
1
Urgent and Emerging Issues in
Prevention:
Marijuana, Kratom, E-cigarettes
Elinore F. McCance-Katz, MD, PhD
Assistant Secretary for Mental Health and Substance Use
Substance Abuse and Mental Health Services Administration
U.S. Department of Health and Human Services
SAMHSA Prevention Day 2019

2
Preventionists-Key to the Health and Welfare of Americans
• Opioids crisis continues, but with evidence for positive effects of government
efforts in partnership with states, communities, organizations
• Ongoing work of preventionists, clinicians, peers, first responders, faith-based
groups, volunteers, families
• Major decline in heroin initiates in 2017
• Large increases in naloxone distribution, overdose reversals
• Prevention becomes even more important as we watch the unfolding story of the
impact of substance use on American communities
• Preventionists: the first line in addressing the risks presented by substance use in
our communities
• Increased focus on potential harms of substances
• Raise awareness of risks with substance use
• Community outreach to youth as well as adults

3
Substances of Increasing Importance: Marijuana, Kratom
and E-cigarettes (Nicotine)
• Marijuana/cannabis:
• Increasing prevalence of use
• Increasing understanding of risks associated with use
• Public lack of information on these risks
• Opioids Issues:
• Fentanyl-Contaminated Cocaine
• Kratom
• Botanical that at low doses produce stimulation and at higher doses produce opioid
effects
• Potential for physical dependence and opioid-type effects/toxicities
• Marketed in Western countries and increasing use/toxicities being reported
• E-cigarettes
• Vaping: heating and aerosolizing nicotine for inhalation
• Nicotine is addictive and has adverse health effects
• In 2017 e-cigs were the most commonly used nicotine product among high (11.7%;
1.73 million) and middle (3.3%; 0.39 million) school students.

4
Marijuana: The Issue
• Marijuana is rapidly becoming more widely available in the U.S.
• 33 states: allow medical marijuana with reduced penalties for
possession; 9 states plus DC have legalized recreational use
• Huge and profitable industry that markets heavily with health
claims that have little to no basis and which have had virtually
no counter arguments put forward until the present time
• Numerous forms: smoked, edibles, oil for vaping, lotions,
transdermal patches

5
Marijuana: The Issue
• Increasing potency of marijuana:
• THC content: 3.8% (1990s) increased to 12.2% (2014)
• Average MJ extract has THC levels at > 50%
• THC: component responsible for euphoria/intoxication
• Can also produce anxiety, agitation, paranoia, and psychosis
• Responsible for addiction liability with estimates that 10-20% of
users will develop a use disorder (Volkow ND et al. 2016)
• Declining CBD content in currently available MJ
• Not thought to be addictive
• May reduce psychosis
• Medical value: FDA approved for certain seizure disorders (Ehsoly MA et al. 2016)

6
Risks and Adverse Outcomes
• Downplayed by industry; ignored by states
• Low birth weight
• Pulmonary symptoms
• MVAs
• Cognitive impairment
• Poor performance in school and at work
• Addiction

7
State
Effective
Date
2012-13
Percentages
2012-13
Numbers
2013-14
Percentages
2013-14
Numbers
2014-15
Percentages
2014-15
Numbers
2015-16
Percentages
2015-16
Numbers
Alabama
N/A
9.69%
389
9.98%
404
9.60%
389
9.50%
386
Georgia
N/A
11.44%
925
11.75%
963
12.67%
1,052
12.46%
1,048
Idaho
N/A
9.82%
127
11.58%
152
11.40%
152
11.62%
158
Indiana
N/A
11.05%
598
12.86%
700
13.88%
760
13.35%
733
Iowa
N/A
10.40%
266
9.74%
251
9.05%
235
9.75%
254
Kansas
N/A
8.21%
192
11.01%
259
12.38%
292
11.17%
265
Kentucky
N/A
9.22%
334
10.93%
398
12.28%
449
12.79%
470
Louisiana
N/A
10.76%
405
11.23%
425
11.22%
427
11.22%
429
Mississippi
N/A
8.78%
213
9.40%
229
8.67%
212
9.46%
231
Missouri
N/A
11.64%
581
12.73%
639
13.53%
683
13.19%
668
Nebraska
N/A
9.98%
152
10.35%
158
10.75%
166
11.33%
176
North Carolina
N/A
10.88%
877
12.07%
986
11.79%
975
11.90%
996
North Dakota
N/A
9.92%
58
10.25%
62
9.90%
61
9.80%
61
Oklahoma
N/A
9.97%
310
10.75%
338
11.28%
358
11.18%
357
South Carolina
N/A
11.72%
460
11.55%
460
12.56%
507
10.92%
448
South Dakota
N/A
9.64%
66
8.97%
62
10.77%
75
11.85%
83
Tennessee
N/A
9.93%
535
10.29%
560
11.05%
606
12.82%
709
Texas
N/A
9.38%
1,972
9.52%
2,043
10.10%
2,213
10.14%
2,264
Utah
N/A
8.76%
196
9.84%
224
9.07%
211
9.62%
229
Virginia
N/A
12.39%
839
13.04%
891
11.54%
796
11.06%
768
West Virginia
N/A
10.12%
159
10.93%
172
11.07%
174
11.45%
179
Wisconsin
N/A
11.12%
534
11.86%
572
12.05%
584
12.18%
592
Wyoming
N/A
10.11%
48
10.72%
51
10.87%
52
10.62%
51
What Happens as State Laws Liberalize?
Past Year Marijuana Use among Persons Aged 12 or Older Residing in States with No
Legalization of Marijuana, by State: Percentages and Estimated Numbers (in
Thousands), Annual Averages Based on 2012-2013, 2013-2014, 2014-2015, and
2015-2016 NSDUHs
Range: 9-13%

