
1
Final Report
NATIONAL INSTITUTES OF HEALTH
Pathways to Prevention Workshop:
The Role of Opioids in the Treatment of Chronic Pain
September 29–30, 2014
EXECUTIVE SUMMARY
The National Institutes of Health (NIH) workshop is co-sponsored by the NIH Office of Disease Prevention (ODP),
the NIH Pain Consortium, the National Institute on Drug Abuse, and the National Institute of Neurological
Disorders and Stroke. A multidisciplinary Working Group developed the workshop agenda, and an evidence report
was prepared by an Evidence-based Practice Center through a contract with the Agency for Healthcare Research
and Quality to facilitate the workshop discussion. During the 1½-day workshop, invited experts discussed the body
of evidence, and attendees had opportunities to provide comments during open discussion periods. After weighing
evidence from the evidence report, expert presentations, and public comments, an unbiased, independent panel
prepared this draft report, which identifies research gaps and future research priorities. This draft report was
posted on the ODP website and public comments were accepted for 2 weeks. The final report was then released to
coincide with publication in a peer-review journal.
Introduction
Chronic pain affects an estimated 100 million Americans, or one-third of the U.S. population,
although estimates vary depending upon how pain is defined and assessed. Approximately 25
million people experience moderate to severe chronic pain with significant pain-related activity
limitations and diminished quality of life. In addition to the burden of suffering, pain is the
primary reason Americans are on disability. The societal costs of chronic pain are estimated at
between $560 and $630 billion per year as a result of missed work days and medical expenses.
Although numerous treatments are available for treatment of chronic pain, an estimated 5 to 8
million Americans use opioids for long-term management of chronic pain. Moreover, workshop
speakers presented data from numerous sources that indicate a dramatic increase in opioid
prescriptions and use over the past 20 years. For example, the number of prescriptions for
2
opioids written for pain treatment in 1991 was 76 million; in 2011, this number reached
219 million. This striking increase in opioid prescriptions has paralleled the increase in opioid
overdoses and hospital admissions. In fact, hospital admissions for prescription painkillers have
increased more than fivefold in the last two decades. Yet, evidence also indicates that 40 to 70%
of people with chronic pain are not receiving proper medical treatment, with concerns for both
over- and under-treatment of chronic pain. Together, the prevalence of chronic pain and the
increasing use of opioids have created a “silent epidemic” of distress, disability, and danger to a
large percentage of Americans. The overriding question is whether we, as a nation, are currently
approaching chronic pain in the best possible manner that maximizes effectiveness and
minimizes harm. Several workshop speakers indicated that 80% of all opioid prescriptions
worldwide are written in the United States. This suggests, in part, that other countries have found
different treatments for chronic pain.
On September 29–30, 2014, the National Institutes of Health (NIH) convened a Pathways to
Prevention Workshop: The Role of Opioids in the Treatment of Chronic Pain. Specifically, the
workshop addressed four key questions:
1. What is the long-term effectiveness of opioids?
2. What are the safety and harms of opioids in patients with chronic pain?
3. What are the effects of different opioid management strategies?
4. What is the effectiveness of risk mitigation strategies for opioid treatment?
To answer these questions, the Pacific Northwest Evidence-based Practice Center, under contract
to the Agency for Healthcare Research and Quality, completed a review of the literature related
to these questions. The NIH conducted a 1½-day workshop featuring more than 20 speakers with
3
varied expertise and viewpoints. In addition, audience members expressed many other
experiences and views during the discussion periods.
Context
To understand the dilemma of opioids and chronic pain, the panel felt strongly that an
understanding of underlying contextual factors was crucial. Many workshop presentations
provided information about these contextual factors, including background on the scope of
patient pain and its treatment, the patient’s experience of pain and pain management, the current
public health issues associated with treatment of pain, and the historical context that underlies
the current use and overuse of opioids in the treatment of chronic pain.
As noted in the introduction, pain affects millions of Americans, and the societal costs are high.
For patients, chronic pain is often associated with psychological distress, social disruptions,
disability, and high medical expenses. In addition, with an increase in chronic pain, there has
been a simultaneous rise in opioid use. This use has been associated with pain relief, but also
with an increase in adverse outcomes (e.g., addiction, overdose, insufficient pain relief).
Given the rise in chronic pain syndromes and the poor outcomes associated with opioid
treatment, the panel felt it was fundamental to understand the patient’s perspective. At the
workshop, the panel heard from individuals struggling with chronic pain as well as advocates for
afflicted individuals. The burden of dealing with unremitting pain can be devastating to the
patient’s psychological well-being and can negatively affect a person’s ability to maintain
gainful employment or achieve meaningful advancement professionally. It can affect
relationships with spouses and significant others and may limit engagement with friends and
4
other social activities. The prospect of living a lifetime with pain may induce fear and
demoralization and can lead to diagnoses of anxiety and depression.
Coupled with psychological and social effects are the negative encounters that many individuals
with chronic pain experience with the health care system. Health care providers, often poorly
trained in management of chronic pain, are sometimes quick to label patients as “drug-seeking”
or as “addicts” who overestimate their pain. Some doctors “fire” patients for increasing their
dose or merely for continuing to voice concerns about their pain management. Some patients
have had similarly negative interactions with pharmacists. These experiences may make patients
feel stigmatized, or feel as if others view them as criminals. These experiences may heighten
fears that pain-relieving medications will be “taken away,” leaving the patient in chronic,
disabling pain. In addition, negative perceptions by clinicians can create a rupture in the
therapeutic alliance, which some studies have identified as impeding successful opioid treatment.
For example, cultural factors may influence the treatment a patient receives from health care
providers. White providers tend to underestimate the pain of black patients and perceive them to
be at higher risk than white patients for substance abuse.
Biased media reports on opioids also affect patients. Stories that focus on opioid misuse and
fatalities related to opioid overdose may increase anxiety and fear among some stable, treated
patients that their medications could be tapered or discontinued to “prevent addiction.” For
example, one workshop presentation indicated that a typical news story about opioids was likely
to exclude information about the legitimate prescription use of opioids for pain, focusing instead
on overdose, addiction, and criminal activity.
5
However, the panel also wanted to emphasize what was reflected in numerous presentations at
the workshop: Many patients have been compliant with their prescriptions, and some feel that
their pain is managed adequately to the point of satisfactory quality of life. However, many
patients using opioids long-term continue to have moderate to severe pain and diminished quality
of life. While many physicians feel that opioid treatment can be valuable for some patients,
physicians also feel that patient expectations for pain relief may be unrealistic and that long-term
opioid prescribing can complicate and impair their therapeutic alliance with the patient.
The patient perspective is incredibly important, and yet it is only one aspect of the problem.
Another equally important consideration is how prescription opioids used in the treatment of
chronic pain create public health problems. In other words, although some patients experience
substantial pain relief from prescription opioids and do not suffer adverse effects, these benefits
have to be weighed against problems caused by the vast number of opioids now prescribed.
According to the Centers for Disease Control and Prevention, there were approximately 17,000
overdose deaths involving opioids in 2011. From 2000 to 2010, the number of admissions for
addiction to prescription opioids increased more than four-fold, to over 160,000 per year.
Different age groups are affected differently. For example, in 2010, one out of eight deaths of
25- to 34-year-olds was opioid-related. There are also collateral deaths from those who have
been prescribed opioids. In a 3-year period (2003 to 2006), more than 9,000 children were
exposed to opioids; this figure is based on data from toxicology centers, and the actual number
may be higher. Of these, nearly all children ingested the opioid (99%), and the ingestion
occurred in the home (92%). A small number of children died (n=8), but 43 children suffered
major effects, and 214 suffered moderate effects. Neonatal narcotic withdrawal also has
6
increased, with an estimated 29,000 infants affected. Both short-term physiological problems as
well as long-term behavioral consequences result from this withdrawal.
There is some concern that opioids are now becoming gateway drugs for heroin use. For
example, one study found that among individuals with a heroin addiction in the 1960s, the most
common first opioid used (the entry drug into heroin) was heroin itself. However, by the year
2000, the most common entry drug to heroin use was a prescription opioid.
Speakers at the workshop expressed almost unanimous concern that physicians are unable to
distinguish among individuals who would use opioids for pain management and not develop
problems with misuse, those who would use them for pain management and then become
addicted, and those who request a prescription because of a primary substance use disorder. Only
a minority of those who use opioids for chronic pain become addicted. For example, in one study
of individuals treated for chronic pain, the addiction prevalence, depending on criteria, ranged
from about 14 to 19%.
