© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
Hospice: Leading Interdisciplinary Care
Dobson DaVanzo & Associates, LLC Vienna, VA 703.260.1760 www.dobsondavanzo.com

© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
Hospice: Leading Interdisciplinary Care
Submitted to:
The National Hospice and Palliative Care Organization
Submitted by:
Dobson|DaVanzo
Joan E. DaVanzo, Ph.D., M.S.W.
Dorothy Chen, M.P.H.
Jessica Greene, M.P.H.
Allen Dobson, Ph.D.
Monday, March 25, 2019 — Final Report

© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
In 1967, Dame Cicely Saunders founded St. Christopher’s Hospice in south west London. It
is now one of many but is still the leader in the field. It was her personal achievement and
has been imitated all over the world.
St. Christopher’s was the first modern hospice, although there were a number of homes in
existence for the dying, most of which were run by religious orders.
Ms. Saunders raised the funds for the hospice and contributed some of her own money.
She introduced the idea of “total pain” which included the physical, emotional, social, and
spiritual dimensions of distress. She regarded each person, whether patient or staff, as an
individual to the end
1
.
1
British Medical Journal, 2005. https://www.bmj.com/content/suppl/2005/07/18/331.7509.DC1
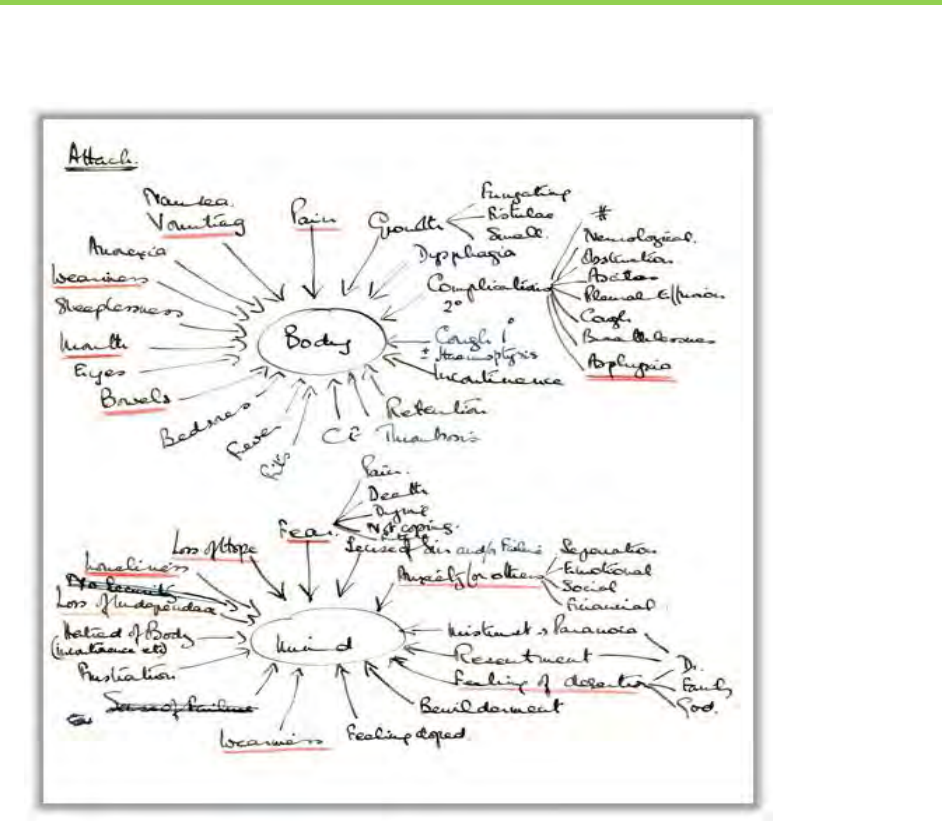
Dame Cicely Saunders’ Archival Notes: Charting within an
Original Coordinated Care Model
In 1967, Dame Cicely Saunders founded St Christopher’s Hospice in
south west London. It is now one of many but is still the leader in
the field. It was her personal achievement and has been imitated
all over the world.
St Christopher’s was the first modern hospice, although there were
a number of homes in existence for the dying, most of which were
run by religious orders.
Ms. Saunders raised the funds for the hospice and contributed
some of her own money. She introduced the idea of "total pain,"
which included the physical, emotional, social, and spiritual
dimensions of distress. She regarded each person, whether patient
or staff, as an individual to the end.
1
1
British Medical Journal 2005, https://www.bmj.com/content/suppl/2005/07/18/331.7509.DC1 NEEDS FOOTNOTE FORMATTING

