucositis).

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 13 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Grade
Adverse Event 0 1 2 3 4
Proctitis none increased stool
frequency, occasional
blood-streaked stools or
rectal discomfort
(including hemorrhoids)
not requiring
medication
increased stool
frequency, bleeding,
mucus discharge, or
rectal discomfort
requiring medication;
anal fissure
increased stool fre-
quency/diarrhea requir-
ing parenteral support;
rectal bleeding requir-
ing transfusion; or per-
sistent mucus discharge,
necessitating pads
perforation, bleeding or
necrosis or other life-
threatening
complication requiring
surgical intervention
(e.g., colostomy)
Also consider Hemorrhage/bleeding with grade 3 or 4 thrombocytopenia, Hemorrhage/bleeding without grade 3 or 4 thrombocytopenia, Pain due to radiation.
Notes: Fistula is graded separately as Fistula-rectal/anal.
Proctitis occurring more than 90 days after the start of radiation therapy is graded in the RTOG/EORTC Late Radiation Morbidity Scoring Scheme. (See
Appendix IV)
Salivary gland changes none
slightly thickened
saliva; may have
slightly altered taste
(e.g., metallic);
additional fluids may be
required
thick, ropy, sticky
saliva; markedly altered
taste; alteration in diet
required
-
acute salivary gland
necrosis
Sense of smell normal slightly altered markedly altered - -
Stomatitis/pharyngitis
(oral/pharyngeal mucositis)
none painless ulcers,
erythema, or mild
soreness in the absence
of lesions
painful erythema,
edema, or ulcers, but
can eat or swallow
painful erythema,
edema, or ulcers
requiring IV hydration
severe ulceration or
requires parenteral or
enteral nutritional
support or prophylactic
intubation
For BMT studies, if
specified in the protocol.
none painless ulcers,
erythema, or mild
soreness in the absence
of lesions
painful erythema,
edema or ulcers but can
swallow
painful erythema,
edema, or ulcers
preventing swallowing
or requiring hydration
or parenteral (or enteral)
nutritional support
severe ulceration
requiring prophylactic
intubation or resulting
in documented
aspiration pneumonia
Note: Radiation-related mucositis is graded as Mucositis due to radiation.
Taste disturbance
(dysgeusia)
normal slightly altered markedly altered - -
Typhlitis
(inflammation of the cecum)
none - - abdominal pain,
diarrhea, fever, and
radiographic or biopsy
documentation
perforation, bleeding or
necrosis or other life-
threatening
complication requiring
surgical intervention
(e.g., colostomy)
Also consider Hemorrhage/bleeding with grade 3 or 4 thrombocytopenia, Hemorrhage/bleeding without grade 3 or 4 thrombocytopenia, Hypotension, Febrile
neutropenia.
Vomiting none
1 episode in 24 hours
over pretreatment
2-5 episodes in 24 hours
over pretreatment
≥6 episodes in 24 hours
over pretreatment; or
need for IV fluids
requiring parenteral
nutrition; or physiologic
consequences requiring
intensive care;
hemodynamic collapse
Also consider Dehydration.
Weight gain is graded in the CONSTITUTIONAL SYMPTOMS category.
Weight loss is graded in the CONSTITUTIONAL SYMPTOMS category.
Gastrointestinal - Other
(Specify, __________)
none mild moderate severe
life-threatening or
disabling

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 14 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Grade
Adverse Event 0 1 2 3 4
HEMORRHAGE
Notes: Transfusion in this section refers to pRBC infusion.
For any bleeding with grade 3 or 4 platelets (<50,000), always grade Hemorrhage/bleeding with grade 3 or 4 thrombocytopenia. Also consider Platelets,
Transfusion: pRBCs, and Transfusion: platelets in addition to grading severity by grading the site or type of bleeding.
If the site or type of Hemorrhage/bleeding is listed, also use the grading that incorporates the site of bleeding: CNS Hemorrhage/bleeding, Hematuria,
Hematemesis, Hemoptysis, Hemorrhage/bleeding with surgery, Melena/lower GI bleeding, Petechiae/purpura (Hemorrhage/bleeding into skin), Rectal
bleeding/hematochezia, Vaginal bleeding.
If the platelet count is ≥50,000 and the site or type of bleeding is listed, grade the specific site. If the site or type is not listed and the platelet count is
≥50,000, grade Hemorrhage/bleeding without grade 3 or 4 thrombocytopenia and specify the site or type in the OTHER category.
Hemorrhage/bleeding with
grade 3 or 4
thrombocytopenia
none mild without
transfusion
requiring transfusion catastrophic bleeding,
requiring major non-
elective intervention
Also consider Platelets, Hemoglobin, Transfusion: platelets, Transfusion: pRBCs, site or type of bleeding. If the site is not listed, grade as Hemorrhage-Other
(Specify site, ___________).
Note: This adverse event must be graded for any bleeding with grade 3 or 4 thrombocytopenia.
Hemorrhage/bleeding
without grade 3 or 4
thrombocytopenia
none mild without
transfusion
requiring transfusion catastrophic bleeding
requiring major non-
elective intervention
Also consider Platelets, Hemoglobin, Transfusion: platelets, Transfusion: pRBCs, Hemorrhage - Other (Specify site, ___________).
Note: Bleeding in the absence of grade 3 or 4 thrombocytopenia is graded here only if the specific site or type of bleeding is not listed elsewhere in the
HEMORRHAGE category. Also grade as Other in the HEMORRHAGE category.
CNS hemorrhage/bleeding none - - bleeding noted on CT or
other scan with no
clinical consequences
hemorrhagic stroke or
hemorrhagic vascular
event (CVA) with
neurologic signs and
symptoms
Epistaxis none mild without
transfusion
- requiring transfusion catastrophic bleeding,
requiring major non-
elective intervention
Hematemesis none mild without
transfusion
- requiring transfusion catastrophic bleeding,
requiring major non-
elective intervention
Hematuria
(in the absence of vaginal
bleeding)
none microscopic only intermittent gross
bleeding, no clots
persistent gross
bleeding or clots; may
require catheterization
or instrumentation, or
transfusion
open surgery or necrosis
or deep bladder
ulceration
Hemoptysis none
mild without
transfusion
- requiring transfusion
catastrophic bleeding,
requiring major non-
elective intervention
Hemorrhage/bleeding
associated with surgery
none mild without
transfusion
- requiring transfusion catastrophic bleeding,
requiring major non-
elective intervention
Note: Expected blood loss at the time of surgery is not graded as an adverse event.
Melena/GI bleeding none mild without
transfusion
- requiring transfusion catastrophic bleeding,
requiring major non-
elective intervention