Finally, there is a major public health concern that opioids are finding their way illicitly into the
public arena. The Substance Abuse and Mental Health Services Administration’s 2013 National
Survey on Drug Use and Health found that, among people age 12 and older abusing analgesics,
53% reported receiving them for free from a friend or relative. Only 23.8% received
prescriptions from one or more doctors.
Another key contextual factor the panel considered was a historical perspective. The panel
identified important historical factors related to approval by the U.S. Food and Drug
Administration (FDA) of opioid medications, introduction of new opioid medications
(particularly extended-release formulations), training of prescribers, and health system changes.
7
Different opioids have undergone varying levels of scrutiny by the FDA. All current, extended-
release opioids have been approved for chronic pain based on 12-week adequate and well-
controlled efficacy studies, although there are safety data for extended-release opioids for a year,
in most cases from open-label studies. A number of immediate-release opioids had been on the
market without prior approval; however, in recent years, all of them have received FDA approval
for acute pain.
The introduction of new opioid drugs on the market over the past decade, particularly those with
extended-release formulations, made them attractive to patients and clinicians who perceived
them as safe and effective. As indicated above, there were limited long-term studies on which to
base clinical decisions. Physicians have little training in how to manage chronic pain patients and
did not have to demonstrate knowledge in how to prescribe these medications.
As described below in “Challenges Within the Health Care System,” changes in the health care
system have provided perverse incentives for clinicians to prescribe opioids in the brief amount
of time they have with patients.
Of course, the historical and current context of opioid use and prescription is complicated by the
heterogeneity of the problem. There are many facets of heterogeneity: patients (e.g., age, gender,
race); the pain etiology (e.g., peripheral vs. central pain), diverse clinical presentations that
include various comorbidities; characteristics of the clinical setting (e.g., providers, payment
structures); and the available opioids for prescription (e.g., differential receptor affinities,
pharmacokinetics, potential for drug interactions).
Given these complexities, the panel struggled with striking a balance between two ethical
principles, beneficence and doing no harm, specifically between the clinically indicated
8
prescribing of opioids on the one hand and the desire to prevent inappropriate prescription abuse
and harmful outcomes on the other. These goals should not be mutually exclusive and, in fact,
approaches that attempt to achieve both goals simultaneously are essential to move the field of
chronic pain management forward. However, one of the central struggles the panel grappled with
in making recommendations is the dearth of empirical evidence to support the four key questions
addressed by the Evidence-based Practice Center (EPC) report. Thus, in order to formulate the
recommendations in this report, the panel synthesized both the evidence from the EPC report and
the workshop presentations that focused on clinical experience as well as on smaller trials and
cohort studies (e.g., non-randomized clinical trials).
Clinical Issues
Patient Assessment and Triage
Chronic pain is a complex clinical issue requiring an individualized, multifaceted approach.
Contributing to the complexity is the fact that chronic pain is not limited to a particular disease
state but rather spans a multitude of conditions, with varied etiologies and presentations. Yet,
traditionally, persons living with chronic pain are “lumped” into a single category, and treatment
approaches have been generalized with little evidence to support this practice. In addition,
although pain is a dynamic phenomenon, waxing and waning and changing in nature over time,
it is often viewed and managed with a static approach. For a number of reasons—including lack
of knowledge, practice settings, resource availability, and reimbursement structure—clinicians
are often ill-prepared to diagnose, appropriately assess, treat, and monitor patients with chronic
pain. Based on the evidence report and the workshop presentations, the panel has identified
several clinical management issues worthy of further discussion.
9
First, there must be recognition that patients’ manifestation of and response to pain is varied,
with genetic, cultural, and psychosocial factors all contributing to this variation. Evidence was
presented that clinicians’ response to patients with pain also differs, often due to preconceived
notions and biases based on racial, ethnic, and other sociodemographic stereotypes. The totality
of the data points to the need for an individualized, patient-centered approach based on a
biopsychosocial model as opposed to the biomedical model that is more commonly employed.
Treating pain and reducing suffering do not always equate, and many times patients and
clinicians have disparate ideas about successful outcomes. A more holistic approach to the
management of chronic pain, inclusive of the patients’ perspectives and desired outcomes,
should be the goal.
Patients, providers, and advocates all agree that there is a subset of patients for whom opioids are
an effective treatment method for their chronic pain, and that limiting or denying access to
opioids for these patients can be harmful. It appears that these patients can be safely monitored
using a structured approach, which includes optimization of opioid therapy, management of
adverse effects, and brief follow-up visits at regular intervals. Therefore, recommendations
regarding the clinical use of opioids should avoid disruptive and potentially harmful changes in
patients currently benefiting from this treatment.
This concept—that some patients benefit while others may receive no benefit or in fact may be
harmed—highlights the current challenges of appropriate patient selection. Data are lacking on
accuracy of and effectiveness of risk prediction instruments for identifying patients at highest
risk for the development of adverse outcomes (e.g., overdose, development of an opioid use
disorder). Yet, longitudinal studies have demonstrated risk factors (e.g., substance use disorders,
other comorbid psychiatric illnesses) that are more likely to be associated with these harmful
10
outcomes, and some studies show that patients who are at high risk are most likely to be
prescribed opioids (and higher doses of opioids). Ideally, patients with these risk factors would
be less likely to receive opioids or more likely to receive them in the context of a maximally
structured approach; however, studies of large clinical databases suggest the opposite.
Although the literature to support use of specific risk assessment tools is insufficient, the
consensus appears to be that the approach to the management of chronic pain should be
individualized, based on a comprehensive clinical assessment that is conducted with dignity and
respect and without value judgments or stigmatization of the patient. Based on the workshop
presentations, this initial evaluation would include an appraisal of pain intensity, functional
status, and quality of life, as well as an assessment of known risk factors for potential harm,
including history of substance use disorders and current substance use; presence of mood, stress,
or anxiety disorders; medical comorbidity; and concurrent use of medications with potential
drug-drug interactions. Additionally, there may be a role for the redesign of the electronic health
record to facilitate such an assessment, including integration of meaningful use criteria to
increase its adoption. Finally, incorporating the use of other clinical tools (e.g., prescription drug
monitoring programs) into this assessment, although not well studied, seems to be widely
supported. These factors also can be used to tailor the clinical approach, triaging those screening
at highest risk for harm to more structured and higher intensity monitoring approaches.
Treatment Options
Despite what is commonly done in current clinical practice, there appear to be few data to
support the long-term use of opioids for chronic pain management. Several workshop speakers
stressed the need to use treatment options that include a range of progressive approaches that
11
might initially include nonpharmacological options, such as physical therapy, behavioral therapy,
and/or proven complementary and alternative medicine approaches with demonstrated efficacy,
followed by pharmacological options, including non-opioid pharmacotherapies. The use of and
progression through these treatment modalities would be guided by the patient’s underlying
disease state, pain, and risk profile as well as clinical and functional status and progress.
However, according to a workshop speaker, lack of knowledge or limited availability of these
nonpharmacological modalities and the ready availability of pharmacological options and
associated reimbursement structure appear to steer clinicians towards the use of pharmacological
treatment and, more specifically, opioids.
One area of clinical importance the panel reviewed was the notion that pain type could influence
pain management. Data were presented on three distinct pain mechanisms: (1) peripheral
nociceptive—caused by tissue damage or inflammation, (2) peripheral neuropathic—damage or
dysfunction of peripheral nerves, and (3) centralized—characterized by a disturbance in the
processing of pain by the brain and spinal cord. Individuals with more peripheral/nociceptive
types of pain (e.g., acute pain due to injury, rheumatoid arthritis, cancer pain) may respond better
to opioid analgesics. In contrast, those with central pain syndromes—exemplified by
fibromyalgia, irritable bowel syndrome, temporal-mandibular joint disease and tension
headache—do not respond as well to opioids, as to centrally acting neuroactive compounds
(e.g., certain antidepressant medications, anticonvulsants). In particular, there is strong evidence
for non-opioid interventions in treatment of fibromyalgia, one of the most common conditions
presenting in primary care and pain clinics. In fact, the workshop presented interesting
preliminary evidence that if an initial evaluation for pain demonstrated even a few signs of
fibromyalgia (not meeting criteria for the full syndrome), the patient was at risk for poor
12
response to opioids and a worse long-term course of pain. In addition, speakers presented
evidence that nearly all chronic pain may have a centralized component, and it was suggested
that opioids may promote progression from acute nociceptive pain to chronic centralized pain.