ii
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
Table of Contents
Executive Summary
Purpose and Context……………………………………………………………………………..1
Defining Hospice Care ............................................................................ 5
The Location of Hospice Care ................................................................. 9
Characteristics by Disease Diagnosis .................................................... 11
Hospice Payment ........................................................................................ 13
Hospice Payment Model....................................................................... 13
Hospice Payment Limits........................................................................ 14
Evidence of the Hospice Value Proposition ............................................... 15
Quantifiable Savings to the Medicare Program ................................... 15
Documented Benefits to Hospice Patients and Families ..................... 21
Hospice: A Service Underutilized ............................................................... 24
Discussion: Policy Considerations for the Future of Hospice.................... 28
i
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
Executive Summary
The Medicare hospice benefit is unique and has numerous attributes; many of which are
not universally understood. Dobson | DaVanzo was commissioned by the National Hospice
and Palliative Care Organization (NHPCO) to develop a policy brief on hospice care that
could serve as a concise single source document highlighting key aspects of past – present
– and future hospice care and its operations. This document is intended to be widely
distributed to stakeholders and policymakers as they consider how to best integrate the
hospice program into a rapidly changing health care system while preserving its essential
and unique character.
Today, value across the health care system in large part involves diverse clinical disciplines
to coordinate care, while reducing overall costs without compromising patient outcomes.
For decades, the hospice program includes terminally ill patients and their families to
collaboratively develop care plans with their hospice interdisciplinary team and take
control of patients’ end of life care.
The hospice value proposition brings care to patients and their families that is unique and
meaningful, as it provides comfort care as well as physical, emotional, and spiritual
support to patients and their families on terms that they themselves choose. Hospice
provides each family services that are tailored to their preferences and the patient’s
clinical condition.
Executive Summary
ii
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
Dimensions of the Hospice Value Proposition
Hospice: The first patient care system in the U.S. to employ comprehensive person and family-centered
care
o Medicare benefit established in 1982 with bipartisan Congressional support
o Care is available to patients and their families seven days a week, 24 hours a day
o Hospice care closely integrates inpatient care and home care to ensure coordination and continuity
o The patients, their families, and anyone essential to the patients’ life create the “unit of care”
o Volunteers are crucial to the success of the hospice care model
o Palliative and supportive care is directed at ameliorating the physical, emotional and spiritual discomfort
associated with terminal illness
o Anticipatory grief counseling is available for the patient and his or her family before death. Bereavement
services are available for the family after the patient has died, including phone calls, follow-up visits and
support.
Hospice Works…
o Because it is a unique and multi-dimensional benefit that integrates person-centered interdisciplinary
approaches resulting in high patient and family satisfaction
o Because the hospice team works closely with the patient and their family to honor the patient’s
preferences and wishes and enables and encourages families to remain closely involved in the care of
the patient and provides support and education for the patient and family concerning death and dying
o Because it allows for the patient’s and families’ choice of setting, most often in whatever setting the
patient calls home
o Because the Medicare payment system “bundles” payment to facilitate program savings
Preserving the Hospice Value Proposition Will Require Policies That:
o Preserve the integrity of the hospice benefit as Medicare Advantage (MA) plans, ACOs and other
organizational delivery forms as they expand in coming years
o Concurrently coordinate the hospice benefit with medical and psychological care under all Medicare
payment models
o Expand timely access to hospice and palliative care based on the individual’s unique care needs
o Ensure high-quality supply of hospice care providers and professionals who are poised to address the
rapidly aging population seeking hospice and palliative care
Source: (1) The Tax Equity and Fiscal Responsibility Act of 1982 Section 122 and (2) The Hospice Experiment. Edited by Mor, V.
PhD, Greer, D. PhD, Kastenbaum, R. PhD. 1988. The Johns Hopkins University Press.