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 15 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Grade
Adverse Event 0 1 2 3 4
Petechiae/purpura
(hemorrhage/bleeding into
skin or mucosa)
none rare petechiae of skin petechiae or purpura in
dependent areas of skin
generalized petechiae or
purpura of skin or
petechiae of any
mucosal site
-
Rectal bleeding/
hematochezia
none mild without
transfusion or
medication
persistent, requiring
medication (e.g., steroid
suppositories) and/or
break from radiation
treatment
requiring transfusion catastrophic bleeding,
requiring major non-
elective intervention
Vaginal bleeding none spotting, requiring <2
pads per day
requiring ≥2 pads per
day, but not requiring
transfusion
requiring transfusion catastrophic bleeding,
requiring major non-
elective intervention
Hemorrhage - Other
(Specify site, ___________)
none
mild without
transfusion
- requiring transfusion
catastrophic bleeding,
requiring major non-
elective intervention
HEPATIC
Alkaline phosphatase WNL >ULN - 2.5 x ULN >2.5 - 5.0 x ULN >5.0 - 20.0 x ULN >20.0 x ULN
Bilirubin WNL >ULN - 1.5 x ULN >1.5 - 3.0 x ULN >3.0 - 10.0 x ULN >10.0 x ULN
Bilirubin associated with
graft versus host disease
(GVHD) for BMT studies, if
specified in the protocol.
normal
≥2 - <3 mg/100 mL ≥3 - <6 mg/100 mL ≥6 - <15 mg/100 mL ≥15 mg/100 mL
GGT
(γ - Glutamyl transpeptidase)
WNL >ULN - 2.5 x ULN >2.5 - 5.0 x ULN >5.0 - 20.0 x ULN >20.0 x ULN
Hepatic enlargement absent - - present -
Note: Grade Hepatic enlargement only for treatment related adverse event including Veno-Occlusive Disease.
Hypoalbuminemia WNL <LLN - 3 g/dL
≥2 - <3 g/dL
<2 g/dL -
Liver dysfunction/ failure
(clinical)
normal - - asterixis encephalopathy or coma
Portal vein flow normal -
decreased portal vein
flow
reversal/retrograde
portal vein flow
-
SGOT (AST)
(serum glutamic oxaloacetic
transaminase)
WNL >ULN - 2.5 x ULN >2.5 - 5.0 x ULN >5.0 - 20.0 x ULN >20.0 x ULN
SGPT (ALT)
(serum glutamic pyruvic
transaminase)
WNL >ULN - 2.5 x ULN >2.5 - 5.0 x ULN >5.0 - 20.0 x ULN >20.0 x ULN
Hepatic - Other
(Specify, __________)
none mild moderate severe
life-threatening or
disabling
INFECTION/FEBRILE NEUTROPENIA
Catheter-related infection none mild, no active
treatment
moderate, localized
infection, requiring
local or oral treatment
severe, systemic
infection, requiring IV
antibiotic or antifungal
treatment or
hospitalization
life-threatening sepsis
(e.g., septic shock)

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 16 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Grade
Adverse Event 0 1 2 3 4
Febrile neutropenia
(fever of unknown origin
without clinically or
microbiologically
documented infection)
none - - Present Life-threatening sepsis
(e.g., septic shock)
(ANC <1.0 x 10
9
/L, fever
≥38.5°C)
Also consider Neutrophils.
Note: Hypothermia instead of fever may be associated with neutropenia and is graded here.
Infection (documented
clinically or
microbiologically) with
grade 3 or 4 neutropenia
none - - present
life-threatening sepsis
(e.g., septic shock)
(ANC <1.0 x 10
9
/L)
Also consider Neutrophils.
Notes: Hypothermia instead of fever may be associated with neutropenia and is graded here.
In the absence of documented infection grade 3 or 4 neutropenia with fever is graded as Febrile neutropenia.
Infection with unknown
ANC
none - - present life-threatening sepsis
(e.g., septic shock)
Note: This adverse event criterion is used in the rare case when ANC is unknown.
Infection without
neutropenia
none mild, no active
treatment
moderate, localized
infection, requiring
local or oral treatment
severe, systemic
infection, requiring IV
antibiotic or antifungal
treatment, or
hospitalization
life-threatening sepsis
(e.g., septic shock)
Also consider Neutrophils.
Wound-infectious is graded in the DERMATOLOGY/SKIN category.
Infection/Febrile
Neutropenia - Other
(Specify, __________)
none mild moderate severe
life-threatening or
disabling
LYMPHATICS
Lymphatics normal mild lymphedema moderate lymphedema
requiring compression;
lymphocyst
severe lymphedema
limiting function;
lymphocyst requiring
surgery
severe lymphedema
limiting function with
ulceration
Lymphatics - Other
(Specify, __________)
none mild moderate severe life-threatening or
disabling
METABOLIC/LABORATORY
Acidosis
(metabolic or respiratory)
normal
pH <normal, but ≥7.3
- pH <7.3 pH <7.3 with life-
threatening physiologic
consequences
Alkalosis
(metabolic or respiratory)
normal
pH >normal, but ≤7.5
- pH >7.5 pH >7.5 with life-
threatening physiologic
consequences
Amylase WNL >ULN - 1.5 x ULN >1.5 - 2.0 x ULN >2.0 - 5.0 x ULN >5.0 x ULN
Bicarbonate WNL <LLN - 16 mEq/dL 11 - 15 mEq/dL 8 - 10 mEq/dL <8 mEq/dL

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 17 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Grade
Adverse Event 0 1 2 3 4
CPK
(creatine phosphokinase)
WNL >ULN - 2.5 x ULN >2.5 - 5 x ULN >5 - 10 x ULN >10 x ULN
Hypercalcemia WNL
>ULN - 11.5 mg/dL
>ULN - 2.9 mmol/L
>11.5 - 12.5 mg/dL
>2.9 - 3.1 mmol/L
>12.5 - 13.5 mg/dL
>3.1 - 3.4 mmol/L
>13.5 mg/dL
>3.4 mmol/L
Hypercholesterolemia WNL
>ULN - 300 mg/dL
>ULN - 7.75 mmol/L
>300 - 400 mg/dL
>7.75 - 10.34 mmol/L
>400 - 500 mg/dL
>10.34 - 12.92 mmol/L
>500 mg/dL
>12.92 mmol/L
Hyperglycemia WNL >ULN - 160 mg/dL
>ULN - 8.9 mmol/L
>160 - 250 mg/dL
>8.9 - 13.9 mmol/L
>250 - 500 mg/dL
>13.9 - 27.8 mmol/L
>500 mg/dL
>27.8 mmol/L or
acidosis
Hyperkalemia WNL >ULN - 5.5 mmol/L >5.5 - 6.0 mmol/L >6.0 - 7.0 mmol/L >7.0 mmol/L
Hypermagnesemia WNL
>ULN - 3.0 mg/dL
>ULN - 1.23 mmol/L
-
>3.0 - 8.0 mg/dL
>1.23 - 3.30 mmol/L
>8.0 mg/dL
>3.30 mmol/L
Hypernatremia WNL >ULN - 150 mmol/L >150 - 155 mmol/L >155 - 160 mmol/L >160 mmol/L
Hypertriglyceridemia WNL >ULN - 2.5 x ULN >2.5 - 5.0 x ULN >5.0 - 10 x ULN >10 x ULN
Hyperuricemia WNL
>ULN - ≤10 mg/dL
≤0.59 mmol/L without
physiologic
consequences
-
>ULN - ≤10 mg/dL
≤0.59 mmol/L with
physiologic
consequences
>10 mg/dL
>0.59 mmol/L
Also consider Tumor lysis syndrome, Renal failure, Creatinine, Hyperkalemia.
Hypocalcemia WNL <LLN - 8.0 mg/dL
<LLN - 2.0 mmol/L
7.0 - <8.0 mg/dL
1.75 - <2.0 mmol/L
6.0 - <7.0 mg/dL
1.5 - <1.75 mmol/L
<6.0 mg/dL
<1.5 mmol/L
Hypoglycemia WNL
<LLN - 55 mg/dL
<LLN - 3.0 mmol/L
40 - <55 mg/dL
2.2 - <3.0 mmol/L
30 - <40 mg/dL
1.7 - <2.2 mmol/L
<30 mg/dL
<1.7 mmol/L
Hypokalemia WNL <LLN - 3.0 mmol/L - 2.5 - <3.0 mmol/L <2.5 mmol/L
Hypomagnesemia WNL <LLN - 1.2 mg/dL
<LLN - 0.5 mmol/L
0.9 - <1.2 mg/dL
0.4 - <0.5 mmol/L
0.7 - <0.9 mg/dL
0.3 - <0.4 mmol/L
<0.7 mg/dL
<0.3 mmol/L
Hyponatremia WNL <LLN - 130 mmol/L - 120 - <130 mmol/L <120 mmol/L
Hypophosphatemia WNL <LLN -2.5 mg/dL
<LLN - 0.8 mmol/L
≥2.0 - <2.5 mg/dL
≥0.6 - <0.8 mmol/L
≥1.0 - <2.0 mg/dL
≥0.3 - <0.6 mmol/L
<1.0 mg/dL
<0.3 mmol/L
Hypothyroidism is graded in the ENDOCRINE category.
Lipase WNL >ULN - 1.5 x ULN >1.5 - 2.0 x ULN >2.0 - 5.0 x ULN >5.0 x ULN
Metabolic/Laboratory -
Other (Specify,
__________)
none mild moderate severe
life-threatening or
disabling
MUSCULOSKELETAL
Arthralgia is graded in the PAIN category.
Arthritis none mild pain with
inflammation, erythema
or joint swelling but not
interfering with
function
moderate pain with
inflammation,
erythema, or joint
swelling interfering
with function, but not
interfering with
activities of daily living
severe pain with
inflammation,
erythema, or joint
swelling and interfering
with activities of daily
living
disabling