8
State
Effective Date 2012-13
Percentages
2012-13
Numbers
2013-14
Percentages
2013-14
Numbers
2014-15
Percentages
2014-15
Numbers
2015-16
Percentages
2015-16
Numbers
Arizona
Nov 2, 2010
12.94%
699
13.69%
752
13.12%
734
12.22%
696
Arkansas
Nov 9, 2016
9.69%
235
11.37%
277
11.59%
284
11.14%
274
Connecticut
Oct 1, 2012
14.00%
425
14.00%
427
15.67%
479
15.08%
461
Delaware
Jul 1, 2011
13.97%
108
13.98%
109
13.06%
103
13.18%
105
Florida
Jan 3, 2017
11.43%
1,885
11.87%
1,990
12.59%
2,152
13.07%
2,275
Hawaii
Dec 28, 2000
13.37%
151
12.58%
144
12.72%
147
13.05%
151
Illinois
Jan 1, 2014
11.66%
1,247
12.16%
1,305
12.47%
1,339
12.31%
1,320
Maryland
Jun 1, 2014
11.47%
565
13.48%
670
15.13%
757
15.50%
779
Michigan
Dec 4, 2008
15.22%
1,268
15.60%
1,304
15.10%
1,266
15.68%
1,317
Minnesota
May 30, 2014
11.93%
536
12.22%
553
12.69%
579
12.91%
592
Montana
Nov 2, 2004
15.78%
134
14.07%
120
15.38%
133
18.41%
160
New Hampshire
Jul 23, 2013
15.39%
175
16.95%
194
17.35%
199
17.58%
202
New Jersey
Jul 1, 2010
10.18%
759
11.25%
844
11.86%
894
12.01%
907
New Mexico
Jul 1, 2007
15.09%
257
15.61%
267
14.72%
253
15.83%
272
New York
Jul 5, 2014
14.13%
2,342
14.24%
2,372
15.04%
2,519
14.86%
2,491
Ohio
Sep 8, 2016
12.81%
1,237
11.57%
1,122
12.13%
1,179
13.81%
1,344
Pennsylvania
May 17, 2016
11.33%
1,223
11.70%
1,265
12.35%
1,339
13.05%
1,415
Rhode Island
Jan 3, 2006
20.22%
181
18.95%
170
18.81%
170
20.31%
184
Vermont
Jul 1, 2004
19.10%
104
19.97%
108
20.50%
111
21.79%
118
What Happens as State Laws Liberalize?
Past Year Marijuana Use among Persons Aged 12 or Older Residing in States with
Legal Medical Marijuana Use Only, by State: Percentages and Estimated Numbers
(in Thousands), Annual Averages Based on 2012-2013, 2013-2014, 2014-2015, and
2015-2016 NSDUHs
Range: 11-21.8%

9
State
Effective Date 2012-13
Percentages
2012-13
Numbers
2013-14
Percentages
2013-14
Numbers
2014-15
Percentages
2014-15
Numbers
2015-16
Percentages
2015-16
Numbers
Alaska
Feb 24, 2015 19.69% 114 19.60% 114 21.92% 127 23.00% 134
California
Nov 9, 2016
(revised penalties) 13.89% 4,384 14.49% 4,633 15.25% 4,936 16.23% 5,296
Colorado
Dec 10, 2012
(revised penalties);
Jan 1, 2014
(commercial sales) 18.92% 814 20.74% 909 23.09% 1,033 23.12% 1,057
District of
Columbia
Feb 26, 2015 21.02% 116 21.70% 121 23.51% 134 24.68% 143
Maine
Jan 30, 2017
(grow and possess) 16.24% 186 19.55% 224 19.69% 227 19.81% 228
Massachusetts
Dec 15, 2016 15.57% 885 17.23% 989 18.26% 1,058 18.64% 1,088
Nevada
Jan 1, 2017 14.10% 324 13.01% 304 12.95% 309 13.13% 319
Oregon
Mar 29, 2016 19.03% 630 19.39% 649 19.42% 659 22.70% 783
Washington
Dec 6, 2012 17.48% 1,008 18.92% 1,105 17.49% 1,037 18.93% 1,140
What Happens as State Laws Liberalize?
Past Year Marijuana Use among Persons Aged 12 or Older Residing in States with Legal
Medical and Recreational Marijuana Use, by State: Percentages and Estimated Numbers
(in Thousands), Annual Averages Based on 2012-2013, 2013-2014, 2014-2015, and
2015-2016 NSDUHs
Range: 13-25%