Executive Summary
iii
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
Hospice Works…
Hospice works because it is a unique and multi-dimensional benefit that leverages
person-centered interdisciplinary care resulting in high patient and family satisfaction.
Hospice care combines interdisciplinary approaches with the care provided by the hospice
team and family and friends. The integrated care team works with patients’ families who
are the main source of care for the patient. Patients can choose to receive hospice services
in many settings, often choosing to receive care in their homes rather than in a facility (e.g.
a hospital, nursing home). Hospice providers involve the family throughout the duration of
care, while providing family members respite as needed. The involvement of family and
friends in end of life care has been shown to be of high value to many terminally ill
patients. It supports invaluable time spent together and allows for both the patient and
the family to adjust to the new reality of losing a loved one. Hospice care fulfills the unique
needs of terminally ill patients that curative treatment is generally not able to provide with
physical and emotional support throughout the duration of care.
Hospice works because it allows the patients’ and families’ choice of setting, most often
the home—the hospice team works closely with the patient and their family to honor
the patient’s preferences and wishes and enables and encourages families to remain
closely involved in the care of the patient.
Patients receiving hospice services may do so in a variety of locations based on their
situation, needs, and preferences. While the patient’s home is the most common setting
for hospice care, patients may also receive hospice care at an assisted living facility, a
nursing home, a residential hospice facility, or any other location the patient calls home.
For complex care and symptom management needs that cannot be addressed in the home
setting, short-term inpatient care can also be provided in a hospice inpatient facility,
hospital, or skilled nursing facility. Hospice services can be provided wherever the patient
and family feel most comfortable and individualized care planning allows for changes in
the location of care based on the patient’s needs. Caregiver education, support and
assistance is available to family members who will be working closely with the care team.
Hospice works because the Medicare payment system “bundles” payment in order to
facilitate program savings – hospice savings are well-documented.
Hospice care under the Medicare program aims to prevent pain and suffering for the
terminally ill, through medical, non-medical interventions, and comfort care. To elect hospice
care under Medicare, a patient must agree to forgo curative medical treatment for his or her
terminal illness and related conditions. The Medicare payment model for hospice is comprised
of an all-inclusive per diem payment to the hospice provider, who then manages the entire
interdisciplinary team under the bundled payment. This payment is meant to cover visits by

Executive Summary
iv
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
any hospice professional as well as ancillary services, such as: on-call services, medical
equipment, and medications related to the terminal prognosis.
The four levels of hospice care include:
1) routine home care
2) continuous home care
3) inpatient respite care, and
4) general inpatient care
Each level of care has its own per diem payment rate. The hospice Medicare payment was
designed to ensure patients are provided with the appropriate intensity of care for their
individual needs without receiving unnecessary services.
Several studies have demonstrated that hospice care results in substantive cost savings to the
Medicare program.
2, 3
Patients in hospice care do not receive procedures, treatments, or tests
solely meant to prolong life as related to the terminal illness. These types of services can drive
up the cost of caring for a terminally ill patient. For instance, a study by Powers et al. indicates
that longer durations of hospice care use and higher percentages of hospice users in the
Medicare population equate to greater savings for the Medicare program. As an example, if
80 percent (as opposed to the current 50 percent) of decedent Medicare beneficiaries used
hospice for 24 months, nearly $2 billion could be saved by the Medicare program annually.
4
Currently, providers, payers, and policymakers are placing enormous value on the hospice
care delivery model by recognizing the value of hospice as a bundled payment model as well
as honoring patient and family preferences. Specifically, the Centers for Medicare & Medicaid
Services’ (CMS) Innovation Center (CMMI) is testing the Medicare Care Choice Model
(MCCM) which recognizes the value of hospices being able to offer support to a patient and
families without requiring them to elect the hospice benefit until the patient and family are
ready, through their experience with MCCM or at any time.
Furthermore, in early 2018, CMS released a new interpretation of “primarily health related”
pertaining to Medicare Advantage (MA) Plans to develop supplemental benefits for the
chronically ill. Within the same month, Congress passed the Bipartisan Budget Act of 2018 to
further appreciate the need for supplemental benefits for Medicare Advantage enrollees -
recognizing the value of supplemental services for patients and families.
2
Taylor Jr. et al. What length of hospice use maximizes reduction in medical expenditures near death in the US Medicare
program? June 2007. Social Science & Medicine 65 (2007): 1466-1478.
3
Kerr et al. Cost Savings and Enhanced Hospice Enrollment with a Home-Based Palliative Care Program Implemented as a
Hospice-Private Payer Partnership. J Palliative Med, 2014; 17(12).
4
Powers et al. Cost Savings Associated with Expanded Hospice Use in Medicare. J Palliative Med. 2015 May 1; 18(5):400-
401.