However, several speakers and audience members cautioned against making blanket statements
about who is or is not likely to benefit from opioids, again highlighting the importance of
individualized patient assessment and management. The health care system would benefit from
additional research on these different mechanisms of pain and the optimal approaches for each,
including the value of individualized versus general approaches; identifying risk factors for
patients most likely to develop chronic pain after an acute or subacute pain syndrome, and ways
to mitigate or reduce the risk of transitioning to a chronic pain syndrome.
Clinical Management
There is little evidence to guide clinicians once they have made the decision to initiate opioids
for chronic pain therapy. Data on selection of specific agents based on opioid characteristics,
dosing strategies, and titration or tapering of opioids are insufficient to guide current clinical
practice. Discussed during the workshop was the concept of opioid rotation, in which a clinician
transitions a patient from an existing opioid regimen to another with the goal of improving
therapeutic outcomes. However, this approach has not been formally evaluated. The use of
equianalgesic tables (opioid conversion tables), which provide a list of equianalgesic doses of
various opioids to guide clinicians in determining doses for converting from one opioid to
another, was an issue of particular concern. The equianalgesic dose is a construct based on
estimates of relative opioid potency. A multitude of these opioid conversion tables are available
in both the peer-reviewed and non-peer-reviewed literature, and speakers noted the lack of
consistency between the tables. Many of the studies to determine these equianalgesic doses were
13
conducted in a sample of the study population and using data points that may not generalize to
patients presenting with chronic pain. The FDA has begun including data obtained from drug
trials and post-marketing studies in package inserts to aid clinicians in switching between
opioids, but it appears that many clinicians and pharmacists are not aware of this. Furthermore,
although three known classes of opioid receptors—mu (μ), kappa (κ), and delta (Δ)—have been
identified, multiple receptor subtypes within each of these classes can alter the effect of opioids
based on receptor subtype binding. This led to a discussion between workshop speakers of the
concept of incomplete cross-tolerance, in which providers may need to reduce the dose by 25 to
30% when converting between one opioid and another. Because of its longer half-life,
methadone may require a larger reduction (up to 90%); in fact, some speakers argued that
methadone should be excluded from these tables and suggested that the use of these tables may
have led to harm and should not be broadly used. There was a call for the development of
validated and patient-specific types of equianalgesic tables. It was also noted that the majority of
clinicians receive little to no education on use of these tables and on converting from one opioid
regimen to another; this should be a focus of future clinical education and clinical decision
support efforts.
Determination and Assessment of Outcomes
Several workshop speakers noted that patient assessments should be ongoing, including both
positive and negative outcomes. The range of items on such assessments might include pain
intensity and pain frequency, using both a short time reference as well as a longer timeframe for
comparative purposes, functional status including impact on functions of daily living; quality of
life; depression; anxiety; potential misuse or abuse of opioid medications; potential adverse
medical effects of opioids; and other measures that mimic those items obtained during the initial
14
clinical risk profiling. These frequent reassessments should guide maintenance or modification of
the current treatment regimen, and patients who are failing to meet the mutually agreed upon
clinical outcomes should be considered for discontinuation of opioid therapy. Although there
appeared to be consensus among speakers on the need for an “exit strategy,” there was less
consensus and very few data on how one should be implemented.
Adverse Events and Side Effects
In addition to the very real risk of development of an opioid use disorder, chronic administration
of opioids are associated with other adverse effects, including increased risk of falls and
fractures, hypogonadism with resultant sexual dysfunction, and, in at least two studies, increased
risk of myocardial infarction. These factors are important to the discussion of risks versus
benefits with patients, and realistic expectations regarding adverse events and side effects from
various treatment options may need to be explained to patients as well as relatives and home care
providers. New patient communication options may be of value for the patients or relatives to
discuss evolving concerns. Adverse events and side effects might be monitored regularly and
reported to the clinician between regularly scheduled visits using web or other communication
channels.
Risk Mitigation Strategies
As with much of the other data on opioid use for chronic pain, data are limited on the efficacy of
various risk mitigation strategies, including patient agreements, urine drug screening, and pill
counts. Some speakers expressed concern as to the effectiveness of patient agreements as few
data are available to support their use. However, the use of patient agreements and other care
support mechanisms might be an option as part of a comprehensive care management plan and
15
might be reinforced without the use of judgmental perspectives that could impact the relationship
between patient and provider. Naloxone, which traditionally has been used to reverse heroin
overdose, was highlighted as a potential risk mitigation strategy for patients who are prescribed
opioids for chronic pain. Guided by the premise that these are risky drugs as opposed to risky
patients, a workshop speaker suggested that naloxone might be provided to patients at the same
time as the original prescription for the opioid and that this might provide an opportunity for
additional patient education. Other speakers were more cautious about using this strategy for all
patients, yet were willing to consider that it might be explored from an individual patient risk-
benefit perspective.
Reducing the Next Generation of Chronic Opioid Users
Speakers stated that a multidisciplinary team approach that emulates the functions of a
multidisciplinary pain clinic would be desirable, given the prior history of success of such
models in treating the whole person and not merely the pain condition, which may not be a
simple, single entity. As noted above, different types of pain—peripheral nocioceptive,
peripheral neuropathic, and centralized pain—appear to have different profiles of response to
such treatments. Furthermore, the use of a more effective chronic disease care model may have
implications for reducing the potential of a new generation of chronic opioid users as the
continued first-line use of opioids for chronic pain treatment is generally suboptimal and has the
potential for addiction. Although the team composition may vary, members might include the
primary care provider, case or care managers, nurses, pharmacists, psychologists, psychiatrists,
social workers, and other pain specialists. However, the current health care financial incentives
do not appear to bode well for the re-initiation of such an approach (see below for a more
detailed discussion of this point). Finally, one simple approach the panel considered to decrease
16
the conversion of acute users to chronic users was to advise those prescribing opioid medications
for the treatment of acute pain (e.g., in the post-operative setting or for an injury) to prescribe
fewer pills to be taken over a shorter but clinically reasonable timeframe, as there is some
evidence that higher numbers of pills initially prescribed is related to risk of chronicity of use.
Challenges Within the Health Care System
A major influence on opioid prescribing is the evolution of the larger health care system and the
current state of primary care. The panel heard reports of major problems with the current health
care system, including:
Poor support for team-based care and specialty pain clinics
Over-burdened primary care providers
A lack of knowledge and decision support for chronic pain management
Financial misalignment favoring the use of medications
Fragmentation of care across different providers.
Pain is a multidimensional problem ranging from discomfort to agony and affecting physical,
emotional, and cognitive function as well as interpersonal relationships and social roles. As with
other chronic conditions, chronic pain management requires a more comprehensive
biopsychosocial model of care. Therefore, best practice models for chronic pain management
require a multidisciplinary approach similar to that recommended for other chronic complex
illnesses such as depression, dementia, eating disorders, or diabetes. Research demonstrates that
these conditions can be managed successfully using an interdisciplinary team-based approach to
care (e.g., medicine, psychology, nursing, pharmacy, social work). Early efforts to manage pain
in the late 20th century were based on similar effective models of interdisciplinary,
17
comprehensive, and individualized care. Unfortunately, as health care systems evolved and
increasingly implemented and maintained only those interventions that were declared to be
revenue-generating, team-based approaches to care for pain were largely abandoned.
Instead, management of chronic pain has been largely relegated to the primary care providers
working in health systems not designed or equipped for chronic pain management. Moreover,
expectations for primary care providers increasingly evolved towards productivity-based metrics,
with more tasks expected to be completed within a 10- to 20-minute office visit. Primary care
providers often face competing clinical priorities in patients with chronic pain because these
patients often have multi-morbidity and polypharmacy. Administrative responsibilities also
compete for the provider’s time. For example, growing requirements for documentation in the
electronic health record are consuming a larger portion of the office visit. Hence, time-
consuming but important clinical tasks—such as conducting multidimensional assessments,
developing personalized care plans, and counseling—have given way to care processes that can
be accomplished more quickly and with fewer resources, such as prescription writing and
referrals. In the case of pain management, which often takes substantial face-to-face time,
quicker alternatives have become the default option. As a result, providers often prescribe
opioids for pain even when, for any given patient, the pain might be treated more safely and
effectively with other modalities.