10
Illicit Drug Use Impacts Millions: Marijuana Most Widely Used Drug
20.1
MILLION
People aged 12 or
older had a
substance use
disorder
0.3%
0.6%
0.6%
1.9%
2.2%
6.6%
15.0%
Heroin
Methamphetamines
Inhalants
Hallucinogens
Cocaine
Psychotherapeutic Drugs
Marijuana
40.9 MILLION
18.1 MILLION
5.9 MILLION
5.1 MILLION
1.6 MILLION
1.8 MILLION
886,000
0%
2%
4%
8%
12%
14%
10%
6%
16%
Prescription opioids, sedatives,
tranquilizers, stimulants
PAST YEAR, 2017, 12+

11
How did we get to where we are and
what does the data tell us about
ongoing risks?

12
Young Adult Perceptions of Great Risk of Harm From Substance Use
See table 3.1 in the 2016 and 2017 NSDUH detailed tables for additional information.
PAST YEAR, 2015 - 2017, 18-25
+ Difference between this estimate and the 2017
estimate is statistically significant at the .05 level.

13
Perceptions of Great Risk of Harm From Substance Use Among Adults Aged
26 or Older
See table 3.1 in the 2016 and 2017 NSDUH detailed tables for additional information.
PAST YEAR, 2015 - 2017, 26+
+ Difference between this estimate and the 2017
estimate is statistically significant at the .05 level.
14
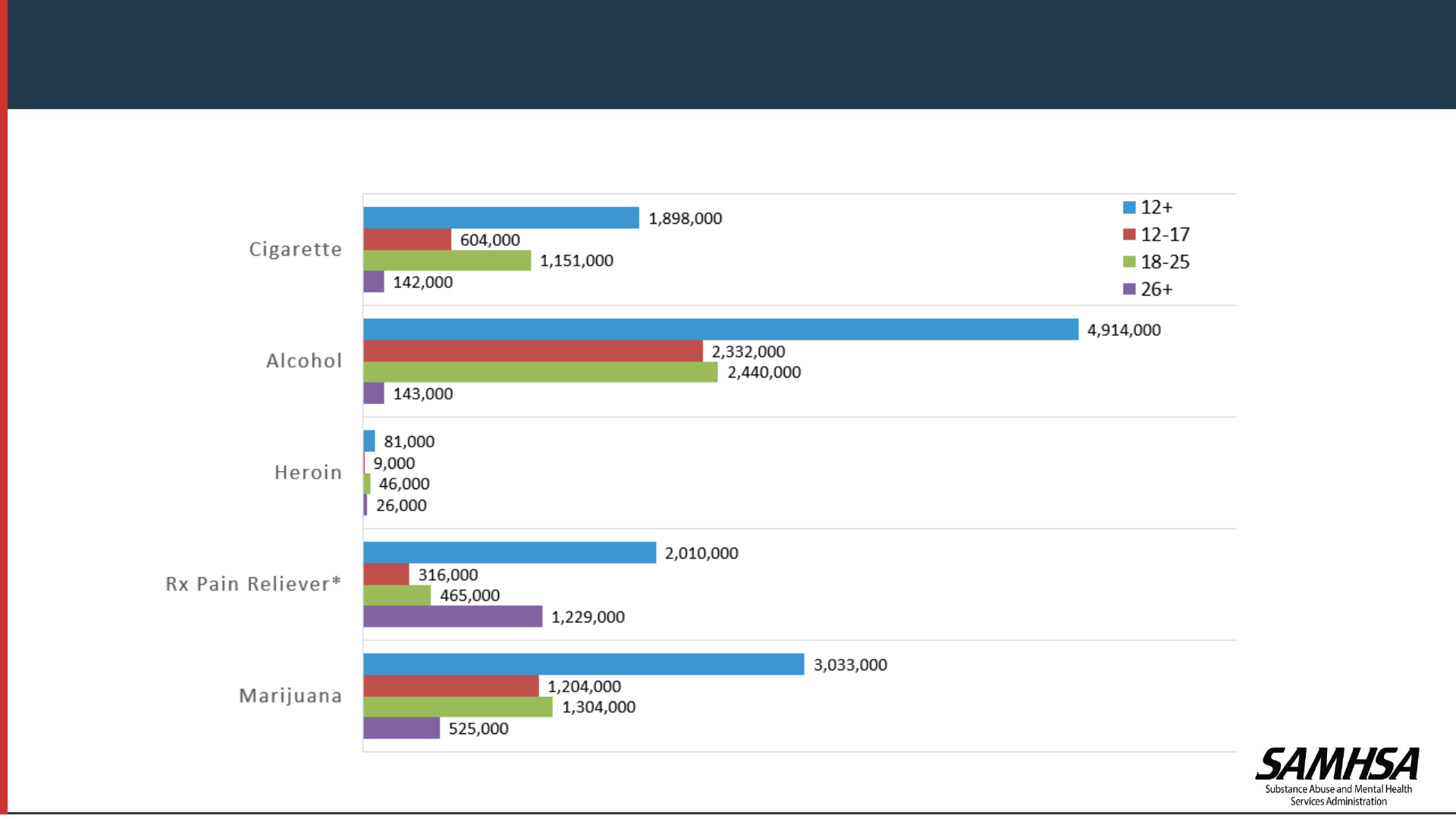
Past Year Initiates, Age Group & Substance
PAST YEAR, 2017, 12+
* Initiation of misuse