Executive Summary
v
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
Finally, in 2018, the Physician-Focused Payment Model Technical Advisory Committee also
emphasized to Secretary Alex Azar at the Department of Health and Human Services (HHS) a
model to address the seriously ill population is of the “highest possible priority”.
The Innovation Center continues to emphasize the value of hospice by announcing that the
CY 2021 Medicare Advantage Value Based Insurance Design (VBID) model would include the
hospice benefit and actively seeks stakeholder engagement and expertise.

1
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
Purpose and Context
The Hospice Value Proposition
Hospice is widely recognized as being the first healthcare program to integrate palliative and supportive
care for terminally ill patients at the end of their lives. For more than 50 years, hospice care has allowed
these patients to die with dignity, compassion, and respect. Since the first U.S. hospice began operations
in 1974, more than 4,500 hospices have joined the Medicare program. Medicaid and most private payers
also support hospice services.
5
The hospice benefit is unique in that the patient and family comprise the “unit of care.” Throughout a
patient’s time in hospice care, the family receives support through
direct caregiving, social work services, spiritual support,
bereavement counseling, and ongoing communication with the
interdisciplinary care team. The patient receives an array of
services based on the development of a care plan by the hospice,
in collaboration with the patient and family, which can include
physician and nursing services to ensure that medical needs are
met and that he or she is comfortable, aide services to assist with
personal care, physical therapy, occupational therapy or speech language pathology, massage, music and
art therapy, and counseling and support to fashion his or her own personal end of life experience. The
inter-disciplinary care team is charged with addressing the patient’s physical, mental, and spiritual
wellbeing; fear, anxiety, bewilderment, and loneliness are addressed as shown in Figure 1, which is Dame
Saunders’ original schematic representation of hospice care.
5
National Hospice and Palliative Care Organization. Facts and Figures: Hospice Care in America. 2017 Edition (Revised
April 2018). https://www.nhpco.org/sites/default/files/public/Statistics_Research/2017_Facts_Figures.pdf
Care coordination is the deliberate
organization of patient care activities
between two or more participants
(including the patient) involved in a
patient's care to facilitate the
appropriate delivery of health
care services.
—Agency for Healthcare Research and Quality
(AHRQ)
Purpose and Context
2
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
Figure 1: Dame Saunders’ Original Concept of Hospice Care
Physicians and nurses, physical, and occupational therapists, speech language pathologists,
hospice aides, grief counselors, social workers, chaplains, volunteers, and any other discipline
identified as a part of the patient’s care plan are made available to patients and their families. The
hospice interdisciplinary team works to address all components of the patient and family’s care, to
provide training and support to the family caregivers, and to describe what will happen during
their time in hospice care prior to death. Care is also provided after the patient’s death with
bereavement support for family members through follow up phone calls, individual and group
counseling through the first anniversary of the patient’s death.
Purpose and Context
3
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
For the past four decades, long before the current health care system’s transition to coordinated
care and value-based payment,
6
hospice has been coordinating care among different clinical
disciplines, providers and caregivers to deliver an integrated program of supportive and palliative
care to the dying. Hospice is the only care modality in which
the focus is to care for both the patient and the family. In
fact, hospice care is often referred to as one of the nation’s
first “coordinated care” programs.
7
Care is person-centered,
with patients’ wishes being respected.
Its proponents point out that in addition to its widely
recognized clinical benefits, hospice care’s potential for cost
savings stems from two factors: 1) the U.S. hospice model
emphasizes end-of-life care at home and treatments
provided in the home setting are generally less costly than
those provided in the inpatient setting; and 2) hospice care
focuses on proactive symptom management that is less
medically aggressive than conventional curative treatments.
Hospice care involves less rigorous use of expensive and
often debilitating and painful ancillary services which all add to quality of life.
8
Qualitative and quantitative research, as well as numerous patient experiences, demonstrate
the benefits of the hospice program to enrollees and their family members, as well as its cost-
effectiveness to Medicare, its primary payer.
In 1979, the Robert Wood Johnson Foundation and the John A. Hartford Foundation,
together with the Health Care Financing Administration (HCFA)
9
– now the Centers for
Medicare & Medicaid Services (CMS) funded a demonstration project, the National
Hospice Study, to “compare patients served in hospital-based and home-based hospices
with terminal cancer patients receiving care from a variety of conventional (nonhospice)
oncological-care settings.”
10
The intent of the demonstration was to determine which care
models best incorporate the hospice concept.
The National Hospice Study (NHS) aimed to determine the cost-effectiveness of providing
hospice care to terminally ill Medicare and Medicaid beneficiaries. Brown University was
selected to evaluate the program under the direction of Vincent Mor, Ph.D. The evaluation
6
As exemplified by the launch of Accountable Care Organizations in 2011, the implementation of the Bundled Payments for Care
Improvement (BPCI) initiative in 2013, as well as the passage of the Affordable Care Act (ACA) in 2014.
7
Banach, Edo. Coordinated Care Is More Than a Buzzword for Hospice Providers. National Hospice and Palliative Care
Organization (NHPCO). April 24, 2018. https://www.nhpco.org/press-room/press-releases/op-ed-coordinated-care
8
Mor, V., Greer, DS., and Kastenbaum, R. The Hospice Experiment. 1988. The Johns Hopkins University Press.
9
HCFA was the name for CMS beginning in 1977.
10
Mor, V., Greer, DS., and Kastenbaum, R. The Hospice Experiment. 1988. The Johns Hopkins University Press
“Sometimes we can offer a cure, sometimes
only a salve, sometimes not even that. But
whatever we can offer, our interventions, and
the risks and sacrifices they entail, are justified
only if they serve the larger aims of a person’s
life. When we forget that, the suffering we
inflict can be barbaric. When we remember it
the good we do can be breathtaking.”
― Atul Gawande, Being Mortal: Medicine and
What Matters in the End