Primary care providers are charged with relieving pain as a professional obligation and a
fundamental goal of health care. However, these providers have often received little specific
training in chronic pain management or in the use and management of opioids. This may be
particularly true for those providers who were trained before newer formulations of opioids or
other alternatives were available. As the systematic review clearly reveals, these providers do not
18
have access to evidence-based dosing schedules, adjustment and switching rules, or tapering and
stopping rules to guide pain management. Even if primary care providers had the requisite
knowledge, skill, and intent, they often do not have access to the resources needed to manage
pain according to current guidelines. This is often true because alternative first-line treatment
strategies are not available. For example, most practices do not have access to experts in pain
management, including specialty pain clinics, or access to the alternative approaches to pain
management (e.g., physical therapy, cognitive and behavioral approaches, acupuncture, yoga,
meditation, other complementary and alternative medicine). Therefore, clinicians provide a
prescription for opioids because they and their patients feel it is the only or the most expedient
alternative. Once the decision to initiate opioids has been made, patients and providers lack
practical tools to monitor the outcomes of chronic pain management. For example, simple
monitoring tools (e.g., the Patient Health Questionnaire-9 for depression) assist in the diagnosis
and management of depression. Although widely available, pain rating scales alone are not
comprehensive enough to measure the adequacy of pain control on important dimensions such as
quality of life, function, and employment.
Payment structures and incentives also represent an important system-level facilitator for
excessive opioid use. Fee-for-service payment traditionally has not focused on the outcomes of
care valued by patients, but rather on the processes of medical care. Current reimbursement for
evaluation and management may be inadequate to reflect the time and team-based approaches
needed for integrative treatment. In some instances, payment structures place barriers to non-
opioid therapy, such as formulary restrictions that require evidence of failure of multiple
therapies before covering non-opioid alternatives (e.g., pregabalin). Other payment structures,
such as tiered coverage systems, keep non-opioid alternatives as second- or third-line options
19
rather than placing them more appropriately as first-line therapy. Other incentives encourage
prescribing opioids for several months at a time rather than for a shorter term or using lower-
volume prescriptions, because providers are instructed that patient and administrative costs are
lower, and that convenience is improved with longer-duration and larger-volume prescriptions.
The panel heard reports that this apparently benign incentive actually may lead to an increased
risk of opioid dependence or other adverse events, including harm through nonmedical uses.
Moreover, current reimbursement policies do not provide payment for some of the health
professionals who are needed to provide best-practice pain management (e.g., pharmacists, care
coordinators) and others may be reimbursed insufficiently (e.g., for only a single visit). In health
systems that are primarily fee-for-services, there may be incentives to generate short-term
revenue, whereas in capitated systems, where physicians receive a set amount for each enrolled
person per given period of time, there may be greater incentive to invest in upfront resources
(e.g., team-based care) if they can prevent downstream utilization (e.g., hospitalization). Given
the current vagaries of payment structures, perhaps it is not surprising that providers and patients
chose opioids more often than is clinically appropriate and more often than guidelines suggest.
Finally, fragmentation of care across multiple providers and sites of care often leads to patients
receiving prescriptions from multiple providers. This may lead not only to inappropriate
prescribing of opioids but also to inappropriate prescribing of unsafe combinations of drugs such
as opioids and benzodiazepines. Up to 25% of patients who have chronic pain receive their
medications in the emergency department, often effectively bypassing the primary care system.
Patients with chronic pain may see multiple specialists with relevant expertise in chronic pain
(e.g., neurologists, orthopedists, rheumatologists, psychiatrists), but these specialists may often
prescribe opioids without the knowledge of primary care providers. The specialists may focus on
20
pain in isolation and may not recognize or consider the patient’s comorbid conditions,
concomitant medications, or goals of care. Patients may actively “shop” for providers (within or
across health care systems or state lines) to find a provider who is willing to prescribe opioids.
The panel heard recommendations that there is a clear need to address these system-level
problems. Chief among these recommendations is the need to develop, evaluate, and implement
new models of care for chronic pain management. To accomplish this fundamental goal, research
must address health care aims and thus assess the costs and benefits to individuals and
populations. Moving to team-based care is unlikely to happen without restructuring
reimbursement systems, building patient-centered clinical information systems, expanding the
roles and responsibilities of health care professionals beyond the physician, and conducting new
basic research on which patients require which care in which settings.
Methods and Measurement
Reliable and valid clinical and research methods are essential as the medical field seeks to
understand best practices for chronic pain management. The EPC report found few long-term
(more than 1 year) studies of opioid treatment, and those identified in the literature were
typically of poor quality (see Summary of Findings Table). It is particularly difficult to
extrapolate from studies examining the effects of opioids on acute pain to chronic pain. The
panel identified methodological problems related to definitions, measurement, and research
design.
Definitions. One of the central definitional problems is defining acute versus chronic pain.
Various durations are used to define chronic pain, including “lasting more than 3 months” or
“lasting more than 6 months” or a time-based definition that is somewhat arbitrary. For example,
21
the American Academy of Pain Medicine suggests that chronic pain is best defined as pain that
does not remit in the expected amount of time. This is clearly an individualized pain assessment
and, although it may be useful to the individual clinician, does not provide a standard definition
that could be used for research purposes. The panel suggested that detectable changes in brain
function occur as pain moves from acute to chronic states; however, although this may provide a
more precise, functional definition of pain, it is unrealistic to expect that most research will
incorporate neuroimaging modalities.
Unclear definitions also impair the understanding of the types of pain that patients experience.
Many research studies compare patients with cancer-derived and non-cancer-derived pain. This
dichotomy is clearly insufficient, as neither cancer pain nor non-cancer pain are homogeneous, in
large part because individual differences in sensory processing and augmented pain affect
perception and reporting of pain. In other words, chronic pain is heterogeneous and complex. As
mentioned previously, one workshop presentation classified pain by its source: peripheral
(nociceptive) pain, peripheral (non-nociceptive) pain, and centralized. Although this rubric may
be useful for considerations of acute pain, chronic pain should not be partitioned into mutually
exclusive, discrete categories. This definitional problem affects diagnosis, treatment, and drug
regulation.
Finally, definitions are important when considering how to measure outcomes. Pain relief is a
major focus of treatment and research. However, it is difficult to quantify pain. The typically
used 0–10 pain scale provides an overall sense of pain, but not an assessment of individual
components related to pain. For example, recent work on the concept of “fibromyalgianess” (the
tendency to respond to illness and psychosocial stress with fatigue, widespread pain, general
increase in symptoms, and similar factors) identifies at least three components to chronic pain
22
that are important to measure: chronic pain or irritation in specific body regions, somatic
symptoms (e.g., fatigue, sleep, mood, memory), and sensitivity to sensory stimuli.
Measurement. Research also suffers from significant measurement problems. Risk screening
instruments would help clinicians implement better risk management strategies. Many speakers
at the workshop indicated that the field does not have good risk assessment tools. The EPC
report found that standardized tools lacked sufficient sensitivity and specificity to make them
clinically useful. In large part, the problem with screening is that it is not clear what risk factors
should be measured or whether it is feasible or sensible to screen for risk. Some speakers
indicated that clinicians should assume that all patients are at risk and not use valuable resources
(including clinician time) to screen.
Finally, patient outcomes (typically measured in an ongoing manner) are important. Numerous
speakers indicated that the primary goal for researchers and clinicians may be the reduction in
patient pain; however, patients may be more interested in improving quality of life, rather than
absolute pain reduction. Functional behavior related to pain also needs to be assessed.
The most important aspect of measuring patient outcomes is to acknowledge that they are
determined by multiple factors and therefore will need to be multidimensional in scope. Key
components of a thorough assessment of patient outcomes would include measures of pain,
psychopathology, quality of life, social factors (e.g., days worked), safety, and adverse outcomes.
Research Design. The panel reviewed several presentations related to study design. Based on
the EPC report, there is a clear need for well-designed longitudinal studies of effectiveness and
safety of long-term opioid use in the management of chronic pain; this is an immediate concern.