15
• Since 2007, past
year marijuana use
has increased 37%
• Frequent marijuana
use (using ≥ 200
days in the past
year) increased 37%
since 2002
• Nearly 1 in 3 people
using marijuana in
2016 reported using
≥ 200 days in the
past year
0
5
10
15
20
25
30
35
Past Year Marijuana Use Use of Marijuana 200 Days or More in
Past Year Among Those Reporting
Past Year Marijauna Use
Percent
2002
2003
2004
2005
2006
2007
2008
2009
2010
2011
2012
2013
2014
2015
2016
Source: Jones CM Analysis of the NSDUH 2002-2016 Public Use Files
Marijuana Use Is Increasing in the U.S.

16
Marijuana Use
PAST MONTH, 2015 - 2017, 12+
See figure 13 in the 2017 NSDUH Report for additional information.
+ Difference between this estimate and the 2017
estimate is statistically significant at the .05 level.

17
+ Difference between this
estimate and the 2017
estimate is statistically
significant at the .05 level.
Marijuana Use among Young Adults: Significant Increases in Women
PAST MONTH, 2015 - 2017, 18 - 25
Special analysis of the 2017 NSDUH Report.
+ Difference between this estimate and the 2017
estimate is statistically significant at the .05 level.

18
Substance Use in Past Month Among Pregnant Women
Special analysis of the 2017 NSDUH Report.
+ Difference between this estimate and the 2017
estimate is statistically significant at the .05 level.
PAST MONTH, 2015 - 2017, 15 - 44

19
Daily or Almost Daily Marijuana Use among Women by Pregnancy Status
PAST YEAR, 2015 - 2017, 15 - 44
Special analysis of the 2017 NSDUH Report.
+ Difference between this estimate and the 2017
estimate is statistically significant at the .05 level.

20
Why is this Data Important?
Marijuana and Pregnancy
May be associated with:
• Fetal growth restriction
• Stillbirth
• Preterm birth
May cause problems with neurological
development:
• Hyperactivity
• Poor cognitive function (Metz TD and Stickrath EH, 2015)

21
Co-Occurring Disorders: Youth Opioid Misuse, Heavy Alcohol Use, and
Major Depressive Episode (MDE) by Marijuana Use Status
Special analysis of the 2017 NSDUH Report.
+ Difference between this estimate and the
estimate youth with past year marijuana use is
statistically significant at the .05 level.
PAST YEAR/MONTH, 2017, 12 - 17

22
Co-Occurring Disorders: Young Adult Opioid Misuse, Heavy Alcohol Use,
and Major Depressive Episode by Marijuana Use Status
PAST YEAR/MONTH, 2017, 18 - 25
Special analysis of the 2017 NSDUH Report.
+ Difference between this estimate and the
estimate with past year marijuana use is
statistically significant at the .05 level.

23
Co-Occurring Disorders: Adult Opioid Misuse, Heavy Alcohol Use, and
Major Depressive Episode by Marijuana Use Status
PAST YEAR/MONTH, 2017, 26+
Special analysis of the 2017 NSDUH Report.
+ Difference between this estimate and the
estimate with past year marijuana use is
statistically significant at the .05 level.
24
Average Point Difference in IQ Score
(IQ at age 38
– IQ at age 13)
Intelligence:
PERSISTENT CANNABIS (MARIJUANA) USE DISORDER
LINKED TO SIGNIFICANT IQ DROP
BETWEEN CHILDHOOD AND MIDLIFE
Source: Meier MH et al., PNAS Early Edition 2012
Followed 1,037 individuals from birth to age 38.
Tested marijuana use and disorders at 18, 21, 26, 32 and 38 years of
age.
Tested for IQ at ages 13 and 38
-8
-6
-4
-2
0
2
Never Used Marijuana Cannabis Dependence in 1
Study Wave
Cannabis Dependence in 2
Study Waves
Cannabis Dependence in 3
Study Waves
All groups started with roughly
equivalent IQ scores at age 13
By age 38, those who were
diagnosed with cannabis
dependence in 3 study waves
(the most persistent
users of cannabis) had lost nearly
6 IQ points by the age of 38
There was a consistent dose-
response relationship across the
groups

25
Marijuana Use: Link to Prescription Pain Medication (Opioid) Abuse
Association of marijuana use with abuse of prescription pain medications and addiction
2.62
2.78
0
1
2
3
4
5
Risk of incident prescription
opioid misuse
Risk of incident prescription
opioid use disorder
Risk of subsequent prescription opioid
misuse and use disorder was increased
among people who reported marijuana use
5 years earlier