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 18 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Grade
Adverse Event 0 1 2 3 4
Muscle weakness
(not due to neuropathy)
normal asymptomatic with
weakness on physical
exam
symptomatic and
interfering with
function, but not
interfering with
activities of daily living
symptomatic and
interfering with
activities of daily living
bedridden or disabling
Myalgia [tenderness or pain in muscles] is graded in the PAIN category.
Myositis
(inflammation/damage of
muscle)
none mild pain, not
interfering with
function
pain interfering with
function, but not
interfering with
activities of daily living
pain interfering with
function and interfering
with activities of daily
living
bedridden or disabling
Also consider CPK.
Note: Myositis implies muscle damage (i.e., elevated CPK).
Osteonecrosis
(avascular necrosis)
none asymptomatic and
detected by imaging
only
symptomatic and
interfering with
function, but not
interfering with
activities of daily living
symptomatic and
interfering with
activities of daily living
symptomatic; or
disabling
Musculoskeletal - Other
(Specify, __________)
none mild moderate severe life-threatening or
disabling
NEUROLOGY
Aphasia, receptive and/or expressive, is graded under Speech impairment in the NEUROLOGY category.
Arachnoiditis/meningismus/
radiculitis
absent mild pain not interfering
with function
moderate pain
interfering with
function, but not
interfering with
activities of daily living
severe pain interfering
with activities of daily
living
unable to function or
perform activities of
daily living; bedridden;
paraplegia
Also consider Headache, Vomiting, Fever.
Ataxia (incoordination) normal asymptomatic but
abnormal on physical
exam, and not
interfering with
function
mild symptoms
interfering with
function, but not
interfering with
activities of daily living
moderate symptoms
interfering with
activities of daily living
bedridden or disabling
CNS cerebrovascular
ischemia
none - - transient ischemic event
or attack (TIA)
permanent event (e.g.,
cerebral vascular
accident)
CNS hemorrhage/bleeding is graded in the HEMORRHAGE category.
Cognitive disturbance/
learning problems
none
cognitive disability; not
interfering with
work/school
performance;
preservation of
intelligence
cognitive disability;
interfering with
work/school
performance; decline of
1 SD (Standard
Deviation) or loss of
developmental
milestones
cognitive disability;
resulting in significant
impairment of
work/school
performance; cognitive
decline >2 SD
inability to work/frank
mental retardation

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 19 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Grade
Adverse Event 0 1 2 3 4
Confusion normal confusion or
disorientation or
attention deficit of brief
duration; resolves
spontaneously with no
sequelae
confusion or
disorientation or
attention deficit
interfering with
function, but not
interfering with
activities of daily living
confusion or delirium
interfering with
activities of daily living
harmful to others or
self; requiring
hospitalization
Cranial neuropathy is graded in the NEUROLOGY category as Neuropathy-cranial.
Delusions normal - - present toxic psychosis
Depressed level of
consciousness
normal somnolence or sedation
not interfering with
function
somnolence or sedation
interfering with
function, but not
interfering with
activities of daily living
obtundation or stupor;
difficult to arouse;
interfering with
activities of daily living
coma
Note: Syncope (fainting) is graded in the NEUROLOGY category.
Dizziness/lightheadedness none not interfering with
function
interfering with
function, but not
interfering with
activities of daily living
interfering with
activities of daily living
bedridden or disabling
Dysphasia, receptive and/or expressive, is graded under Speech impairment in the NEUROLOGY category.
Extrapyramidal/
involuntary movement/
restlessness
none mild involuntary
movements not
interfering with
function
moderate involuntary
movements interfering
with function, but not
interfering with
activities of daily living
severe involuntary
movements or torticollis
interfering with
activities of daily living
bedridden or disabling
Hallucinations normal - - present toxic psychosis
Headache is graded in the PAIN category.
Insomnia normal
occasional difficulty
sleeping not interfering
with function
difficulty sleeping
interfering with
function, but not
interfering with
activities of daily living
frequent difficulty
sleeping, interfering
with activities of daily
living
-
Note: This adverse event is graded when insomnia is related to treatment. If pain or other symptoms interfere with sleep do NOT grade as insomnia.
Irritability
(children <3 years of age)
normal mild; easily consolable
moderate; requiring
increased attention
severe; inconsolable -
Leukoencephalopathy
associated radiological
findings
none
mild increase in SAS
(subarachnoid space)
and/or mild
ventriculomegaly;
and/or small (+/-
multiple) focal T2
hyperintensities,
involving
periventricular white
matter or <1/3 of
susceptible areas of
cerebrum
moderate increase in
SAS; and/or moderate
ventriculomegaly;
and/or focal T2
hyperintensities
extending into centrum
ovale; or involving 1/3
to 2/3 of susceptible
areas of cerebrum
severe increase in SAS;
severe
ventriculomegaly; near
total white matter T2
hyperintensities or
diffuse low attenuation
(CT); focal white matter
necrosis (cystic)
severe increase in SAS;
severe
ventriculomegaly;
diffuse low attenuation
with calcification (CT);
diffuse white matter
necrosis (MRI)
Memory loss normal
memory loss not
interfering with
function
memory loss interfering
with function, but not
interfering with
activities of daily living
memory loss interfering
with activities of daily
living
amnesia

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 20 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Grade
Adverse Event 0 1 2 3 4
Mood alteration-anxiety,
agitation
normal mild mood alteration
not interfering with
function
moderate mood
alteration interfering
with function, but not
interfering with
activities of daily living
severe mood alteration
interfering with
activities of daily living
suicidal ideation or
danger to self
Mood alteration-depression normal
mild mood alteration
not interfering with
function
moderate mood
alteration interfering
with function, but not
interfering with
activities of daily living
severe mood alteration
interfering with
activities of daily living
suicidal ideation or
danger to self
Mood alteration-euphoria normal
mild mood alteration
not interfering with
function
moderate mood
alteration interfering
with function, but not
interfering with
activities of daily living
severe mood alteration
interfering with
activities of daily living
danger to self
Neuropathic pain is graded in the PAIN category.
Neuropathy-cranial absent -
present, not interfering
with activities of daily
living
present, interfering with
activities of daily living
life-threatening,
disabling
Neuropathy-motor normal
subjective weakness but
no objective findings
mild objective
weakness interfering
with function, but not
interfering with
activities of daily living
objective weakness
interfering with
activities of daily living
paralysis
Neuropathy-sensory normal loss of deep tendon
reflexes or paresthesia
(including tingling) but
not interfering with
function
objective sensory loss
or paresthesia
(including tingling),
interfering with
function, but not
interfering with
activities of daily living
sensory loss or
paresthesia interfering
with activities of daily
living
permanent sensory loss
that interferes with
function
Nystagmus absent present - - -
Also consider Vision-double vision.
Personality/behavioral normal
change, but not
disruptive to patient or
family
disruptive to patient or
family
disruptive to patient and
family; requiring mental
health intervention
harmful to others or
self; requiring
hospitalization
Pyramidal tract dysfunction
(e.g., ↑ tone, hyperreflexia,
positive Babinski, ↓ fine
motor coordination)
normal
asymptomatic with
abnormality on physical
examination
symptomatic or
interfering with
function but not
interfering with
activities of daily living
interfering with
activities of daily living
bedridden or disabling;
paralysis
Seizure(s) none - seizure(s) self-limited
and consciousness is
preserved
seizure(s) in which
consciousness is altered
seizures of any type
which are prolonged,
repetitive, or difficult to
control (e.g., status
epilepticus, intractable
epilepsy)
Speech impairment
(e.g., dysphasia or aphasia)
normal -
awareness of receptive
or expressive dysphasia,
not impairing ability to
communicate
receptive or expressive
dysphasia, impairing
ability to communicate
inability to
communicate
Syncope (fainting) absent - - present -
Also consider CARDIOVASCULAR (ARRHYTHMIA), Vasovagal episode, CNS cerebrovascular ischemia.