Such studies—both because of their length and the heterogeneity of factors to be accounted for—
23
would need to be large and would therefore be expensive. In addition, it is not clear from a
practical standpoint that patients with chronic pain would be willing to be randomized to
placebo, nonpharmacological treatments, or non-opioid medications. The workshop speakers
also proposed an alternative design, which involved accepting patients on long-term treatment
into a study and randomizing them to maintenance versus tapering of the opioid. However,
speakers noted similar practical issues around recruitment of individuals willing to have their
medication tapered. Pragmatic designs (with some flexibility in the treatments used) could help
bypass some of the challenges with conducting long-term randomized control trials.
With these limitations, workshop speakers suggested other types of longitudinal studies; for
example, an approach using a small cohort study was seen as a more feasible option. Also from a
feasibility standpoint, the use of the electronic health record to track pain and markers of
improvement as well as adverse outcomes and side effects may provide the best data on large
populations. In addition, some speakers noted limitations of FDA-mandated post-marketing
surveillance studies by pharmaceutical companies, but also saw this as an opportunity to gain
valuable information in this area.
Another design issue considered by the panel related to how best to account for heterogeneity
across patients, medications, and outcomes. Novel design and statistical approaches may be
needed to manage this complexity. For example, ecological designs that embrace heterogeneity
and help to understand diversity among patients and to identify key subgroups that may respond
differently to various treatments should be considered. This methodology often incorporates
novel statistical methods (e.g., latent class and profile analyses).
24
The panel also noted several specific research issues that merit further exploration. These include
the following:
1. Better understanding is needed of the window between effective dose and dose at which
side effects and adverse outcomes occur. These may include studies on how this window
is defined and assessed as well as the drug-related, genetic, and other patient-related
factors that might affect the targeted dose range.
2. In adverse outcomes research, it is important to determine how best to model more
immediate versus longer-term side effects based on the length of exposure to opioids. The
notion was presented that some poor outcomes (e.g., falls) might occur soon after
initiation of treatment, whereas others (e.g., hypogonadism) might be more associated
with longer-term exposure. Future studies will need to encompass this time-varying
aspect of certain adverse effects and poor outcomes.
3. Few studies have looked at genetic predictors of response and poor outcomes. There are
several promising areas and specific loci for genetic research in this area, including a
panel of gene variants related to cytochrome P450 metabolism (e.g., examining outcomes
in people who are slow, intermediate, or fast drug metabolizers), receptor target single
nucleotide polymorphisms (SNPs) as well as SNPs related to indirect modulation
(e.g., COMT, the gene coding for catechol-O-mehtyltransferase), the drug transporter
(e.g., ABCB1), and other polymorphisms derived from genome-wide association studies
(e.g., rs2952768).
Incorporation of biological approaches will be important to gaining a better understanding of the
etiology of chronic pain and the mechanisms involved in opiate response and poor outcomes.
25
Greater incorporation of functional imaging studies of pain, as well as clinical neuroscience
findings about salient psychological factors, hold promise for identifying patients who would
best respond to opioids versus other pharmacological or nonpharmacological modalities. Finally,
future studies might examine the utility of variables such as evoked pain sensitivity and
endogenous opioid activity.
Implementation science may be useful to address some of the clinical and practice issues. For
example, research on how to bring prescription monitoring systems into an electronic health
record may be particularly important. Finding ways to incorporate pharmacists and nurses in care
groups is also essential. A final example includes research into the cost-effectiveness of chronic
pain management teams, particularly given potential incentives for providing high quality of care
(e.g., pay for performance).
Complementary Efforts
As the medical community looks for ways to increase available options to control pain and
suffering, many complementary groups are at work. A 2011 report by the Institute of Medicine,
Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and
Research, has sparked efforts from various agencies to partner in addressing this issue.
The NIH Pain Consortium has selected 12 health professional schools as Centers of Excellence
in Pain Education (CoEPEs). The CoEPEs will act as hubs for the development, evaluation, and
distribution of pain management curriculum resources for medical, dental, nursing, and
pharmacy schools to enhance and improve how health care professionals are taught about pain
and its treatment.

26
The Stanford-NIH Pain Registry, now called the National Collaborative Health Outcomes
Information Registry (CHOIR) system, provides clinicians with valuable information regarding
treatment outcomes. This platform collects outcome data on large numbers of patients suffering
from chronic pain.
The Interagency Pain Research Coordinating Committee is a federal advisory committee charged
with coordination of all pain research efforts across all federal agencies. The ultimate goal of the
committee is to advance the fundamental understanding of pain and to improve pain-related
treatment strategies.
The FDA has recognized that extended-release and long-acting opioids are associated with
serious risks. The FDA is now requiring additional studies and clinical trials to assess these risks,
which include misuse, abuse, hyperalgesia, addiction, overdose, and death.
Many professional societies have taken a stance on the use of opioids for chronic pain. The
American Academy of Neurology recently published a position paper on non-cancer pain.
Initiatives such as the American Board of Internal Medicine Foundation’s “Choosing Wisely”
are underway.
Summary of EPC Report Findings
1. Effectiveness and comparative effectiveness
a. In patients with chronic pain, what is the effectiveness of long-term opioid therapy for long-
term (>1 year) outcomes related to pain, function, and quality of life?

27
Key Question
Strength of
Evidence
Conclusion
Pain, function, quality of life
Insufficient
No study of opioid therapy versus placebo
or no opioid therapy evaluated long-term
(>1 year) outcomes related to pain,
function, or quality of
life.
2. Harms and adverse events
a. In patients with chronic pain, what are the risks of opioids versus placebo or no opioid on
(1) opioid abuse, addiction, and related outcomes; (2) overdose; and (3) other harms?
Key Question
Strength of
Evidence
Conclusion
Abuse, addiction
Low
No randomized trial was evaluated. One
retrospective cohort study found prescribed
long-term opioid use was associated with
significantly increased risk of abuse or
dependence versus no opioid use.
Abuse, addiction
Insufficient
In 10 uncontrolled studies, estimates of
opioid abuse, addiction, and related
outcomes varied substantially even after
stratification by clinic
setting.
Overdose
Low
Current opioid use was associated with
increased risk of any overdose events
(adjusted HR 5.2, 95% CI 2.1 to 12) and
serious overdose events (adjusted HR 8.4,
95% CI 2.5 to 28) versus current nonuse.
Fractures
Low
Opioid use was associated with increased
risk of fracture in one cohort study
(adjusted HR 1.28, 95% CI 0.99 to 1.64)
and one case-control study (adjusted OR
1.27, 95% CI 1.21 to 1.33).
Myocardial infarction
Low
Current opioid use was associated with
increased risk of myocardial infarction
versus nonuse (adjusted OR 1.28, 95% CI
1.19 to 1.37 and incidence rate ratio 2.66,
95% CI 2.30 to 3.08).
Endocrine
Low
Long-term opioid use was associated with
increased risk of use of medications for
erectile dysfunction or testosterone
replacement versus nonuse (adjusted OR
1.5, 95% CI 1.1 to 1.9).

28
b. How do harms vary depending on the dose of opioids used?
Key Question
Strength of
Evidence
Conclusion
Abuse, addiction
Low
One retrospective cohort study found
higher doses of long-term opioid therapy
associated with increased risk of opioid
abuse or dependence than lower doses.
Compared to no opioid prescription, the
adjusted odds ratios were 15 (95% CI 10 to
21) for 1-36 MED/day, 29 (95% CI 20 to
41) for 36-120 MED/day, and 122 (95%
CI 73 to 205) for ≥120 MED/day.
Overdose
Low
Versus 1 to 19 mg MED/day, one cohort
study found an adjusted HR for an
overdose event of 1.44 (95% CI 0.57 to
3.62) for 20 to 49 mg MED/day and 11.18
(95% CI 4.80 to 26.03) at >100 mg
MED/day; one case-control study found an
adjusted OR for an opioid-related death of
1.32 (95% CI 0.94 to 1.84) for 20 to 49 mg
MED/day and 2.88 (95% CI 1.79 to 4.63)
at ≥200 mg MED/day.
Fracture
Low
Risk of fracture increased from an adjusted
HR of 1.20 (95% CI 0.92 to 1.56) at 1 to
<20 mg MED/day to 2.00 (95% CI 1.24 to
3.24) at ≥50 mg MED/day; the trend was
of borderline statistical significance.