26
Marijuana-Associated Psychosis
Source: Andréasson et al Lancet, 1987.
0
1
2
10
<50
>50
30
20
10
0
Number of times marijuana taken
Cases per 1,000
4.5
1.6
0
1
2
3
4
5
6
7
8
9
Cannabis users by age
15 years
Cannabis users by age
18 years
Odds ratio
Risk of schizophrenia
increases as
marijuana use
increases
Higher risk of
schizophrenia-like
psychosis with younger age
of first marijuana use
Source: Arseneault et al BMJ, 2002

27
Drug Risks Associated with Marijuana Use Among U.S. Adults 18 and Older
*
* Result is not statistically significantly different
2.9
3.0
1.6
2.9
3.8
5.6
15.5
6.6
4.0
2.2
6.0
9.0
10.8
23.0
6.3
4.1
3.1
8.0
9.8
7.6
36.8
0.0
5.0
10.0
15.0
20.0
25.0
30.0
35.0
40.0
Increased Risk for Adverse Outcome
Increased Risk for Ever Using Marijuana (but no past year use) Compared
to Never Using Marijuana
Increased Risk for Past Year Marijuana Use Compared to Never Using
Marijuana
Increased Risk for Past Year Use of Marijuana 200 Days or More Compared
to Never Using Marijuana
Source: Jones CM Analysis of 2015-2016 NSDUH Public Use File Data

28
Mental Health and Social Risks of Marijuana Use Among U.S. Adults 18 and Older
Source: Jones CM Analysis of 2015-2016 NSDUH Public Use File
Data
* Result is not statistically significantly different
*
¥
¥
¥
1.6
1.4
1.1
2.5
1.2
2.0
1.5
1.2
2.1
1.2
2.2
1.7
1.4
2.4
1.3
0.0
0.5
1.0
1.5
2.0
2.5
3.0
Any mental illness Serious mental illness Unemployed Probation or parole Government assistance program
Increased Risk for Ever Using Marijuana (but no past year use) Compared to Never Using Marijuana
Increased Risk for Past Year Marijuana Use Compared to Never Using Marijuana
Increased Risk for Past Year Use of Marijuana 200 Days or More Compared to Never Using Marijuana
Increased Risk for Adverse Outcome

29
Adverse outcomes linked to marijuana use by youth:
Poor school performance and increased drop out rates
Chronic use in adolescence has been linked to decline in IQ that
may not recover with cessation (Meier et al. 2012)
Marijuana use in adolescence is associated with an increased risk
for later psychotic disorder in adulthood (D’Souza, et al. 2016)
Marijuana use linked to earlier onset of psychosis in youth known
to be at risk for schizophrenia (McHugh, et al. 2017)
Summary: Consequences of Marijuana Use
Acute, intoxicating effects of marijuana:
• Distorts perception; poor judgment and poor decision making
(e.g.: unprotected sex, driving while intoxicated)
• Impairment in balance and coordination (important to injury risk
in activities such as driving, sports)
• Difficulty with attention, concentration, and problem solving
• Difficulty with learning and memory (immediate and recall)

30
Marijuana Use: Health Consequences
• Significant numbers who try marijuana will become addicted
(Lopez-Quintero, et al. 2011)
• Higher overall rates of car crashes in states that have
legalized (WAPO, June 2017)
• Association of marijuana use with abuse of prescription pain
medications (Olfson et al. 2017)
Summary: Consequences of Marijuana Use

31
Is There Medical Use for Marijuana?
• Evidence for some medical value of some components
• CBD and seizure disorder (Dravet’s syndrome and Lennox-Gastaut syndrome)
• THC products for wasting illnesses and appetite production
• Medications must have undergone substantial research to answer critical
questions before getting to market and widespread use in humans:
• Isolation of single components; manufacture processes
• Delivery mechanism
• Pharmacokinetics/pharmacodynamics
• Dose-response relationships (e.g.: doubling a dose may or may not double
the effect)
• Therapeutic range
• Adverse events: what are they and how best to avoid/address should they
occur?
• These types of studies would be difficult for marijuana because there are so
many components
31

32
Where Do We Go From Here?
• Government has a responsibility to inform Americans of the risks of marijuana use
• People need to be able to make informed choices
• States should consider short and long term issues related to marijuana
• Tax revenue
• Societal costs
• Government costs
Major Issue to Consider: Marijuana has gotten ahead of regulation
• How do we define intoxication?
• What are the ‘legal limits’ of use (equivalent to BAC)
• How should marijuana sales centers be regulated (should we better control the opening of marijuana
sales locations?)
• Should warning labels be required on marijuana products?
• How do we assure that underage sales are not occurring? (as with tobacco products, for example)
• Should people be allowed to openly use in public?
• Should people be allowed to use and operate motor vehicles?
• What are the penalties?
33
New Stimulant Toxicity: Fentanyl-Contaminated Cocaine
Cocaine laced with fentanyl:
7% of cocaine seized in New England in 2017 was contaminated with fentanyl
Connecticut: deaths involving fentanyl-laced cocaine up 420% in last 3 years
Reported increases in deaths in NYC, PA, MA, NJ, OH, CA
https://www.ncadd.org/blogs/in-the-news/cocaine-laced-with-fentanyl-causing-growing-number-of-deaths
Why?
Poor quality control in packaging?
High Risk Groups:
Primary cocaine users
Opioid users may use cocaine to counteract sedation/intensify effect of opioid
• Underscores the need to warn the public and provide treatment for cocaine use disorders
• Epidemic is not just about opioid addiction
Cocaine users lack opioid tolerance: fentanyl overdose/death more likely
• Naloxone
• Discourage use alone
https://www.npr.org/sections/health-shots/2018/03/29/597717402/fentanyl-laced-cocaine-becoming-a-deadly-problem-among-drug-users

