
Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
0
Month Year
Report
Title
Here
Maricopa CountyDivision Name
October 2023
Assessment of
Service Needs of
People Who Use
Drugs in Maricopa
County, AZ
Maricopa County
Department of Public Health
Division of Epidemiology

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
1
Table of Contents
Acknowledgements ............................................................................................................................ 2
Key Terms ............................................................................................................................................ 2
Executive Summary ............................................................................................................................. 2
Background .......................................................................................................................................... 6
Methods ............................................................................................................................................... 7
Results................................................................................................................................................ 11
Demographics ............................................................................................................................... 11
Housing .......................................................................................................................................... 13
Energy Insecurity ........................................................................................................................... 21
Drug Use and Harm Reduction Knowledge ................................................................................. 22
Substance Use Treatment ............................................................................................................ 31
Health Services and Basic Needs ................................................................................................ 40
Reproductive Health ...................................................................................................................... 43
Limitations ......................................................................................................................................... 44
References ......................................................................................................................................... 45
Appendix A. Participating Community Partners ............................................................................. 49
Appendix B. Survey Questionnaire ................................................................................................... 50
Appendix C. Interview Guide ............................................................................................................ 65
Appendix D. Informed Consent Form .............................................................................................. 73
Informed Consent Form for Participants .................................................................................... 73
Informed Consent Script for Data Collectors .............................................................................. 75
Appendix E. List of all Participant-Suggested Locations for Mobile Services ............................. 78
Appendix F. Survey Frequencies ...................................................................................................... 79

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
2
Acknowledgements
First and foremost, the Maricopa County Department of Public Health (MCDPH) would like to
thank the many people with lived experience who participated in this needs assessment and
generously shared their experiences with us.
This work would not have been possible without the support of many of our community
partners, who welcomed us into their spaces to allow for project recruitment and data
collection.
Additionally, MCDPH contracted with LeCroy and Milligan Associates, Inc. (LMA) on this
project and is thankful for their collaboration and hard work.
Key Terms
Below are some of the key terms and acronyms that will be used throughout this report.
Arizona Health Care Cost Containment System (AHCCCS): Arizona's Medicaid agency.
Chronic homelessness: While the U.S. Department of Housing and Urban Development has a
specific definition for people who are considered chronically homeless, in general, chronic
homelessness refers to homelessness (sheltered or unsheltered) that continues for longer
than 1 year, often longer, often while managing disabling physical or mental health conditions.
1
Energy insecurity: The inability of a household to meet its basic heating, cooling, and energy
needs over time.
Medication-Assisted Treatment (MAT): Medications used as treatment in combination with
other behavioral health therapy, to manage chronic substance misuse that is not limited to
drugs. The term MAT includes medications to treat Alcohol Use Disorder (AUD) as well as
medications to treat Opioid Use Disorder (OUD).
2
Medication for Opioid Use Disorder (MOUD): Medications used to help treat Opioid Use
Disorder. Three Food and Drug Administration (FDA)-approved medications are available to
treat Opioid Use Disorder—methadone, naltrexone, and buprenorphine. These medications can
be used during a person’s treatment and recovery in combination with other therapies. MOUD
can help reduce or eliminate withdrawal symptoms and cravings to opioid use, and blunt or
block the effects of illicit opioids which can be assistive to a person’s treatment for opioid use
disorder. Methadone and buprenorphine treatments have resulted in a reduced risk of
overdose death.
3

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
3
Naloxone/Narcan: Naloxone is the most common opioid overdose reversal medication.
Available as both an intramuscular injection and a nasal spray applicator, naloxone is widely
considered to be a life-saving medication and a key tool against the opioid overdose epidemic.
Narcan is the brand name for a naloxone nasal spray.
Opioid use disorder (OUD): A specific type of treatable, chronic substance use disorder, where
the primary substance is an opioid.
4
Polysubstance use: When a person takes more than one substance together, including when
two or more are taken together within a short timeframe, whether intentionally or
unintentionally. People may take multiple substances together for various reasons, including to
amplify or balance the effects of the substances. Unintentional polysubstance use occurs
when a substance is mixed or “cut” with another substance without a person’s knowledge (ex.
fentanyl in methamphetamine).
5
Stigma: Stigma is discrimination against an identifiable group of people. When people who use
drugs (PWUD) and people with a substance use disorder (SUD) are stigmatized, it can result in
fear or delay in seeking resources for harm reduction and recovery. Stigma can be seen in the
language used to describe PWUD and people with SUD, how people are treated in medical
settings, and a misguided viewpoint that drug use is a moral failing.
6
Substance use disorder (SUD): A treatable, chronic condition that is the result of changes to a
person’s brain and behavior, which leads to their inability to manage the use of substances
including alcohol, tobacco, or drugs — legal and illegal. SUD often impairs day-to-day tasks.
Even when a person is aware of changes to their judgment, behavior, or personality as a result
of SUD, they may not be able to stop using substances even if they want to.
7
Syringe service provider (SSP): An organization that offers sterile syringes to community
members to prevent bloodborne illnesses such as human immunodeficiency virus (HIV),
hepatitis C virus (HCV), and endocarditis. They also act as a community medical home to
people who may not feel comfortable seeking services from traditional medical providers.
Often these providers also offer healthcare screenings in-house, and healthcare referrals
through their own trusted networks.
8
Recovery: A continuum, guided by hope, with the goal of improved health and wellness. This
approach to substance use disorders is tailored to the strengths of an individual and their
environment, and can include MAT, MOUD, faith-based approaches, peer support, family
support, and clinical treatments. There is an emphasis in the recovery model on managing
setbacks and building resilience.
9
Unsheltered vs. Sheltered homelessness: People who are unsheltered and experiencing
homelessness are without a permanent home, and without temporary shelter from natural
elements (e.g., living in a tent on the street, sleeping in an underpass, camping in an arroyo).
People who are sheltered and experiencing homelessness are without a permanent home but

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
4
are currently housed in a temporary residence (this could be an emergency shelter system,
living temporarily in a hotel, couch surfing between friends and family, etc.).
Executive Summary
In 2022, manufacturer Johnson & Johnson and the “big three” pharmaceutical distributors
McKesson, AmerisourceBergen, and Cardinal Health finalized a $26 billion opioid settlement
agreement to resolve their liabilities in over 3,000 opioid crisis-related suits nationwide.
Through these settlements, Maricopa County will receive an estimated $80 million over 18
years, with additional funds expected as other settlements are finalized. To coordinate the
funding priorities for the opioid settlement funds, the Maricopa County Department of Public
Health (MCDPH) is developing a countywide substance use prevention and response strategic
plan. This report serves as an opportunity to ensure the voices of those intended to be served
by these funds, people who use drugs (PWUD), are reflected within the strategic planning
process.
Through the analysis of survey and interview data collected directly from PWUD, this report will
summarize key findings regarding PWUD’s unique experiences with service utilization, unmet
needs, and suggested service improvements. The findings from these data have led to 30
recommendations for consideration. These recommendations fall within six major categories:
housing, energy insecurity, drug use and harm reduction, substance use treatment, health
services and basic needs, and reproductive health. In addition to being considered within
opioid settlement fund planning, the recommendations proposed can generally inform the
improvement of services provided to PWUD by local governments, community-based
organizations, and providers.
The 30 recommendations are listed below and will be discussed in detail within their
respective sections of the report.
- Increase access to affordable housing
- Invest in eviction prevention and diversion programs
- Streamline housing navigation processes
- Reform the use of criminal records in housing applications
- Improve housing navigation for individuals exiting incarceration
- Remove barriers to replacement identification documents
- Address barriers to shelter use
Recommendations related to housing

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
5
- Increase cooling center awareness
- Increase cooling center accessibility
- Expand cooling center services
- Provide wrap-around services to people experiencing homelessness
- Prioritize substance use prevention among youth
- Expand naloxone education and access as well as overdose response education
- Increase awareness and distribution of safer use supplies
- Increase messaging for people who use drugs that are not opioids
- Explore legal pathways to create a safe use site to optimize harm reduction and reduce
opioid overdoses and overdose fatalities
- Increase education on fentanyl test strips (FTS)
- Incorporate harm reduction into areas where PWUD congregate
- Prioritize connections to low-barrier treatment, including through mobile services
- Improve access to take-home MOUD
- Reduce or supplement treatment costs and assist with issues related to health care
coverage
- Increase access to affordable housing
- Reduce stigma among healthcare providers
- Increase capacity of substance use treatment providers
- Increase the integration of peer support into treatment
- Share MOUD treatment success stories
- Invest in evidence-based treatment for non-opioid use and polysubstance use
Recommendations related to energy
insecurity
Recommendations related to drug use and
harm reduction
Recommendations related to substance use
treatment

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
6
- Increase services for basic health needs
- Expand the availability of mobile services
- Support pregnant persons who are treating SUD with MOUD by excluding them from
mandatory healthcare provider reporting requirements
Background
The Centers for Disease Control and Prevention (CDC) outlines three waves to characterize
how the opioid overdose epidemic has accommodated the changing opioid supply in the
United States.
10
The third wave, which began in 2013 and continues to characterize current
overdose patterns, is defined by an increase in overdose deaths that involve synthetic opioids,
such as illicitly manufactured fentanyl. From 2012–2021, Maricopa County’s overall opioid
overdose death rate increased from 5.2 to 28.8 per 100,000 residents.
11
During this time frame,
there was a 6000% increase in synthetic opioid overdose deaths in Maricopa County, indicating
a catastrophic public health concern. Opioids were involved in 73% of all drug overdose deaths
in Maricopa County in 2021. Maricopa County’s overall drug overdose death rate is also higher
than the national rate. In 2021, the national drug overdose death rate was 32.4 deaths per
100,000 residents
12
compared to 37.6 in Maricopa County.
13
In 2019, MCDPH conducted a vulnerability assessment of people who inject drugs (PWID),
collecting over 600 surveys from this community. The assessment was focused on the
healthcare experiences and harm reduction practices of PWID and revealed important
vulnerabilities unique to this population. The assessment also highlighted that service needs
may be unique to different sub-populations of PWUD.
After being awarded the Opioid Data to Action grant from the CDC in late 2019, MCDPH
decided to build upon this prior work. In 2021, MCDPH completed a feasibility assessment to
(1) ask key community partners about their perceptions of difficult-to-reach sub-populations
within the community of PWUD; and (2) to obtain feedback on the methodology and survey
questions that would be used to conduct a needs assessment among the identified
Recommendations related to health services
and basic needs
Recommendations related to reproductive
health

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
7
population. These Key Community Partners, representing a range of sectors and services, were
invited to share their experience.
Key Community Partners represented harm reduction organizations, mental health providers,
academia, public health, law enforcement, emergency services as well as people with lived
experience with drug use. Among the populations of PWUD in Maricopa County, the
populations the Key Community Partners were interested in learning more about people who
were adversely affected by extreme poverty and people experiencing homelessness (PEH).
Key Community Partners were specifically interested in these populations’ access to services,
unique barriers, and unmet needs. In addition, emphasis was placed on the importance of
collecting the nuance in the narrative of people who navigate the existing paths to services
such as substance use recovery and housing – where was there success, or where were there
unexpected challenges?
As MCDPH was wrapping up this feasibility assessment, a national $26 billion legal settlement
agreement was reached with the three largest pharmaceutical distributors: McKesson,
Cardinal Health, and AmerisourceBergen, and manufacturer Johnson & Johnson. As part of
these settlements, Maricopa County will receive an estimated $80 million over 18 years with
additional funds expected as other settlements are finalized.
To better direct these funds and define funding priorities, MCDPH has engaged in a substance
use strategic planning process that involves conducting two needs assessments that
complement one another:
1. An assessment focused on provider organizations’ experiences with PWUD, care
coordination, and regulations affecting OUD/SUD services.
2. An assessment of PWUD, with emphasis on the unique challenges of people
experiencing homelessness or unstable housing.
This report will focus on summarizing findings from the needs assessment of PWUD
(objective two). The purpose of the PWUD needs assessment is to create space in strategic
planning for the voices and experiences of PWUD in Maricopa County. These data were
collected with the goal of better-directing resources to actively meet the needs identified by
the people surveyed and to better inform service provision.
Methods
MCDPH contracted with LeCroy, Milligan & Associates, Inc. (LMA) to complete a mixed
methods needs assessment among Maricopa County residents who use drugs from April to
June 2023. The assessment had two components to data collection: (1) the distribution of 525
surveys among PWUD; and (2) conducting 40 semi-structured qualitative interviews among
PWUD who were also experiencing homelessness.

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
8
Data Collection
Eligibility criteria: Eligibility for survey participants was limited to people who self-reported
using non-prescribed medications or street drugs in the prior 30 days, had lived in Maricopa
County for at least 30 days, were at least 18 years of age, and had not participated in the
survey before. Eligibility for the interviews included an additional question to verify that a
participant was currently experiencing homelessness or without a permanent place to live. To
ensure that both groups of people would be reached, LMA partnered with community
organizations throughout all five regions of Maricopa County (Northeast, Northwest, Central,
Southeast, and Southwest) to serve as host field sites for participant recruitment and data
collection.
Central cities: Phoenix
Northeast cities: Carefree, Cave
Creek, Fountain Hills, Paradise
Valley, Scottsdale
Northwest cities: Aguila, Glendale,
El Mirage, Peoria, Surprise,
Wickenburg, Youngtown
Southeast cities: Chandler,
Gilbert, Guadalupe, Mesa, Tempe,
Queen Creek
Southwest cities: Avondale,
Buckeye, Gila Bend, Goodyear,
Litchfield Park, Tolleson
Recruitment and field sites: This project employed a venue-based sampling approach. Initial
field sites were identified from service providers that had participated in Key Community
Partner conversations. Additional sites were recruited with an emphasis on populations that
were not well-represented in the 2019 PWID assessment, including the LGBTQIA+ population.
Since surveys aimed to collect feedback from people who were both sheltered and
unsheltered, partners who regularly conduct outreach to local encampments were also
contacted.
Over 30 organizations were identified and invited to participate in the needs assessment.
There were 27 survey events held among 16 unique field sites between April 13, 2023, to June
8, 2023. Of the 16 sites, seven were mobile harm reduction outreach events from local Syringe
Service Providers (SSP’s). Five host field sites were brick-and-mortar medical facilities, which

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
9
among other services, provide treatment for substance use disorder. One organization was
focused on HIV care. One host field site provides services to caregivers managing substance
use while they look after new babies. Two sites were specifically encampment outreach events
to people who are unhoused. Interviews were offered at all host field sites but were completed
at only 9 field sites due to the number of interested individuals and number who met the
additional eligibility criteria. Appendix A contains a list of all participating organizations.
All sites were offered a personalized flyer to explain the project, incentives, and collection of
information in advance of the events, with the goal of providing staff and regular clients the
opportunity to plan to participate. Prior to the first encampment outreach event, Data
Collectors participated in a trial accompaniment to understand how the outreach team
maneuvered through the large urban encampment and how the Data Collectors would
ingratiate themselves into their approach for recruitment.
Field site logistics, and consent: Data Collectors were responsible for setting up data
collection field sites and recruiting participants on-site. Each site required a semi-private space
for surveys to be completed on tablets with security screen protection, and a private space in
which to complete longer, one-on-one interviews. The time spent per event varied between two
to three hours. Because field sites were both indoor events equipped with a table, chairs, and a
private room available, as well as outdoor meetups, the exact logistics varied between events.
Data Collectors reviewed an informed consent script with each participant (Appendix D) and
provided a printed copy of the informed consent form to each participant for both surveys and
interviews. Data Collectors did not collect identifying information except general demographic
questions including primary area of residency, age, and race. Data Collectors were present for
survey completion and were available to assist if a participant required support in entering
their responses. Paper surveys were available upon request. Data Collectors were responsible
for storing incentive gift cards and completed paper surveys in a lockbox.
A Unique ID was assigned by Data Collectors during the eligibility screening process for each
participant to avoid duplication of the survey by the same participant. Unique IDs were logged
in real-time in a live, incentive, Google sheet.
Survey instruments: MCDPH created two survey tools to capture both survey and interview
data. Drafts of these instruments were shared with Key Community Partners in group feedback
sessions in late 2021 to ensure questions were both appropriate and informative. Both survey
tools were available in English and Spanish (Appendix C).
The survey was created in Qualtrics and contained 77 unique questions. Questions were
grouped into the following thematic sections: (1) Housing Experiences, (2) Drug Use, (3) Harm
Reduction Knowledge, (4) Substance Use Treatment, (5) General Services & Needs, (6) Health

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
10
Insurance, (7) Reproductive Health, and (8) Demographics. Respondents were informed that
they could skip any question or stop the survey at any time.
For interviews, the semi-structured interview guide (Appendix D) outlined four thematic
sections in which a participant could be prompted by the Data Collector to speak about their
experience: (1) Demographics, (2) Housing, (3) Substance Use/Overdose, and (4) Perceptions
of Treatment Options. Within these sections, open-ended questions and pre-planned prompts
were created to help guide the conversation with interview participants. Participants were
informed that they could refuse to answer any pre-planned prompt or decline to speak about a
subject. Data Collectors were encouraged to allow a participant to share details and stories
that were not prompted.
Interview appointment cards were created after identifying that more people were interested in
completing a one-on-one interview than the planned event duration would allow. By passing
out cards at preceding events, Data Collectors allowed participants to plan for a set interview
time and field site in which to complete an interview.
Incentives and resources: Participants who completed a survey received a $20 gift card to a
large chain retailer with multiple locations around Maricopa County. The survey took between
15-20 minutes to complete. Participants who completed an interview received a $50 gift card
to the same chain retailer. Interviews typically lasted 45 minutes depending on the individual’s
experience and level of comfort. Participants could complete one or both data collection
components if they were eligible. Data Collectors also offered a resource list to all participants.
Recruitment monitoring: Throughout the data collection period, MCDPH monitored participant
demographics, the number of completed surveys and interviews, and the number of refusals.
To ensure geographical reach and demographic representation, MCDPH compared participant
demographics to the demographics of fatal and nonfatal overdoses within Maricopa County
and coordinated with LMA to add field sites that would enhance regional representation.
Monitoring each event helped to identify unique needs such as the interview appointment
cards.
Analysis
Survey data analysis: Responses where individuals partially completed the survey but left
before they could receive a gift card were removed from the analysis. 525 survey responses
were analyzed by MCDPH using SAS Enterprise Guide version 8.2.
Interview analysis: Interviews were voice recorded and detailed notes were taken by the Data
Collectors. The interview notes were analyzed by LMA staff using NVivo 12 software and
transcripts were used for reference and to identify representative quotes. Members of the LMA

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
11
evaluation team used a deductive approach to code the interview notes. A sample of five
interviews were used to identify initial codes and inductive codes were added based on
new/unexpected information from the interviews. The evaluation team met weekly to discuss
questions about appropriate coding and to identify initial themes. After coding was complete,
the LMA evaluation team expanded on initial themes to develop findings and
recommendations.
Results
In total, 525 survey responses were collected during April 13, 2023–June 8, 2023, across 27
events. Exhibit 1 below displays how survey and interview completion compared across
different types of venue events. Results will be presented within the following thematic
groupings: (1) demographics; (2) housing; (3) energy insecurity; (4) drug use and harm
reduction knowledge; (5) substance use treatment; (6) health services; and (7) reproductive
health.
Exhibit 1. Survey and interview completion by event type
Event Type
Surveys
Completed
(N=525)
Interviews
Completed
(N=40)
Mobile Harm Reduction Outreach
330 (63%)
28 (70%)
Medical Facility - OUD/SUD
135 (26%)
12 (30%)
Encampment Outreach
40 (8%)
-
Medical Facility - HIV Care
12 (2%)
-
Medical Home for Substance-Exposed Babies
8 (2%)
-
Demographics
Surveys
The majority (62.8%) of respondents were between the ages of 18 to 44. Individuals who
reported using any opioid in the past 30 days (N=309) were slightly younger than those who
reported using only non-opioids (N=179). The median age for those who reported using
opioids in the past 30 days was 37, compared to 43 for those who reported only using non-
opioids.
Most (57.1%) respondents identified as male. Racial and ethnic identity information was
collected as a “select all that apply” measure, allowing respondents to identify as more than
one racial or ethnic identity. A little over a third (35.8%) of respondents identified as White;

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
12
29.3% identified as Hispanic or Latino/x; 18.1% identified as American Indian, Alaska Native, or
Native American; and 15.2% identified as Black or African American.
Sexual orientation was also collected as a “select all that apply” measure. Over two-thirds
(68.0%) of respondents identified as straight/heterosexual; 6.5% as asexual; 8.8% as bisexual;
4.6% as gay or lesbian; and 4.4% as pansexual, queer, questioning, or self-described.
4.6% stated they were a veteran of the U.S. Armed Forces.
A little over a quarter of respondents (26.5%) stated that they had been in jail or prison for at
least 24 hours at some point in the past 12 months, among which 45.3% (n=63) were on
probation or parole at the time of the survey.
About three-quarters (76.0%) of respondents stated they had health insurance, with most
(82.5%) having insurance through the Arizona Health Care Cost Containment System
(AHCCCS) (n=329). Among those without health insurance (N=75), the most common barriers
were not having an address to receive mail (n=23; 30.7%); not having a computer or phone to
enroll (n=23; 30.7%); and cost (n=18; 24.0%). Of the 17.3% (n=13) that provided some other
response for not having health insurance, a few individuals wrote in that they had challenges
with renewing their AHCCCS.
Interviews
There was almost an equal representation of both men and women among interview
participants (52.5% and 47.5%, respectively). No participant identified as non-binary, gender-
queer, or other gender identity. The ages of participants ranged from 19 to 69 years old, and
40% of participants were 36 to 50 years old (N=29). Although interview participants had the
opportunity to select more than one racial/ethnic identity, all participants self-identified as one
race or ethnicity: 30% identified as white; 25% as Hispanic, Latino/a/x, or Spanish; 25% as
American Indian or Alaska Native; and 20% as Black or African American. The majority of
interview participants said they lived in Maricopa County for 10 or more years.
The last demographic question asked participants about the size of their household. Almost
half of all participants shared that they lived by themselves (N=18, 45%). Because participants
were experiencing homelessness, interviewers prompted participants with a definition of
“household size”, indicating that this should include the participant, as well as any family
member, relative, partner, or spouse they live with or who helps pay for expenses or with whom
they share resources.
Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
13
Housing
Background
Maricopa County’s 2023 annual point-in-time count showed a 6.8% increase in people
experiencing homelessness (PEH) from the previous year, with a roughly even split in people
experiencing sheltered versus unsheltered homelessness.
14
Homelessness and housing
affordability are conjointly related. Rates of homelessness increase significantly as people’s
rent exceeds 30-34% of their income.
15
Metro Phoenix rents increased by 80% from 2016 to
2021.
16
The National Low Income Housing Association estimates that Arizona has 24
affordable and available rental homes per 100 extremely low-income renter households in
need, while the estimate for the Phoenix-Mesa-Chandler area is just 19.
17
People often attribute homelessness to individual-level characteristics. Though individual-level
characteristics may increase one’s risk of homelessness, they are not the root cause of
homelessness. Rather, within the constraints of a tight housing market (i.e., high levels of rent
and a low rental housing vacancy rate), the most vulnerable populations will be left unhoused
and a single misfortunate event, such as an argument or divorce, can trigger an episode of
homelessness. The book Homelessness Is a Housing Problem: How Structural Factors Explain
U.S. Patterns explains this important distinction between “precipitating events” and “root
causes”:
“A key point to which we return in this book is that under certain conditions, a range of
precipitating events (like divorce) can result in homelessness — but these events ought not be
considered root causes of housing instability and loss…. when housing is scarce, vulnerabilities
and barriers to housing are magnified.”
18
Securing housing is only a part of the conversation, as ensuring stable housing is also of
concern. Maricopa County’s eviction rate is nearly twice the national average.
19
Evictions not
only cause housing displacement, but individuals can also lose their possessions during the
process, they can lose their jobs, and the eviction record can make individuals ineligible for
future housing, including federal housing programs.
20
Background checks can be a significant hurdle for people in search of affordable housing. A
2019 study published in the American Journal of Public Health found that 43.4% of housing
authorities required residents to have 4- to 5- years with no criminal justice encounters to be
re-eligible for public housing, while 9.9% required 6 years or more. The study authors explain,
“While federal statute (24 CFR§982.553) specifies some circumstances in which people with
criminal justice histories are restricted from public housing (e.g., 3-year ban following eviction
from public housing for drug-related criminal activity), local housing authorities have
tremendous discretion when setting policy to determine who gets admitted to public housing
and the circumstances under which they can be evicted.”
21