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 21 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Grade
Adverse Event 0 1 2 3 4
Tremor none mild and brief or
intermittent but not
interfering with
function
moderate tremor
interfering with
function, but not
interfering with
activities of daily living
severe tremor
interfering with
activities of daily living
-
Vertigo none
not interfering with
function
interfering with
function, but not
interfering with
activities of daily living
interfering with
activities of daily living
bedridden or disabling
Neurology - Other
(Specify, __________)
none mild moderate severe life-threatening or
disabling
OCULAR/VISUAL
Cataract none asymptomatic symptomatic, partial
visual loss
symptomatic, visual
loss requiring treatment
or interfering with
function
-
Conjunctivitis none abnormal
ophthalmologic
changes, but
asymptomatic or
symptomatic without
visual impairment (i.e.,
pain and irritation)
symptomatic and
interfering with
function, but not
interfering with
activities of daily living
symptomatic and
interfering with
activities of daily living
-
Dry eye normal
mild, not requiring
treatment
moderate or requiring
artificial tears
--
Glaucoma none
increase in intraocular
pressure but no visual
loss
increase in intraocular
pressure with retinal
changes
visual impairment
unilateral or bilateral
loss of vision
(blindness)
Keratitis
(corneal inflammation/
corneal ulceration)
none
abnormal
ophthalmologic changes
but asymptomatic or
symptomatic without
visual impairment (i.e.,
pain and irritation)
symptomatic and
interfering with
function, but not
interfering with
activities of daily living
symptomatic and
interfering with
activities of daily living
unilateral or bilateral
loss of vision
(blindness)
Tearing (watery eyes) none
mild: not interfering
with function
moderate: interfering
with function, but not
interfering with
activities of daily living
interfering with
activities of daily living
-
Vision-blurred vision normal - symptomatic and
interfering with
function, but not
interfering with
activities of daily living
symptomatic and
interfering with
activities of daily living
-
Vision-double vision
(diplopia)
normal -
symptomatic and
interfering with
function, but not
interfering with
activities of daily living
symptomatic and
interfering with
activities of daily living
-
Vision-flashing
lights/floaters
normal
mild, not interfering
with function
symptomatic and
interfering with
function, but not
interfering with
activities of daily living
symptomatic and
interfering with
activities of daily living
-

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 22 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Grade
Adverse Event 0 1 2 3 4
Vision-night blindness
(nyctalopia)
normal abnormal electro-
retinography but
asymptomatic
symptomatic and
interfering with
function, but not
interfering with
activities of daily living
symptomatic and
interfering with
activities of daily living
-
Vision-photophobia normal -
symptomatic and
interfering with
function, but not
interfering with
activities of daily living
symptomatic and
interfering with
activities of daily living
-
Ocular/Visual - Other
(Specify, __________)
normal mild moderate severe
unilateral or bilateral
loss of vision
(blindness)
PAIN
Abdominal pain or cramping none
mild pain not interfering
with function
moderate pain: pain or
analgesics interfering
with function, but not
interfering with
activities of daily living
severe pain: pain or
analgesics severely
interfering with
activities of daily living
disabling
Arthralgia
(joint pain)
none mild pain not interfering
with function
moderate pain: pain or
analgesics interfering
with function, but not
interfering with
activities of daily living
severe pain: pain or
analgesics severely
interfering with
activities of daily living
disabling
Arthritis (joint pain with clinical signs of inflammation) is graded in the MUSCULOSKELETAL category.
Bone pain none
mild pain not interfering
with function
moderate pain: pain or
analgesics interfering
with function, but not
interfering with
activities of daily living
severe pain: pain or
analgesics severely
interfering with
activities of daily living
disabling
Chest pain
(non-cardiac and non-
pleuritic)
none mild pain not interfering
with function
moderate pain: pain or
analgesics interfering
with function, but not
interfering with
activities of daily living
severe pain: pain or
analgesics severely
interfering with
activities of daily living
disabling
Dysmenorrhea none mild pain not interfering
with function
moderate pain: pain or
analgesics interfering
with function, but not
interfering with
activities of daily living
severe pain: pain or
analgesics severely
interfering with
activities of daily living
disabling
Dyspareunia none
mild pain not interfering
with function
moderate pain
interfering with sexual
activity
severe pain preventing
sexual activity
-
Dysuria is graded in the RENAL/GENITOURINARY category.
Earache (otalgia) none mild pain not interfering
with function
moderate pain: pain or
analgesics interfering
with function, but not
interfering with
activities of daily living
severe pain: pain or
analgesics severely
interfering with
activities of daily living
disabling
Headache none
mild pain not interfering
with function
moderate pain: pain or
analgesics interfering
with function, but not
interfering with
activities of daily living
severe pain: pain or
analgesics severely
interfering with
activities of daily living
disabling

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 23 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Grade
Adverse Event 0 1 2 3 4
Hepatic pain none mild pain not interfering
with function
moderate pain: pain or
analgesics interfering
with function, but not
interfering with
activities of daily living
severe pain: pain or
analgesics severely
interfering with
activities of daily living
disabling
Myalgia
(muscle pain)
none
mild pain not interfering
with function
moderate pain: pain or
analgesics interfering
with function, but not
interfering with
activities of daily living
severe pain: pain or
analgesics severely
interfering with
activities of daily living
disabling
Neuropathic pain
(e.g., jaw pain, neurologic
pain, phantom limb pain,
post-infectious neuralgia, or
painful neuropathies)
none
mild pain not interfering
with function
moderate pain: pain or
analgesics interfering
with function, but not
interfering with
activities of daily living
severe pain: pain or
analgesics severely
interfering with
activities of daily living
disabling
Pain due to radiation none mild pain not interfering
with function
moderate pain: pain or
analgesics interfering
with function, but not
interfering with
activities of daily living
severe pain: pain or
analgesics severely
interfering with
activities of daily living
disabling
Pelvic pain none mild pain not interfering
with function
moderate pain: pain or
analgesics interfering
with function, but not
interfering with
activities of daily living
severe pain: pain or
analgesics severely
interfering with
activities of daily living
disabling
Pleuritic pain none
mild pain not interfering
with function
moderate pain: pain or
analgesics interfering
with function, but not
interfering with
activities of daily living
severe pain: pain or
analgesics severely
interfering with
activities of daily living
disabling
Rectal or perirectal pain
(proctalgia)
none mild pain not interfering
with function
moderate pain: pain or
analgesics interfering
with function, but not
interfering with
activities of daily living
severe pain: pain or
analgesics severely
interfering with
activities of daily living
disabling
Tumor pain
(onset or exacerbation of
tumor pain due to treatment)
none mild pain not interfering
with function
moderate pain: pain or
analgesics interfering
with function, but not
interfering with
activities of daily living
severe pain: pain or
analgesics severely
interfering with
activities of daily living
disabling
Tumor flare is graded in the SYNDROME category.
Pain - Other
(Specify, __________)
none mild moderate severe disabling
PULMONARY
Adult Respiratory Distress
Syndrome (ARDS)
absent---present
Apnea none - - present requiring intubation