34
34
Kratom
• Kratom is a tropical tree (Mitragyna speciose) native to Southeast Asia, used
traditionally to combat fatigue and improve work productivity among farm
populations in Southeast Asia
• Has recently become popular as a novel psychoactive substance in Western
countries (Cinosi et al, 2015).
• FDA is concerned that kratom, which affects the same opioid brain receptors as
morphine, appears to have properties that expose users to the risks of addiction,
abuse, and dependence
• Currently, there are no FDA-approved uses for kratom, and the agency
has received concerning reports about its safety

35
35
• Kratom preparations contain varying amounts of several
phytochemicals, making their pharmacological and
toxicological evaluation unique and difficult.
• More than 20 alkaloids in kratom have been identified in
the laboratory.
• Mitragynine is classified as a kappa-opioid receptor agonist
and is roughly 13 times more potent than morphine.
• Mitragynine/OH-mitragynine thought to be responsible for
the opioid-like effects.
Kratom Extract Composition
Source: Cinosi E.; Martinotti; et all. Following “the Roots” of Kratom (Mitragyna speciosa): The Evolution of an Enhancer from a
Traditional Use to Increase Work and Productivity in Southeast Asia to a Recreational Psychoactive Drug in Western Countries; Biomed
Res Int. 2015; 2015: 968786
36
• Capsules
• Pills
• Extract
• Leaves
• Chewed
• Brewed as tea
• Smoked
Kratom: How Used

37
The effects of kratom in humans are dose-dependent:
• Small doses produce stimulatory effects resembling
the stimulant effect of drugs such as cocaine or
amphetamines.
• Larger dosages associated with sedative-narcotic,
pain reducing effects that resemble drugs such as
opiates.
• Regular kratom use is associated with addictive
disorders, as evidenced by craving and compulsive
use. Opioid withdrawal symptoms upon cessation.
Kratom: Effects
SOURCE: Prozialeck W. C., Jivan J. K., Andurkar S. V. Pharmacology of Kratom: an emerging botanical agent with stimulant, analgesic and opioid-
like effects. Journal of the American Osteopathic Association. 2012;112(12):792–799; Singh, 2014; Suwanlert, 1975; Ahmad and Aziz, 2012;
Vicknasingam et al., 2010; Singh et al., 2014

38
• An anonymous online survey was conducted in October 2016 of 10,000 current
kratom users through available social media and from the American Kratom
Association (https://speciosa.org/home/ )
• 8,049 respondents completed the survey.
• Findings:
• Kratom was primarily used by a middle-aged (31-50 years) males (56.91%) with
income $35,000 or higher with private insurance (61.31%).
• Kratom was used to self-treat pain (68%) and emotional or mental conditions
(66%) and for withdrawal symptoms associated with prescription opioid use.
• Subjects reported dose-dependent nausea and constipation with high doses
(5g) and with and frequent dosing (Q22 doses/wk).
Use of Kratom in the US
SOURCE: Grundmann O.; Patterns of kratom use and health impact in the USVresults from an online survey. Drug Alcohol Depend. 2017;
175(5):63Y70.

39
National Poison Data System - United States and Puerto Rico
January 2010–December 2015
Number of Kratom-related Reported Exposure Calls to Poison Centers in
the US
SOURCE: Anwar M, Law R, Schier J. Notes from the Field. Kratom (Mitragyna speciosa) Exposures Reported to Poison Centers — United
States, 2010–2015. MMWR Morb Mortal Wkly Rep 2016;65:748–749. DOI: http://dx.doi.org/10.15585/mmwr.mm6529a4

40
Fatal Overdoses Involving Kratom
States ME
NH
NM
OH PA RI
WV
WI
Total
Opioid overdose
deaths
301 402 322
4,534
3,231
265 844
825
10,724
Deaths involving
kratom
4 2 1 3 8 1 5 1 25
Percent
involving
kratom
1.3%
0.5%
0.3%
0.07
%
0.25
%
0.4%
0.6%
0.1%
0.23%
Source: CDC SUDORS Overdose Death Data
From July 2016 to June 2017, 25 fatal overdoses involving
kratom across 8 CDC SUDORS states were identified
Caution: testing of kratom is not uniform thus these numbers are underestimates
In 2017, the Food and Drug
Administration (FDA) began
issuing a series of warnings
about kratom and has now
identified at least 44 deaths
related to its use.
Most kratom associated deaths
appeared to have resulted from
adulterated products or taking
kratom along with other potent
substances.