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
14
People who have been formerly incarcerated are at heightened risk for experiencing
homelessness. The first 30 days after release from jail or prison is when risk of entering
homelessness is highest.
22
Unfortunately, once these individuals enter homelessness, they
may become trapped in a cycle of incarceration, release, and homelessness. Among those
with just one incarceration history, the rate of homelessness is nearly 7 times higher than the
general public. People who have been incarcerated multiple times are twice as likely to
experience homelessness as those who are returning from their first prison term.
23
Identity documents can also be a significant obstacle for PEH. Not having a permanent mailing
address or not having the necessary documents required for a replacement ID (e.g., birth
certificate) may prevent some individuals from being able to obtain a replacement ID, as can
the cost to obtain a replacement.
24
Surveys
To differentiate between individuals ever experiencing homelessness, recently experiencing
homelessness, and currently experiencing homelessness, housing status was assessed
through three different self-report questions. In total, 89.7% of all survey respondents reported
either currently experiencing homelessness or experiencing homelessness at some point in
their lives:
- Over three-quarters of all respondents (79.2%) reported experiencing homelessness or
unstable housing in the past 12 months and 63.2% of all respondents reported currently
experiencing homelessness.
- Among those who reported experiencing homelessness in the past 12 months (N=416),
38.7% reported that they mostly slept on streets (including parks, abandoned buildings,
etc.) during this time period and 79.8% were currently experiencing homelessness.
- Among respondents who did not explicitly report experiencing homelessness in the past
12 months (N=109), half (50.5%) reported that they had experienced homelessness at
some point in their life.
For those who reported currently experiencing homelessness (N=332), 60.8% reported that
they had been experiencing homelessness for a year or longer, thus meeting the definition of
chronic homelessness. Among the respondents who explicitly stated that they did not
experience homelessness in the past year (N=91), 42.9% reported living in a house, apartment,
or condo that they rented or owned for most of the past 12 months and 24.2% reported living
in a house, apartment, or condo that someone else rents or owns.
Asked in which region respondents primarily lived, 47.0% lived in the central region, 19.2% lived
in the southwest, 18.9% lived in the southeast, 7.8% lived in the northwest, and 5.9% lived in the
northeast. Exhibit 2 shows how this regional representation compares to regional trends in the
location of 2021 fatal overdoses. Efforts to ensure that representation was not limited to the
Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
15
central region were successful, though the southwest region was slightly overrepresented, and
the northwest region was slightly underrepresented.
Exhibit 2. Survey responses by region compared to the location of 2021 fatal overdoses
Region
Proportion of 2021 fatal
overdoses
Survey Respondent Region
Central
49.8%
47.0%
Northeast
4.5%
5.9%
Northwest
12.8%
7.8%
Southeast
23.1%
18.9%
Southwest
6.5%
19.2%
Respondents who reported experiencing homelessness in the past year (N=416) were asked
about events or circumstances that led to their loss of stable housing. Almost a third (n=132;
31.7%) indicated that their alcohol or drug use contributed to their loss of housing; 22.8%
(n=95) could not afford the rent increase; 22.1% (n=92) stated an argument with a
family/friend/roommate contributed to their loss of housing; one in five respondents (n=84;
20.2%) were evicted; one in five respondents (n=87; 20.9%) stated that family or friends
stopped letting them stay with them; 18.3% stated they went to jail or prison (n=76); 18.3%
(n=76) experienced a divorce or break-up; 13.0% (n=54) experienced a death of parent, spouse,
or child; and almost a tenth reported domestic violence (n=39; 9.4%). Over a quarter (27.2%)
attributed the loss of their housing to job loss (n=113). Among those who specifically stated
that they lost their jobs due to the COVID-19 pandemic (N=51), the majority (60.8%) reported
that they had been laid off.
Some individuals stated that discrimination was a factor in their job loss. Among individuals
who stated they experienced some form of discrimination (N=39), 46.2% stated the
discrimination was based on their race or ethnicity; 33.3% stated the discrimination was based
on their disability; 28.2% stated their discrimination was based on their age; 20.5% stated their
discrimination was based on their gender presentation; and 20.5% stated their discrimination
was based on their sexual orientation.
Regardless of current housing status, all respondents (N=525) were asked about their interest
in finding stable housing. Over three-quarters (76.8%) of all respondents expressed interest in
finding stable housing. These individuals who expressed interest in stable housing (N=403)
were also asked what would help them with finding stable housing. Assistance with paying
rent (n=268; 66.5%) and help finding affordable housing (n=211; 52.4%) were the top two
responses for what would be helpful. However, several other barriers were reflected through
responses to this question. For example, just under a third (n=121; 30.0%) of respondents
interested in obtaining stable housing stated that a replacement identity document would help

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
16
them secure stable housing; and help finding housing that allows for a prior felony was
another common response (n=114; 28.3%). Among individuals who stated something else
would be helpful (n=19), two individuals wrote-in that finding a place that would accept their
voucher would be helpful.
Almost a fifth of all respondents (19.4%) indicated they had dependents under the age of 18
who either lived with them or whom they had regular responsibility for, while a tenth of all
respondents (10.3%) had elders living with them or whom they had regular responsibility for.
Among respondents who were interested in housing and had a child dependent (N=72), 16.7%
stated that childcare assistance would help them with finding stable housing. Among
individuals who were interested in housing and reported caring for an elder (N=38), 5.3%
indicated that eldercare assistance would be helpful.
A little over a quarter (26.9%) of all respondents (N=525) reported that a background check
had at some point prevented them from accessing housing in the past.
Among all respondents, only 12.2% reported that they were currently receiving support from an
affordable housing program and an additional 3.8% stated they were on a waitlist. Half of the
individuals who stated they were on a waitlist stated they had been on the waitlist for at least
two years.
Individuals who denoted ever experiencing homelessness but were not currently experiencing
homelessness (N=55) were asked an open-ended question of who or what specifically helped
them secure housing. While a couple of individuals specified that treatment and getting sober
is what helped them, many attributed their living situation to the support of friends and family.
It is possible that individuals who reported to be living with a parent, child, or partner but were
previously experiencing homelessness are still in unstable housing situations (i.e., hidden
homelessness).
Due to an error in survey logic, a survey question about shelters was only asked of those who
had indicated ever experiencing homelessness but were not currently experiencing
homelessness. Among these respondents (N=55), common barriers to shelter use in the past
had been sobriety requirements (N=10; 18.2%); concerns about safety (N=9; 16.4%); concerns
about getting sick (N=9; 16.4%); and the shelter not having space (N=9; 16.4%) or being too
crowded (N=9; 16.4%).
Interviews
When interview participants were asked to describe their current housing situation, the amount
of time without stable housing varied from 2 months to 20 years. At the time of interview,
60.0% (N=24) were living on the street, in tents, or in a car. 17.5% (N=7) were sleeping in
homes belonging to friends or family, and 12.5% (N=5) were living in shelters. As shown in
Exhibit 3, most interview participants indicated they had been experiencing housing instability
for a year or longer.

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
17
Exhibit 3. Length of time experiencing housing instability among interview participants
N=36; four participants did not specify their amount of time without stable housing.
When asked what led to participants' housing insecurity, 42.5% of participants mentioned
personal drug use (N=17) in addition to other factors, and of those, 5 (29.4%) solely stated
personal drug use. Other than personal drug use, factors that contributed to housing insecurity
included experiencing hardships such as estranged relationships with household members
(n=16; 40.0%); low to no income (n=11; 27.5%); debilitating medical conditions (n=6; 15.0%);
and lack of access to health care coverage (n=3; 7.5%). Participants shared that the
combination of low to no income and rising costs of rent have been barriers to their housing
stability. Additionally, participants described losing their employment due to debilitating
medical conditions and lack of health care coverage to receive health care treatment.
Interview participants with mental health
conditions including depression and anxiety
shared needing medication to maintain stable
employment and housing. They also described
losing their shared and/or provided housing
due to estranged relationships. Some
participants lost stable housing after
experiencing divorce, the death of a family
member, or were kicked out of the house by
parents or other family members.
Some participants said they are not comfortable in shared housing (including shelters,
recovery housing, and temporary living with family or friends) due to experiences with violence,
theft, and continued substance use.
“I had certain medications that were prescribed
to me by a psychiatrist... I had Insurance issues
and couldn’t continue to use my medication…
They helped me be stable and with those drugs
I was able to be consistent… Without the
medication, I don’t have ability to complete
tasks. I tried to go to other places for
medications but then started self-medication.”
- Interview 18
n=6, 16.7%
n=9, 25.0%
n=14, 38.9%
n=7, 19.4%
10 or more years
5-9 years
1-4 years
Less than 1 year
Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
18
Finally, many people with lived experience described the interrelatedness between their
substance use and housing instability. Interview participants noted that drug use impacted
their housing when they prioritized their drug use over obtaining housing. They might choose
substance use over available housing options if there are rules that prohibit substance use in
their available housing. They also noted that limited available housing and the stress of
housing instability and life on the street creates the need for substance use as a coping
mechanism.
Interview participants living in subsidized housing, emergency shelter housing, and transitional
living homes have also had trouble relying on these services due to negative interactions with
agency staff and limited-service capacity. Over half of the interviewees indicated they did not
find any help through housing organizations, and they had negative experiences when
searching for help (N=24; 60.0%). Interview participants described negative interpersonal
relationships with managers or leadership of various organizations and housing units. These
experiences included managers showing favoritism and overlooking threatening behavior.
Participants also described organizational service capacity as a barrier to obtaining stable
housing. A recurring theme related to service capacity for all housing services was the lack of
available space at housing organizations,
long wait lists, and difficulty communicating
with service organizations. For instance, 16
interviewees (40.0%) stated being on a
waitlist and, of those, 12 of them have been
waiting for two or more years. Difficulty with
communication included not receiving a call
back after leaving multiple messages and
being hung up on while trying to make
housing arrangements.
Systems and policies have also served as a barrier to stable housing, including interactions
with the justice system, business and city policies, and housing facility policies. Participants
who have been involved with the justice system said they are prohibited from applying for
housing or from applying for assistance through city-run programs. Additionally, city policies
that prohibit gathering in parks and heavy police presence discourage people from seeking
services in those areas. To find steady employment, participants described needing to be able
to look presentable, yet local business policies often prevent them from using showers or
bathrooms to establish proper hygiene. Additionally, interviewees described housing facility
policies that prevent them from applying for or maintaining housing. For example, participants
“You can’t get clean when you’re homeless because it affects you mentally. I have nowhere to live.
There’s no reason for me to be doing good if I don’t have anything.” –Interview 13
“I applied to Section 8 and various different places,
[Agency] and other housing opportunities, these
people can’t reach me, my phone was stolen, and I
have to start all over. It’s a run around. It’s a big
old mess. I applied to Section 8 with [Agency] in
2015. I was never asked how to get ahold of you.
I’m a convicted felon and unemployed. I lack a real
advocate for help.” –Interview 24

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
19
felt there were more opportunities for housing for individuals with a serious mental illness
(SMI) or for individuals who identify with diverse racial/ethnic groups. Some interview
participants also had difficulty adhering to housing facility policies and requirements, including
staying sober while living at the facility.
Interview participants largely requested resources to support self-efficacy in the housing
application process so they will be empowered to navigate the system themselves. For
example, many people said they do not know how or where to start the process while others
mentioned that their personal literacy and lack of skills with technology were a challenge in
navigating the system. Participants also requested resources on learning how to keep stable
housing once they obtained it, including learning coping skills to prevent relapse. Additionally,
participants requested more secure resources/locations to address their basic needs including
showering, sleeping, and eating.
Recommendations Related to Housing
Increase access to affordable housing: Since 2021, Maricopa County has invested more than
$500 million in homelessness services, including funding directed for the construction of
affordable housing and additional shelter beds.
25
These investments are greatly needed. The
top two facilitators to stable housing identified in our survey were rental assistance and
housing affordability. Many interview participants also stated they were currently on a waitlist
for housing assistance programs. A report published in June 2023 by The University of
California San Francisco summarizing findings from a representative study of PEH in
California asked its participants about hypothetical interventions for homelessness prevention.
70% of participants believed that a shallow subsidy of $300-$500 a month would have allowed
them to avoid homelessness for at least two years. 90% believed that an ongoing subsidy that
capped their housing costs at 30% of their income (e.g., housing vouchers) would have
prevented their homelessness.
26
Additionally, a study published in August 2023 demonstrated
that recipients of a one-time unconditional cash transfer spent fewer days experiencing
homelessness and increased their savings and spending with no increase in “temptation
goods spending” defined as alcohol, drugs, or cigarettes.
27
These findings indicate that
modest rental assistance could be invaluable to PEH.
Invest in eviction prevention and diversion programs: Eviction prevention programs and eviction
diversion programs are effective ways of intervening before an eviction filing occurs.
28
Eviction
prevention programs may include providing clients with housing counseling, legal assistance,
“I try so hard every day at meeting my deadlines at the main offices… I had an appointment at 9 o’ clock
and then had two more appointments after that. I’m doing my part anyway I can. It’s good that I’m able
to reach them to apply, I still can’t read or write, but I’m trying.” –Interview 10

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
20
emergency rental assistance, and other supports. Eviction diversion programs focus on
diverting cases from formal legal proceedings through negotiation and mediation.
29
Streamline housing navigation processes: Interview participants discussed challenges with the
housing navigation process, including knowing how to initiate the process, having difficulties
when communicating with agencies, and encountering difficulties with the technology required
and their own literacy levels. Simplifying housing application processes, with a goal of
promoting self-efficacy, should be prioritized.
Reform the use of criminal records in housing applications: Arizona Senate Bill 1294 went into
effect in January 2023, allowing Arizonans to petition the court and seal criminal records.
While this law is well intentioned, there are many challenges that may limit its impact: (1) a
petition-based process requires that individuals know their eligibility status and having the
resources to pursue a petition; (2) there are significant costs to record sealing that make it
unlikely for low-income populations to have the means to pursue; (3) many privately-owned
data companies, including people-search websites, do not comply with credit reporting rules
and keep records even after they have been sealed.
30
While this law is a step in the right
direction, ways to address these challenges should be considered, including the adoption of an
automatic record clearance process. Also, local housing authorities should have more
oversight to ensure they are not more restrictive than the federal minimum.
Improve housing navigation for individuals exiting incarceration: Housing navigation should be
provided to individuals prior to release from jail or prison. Reforming the use of criminal
records will also help people who have been formerly incarcerated with finding housing.
Remove barriers to replacement identification documents: Better outreach is needed to assist
individuals with securing replacement ID’s and helping with the secure storage of these
documents. Additionally, it's important to allow PEH to keep their belongings when being
relocated.
Address barriers to shelter use: While we were not able to assess local barriers to shelter usage
among all survey respondents who had experienced homelessness, some survey respondents
indicated that sobriety requirements, overcrowding, no space, and safety were all barriers to
usage. Interview participants also expressed that shared housing, which includes shelters, are
prone to theft, violence, and substance use. While shelters on their own are not a solution to
the shortage of affordable housing, addressing these barriers to their usage will help provide
individuals with temporary relief and may help individuals get connected to services.

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
21
Energy Insecurity
Background
The interaction between heat and stimulant use contributes to an annual uptick in fatal
overdoses during the summer months in Maricopa County. Stimulants such as
methamphetamines and cocaine increase body temperature and, especially when
temperatures are high, increase the risk of dehydration and heat-related illness.
31
In 2022,
43.5% of fatal overdoses that occurred in the county were during June–September.
32
Questions on energy insecurity and cooling center usage were incorporated into the survey to
better understand potential barriers to accessing these spaces.
Surveys
Individuals who did not report currently experiencing homelessness (N=193) were asked two
questions about their energy security. Just under half (47.2%) reported struggling to pay their
gas and/or electric bills, while a little over two-thirds (69.4%) reported that it was always, often,
or sometimes too cold or too warm inside. Between these two questions, 154 of the 193
(79.8%) were categorized as energy insecure.
All survey respondents (N=525) were asked to identify the places they visit to stay cool during
the summer. The most common responses included a friend or family member’s house
(n=207; 39.4%); library (n=193; 36.8%); and mall (n=128; 24.4%). Nearly twenty percent stayed
at their own place (n=104). 93 (17.7%) specifically identified seeking refuge at a Heat Relief
Network cooling center. Among individuals who stated they go some other place to cool off
(N=56), common responses included transit (bus/light rail); shaded areas, including parks; and
water sources, including lakes, rivers, and pools.
Respondents who stated they cooled off by visiting any public place outside of their own
residence (N=455) were asked to identify the reasons they may not be able to choose to use a
cooling center. The three biggest barriers to cooling center usage were not being aware that
cooling centers existed (n=222; 48.8%); lack of transportation to a cooling center (n=156;
34.3%); and not knowing how to find the location of a cooling center (n=127; 27.9%). One
participant wrote-in, “No cooling center that I’ve tried has ever even known that that’s what they
were and I was turned away.”
Individuals who were experiencing homelessness or were experiencing energy insecurity
(N=486) were asked what would help encourage their use of cooling centers. Food was the
most common response (n=234; 48.1%). Other facilitators to cooling center usage included
having a place to charge their phone (n=187; 38.5%); transportation to the cooling center
(n=173; 35.6%); and having someone onsite that could connect them to wraparound services
such as housing and healthcare (n=172; 35.4%). Additionally, a quarter of respondents (n=125;

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
22
25.7%) stated that safer drug use supplies would encourage their use of cooling centers. Three
individuals wrote-in that showers would encourage their use of cooling centers.
Among individuals who were experiencing homelessness or were experiencing energy
insecurity who reported opioid use in the past 30 days (N=293), 39.2% were interested in
having someone onsite connect them to wraparound services (n=115); 31.4% were interested
in safer drug use supplies onsite (n=92); 17.1% were interested in getting help testing their
drugs for fentanyl (n=50); and 15.4% were interested in obtaining naloxone onsite (n=45).
Recommendations Related to Energy Insecurity
Increase cooling center awareness: Despite frequent usage of the types of facilities that
compose Maricopa County’s heat relief cooling center network, our results suggest individuals’
lack of awareness around Heat Relief Network cooling center branding. Additionally,
respondents indicated they were not familiar with how to find cooling center locations,
illustrating a need for increased awareness of the Heat Relief Network resources, such as the
printed map to identify a location.
Increase cooling center accessibility: At the time of writing this report, Maricopa County is
experiencing a historical heatwave. 19 days in July had nightly lows above 90 degrees
Fahrenheit.
33
With most cooling center hours limited to business hours, PWUD who are either
experiencing homelessness or experiencing energy insecurity are highly susceptible to adverse
outcomes from heat. Efforts to expand accessibility to cooling centers, including the
expansion of operational hours and providing transportation, are critical.
Expand cooling center services: Because survey respondents indicated that providing
wraparound services and safer drug use supplies at cooling centers would encourage their use
of these spaces, these findings present an opportunity to expand upon the services that
cooling centers provide, perhaps by partnering with organizations that already provide these
services, thus transforming them into hubs that can offer a variety of services to our most
marginalized communities.
Drug Use and Harm Reduction Knowledge
Background
From 2019 to 2021, 81.8% of overdose deaths that occurred in Maricopa County involved more
than one drug.
34
The effects of various drug combinations can be unpredictable. Mixing
stimulants and opioids, for example, can cause the effects of the drugs to be masked, tricking
the individual into thinking they’re not affected by the drugs, therefore increasing their
overdose risk.
35

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
23
Fentanyl, a synthetic opioid up to fifty times stronger than heroin
36
, was involved in nearly two-
thirds of overdose deaths in Maricopa County in 2021.
37
Exposure to fentanyl can be
intentional or unintentional. Estimates of unintentional versus intentional fentanyl exposure
vary, but most studies on this topic indicate that a minority of PWUD prefer to use fentanyl.
38
Injection drug use (IDU) is associated with an increased risk of overdose compared to smoking
or snorting drugs.
39
IDU also increases one’s risk for invasive bacterial and fungal infections,
human immunodeficiency virus (HIV), and viral hepatitis.
40
Syringe service programs (SSPs)
are an evidence-based approach to providing people who inject drugs with access to and
disposal of sterile syringes and injection equipment. SSPs can also function as way to provide
other important health services, including vaccination, testing for infectious diseases, linkage
to infectious disease care, and substance use treatment. New users of SSPs are five times
more likely to enter substance use treatment and about three times more likely to stop using
drugs than those who don’t use the programs.
41
While smoking is considered a safer route of drug use compared to injection, programs that
distribute safe smoking equipment can reduce health problems associated with smoking, such
as burns, mouth sores, and coughing blood.
42
Additionally, because the sharing of smoking
supplies can still serve as a transmission route for hepatitis C virus
43
as well as respiratory
diseases such as tuberculosis
44
, the distribution of safe smoking supplies can help to prevent
these negative outcomes.
Our survey did not seek to answer when respondents’ drug use began. While some
respondents identified drug use as one of the factors that contributed to their loss of housing,
some research also shows that drug use often begins after entering homelessness.
45
People
may use stimulants such as meth to stay awake and watch over their belongings, to avoid
being discovered by authorities, and to stay alert and protect one’s personal safety.
46
Some
research has also indicated that people who use opioids may start to use stimulants for
additional perceived benefits, including the belief that concurrent use may reduce one’s risk of
an overdose.
47
To mitigate the risks of drug use, harm reduction is a set of practical strategies and ideas
aimed at reducing the negative consequences associated with drug use.
48
Understanding what
harm reduction techniques are practiced by PWUD is critical in understanding where there are
service gaps and where better outreach may be needed.
Surveys
All respondents (N=525) were asked about the drugs they had used in the past 30 days.
Stimulant use was more common than opioid use, as 75.0% of all respondents reported the
use of a stimulant (e.g., methamphetamines, cocaine) in the past 30 days, while 58.9%
reported the use of an opioid (e.g., fentanyl, commonly prescribed opioids including
Oxycodone). About a third (32.2%) of all respondents reported stimulant use without the use of

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
24
an opioid, while only 16.0% reported the use of an opioid without a stimulant. In total, 179
(34.1%) reported only the use of a non-opioid (e.g., stimulants, benzodiazepines). 42.9%
reported the use of both opioids and stimulants. Exhibit 4 summarizes these drug categories
and combinations.
Exhibit 4. Drug category used in past 30 days
N=525
Methamphetamines were the most common drug reported to be used in the past 30 days,
reported by nearly two-thirds of respondents (n=342; 65.1%). Following methamphetamines,
the most common drugs reported were fentanyl (n=264; 50.3%); opioid pain medications, such
as Oxycodone and Percocet (n=95; 18.1%); and cocaine powder (n=82; 15.6%).
Among the drugs selected as used in the past 30 days, respondents were asked to choose
their “drugs of choice”, or the drugs they most prefer to use. Interestingly, this question had the
highest missingness of all the survey questions (20.4%), suggesting that the phrasing of this
question was potentially problematic; for example, it’s possible the distinction with the
previous question was not understood or that the word “choice” was offensive. Approaching
interpretation of this question with caution, methamphetamines (n=214; 40.8%) and fentanyl
(n=192; 36.6%) were the drugs respondents most preferred to use.
Four out of five respondents reported that they smoke their drugs (n=422; 80.4%) and about a
quarter of respondents reported snorting their drugs (n=136; 25.9%). Injection drug use (IDU)
was reported by about a fifth of respondents (n=114; 21.7%), though IDU was higher among
respondents who reported using opioids in the past 30 days compared to those who reported
using only non-opioids (26.2% vs. 17.3%, respectively). These patterns in how respondents
reported using their drugs explain why pipes (n=288; 54.9%) and straws (n=199; 37.9%) were
the most common types of equipment that respondents reported sharing with someone else.
In contrast, needle-sharing was reported by 28.1% of those who specifically reported IDU.
n=84, 16.0%
n=169, 32.2%
n=179, 34.1%
n=225, 42.9%
n=309, 58.9%
n=394, 75.0%
Any opioid, no stimulant
Any stimulant, no opioid
Non-opioids only
Any stimulant AND any opioid
Any opioid
Any stimulant

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
25
Less than a quarter of respondents (n=124; 23.6%) stated that they did not share any of their
drug equipment in the past 30 days. These individuals cited community organizations (n=40;
32.3%) as their primary source for obtaining their unused/clean equipment, with pharmacies
and/or drug stores being the second most common avenue for obtaining clean equipment
(n=25; 20.2%).
Among those who did not name fentanyl as a drug they most preferred to use (N=333), over
half (54.1%) were not familiar with fentanyl test strips (FTS). FTS familiarity was similar
between individuals who reported using opioids and individuals who reported using only non-
opioids (44.4% vs. 44.7%, respectively). Among respondents who stated they were familiar
with FTS (N=138), less than half (47.8%) reported ever using one.
Respondents who stated they had used FTS at some point but did not always use them (N=49)
were asked to identify the reasons they did not always use them. Barriers included not always
carrying them (n=19; 38.8%); not knowing where to get them (n=10; 20.4%); not wanting to
waste drugs on testing (n=10; 20.4%); and hearing that fentanyl is in everything now (n=10;
20.4%). The sentiment that fentanyl was in everything now was more common among
individuals who reported using opioids in the past 30 days compared to those who reported
only using non-opioids (36.4% vs. 7.7%).
Among respondents who were familiar with FTS but had never used them (N=69), a little less
than a third (31.9%) were interested in using them.
All respondents (N=525) were asked about their familiarity with naloxone. About three-quarters
(76.0%) of all respondents indicated they were familiar with naloxone/Narcan. Naloxone
familiarity was higher among those who reported using an opioid in the past 30 days
compared to those who reported using only non-opioids in the past 30 days (85.8% vs. 65.9%,
respectively). Black, Indigenous, and People of Color (BIPOC) populations had larger
proportions of people who were not familiar with naloxone. For example, a quarter of those
who identified as American Indian or Alaska Native were not familiar with naloxone, while just
6.9% of white respondents were not familiar with naloxone (Exhibit 5).
Exhibit 5. Naloxone familiarity by race and ethnicity
Familiar with
naloxone
Not familiar
with naloxone
American Indian/Alaska Native/Native American
69 (72.6%)
24 (25.3%)
Asian*
5 (71.4%)
2 (28.6%)
Black or African American
57 (71.3%)
22 (27.5%)
Hispanic, Latino/a/x, or Spanish
112 (72.7%)
40 (26.0%)
Middle Eastern or North African*
1 (50.0%)
1 (50.0%)
Native Hawaiian or Pacific Islander*
4 (57.1%)
3 (42.9%)
White
172 (91.5%)
13 (6.9%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
26
Other race or ethnicity not listed*
4 (66.7%)
2 (33.3%)
*Total N for this group is less than 10. Approach interpretation of this result with caution, as other data sources may be needed
to strengthen conclusions drawn for this socio-demographic group.
Among those familiar with naloxone/Narcan (N=399), a little over two-thirds (68.9%) reported
that they currently had naloxone/Narcan, a finding that was again higher among those who
specifically reported recent opioid use than those who only reported non-opioid use (76.2% vs.
56.8%).
The most frequent locations where those with naloxone access (N=275) cited receiving their
naloxone included community organizations (n=150; 54.5%); drug treatment facilities (n=63;
22.9%); from a friend or family member (n=56; 20.4%); and from a doctor or health clinic (n=53;
19.3%). Other responses (n=9) had mentions of receiving naloxone from “people at the park”
and “people handing them out” without necessarily attributing to an organization.
For those familiar with naloxone but who did not report access (N=111), common reasons for
not having naloxone were not knowing where to get it (n=29; 26.1%); not thinking they were at
risk for an overdose (n=28; 25.2%); and not using opioids (n=22; 19.8%). Additionally, 64.3% of
those who stated they did not believe they were not at risk of an overdose had reported using
opioids in the past month.
Interviews
Interview participants shared what led to them to initially start using drugs and why they
continued to use them. More than half of all participants began using drugs as minors (N=24)
(Exhibit 6), though more than 40% of interviewees who started using drugs as minors used
marijuana or alcohol first (N=10). The others used illicit drugs including cocaine, heroin, or
methamphetamine either alone or in combination with marijuana and alcohol (n=14; 58.3%).
Participants reported currently using a range of drugs including methamphetamine (n=30);
fentanyl (n=16); marijuana (n=12); cocaine (n=7); oxycodone (n=6); alcohol (n=4); and other
opioids including heroin (n=3).