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 24 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Grade
Adverse Event 0 1 2 3 4
Carbon monoxide diffusion
capacity (DL
CO
)
≥90% of
pretreatment or
normal value
≥75 - <90% of
pretreatment or normal
value
≥50 - <75% of
pretreatment or normal
value
≥25 - <50% of
pretreatment or normal
value
<25% of pretreatment
or normal value
Cough absent
mild, relieved by non-
prescription medication
requiring narcotic
antitussive
severe cough or
coughing spasms,
poorly controlled or
unresponsive to
treatment
-
Dyspnea
(shortness of breath)
normal - dyspnea on exertion dyspnea at normal level
of activity
dyspnea at rest or
requiring ventilator
support
FEV
1
≥90% of
pretreatment or
normal value
≥75 - <90% of
pretreatment or normal
value
≥50 - <75% of
pretreatment or normal
value
≥25 - <50% of
pretreatment or normal
value
<25% of pretreatment
or normal value
Hiccoughs (hiccups,
singultus)
none mild, not requiring
treatment
moderate, requiring
treatment
severe, prolonged, and
refractory to treatment
-
Hypoxia normal -
decreased O
2
saturation
with exercise
decreased O
2
saturation
at rest, requiring
supplemental oxygen
decreased O
2
saturation,
requiring pressure
support (CPAP) or
assisted ventilation
Pleural effusion
(non-malignant)
none asymptomatic and not
requiring treatment
symptomatic, requiring
diuretics
symptomatic, requiring
O
2
or therapeutic
thoracentesis
life-threatening (e.g.,
requiring intubation)
Pleuritic pain is graded in the PAIN category.
Pneumonitis/pulmonary
infiltrates
none
radiographic changes
but asymptomatic or
symptoms not requiring
steroids
radiographic changes
and requiring steroids or
diuretics
radiographic changes
and requiring oxygen
radiographic changes
and requiring assisted
ventilation
Pneumothorax none no intervention required chest tube required sclerosis or surgery
required
life-threatening
Pulmonary embolism is graded as Thrombosis/embolism in the CARDIOVASCULAR (GENERAL) category.
Pulmonary fibrosis none radiographic changes,
but asymptomatic or
symptoms not requiring
steroids
requiring steroids or
diuretics
requiring oxygen requiring assisted
ventilation
Note: Radiation-related pulmonary fibrosis is graded in the RTOG/EORTC Late Radiation Morbidity Scoring Scheme-Lung. (See Appendix IV)
Voice changes/stridor/larynx
(e.g., hoarseness, loss of
voice, laryngitis)
normal
mild or intermittent
hoarseness
persistent hoarseness,
but able to vocalize;
may have mild to
moderate edema
whispered speech, not
able to vocalize; may
have marked edema
marked dyspnea/stridor
requiring tracheostomy
or intubation
Notes: Cough from radiation is graded as cough in the PULMONARY category.
Radiation-related hemoptysis from larynx/pharynx is graded as Grade 4 Mucositis due to radiation in the GASTROINTESTINAL category. Radiation-
related hemoptysis from the thoracic cavity is graded as Grade 4 Hemoptysis in the HEMORRHAGE category.
Pulmonary - Other
(Specify, __________)
none mild moderate severe life-threatening or
disabling

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 25 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Grade
Adverse Event 0 1 2 3 4
RENAL/GENITOURINARY
Bladder spasms absent mild symptoms, not
requiring intervention
symptoms requiring
antispasmodic
severe symptoms
requiring narcotic
-
Creatinine WNL >ULN - 1.5 x ULN >1.5 - 3.0 x ULN >3.0 - 6.0 x ULN >6.0 x ULN
Note: Adjust to age-appropriate levels for pediatric patients.
Dysuria
(painful urination)
none
mild symptoms
requiring no
intervention
symptoms relieved with
therapy
symptoms not relieved
despite therapy
-
Fistula or GU fistula
(e.g., vaginal, vesicovaginal)
none - - requiring intervention requiring surgery
Hemoglobinuria - present - - -
Hematuria (in the absence of vaginal bleeding) is graded in the HEMORRHAGE category.
Incontinence none with coughing,
sneezing, etc.
spontaneous, some
control
no control (in the
absence of fistula)
-
Operative injury to bladder
and/or ureter
none - injury of bladder with
primary repair
sepsis, fistula, or
obstruction requiring
secondary surgery; loss
of one kidney; injury
requiring anastomosis
or re-implantation
septic obstruction of
both kidneys or
vesicovaginal fistula
requiring diversion
Proteinuria normal or <0.15
g/24 hours
1+ or 0.15 - 1.0 g/24
hours
2+ to 3+ or 1.0 - 3.5
g/24 hours
4+ or >3.5 g/24 hours nephrotic syndrome
Note: If there is an inconsistency between absolute value and dip stick reading, use the absolute value for grading.
Renal failure none - - requiring dialysis, but
reversible
requiring dialysis and
irreversible
Ureteral obstruction none
unilateral, not requiring
surgery
-
bilateral, not requiring
surgery
stent, nephrostomy
tube, or surgery
Urinary electrolyte wasting
(e.g., Fanconi’s syndrome,
renal tubular acidosis)
none
asymptomatic, not
requiring treatment
mild, reversible and
manageable with oral
replacement
reversible but requiring
IV replacement
irreversible, requiring
continued replacement
Also consider Acidosis, Bicarbonate, Hypocalcemia, Hypophosphatemia.
Urinary frequency/urgency normal increase in frequency or
nocturia up to 2 x
normal
increase >2 x normal
but <hourly
hourly or more with
urgency, or requiring
catheter
-
Urinary retention normal hesitancy or dribbling,
but no significant
residual urine; retention
occurring during the
immediate
postoperative period
hesitancy requiring
medication or
occasional in/out
catheterization (<4 x per
week), or operative
bladder atony requiring
indwelling catheter
beyond immediate
postoperative period but
for <6 weeks
requiring frequent
in/out catheterization
(≥4 x per week) or
urological intervention
(e.g., TURP, suprapubic
tube, urethrotomy)
bladder rupture

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 26 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Grade
Adverse Event 0 1 2 3 4
Urine color change
(not related to other dietary
or physiologic cause e.g.,
bilirubin, concentrated urine,
hematuria)
normal asymptomatic, change
in urine color
---
Vaginal bleeding is graded in the HEMORRHAGE category.
Vaginitis
(not due to infection)
none mild, not requiring
treatment
moderate, relieved with
treatment
severe, not relieved
with treatment, or
ulceration not requiring
surgery
ulceration requiring
surgery
Renal/Genitourinary - Other
(Specify, __________)
none mild moderate severe
life-threatening or
disabling
SECONDARY MALIGNANCY
Secondary Malignancy -
Other
(Specify type, __________)
excludes metastasis from
initial primary
none---present
SEXUAL/REPRODUCTIVE FUNCTION
Dyspareunia is graded in the PAIN category.
Dysmenorrhea is graded in the PAIN category.
Erectile impotence normal mild (erections
impaired but
satisfactory)
moderate (erections
impaired, unsatisfactory
for intercourse)
no erections -
Female sterility normal - - sterile -
Feminization of male is graded in the ENDOCRINE category.
Irregular menses
(change from baseline)
normal
occasionally irregular or
lengthened interval, but
continuing menstrual
cycles
very irregular, but
continuing menstrual
cycles
persistent amenorrhea -
Libido normal decrease in interest severe loss of interest - -
Male infertility - -
oligospermia
(low sperm count)
azoospermia
(no sperm)
-
Masculinization of female is graded in the ENDOCRINE category.
Vaginal dryness normal mild
requiring treatment
and/or interfering with
sexual function,
dyspareunia
--
Sexual/Reproductive
Function - Other
(Specify, __________)
none mild moderate severe disabling
SYNDROMES (not included in previous categories)
Acute vascular leak syndrome is graded in the CARDIOVASCULAR (GENERAL) category.
ARDS (Adult Respiratory Distress Syndrome) is graded in the PULMONARY category.