41
• Kratom has gained popularity for its euphoric effects and is being popularized as a
safe herbal product capable of giving a “legal” high (Swogger et al., 2015), and as an
alternative to other sedative and stimulant type drugs (Warner et al., 2016).
• Reports of physical dependence on kratom in Western nations emerge from case
reports from the UK (Boyer et al., 2008, McWhirter and Morris, 2010), Germany (Kapp et al., 2011) and the
US (Dorman et al., 2014, Nelsen et al., 2010, Forrester, 2013, Sheleg and Collins, 2011).
• It can be surmised that given the large and growing number of internet purchase
sites for kratom (cited in Cinosi et al., 2015), addiction to kratom is also likely to be growing
in the Western countries.
• No treatment specific for kratom addiction available
• One case of NAS in an infant whose mother was a kratom user and who responded
to opioid treatment.
Kratom Concerns

42
Kratom is restricted or illegal in:
Australia Lithuania Romania
Denmark Myanmar South Korea
Finland Malaysia Sweden
Israel Poland Thailand
United Kingdom
International Status of Kratom
Scheduling under consideration in U.S.
On November 14, 2017, the FDA issued a public health advisory related to
mounting concerns regarding the risks associated with kratom and reported
deaths with use.

43
• Kratom is a recognized emerging public health threat (MMWR. July 29, 2016;65(29):748Y749)
• People need to understand that ‘‘legal’’ and ‘‘available’’ are not the same as
‘‘safe.’’
• In the West, kratom has been valued for its analgesic effects and to aid in
managing opioid withdrawal. However, some of these individual attempts
have resulted in cases of toxicity and fatalities.
• Physicians should be aware of these herbal supplements and potential
toxicity or withdrawal effects in patients including in newborns which cannot
be picked up by the standard toxicology screen (Davidson et al, 2018).
• Preventionists should be aware of this drug and work with their communities
raising awareness, providing education about effects and risks.
Conclusions
44
E-cigarettes
Vaping in the US: Trends and Effects

45
45
Cigarette Smoking Continues to Decline
Source: Adult cigarette smoking prevalence data are from the National Health Interview Survey (NHIS).
High school cigarette smoking prevalence data are from the National Youth Risk Behavior Survey.
0
5
10
15
20
25
30
35
40
1998 1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017
Cigarette
smoking prevalence
Adults 18+ High School Students
15.5% of adults are current smokers
7.6% of youth are current smokers

46
46
E-Cigarette Use on the Rise: Adult Ever Use of E-Cigarettes by Cigarette
Smoking Status – US, 2010-2017
Source: CDC. Styles Survey. 2010-2017
9.8
21.2
31.2
36.5
50.3
53.5
44.9
46.7
2.5
7.4
5.7
9.6
14.7
16.3
17.8
19.3
1.3
1.3
2.3
1.2
4.7
5.9
6.7
6.1
0
10
20
30
40
50
60
2010 2011 2012 2013 2014 2015 2016 2017
Percentage (%)
Year
Current Cigarette Smoker
Former Cigarette Smoker
Never Cigarette Smoker

47
47
Cigarette Smoking Status Among Current
Adult E-Cigarette Users, by Age Group
Source: QuickStats: Cigarette Smoking Status Among Current Adult E-cigarette Users, by Age Group —
National Health Interview Survey, United States, 2015. MMWR Morb Mortal Wkly Rep 2016;65:1177.

48
48
Current E-cigarette Use Among U.S. Adults, BRFSS, 2017
2.3% – 3.7%
3.8% – 4.2%
4.3% – 4.7%
4.8% – 7.1%
Current e-cigarette users: Persons who reported using
e-cigarettes or some other electronic “vaping” product
“some days” or “every day”

49
49
Youth E-cigarette Use: Infographic from CDC’s MMWR
Source: Cullen KA, Ambrose BK, Gentzke AS, Apelberg BJ, Jamal A, King BA. Notes from the Field:
Use of Electronic Cigarettes and Any Tobacco Product Among Middle and High School Students —
United States, 2011–2018. MMWR Morb Mortal Wkly Rep 2018;67:1276–1277.

50
50
Current Use of E-cigarettes and Any Tobacco Product Among Middle and
High School Students— NYTS, US, 2011–2018
Source: Cullen KA, Ambrose BK, Gentzke AS, Apelberg BJ, Jamal A, King BA. Notes from the Field: Use of Electronic Cigarettes and Any Tobacco
Product Among Middle and High School Students — United States, 2011–2018. MMWR Morb Mortal Wkly Rep 2018;67:1276–1277.