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
27
Exhibit 6. Age of first use among interview participants
N=40
Social and community contexts played a
significant role in illicit drug use initiation for
participants. Interview participants started using
because their family members were using or
when they experienced the death of a family
member. Interview participants described using
drugs socially with peers or in response to pain
after an injury, eventually leading to dependence.
Interview participants also discussed initiation of drug use in response to changes to their
physical environment, including loss of stable housing or getting evicted. Some individuals
began using drugs to deal with the stress of living on the streets, which is exacerbated by a
lack of quality sleep and exposure to the elements. Participants described social pressure as a
reason for initiating drug use and described the difficulties in abstaining from drug use while
living on the streets because drug use is prevalent in housing insecure communities.
Participants also gave various reasons why they use their drug/s of choice. Economic
instability has caused participants to turn to cheaper substances, including fentanyl and
methamphetamine, when necessary. Lastly, several participants shared that their substance
use increased over time, or they started using stronger substances after building a tolerance to
their initial drug of choice.
Interview participants were asked about their behaviors around fentanyl use. More than half
(N=24; 60%) of interviewees reported avoiding fentanyl use while 40% (N=16) of interviewees
reported choosing to use fentanyl. They shared that they believed they could recognize its
smell and understood its potency. Some interview participants described avoiding opioids
(including fentanyl) due to a fear of consequences such as experiencing hallucinations, heart
issues, illness, theft of their personal belongings, incarceration, and fatal overdose.
Participants who reported avoiding fentanyl discussed active and passive strategies to
specifically avoid fentanyl use. Active strategies include verbal confrontation (e.g., yelling at
people who are using fentanyl nearby) and using fentanyl testing strips. Passive strategies
include disassociating from groups that use fentanyl and walking away if an individual or
n=5, 12.5%
n=11, 27.5%
n=24, 60.0%
36-64 years old
18-35 years old
Under 18 years old
“I got into drugs three years ago after getting
kicked out of my home for drinking. Slowly, it
was introduced to me. First it was one hit
there and then my craving got really strong.”
–Interview 20

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
28
group uses fentanyl. Interview participants who reported seeking fentanyl mentioned that they
started using fentanyl to manage pain from hunger, injuries, or medical conditions. Some
participants mentioned seeking fentanyl if their drug of choice was not available or if they did
not have enough money for their (more expensive) drug of choice.
“I’ve heard true stories of ‘one pill kills.’ I can't imagine anything more terrifying.” –Interview 18
Interview participants shared that they access harm reduction services because they are
nearby, and the personnel often have lived experienced themselves. Several (N=26; 65%)
shared that they initially received naloxone/Narcan and learned how to use it from one of these
organizations. Participants also found it
beneficial to receive harm reduction
supplies to prevent infections that can result
from sharing supplies (N=3; 7.5%).
Participants shared they feel comfortable
carrying Narcan and engaging in harm-
reduction services after receiving
anonymous syringe service program
participant identification cards that grant
limited immunity from law enforcement for carrying harm reduction supplies. Some
participants also share harm reduction resources and information with others who use
substances.
Lack of awareness of harm reduction services is still an issue. Participants who do not access
harm reduction services are not aware of services available. Participants also discussed their
methods of preventing overdoses including knowing their limits and monitoring their intake.
Some participants only keep a limited supply of drugs with them at any given time, so they are
less likely to overdose. In contrast, others prefer to smoke substances rather than injecting
them, ensuring they take smaller, more controlled doses. Participants described only using
clean or sterile needles when injecting and carrying naloxone or making sure someone they are
with has naloxone. Participants also described the importance of obtaining their supply from
people they trust and using fentanyl test strips (used by N=7; 17.5% of interviewees) to test
their drugs before using them. Additionally, participants noted that they only use substances
when they are with other people in case they overdose and need a dose of naloxone and
having ice cold water ready and available for anyone who is experiencing an overdose. Finally,
some participants prefer to use substances unlikely to cause an opioid overdose, such as
cocaine and methamphetamines.
“Everyone else do what I do, make sure you
keep a nasal spray. Keep Narcan and smoke
with someone and let them know you have it
with you. I got Narcan just in case I
overdose.” –Interview 13

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
29
Suggested improvements to promote harm reduction included increasing access to harm
reduction services and suggestions for additional
locations. Participants described increasing
access due to ongoing needs of harm reduction
supply to prevent co-occurring medical disorders,
including sexually transmitted infections and
infections from open wounds. They also
suggested providing safe, monitored spaces to
use substances without the threat of law
enforcement getting involved. Additionally, some
participants asserted that other PWUD still need
to be made aware of resources and suggested increasing outreach activities. Participants
suggested sites for increased harm reduction services, which are included in Exhibit 9 in the
Treatment section.
Recommendations Related to Drug Use and Harm Reduction
Provide wrap-around services to people experiencing homelessness: For many, drug use may
start or be exacerbated by entering homelessness. While homelessness prevention is
obviously the most effective way to prevent illicit drug use that develops as a coping
mechanism or survival mechanism, providing wraparound services to PEH to reduce the
stressors that they face on the streets is necessary.
Prioritize substance use prevention among youth: Some interview respondents reported that
they started using drugs as minors in response to traumatic events or home environments.
Investing in evidence-based programs that promote protective factors against drug use can go
a long way. Protective factors may be at the individual, family, or school/community level.
Examples include interpersonal skills that help youth integrate feelings, thinking, and actions to
achieve specific social and interpersonal goals (individual level); resiliency, or the ability to
adapt to change and stressful events in healthy and flexible ways (individual level); bonding, or
the attachment, commitment to, and positive communication with, family, schools, and
communities (family/school/community level); and opportunities for positive social
involvement (family/school/community level). Most protective factors associated with
substance use are also associated with other problems affecting youth, such as delinquency,
psychiatric conditions, violence, and school dropout.
49
Expand naloxone education and access as well as overdose response education: While
naloxone familiarity among the majority of respondents is a positive finding, additional
education is needed to both ensure all PWUD understand the utility of naloxone, especially in
the context of fentanyl contamination. Additionally, naloxone distribution programs should
ensure equitable outreach across diverse populations. Some participants also mentioned
“The resources that are available are
not known to the people who need
them most…The info isn’t out there…
Because these resources aren’t well
known, they have no idea where they
would go or prefer to go.”
–Interview 17

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
30
using ice cold water to respond to overdoses, indicating that overall overdose response
education is a need.
Increase awareness and distribution of safer use supplies: With the majority of respondents
reporting that they shared drug equipment, there is a need for access to safer use supplies.
The distribution of safer use supplies should be reflective of the many ways in which people
may use drugs, such as smoking and injecting. The distribution of safer use supplies should be
coupled with increased education around the risks of sharing supplies.
Increase messaging for people who use drugs that are not opioids: These findings stress the
importance of ensuring overdose prevention education campaigns and harm reduction
outreach are inclusive of people who do not specifically use opioids. Opioid-use-focused
messaging may exclude people who use drugs that are not opioids but who may still be at risk
of an opioid overdose due to the proliferation of fentanyl in the drug supply. Additionally,
messaging and harm reduction tools that are specific to stimulant overdoses is critical.
Explore legal pathways to create a safe use site to optimize harm reduction and reduce opioid
overdoses and overdose fatalities: Interview participants indicated that the threat of law
enforcement often prevented them from seeking harm reduction outreach services. Safe
consumption sites offer PWUD a safe space to use drugs. In addition to acting as a safe space
where PWUD may feel comfortable accessing harm reduction services, a 2021 systematic
review found that most supervised injection facilities were associated with reductions in
overdose mortality. For example, there was a 26% net reduction in overdose deaths in the area
immediately surrounding a supervised injection site in Vancouver, Canada in comparison with
the rest of the city.
50
Increase education on fentanyl test strips: Greater awareness of FTS is needed. Education
should also target misconceptions about fentanyl (e.g., that you can detect it in your supply
through smell) as well as misconceptions about FTS (e.g., that drugs need to be wasted on the
test). Efforts to make FTS more widely available in areas where PWUD congregate should also
be prioritized.
Incorporate harm reduction into areas where PWUD congregate: In addition to the distribution of
harm reduction supplies through outreach events, there is a need for finding other ways to
increase access to harm reduction supplies. Incorporating harm reduction access into areas
where PWUD congregate, such as through vending machines, can complement existing
outreach programming, while simultaneously providing a consistent 24/7 access point. It is
possible that vending machine distribution may also reach a different population, one that
values anonymity in accessing services.

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
31
Substance Use Treatment
Background
Eliminating barriers and expanding access to substance use treatment and recovery services
is an instrumental component in combatting the overdose epidemic. Commonly cited barriers
to substance use treatment include stigma, cost, and accessibility.
51
Studies of clinician attitudes toward PWUD have shown high levels of stigma. In a 2019 survey
of primary care physicians across the country, a third of respondents did not perceive
medication treatment to be more effective than nonmedication treatment or safe for long-term
use, despite this being the gold standard for treating opioid use disorder. The survey also
revealed low provider interest in treating individuals with opioid use disorder.
52
For patients
who experience stigma, the effects can translate to diminished feelings of empowerment and
lower patient engagement during treatment.
53
Outside of substance use treatment, these
negative experiences can lead to general healthcare avoidance, including avoiding calling 911
if someone is experiencing an overdose, not accepting transport to a hospital following an
overdose, or leaving a hospital against medical advice.
54
Policies and regulations may cause unnecessary bureaucracy or may not have the intended
effect. For example, federal regulators expanded the allowable take-home doses for
medication for opioid use disorder (MOUD) during the COVID-19 pandemic; however, a recent
study conducted in Arizona found that patients encountered challenges with obtaining take-
home doses, which may be partially explained by these federal allowances not being
mandated.
55
Effective treatments vary by the type of substance use disorder. While medications are
considered a gold-standard for treating OUD, there are no FDA-approved medications available
for stimulant use disorders. The Substance Abuse and Mental Health Services Administration
(SAMHSA) identifies four different evidence-based treatment practices for treating stimulant
use disorders: motivational interviewing, contingency management, community reinforcement
approach, and cognitive behavioral therapy.
56
Surveys
About two-fifths (39.6%; n=208) of all respondents (N=525) indicated that within the past six
months they had either (1) experienced something that made their ability to get into treatment
difficult; or (2) experienced something that made their ability to continue their treatment more
difficult. While the most common challenge reported was not being ready to stop using drugs
(n=87; 41.8%), other common challenges included no program openings or a waitlist (n=54;
26.0%); being treated poorly by staff (n=51; 24.5%); and difficulties with transportation and/or

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
32
distance to the treatment program (n=49; 23.6%). Some individuals also reported not knowing
where to go for treatment and/or what type of treatment to start with (n=38; 18.3%). 28.4%
(n=59) reported cost as a barrier, either due to not having health care coverage (18.3%) or
having coverage that didn’t cover the full cost (17.3%).
About a third of all respondents reported currently being in a treatment program (33.9%;
N=178). The most common type of treatment was MOUD, as roughly half of those currently in
treatment were on MOUD (n=92; 51.7%). Outpatient rehabilitation was the second most
common type of current treatment reported (n=53; 29.8%). Federal guidelines continue to
stress that medication efficacy is strengthened when combined with psychosocial therapy.
57
27.2% of those currently on MOUD were also in one-on-one counseling, highlighting an area for
treatment improvement.
Current treatment was higher among certain demographic sub-groups. 40.8% of female
respondents were currently in treatment and 29.7% of male respondents were currently in
treatment; 44.1% of white non-Hispanic respondents were currently in treatment, while only
25.0% of black respondents were in treatment; 41.7% of veteran respondents were in
treatment compared to 34.7% of non-veterans; and 38.3% of those who reported having health
insurance were in treatment compared to 18.7% among the uninsured.
Exhibit 7. Percentage of socio-demographic group currently in treatment
Socio-Demographic Group
N (%) of socio-
demographic
group currently
in treatment
Total survey
respondents
for socio-
demographic
group
Gender Identity
Man
Woman
Non-binary*
Self-described*
Refused
Missing
89 (29.7%)
75 (40.8%)
1 (20.0%)
4 (50.0%)
4 (40.0%)
6 (26.1%)
300
184
5
8
10
23
Age Category
Ages 18-24
Ages 25-34
Ages 35-44
Ages 45-54
Ages 55-64
Ages 65+
Missing
16 (39.0%)
42 (31.8%)
50 (31.8%)
35 (35.7%)
25 (37.9%)
7 (43.8%)
3 (21.4%)
41
132
157
98
66
16
14

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
33
Race/ethnicity
American Indian/Alaska Native/Native American
Asian*
Black or African American
Hispanic, Latino/a/x, or Spanish
Middle Eastern or North African*
Native Hawaiian or Pacific Islander*
White
Other race or ethnicity not listed*
Refused
Missing
32 (33.7%)
2 (28.6%)
20 (25.0%)
51 (33.1%)
0 (0.0%)
2 (28.6%)
83 (44.1%)
2 (33.3%)
8 (40.0%)
7 (21.9%)
95
7
80
154
2
7
188
6
20
32
Jail/prison in past year
Yes
No
Refused
Missing
45 (32.4%)
121 (36.8%)
2 (10.0%)
10 (27.0%)
139
329
20
37
Health Insurance
Yes
No
I don’t know
Missing
153 (38.3%)
14 (18.7%)
9 (26.5%)
2 (11.8%)
399
75
34
17
Veteran
Yes
No
Refused
Missing
10 (41.7%)
154 (34.7%)
2 (14.3%)
12 (27.9%)
24
444
14
43
Sexual Orientation
Asexual
Bisexual
Gay
Lesbian*
Pansexual*
Queer*
Questioning or unsure*
Straight (heterosexual)
Self-described
Refused
Missing
10 (29.4%)
17 (37.0%)
1 (5.9%)
3 (37.5%)
2 (40.0%)
3 (60.0%)
3 (60.0%)
123 (34.5%)
5 (45.5%)
5 (20.8%)
14 (31.8%)
34
46
17
8
5
5
5
357
11
24
44
*Total N for this group is less than 10. Approach interpretation of this result with caution, as other data sources may be needed
to strengthen conclusions drawn for this socio-demographic group.

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
34
Among those who reported currently being on MOUD (N=92), the majority (88.0%) reported
being on methadone.
Among those who were not currently in a treatment program (N=347), 42.4% stated they were
interested in treatment. The most common types of treatment that were of interest to these
respondents (N=147) were detox facilities (n=81; 55.1%); MOUD (n=52; 35.4%); inpatient
rehabilitation (n=49; n=33.3%); and outpatient rehabilitation (n=47; 32.0%).
Among those interested in treatment who reported using opioids in the past 30 days (N=95),
70.5% were interested in detox programs (n=67); 50.5% were interested in MOUD (n=48); and
40.0% were interested in inpatient rehab (n=38). Among those interested in treatment who
reported only using non-opioids in the past 30 days (N=48), 33.3% were interested in one-on-
one counseling (n=16); 29.2% were interested in outpatient rehab (n=14); and 29.2% were
interested in detox programs (n=14).
Individuals who did not report currently being on MOUD (N=433) were asked if they had ever
tried a medication to help modify, reduce, or stop their drug use. Just over a third (35.6%) of
these respondents reported trying MOUD at some point in the past. When limiting to
respondents who reported using opioids in the past 30 days (N=241), 45.6% indicated being on
MOUD at some point in the past.
Among those who either (1) expressed interest in treatment but did not select MOUD as a type
of treatment they were interested in; or (2) were currently receiving treatment that was not
MOUD (N=181), common reasons for not being on MOUD were: not having an opioid use
disorder (n=55; 30.4%); not being interested (n=32; 17.7%); and indicating interest in using a
medication sometimes but not every day (n=32; 17.7%). Some individuals stated they could not
find a job while being on a medication (n=21; 11.6%). Looking specifically at those who
reported using opioids in the past 30 days (N=95), 25.3% stated they’d be interested in using a
medication sometimes but not every day (n=24); 20.0% stated that transportation was difficult
(n=19); and only 12.6% stated they did not have an OUD (n=12).
Those currently in treatment as well as those who expressed interest in treatment (N=325),
were asked to identify facilitators that would aid in their ability to get treatment. Help with
finding or maintaining housing while in treatment was the most common facilitator, reported
by over forty percent of these respondents (n=142; 43.7%). Help with transportation was the
second most common facilitator to treatment (n=133; 40.9%). Other common facilitators
included help maintaining stable employment while in treatment (n=112; 34.5%); help paying
for treatment (n=106; 32.6%); help with getting a phone (n=114; n=35.1%); and help with
getting an ID (n=102; 31.4%). Among individuals who had indicated having either a child
dependent or caring for an elder and who were currently interested in treatment or already in
treatment (N=82), 20.7% stated that assistance with childcare or eldercare would ease their
ability to get treatment.

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
35
Among those who stated that fewer rules/requirements while in treatment would help make
treatment easier for them (N=82), over half (n=42; 51.2%) specified that sobriety requirements
made treatment difficult and a little less than a third (n=26; 31.7%) stated they couldn’t take
their prescriptions for other conditions while in treatment (e.g., medications for managing
anxiety or depression). For those who provided some other rule/requirement as making their
treatment difficult (n=22; 26.8%), one major theme that emerged was difficulty in obtaining
take-home doses of MOUD, with many writing-in that this option had not been available to
them. Others specified that the schedule required to qualify for take-home dosing was too
long. One participant wrote, “Hard to get on weekly/monthly take home doses because of
certain requirements like not needing to miss for 30-60 days and getting 2 consecutive pee tests
clean.”
Among those who stated they were not interested in treatment (N=110), reasons included not
being ready to stop using drugs right now (n=35; 31.8%) and not being interested in stopping
drug use (n=34; 30.9%).
Interviews
Participants noted that economic instability, low
access to health coverage, and hardships managing
co-occurring medical disorders impede access to
substance use treatment. Interview participants also
described the cost of treatment and transportation
as barriers to seeking treatment. Participants shared
that not having health insurance to cover treatment
and not knowing what treatment options are covered
by state health care plans were barriers. Participants
also alluded to the need to treat co-occurring
medical and mental health disorders while receiving
treatment. Some participants were concerned that
substance use treatment might not treat underlying mental health issues that lead to
substance use.
More than half of interviewees reported that they had received some form of treatment in their
lives (N=21; 52.5%). Nine participants who have received treatment were mandated to attend
and four participants who have received treatment in the past were not interested in seeking
treatment at the time of the interview. Interview participants who received treatment described
both positive and negative experiences with service providers. Access to peer support, ability
to contribute to or work for the program, and programs with flexible schedules and longer
treatment duration characterized positive experiences. Other positive experiences included
having access to integrated care such as dental treatment, being able to start intake and
“People on drugs develop the disorders. Some
are drug induced mental issues like
schizophrenia. severe depression and bipolar.
If you’re doing drugs, you’re causing it to be
worse. Just because I’m on drugs doesn’t
mean I don’t need mental health. I need the
medication and mental health. I shouldn’t be
judged by my drug use... it’s not fair to not
take care of my health needs.”
–Interview 11

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
36
treatment immediately, and interacting with treatment staff who are compassionate and
understanding.
Unfortunately, participants also experienced negative interactions with treatment providers
and facilities. Negative interpersonal interactions with other patients and providers
characterized negative experiences. Specifically, interview participants mentioned treatment
staff who were not attentive to their needs. For example, several interviewees mentioned being
removed from treatment centers if they were not experiencing suicidal ideation, which led
participants to feel their substance use treatment needs were being ignored. Additionally,
several interviewees mentioned that their need for safety was not being met at treatment
centers that do not enforce rules that prohibit violence and theft. Participants also mentioned
negative experiences with staff at detox centers who were unkind during the detox process.
Negative experiences also included feeling like providers only care about profits and are
unwilling to deal with insurance companies when the patient has an issue with coverage and
bullying from other patients (N=5).
Long wait lists also deter people from entering treatment, with some interview participants
stating that they often turn back to substance use by the time it is their turn on the waitlist.
Some participants are wary of coed treatment centers and centers that do not address
behavioral concerns, including continued substance use and violence within the facility. Lack
of oversight and/or short staffing in some facilities has led to substance use and violence
within the facility even if policies prohibit substance use.
Participants felt that systems and policies related
to health coverage and treatment facilities have
also created barriers to seeking treatment.
Interview participants described that their health
care plan has a maximum number of treatment
days allowed, which is not always sufficient to
address issues with a substance use disorder.
Some participants shared that they were refused treatment because of their type of insurance
coverage. Treatment facility policies also prevent people from seeking treatment. For example,
some participants do not feel they can meet curfew requirements or do not qualify for
treatment unless they have an SMI. Additionally, some participants hesitate to seek treatment
because many facilities do not have options for participants to adequately secure their
“Lots of us want to get off drugs but they won’t help us. We don’t have the right help to help us. It’s
because they know we do drugs… Because they know our background, they treat us like we’re less
than.” –Interview 33
“Been to thirty 30-day inpatients over
time. First was in 1982, last one was this
year… 30 days isn’t enough for anyone to
get sober.” –Interview 23

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
37
belongings or pets. This makes them vulnerable to theft of their possessions, including
government documents and identification cards.
Interview participants described a mixture of positive and negative perceptions of treatment.
Nineteen participants had never been in treatment and seven of those interviewees had never
been interested in seeking treatment. Other interviewees who have not been to treatment do
not seek treatment because they do not want to go through the detox process, they are already
accessing prevention programs through church or shelters, they do not like group therapy
programs, or they were having issues with insurance coverage.
In general, interview participants who were not
interested in seeking any type of treatment felt
that way due to witnessing others relapse after
receiving treatment, believing treatment facilities
are only interested in increasing profits, and
believing there is no treatment for OUD. In order to
facilitate trust between patients and
staff/providers, interviewees expressed comfort in
learning from staff/providers with lived experience. Some participants also recognized that
they were not in the right mindset to start treatment, or they were not ready for the pain
associated with the detox process.
Amongst the interview sample, there was also a mixture of history of use of MOUD. Positive
perceptions of MOUD services were primarily shared by interviewees who have used MOUD
and included being able to detox in a slow and safe way and that some medications are
covered by AHCCCS. Some participants noted challenges with using MOUD, including the lack
of awareness that some MOUD are covered by AHCCCS and that AHCCCS will provide
transportation to MOUD providers. Participants who have not received MOUD described a high
rate of relapse when others have used MOUD, referred to it as another drug, and did not want
to deal with regulations surrounding MOUD. In order to improve treatment seeking and
adherence, participants suggested training the workforce to be more compassionate, as well
as including peer support for the purpose of improving treatment services and removing the
stigma surrounding substance use. Some participants also shared wanting to learn more
coping skills to manage their emotions and to aid them in their recovery following treatment.
The majority of participants were in favor of accessing mobile unit services provided by
MCDPH. They suggested providing mobile services, including methadone services, more
“They don’t care about you. They only care
about your insurance paying for them and
wouldn’t do it for free. Sober houses and
other places, they’re getting direct deposits
from [insurance] agencies.”
–Interview 9
“It helped me a lot. I was able to function like a human without having to worry about using.
Methadone does help. You can do your daily functioning. It gets hard if you don’t have a car, you go
back to using for that day.” –Interview 33

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
38
frequently (once a week) and conducting more outreach where resources for various treatment
options are shared. Mobile services were also of interest for services that provide basic needs.
This will be further developed in the Health Services section.
Participants also highlighted the importance of having a social support system, including
family and friends, to remain sober for periods of time in their lives and/or to use less
substances.
Some participants do not seek treatment because they are under the impression that you have
to be completely clean before starting treatment. Because of this thought process, these
participants also called for spaces where people can use drugs safely while being monitored.
This would allow them to taper their usage or use other substances like cigarettes or
marijuana to help curb cravings of more illicit drugs.
Recommendations Related to Substance Use Treatment
Prioritize connections to low-barrier treatment, including through mobile services: Providing
treatment in non-traditional settings to limit treatment barriers has shown success in other
jurisdictions. For example, an evaluation of a Seattle-based buprenorphine program at an SSP
saw reductions in participant opioid use and sustained participant retention.
58
Similar
treatment models with success in decreasing opioid use include a street medicine approach in
San Francisco
59
and a Philadelphia model that used a mobile unit.
60
Improve access to take-home MOUD: Challenges regarding the accessibility of MOUD were
salient throughout both surveys and interviews. Despite federal regulations permitting
flexibilities in providing take-home doses of MOUD, which can help to address the
transportation difficulties many MOUD patients experience, respondents described challenges
with the requirements for eligibility. A better understanding of provider implementation
challenges may be needed. Additionally, to ensure patients are being offered these services,
mandating these types of flexibilities would likely increase access to take-home MOUD.
Reduce or supplement treatment costs and assist with issues related to health care coverage:
Survey respondents identified treatment costs, including healthcare coverage that did not
cover the full cost of treatment, as a challenge to successful treatment completion in the past.
Additionally, interview participants indicated that health care coverage itself may have
constraints on the type of treatment covered or the number of days covered. Reducing
treatment costs, connecting individuals to health care coverage, assisting individuals with
navigating their health plans, and eliminating health plan policy barriers are all critical
components in successfully linking people to treatment.
Increase access to affordable housing: Respondents identified housing as the largest facilitator
of substance use treatment. Housing First models prioritize connecting people to housing

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
39
before addressing additional needs such as mental health and substance use. For people who
have higher service needs, such as those who have experienced chronic homelessness, have a
substance use disorder, have a mental health condition, or have a disability, Housing First can
be implemented through permanent supportive housing (PSH) models, which offer
wraparound services to clients on a voluntary basis. A systematic review published in 2020
found that PSH programs increased housing stability over a six-year period both for
participants with moderate support needs and high support needs.
61
Reduce stigma among healthcare providers: Being treated poorly by staff during substance use
treatment was identified as a barrier. Addressing stigma among healthcare providers is
essential to improving trust and health outcomes among PWUD. Anti-stigma communication
campaigns that target healthcare providers can be effective, if implemented carefully. For
example, a randomized clinical trial conducted by Johns Hopkins University found that a visual
campaign in combination with narrative vignettes from the perspective of people with OUD
was associated with reduced levels of stigma.
62
Increase capacity of substance use treatment providers: Interview participants described
encountering waitlists for substance use treatment. In general, the longer the delay between a
patient’s initial treatment attempt and the scheduled appointment, the less likely the patient is
to attend.
63
Reducing waitlist times will likely require enhancements in provider capacity and
insurance processes, including preauthorization.
Increase the integration of peer support into treatment: Interview participants with positive
treatment experiences described the positive impact of peer support. The integration of peer
support into treatment programs may help to facilitate trust with providers.
Share MOUD treatment success stories: Some interview participants shared that they have a
lack of trust in the effectiveness of MOUD. Sharing the stories of those who have been
successful with MOUD may help to dismantle some of the existing misconceptions and trust
barriers.
Invest in evidence-based treatment for non-opioid use and polysubstance use: Strategies
focused on connecting people to substance use treatment should be careful not to focus only
on treatment for OUD. Substance use treatment is not a “one size fits all” solution. These
strategies need to be reflective of individuals having varying needs and that they may be using
more than one drug. Given increases in the number of people using non-opioids, especially
methamphetamines, investing only in linkage to MOUD or MAT would be a critical mistake.
Additionally, patients should be offered psychosocial treatment based on their individual
needs.