Myocardial infarction
Low
Relative to a cumulative dose of 0 to 1350
mg MED over 90 days, the incidence rate
ratio for myocardial infarction for 1350 to
<2700 mg was 1.21 (95% CI 1.02 to 1.45),
for 2700 to <8100 mg was 1.42 (95% CI
1.21 to 1.67), for 8100 to <18,000 mg was
1.89 (95% CI 1.54 to 2.33), and for
>18,000 mg was 1.73 (95% CI 1.32 to
2.26).
Motor vehicle accidents
Low
No association was found between opioid
dose and risk of motor vehicle accidents.
Endocrine
Low
Relative to 0 to <20 mg MED/day, the
adjusted OR for daily opioid dose of ≥120
mg MED/day for use of medications for
erectile dysfunction or testosterone
replacement was 1.6 (95% CI 1.0 to 2.4).

29
3. Dosing strategies
a. In patients with chronic pain, what is the comparative effectiveness of different methods for
initiating and titrating opioids for outcomes and risk?
Key Question
Strength of
Evidence
Conclusion
Pain
Insufficient
Evidence from three trials on effects of
titration with immediate-release versus
sustained-release opioids reported
inconsistent results on outcomes related to
pain.
c. In patients with chronic pain, what is the comparative effectiveness of different long-acting
opioids on outcomes related to pain, function, and quality of life as well as the risk of overdose,
addiction, abuse, or misuse?
Key Question
Strength of
Evidence
Conclusion
Pain and function
Low
No difference was found between various
long-acting opioids.
Assessment of risk of overdose,
addiction, abuse, or misuse
Insufficient
No studies were designed to assess risk of
overdose, addiction, abuse, or misuse.
Overdose (as indicated by all-
cause mortality)
Low
One cohort study found methadone to be
associated with lower all-cause mortality
risk than sustained-release morphine in a
propensity-
adjusted analysis.
Abuse and related outcomes
Insufficient
One cohort study found some differences
between long-acting opioids in rates of
adverse outcomes related to abuse, but
outcomes were nonspecific for opioid-
related adverse events, precluding reliable
conclusions.

30
f. In patients with chronic pain on long-term opioid therapy, what is the comparative
effectiveness of dose escalation versus dose maintenance or use of dose thresholds on outcomes
related to pain, function, and quality of life?
Key Question
Strength of
Evidence
Conclusion
Pain, function, withdrawal due
to opioid misuse
Low
No difference was found between more
liberal dose escalation versus maintenance
of current doses in pain, function, or risk of
withdrawal due to opioid misuse, but there
was limited separation in opioid doses
between groups (52 vs. 40 mg MED/day at
the end of the trial).
h. In patients on long-term opioid therapy, what is the comparative effectiveness of different
strategies for treating acute exacerbations of chronic pain on outcomes related to pain, function,
and quality of life?
Key Question
Strength of
Evidence
Conclusion
Pain
Moderate
Two randomized trials found buccal
fentanyl more effective than placebo for
treating acute exacerbations of pain, and
three randomized trials found buccal
fentanyl or intranasal fentanyl more
effective than oral opioids for treating
acute exacerbations of pain in patients on
long-term opioid therapy.
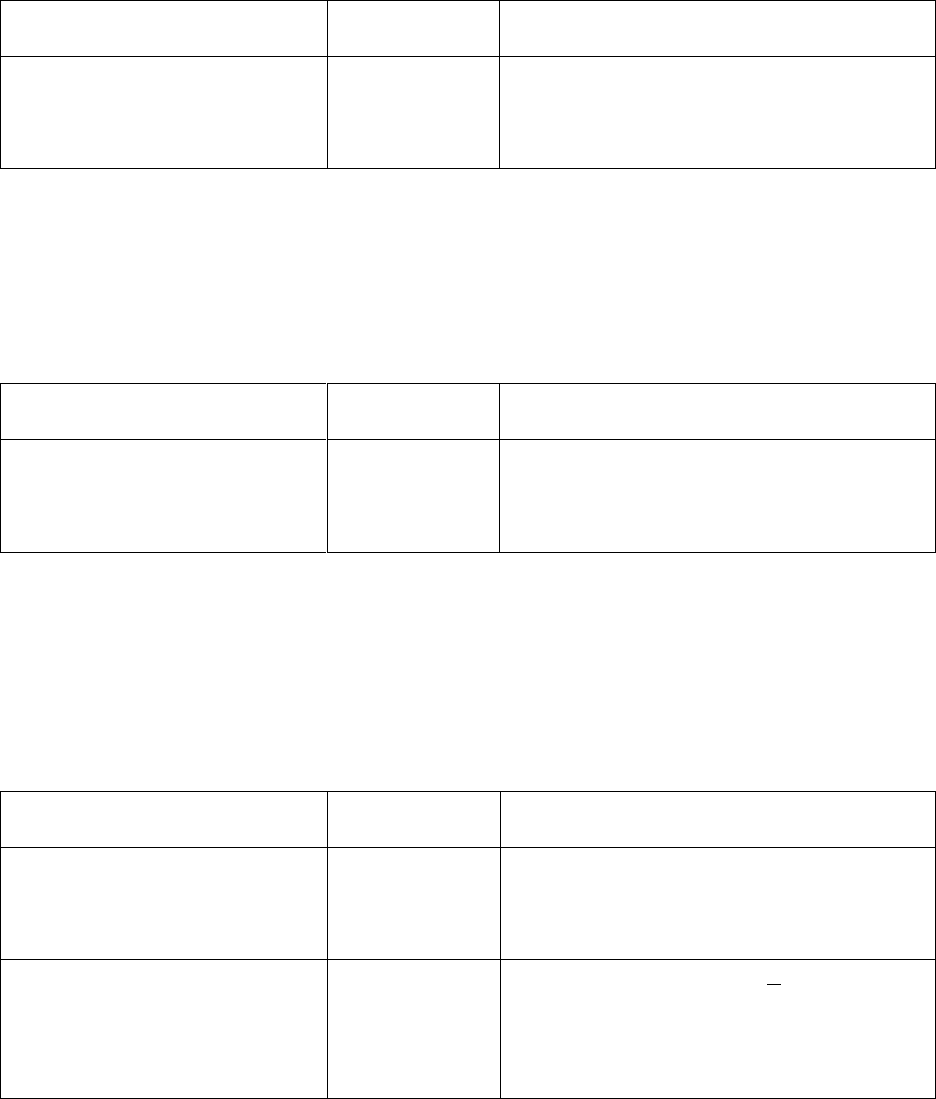
31
i. In patients on long-term opioid therapy, what are the effects of decreasing opioid doses or
tapering off opioids versus continuation of opioids on outcomes related to pain, function, quality
of life, and withdrawal?
Key Question
Strength of
Evidence
Conclusion
Pain, function
Insufficient
Abrupt cessation of morphine was
associated with increased pain and
decreased function
compared to
continuation of morphine.
j. In patients on long-term opioid therapy, what is the comparative effectiveness of different
tapering protocols and strategies on measures related to pain, function, quality of life, withdrawal
symptoms, and likelihood of opioid cessation?
Key Question
Strength of
Evidence
Conclusion
Opioid abstinence
Insufficient
No clear differences were found between
different methods for opioid
discontinuation or tapering in likelihood
of
opioid abstinence after 3 to 6 months.
4. Risk assessment and risk mitigation strategies
a. In patients with chronic pain being considered for long-term opioid therapy, what is the
accuracy of instruments for predicting risk of
opioid overdose, addiction, abuse, or misuse?
Key Question
Strength of
Evidence
Conclusion
Diagnostic accuracy: Opioid
Risk Tool
Insufficient
Based on a cutoff of >4, three studies (all
poor quality) reported very inconsistent
estimates of diagnostic accuracy,
precluding reliable conclusions.
Diagnostic accuracy: Screening
and Opioid Assessment for
Patients with Pain (SOAPP)
version 1
Low
Based on a cutoff score of >8, sensitivity
was 0.68 and specificity of 0.38 in one
study, for a PLR of 1.11 and NLR of 0.83.
Based on a cutoff score of >6, sensitivity
was 0.73 in one study.

32
b. In patients with chronic pain, what is the effectiveness of use of risk prediction instruments on
outcomes related to overdose,
addiction, abuse, or misuse?
Key Question
Strength of
Evidence
Conclusion
Outcomes related to abuse
Insufficient
No study evaluated the effectiveness of
risk prediction instruments for reducing
outcomes
related to overdose, addiction,
abuse, or misuse.