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 27 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Grade
Adverse Event 0 1 2 3 4
Autoimmune reactions are graded in the ALLERGY/IMMUNOLOGY category.
DIC (disseminated intravascular coagulation) is graded in the COAGULATION category.
Fanconi’s syndrome is graded as Urinary electrolyte wasting in the RENAL/GENITOURINARY category.
Renal tubular acidosis is graded as Urinary electrolyte wasting in the RENAL/GENITOURINARY category.
Stevens-Johnson syndrome (erythema multiforme) is graded in the DERMATOLOGY/SKIN category.
SIADH (syndrome of inappropriate antidiuretic hormone) is graded in the ENDOCRINE category.
Thrombotic microangiopathy (e.g., thrombotic thrombocytopenic purpura/TTP or hemolytic uremic syndrome/HUS) is graded in the COAGULATION category.
Tumor flare none
mild pain not interfering
with function
moderate pain; pain or
analgesics interfering
with function, but not
interfering with
activities of daily living
severe pain; pain or
analgesics interfering
with function and
interfering with
activities of daily living
Disabling
Also consider Hypercalcemia.
Note: Tumor flare is characterized by a constellation of symptoms and signs in direct relation to initiation of therapy (e.g., anti-estrogens/androgens or additional
hormones). The symptoms/signs include tumor pain, inflammation of visible tumor, hypercalcemia, diffuse bone pain, and other electrolyte disturbances.
Tumor lysis syndrome absent - - present -
Also consider Hyperkalemia, Creatinine.
Urinary electrolyte wasting (e.g., Fanconi’s syndrome, renal tubular acidosis) is graded in the RENAL/GENITOURINARY category.
Syndromes - Other
(Specify, __________)
none mild moderate severe
life-threatening or
disabling

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 28 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Appendix I
Adverse Event Module
To be implemented at the request of the study sponsor or principal investigator in the protocol or by protocol
amendment when more detailed information is considered pertinent.
Adverse Event: Date of Treatment: Course Number:
Date of onset: Grade at onset:
Date of first change in grade: Grade:
Date of next change in grade: Grade:
Date of next change in grade: Grade:
Date of next change in grade: Grade:
Date of next change in grade: Grade:
Date of next change in grade: Grade:
Did adverse event resolve? Yes______ No______
If so, date of resolution of adverse event:
Date of last observation (if prior to
recovery):
Reason(s) observations stopped (if prior
to recovery):
Was patient retreated? Yes______ No______
If yes, was treatment delayed for
recovery? Yes______ No______
Date of next treatment?
Dose reduced for next treatment? Yes______ No______
Additional Comments:
________________________________________________________________________________________________________
________________________________________________________________________________________________________
If module is being activated for new adverse event not currently in CTC, please provide definitions for adverse event grading:
Grade 0 = ____________________________________________________________________
Grade 1 = ____________________________________________________________________
Grade 2 = ____________________________________________________________________
Grade 3 = ____________________________________________________________________
Grade 4 = ____________________________________________________________________

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 29 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Appendix II
Infection Module
To be implemented at the request of the study sponsor or principal investigator in the protocol or by protocol
amendment when more detailed information is considered pertinent.
1.
Use the Common Toxicity Criteria definitions to grade the severity of the infection.
2.
Specify type of infection from the following (CHOOSE ONE):
BACTERIAL FUNGAL PROTOZOAL VIRAL UNKNOWN
3.
Specify site of infection from the following (CHOOSE ALL THAT APPLY):
BLOOD CULTURE POSITIVE
BONE INFECTION
CATHETER (intravenous)
CATHETER (intravenous), tunnel infection
CENTRAL NERVOUS SYSTEM INFECTION
EAR INFECTION
EYE INFECTION
GASTROINTESTINAL INFECTION
ORAL INFECTION
PNEUMONIA
SKIN INFECTION
UPPER RESPIRATORY INFECTION
URINARY TRACT INFECTION
VAGINAL INFECTION
INFECTION, not otherwise specified (Specify site, __________)
4.
Specify organism, if known: _______________.
5.
Prophylactic antibiotic, antifungal, or antiviral therapy administration
Yes_______ No_______
If prophylaxis was given prior to infection, please specify below:
Antibiotic prophylaxis _____________________________________________________
Antifungal prophylaxis ____________________________________________________
Antiviral prophylaxis ______________________________________________________
Other prophylaxis ________________________________________________________

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 30 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Appendix III
Performance Status Scales/Scores
PERFORMANCE STATUS CRITERIA
Karnofsky and Lansky performance scores are intended to be multiples of 10
.
ECOG (Zubrod) Karnofsky Lansky*
Score Description Score Description Score Description
100 Normal, no complaints, no
evidence of disease.
100 Fully active, normal.
0
Fully active, able to carry on
all pre-disease performance
without restriction.
90 Able to carry on normal
activity; minor signs or
symptoms of disease.
90 Minor restrictions in physically
strenuous activity.
80 Normal activity with effort;
some signs or symptoms of
disease.
80 Active, but tires more quickly
1
Restricted in physically
strenuous activity but
ambulatory and able to carry
out work of a light or
sedentary nature, e.g., light
housework, office work.
70 Cares for self, unable to carry
on normal activity or do active
work.
70 Both greater restriction of and less time
spent in play activity.
60 Requires occasional
assistance, but is able to care
for most of his/her needs.
60 Up and around, but minimal active play;
keeps busy with quieter activities.
2
Ambulatory and capable of all
selfcare but unable to carry
out any work activities. Up
and about more than 50% of
waking hours.
50 Requires considerable
assistance and frequent
medical care.
50 Gets dressed, but lies around much of
the day; no active play; able to
participate in all quiet play and
activities.
40 Disabled, requires special care
and assistance.
40 Mostly in bed; participates in quiet
activities.
3
Capable of only limited
selfcare, confined to bed or
chair more than 50% of
waking hours.
30 Severely disabled,
hospitalization indicated.
Death not imminent.
30 In bed; needs assistance even for quiet
play.
20 Very sick, hospitalization
indicated. Death not imminent.
20 Often sleeping; play entirely limited to
very passive activities.
4
Completely disabled. Cannot
carry on any selfcare. Totally
confined to bed or chair.
10 Moribund, fatal processes
progressing rapidly.
10 No play; does not get out of bed.
*The conversion of the Lansky to ECOG scales is intended for NCI reporting purposes only.