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
40
Health Services and Basic Needs
Background
Individuals who are experiencing homelessness may endure many unmet health needs. ED
utilization among PEH is nearly five times that of people who are not experiencing
homelessness.
64
This can be attributed to a number of factors, such as lack of health
insurance and lack of transportation. PEH are also less likely to be connected to primary care,
dental care, and mental health care while being more likely to face food insecurity or food
insufficiency.
65
Some unmet health needs may act as a competing demand and may make it even more
difficult for PEH to start or continue substance use treatment or to maintain stable housing.
MCDPH was interested in learning more about the unmet needs of PEH in Maricopa County
and the ways in which these services could be delivered.
Surveys
MCDPH was interested in collecting feedback around other services needed by this
community. Respondents expressed interest in a variety of health services, among which the
top three were food assistance (n=261; 49.7%); dental care (n=254; 48.4%); and clothes or
shoes (n=243; 46.3%).
Nearly three-quarters of respondents stated they were very likely (57.5%) or somewhat likely
(16.0%) to go to a mobile unit to obtain the services they identified as being of interest. Among
individuals who stated they were very or somewhat likely to utilize mobile services (N=386),
59.3% had selected dental care as a health need; 33.2% had selected mental health services as
a health need; 21.5% had selected MOUD as a health need; and 24.4% had selected safer use
supplies as a health need (Exhibit 8).

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
41
Exhibit 8. Health needs among those interested in mobile services versus all respondents
Using the regional map, respondents indicated where it would be easiest to access a mobile
unit that provided these services. These results mostly mirrored the trends on where
participants lived, with 43.2% stating the central region would be easiest, 15.8% stating the
southeast, and 12.4% stating the southwest.
Interviews
In addition to interest in the delivery of substance use treatment services through mobile
outreach (described above in the Substance Use Treatment section), interview participants
also described the need for more support in meeting their basic needs, including dental and
vision treatment, bus passes, bicycle repair, food, pet services, showers, legal services, and
clothing. Interview participants primarily suggested mobile units to be located near them as
transportation to other locations would be a barrier. Some participants emphasized focusing
efforts near downtown Phoenix due to the larger concentrations of individuals experiencing
homelessness and/or drug use. One participant also suggested having mobile units at heat
relief sites. Interview participants who stated they wanted mobile services near them were
asked to share major crossroads for clarity. Exhibit 9 maps the major crossroads participants
4.6%
7.8%
8.6%
10.1%
10.1%
12.0%
14.7%
14.7%
16.2%
17.3%
19.6%
19.6%
26.3%
32.4%
46.3%
48.4%
49.7%
4.2%
8.6%
10.6%
11.9%
11.9%
13.7%
17.4%
17.6%
18.9%
21.5%
23.8%
24.4%
33.2%
39.1%
55.2%
59.3%
60.1%
Pregnancy tests
COVID-19, flu, or other vaccinations
Contraception
Hepatitis C testing
HIV testing
Sexually Transmitted Infection testing
Help w/ testing drugs for fentanyl
Naloxone
Sun protection
MOUD
Wound care kits
Safer use supplies
Mental health services
Hygiene kits
Clothes and/or shoes
Dental care
Food assistance
Very likely or somewhat likely to use mobile services (N=386) All respondents N=525
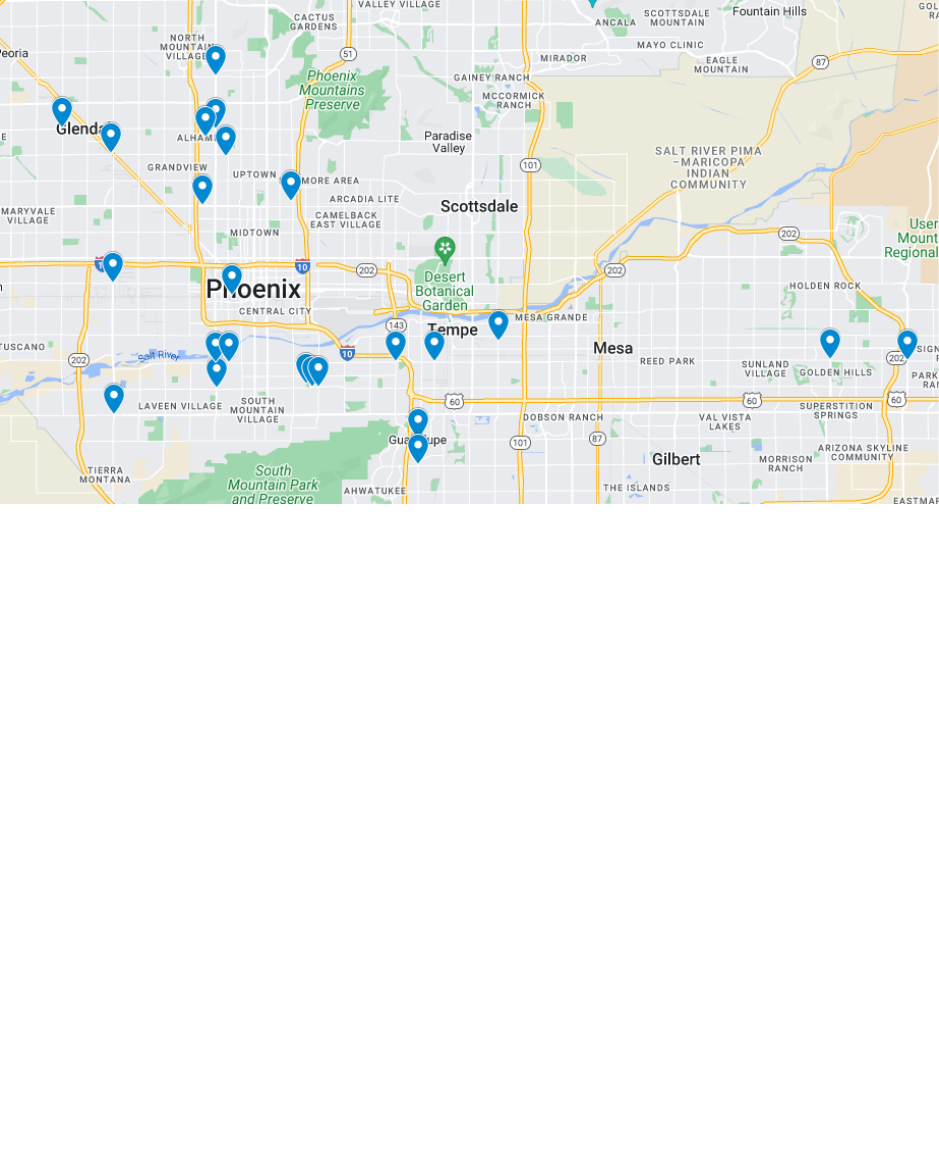
Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
42
shared for suggested locations and Appendix E provides a list of these suggestions for mobile
units and harm reduction sites.
Exhibit 9. Suggested locations of mobile services among interview participants
Recommendations Related to Health Services
Increase services for basic health needs: Across both the survey and interviews, PWUD
expressed interest in a variety of services that address basic needs. A few of the top needs
were for food, dental care, clothing, and mental health care. Organizations providing these
types of services should avoid having a disconnect between what they are providing and the
needs of the community they are serving. For example, one individual wrote into the survey,
“Please im drowning in bars of soap please figure out a place to use them. Please.”
Expand the availability of mobile services: While not all PWUD may engage with mobile
services, given the high degree of interest among our respondents, this is an approach that
should be further expanded. To prevent transportation barriers, mobile services should be
provided near known areas where PWUD congregate and near public transit.

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
43
Reproductive Health
Background
Even among infants exposed to illicit drugs during pregnancy, prenatal care is protective
against negative birth outcomes, including low birth weight, prematurity, and small gestational
age.
66
Additionally, punitive policies are associated with increased rates of neonatal
abstinence syndrome, a condition wherein the infant experiences withdrawal symptoms.
67
Prenatal care visits also serve as an important opportunity to test, diagnose, and treat syphilis
in mothers prior to delivery, preventing the transmission of the infection from mother to baby
(i.e., congenital syphilis). Congenital syphilis can lead to complications with delivery such as
miscarriage, premature delivery, or stillbirth. Congenital syphilis can also cause various ill
health effects for the baby, such as bone disorders, blindness, or deafness.
68
Between 2010
and 2018, rates of congenital syphilis increased by 125% in Maricopa County.
69
The fear pregnant persons who use drugs face in accessing services while pregnant is well
documented in the literature. Qualitative interview studies have demonstrated pregnant
persons’ fear of loss of child custody as a result of drug use, fearing both losing custody of
their newborn and/or other children.
70,71
This evidence extends to quantitative studies as well.
A study published in JAMA Pediatrics in 2022 examined the association of state child abuse
policies and mandated reporting policies with prenatal and postpartum care among persons
who engaged in substance use and found that these policies reduced receipt of prenatal and
postpartum care among pregnant persons who use drugs.
72
This fear is not limited to pregnant
persons who are using illicit drugs but also includes pregnant persons who are on MOUD to
stop their drug use. As a recent New York Times article reported, “In Arizona, which doesn’t
track buprenorphine cases, hospitals reported about 400 new mothers who only had methadone
in their systems.”
73
Surveys
Overall, 8.6% of respondents either had a pregnancy in the past two years or were currently
pregnant. For every five respondents who had experienced a pregnancy in the past two years
(N=28), two did not receive prenatal care (42.9%).
Recommendations Related to Reproductive Health
Support pregnant persons who are treating SUD with MOUD by excluding them from mandatory
healthcare provider reporting requirements: To encourage utilization of prenatal care services,
Arizona should reform its policies around the reporting of drug use in pregnant persons,
specifically ensuring they are not penalized for utilizing MOUD or MAT, which is the standard
of care for pregnant persons with SUD. Efforts should instead focus on making substance use

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
44
treatment more accessible to this population. This strategy will reduce overdoses in the
mother and negative outcomes in the baby related to a lack of prenatal care.
Limitations
This report is subject to at least four limitations. First, this report is not representative of all
PWUD, nor is it representative of all PEH. For example, the sampling methods employed
ensured that a greater proportion of the unsheltered population was represented. Second, this
project also utilized a venue-based sampling approach, working with community agencies that
provide outreach to PEH to identify settings and events where these hard-to-reach populations
may congregate. This approach may lead to an overrepresentation of individuals who are
already connected to harm reduction tools as well as individuals who are more likely to engage
with services or with a governmental agency. Third, despite efforts to ensure survey events
were targeting known areas where PWUD congregate, some areas may have been missed.
Fourth, self-reported data, specifically when collecting sensitive information, are prone to
social desirability bias. However, four factors likely minimize the impact of social desirability
bias in this report: (1) data collectors reviewed confidentiality protocols in detail with each
respondent as part of the consent process; (2) identifiable information was not collected; (3)
respondents were able to complete the survey on their own in a private area; (4) respondents
could skip any question at any time.

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
45
References
1. National Alliance to End Homelessness. Chronically Homeless. Accessed August 23, 2023.
https://endhomelessness.org/homelessness-in-america/who-experiences-homelessness/chronically-
homeless.
2. U.S. Food & Drug Administration (FDA). Information about Medication-Assisted Treatment (MAT).
Accessed August 23, 2023. https://www.fda.gov/drugs/information-drug-class/information-about-
medication-assisted-treatment-mat.
3. Substance Abuse and Mental Health Services Administration (SAMHSA). Medications for Substance Use
Disorders. Accessed August 23, 2023. https://www.samhsa.gov/medications-substance-use-disorders.
4. American Psychiatric Association. Opioid Use Disorder. Accessed August 23, 2023.
https://www.psychiatry.org/patients-families/opioid-use-disorder.
5. Centers for Disease Control and Prevention (CDC). Polysubstance Use Facts. Accessed August 23, 2023.
https://www.cdc.gov/stopoverdose/polysubstance-use/index.html
6. National Institute on Drug Abuse. Words Matter - Terms to Use and Avoid When Talking About Addiction.
Accessed August 23, 2023. https://nida.nih.gov/nidamed-medical-health-professionals/health-
professions-education/words-matter-terms-to-use-avoid-when-talking-about-addiction.
7. National Institute of Mental Health. Substance Use and Co-Occurring Mental Disorders. Accessed August
23, 2023. https://www.nimh.nih.gov/health/topics/substance-use-and-mental-health.
8. Centers for Disease Control and Prevention (CDC). Syringe Services Programs. Accessed August 23,
2023. https://www.cdc.gov/hiv/effective-interventions/prevent/syringe-services-programs/index.html.
9. Substance Abuse and Mental Health Services Administration (SAMHSA). Recovery and Recovery Support.
Accessed August 23, 2023. https://www.samhsa.gov/find-help/recovery.
10. Centers for Disease Control and Prevention (CDC). Understanding the Opioid Overdose Epidemic.
Accessed July 25, 2023. https://www.cdc.gov/opioids/basics/epidemic.html.
11. Maricopa County Department of Public Health. Mental Health and Substance Use Data. Accessed July 25,
2023. https://www.maricopa.gov/5079/Mental-Health-and-Substance-Use#fataloverdose.
12. National Institute on Drug Abuse (NIDA). Drug Overdose Death Rates. Accessed July 25, 2023.
https://nida.nih.gov/research-topics/trends-statistics/overdose-death-rates#.
13. Maricopa County Department of Public Health. Mental Health and Substance Use Data. Accessed July 25,
2023. https://www.maricopa.gov/5079/Mental-Health-and-Substance-Use#fataloverdose.
14. Maricopa Association of Governments (MAG). Point-In-Time Homelessness Count. Accessed July 20,
2023. https://azmag.gov/Programs/Homelessness/Data/Point-In-Time-Homelessness-Count#pit-count-
reports.
15. Glynn C, Byrne TH, Culhane DP. Inflection points in community-level homeless rates. Annals of Applied
Statistics. 2021;15(2):1037-1053. doi: 10.1214/20-AOAS1414.
16. Arizona PBS. Why rent is skyrocketing in the Phoenix Metro Area. Published March 24, 2022.
https://azpbs.org/horizon/2022/03/why-rent-is-skyrocketing-in-the-phoenix-metro-area/.
17. National Low Income Housing Coalition. The Gap – A Shortage of Affordable Rental Homes. Accessed
July 26, 2023. https://nlihc.org/gap.
18. Aldern CP, Colburn G. Homelessness is a Housing Problem: How Structural Factors Explain U.S. Patterns.
University of California Press; 2022.
19. Arizona State University (ASU). Maricopa County: Eviction Dashboard. Accessed July 26, 2023.
https://resilience.asu.edu/evictions-dashboard.
20. Desmond M, Kimbro RT. Eviction’s Fallout: Housing, Hardship, and Health. Social Forces. 2015;94(1):295-
324. https://doi.org/10.1093/sf/sov044.
21. Purtle J, Gebrekristos LT, Keene D, Schlesinger P, Niccolai L, Blankenship KM. Quantifying the
Restrictiveness of Local Housing Authority Policies Toward People With Criminal Justice Histories: United
States, 2009–2018. American Journal of Public Health. 2020;110, S137_S144.
https://doi.org/10.2105/AJPH.2019.305437.

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
46
22. Reentry and Housing Coalition. Homelessness – What We Know. Accessed July 26, 2023.
http://www.reentryandhousing.org/public-housing.
23. Prison Policy Initiative. Nowhere to Go: Homelessness among formerly incarcerated people. Published
August 2018. https://www.prisonpolicy.org/reports/housing.html.
24. Movement Advancement Project (MAP). The ID Divide: How Barriers to ID Impact Different Communities
and Affect Us All. Published November 2022. https://www.mapresearch.org/file/MAP-Identity-
Documents-report-2022.pdf.
25. Maricopa County Department of Human Services. Homeless Services. Published August 29, 2023.
https://www.maricopa.gov/CivicAlerts.aspx?AID=2809.
26. Kushel M, Moore T, et al. Toward a New Understanding: The California Statewide Study of People
Experiencing Homelessness. UCSF Benioff Homelessness and Housing
Initiative.https://homelessness.ucsf.edu/our-impact/our-studies/california-statewide-study-people-
experiencing-homelessness. June 2023.
27. Dwyer, R, Palepu A, Williams C, Daly-Grafstein D, Zhao J. Unconditional cash transfers reduce
homelessness. Proceedings of the National Academy of Sciences. 2023;120(36).
https://doi.org/10.1073/pnas.222210312.
28. Center for Evidence-based Solutions to Homelessness. Homelessness Prevention. Last updated January
2019. http://www.evidenceonhomelessness.com/topic/homelessness-prevention/.
29. Urban Institute. Eviction Prevention and Diversion Programs: Early Lessons from the Pandemic. Accessed
July 26, 2023. https://www.urban.org/research/publication/eviction-prevention-and-diversion-programs-
early-lessons-pandemic.
30. Dedrick T, Konieczny R, Manning B, Santa Cruz E. New Arizona law on sealing criminal records may help
some renters, but there are limitations. Cronkite News. Published May 23, 2022.
https://cronkitenews.azpbs.org/2022/05/23/new-arizona-law-sealing-criminal-records-brings-
opportunities/.
31. Auger N, Bilodeau-Bertrand M, Labesse ME, Kosatsky T. Association of elevated ambient temperature
with death from cocaine overdose. Drug Alcohol Depend. 2017;78:101-105. doi:
10.1016/j.drugalcdep.2017.04.019.
32. Maricopa County Department of Public Health. Data request. August 29, 2023.
33. Cervantes, F. Maricopa County on pace to break heat-associated deaths record; 89 confirmed in 2023.
The Arizona Republic. Published August 16, 2023. https://www.azcentral.com/story/news/local/phoenix-
weather/2023/08/16/maricopa-county-heat-associated-deaths-jump-to-89-so-far-in-2023/70605202007/
34. Maricopa County Department of Public Health. Mental Health and Substance Use Data. Accessed July 18,
2023. https://www.maricopa.gov/5079/Mental-Health-and-Substance-Use#fataloverdose.
35. Centers for Disease Control and Prevention (CDC). Polysubstance Use Facts. Accessed July 18, 2023.
https://www.cdc.gov/stopoverdose/polysubstance-use/index.html.
36. Centers for Disease Control and Prevention (CDC). Fentanyl Facts. Accessed September 15, 2023.
https://www.cdc.gov/stopoverdose/fentanyl/index.html.
37. Maricopa County Department of Public Health. Mental Health and Substance Use Data. Accessed July 18,
2023. https://www.maricopa.gov/5079/Mental-Health-and-Substance-Use#fataloverdose.
38. Gryczynski J, Nichols H, Schwartz RP, Mitchell SG, Hill P, Wireman K. Fentanyl exposure and preferences
among individuals starting treatment for opioid use disorder. Drug Alcohol Depend. 2019;204:107515. doi:
10.1016/j.drugalcdep.2019.06.017.
39. Brugal MT, Barrio G, De LF, Regidor E, Royuela L, Suelves JM. Factors associated with non-fatal heroin
overdose: assessing the effect of frequency and route of heroin administration. Addiction.
2002;97(3):319-27. doi: 10.1046/j.1360-0443.2002.00058.x.
40. Marks LR, Nolan NS, Liang SY, Durkin MJ, Weimer MB. Infectious Complications of Injection Drug Use.
Med Clin North Am. 2022;106(1):187-200. doi: 10.1016/j.mcna.2021.08.006.
41. Centers for Disease Control and Prevention (CDC). Summary of Information on The Safety and
Effectiveness of Syringe Services Programs (SSPs). Accessed July 27, 2023.
https://www.cdc.gov/ssp/syringe-services-programs-summary.html.
Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
47
42. Prangnell A, Dong H, Daly P, Milloy MJ, Kerr T, Hayashi K. Declining rates of health problems associated
with crack smoking during the expansion of crack pipe distribution in Vancouver, Canada. BMC Public
Health. 2017;17(1):163. doi: 10.1186/s12889-017-4099-9.
43. Scheinmann R, Hagan H, Lelutiu-Weinberger C, et al. Non-injection drug use and Hepatitis C Virus: a
systematic review. Drug Alcohol Depend. 2007;89(1):1-12. doi: 10.1016/j.drugalcdep.2006.11.014.
44. Deiss RG, Rodwell TC, Garfein RS. Tuberculosis and illicit drug use: review and update. Clin Infect Dis.
2009;48(1):72-82. doi: 10.1086/594126.
45. Johnson G, Chamberlain C. (2008) Homelessness and Substance Abuse: Which Comes First?. Australian
Social Work. 2008;61(4):342-356. doi:10.1080/03124070802428191.
46. McKenna SA. "We're Supposed to Be Asleep?" Vigilance, Paranoia, and the Alert Methamphetamine User.
Anthropol Conscious. 2013;24(2):172-190. doi: 10.1111/anoc.12012.
47. Corser J, Palis H, Fleury M., et al. Identifying behaviours for survival and wellness among people who use
methamphetamine with opioids in British Columbia: a qualitative study. Harm Reduct J. 2022;19(46).
https://doi.org/10.1186/s12954-022-00630-8.
48. National Harm Reduction Coalition. Principles of Harm Reduction. Accessed July 30, 2023.
https://harmreduction.org/about-us/principles-of-harm-reduction/.
49. Substance Abuse and Mental Health Services Administration (US); Office of the Surgeon General. Facing
Addiction in America: The Surgeon General's Report on Alcohol, Drugs, and Health [Internet]. US
Department of Health and Human Services. November 2016. PMID: 28252892.
50. Levengood TW, Yoon GH, Davoust MJ, Ogden SN, Marshall BDL, Cahill SR, Bazzi AR. Supervised Injection
Facilities as Harm Reduction: A Systematic Review. Am J Prev Med. 2021;61(5):738-749. doi:
10.1016/j.amepre.2021.04.017.
51. Adeniran E, Quinn M, Wallace R, et al. A scoping review of barriers and facilitators to the integration of
substance use treatment services into US mainstream health care. Drug and Alcohol Dependence Reports.
2023;7(). https://doi.org/10.1016/j.dadr.2023.100152.
52. McGinty EE, Stone EM, Kennedy-Hendricks A, Bachhuber MA, Barry CL. Medication for Opioid Use
Disorder: A National Survey of Primary Care Physicians. Ann Intern Med. 2020;173(2):160-162. doi:
10.7326/M19-3975.
53. Leonieke C. van Boekel, Evelien P.M. Brouwers, Jaap van Weeghel, Henk F.L. Garretsen. Stigma among
health professionals towards patients with substance use disorders and its consequences for healthcare
delivery: Systematic review. Drug and Alcohol Dependence. 2013;131(1–2):23-35.
https://doi.org/10.1016/j.drugalcdep.2013.02.018.
54. Simon R, Snow R, Wakeman S. Understanding why patients with substance use disorders leave the
hospital against medical advice: A qualitative study. Subst Abus. 2020;41(4):519-525. doi:
10.1080/08897077.2019.1671942.
55. Meyerson BE, Bentele KG, Russell DM, et al. Nothing really changed: Arizona patient experience of
methadone and buprenorphine access during COVID. PLoS ONE. 2022;17(10).
https://doi.org/10.1371/journal.pone.0274094.
56. Substance Abuse and Mental Health Services Administration (SAMHSA). Treatment of Stimulant Use
Disorders. National Mental Health and Substance Use Policy Laboratory. June 2020.
https://store.samhsa.gov/sites/default/files/pep20-06-01-001.pdf.
57. The ASAM National Practice Guideline for the Treatment of Opioid Use Disorder: 2020 Focused Update. J
Addict Med. 2020;14(2S Suppl 1):1-91. doi: 10.1097/ADM.0000000000000633.
58. Hood JE, Banta-Green CJ, Duchin JS, et al. Engaging an Unstably Housed Population with Low-Barrier
Buprenorphine Treatment at a Syringe Services Program: Lessons Learned from Seattle, Washington.
Substance Abuse. 2020;41(3):356-364. doi:10.1080/08897077.2019.1635557.
59. Carter J, Zevin B, Lum PJ. Low barrier buprenorphine treatment for persons experiencing homelessness
and injecting heroin in San Francisco. Addict Sci Clin Pract. 2019;14(20). https://doi.org/10.1186/s13722-
019-0149-1. Accessed August 2, 2023.
60. O'Gurek D, Jatres J, Gibbs J, Latham I, Udegbe B, Reeves K. Expanding buprenorphine treatment to people
experiencing homelessness through a mobile, multidisciplinary program in an urban, underserved setting.
Journal of Substance Abuse Treatment. 2021;127(108342).