Abbreviations: CI=confidence interval, HR=hazard ratio, MED=morphine equivalent dose,
mg=milligrams, NLR=negative likelihood ratio, OR=odds ratio, PLR=positive likelihood ratio
As can be seen in the above table, the EPC found a paucity of studies on the long-term (more
than 1 year) outcomes of opioid treatment for chronic pain, and those identified in the literature
were typically of poor quality. Further, there are insufficient data to guide appropriate patient
assessment, opioid selection, dosing strategies, or risk mitigation. This underscores the need for
high-quality research that focuses on establishing the appropriateness of long-term opioid
treatment for the management of chronic pain. After listening to workshop speakers and
audience members and examining the limited availability of studies on long-term opioid
treatment, the panel makes the following recommendations:
1. Federal and non-federal agencies should sponsor research to identify which types of pain,
specific diseases, and patients are most likely to benefit and incur harm from opioids.
Such studies could use a range of study approaches and could include demographic,
psychological, socio-cultural, ecological, and biological characterizations of patients in
combinations with clear and accepted definitions of chronic pain and well-characterized
records for opioid and other pain medications.
33
2. Federal and non-federal agencies should sponsor the development and evaluation of
multidisciplinary pain interventions, including cost-benefit analyses and identification of
barriers to dissemination.
3. Federal and non-federal agencies should sponsor research to develop and validate
research measurement tools for identification of patient risk and outcomes (including
benefit and harm) related to long-term opioid use that can be adapted for clinical settings.
4. Electronic health record vendors and health systems should incorporate decision support
for pain management and facilitate export of clinical data to be combined with data from
other health systems to better identify patients who benefit from or are harmed by opioid
use.
5. Researchers on the effectiveness and harm of opioids should consider alternative designs
(e.g., N of 1 trials, qualitative studies, implementation science, secondary analysis, Phase
1 and 2 design) in addition to randomized clinical trials.
6. Federal and non-federal agencies should sponsor research on risk identification and
mitigation strategies, including drug monitoring, prior to widespread integration of these
into clinical care. This research should also assess how policy initiatives impact
patient/public health outcomes.
7. Federal and non-federal agencies and health care systems should sponsor research and
quality improvement efforts to facilitate evidence-based decision-making at every step of
the clinical decision process.
8. In the absence of definitive evidence, clinicians and health care systems should follow
current guidelines by professional societies about which patients and which types of pain
34
should be treated with opioids, and about how best to monitor patients and mitigate risk
for harm.
9. NIH or other federal agencies should sponsor conferences to promote harmonization of
guidelines of professional organizations to facilitate their implementation more
consistently in clinical care.
Summary
The rise in the number of Americans with chronic pain and the concurrent increase in the use of
opioids to treat this pain have created a situation where large numbers of Americans are
receiving suboptimal care. Patients who are in pain are often denied the most effective
comprehensive treatments; conversely, many patients are inappropriately prescribed medications
that may be ineffective and potentially harmful. At the root of the problem is the inadequate
knowledge about the best approaches to treat various types of pain, balancing the effectiveness
with the potential for harm, as well as a dysfunctional health care delivery system that
encourages clinicians to prescribe the easiest rather than the best approach for addressing pain.
The EPC report identified few studies that were able to answer the key questions, suggesting the
dire need for research on the effectiveness and safety of opioids as well as optimal management
and risk mitigation strategies. What was particularly striking to the panel was the realization that
there is insufficient evidence for every clinical decision that a provider needs to make regarding
the use of opioids for chronic pain, leaving the provider to rely on his or her own clinical
experience.
35
Because of the inherent difficulties of studying pain and the large number of patients already
receiving opioids, new research designs and analytic methods will be needed to adequately
answer the important clinical and research questions.
Until the needed research is conducted, health care delivery systems and clinicians must rely on
the existing evidence as well as guidelines issued by professional societies, which need to be
continually updated and harmonized to reflect recent research evidence and changes in expert
opinion. Systems of care must facilitate the implementation of these guidelines rather than
relying solely on individual clinicians, who are often overburdened and have insufficient
resources.
Clearly, there are some patients for whom opioids are the best treatment for their chronic pain.
However, for many more, there are likely to be more effective approaches. The challenge is to
identify the conditions in patients for which opioid use is most appropriate, the regimens that are
optimal, the alternatives for those who are unlikely to benefit from opioids, and the best
approach to ensuring that every patient’s individual needs are met by a patient-centered health
care system. For the more than 100 million Americans living with chronic pain, meeting this
challenge cannot wait.
National Institutes of Health Office of Disease Prevention
Pathways to Prevention Workshop:
The Role of Opioids in the Treatment of Chronic Pain
September 29 – 30, 2014
Panelists
36
David B. Reuben, M.D., Panel Chairperson
Chief
Division of Geriatrics
Director
Multicampus Program in Geriatric Medicine and
Gerontology
Professor of Medicine
Division of Geriatrics
David Geffen School of Medicine at the University of
California, Los Angeles
Anika A. H. Alvanzo, M.D., M.S.
Assistant Professor of Medicine
Medical Director
Substance Use Disorders Consultation
Service
Johns Hopkins University School of Medicine
Baltimore, Maryland
Takamaru Ashikaga, Ph.D.
Director
Biometry Facility
College of Medicine
University of Vermont
Burlington, Vermont
G. Anne Bogat, Ph.D.
Professor
Department of Psychology
Michigan State University
East Lansing, Michigan
Christopher M. Callahan, M.D.
Professor of Medicine
Cornelius and Yvonne Pettinga Professor
Indiana University (IU) School of Medicine
Director and Research Scientist
IU Center for Aging Research
Research Scientist
Regenstrief Institute, Inc.
Indianapolis, Indiana
Victoria Ruffing, R.N., CCRC
Director of Patient Education
Director of Nursing
Johns Hopkins University Arthritis Center
Johns Hopkins School of Medicine
Adjunct Faculty
Johns Hopkins University School of Nursing
Baltimore, Maryland
David C. Steffens, M.D., M.H.S.
Professor and Chair
Department of Psychiatry
University of Connecticut Health Center
Farmington, Connecticut
37
Speakers
Jane C. Ballantyne, M.D.
Professor, Retired
Department of Anesthesiology and Pain
Medicine
University of Washington
Philadelphia, Pennsylvania
Stephen Bruehl, Ph.D.
Professor
Department of Anesthesiology
Vanderbilt University School of Medicine
Nashville, Tennessee
Roger Chou, M.D., FACP
Director
Pacific Northwest Evidence-based Practice
Center
Professor of Medicine
Department of Medical Informatics &
Clinical Epidemiology
Oregon Health & Science University
Portland, Oregon
Myra Christopher, L.H.D. (Hon.)
Kathleen M. Foley Chair for Pain and
Palliative Care
Center for Practical Bioethics
Kansas City, Missouri
Daniel J. Clauw, M.D.
Professor of Anesthesiology, Medicine and
Psychiatry
Director
Chronic Pain and Fatigue Research Center
University of Michigan Medical Center
Ann Arbor, Michigan
Phillip O. Coffin, M.D., M.I.A.
Director of Substance Use Research
HIV Prevention Section
San Francisco Department of Public Health
San Francisco, California
Wilson M. Compton, M.D., M.P.E.
Deputy Director
National Institute on Drug Abuse
National Institutes of Health
Bethesda, Maryland
Edward C. Covington, M.D.
Director
Neurological Center for Pain
Cleveland Clinic
Cleveland, Ohio
Ricardo A. Cruciani, M.D., Ph.D.
Director
Center for Comprehensive Pain
Management and Palliative Care
Capital Institute for Neuroscience
Capital Health Medical Center
Hopewell, New Jersey
Tracy W. Gaudet, M.D.
Director
Office of Patient Centered Care and Cultural
Transformation
Veterans Health Administration
U.S. Department of Veterans Affairs
Washington, DC
Joseph T. Hanlon, Pharm.D., M.S.
Professor
Division of Geriatrics/Gerontology
Department of Medicine
University of Pittsburgh School of Medicine
Pittsburgh, Pennsylvania
38
Nathaniel P. Katz, M.D., M.S.
President and Chief Executive Officer
Analgesic Solutions
Adjunct Assistant Professor of Anesthesia
Tufts University School of Medicine
Natick, Massachusetts
Erin E. Krebs, M.D., M.P.H.