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 31 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Appendix IV
RTOG/EORTC Late Radiation Morbidity Scoring Scheme
Use for adverse event occurring greater than 90 days after radiation therapy.
Grade
Adverse Event 0 1 2 3 4
Bladder-
Late RT Morbidity Scoring
No change from
baseline
Slight epithelial
atrophy/minor
telangiectasia
(microscopic hematuria)
Moderate frequency/
generalized
telangiectasia/
intermittent
macroscopic hematuria
Severe frequency and
dysuria/severe
generalized
telangiectasia (often
with petechiae);
frequent hematuria;
reduction in bladder
capacity (<150 mL)
Necrosis/contracted
bladder (capacity <100
mL)/severe
hemorrhagic cystitis
Bone-
Late RT Morbidity Scoring
No change from
baseline
Asymptomatic; no
growth retardation;
reduced bone density
Moderate pain or
tenderness; growth
retardation; irregular
bone sclerosis
Severe pain or
tenderness; complete
arrest of bone growth;
dense bone sclerosis
Necrosis/
spontaneous fracture
Brain-
Late RT Morbidity Scoring
No change from
baseline
Mild headache; slight
lethargy
Moderate headache;
great lethargy
Severe headaches;
severe CNS dysfunction
(partial loss of power or
dyskinesia)
Seizures or paralysis;
coma
Esophagus-
Late RT Morbidity Scoring
No change from
baseline
Mild fibrosis; slight
difficulty in swallowing
solids; no pain on
swallowing
Unable to take solid
food normally;
swallowing semi-solid
food; dilation may be
indicated
Severe fibrosis; able to
swallow only liquids;
may have pain on
swallowing; dilation
required
Necrosis/
perforation; fistula
Eye-
Late RT Morbidity Scoring
No change from
baseline
Asymptomatic cataract;
minor corneal
ulceration or keratitis
Symptomatic cataract;
moderate corneal
ulceration; minor
retinopathy or glaucoma
Severe keratitis; severe
retinopathy or
detachment; severe
glaucoma
Panophthalmitis;
blindness
Heart-
Late RT Morbidity Scoring
No change from
baseline
Asymptomatic or mild
symptoms; transient T
wave inversion and ST
changes; sinus
tachycardia >110 (at
rest)
Moderate angina on
effort; mild pericarditis;
normal heart size;
persistent abnormal T
wave and ST changes;
low QRS
Severe angina;
pericardial effusion;
constrictive pericarditis;
moderate heart failure;
cardiac enlargement;
EKG abnormalities
Tamponade/severe heart
failure/severe
constrictive pericarditis
Joint-
Late RT Morbidity Scoring
No change from
baseline
Mild joint stiffness;
slight limitation of
movement
Moderate stiffness;
intermittent or moderate
joint pain; moderate
limitation of movement
Severe joint stiffness;
pain with severe
limitation of movement
Necrosis/complete
fixation
Kidney-
Late RT Morbidity Scoring
No change from
baseline
Transient albuminuria;
no hypertension; mild
impairment of renal
function; urea 25 - 35
mg%; creatinine 1.5 -
2.0 mg%; creatinine
clearance >75%
Persistent moderate
albuminuria (2+); mild
hypertension; no related
anemia; moderate
impairment of renal
function; urea >36 - 60
mg%; creatinine
clearance >50 - 74%
Severe albuminuria;
severe hypertension;
persistent anemia (<10
g%); severe renal
failure; urea >60 mg%;
creatinine >4 mg%;
creatinine clearance
<50%
Malignant hypertension;
uremic coma/urea
>100%
Larynx-
Late RT Morbidity Scoring
No change from
baseline
Hoarseness; slight
arytenoid edema
Moderate arytenoid
edema; chondritis
Severe edema; severe
chondritis
Necrosis

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 32 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Appendix IV (continued)
RTOG/EORTC Late Radiation Morbidity Scoring Scheme
Use for adverse event occurring greater than 90 days after radiation therapy.
Grade
Adverse Event 0 1 2 3 4
Liver-
Late RT Morbidity Scoring
No change from
baseline
Mild lassitude; nausea;
dyspepsia; slightly
abnormal liver function
Moderate symptoms;
some abnormal liver
function tests; serum
albumin normal
Disabling hepatic
insufficiency; liver
function tests grossly
abnormal; low albumin;
edema or ascites
Necrosis/hepatic coma
or encephalopathy
Lung-
Late RT Morbidity Scoring
No change from
baseline
Asymptomatic or mild
symptoms (dry cough);
slight radiographic
appearances
Moderate symptomatic
fibrosis or pneumonitis
(severe cough); low
grade fever; patchy
radiographic
appearances
Severe symptomatic
fibrosis or pneumonitis;
dense radiographic
changes
Severe respiratory
insufficiency/
continuous O
2
/assisted
ventilation
Mucous membrane-
Late RT Morbidity Scoring
No change from
baseline
Slight atrophy and
dryness
Moderate atrophy and
telangiectasia; little
mucus
Marked atrophy with
complete dryness;
severe telangiectasia
Ulceration
Salivary glands-
Late RT Morbidity Scoring
No change from
baseline
Slight dryness of
mouth; good response
on stimulation
Moderate dryness of
mouth; poor response
on stimulation
Complete dryness of
mouth; no response on
stimulation
Fibrosis
Skin-
Late RT Morbidity Scoring
No change from
baseline
Slight atrophy;
pigmentation change;
some hair loss
Patchy atrophy;
moderate telangiectasia;
total hair loss
Marked atrophy; gross
telangiectasia
Ulceration
Small/Large intestine-
Late RT Morbidity Scoring
No change from
baseline
Mild diarrhea; mild
cramping; bowel
movement 5 x daily;
slight rectal discharge
or bleeding
Moderate diarrhea and
colic; bowel movement
>5 x daily; excessive
rectal mucus or
intermittent bleeding
Obstruction or bleeding,
requiring surgery
Necrosis/perforation
fistula
Spinal cord-
Late RT Morbidity Scoring
No change from
baseline
Mild Lhermitte’s
syndrome
Severe Lhermitte’s
syndrome
Objective neurological
findings at or below
cord level treatment
Mono-, para-,
quadriplegia
Subcutaneous tissue-
Late RT Morbidity Scoring
No change from
baseline
Slight induration
(fibrosis) and loss of
subcutaneous fat
Moderate fibrosis but
asymptomatic; slight
field contracture; <10%
linear reduction
Severe induration and
loss of subcutaneous
tissue; field contracture
>10% linear
measurement
Necrosis
Radiation - Other
(Specify, __________)
None Mild Moderate Severe Life-threatening or
disabling

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 33 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Appendix V
BMT-Specific Adverse Events
Summary of BMT-Specific Adverse Events that may be used
if specified by the protocol
. These differ
from the standard CTC and may be more relevant to the transplant setting. They are listed here for the
convenience of investigators writing transplant protocols. They are also included in the CTC document.
Grade
Adverse Event 0 1 2 3 4
Bilirubin associated with
graft versus host disease for
BMT studies .
normal
≥2 - <3 mg/100 mL ≥3 - <6 mg/100 mL ≥6 - <15 mg/100 mL ≥15 mg/100 mL
Diarrhea associated with
graft versus host disease
(GVHD) for BMT studies.
none
>500 - ≤1000mL of
diarrhea/day
>1000 - ≤1500mL of
diarrhea/day
>1500mL of
diarrhea/day
severe abdominal pain
with or without ileus
Diarrhea for pediatric BMT
studies.
>5 -
≤
10 mL/kg of
diarrhea/day
>10 -
≤
15 mL/kg of
diarrhea/day
>15 mL/kg of
diarrhea/day
-
Hepatic enlargement absent - - present -
Leukocytes (total WBC) for
BMT studies.
WNL
≥2.0 - <3.0 X 10
9
/L
≥2000 - <3000/mm
3
≥1.0 - <2.0 x 10
9
/L
≥1000 - <2000/mm
3
≥0.5 - <1.0 x 10
9
/L
≥500 - <1000/mm
3
<0.5 x 10
9
/L
<500/mm
3
Leukocytes (total WBC) for
pediatric BMT studies (using
age, race and sex normal
values).
≥
75 - <100% LLN
≥
50 - <75% LLN
≥
25 - 50% LLN
<25% LLN
Lymphopenia for pediatric
BMT studies (using age,
race and sex normal values).
mm
3
≥
75-<100%LLN
≥
50-<75%LLN
≥
25-<50%LLN
<25%LLN
Neutrophils/granulocytes
(ANC/AGC) for BMT
studies.
WNL
≥1.0 - <1.5 x 10
9
/L
≥1000 - <1500/mm
3
≥0.5 - <1.0 x 10
9
/L
≥500 - <1000/mm
3
≥0.1 - <0.5 x 10
9
/L
≥100 - <500/mm
3
<0.1 x 10
9
/L
<100/mm
3
Platelets for BMT studies. WNL
≥50.0 - <75.0 x 10
9
/L
≥50,000 - <75,000/mm
3
≥20.0 - <50.0 x 10
9
/L
≥20,000 - <50,000/mm
3
≥10.0 - <20.0 x 10
9
/L
≥10,000 - <20,000/mm
3
<10.0 x 10
9
/L
<10,000/mm
3
Rash/dermatitis associated
with high-dose
chemotherapy or BMT
studies.
none
faint erythema or dry
desquamation
moderate to brisk
erythema or a patchy
moist desquamation,
mostly confined to skin
folds and creases;
moderate edema
confluent moist
desquamation, ≥1.5 cm
diameter, not confined
to skin folds; pitting
edema
skin necrosis or
ulceration of full
thickness dermis; may
include spontaneous
bleeding not induced by
minor trauma or
abrasion
Rash/desquamation
associated with graft versus
host disease (GVHD) for
BMT studies.
none macular or papular
eruption or erythema
covering <25% of body
surface area without
associated symptoms
macular or papular
eruption or erythema
with pruritus or other
associated symptoms
covering ≥25 - <50% of
body surface or
localized desquamation
or other lesions
covering ≥25 - <50% of
body surface area
symptomatic
generalized
erythroderma or
symptomatic macular,
papular or vesicular
eruption, with bullous
formation, or
desquamation covering
≥50% of body surface
area
generalized exfoliative
dermatitis or ulcerative
dermatitis or bullous
formation