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
48
61. Aubry T, Bloch G, Brcic V, et al. Effectiveness of permanent supportive housing and income assistance
interventions for homeless individuals in high-income countries: a systematic review. Lancet Public
Health. 2020;5(6):e342-e360. doi: 10.1016/S2468-2667(20)30055-4.
62. Kennedy-Hendricks A, McGinty EE, Summers A, Krenn S, Fingerhood MI, Barry CL. Effect of Exposure to
Visual Campaigns and Narrative Vignettes on Addiction Stigma Among Health Care Professionals: A
Randomized Clinical Trial. JAMA Netw Open. 2022;5(2):e2146971.
doi:10.1001/jamanetworkopen.2021.46971.
63. Festinger DS, Lamb RJ, Kountz MR, Kirby KC, Marlowe D. Pretreatment dropout as a function of treatment
delay and client variables. Addict Behav. 1995;20(1):111-5. doi: 10.1016/0306-4603(94)00052-z.
64. QuickStats: Rate of Emergency Department (ED) Visits, by Homeless Status and Geographic Region —
National Hospital Ambulatory Medical Care Survey, United States, 2015–2018. MMWR Morb Mortal Wkly
Rep. 2020;69:1931. doi: http://dx.doi.org/10.15585/mmwr.mm6950a8
65. Baggett TP, O'Connell JJ, Singer DE, Rigotti NA. The unmet health care needs of homeless adults: a
national study. Am J Public Health. 2010;100(7):1326-33. doi: 10.2105/AJPH.2009.180109.
66. El-Mohandes A, Herman AA, Nabil El-Khorazaty M, Katta PS, White D, Grylack L. Prenatal care reduces the
impact of illicit drug use on perinatal outcomes. J Perinatol. 2003;23(5):354-60. doi:
10.1038/sj.jp.7210933.
67. Meinhofer A, Witman A, Maclean JC, Bao Y. Prenatal substance use policies and newborn health. Health
Econ. 2022;31(7):1452-1467. doi: 10.1002/hec.4518.
68. Centers for Disease Control and Prevention (CDC). Congenital Syphilis – CDC Fact Sheet. Accessed
August 17, 2023. https://www.cdc.gov/std/syphilis/stdfact-congenital-syphilis.htm.
69. Maricopa County Department of Public Health. Increase in Congenital Syphilis in Maricopa County,
Physicians Reminded of Testing Requirements. Accessed August 17, 2023.
https://www.maricopa.gov/5099/Congenital-Syphilis-Testing-Requirements.
70. Syvertsen JL, Toneff H, Howard H, Spadola C, Madden D, Clapp J. Conceptualizing stigma in contexts of
pregnancy and opioid misuse: A qualitative study with women and healthcare providers in Ohio. Drug
Alcohol Depend. 2021;222:108677. doi: 10.1016/j.drugalcdep.2021.108677.
71. Stone, R. Pregnant women and substance use: fear, stigma, and barriers to care. Health Justice.
2015;3(2). https://doi.org/10.1186/s40352-015-0015-5
72. Austin AE, Naumann RB, Simmons E. Association of State Child Abuse Policies and Mandated Reporting
Policies With Prenatal and Postpartum Care Among Women Who Engaged in Substance Use During
Pregnancy. JAMA Pediatr. 2022;176(11):1123–1130. doi:10.1001/jamapediatrics.2022.3396
73. Walter, S. They Followed Doctors’ Orders. Then Their Children Were Taken Away. The New York Times
Magazine. Published June 29, 2023. https://www.nytimes.com/2023/06/29/magazine/pregnant-women-
medication-suboxonbabies.html.

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
49
Appendix A. Participating Community
Partners
Community Partner Name
Type Hosted Field Site
Community Medical Services
Medical Facility - OUD/SUD
Hushabye Nursery
Medical Home for Substance-Exposed Babies
Intensive Treatment Services
Medical Facility - OUD/SUD
The MASA Project of Arizona
Encampment Outreach
Shot in the Dark (SITD)
Mobile Harm Reduction Outreach
Sonoran Prevention Works
Mobile Harm Reduction Outreach
Southwest Center for HIV/AIDS
Medical Facility - HIV Care
Southwest Recovery Alliance
Mobile Harm Reduction Outreach
Street Medicine Phoenix
Encampment Outreach
TERROS
Medical Facility - OUD/SUD
Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
50
Appendix B. Survey Questionnaire
DOES NOT INCLUDE QUALTRICS DISPLAY/SKIP LOGIC
Start of Block: STAFF LED - ELIGIBILITY
Q1 Please enter the participant's Unique ID:
________________________________________________________________
Q2 Please enter your staff initials:
________________________________________________________________
Q3 Have you used any medications not prescribed to you or street drugs in the past 30 days?
Yes (1)
No (2)
Q4 Have you lived in Maricopa County for at least 30 days?
Yes (1)
No (2)
Q5 Are you at least 18 years of age?
Yes (1)
No (2)
Q6 To the best of your knowledge, have you participated in this survey before?
Yes (1)
No (2)
Start of Block: STAFF LED - CONSENT
Q7 "Based on your responses, you are eligible to participate in our survey. Before you decide whether you
would like to continue, I am going to review the project with you and make sure you understand the goals
of the survey and your rights as a participant."
Q8 Has the participant consented to participate in this survey?
Yes (1)
No (2)
Q9 Will the participant be completing this survey independently?
Yes (1)
No (2)
Start of Block: Housing

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
51
Q10 Thank you for agreeing to take our survey. These first few questions are about your housing
status.
Q11 In the past 12 months, where have you lived? Select all that apply.
I rent or own a house, apartment, condo, or townhouse (1)
A home/apartment/condo that someone else rents or owns (2)
A hospital or rehabilitation facility (3)
Car or other vehicle (4)
Domestic violence shelter (5)
Foster care (6)
Halfway/recovery house (7)
Homeless shelter (8)
Hotel/motel (9)
Jail, prison, or detention center (10)
Street: tents, parks, public spaces, abandoned buildings (11)
Transitional housing (i.e., temporary or short-term housing) (12)
Other - please specify: (13)
Q12 In the past 12 months, where have you lived most of the time? Select one.
I rent or own a house, apartment, condo, or townhouse (1)
A home/apartment/condo that someone else rents or owns (2)
A hospital or rehabilitation facility (3)
Car or other vehicle (4)
Domestic violence shelter (5)
Foster care (6)
Halfway/recovery house (7)
Homeless shelter (8)
Hotel/motel (9)
Jail, prison, or detention center (10)
Street: tents, parks, public spaces, abandoned buildings (11)
Transitional housing (i.e., temporary or short-term housing) (12)
Other - please specify: (13)
Q13 Please look at the map. In the past 12 months, which region have you primarily lived in?
Northwest (498)
Northeast (499)
Central (500)
Southwest (501)
Southeast (502)
Q14 Have you experienced homelessness or had unstable housing in the past 12 months?
This includes living without a steady home, on the streets, in a shelter, in a single room occupancy
(SRO) hotel, or in a car, and couch-surfing.
Yes (1)
No (2)
I don't know (3)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
52
Q15 Are you currently experiencing homelessness or unstable housing?
This includes living without a steady home, on the streets, in a shelter, in a single room occupancy
(SRO) hotel, or in a car, and couch-surfing.
Yes (1)
No (2)
I don't know (3)
Q16 Have you EVER experienced homelessness or had unstable housing?
This includes living without a steady home, on the streets, in a shelter, in a single room occupancy
(SRO) hotel, or in a car, and couch-surfing.
Yes (1)
No (2)
I don't know (3)
Q17 Did any of these events or circumstances cause you to lose stable housing? *Select all that apply.*
Death of a parent/spouse/child (1)
Divorce/separation/break-up (2)
Family or friends could not afford to let me stay (3)
Family or friends stopped letting me stay with them (4)
I aged out of the foster care system (5)
I could not afford the rent increase (6)
I had an argument with family/friend/roommate (7)
I lost my job due to Covid-19 (8)
I lost my job due to another reason (9)
I was discriminated against (10)
I was evicted (11)
I was experiencing domestic violence (12)
I was managing my alcohol or drug use (13)
I was managing my physical health (14)
I was managing my mental health (15)
I went to jail/prison (16)
Other - please specify: (17)
⊗None of these (18)
Q18 What type of discrimination did you face? *Select all that apply*
Discrimination based on my age (1)
Discrimination based on my disability (2)
Discrimination based on my gender presentation (3)
Discrimination based on my race or ethnicity (4)
Discrimination based on my sexual orientation (5)
Other - please specify: (6)
Q19 You stated that you lost your job due to COVID-19. Do any of these statements help explain what
happened?
I was sick with Covid-19 and lost or quit my job (1)
I was caring for someone with Covid-19 and lost my job (2)
I was laid off because of the Covid-19 pandemic (3)
Other, please specify: (4)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
53
Q20 Have you EVER been asked to leave a shelter because of your drug use?
Yes (1)
No (2)
I don't know (3)
Q21 Have you EVER avoided going to a shelter or left a shelter because: (Select all that apply.)
I felt unsafe (1)
I was worried I would get sick (2)
I was worried my stuff would get stolen / my stuff had been stolen in the past (3)
My pet was not allowed (4)
The shelter didn't have space (5)
The shelter felt too crowded (6)
The shelter had too many rules (7)
The shelter required me to be sober (8)
There was no where to put my stuff (9)
There was not enough room for a family member, friend, or significant other (10)
The shelter was too far away from me or too difficult to get to (11)
They wanted to separate me from my family (15)
The shelter felt dirty (12)
Other - please specify: (13) __________________________________________________
⊗None of these apply (14)
Q22 It sounds like you have experienced homelessness in the past, but you are not currently
experiencing homelessness. Is there anyone or anything that helped you find a place to live?
________________________________________________________________
Q23 How long has it been since you have had a stable place to live?
A month or less (1)
1-3 months (2)
4-6 months (3)
7-11 months (4)
A year or more (5)
I don't know (6)
Q24 Are you currently interested in finding a stable place to live?
Yes (1)
No (2)
Q25 Would anything from the list below help you to find a stable place to live? *Select all that apply.*
Assistance with paying rent (1)
Assistance with moving costs (2)
Child care assistance (3)
Elder care assistance (4)
Help clearing credit (5)
Help clearing rental history (6)
Help finding affordable housing (7)
Help finding a job (8)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
54
Help finding housing for people with disabilities (9)
Help finding housing that allows a prior felony (10)
Help finding substance use treatment (11)
Immigration/refugee assistance (12)
Legal assistance (13)
Replacement ID (14)
Other - please specify: (15) __________________________________________________
⊗I don't know (16)
Q26 Do you currently receive support from an affordable housing program? This includes living in public
housing or receiving a housing voucher to help pay for rent.
Yes (1)
No (2)
No, but I am on the waitlist (3)
Q27 How long have you been on the waitlist?
Less than 1 year (1)
1-2 years (2)
More than 2 years (3)
Q28 Do you have any children under the age of 18 who live with you, or who you have regular
responsibility for?
Yes (1)
No (2)
Q29 Do you have any elders living with you, or who you have regular responsibility for?
Yes (1)
No (2)
Q30 Has a background check EVER prevented your access to housing?
Yes (1)
No (2)
I don't know (3)
Q31 Do you struggle to pay your gas and/or electric bills?
Yes (1)
No (2)
Q32 Thinking of where you have lived most of the time in the past 12 months, how often was it too
cold or too warm inside?
Always (1)
Often (2)
Sometimes (3)
Rarely (4)
Never (5)
Q33 Are there any places that you visit to stay cool during the summer? Select all that apply.
Mall (1)
Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
55
Library (2)
Community organization (3)
Senior center (4)
Friend or family member's house (5)
My own place (6)
Government building (7)
Heat relief network cooling center (8)
Other, please specify (9) __________________________________________________
⊗I do not go anywhere to cool off during the summer (10)
Q34 A cooling center is a public place people can go to cool off during hot summer days. What do you
feel are the reason(s) you may not be able to access or choose not to use a cooling center?
I was not aware that cooling centers exist (1)
I do not know how to find the location of a cooling center (2)
No transportation (3)
Pets may not be allowed (4)
Concerns about safety (5)
Too crowded (6)
Concerns about feeling welcome (7)
Do not want to be seen at a cooling center (8)
Need to care for family or friends (9)
Cooling centers are not open when I can access them (10)
I go somewhere else to cool off instead (11)
I do not want to transport all of my belongings (12)
The cooling center is not open when I need it (13)
Other, please specify (14) __________________________________________________
⊗I can go to a cooling center whenever I want, so no reasons to report (15)
Q35 Have you ever been denied entry or asked to leave a cooling center because of drug use?
Yes (1)
No (2)
Q36 Is there anything from this list that would make you more likely to use a cooling center during the
summer if it were available to you there? Select all that apply.
Naloxone or Narcan (1)
Safer drug use supplies (e.g., unused syringes, pipes) (2)
Help testing my drugs for fentanyl (3)
Hygiene kits (4)
Wound care kits (5)
Someone who can connect me to services like housing, healthcare, etc. (6)
Food (7)
Being treated better by staff (8)
Place to charge my phone (11)
Transportation to the cooling center (12)
Other, please specify (9) __________________________________________________
⊗Nothing (10)
Start of Block: Drug Use

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
56
Q37 The next few questions ask about drug use. We ask questions about drug use to inform services and
resources that can be provided so that drugs can be used more safely and to prevent overdoses.
Our team is not associated with law enforcement and will not share your information with law
enforcement. If you feel uncomfortable answering a question, you may skip it.
Q38 In the past 30 days, which of these drugs have you used for a non-medical purpose? Select all that
apply.
Benzodiazepines/Tranquilizers (e.g., downers, Xanax, Valium, Ativan, Klonopin, Ambien) (1)
Cocaine powder (2)
Crack cocaine (3)
Fentanyl (4)
Hallucinogens (e.g., acid, LSD, MDMA, PCP) (5)
Heroin (6)
Methamphetamines (meth, ice, speed) (7)
Opioid pain medications (e.g., Oxycontin, Percocet, etc.) (8)
Prescription Stimulants (e.g., Adderall, Ritalin) (9)
Other - please specify: (10) __________________________________________________
⊗I don't know (11)
Q39 Which of these drugs are your drugs of choice (i.e., the drugs you most prefer to use)?
Benzodiazepines/Tranquilizers (e.g., downers, Xanax, Valium, Ativan, Klonopin, Ambien) (1)
Cocaine powder (2)
Crack cocaine (3)
Fentanyl (4)
Hallucinogens (e.g., acid, LSD, MDMA, PCP) (5)
Heroin (6)
Methamphetamines (meth, ice, speed) (7)
Opioid pain medications (e.g., Oxycontin, Percocet, etc.) (8)
Prescription Stimulants (e.g., Adderall, Ritalin) (9)
Other - please specify: (10) __________________________________________________
⊗I don't know (11)
Q40 How do you use your drugs? Select all that apply.
Inject (1)
Smoke (2)
Snort (3)
Oral (4)
Other - please specify: (5) __________________________________________________
⊗I don't know (6)
Q41 In the past 30 days, did you use any of the following items after someone else had already used
them? Select all that apply.
Needles (1)
Cookers (2)
Straws (3)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
57
Pipes (4)
Other - please specify: (5) __________________________________________________
⊗I did not share any of my drug equipment (6)
Q42 Where do you usually get UNUSED/CLEAN equipment such as unused needles or pipe covers?
Select all that apply.
Friend or family member (1)
Doctor or health clinic (2)
Pharmacy or drug store (3)
Drug treatment center (4)
A community organization (5)
My drug dealer (6)
Other - please specify: (7) __________________________________________________
⊗I don't know (8)
Start of Block: Harm Reduction Knowledge
Q43 Are you familiar with fentanyl test strips?
Yes (1)
No (2)
Q44 Have you EVER used a fentanyl test strip?
Yes (1)
No (2)
I don't know (3)
Q45 In the past 30 days, how often did you test a new batch of drugs for fentanyl with a fentanyl test
strip?
Always (1)
Most of the time (2)
Some of the time (3)
Never (4)
I don't know (5)
Q46 Read through the list below. Do any of these statements help to explain why you do not always use
fentanyl test strips to check your drugs? Select all that apply.
I don't always carry them with me (1)
I don't have internet access to order them online (2)
I don't know how to use them (3)
I don't know where to get them (4)
I don't want to waste my drugs (5)
I have heard that fentanyl is in everything now (6)
I prefer to use drugs that contain fentanyl (7)
It costs too much to buy them (8)
It takes too long to do the test (9)
Other - please specify: (10) __________________________________________________
⊗I don't know (11)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
58
Q47 Are you interested in using fentanyl test strips?
Yes (1)
No (2)
Q48 Are you familiar with naloxone (or Narcan)?
Yes (1)
No (2)
Q49 Do you currently have naloxone/Narcan?
Yes (1)
No (2)
I don't know (3)
Q50 Where do you get naloxone/Narcan? Select all that apply.
Friend/family (1)
Hospital or Emergency Room (2)
Doctor or other health clinic (3)
Drug treatment facility (4)
Jail or prison (5)
Pharmacy or drug store (6)
Community Organization (e.g., Sonoran Prevention Works, Shot in the Dark, Southwest Recovery Alliance,
etc.) (7)
Other - please specify: (8) __________________________________________________
⊗I don't know (9)
Q51 Read through the list below. Do any of these statements help to explain why you do NOT have
naloxone/Narcan? Select all that apply.
A pharmacist told me I needed a prescription and I did not have one (1)
I don't feel comfortable using it (2)
I don't know how to use it (3)
I don't know where to get it (4)
I don't want to carry it with me everywhere (5)
I don't want other people to know that I use drugs (6)
I don't think I am at risk for an overdose (7)
I don't use opioids (8)
I used it and have not replaced it yet (9)
I worry that law enforcement would bother me (10)
It costs too much (11)
Other - please specify: (12) __________________________________________________
⊗I don't know (13)
Start of Block: Substance Use Treatment
Q52 These next few questions ask about your experiences with substance use treatment.
Q53 In the past 12 months, was there ever a time when you tried to get into a program to modify,
reduce, or stop your drug use and were not able to OR
a time when you were in a treatment program and were not able to continue?

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
59
Yes (1)
No (2)
I don't know (3)
Q54 Read through the list below. Do any of these statements help to explain any challenges that got in
the way of your ability to get treatment? *Select all that apply.*
I did not have health care coverage and could not afford the cost (1)
I had health care coverage, but it didn't cover treatment or didn't cover the full cost (2)
I could not get through on the telephone (3)
I did not know where to go for treatment / what type of treatment to start with (4)
I did not have childcare or eldercare (12)
I was not ready to stop using drugs (5)
I was treated poorly by staff (6)
The hours were inconvenient (e.g., interfered with my job) (7)
There were no openings or there was a waitlist (8)
Transportation was difficult / the treatment program was too far away (9)
Other - please specify: (10) __________________________________________________
⊗I don't know (11)
Q55 Are you currently receiving treatment to modify, reduce, or stop your drug use?
Yes (1)
No (2)
Q56 What type of treatment are you currently receiving?
Detox (1)
Medication for Opioid Use Disorder (e.g., Methadone, Suboxone, etc.) (2)
Outpatient Rehabilitation (3)
Inpatient Rehabilitation (staying overnight) (4)
One-on-One Counseling (5)
Group Counseling (6)
Peer Recovery Coaching (7)
Support Group (e.g., Narcotics Anonymous) (8)
Other - please specify: (9) __________________________________________________
⊗I don't know (10)
Q57 Which of these medications are you currently taking/receiving:
Methadone (1)
Buprenorphine (Suboxone, Subutex, Sublocade, etc.) (2)
Naltrexone (Vivitrol) (3)
⊗I don't know (4)
Q58 Are you interested in receiving treatment to modify, reduce, or stop your drug use?
Yes (1)
No (2)
I don't know (3)
Q59 What type of treatment are you interested in? Select all that apply.
Detox (1)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
60
Medication for Opioid Use Disorder (e.g., Methadone, Suboxone, etc.) (2)
Outpatient Rehabilitation (3)
Inpatient Rehabilitation (staying overnight) (4)
One-on-One Counseling (5)
Group Counseling (6)
Peer Recovery Coaching (7)
Support Group (e.g., Narcotics Anonymous) (8)
Other - please specify: (9) __________________________________________________
⊗I don't know (10)
Q60 Have you EVER tried medications to help modify, reduce, or stop your drug use?
Yes (1)
No (2)
I don't know (3)
Q61 Read through the list below. Do any of these statements help explain why you are not currently on
a medication for treating opioid use disorder?
I am not interested in using a medication to treat opioid use disorder (1)
I could not find a job while being on a medication (9)
I do not have an opioid use disorder (2)
I would be interested in using a medication SOMETIMES but not every day (3)
The medication is too expensive (4)
The programs have too many rules or requirements (5)
Transportation is difficult (6)
Other - please specify: (7) __________________________________________________
⊗I don't know (8)
Q62 Read through the list below. Would anything from the list help make getting treatment easier for
you? Select all that apply.
Help paying for treatment (1)
Help maintaining stable employment while in treatment (2)
Help with child care / elder care (3)
Help with finding or maintaining housing while in treatment (4)
Help with getting a new ID (5)
Help with getting a phone (6)
Help with transportation to appointments (7)
Fewer rules/requirements while in treatment (8)
Virtual options (e.g., telehealth) (9)
Other - please specify: (10) __________________________________________________
⊗I don't know (11)
Q63 Tell me about the rules or requirements that have made treatment difficult for you in the past.
Were any of these rules that made treatment difficult? *Select all that apply*
The program required sobriety (1)
The program did not allow me to take my prescribed medications (e.g., anxiety medications, depression
medications) (2)
Other - please specify: (3) __________________________________________________

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
61
Q64 Read through the list below. Do any of these statements help explain why you are not interested in
treatment? Select all that apply.
I am not comfortable talking to someone about my drug use (1)
I am not interested in stopping my drug use at this time (2)
I am not ready to stop using drugs right now (3)
I have tried it before and it's not for me (4)
Other - please specify: (5) __________________________________________________
⊗I don't know (6)
Start of Block: Services + Needs
Q65 The next few questions ask for your feedback about general health services and programs. This
information can help us improve services in the community.
Q66 Do you currently need any of these health services? Select all that apply.
Clothes and/or shoes (1)
Contraception (birth control, condoms) (2)
Covid, flu, or other vaccines (3)
Dental care (4)
Food assistance (19)
Help with testing drugs for fentanyl (5)
Hepatitis C testing (6)
HIV testing (7)
Hygiene kits (8)
Medications for opioid use disorder (9)
Mental health services (10)
Naloxone or Narcan (11)
Safer use supplies (e.g., unused needles or syringes, pipes) (12)
Sexually Transmitted Infection (STI) testing (13)
Sun protection (14)
Pregnancy tests (15)
Wound care kits (16)
Other - please specify: (17) __________________________________________________
⊗I don't know (18)
⊗I do not need anything (20)
Q67 Thinking about the services you said you needed, if you could get these items from a mobile unit
like a van, how likely would you be to go there?
Very likely (1)
Somewhat likely (2)
Neither likely nor unlikely (3)
Somewhat unlikely (4)
Very unlikely (5)
Q68 Please look at the map. Where in Maricopa County would it be easiest for you to access a mobile
unit that provides these services?
Northwest (502)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
62
Northeast (503)
Central (504)
Southwest (505)
Southeast (506)
Start of Block: Healthcare
Q69 Do you currently have health insurance?
Yes (1)
No (2)
I don't know (3)
Q70 Here is a list of reasons why some people do not have health insurance. Please select all the
reasons that help explain why you do not have health insurance.
It is too expensive (1)
I don't know how to sign up (2)
I am not eligible because of my immigration status (3)
I don't have a computer or phone to sign up (4)
I do not have an address to receive mail (5)
Other, please specify: (6) __________________________________________________
Q71 What kind of health insurance do you currently have? Select all that apply.
Insurance through an employer (1)
Insurance purchased from a health insurance company (e.g., Marketplace) (2)
Medicaid (AHCCCS) (3)
Medicare (4)
VA Medical Care (5)
Indian Health Service (6)
Other - please specify: (7) __________________________________________________
⊗I don't know (8)
Start of Block: Reproductive Health
Q72 Have you had a pregnancy in the past two years?
Yes, I was pregnant in the past two years (1)
Yes, I am currently pregnant (2)
No (3)
I don't know (4)
Not applicable (5)
Q73 Did you receive prenatal care?
Yes (1)
No (2)
I don't know (3)
Q74 Where did you receive your prenatal care? Select all that apply.
Adelante (1)
Circle the City (2)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
63
Mountain Park Health Center (3)
Planned Parenthood (4)
Terros (5)
Valleywise (6)
Valle del Sol (7)
Other - please specify: (8) __________________________________________________
⊗I don't know (9)
Start of Block: Demographics
Q75 What is your age (in years)?
________________________________________________________________
Q76 What is your gender identity? Select all that apply.
Man (1)
Woman (2)
Nonbinary or genderqueer (3)
I prefer to self-describe: (4) __________________________________________________
⊗I prefer not to answer (5)
Q77 What is your race and ancestral/ethnic/national origin? Select all that apply.
American Indian/Alaska Native/Native American (1)
Asian (2)
Black or African American (3)
Hispanic, Latino/a/x, or Spanish (4)
Middle Eastern or North African (5)
Native Hawaiian or other Pacific Islander (6)
White (7)
An other race or ethnicity not listed (8)
⊗I prefer not to answer (9)
Q78 What is your sexual orientation? Select all that apply.
Asexual (1)
Bisexual (2)
Gay (3)
Lesbian (4)
Pansexual (5)
Queer (6)
Questioning or unsure (7)
Straight (heterosexual) (8)
I prefer to self-describe (9) __________________________________________________
⊗I prefer not to answer (10)
Q79 Are you a veteran of the US Armed Forces?
Yes (1)
No (2)
I prefer not to answer (3)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
64
Q80 In the past 12 months, have you been in jail or prison for at least 24 hours?
Yes (1)
No (2)
I prefer not to answer (3)
Q81 Are you currently on probation or parole?
Yes (1)
No (2)
Start of Block: END
Q82 You have reached the end of our survey. Thank you so much for your time today. Is there anything
else you would like to share?
________________________________________________________________

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
65
Appendix C. Interview Guide
Introduction: Maricopa County Department of Public Health (MCDPH) wants to learn from people
most impacted by the opioid epidemic—people who use drugs. The information you share today will
help us understand your needs and will help inform harm reduction and overdose prevention
strategies in Maricopa County. MCDPH has contracted with LeCroy & Milligan Associates, an Arizona
research and evaluation company to collect data including these interviews with people who have
lived experience of homelessness and substance use. This interview will take about an hour. I will be
typing notes and voice recording it. Everything you say will be kept anonymous, and we won’t ask for
your name or any other identifying information. Nothing you tell me today will be linked to you as an
individual. As a thank you for your time, you will receive a $50 gift card.
Can I ask you some eligibility questions before we begin?
Eligibility Questions:
1. Are you currently experiencing homelessness or are you without a permanent place to live?
2. Have you used any medications not prescribed to you or street drugs in the past 30 days? (This
does not include marijuana.)
3. Have you lived in Maricopa County for at least 30 days?
4. Are you at least 18 years of age?
5. Have you completed this MCDPH interview before?
If participant answers Y to #1-4 and N to #5: You are eligible to participate in our interview. Before
we continue, I will explain this project a little more in detail and make sure you would like to still
participate.
{Interviewer reviews INFORMED CONSENT SCRIPT FOR QUALITATIVE INTERVIEW and provides
participant with INFORMED CONSENT FORM FOR INTERVIEW PARTICIPANTS. Only proceed if
participant has provided verbal consent.}
______________________________________________
Interviewer: Thank you for agreeing to meet with me. First, we will go through a list of quick
questions about your background.
Question
Response
DEMOGRAPHICS
How old are you (in years)?