Core Investigator
Center for Chronic Disease Outcomes
Research
Medical Director
Women Veterans Comprehensive Health
Center
Minneapolis Veterans Administration
Associate Professor
Department of Medicine
University of Minnesota
Minneapolis, Minnesota
Story C. Landis, Ph.D.
Director
National Institute of Neurological Disorders
and Stroke
National Institutes of Health
Bethesda, Maryland
Jane C. Maxwell, Ph.D.
Senior Research Scientist
Addiction Research Institute
The University of Texas at Austin School of
Social Work
Austin, Texas
David M. Murray, Ph.D.
Associate Director for Prevention
Director
Office of Disease Prevention
Division of Program Coordination,
Planning, and Strategic Initiatives
Office of the Director
National Institutes of Health
Bethesda, Maryland
Steven D. Passik, Ph.D.
Vice President
Clinical Research and Advocacy
Millenium Research Institute
Millennium Laboratories
San Diego, California
Russell K. Portenoy, M.D.
Chief Medical Officer
Metropolitan Jewish Health System (MJHS)
Hospice and Palliative Care
Director
MJHS Institute for Innovation in Palliative
Care
Professor of Neurology
Albert Einstein College of Medicine
New York, New York
David B. Reuben, M.D.
Chief
Division of Geriatrics
Director
Multicampus Program in Geriatric Medicine
and Gerontology
Professor of Medicine
Division of Geriatrics
David Geffen School of Medicine at the
University of California, Los Angeles
Los Angeles, California
Wendy B. Smith, Ph.D., M.A., BCB
Senior Scientific Advisor for Research
Development and Outreach
Office of Behavioral and Social Sciences
Research
Office of the Director
National Institutes of Health
Bethesda, Maryland
David J. Tauben, M.D.
Clinical Associate Professor
Department of Medicine
Chief (Interim)
Division of Pain Medicine
Medical Director
Center for Pain Relief
University of Washington
Seattle, Washington
39
David A. Thomas, Ph.D.
Deputy Director
Division of Clinical Neurosciences and
Behavioral Research
National Institute on Drug Abuse
National Institutes of Health
Bethesda, Maryland
Judith Turner, Ph.D.
Professor
Department of Psychiatry and Behavioral
Sciences
University of Washington
Seattle, Washington
Nora D. Volkow, M.D.
Director
National Institute on Drug Abuse
National Institutes of Health
Bethesda, Maryland
Sharon Walsh, Ph.D.
Professor of Behavioral Sciences,
Psychiatry, Pharmacology, and
Pharmaceutical Sciences
Director
Center on Drug and Alcohol Research
University of Kentucky College of Medicine
Lexington, Kentucky
Working Group Planning Meeting for the National Institutes of Health (NIH) Pathways to
Prevention Workshop:
Effectiveness and Risks of Long-Term Opioid Treatment of Chronic Pain
August 28–29, 2013
Working Group
40
Chairpersons: David A. Thomas, Ph.D.
Deputy Director
Division of Clinical Neurosciences and Behavioral Research
National Institute on Drug Abuse
National Institutes of Health
Richard A. Denisco, M.D., Ph.D.
Services Research Branch
National Institute on Drug Abuse
National Institutes of Health
Caroline Acker, Ph.D.
Associate Professor and Head
Department of History
Carnegie Mellon University
Pittsburgh, Pennsylvania
Jane C. Ballantyne, M.D.
Professor, Retired
Department of Anesthesiology and Pain
Medicine
University of Washington
Philadelphia, Pennsylvania
Wen G. Chen, Ph.D.
Program Director
Sensory and Motor Disorders of Aging
Behavioral and Systems Neuroscience
Branch
Division of Neuroscience
National Institute on Aging
National Institutes of Health
Bethesda, Maryland
Edward C. Covington, M.D.
Director
Neurological Center for Pain
Cleveland Clinic
Cleveland, Ohio
Jody Engel, M.A., R.D.
Director of Communications
Office of Disease Prevention
Division of Program Coordination,
Planning, and Strategic Initiatives
Office of the Director
National Institutes of Health
Bethesda, Maryland
Roger B. Fillingim, Ph.D.
Professor
University of Florida College of Dentistry
Director
University of Florida Pain Research and
Intervention Center of Excellence
Gainesville, Florida
Joseph T. Hanlon, Pharm.D., M.S.
Professor of Medicine and
Health Scientist
Division of Geriatric Medicine
University of Pittsburgh
Pittsburgh, Pennsylvania
Working Group Planning Meeting for the National Institutes of Health (NIH) Pathways to
Prevention Workshop:
Effectiveness and Risks of Long-Term Opioid Treatment of Chronic Pain
August 28–29, 2013
Working Group
41
Christopher M. Jones, Pharm.D., M.P.H.
Lieutinent Commander, U.S. Public Health
Service
Team Lead
Prescription Drug Overdose Team
Division of Unintentional Injury Prevention
National Center for Injury Prevention and
Control
Centers for Disease Control and Prevention
Chamblee, Georgia
Margaret Kotz, D.O.
Director
Addiction Recovery Services
Department of Psychiatry-Adult
University Hospitals Case Medical Center
Professor, Psychiatry
Professor, Anesthesiology
Case Western Reserve University School of
Medicine
Cleveland, Ohio
Deborah Langer, M.P.H.
Senior Communications Advisor
Office of Disease Prevention
Division of Program Coordination,
Planning, and Strategic Initiatives
Office of the Director
National Institutes of Health
Bethesda, Maryland
Elinore F. McCance-Katz, M.D., Ph.D.
Chief Medical Officer
Substance Abuse and Mental Health
Services Administration
Rockville, Maryland
David M. Murray, Ph.D.
Associate Director for Prevention
Director
Office of Disease Prevention
Division of Program Coordination,
Planning, and Strategic Initiatives
Office of the Director
National Institutes of Health
Bethesda, Maryland
Elizabeth Neilson, M.S.N., M.P.H.
Senior Communications Advisor
Office of Disease Prevention
Division of Program Coordination,
Planning, and Strategic Initiatives
Office of the Director
National Institutes of Health
Bethesda, Maryland
Ann O’Mara, Ph.D., R.N., FAAN
Head
Palliative Care Research
Community Oncology and Prevention Trials
Research Group
Division of Cancer Prevention
National Cancer Institute
National Institutes of Health
Bethesda, Maryland
Wilma Peterman Cross, M.S.
Deputy Director
Office of Disease Prevention
Division of Program Coordination,
Planning, and Strategic Initiatives
Office of the Director
National Institutes of Health
Bethesda, maryland
Working Group Planning Meeting for the National Institutes of Health (NIH) Pathways to
Prevention Workshop:
Effectiveness and Risks of Long-Term Opioid Treatment of Chronic Pain
August 28–29, 2013
Working Group
42
Bob A. Rappaport, M.D.
Director
Division of Anesthesia, Analgesia, and
Addiction Products
Center for Drug Evaluation and Research
(CDER)
Food and Drug Administration
Silver Spring, Maryland
David B. Reuben, M.D.
Chief
Geriatric Division
Director
Multicampus Program in Geriatric Medicine
and Gerontology
Professor of Medicine
Division of Geriatrics
David Geffen School of Medicine at the
University of California, Los Angeles
Los Angeles, California
Wendy B. Smith, Ph.D., M.A., B.C.B.
Director for Research Development and
Outreach
Office of Behavioral and Social Sciences
Research
Office of the Director
National Institutes of Health
Bethesda, Maryland
Judith Turner, Ph.D.
Professor
Department of Psychiatry and Behavioral
Sciences
University of Washington
Seattle, Washington
Michael Von Korff, Sc.D.
Senior Investigator
Group Health Research Institute
Group Health Cooperative
Paris A. Watson
Senior Advisor
Office of Disease Prevention
Division of Program Coordination,
Planning, and Strategic Initiatives
Office of the Director
National Institutes of Health
Jessica Wu, Ph.D.
Health Scientist
Office of Disease Prevention
Division of Program Coordination,
Planning, and Strategic Initiatives
Office of the Director
National Institutes of Health
43
Workshop Sponsors
NIH Office of Disease Prevention
David M. Murray, Ph.D.
Director
NIH Pain Consortium
Story Landis, Ph.D.
Chair
National Institute on Drug Abuse
Nora D. Volkow, M.D.
Director
National Institute of Neurological Disorders and Stroke
Story Landis, Ph.D.
Director