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 34 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Appendix V (Continued)
BMT-Specific Adverse Events
Summary of BMT-Specific Adverse Events that may be used
if specified by the protocol
. These differ
from the standard CTC and may be more relevant to the transplant setting. They are listed here for the
convenience of investigators writing transplant protocols. They are also included in the CTC document.
Grade
Adverse Event 0 1 2 3 4
Stomatitis/pharyngitis
(oral/pharyngeal mucositis)
for BMT studies.
none painless ulcers,
erythema, or mild
soreness in the absence
of lesions
painful erythema,
edema or ulcers but can
swallow
painful erythema,
edema, or ulcers
preventing swallowing
or requiring hydration
or parenteral (or enteral)
nutritional support
severe ulceration
requiring prophylactic
intubation or resulting
in documented
aspiration pneumonia
Transfusion: Platelets for
BMT studies.
none 1 platelet transfusion in
24 hours
2 platelet transfusions in
24 hours
≥3 platelet transfusions
in 24 hours
platelet transfusions and
other measures required
to improve platelet
increment; platelet
transfusion
refractoriness associated
with life-threatening
bleeding. (e.g., HLA or
cross matched platelet
transfusions)
Transfusion: pRBCs for
BMT studies.
none
≤2 u pRBC in 24 hours
elective or planned
3 u pRBC in 24 hours
elective or planned
≥4 u pRBC in 24 hours
hemorrhage or
hemolysis associated
with life-threatening
anemia; medical
intervention required to
improve hemoglobin
Transfusion: pRBCs for
pediatric BMT studies.
none
≤
15mL/kg in 24 hours
elective or planned
>15 -
≤
30mL/kg in 24
hours elective or
planned
>30mL/kg in 24 hours
hemorrhage or
hemolysis associated
with life-threatening
anemia; medical
intervention required to
improve hemoglobin
Thrombotic
microangiopathy (e.g.,
thrombotic
thrombocytopenic
purpura/TTP or hemolytic
uremic syndrome/HUS) for
BMT studies.
-
evidence of RBC
destruction
(schistocytosis) without
clinical consequences
evidence of RBC
destruction with
elevated creatinine (≤3
x ULN)
evidence of RBC
destruction with
creatinine (>3 x ULN)
not requiring dialysis
evidence of RBC
destruction with renal
failure requiring
dialysis and/or
encephalopathy
Weight gain associated with
Veno-Occlusive Disease
(VOD) for BMT studies.
<2%
≥2 - <5% ≥5 - <10% ≥10% or as ascites
≥10% or fluid retention
resulting in pulmonary
failure

CTC Version 2.0
Publish Date: April 30, 1999
Cancer Therapy Evaluation Program 35 Revised March 23, 1998
Common Toxicity Criteria, Version 2.0
DCTD, NCI, NIH, DHHS March 1998
Appendix VI
BMT Complex/Multicomponent Events
Grade
Adverse Event 0 1 2 3 4
Note: The grading of Complex/Multicomponent Events in bone marrow transplant will be defined in the protocol. The grading scale must use the CTC criteria for
grading the specific component events (adverse events).
Failure to engraft absent mild moderate severe life-threatening
Also consider Hemoglobin, Neutrophils/granulocytes (ANC/AGC), Neutrophils/granulocytes (ANC/AGC) for BMT studies, if specified in the protocol, Platelets,
Platelets for BMT studies, if specified in the protocol
Graft versus host disease absent mild moderate severe life-threatening
Also consider Fatigue, Rash/desquamation, Rash/desquamation associated with graft versus host disease (GVHD) for BMT studies, if specified in the protocol,
Diarrhea for patients without colostomy, Diarrhea for patients with colostomy, Diarrhea associated with graft versus host disease (GVHD) for BMT studies, if
specified in the protocol, Diarrhea for pediatric BMT studies, if specified in the protocol, Bilirubin, Bilirubin associated with graft versus host disease (GVHD) for
BMT studies, if specified in the protocol
Stem cell infusion
complications
absent mild moderate severe life-threatening
Also consider Allergic reaction/hypersensitivity, Conduction abnormality/Atrioventricular heart block, Nodal/junctional arrhythmia/dysrhythmia, Prolonged QTc
interval (QTc >0.48 seconds), Sinus bradycardia, Sinus tachycardia, Supraventricular arrhythmias (SVT/atrial fibrillation/flutter), Vasovagal episode, Ventricular
arrhythmia (PVCs/bigeminy/trigeminy/ventricular tachycardia), Cardiovascular/Arrhythmia - Other (Specify, ___________), Hypertension, Hypotension, Fever (in
the absence of neutropenia, where neutropenia is defined as AGC <1.0 x 10
9
/L), Rigors/chills, Sweating (diaphoresis), Rash/desquamation, Rash/desquamation
associated with graft versus host disease (GVHD) for BMT studies, if specified in the protocol, Urticaria (hives, welts, wheals), Diarrhea for patients without
colostomy, Diarrhea for patients with colostomy, Diarrhea associated with graft versus host disease (GVHD) for BMT studies, if specified in the protocol, Diarrhea
for pediatric BMT studies, if specified in the protocol, Nausea, Vomiting, Hemorrhage/bleeding with grade 3 or 4 thrombocytopenia, Hemorrhage/bleeding without
grade 3 or 4 thrombocytopenia, Hemoptysis, Alkaline phosphatase, Bilirubin, Bilirubin associated with graft versus host disease (GVHD) for BMT studies, if
specified in the protocol, GGT, SGOT (AST), SGPT (ALT), Infection (documented clinically or microbiologically) with grade 3 or 4 neutropenia (ANC <1.0 x
10
9
/L), Infection without neutropenia, Hyperkalemia, Hypernatremia, Hypokalemia, Depressed level of consciousness, Seizures, Abdominal pain, Headache,
Creatinine, Hemoglobinuria
Veno-Occlusive Disease
(VOD)
absent mild moderate severe life-threatening
Also consider Weight gain associated with Veno-Occlusive Disease (VOD) for BMT studies, if specified in the protocol, Bilirubin, Bilirubin associated with graft
versus host disease (GVHD) for BMT studies, if specified in the protocol, Depressed level of consciousness, Hepatic pain, Renal failure, Hepatic enlargement