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
66
What is your gender identity?
Man
Woman
Nonbinary or genderqueer
Prefer to self-describe: _______________
Declined to answer
What is your race and
ancestral/ethnic/national origin? (Select all
that apply)
American Indian/Alaskan Native/Native American
Asian
Black or African American
Hispanic, Latino/a/x, or Spanish
Middle Eastern or North African
Native Hawaiian or other Pacific Islander
White
Another race or ethnicity not listed. Write-in:
_____________________________
Declined to answer
How long have you been living in Maricopa
County?
(Select one)
<1 year
1-4 years
5-9 years
10 years or more
What is the size of your household (your family
unit)?
-People define households differently. Your
household includes you, any family member,
relative, partner, or spouse you live with who
helps pay for expenses or share resources.
1
2
3
4
5 or more
Next, I’d like to ask you a few questions about your housing status.
HOUSING
A. Tell me about your current housing
situation.
1. We think of stability as having a permanent,
safe place to live. Do you feel you need stable
housing?
2. How long have you been without a stable
place to live?
3. What led to your homelessness? Were there
any significant events in your life?
A.
1.
Yes:
No:
2.
3.

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
67
B. What has your experience been in trying to
find or maintain stable housing?
1. What challenges have you faced?
2. Have any community organizations or
government agencies helped you? Which ones?
3. Are there any community organizations or
government agencies that have NOT been
helpful or that you avoid? Why?
4. Tell me about your experience with
subsidized housing/public housing/housing
vouchers.
- Subsidized housing are government programs
that help with housing costs and expenses.
B.
1.
2.
Yes:
No:
Refused
3.
Yes:
No:
Refused
4.
Yes, has experience:
No experience:
Refused
C. Has drug use impacted your housing
situation? If so, how?
1. Did it make you (or someone you care for)
ineligible for services, shelters, or programs?
2. Did it result in you losing your housing?
C.
Yes:
No:
Refused
Yes:
No:
Refused
Yes:
No:
Refused
D. What might help you find more stable
housing?
D.
□ Don’t know:
□ Refused

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
68
Next, I’m going to ask you questions about drug use.
As a reminder, I am not going to report this information to law enforcement, and I am not a part of
law enforcement. I am not writing down your name or any other identifying information about you.
Please answer questions honestly. If you feel that a question is too personal, you can decline to
answer.
SUBSTANCE USE/OVERDOSE
E. Can you tell me about your drug use?
1. When did you first start using drugs? Which
drugs did you first use?
2. What drugs do you use now? How
frequently?
3. Are there drugs you like[d] to use together?
4. How do you prefer to use your drugs (inject,
smoke, etc.)
5. How has your drug use changed over time?
What caused these changes?
E.
1.
Refused
2.
3.
Yes:
No:
Refused
4.
Preferred method:
No preference:
Refused
5.
Yes, changed:
No change:
Refused
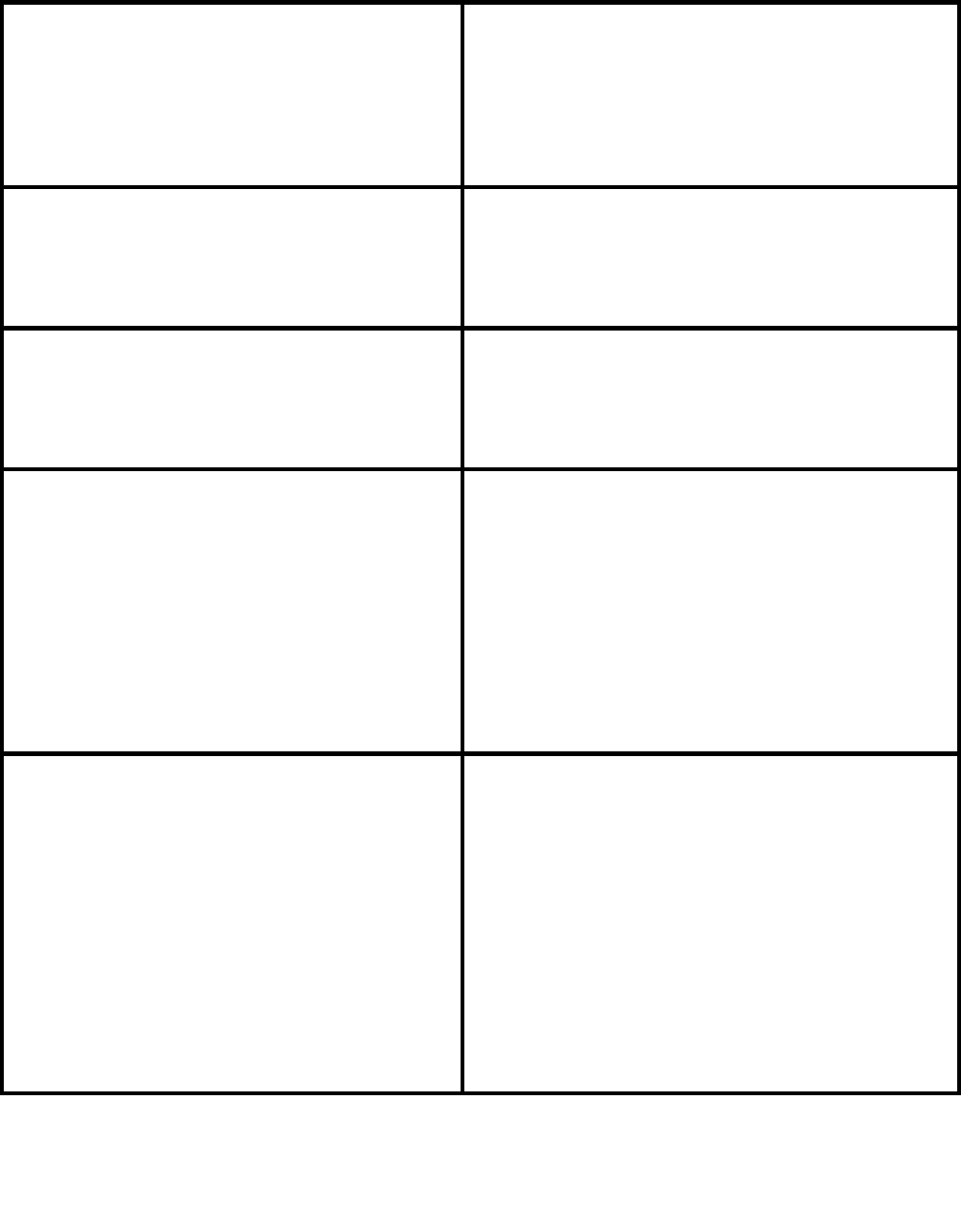
Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
69
F. Can you tell me what you know about
fentanyl?
1. What is your relationship with fentanyl? Do
you seek it out or do you try to avoid it? Why?
F.
1.
Refused
-AVOIDS fentanyl: What are some of the ways
that you try to avoid fentanyl (e.g., fentanyl test
strips)?
AVOIDS fentanyl:
Refused
-SEEKS fentanyl- How long have you been
using fentanyl? What led you to start using it?
SEEKS fentanyl-
Refused
G. Is there anything you do to protect yourself
from having an opioid overdose?
1. Do you ever use naloxone? Why/why not?
G.
Yes:
No:
Refused
1.
Yes:
No:
Refused
H. What resources or tools would be helpful
for you or others you know to protect
yourselves from an opioid overdose?
1. What would be the best way for you to get
those resources or tools?
2. Is there a location or area where you would
most prefer to pick up these types of resources
or tools?
H:
□ Don’t know:
1.
□ Don’t know:
2.
□ Don’t know:
Next, I’m going to ask you questions about treatment programs available for people who use drugs in
Maricopa County.

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
70
PERCEPTIONS OF TREATMENT OPTIONS
I: Have you ever received treatment for
substance use?
I: -RECEIVED TREATMENT- Tell me about your
experience receiving treatment for substance
use in Maricopa County.
1. What type of treatment was it?
(inpatient/outpatient rehab, one on one
counseling, group counseling, support groups)
What did you like about it? What could have
made it better?
2. How did you get connected? What was that
process like?
3. How long did it take to get in?
4. How long does it take to go from intake to
actual treatment in your experience?
5. What was your experience trying to stick to
the treatment plan? Were there any
challenges? What could have helped you stick
to the treatment plan?
HAS NOT RECEIVED TREATMENT- Can you tell
me a little more about what has prevented you
from receiving treatment for substance use?
I:
Yes:
No:
Refused
-RECEIVED TREATMENT:
1.
2.
3.
4.
5.
HAS NOT RECEIVED TREATMENT-
J. Can you tell me about any times that you
either had wanted to access a drug treatment
program, but you weren’t able to go, or you
were able to go but weren’t able to continue
treatment? {Interviewer: please specify which
scenario the individual is responding to.}
1. What challenges did you face? What got in
the way?
J.
1.

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
71
2. Is there anything that would have helped?
2.
□ Don’t know:
K. Would you share with me your thoughts on
medication for opioid use disorder
(methadone, buprenorphine, suboxone, etc.)?
1. Have you ever used medication for the
treatment of opioid use disorder? What was
your experience?
2. What are the reasons that people might like
this treatment option?
3. What are the reasons they may not like this
treatment option?
K.
1.
Yes:
No:
Don’t know:
Refused
2.
Don’t know:
3.
Don’t know:
L. Have you had experience with accessing
mobile services for harm reduction or medical
testing (syringes, fentanyl test strips, hep C
testing, HIV testing, wound care, etc.)?
EXPERIENCE WITH MOBILE SERVICES- Where
in Maricopa County would you like to see more
mobile services?
NO EXPERIENCE WITH MOBILE SERVICES-
Would this be something you would benefit
from?
1. Where in Maricopa County would you want to
see mobile services?
L:
Yes:
No:
EXPERIENCE WITH MOBILE SERVICES-
NO EXPERIENCE WITH MOBILE SERVICES-
Yes:
No:
Don’t know:
1.
Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
72
M: What mobile services would be helpful if
they were offered or what has been helpful to
receive from mobile service providers?
1. Would you want to receive these services
from a mobile unit if it were run by the county
health department?
M:
□ Don’t know
1.
Yes:
No:
N: What types of treatment or help do people
who use drugs really want, if any?
N:
□ Don’t know:
Is there anything that you wanted to add before we end today?
Final thoughts . . .
That is the end of my questions. Thank you again for sharing your time and feedback with me.
If you have any questions, {or want to refer a friend to take this survey}, here is our contact information
and resource guide.

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
73
Appendix D. Informed Consent Form
Informed Consent Form for Participants
This paper tells you about the interview. You will be given this paper to take with you. This
interview is being conducted by the Maricopa County Department of Public Health.
Your participation is voluntary (your choice). You will choose if you take this interview or not.
If you choose to do this interview and begin to answer questions, you may choose to stop at
any time without penalty or loss of benefits. You may skip any questions that you do not want
to answer. If you choose not to do this interview, there will be no penalty or loss of benefits to
which you are otherwise entitled.
Take your time to consider whether or not you will participate in this interview. Please ask ANY
question about ANY part of this form or the interview that you do not understand.
What is the purpose of this interview?
The purpose of this interview is to review specific health and housing needs and to determine
whether public health services are available or missing in the community.
What will happen if I choose to do this interview?
A staff member will lead you to a private area with a table, chair, and laptop. This way, others
will not be able to listen to your answers. Your voice along with the interviewer staff’s will be
recorded. They will also take notes that you can ask to see. The questions will ask about your
experience with housing and your experience with different high-risk behaviors. There will be
no way to identify you because we will not collect your name or any other personally
identifiable information. At the end of today’s visit, you will be given a $50 gift card for your
participation, even if you do not do all parts of the interview.
What will happen if I choose NOT to do this interview?
There will be no penalty or loss of benefits to which you are otherwise entitled.
How long will it take to complete?
It will take about 45-60 minutes to answer the interview questions and 5 minutes to receive a
gift card for your participation. (About 1 hour and 5 minutes total)
What if I want to stop being in the interview?
You can stop taking the interview at any time. You can choose to be in all parts of the interview
or only some of them. If you choose to skip questions or if you stop all together, your access to
health services will not be impacted.
Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
74
Do I have to answer every question?
No. You may skip any questions that you do not want to answer. There is no penalty for
skipping questions.
What risks can I expect from being in the interview?
The interview includes questions that ask about sensitive topics. Some people may feel
uncomfortable with these questions. Please keep in mind that you can skip any question you
do not want to answer or may stop the interview at any time. You may ask the interview staff
to give you a phone number for an organization that can provide information and referral for
these concerns.
Interview data are kept private, and we do not collect identifying information from you. It is
possible that someone you know may have seen you interested in completing the interview.
How will the interview team protect my privacy and keep my information secure?
We will protect your privacy by not asking you for your name, full birthday, address, or
any other information that can identify you. Your interview responses cannot be linked to you
as an individual. Your responses will be stored in a secure location on a computer server at
Maricopa County Department of Public Health. At no point will anyone be able to link your
responses with you as an individual.
What does it cost me for me to be in the interview?
It does not cost you any money to take this interview; however, the interview may take 45-60
minutes of your time to complete.
Will I get anything for taking part in the interview?
If you choose to take the interview, you will be given a $50 gift card today.
What are the benefits of taking part in this interview?
You will not receive any immediate, direct benefits by taking part in this interview. However,
your responses, along with responses from others in the community, will help the community
at large.
If you choose to take this interview, you will help us to better understand your health and your
experience with accessing various health and housing services in Maricopa County. Your
responses might help us identify what services you want to see for you and your peers. Your
thoughts and opinions might help us identify better ways to provide health and housing
services. All of the information that you provide will help us advocate for better services for
people who engage in high-risk health behaviors.
Who can answer my questions about the interview?
E-mail address
Phone number

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
75
You can ask the interview staff
any questions that you have.
You may also contact the
people in charge of this
interview.
[email provided]
[phone number provided]
If you have questions or would
like to voice concerns about
the interview methods, please
contact the interview
investigators.
[email provided]
[phone number provided]
If you have questions or would
like to voice concerns about
your rights as a interview
respondent or interview-related
injuries, please contact the
interview investigators.
[email provided]
[phone number provided]
Informed Consent Script for Data Collectors
SET UP:
Begin a new interview in protocol template. Confirm the potential participant is eligible by
using screening questions 1-5.
If the participant is eligible (is at least 18 years old, has lived in Maricopa County for at least 30
days, has used drugs in past 30 days, and has not participated previously), give the potential
participant the “Informed Consent Form for Interview Participants” – this full written consent
form is for the participant to take home.
Let them know that:
The “Informed Consent Form” tells them about the interview but DOES NOT include any
information about drug use.
You will read through a list of information about the interview that corresponds with the form
that you just handed them.
They can ask you any questions at any time. You have time and want to make sure they
understand the purpose of the interview and what to expect.
READ THE FOLLOWING POINTS VERBATIM:
Thank you for taking time to discuss this interview. My name is ____. Before we start, I must go
through the following script to ensure you understand the purpose of the interview and what it
means to participate.
This interview is being conducted by the Maricopa County Department of Public Health.

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
76
We are asking people who use drugs about their housing, access to harm reduction services,
access to substance use treatment options, and access to other services in the community.
Your experiences, opinions, and thoughts are important for making decisions about what
services are most important and where there need to be improvements.
The purpose of this interview is to determine whether public health services are available or
missing in the community. All of the information that you provide will help us advocate for
better services for people who use drugs.
Throughout this process, we will not ask you for your name, your full birthdate, your address,
or any type of information that could identify you as an individual. The entire process is
anonymous. Everything you tell us will be kept private – it will only be available to people
working on this interview. Your responses cannot be linked to you as an individual.
Taking part in this interview is your decision. Your choice will not affect your right to healthcare
or other services. If you decide not to participate, there will be no penalty to you.
If you agree to participate, I will interview you in a private space where only our voices will be
recorded. I will also take notes that you can ask to see. The questions will ask about your
health, your drug use, and your experience with healthcare and accessing services. You can
refuse to answer any questions. You can stop the interview at any time. There is no penalty
for skipping questions or stopping.
The interview should take about an hour to complete.
There are minimal risks from completing this interview. Some interview questions ask about
sensitive topics and might make you feel uncomfortable. Remember that you may skip any
question or stop the interview all together. I am here to discuss any concerns you have.
Interview data including notes and voice recording are kept on a password protected device.
They will be uploaded to a secured server and deleted from the password protected device on
a daily basis. We do not collect identifying information from you. It is possible that someone
you know may have seen you interested in completing the interview.
You will not receive any immediate, direct benefits by taking part in this interview. However,
your responses, along with responses from others in the community, will help the community
at large.
If you choose to complete the interview today, you will be given a $50 gift card for your
participation, even if you do not do all parts of the interview.

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
77
If you have any questions about this interview or your rights as a participant, you can talk to the
interview staff here today. You can also contact people in charge of this interview at these
phone numbers. [POINT OUT CONTACT INFORMATION ON “INFORMED CONSENT FORM”]
Take your time to consider whether or not you will participate in this interview.
Please ask ANY question about ANY part of this form or the interview that you do not
understand.