51
51
Adverse Health Effects of Nicotine
• Nicotine exposure during adolescence can result in addiction.
• Nicotine can harm the developing adolescent brain.
• Nicotine delivered by e-cigarettes during pregnancy can result
in multiple adverse consequences, including sudden infant
death syndrome, and could result in altered corpus callosum,
deficits in auditory processing, and obesity.
• Ingestion of e-cigarette liquids containing nicotine can cause
acute toxicity and possibly death if the contents of refill
cartridges or bottles containing nicotine are consumed.
Source: U.S. Department of Health and Human Services. E-Cigarette Use Among Youth and Young
Adults. A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human
Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention
and Health Promotion, Office on Smoking and Health, 2016.

52
52
E-cigarette Adverse Health Effects
• E-cigarettes expose users to several chemicals, in addition to
nicotine: heavy metals (chromium, lead, manganese, nickel and
zinc), arsenic, volatile organic compounds (propylene glycol or
glycerol), all known to have adverse health effects.
• The health effects and potentially harmful effects of doses of
heated and aerosolized constituents of e-cigarette liquids,
including solvents, flavorants, and toxicants, are not completely
understood.
• E-cigarettes can also be used to deliver other drugs, including
marijuana. In 2016, one-third of U.S. middle and high school
students who ever used e-cigarettes had used marijuana in e-
cigarettes.
Sources (Bullets 1-2): U.S. Department of Health and Human Services. E-Cigarette Use Among Youth
and Young Adults. A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and
Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease
Prevention and Health Promotion, Office on Smoking and Health, 2016.
Bullet 3: Trivers KF, Phillips E, Gentzke AS, Tynan MA, Neff LJ. Prevalence of Cannabis Use in
Electronic Cigarettes Among US Youth. JAMA pediatrics. 2018;172(11):1097-1099.

53
53
• Marijuana:
• Continue NSDUH and DAWN data collection related to marijuana
• Provide education/training materials oriented to providers and to the public
related to marijuana risks
• Specific materials aimed at special populations e.g.: pregnant women, youth
• Assist in identification of hazardous use and use disorders with SBIRT
• Fund prevention, treatment and recovery services in states/communities
• Kratom
• Education for healthcare providers and the public on kratom properties/adverse effects
• PSAs
• E-cigarettes/vaping
• Add NSDUH questions to better understand epidemiology
• Education for healthcare professionals and public, PSAs
• Continue to speak out on known risks and accumulating evidence for adverse
effects of marijuana, kratom, and e-cigarettes/nicotine
SAMHSA Actions in coming year


55
55
Kratom:
Cinosi E.; Martinotti; et al. Following “the Roots” of Kratom (Mitragyna speciosa): The Evolution of an Enhancer from
a Traditional Use to Increase Work and Productivity in Southeast Asia to a Recreational Psychoactive Drug in Western
Countries; Biomed Res Int. 2015; 2015: 968786.
https://www.fda.gov/NewsEvents/PublicHealthFocus/ucm584952.htm

56
56
The Surgeon General's Warning on Marijuana
The Surgeon General of the Public Health Service has issued the following warning on marijuana:
Marijuana use is a major public health problem in the United States. In the past 20 years, its' use has increased 30-fold; it estimated that more than a quarter of the
American population has used it. The age at which persons first use marijuana has decreased gradually to the junior high school years. Until recently, nearly 11% of
high school seniors used it, and although that figure has declined to 7%, its daily use still exceeds that of alcohol; more high school seniors use marijuana than smoke
cigarettes. In a recent study, 32% of those surveyed had used marijuana during the previous 30 days, while 25% had smoked tobacco.
On March 24, 1982, the Department of Health and Human Services submitted to Congress a report reviewing the consequences of marijuana use. Marijuana and
Health, 1982, ninth in a series, is primarily based on two recently conducted, comprehensive, scientific reviews by the Institute of Medicine of the National Academy
of Sciences, the Canadian Addiction Research Foundation, and the World Health Organization (WHO).
Both independent reviews corroborate the Public Health Service's findings of health hazards associated with marijuana use: Acute intoxication with marijuana
interferes with many aspects of mental functioning and has serious, acute effects on perception and skilled performance, such as driving and other complex tasks
involving judgement or fine motor skills.
Among the known or suspected chronic effects of marijuana are:
short-term memory impairment and slowness of learning.
impaired lung function similar to that found in cigarette smokers. Indications are that more serious effects, such as cancer and other lung disease, follow extended use.
decreased sperm count and sperm motility.
interference with ovulation and pre-natal development.
impaired immune response.
possible adverse effects on heart function.
by-products of marijuana remaining in body fat for several weeks, with unknown consequences. The storage of these by-products increases the possiblilties for
chronic, as well as residual, effects on performance, even after the acute reaction to the drug has worn off. Of special concern are the long-term developmental
effects in children and adolescents, who are particularly vulnerable to the drug's behavioral and psychological effects. The "amotivational syndrome," characterized
by a pattern of energy loss, diminished school performance, harmed parental relationships, and other behavorial disruptions, has been associated with prolonged
marijuana use by young persons. Although more research is required, recent national surveys report that 40% of heavy users experience some or all of those symptoms.
The Public Health Service concludes that marijuana has a broad range of psychological and biological effects, many of which are dangerous and
harmful to health, and it supports the major conclusion of the National Academy of Sciences' Institute of Medicine.