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
78
Appendix E. List of all Participant-
Suggested Locations for Mobile Services
South McClintock Drive & East Hayden Lane
19
th
Ave & Glendale Ave
Near Christown Spectrum (Bethany Home Rd
and 15
th
Ave)
51st Ave & West Baseline Rd.
19th Ave & Southern Ave
Calle Guadalupe & South Avenida del Yaqui
Near CASS, Downtown Phoenix
West Elliot Rd & Priest Dr
I-17 corridor along Central Ave, Downtown
Phoenix
19th Ave & West Broadway Rd
West Broadway Rd & South 15
th
Heat Relief Sites
Garfield, Phoenix, AZ
South Power & East Broadway
South Ellsworth Road & East Broadway Rd
Ellsworth to Signal Butte
Hermoso Park
22nd St & East Southern Ave
24th St & East Southern Ave
Bethany Home Rd & 51st Ave
North 67th Ave & West Glendale Ave
Indian School Rd & 23rd Ave
North 51st Avenue & West Van Buren Street
Washington Park
19
th
Ave & Dunlap Ave (las stop before light
rail)
South 48th Street & East Broadway Road
West Broadway Road & South Hardy Drive
(by the park)
Phoenix Indian Medical Center
Downtown Phoenix
Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
79
Appendix F. Survey Frequencies
Table 1A. Demographics
N (%)
Age Category
Ages 18-24
Ages 25-34
Ages 35-44
Ages 45-54
Ages 55-64
Ages 65+
Refused
Missing
N=525
41 (7.8%)
132 (25.1%)
157 (29.9%)
98 (18.7%)
66 (12.6%)
16 (3.0%)
1 (0.2%)
14 (2.7%)
Gender identity*
Man
Woman
Nonbinary
Self-described
Refused
Missing
N=525
300 (57.1%)
184 (35.0%)
5 (1.0%)
8 (1.5%)
10 (1.9%)
23 (4.4%)
Race/Ethnicity*
American Indian/Alaska Native/Native American
Asian
Black or African American
Hispanic, Latino/a/x, or Spanish
Middle Eastern or North African
Native Hawaiian or Pacific Islander
White
An other race or ethnicity not listed
Refused
Missing
N=525
95 (18.1%)
7 (1.3%)
80 (15.2%)
154 (29.3%)
2 (0.4%)
7 (1.3%)
188 (35.8%)
6 (1.1%)
20 (3.8%)
32 (6.1%)
Sexual Orientation*
Asexual
Bisexual
Gay
Lesbian
Pansexual
Queer
Questioning or unsure
Straight (heterosexual)
Self-described
Refused
Missing
N=525
34 (6.5%)
46 (8.8%)
17 (3.2%)
8 (1.5%)
5 (1.0%)
5 (1.0%)
5 (1.0%)
357 (68.0%)
11 (2.1%)
24 (4.6%)
44 (8.4%)
Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
80
Veteran status
Veteran
Not veteran
Refused
Missing
N=525
24 (4.6%)
444 (84.6%)
14 (2.7%)
43 (8.2%)
Do you currently have health insurance?
Yes
No
I don’t know
Missing
N=525
399 (76.0%)
75 (14.3%)
34 (6.5%)
17 (3.2%)
Here is a list of reasons why some people do not have
health insurance. Please select all the reasons that help
explain why you do not have health insurance.* (Among
individuals who did not report having health insurance.)
It is too expensive
I don’t know how to sign up
I am not eligible because of my immigration status
I don’t have a computer or phone to sign up
I do not have an address to receive mail
Other
Missing
N=75
18 (24.0%)
8 (10.7%)
8 (10.7%)
23 (30.7%)
23 (30.7%)
13 (17.3%)
4 (5.3%)
What kind of health insurance do you currently have?*
(Among individuals who reported having health insurance.)
Insurance through an employer
Insurance purchased from a health insurance company
Medicaid (AHCCCS)
Medicare
VA Medical Care
Indian Health Service
Other
I don’t know
Missing
N=399
7 (1.8%)
9 (2.3%)
329 (82.5%)
40 (10.0%)
9 (2.3%)
28 (7.0%)
12 (3.0%)
7 (1.8%)
2 (0.5%)
In the past 12 months, have you been in jail or prison for
at least 24 hours?
Yes
No
Refused
Missing
N=525
139 (26.5%)
329 (62.7%)
20 (3.8%)
37 (7.0%)
Are you currently on probation or parole? (Among individuals
who reported jail/prison.)
Yes
No
Missing
N=139
63 (45.3%)
75 (54.0%)
1 (0.7%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
81
Table 1B. Demographics – stratified by opioid use vs. non-opioid use in past 30 days
Opioid use in past 30
days
Only non-opioid use
in past 30 days
Age Category
Ages 18-24
Ages 25-34
Ages 35-44
Ages 45-54
Ages 55-64
Ages 65+
Refused
Missing
N=309
28 (9.1%)
93 (30.1%)
98 (31.7%)
43 (13.9%)
35 (11.3%)
8 (2.6%)
0 (0.0%)
4 (1.3%)
N=179
9 (5.0%)
31 (17.3%)
54 (30.2%)
47 (26.3%)
29 (16.2%)
6 (3.4%)
0 (0.0%)
3 (1.7%)
Gender identity*
Man
Woman
Nonbinary
Self-described
Refused
Missing
N=309
176 (57.0%)
116 (37.5%)
0 (0.0%)
7 (2.3%)
2 (0.6%)
10 (3.2%)
N=179
107 (59.8%)
60 (33.5%)
3 (1.7%)
1 (0.6%)
5 (2.8%)
4 (2.2%)
Race/Ethnicity*
American Indian/Alaska Native/Native
American
Asian
Black or African American
Hispanic, Latino/a/x, or Spanish
Middle Eastern or North African
Native Hawaiian or Pacific Islander
White
An other race or ethnicity not listed
Refused
Missing
N=309
57 (18.4%)
5 (1.6%)
43 (13.9%)
102 (33.0%)
0 (0.0%)
6 (1.9%)
118 (38.2%)
3 (1.0%)
11 (3.6%)
9 (2.9%)
N=179
30 (16.8%)
2 (1.1%)
31 (17.3%)
46 (25.7%)
2 (1.1%)
1 (0.6%)
64 (35.8%)
2 (1.1%)
3 (1.7%)
14 (7.8%)
Sexual Orientation*
Asexual
Bisexual
Gay
Lesbian
Pansexual
Queer
Questioning or unsure
Straight (heterosexual)
Self-described
Refused
Missing
N=309
20 (6.5%)
27 (8.7%)
6 (1.9%)
3 (1.0%)
3 (1.0%)
2 (0.7%)
2 (0.7%)
227 (73.5%)
8 (2.6%)
11 (3.6%)
13 (4.2%)
N=179
13 (7.3%)
17 (9.5%)
10 (5.6%)
4 (2.2%)
1 (0.6%)
2 (1.1%)
3 (1.7%)
114 (63.7%)
2 (1.1%)
8 (4.5%)
19 (10.6%)
Veteran status
Veteran
Not veteran
N=309
12 (3.9%)
275 (89.0%)
N=179
9 (5.0%)
148 (82.7%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
82
Refused
Missing
7 (2.3%)
15 (4.9%)
4 (2.2%)
18 (10.1%)
Do you currently have health insurance?
Yes
No
I don’t know
Missing
N=309
242 (78.3%)
45 (14.6%)
18 (5.8%)
4 (1.3%)
N=179
137 (76.5%)
27 (15.1%)
11 (6.2%)
4 (2.2%)
Here is a list of reasons why some people
do not have health insurance. Please select
all the reasons that help explain why you do
not have health insurance.* (Among those who
did not report having health insurance.)
It is too expensive
I don’t know how to sign up
I am not eligible because of my
immigration status
I don’t have a computer or phone to sign
up
I do not have an address to receive mail
Other
Missing
N=45
13 (28.9%)
7 (15.6%)
4 (8.9%)
18 (40.0%)
13 (28.9%)
5 (11.1%)
3 (6.7%)
N=27
4 (14.8%)
1 (3.7%)
4 (14.8%)
5 (18.5%)
10 (37.0%)
6 (22.2%)
1 (3.7%)
What kind of health insurance do you
currently have?* (Among those who reported having
health insurance.)
Insurance through an employer
Insurance purchased from a health
insurance company
Medicaid (AHCCCS)
Medicare
VA Medical Care
Indian Health Service
Other
I don’t know
Missing
N=242
4 (1.7%)
5 (2.1%)
204 (84.3%)
25 (10.3%)
5 (2.1%)
21 (8.7%)
7 (2.9%)
3 (1.2%)
0 (0.0%)
N=137
1 (0.7%)
4 (2.9%)
118 (86.1%)
11 (8.0%)
2 (1.5%)
4 (2.9%)
2 (1.5%)
3 (2.2%)
2 (1.5%)
In the past 12 months, have you been in jail
or prison for at least 24 hours?
Yes
No
Refused
Missing
N=309
97 (31.4%)
191 (61.8%)
10 (3.2%)
11 (3.6%)
N=179
38 (21.2%)
116 (64.8%)
7 (3.9%)
18 (10.1%)
Are you currently on probation or parole?
(Among those who reported jail/prison.)
Yes
No
Missing
N=97
44 (45.4%)
53 (54.6%)
0 (0.0%)
N=38
18 (47.4%)
19 (50.0%)
1 (2.6%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
83
Table 2A. Housing
N (%)
In the past 12 months, where have you lived?*
I rent or own a house, apartment, condo, etc.
A home/apt/condo that someone else rents or owns
A hospital or rehabilitation facility
Car or other vehicle
Domestic violence shelter
Foster care
Halfway/recovery house
Homeless shelter
Hotel/motel
Jail, prison, or detention center
Street: tents, parks, public spaces, etc.
Transitional housing (temporary or short-term housing)
Other
Missing
N=525
109 (20.8%)
162 (30.9%)
48 (9.1%)
83 (15.8%)
8 (1.5%)
7 (1.3%)
56 (10.7%)
77 (14.7%)
76 (14.5%)
60 (11.4%)
253 (48.2%)
41 (7.8%)
21 (4.0%)
7 (1.3%)
In the past 12 months, where have you lived MOST of the
time?
I rent or own a house, apartment, condo, etc.
A home/apt/condo that someone else rents or owns
A hospital or rehabilitation facility
Car or other vehicle
Domestic violence shelter
Foster care
Halfway/recovery house
Homeless shelter
Hotel/motel
Jail, prison, or detention center
Street: tents, parks, public spaces, etc.
Transitional housing (temporary or short-term housing)
Other
Missing
N=525
70 (13.3%)
78 (14.9%)
2 (0.4%)
21 (4.0%)
0 (0.0%)
0 (0.0%)
14 (2.7%)
32 (6.1%)
20 (3.8%)
8 (1.5%)
168 (32.0%)
5 (1.0%)
12 (2.3%)
95 (18.1%)
In the past 12 months, which region have you lived in?
Northwest
Northeast
Central
Southwest
Southeast
Missing
N=525
41 (7.8%)
31 (5.9%)
247 (47.0%)
101 (19.2%)
99 (18.9%)
6 (1.1%)
Have you experienced homelessness or had unstable
housing in the past 12 months?
Yes
No
I don’t know
N=525
416 (79.2%)
91 (17.3%)
12 (2.3%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
84
Missing
6 (1.1%)
Are you currently experiencing homelessness or unstable
housing? (Among those who experienced homelessness in past 12 months.)
Yes
No
I don’t know
Missing
N=416
332 (79.8%)
65 (15.6%)
7 (1.7%)
12 (2.9%)
Have you ever experienced homelessness or had unstable
housing? (Among those who did not respond “yes” to homelessness in past
12 months.)
Yes
No
I don’t know
Missing
N=109
55 (50.5%)
42 (38.5%)
6 (5.5%)
6 (5.5%)
Did any of these events or circumstances cause you to
lose stable housing?* (Among those who experienced homelessness in
past 12 months.)
Death of a parent/spouse/child
Divorce/separation/break-up
Family or friends could not afford to let me stay
Family or friends stopped letting me stay with them
I aged out of the foster care system
I could not afford the rent increase
I had an argument with family/friend/roommate
I lost my job due to Covid-19
I lost my job due to another reason
I was discriminated against
I was evicted
I was experiencing domestic violence
I was managing my alcohol or drug use
I was managing my physical health
I was managing my mental health
I went to jail/prison
Other
None of these
Missing
N=416
54 (13.0%)
76 (18.3%)
59 (14.2%)
87 (20.9%)
9 (2.2%)
95 (22.8%)
92 (22.1%)
51 (12.3%)
77 (18.5%)
39 (9.4%)
84 (20.2%)
39 (9.4%)
132 (31.7%)
46 (11.1%)
67 (16.1%)
76 (18.3%)
24 (5.8%)
14 (3.4%)
6 (1.4%)
What type of discrimination did you face?* (Among those who
reported that discrimination led to housing loss.).
Discrimination based on my age
Discrimination based on my disability
Discrimination based on my gender presentation
Discrimination based on my race or ethnicity
Discrimination based on my sexual orientation
Discrimination – other
Missing
N=39
11 (28.2%)
13 (33.3%)
8 (20.5%)
18 (46.2%)
8 (20.5%)
9 (23.1%)
1 (2.6%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
85
You stated that you lost your job due to COVID-19? Do any
of these statements help explain what happened? (Among
those who reported that job loss due to COVID-19 led to housing loss.).
I was sick with COVID-19 and lost or quit my job
I was caring for someone with COVID-19 and lost my job
I was laid off because of the COVID-19 pandemic
Other
Missing
N=51
7 (13.7%)
6 (11.8%)
31 (60.8%)
3 (5.9%)
4 (7.8%)
Have you ever been asked to leave a shelter because of
your drug use? (Among those who reported experiencing homelessness at
some point but not in past year.)
Yes
No
I don’t know
N=55
10 (18.2%)
43 (78.2%)
2 (3.6%)
Have you ever avoided going to a shelter or left a shelter
because…* (Among those who reported experiencing homelessness at
some point but not in past year.)
I felt unsafe
I was worried I would get sick
I was worried my stuff would get stolen / my stuff had
been stolen in the past
My pet was not allowed
The shelter didn’t have space
The shelter felt too crowded
The shelter had too many rules
The shelter required me to be sober
There was no where to put my stuff
There was not enough room for a family member, friend,
or significant other
The shelter was too far away from me or difficult to get
to
They wanted to separate me from my family
The shelter felt dirty
Other
None of these apply
Missing
N=55
9 (16.4%)
9 (16.4%)
7 (12.7%)
8 (14.6%)
9 (16.4%)
9 (16.4%)
3 (5.5%)
10 (18.2%)
3 (5.5%)
5 (9.1%)
7 (12.7%)
5 (9.1%)
5 (9.1%)
3 (5.5%)
17 (30.9%)
4 (7.3%)
How long has it been since you’ve had a stable place to
live? (Among those currently experiencing homelessness.)
A month or less
1-3 months
4-6 months
7-11 months
A year or more
I don’t know
Missing
N=332
20 (6.0%)
26 (7.8%)
36 (10.8%)
29 (8.7%)
202 (60.8%)
12 (3.6%)
7 (2.1%)
Are you currently interested in finding a place to live?
Yes
N=525
403 (76.8%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
86
No
Missing
114 (21.7%)
8 (1.5%)
Would anything from the list below help you find a stable
place to live?* (Among those interested in finding stable housing.)
Assistance with paying rent
Assistance with moving costs
Childcare assistance
Eldercare assistance
Help clearing credit
Help clearing rental history
Help finding affordable housing
Help finding a job
Help finding housing for people with disabilities
Help finding housing that allows a prior felony
Help finding substance use treatment
Immigration/refugee assistance
Legal assistance
Replacement ID
Other
I don’t know
Missing
N=403
268 (66.5%)
130 (32.3%)
19 (4.7%)
16 (4.0%)
114 (28.3%)
75 (18.6%)
211 (52.4%)
190 (47.1%)
67 (16.6%)
114 (28.3%)
93 (23.1%)
9 (2.2%)
51 (12.7%)
121 (30.0%)
19 (4.7%)
7 (1.7%)
5 (1.2%)
Do you currently receive support from an affordable
housing program?
Yes
No
No, but I am on the waitlist
Missing
N=525
64 (12.2%)
429 (81.7%)
20 (3.8%)
12 (2.3%)
How long have you been on the waitlist? (Among those who
reported being on housing waitlist.)
Less than 1 year
1-2 years
More than 2 years
Missing
N=20
7 (35.0%)
2 (10.0%)
10 (50.0%)
1 (5.0%)
Do you have children under the age of 18 who live with
you or whom you have regular responsibility for?
Yes
No
Missing
N=525
102 (19.4%)
415 (79.0%)
8 (1.5%)
Do you have elders living with you, or whom you have
regular responsibility for?
Yes
No
Missing
N=525
54 (10.3%)
434 (82.7%)
37 (7.0%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
87
Has a background check ever prevented your access to
housing?
Yes
No
I don’t know
Missing
N=525
141 (26.9%)
287 (54.7%)
89 (17.0%)
8 (1.5%)
Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
88
Housing 2B – stratified by opioid use vs. non-opioid use in past 30 days
Opioid use in past
30 days
Only non-opioid use
in past 30 days
In the past 12 months, where have you
lived?*
I rent or own a house, apartment, condo,
etc.
A home/apt/condo that someone else
rents or owns
A hospital or rehabilitation facility
Car or other vehicle
Domestic violence shelter
Foster care
Halfway/recovery house
Homeless shelter
Hotel/motel
Jail, prison, or detention center
Street: tents, parks, public spaces, etc.
Transitional housing (temporary or short-
term housing)
Other
Missing
N=309
62 (20.1%)
97 (31.4%)
30 (9.7%)
53 (17.2%)
3 (1.0%)
5 (1.6%)
37 (12.0%)
38 (12.3%)
49 (15.9%)
43 (13.9%)
160 (51.8%)
28 (9.1%)
10 (3.2%)
2 (0.7%)
N=179
40 (22.3%)
54 (30.2%)
9 (5.0%)
24 (13.4%)
2 (1.1%)
1 (0.6%)
12 (6.7%)
28 (15.6%)
25 (14.0%)
12 (6.7%)
83 (46.4%)
11 (6.1%)
8 (4.5%)
3 (1.7%)
In the past 12 months, where have you lived
MOST of the time?
I rent or own a house, apartment, condo,
etc.
A home/apt/condo that someone else
rents or owns
A hospital or rehabilitation facility
Car or other vehicle
Domestic violence shelter
Foster care
Halfway/recovery house
Homeless shelter
Hotel/motel
Jail, prison, or detention center
Street: tents, parks, public spaces, etc.
Transitional housing (temporary or short-
term housing)
Other
Missing
N=309
42 (13.6%)
43 (13.9%)
0 (0.0%)
15 (4.9%)
0 (0.0%)
0 (0.0%)
12 (3.9%)
12 (3.9%)
15 (4.9%)
7 (2.3%)
105 (34.0%)
3 (1.0%)
4 (1.3%)
51 (16.5%)
N=179
26 (14.5%)
27 (15.1%)
1 (0.6%)
5 (2.8%)
0 (0.0%)
0 (0.0%)
2 (1.1%)
12 (6.7%)
5 (2.8%)
1 (0.6%)
58 (32.4%)
2 (1.1%)
7 (3.9%)
33 (18.4%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
89
In the past 12 months, which region have
you lived in?
Northwest
Northeast
Central
Southwest
Southeast
Missing
N=309
24 (7.8%)
22 (7.1%)
145 (46.9%)
58 (18.8%)
58 (18.8%)
2 (0.7%)
N=179
14 (7.8%)
9 (5.0%)
86 (48.0%)
34 (19.0%)
35 (19.6%)
1 (0.6%)
Have you experienced homelessness or had
unstable housing in the past 12 months?
Yes
No
I don’t know
Missing
N=309
252 (81.6%)
48 (15.5%)
6 (1.9%)
3 (1.0%)
N=179
140 (78.2%)
36 (20.1%)
3 (1.7%)
0 (0.0%)
Are you currently experiencing
homelessness or unstable housing?
Yes
No
I don’t know
Missing
N=252
203 (80.6%)
38 (15.1%)
5 (2.0%)
6 (2.4%)
N=140
113 (80.7%)
21 (15.0%)
1 (0.7%)
5 (3.6%)
Have you ever experienced homelessness or
had unstable housing?
Yes
No
I don’t know
Missing
N=57
33 (57.9%)
21 (36.8%)
1 (1.8%)
2 (3.5%)
N=39
21 (53.8%)
16 (41.0%)
2 (5.1%)
0 (0.0%)
Did any of these events or circumstances
cause you to lose stable housing?*
Death of a parent/spouse/child
Divorce/separation/break-up
Family or friends could not afford to let me
stay
Family or friends stopped letting me stay
with them
I aged out of the foster care system
I could not afford the rent increase
I had an argument with
family/friend/roommate
I lost my job due to Covid-19
I lost my job due to another reason
I was discriminated against
I was evicted
I was experiencing domestic violence
I was managing my alcohol or drug use
I was managing my physical health
I was managing my mental health
I went to jail/prison
N=252
34 (13.5%)
48 (19.1%)
38 (15.1%)
60 (23.8%)
7 (2.8%)
61 (24.2%)
62 (24.6%)
29 (11.5%)
42 (16.7%)
22 (8.7%)
49 (19.4%)
29 (11.5%)
99 (39.3%)
29 (11.5%)
47 (18.7%)
54 (21.4%)
N=140
17 (12.1%)
24 (17.1%)
18 (12.9%)
22 (15.7%)
2 (1.4%)
29 (20.7%)
22 (15.7%)
19 (13.6%)
30 (21.4%)
12 (8.6%)
31 (22.1%)
8 (5.7%)
27 (19.3%)
15 (10.7%)
17 (12.1%)
19 (13.6%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
90
Other
None of these
Missing
10 (4.0%)
6 (2.4%)
2 (0.8%)
12 (8.6%)
6 (4.3%)
3 (2.1%)
How long has it been since you’ve had a
stable place to live?
A month or less
1-3 months
4-6 months
7-11 months
A year or more
I don’t know
Missing
N=203
12 (5.9%)
18 (8.9%)
20 (9.9%)
17 (8.4%)
124 (61.1%)
6 (3.0%)
6 (3.0%)
N=113
6 (5.3%)
8 (7.1%)
13 (11.5%)
11 (9.7%)
68 (60.2%)
6 (5.3%)
1 (0.9%)
Are you currently interested in finding a
place to live?
Yes
No
Missing
N=309
246 (79.6%)
60 (19.4%)
3 (1.0%)
N=179
134 (74.9%)
44 (24.6%)
1 (0.6%)
Would anything from the list below help you
find a stable place to live?*
Assistance with paying rent
Assistance with moving costs
Childcare assistance
Eldercare assistance
Help clearing credit
Help clearing rental history
Help finding affordable housing
Help finding a job
Help finding housing for people with
disabilities
Help finding housing that allows a prior
felony
Help finding substance use treatment
Immigration/refugee assistance
Legal assistance
Replacement ID
Other
I don’t know
Missing
N=246
177 (72.0%)
80 (32.5%)
15 (6.1%)
11 (4.5%)
77 (31.3%)
51 (20.7%)
140 (56.9%)
134 (54.5%)
36 (14.6%)
80 (32.5%)
71 (28.9%)
6 (2.4%)
35 (14.2%)
78 (31.7%)
12 (4.9%)
0 (0.0%)
3 (1.2%)
N=134
80 (59.7%)
44 (32.8%)
3 (2.2%)
5 (3.7%)
29 (21.6%)
23 (17.2%)
61 (45.5%)
48 (35.8%)
26 (19.4%)
32 (23.9%)
21 (15.7%)
3 (2.2%)
13 (9.7%)
39 (29.1%)
5 (3.7%)
6 (4.5%)
1 (0.8%)
Do you currently receive support from an
affordable housing program?
Yes
No
No, but I am on the waitlist
Missing
N=309
44 (14.2%)
253 (81.9%)
9 (2.9%)
3 (1.0%)
N=179
19 (10.6%)
149 (83.2%)
8 (4.5%)
3 (1.7%)
Has a background check ever prevented
your access to housing?
Yes
N=309
92 (29.8%)
N=179
44 (24.6%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
91
No
I don’t know
Missing
160 (51.8%)
55 (17.8%)
2 (0.7%)
103 (57.5%)
30 (16.8%)
2 (1.1%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
92
Table 3A. Energy security
N (%)
Do you struggle to pay your gas and/or electric bills?
(Among those who did not respond “yes” to current homelessness.)
Yes
No
Missing
N=193
91 (47.2%)
94 (48.7%)
8 (4.1%)
Thinking of where you have lived most of the time in the
past 12 months, how often was it too cold or too warm
inside? (Among those who did not respond “yes” to current homelessness.)
Always
Often
Sometimes
Rarely
Never
Missing
N=193
26 (13.5%)
46 (23.8%)
62 (32.1%)
25 (13.0%)
26 (13.5%)
8 (4.1%)
Are there any places that you visit to stay cool during the
summer?*
Mall
Library
Community organization
Senior center
Friend or family member’s house
My own place
Government building
Heat relief network cooling center
Other
I do not go anywhere to cool off during the summer
Missing
N=525
128 (24.4%)
193 (36.8%)
69 (13.1%)
17 (3.2%)
207 (39.4%)
104 (19.8%)
56 (10.7%)
93 (17.7%)
56 (10.7%)
57 (10.9%)
18 (3.4%)
A cooling center is a public place people go to cool off
during hot summer days. What do you feel are the
reason(s) you may not be able to choose to use a cooling
center? (Among those who reported staying cool by visiting any public place.)
I was not aware that cooling centers exist
I do not know how to find the location of a cooling
center
No transportation
Pets may not be allowed
Concerns about safety
Too crowded
Concerns about feeling welcome
Do not want to be seen at a cooling center
Need to care for family or friends
Cooling centers are not open when I can access them
I go somewhere else to cool off instead
N=455
222 (48.8%)
127 (27.9%)
156 (34.3%)
52 (11.4%)
46 (10.1%)
79 (17.4%)
80 (17.6%)
23 (5.0%)
34 (7.5%)
29 (6.4%)
54 (11.9%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
93
I do not want to transport all my belongings
The cooling center is not open when I need it
Other
I can go to a cooling center whenever I want, so no
reasons to report
63 (13.9%)
45 (9.9%)
18 (4.0%)
35 (7.7%)
Have you ever been denied entry or asked to leave a
cooling center because of drug use? (Among those currently
experiencing homelessness OR who reported energy insecurity.).
Yes
No
Missing
N=486
41 (8.4%)
399 (82.1%)
46 (9.5%)
Is there anything from this list that would make you more
likely to use a cooling center during the summer if it were
available to you there? (Among those currently experiencing
homelessness OR who reported energy insecurity.).
Naloxone or Narcan
Safer drug use supplies
Help testing my drugs for fentanyl
Hygiene kits
Wound care kits
Someone who can connect me to services like housing,
healthcare
Food
Being treated better by staff
Place to charge my phone
Transportation to the cooling center
Other
Nothing
Missing
N=486
52 (10.7%)
125 (25.7%)
65 (13.4%)
154 (31.7%)
96 (19.8%)
172 (35.4%)
234 (48.1%)
104 (21.4%)
187 (38.5%)
173 (35.6%)
17 (3.5%)
53 (10.9%)
41 (8.4%)
Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
94
Table 3B. Energy security – stratified by opioid use vs. non-opioid use in past 30 days
Opioid use in past 30
days
Only non-opioid use
in past 30 days
Do you struggle to pay your gas and/or
electric bills?
Yes
No
Missing
N=106
52 (49.1%)
51 (48.1%)
3 (2.8%)
N=66
29 (43.9%)
35 (53.0%)
2 (3.0%)
Thinking of where you have lived most of
the time in the past 12 months, how often
was it too cold or too warm inside?
Always
Often
Sometimes
Rarely
Never
Missing
N=106
15 (14.2%)
25 (23.6%)
37 (34.9%)
15 (14.2%)
11 (10.4%)
3 (2.8%)
N=66
8 (12.1%)
17 (25.8%)
18 (27.3%)
8 (12.1%)
13 (19.7%)
2 (3.0%)
Are there any places that you visit to stay
cool during the summer?*
Mall
Library
Community organization
Senior center
Friend or family member’s house
My own place
Government building
Heat relief network cooling center
Other
I do not go anywhere to cool off during
the summer
Missing
N=309
86 (27.8%)
110 (35.6%)
49 (15.9%)
14 (4.5%)
132 (42.7%)
70 (22.7%)
38 (12.3%)
45 (14.6%)
34 (11.0%)
34 (11.0%)
7 (2.3%)
N=179
33 (18.4%)
70 (39.1%)
16 (8.9%)
2 (1.1%)
62 (34.6%)
27 (15.1%)
15 (8.4%)
45 (25.1%)
16 (8.9%)
21 (11.7%)
5 (2.8%)
A cooling center is a public place people go
to cool off during hot summer days. What
do you feel are the reason(s) you may not
be able to choose to use a cooling center?
I was not aware that cooling centers exist
I do not know how to find the location of
a cooling center
No transportation
Pets may not be allowed
Concerns about safety
Too crowded
Concerns about feeling welcome
Do not want to be seen at a cooling
center
Need to care for family or friends
N=269
144 (53.5%)
78 (29.0%)
103 (38.3%)
37 (13.8%)
28 (10.4%)
48 (17.8%)
52 (19.3%)
16 (5.9%)
22 (8.2%)
N=158
67 (42.4%)
45 (28.5%)
48 (30.4%)
15 (9.5%)
14 (8.9%)
28 (17.7%)
24 (15.2%)
6 (3.8%)
11 (7.0%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
95
Cooling centers are not open when I can
access them
I go somewhere else to cool off instead
I do not want to transport all my
belongings
The cooling center is not open when I
need it
Other
I can go to a cooling center whenever I
want, so no reasons to report
Missing
18 (6.7%)
34 (12.6%)
43 (16.0%)
27 (10.0%)
3 (1.1%)
9 (3.3%)
4 (1.5%)
10 (6.3%)
18 (11.4%)
20 (12.7%)
16 (10.1%)
12 (7.6%)
10 (6.3%)
6 (3.8%)
Have you ever been denied entry or asked
to leave a cooling center because of drug
use?
Yes
No
Missing
N=293
28 (9.6%)
243 (82.9%)
22 (7.5%)
N=160
11 (6.9%)
134 (83.8%)
15 (9.4%)
Is there anything from this list that would
make you more likely to use a cooling
center during the summer if it were
available to you there?
Naloxone or Narcan
Safer drug use supplies
Help testing my drugs for fentanyl
Hygiene kits
Wound care kits
Someone who can connect me to
services like housing, healthcare
Food
Being treated better by staff
Place to charge my phone
Transportation to the cooling center
Other
Nothing
Missing
N=293
45 (15.4%)
92 (31.4%)
50 (17.1%)
103 (35.2%)
63 (21.5%)
115 (39.2%)
146 (49.8%)
69 (23.6%)
111 (37.9%)
116 (39.6%)
7 (2.4%)
26 (8.9%)
22 (7.5%)
N=160
6 (3.8%)
32 (20.0%)
14 (8.9%)
41 (25.6%)
30 (18.8%)
51 (31.9%)
81 (50.6%)
31 (19.4%)
68 (42.5%)
55 (34.4%)
7 (4.4%)
20 (12.5%)
11 (6.9%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
96
Table 4A. Drug use
N (%)
In the past 30 days, which of these drugs have you used
for a non-medical purpose?*
Benzodiazepines/tranquilizers
Cocaine powder
Crack cocaine
Fentanyl
Hallucinogens
Heroin
Methamphetamines
Opioid pain medications
Prescription stimulants
Other
I don’t know
Missing
N=525
41 (7.8%)
82 (15.6%)
51 (9.7%)
264 (50.3%)
30 (5.7%)
69 (13.1%)
342 (65.1%)
95 (18.1%)
26 (5.0%)
34 (6.5%)
11 (2.1%)
13 (2.5%)
Which of these drugs are your drugs of choice (i.e., the
drugs you most prefer to use)?*
Benzodiazepines/tranquilizers
Cocaine powder
Crack cocaine
Fentanyl
Hallucinogens
Heroin
Methamphetamines
Opioid pain medications
Prescription stimulants
Other
I don’t know
Missing
N=525
11 (2.1%)
32 (6.1%)
21 (4.0%)
192 (36.6%)
12 (2.3%)
36 (6.9%)
214 (40.8%)
36 (6.9%)
10 (1.9%)
18 (3.4%)
6 (1.1%)
107 (20.4%)
How do you use your drugs?*
Inject
Smoke
Snort
Oral
Other
I don’t know
Missing
N=525
114 (21.7%)
422 (80.4%)
136 (25.9%)
83 (15.8%)
12 (2.3%)
8 (1.5%)
15 (2.9%)
In the past 30 days, did you use any of the following
items after someone had already used them?
Needles
Cookers
Straws
Pipes
Other
N=525
46 (8.8%)
28 (5.3%)
199 (37.9%)
288 (54.9%)
13 (2.5%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
97
I did not share any of my drug equipment
Missing
124 (23.6%)
46 (8.8%)
Where do you usually get unused/clean equipment such
as unused needles or pipe covers? (Among those who did not
share drug equipment.)
Friend or family member
Doctor or health clinic
Pharmacy or drug store
Drug treatment center
A community organization
My drug dealer
Other
I don’t know
Missing
N=124
13 (10.5%)
5 (4.0%)
25 (20.2%)
5 (4.0%)
40 (32.3%)
8 (6.5%)
15 (12.1%)
30 (24.2%)
5 (4.0%)
Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
98
Table 4B. Drug use - stratified by opioid use vs. non-opioid use in past 30 days
Opioid use in past
30 days
Only non-opioid use
in past 30 days
In the past 30 days, which of these drugs have
you used for a non-medical purpose?*
Benzodiazepines/tranquilizers
Cocaine powder
Crack cocaine
Fentanyl
Hallucinogens
Heroin
Methamphetamines
Opioid pain medications
Prescription stimulants
Other
I don’t know
Missing
N=309
29 (9.4%)
47 (15.2%)
38 (12.3%)
264 (85.4%)
24 (7.7%)
69 (22.3%)
206 (66.7%)
95 (30.7%)
19 (6.2%)
9 (2.9%)
0 (0.0%)
0 (0.0%)
N=179
12 (6.7%)
35 (19.6%)
13 (7.3%)
0 (0.0%)
6 (3.4%)
0 (0.0%)
136 (76.0%)
0 (0.0%)
7 (3.9%)
7 (3.9%)
0 (0.0%)
0 (0.0%)
Which of these drugs are your drugs of choice
(i.e., the drugs you most prefer to use)?*
Benzodiazepines/tranquilizers
Cocaine powder
Crack cocaine
Fentanyl
Hallucinogens
Heroin
Methamphetamines
Opioid pain medications
Prescription stimulants
Other
I don’t know
Missing
N=309
8 (2.6%)
15 (4.9%)
14 (4.5%)
192 (62.1%)
10 (3.2%)
36 (11.7%)
117 (37.9%)
36 (11.7%)
6 (1.9%)
3 (1.0%)
0 (0.0%)
32 (10.4%)
N=179
3 (1.7%)
17 (9.5%)
7 (3.9%)
0 (0.0%)
2 (1.1%)
0 (0.0%)
96 (53.6%)
0 (0.0%)
4 (2.2%)
5 (2.8%)
0 (0.0%)
55 (30.7%)
How do you use your drugs?*
Inject
Smoke
Snort
Oral
Other
I don’t know
Missing
N=309
81 (26.2%)
264 (85.4%)
79 (25.6%)
50 (16.2%)
3 (1.0%)
4 (1.3%)
3 (1.0%)
N=179
31 (17.3%)
138 (77.1%)
53 (29.6%)
29 (16.2%)
3 (1.7%)
1 (0.6%)
2 (1.1%)
In the past 30 days, did you use any of the
following items after someone had already
used them?
Needles
Cookers
Straws
Pipes
N=309
39 (12.6%)
22 (7.1%)
172 (55.7%)
182 (58.9%)
N=179
6 (3.4%)
5 (2.8%)
26 (14.5%)
99 (55.3%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
99
Other
I did not share any of my drug equipment
Missing
6 (1.9%)
63 (20.4%)
19 (6.1%)
2 (1.1%)
47 (26.3%)
15 (8.4%)
Where do you usually get unused/clean
equipment such as unused needles or pipe
covers?
Friend or family member
Doctor or health clinic
Pharmacy or drug store
Drug treatment center
A community organization
My drug dealer
Other
I don’t know
Missing
N=63
7 (11.1%)
4 (6.3%)
17 (27.0%)
3 (4.8%)
24 (38.1%)
3 (4.8%)
6 (9.5%)
11 (17.5%)
1 (1.6%)
N=47
5 (10.6%)
1 (2.1%)
8 (17.0%)
2 (4.3%)
14 (29.8%)
4 (8.5%)
7 (14.9%)
13 (27.7%)
2 (4.3%)
Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
100
Table 5A. Fentanyl test strips
N (%)
Are you familiar with fentanyl test strips?
Yes
No
Missing
N=333
138 (41.4%)
180 (54.1%)
15 (4.5%)
Have you ever used a fentanyl test strip? (Among those who
were familiar with fentanyl test strips.).
Yes
No
I don’t know
Missing
N=138
66 (47.8%)
69 (50.0%)
1 (0.7%)
2 (1.4%)
In the past 30 days, how often did you test a new batch of
drugs with a fentanyl test strip? (Among those who reported ever
using fentanyl test strips.).
Always
Most of the time
Some of the time
Never
I don’t know
N=66
17 (25.8%)
11 (16.7%)
17 (25.8%)
19 (28.8%)
2 (3.0%)
Read through the list below. Do any of these statements
help explain why you do not always use fentanyl test
strips to check your drugs?* (Among those who reported ever using
fentanyl test strips but did not always use them.) .
I don’t always carry them with me
I don’t have internet access to order them online
I don’t know how to use them
I don’t know where to get them
I don’t want to waste my drugs
I have heard that fentanyl is in everything now
I prefer to use drugs that contain fentanyl
It costs too much to buy them
It takes too long to do the test
Other
I don’t know
Missing
N=49
19 (38.8%)
7 (14.3%)
3 (6.1%)
10 (20.4%)
10 (20.4%)
10 (20.4%)
2 (4.1%)
7 (14.3%)
7 (14.3%)
5 (10.2%)
1 (2.0%)
1 (2.0%)
Are you interested in using fentanyl test strips? (Among those
familiar with fentanyl test strips who had not used them.)
Yes
No
Missing
N=69
22 (31.9%)
46 (66.7%)
1 (1.4%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
101
Table 5B. Fentanyl test strips - stratified by opioid use vs. non-opioid use in past 30 days
Opioid use in past 30
days
Only non-opioid use
in past 30 days
Are you familiar with fentanyl test strips?
Yes
No
Missing
N=117
52 (44.4%)
62 (53.0%)
3 (2.6%)
N=179
80 (44.7%)
97 (54.2%)
2 (1.1%)
Have you ever used a fentanyl test strip?
Yes
No
I don’t know
Missing
N=52
29 (55.8%)
22 (42.3%)
0 (0.0%)
1 (1.9%)
N=80
36 (45.0%)
43 (53.8%)
0 (0.0%)
1 (1.3%)
In the past 30 days, how often did you test
a new batch of drugs with a fentanyl test
strip?
Always
Most of the time
Some of the time
Never
I don’t know
N=29
7 (24.1%)
6 (20.7%)
8 (27.6%)
7 (24.1%)
1 (3.4%)
N=36
10 (27.8%)
5 (13.9%)
9 (25.0%)
11 (30.6%)
1 (2.8%)
Read through the list below. Do any of
these statements help explain why you do
not always use fentanyl test strips to check
your drugs?*
I don’t always carry them with me
I don’t have internet access to order them
online
I don’t know how to use them
I don’t know where to get them
I don’t want to waste my drugs
I have heard that fentanyl is in everything
now
I prefer to use drugs that contain fentanyl
It costs too much to buy them
It takes too long to do the test
Other
I don’t know
Missing
N=22
8 (36.4%)
2 (9.1%)
2 (9.1%)
4 (18.2%)
4 (18.2%)
8 (36.4%)
2 (9.1%)
3 (13.6%)
4 (18.2%)
3 (13.6%)
0 (0.0%)
1 (4.5%)
N=26
11 (42.3%)
5 (19.2%)
1 (3.9%)
6 (23.1%)
6 (23.1%)
2 (7.7%)
0 (0.0%)
4 (15.4%)
2 (7.7%)
2 (7.7%)
1 (3.9%)
0 (0.0%)
Are you interested in using fentanyl test
strips?
Yes
No
Missing
N=22
6 (27.3%)
16 (72.7%)
0 (0.0%)
N=43
15 (34.9%)
27 (62.8%)
1 (2.3%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
102
Table 6A. Naloxone
N (%)
Are you familiar with naloxone (or Narcan)?
Yes
No
Missing
N=525
399 (76.0%)
108 (20.6%)
18 (3.4)
Do you currently have naloxone/Narcan? (Among those familiar
with naloxone.) .
Yes
No
I don’t know
Missing
N=399
275 (68.9%)
111 (27.8%)
5 (1.3%)
8 (2.0%)
Where do you get naloxone/Narcan?* (Among those who
reported currently having naloxone.) .
Friend/family
Hospital or emergency room
Doctor or other health clinic
Drug treatment facility
Jail or prison
Pharmacy or drug store
Community organization
Other
I don’t know
Missing
N=275
56 (20.4%)
22 (8.0%)
53 (19.3%)
63 (22.9%)
13 (4.7%)
28 (10.2%)
150 (54.5%)
9 (3.3%)
3 (1.1%)
2 (0.7%)
Read through the list below. Do any of these statements
help to explain why you do not have naloxone/Narcan?*
(Among those familiar with naloxone who did not currently have access.)
A pharmacist told me I needed a prescription, and I did
not have one
I don’t feel comfortable using it
I don’t know how to use it
I don’t know where to get it
I don’t want to carry it with me everywhere
I don’t want other people to know that I use drugs
I don’t think I am at risk for an overdose
I don’t use opioids
I used it and have not replaced it yet
I worry that law enforcement would bother me
It costs too much
Other
I don’t know
Missing
N=111
7 (6.3%)
2 (1.8%)
17 (15.3%)
29 (26.1%)
14 (12.6%)
8 (7.2%)
28 (25.2%)
22 (19.8%)
8 (7.2%)
14 (12.6%)
7 (6.3%)
5 (4.5%)
8 (7.2%)
3 (2.7%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
103
Table 6B. Naloxone – stratified by opioid use vs. non-opioid use in past 30 days
Opioid use in past 30
days
Only non-opioid use
in past 30 days
Are you familiar with naloxone (or Narcan)?
Yes
No
Missing
N=309
265 (85.8%)
40 (12.9%)
4 (1.3%)
N=179
118 (65.9%)
57 (31.8%)
4 (2.2%)
Do you currently have naloxone/Narcan?
Yes
No
I don’t know
Missing
N = 265
202 (76.2%)
59 (22.3%)
2 (0.8%)
2 (0.8%)
N=118
67 (56.8%)
44 (37.3%)
1 (0.9%)
6 (5.1%)
Where do you get naloxone/Narcan?*
Friend/family
Hospital or emergency room
Doctor or other health clinic
Drug treatment facility
Jail or prison
Pharmacy or drug store
Community organization
Other
I don’t know
Missing
N=202
48 (23.8%)
19 (9.4%)
41 (20.3%)
51 (25.3%)
10 (5.0%)
21 (10.4%)
103 (51.0%)
7 (3.5%)
3 (1.5%)
1 (0.5%)
N=67
8 (11.9%)
2 (3.0%)
10 (14.9%)
10 (14.9%)
2 (3.0%)
5 (7.5%)
43 (64.2%)
2 (3.0%)
0 (0.0%)
1 (1.5%)
Read through the list below. Do any of
these statements help to explain why you
do not have naloxone/Narcan?*
A pharmacist told me I needed a
prescription, and I did not have one
I don’t feel comfortable using it
I don’t know how to use it
I don’t know where to get it
I don’t want to carry it with me
everywhere
I don’t want other people to know that I
use drugs
I don’t think I am at risk for an overdose
I don’t use opioids
I used it and have not replaced it yet
I worry that law enforcement would
bother me
It costs too much
Other
I don’t know
Missing
N=59
7 (11.9%)
2 (3.4%)
13 (22.0%)
18 (30.5%)
6 (10.2%)
5 (8.5%)
18 (30.5%)
3 (5.1%)
5 (8.5%)
7 (11.9%)
5 (8.5%)
1 (1.7%)
7 (11.9%)
1 (1.9%)
N=44
0 (0.0%)
0 (0.0%)
3 (6.8%)
9 (20.5%)
7 (15.9%)
3 (6.8%)
7 (15.9%)
17 (38.6%)
3 (6.8%)
7 (15.9%)
2 (4.6%)
2 (4.6%)
1 (2.3%)
2 (4.6%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
104
Table 7A. Substance use treatment
N (%)
In the past six months, was there ever a time when you
tried to get into a program to modify, reduce, or stop your
drug use and were not able to OR a time when you were in
a treatment program and were not able to continue?
Yes
No
I don’t know
Missing
N=525
208 (39.6%)
271 (51.6%)
31 (5.9%)
15 (2.9%)
Read through the list below. Do any of these statements
help to explain the challenges that got in the way of your
treatment?* (Among those who reported trying substance use treatment in
past six months and not being able to continue.)
I do not have health care coverage and could not afford
the cost
I had health care coverage, but it didn’t cover treatment
or didn’t cover the full cost
I could not get through on the telephone
I did not know where to go for treatment and/or what
type of treatment to start with
I did not have childcare or eldercare
I was not ready to stop using drugs
I was treated poorly by staff
The hours were inconvenient
There were no openings or there was a waitlist
Transportation was difficult and/or the treatment
program was too far away
Other
I don’t know
Missing
N=208
38 (18.3%)
36 (17.3%)
34 (16.3%)
38 (18.3%)
10 (4.8%)
87 (41.8%)
51 (24.5%)
15 (7.2%)
54 (26.0%)
49 (23.6%)
16 (7.7%)
9 (4.3%)
7 (3.4%)
Are you currently receiving treatment to modify, reduce,
or stop your drug use?
Yes
No
Missing
N=525
178 (33.9%)
328 (62.5%)
19 (3.6%)
What type of treatment are you currently receiving?*
(Among those currently receiving substance use treatment.).
Detox
Medication for opioid use disorder
Outpatient rehabilitation
Inpatient rehabilitation
One-on-one counseling
Group counseling
Peer recovery coaching
N=178
20 (11.2%)
92 (51.7%)
53 (29.8%)
16 (9.0%)
47 (26.4%)
33 (18.5%)
19 (10.7%)
Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
105
Support group
Other
I don’t know
Missing
25 (14.0%)
15 (8.4%)
7 (3.9%)
1 (0.6%)
Which of these medications are you currently
taking/receiving? (Among those currently receiving MOUD.)
Methadone
Buprenorphine (Suboxone, Subutex, Sublocade, etc.)
Naltrexone (Vivitrol)
I don’t know
Missing
N=92
81 (88.0%)
4 (4.3%)
1 (1.1%)
5 (5.4%)
1 (1.1%)
Are you interested in receiving treatment to modify,
reduce, or stop your drug use? (Among those who did not respond
“yes” to currently receiving substance use treatment.) .
Yes
No
I don’t know
Missing
N=347
147 (42.4%)
110 (31.7%)
74 (21.3%)
16 (4.6%)
What type of treatment are you interested in?* (Among those
interested in treatment.).
Detox
Medication for opioid use disorder
Outpatient rehabilitation
Inpatient rehabilitation
One-on-one counseling
Group counseling
Peer recovery coaching
Support group
Other
I don’t know
Missing
N=147
81 (55.1%)
52 (35.4%)
47 (32.0%)
49 (33.3%)
44 (29.9%)
22 (15.0%)
34 (23.1%)
29 (19.7%)
3 (2.0%)
8 (5.4%)
2 (1.4%)
Have you ever tried medications to help modify, reduce,
or stop your drug use? (Among those who were not currently receiving
MOUD.).
Yes
No
I don’t know
Missing
N=433
154 (35.6%)
235 (54.3%)
19 (4.4%)
25 (5.8%)
Read through the list below. Do any of these statements
help to explain why you are not currently on a medication
for treating opioid use disorder?* (Among those currently in
treatment exclusive of MOUD or who were interested in treatment but did not
select MOUD.)
I am not interested in using a medication to treat opioid
use disorder
I could not find a job while being on a medication
I do not have an opioid use disorder
N=181
32 (17.7%)
21 (11.6%)
55 (30.4%)
32 (17.7%)
Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
106
I would be interested in using a medication sometimes
but not every day
The medication is too expensive
The programs have too many rules or requirements
Transportation is difficult
Other
I don’t know
Missing
25 (13.8%)
23 (12.7%)
24 (13.3%)
8 (4.4%)
19 (10.5%)
7 (3.9%)
Read through the list below. Would anything from the list
help make getting treatment easier for you? (Among those
currently in treatment or interested in treatment.).
Help paying for treatment
Help maintaining stable employment while in treatment
Help with childcare / eldercare
Help with finding or maintaining housing while in
treatment
Help with getting a new ID
Help with getting a phone
Help with transportation to appointments
Fewer rules/requirements while in treatment
Virtual options (e.g., telehealth)
Other
I don’t know
Missing
N=325
106 (32.6%)
112 (34.5%)
28 (8.6%)
142 (43.7%)
102 (31.4%)
114 (35.1%)
133 (40.9%)
82 (25.2%)
52 (16.0%)
12 (3.7%)
25 (7.7%)
12 (3.7%)
Tell me about the rules or requirements that have made
treatment difficult for you in the past. Were any of these
rules that made treatment difficult?* (Among those who
responded that fewer rules would make treatment easier.)
The program required sobriety
The program did not allow me to take my prescribed
medications (e.g., anxiety or depression medication)
Other
Missing
N=82
42 (51.2%)
26 (31.7%)
22 (26.8%)
11 (13.4%)
Read through the list below. Do any of these statements
help explain why you are not interested in treatment?*
(Among those who were not interested in treatment.).
I am not comfortable talking to someone about my drug
use
I am not interested in stopping my drug use at this time
I am not ready to stop using drugs right now
I have tried it before and it’s not for me
Other
I don’t know
Missing
N=110
16 (14.5%)
34 (30.9%)
35 (31.8%)
26 (23.6%)
12 (10.9%)
14 (12.7%)
2 (1.8%)
Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
107
Table 7B. Substance use treatment - stratified by opioid use vs. non-opioid use in past 30 days
Opioid use in past 30
days
Only non-opioid
use in past 30 days
In the past six months, was there ever a
time when you tried to get into a program to
modify, reduce, or stop your drug use and
were not able to OR a time when you were in
a treatment program and were not able to
continue?
Yes
No
I don’t know
Missing
N=309
134 (43.4%)
151 (48.9%)
18 (5.8%)
6 (1.9%)
N=179
64 (35.8%)
105 (58.7%)
9 (5.0%)
1 (0.6%)
Read through the list below. Do any of these
statements help to explain the challenges
that got in the way of your treatment?*
I do not have health care coverage and
could not afford the cost
I had health care coverage, but it didn’t
cover treatment or didn’t cover the full cost
I could not get through on the telephone
I did not know where to go for treatment
and/or what type of treatment to start with
I did not have childcare or eldercare
I was not ready to stop using drugs
I was treated poorly by staff
The hours were inconvenient
There were no openings or there was a
waitlist
Transportation was difficult and/or the
treatment program was too far away
Other
I don’t know
Missing
N=134
26 (19.4%)
21 (15.7%)
29 (21.6%)
25 (18.7%)
5 (3.7%)
63 (47.0%)
34 (25.4%)
11 (8.2%)
38 (28.4%)
34 (25.4%)
9 (6.7%)
5 (3.7%)
1 (0.8%)
N=64
9 (14.1%)
12 (18.8%)
4 (6.3%)
12 (18.8%)
4 (6.3%)
22 (34.4%)
13 (20.3%)
4 (6.3%)
14 (21.9%)
14 (21.9%)
4 (6.3%)
4 (6.3%)
4 (6.3%)
Are you currently receiving treatment to
modify, reduce, or stop your drug use?
Yes
No
Missing
N=309
116 (37.5%)
186 (60.2%)
7 (2.3%)
N=179
46 (25.7%)
131 (73.2%)
2 (1.1%)
What type of treatment are you currently
receiving?*
Detox
Medication for opioid use disorder
Outpatient rehabilitation
Inpatient rehabilitation
One-on-one counseling
N=116
12 (10.3%)
68 (58.6%)
37 (31.9%)
10 (8.6%)
32 (27.6%)
N=46
8 (17.4%)
18 (39.1%)
10 (21.7%)
4 (8.7%)
10 (21.7%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
108
Group counseling
Peer recovery coaching
Support group
Other
I don’t know
Missing
21 (18.1%)
11 (9.5%)
16 (13.8%)
8 (6.9%)
4 (3.4%)
1 (0.9%)
7 (15.2%)
5 (10.9%)
7 (15.2%)
5 (10.9%)
0 (0.0%)
0 (0.0%)
Which of these medications are you
currently taking/receiving?
Methadone
Buprenorphine (Suboxone, Subutex,
Sublocade, etc.)
Naltrexone (Vivitrol)
I don’t know
Missing
N=68
60 (88.2%)
3 (4.4%)
1 (1.5%)
4 (5.9%)
0 (0.0%)
N=18
17 (94.4%)
1 (5.6%)
0 (0.0%)
0 (0.0%)
0 (0.0%)
Are you interested in receiving treatment to
modify, reduce, or stop your drug use?
Yes
No
I don’t know
Missing
N=193
95 (49.2%)
57 (29.5%)
34 (17.6%)
7 (3.6%)
N=133
48 (36.1%)
47 (35.3%)
37 (27.8%)
1 (0.8%)
What type of treatment are you interested
in?*
Detox
Medication for opioid use disorder
Outpatient rehabilitation
Inpatient rehabilitation
One-on-one counseling
Group counseling
Peer recovery coaching
Support group
Other
I don’t know
Missing
N=95
67 (70.5%)
48 (50.5%)
32 (33.7%)
38 (40.0%)
28 (29.5%)
14 (14.7%)
21 (22.1%)
19 (20.0%)
1 (1.5%)
2 (2.1%)
0 (0.0%)
N=48
14 (29.2%)
4 (8.3%)
14 (29.2%)
11 (22.9%)
16 (33.3%)
8 (16.7%)
12 (25.0%)
10 (20.8%)
1 (2.1%)
6 (12.5%)
1 (2.1%)
Have you ever tried medications to help
modify, reduce, or stop your drug use?
Yes
No
I don’t know
Missing
N=241
110 (45.6%)
113 (46.9%)
8 (3.3%)
10 (4.2%)
N=161
37 (23.0%)
110 (68.3%)
7 (4.4%)
7 (4.4%)
Read through the list below. Do any of these
statements help to explain why you are not
currently on a medication for treating opioid
use disorder?*
I am not interested in using a medication
to treat opioid use disorder
I could not find a job while being on a
medication
N=95
20 (21.1%)
15 (15.8%)
N=72
7 (9.7%)
6 (8.3%)
Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
109
I do not have an opioid use disorder
I would be interested in using a
medication sometimes but not every day
The medication is too expensive
The programs have too many rules or
requirements
Transportation is difficult
Other
I don’t know
Missing
12 (12.6%)
24 (25.3%)
17 (17.9%)
17 (17.9%)
19 (20.0%)
5 (5.3%)
6 (6.3%)
4 (4.2%)
40 (55.6%)
8 (11.1%)
8 (11.1%)
5 (6.9%)
4 (5.6%)
0 (0.0%)
10 (13.9%)
3 (4.2%)
Read through the list below. Would anything
from the list help make getting treatment
easier for you?
Help paying for treatment
Help maintaining stable employment
while in treatment
Help with childcare / eldercare
Help with finding or maintaining housing
while in treatment
Help with getting a new ID
Help with getting a phone
Help with transportation to appointments
Fewer rules/requirements while in
treatment
Virtual options (e.g., telehealth)
Other
I don’t know
Missing
N=211
77 (36.5%)
83 (39.3%)
19 (9.0%)
103 (48.8%)
72 (34.1%)
84 (39.8%)
100 (47.4%)
56 (26.5%)
32 (15.2%)
8 (3.8%)
10 (4.7%)
6 (2.8%)
N=94
26 (27.7%)
26 (27.7%)
7 (7.5%)
34 (36.2%)
26 (27.7%)
24 (25.5%)
30 (31.9%)
21 (22.3%)
16 (17.0%)
1 (1.1%)
9 (9.6%)
4 (4.3%)
Tell me about the rules or requirements that
have made treatment difficult for you in the
past. Were any of these rules that made
treatment difficult?*
The program required sobriety
The program did not allow me to take my
prescribed medications (e.g., anxiety or
depression medication)
Other
Missing
N=56
28 (50.0%)
19 (33.9%)
14 (25.0%)
8 (14.3%)
N=21
13 (61.9%)
4 (19.1%)
5 (23.8%)
2 (9.5%)
Read through the list below. Do any of these
statements help explain why you are not
interested in treatment?*
I am not comfortable talking to someone
about my drug use
I am not interested in stopping my drug
use at this time
I am not ready to stop using drugs right
now
N=57
8 (14.0%)
21 (36.8%)
23 (40.4%)
N=47
8 (17.0%)
12 (25.5%)
10 (21.3%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
110
I have tried it before and it’s not for me
Other
I don’t know
Missing
16 (28.1%)
4 (7.0%)
7 (12.3%)
0 (0.0%)
9 (19.2%)
7 (14.9%)
6 (12.8%)
1 (2.1%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
111
Table 8A. Health services
N (%)
Do you currently need any of these health services?
Clothes and/or shoes
Contraception (birth control, condoms)
Covid, flu, or other vaccines
Dental care
Food assistance
Help with testing drugs for fentanyl
Hepatitis C testing
HIV testing
Hygiene kits
Medications for opioid use disorder
Mental health services
Naloxone or Narcan
Safer use supplies (e.g., unused needles, pipes)
Sexually Transmitted Infection (STI) testing
Sun protection
Pregnancy tests
Wound care kits
Other
I don’t know
I do not need anything
Missing
N=525
243 (46.3%)
45 (8.6%)
41 (7.8%)
254 (48.4%)
261 (49.7%)
77 (14.7%)
53 (10.1%)
53 (10.1%)
170 (32.4%)
91 (17.3%)
138 (26.3%)
77 (14.7%)
103 (19.6%)
63 (12.0%)
85 (16.2%)
24 (4.6%)
103 (19.6%)
26 (5.0%)
18 (3.4%)
47 (9.0%)
17 (3.2%)
Thinking about the services you said you needed, if you
could get them from a mobile unit like a van, how likely
would you be to go there?
Very likely
Somewhat likely
Neither likely nor unlikely
Somewhat unlikely
Very unlikely
Missing
N=525
302 (57.5%)
84 (16.0%)
33 (6.3%)
17 (3.2%)
15 (2.9%)
74 (14.1%)
Where in Maricopa County would it be easiest for you to
access a mobile unit that provides these services?
Northwest
Northeast
Central
Southwest
Southeast
Missing
N=525
28 (5.3%)
36 (6.9%)
227 (43.2%)
65 (12.4%)
83 (15.8%)
86 (16.4%)
Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
112
Table 8B. Health services - stratified by opioid use vs. non-opioid use in past 30 days
Opioid use in past 30
days
Only non-opioid
use in past 30 days
Do you currently need any of these health
services?
Clothes and/or shoes
Contraception (birth control, condoms)
Covid, flu, or other vaccines
Dental care
Food assistance
Help with testing drugs for fentanyl
Hepatitis C testing
HIV testing
Hygiene kits
Medications for opioid use disorder
Mental health services
Naloxone or Narcan
Safer use supplies (e.g., unused needles,
pipes)
Sexually Transmitted Infection (STI)
testing
Sun protection
Pregnancy tests
Wound care kits
Other
I don’t know
I do not need anything
Missing
N=309
153 (49.5%)
27 (8.7%)
22 (7.1%)
163 (52.8%)
167 (54.1%)
59 (19.1%)
33 (10.7%)
31 (10.0%)
108 (35.0%)
77 (24.9%)
86 (27.8%)
58 (18.8%)
71 (23.0%)
35 (11.3%)
53 (17.2%)
16 (5.2%)
62 (20.1%)
13 (4.2%)
10 (3.2%)
22 (7.1%)
4 (1.3%)
N=179
79 (44.1%)
13 (7.3%)
15 (8.4%)
82 (45.8%)
83 (46.4%)
17 (9.5%)
15 (8.4%)
16 (8.9%)
54 (30.2%)
12 (6.7%)
43 (24.0%)
17 (9.5%)
32 (17.9%)
23 (12.9%)
32 (17.9%)
6 (3.4%)
37 (20.7%)
10 (5.6%)
5 (2.8%)
21 (11.7%)
5 (2.8%)
Thinking about the services you said you
needed, if you could get them from a mobile
unit like a van, how likely would you be to go
there?
Very likely
Somewhat likely
Neither likely nor unlikely
Somewhat unlikely
Very unlikely
Missing
N=309
196 (63.4%)
50 (16.2%)
22 (7.1%)
9 (2.9%)
6 (1.9%)
26 (8.4%)
N=179
97 (54.2%)
29 (16.2%)
8 (4.5%)
6 (3.4%)
8 (4.5%)
31 (17.3%)
Where in Maricopa County would it be
easiest for you to access a mobile unit that
provides these services?
Northwest
Northeast
Central
Southwest
Southeast
N=309
21 (6.8%)
26 (8.4%)
134 (43.4%)
42 (13.6%)
53 (17.2%)
N=179
5 (2.8%)
8 (4.5%)
81 (45.3%)
20 (11.2%)
26 (14.5%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
113
Missing
33 (10.7%)
39 (21.8%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
114
Table 9. Reproductive health
N (%)
Have you had a pregnancy in the past two years?
Yes, I was pregnant in the past two years
Yes, I am currently pregnant
No
I don’t know
Not applicable
Missing
N=525
28 (5.3%)
17 (3.2%)
296 (56.4%)
20 (3.8%)
132 (25.1%)
32 (6.1%)
Did you receive prenatal care? (Among those who were pregnant in
the past two years.).
Yes
No
I don’t know
N=28
15 (53.6%)
12 (42.9%)
1 (3.6%)

Maricopa County • Department of Public Health • Division of Epidemiology • October 2023
115
Maricopa County
Department of Public Health
Division of Epidemiology