Purpose and Context
4
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
found that hospice (both home-based programs and hospital-based programs) was less costly
than conventional care over the last year of life. “Despite the high costs associated with the
entry of patients into hospice relatively early in the course of the terminal phase of their
disease, the size of the cost differences in the last month or two before death more than make
up for the extra costs of extended stay in hospice.”
11
Demonstration findings also showed
declining intensity in ancillary services and number of inpatient days provided to hospice
patients as compared to non-hospice patients.
12
As the National Hospice Study was being completed, advocates for the inclusion of hospice in
the Medicare program began working tirelessly with members of Congress and mobilized a large
grass roots force. Legislation to create a Medicare Hospice Benefit had been introduced in
December of 1981 in the House (H.R. 5180, sponsored by Reps. Leon Panetta, D-CA, and Bill
Gradison, R-OH) and in the Senate (S. 1958, by Sen. Bob Dole, D-KS). Their bill enjoyed
favorable hearings in the House Ways and Means Health Subcommittee in March of 1982, but
budget issues blocked its way forward. Looking for a legislative vehicle, bill sponsors and
advocates determined that the budget bill being debated in the Senate was an option. On July
22, 1982, during a debate in the U.S. Senate chambers over technical provisions of the Tax Equity
and Fiscal Responsibility Act, Senator John Heinz (D-PA) walked around the Senate chamber
getting signature supporting an amendment to establish hospice under Medicare. He needed,
and got, the needed 68 signatures to overcome an anticipated objection to the amendment.
The amendment passed and a hospice benefit under Medicare was created.
13
HCFA
subsequently issued regulations issued by HCFA (now CMS) in December 1983.
The Medicare Care Choices Model (MCCM) is designed to learn whether the value hospice brings
to the patient and family, during a time when the patient is eligible to elect hospice, as
determined by the attending physician and hospice medical director, sheds light on the rate of
patients choosing hospice or not. The MCCM provides a new option for Medicare beneficiaries
to receive palliative care services from certain hospice providers without waiving their right for
coverage from all parts of the Medicare program. CMS will evaluate whether concurrent care
prior to the selection of the Medicare hospice benefit can improve the quality of life and care
received by Medicare beneficiaries and increase patient satisfaction.
14
Participating hospices
were randomly assigned to one of two cohorts. The first hospice cohort began providing services
to beneficiaries on January 1, 2016, and the second cohort began providing services on January
11
Mor V, Kidder D. (1985) Cost savings in hospice: Final results of the National Hospice Study. Health Services Research, Vol
20, No.4: 407-422.
12
Mor V, Greer, DS., and Kastenbaum, R. The Hospice Experiment. The Johns Hopkins University Press Baltimore and London.
1988.
13
TEFRA 1982, § 122, Pub. L. 97-248
14
https://innovation.cms.gov/initiatives/medicare-care-choices/

Purpose and Context
5
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
1, 2018. CMS originally planned to select at least 30 Medicare-certified hospices to participate in
the Model. However, due to robust interest, CMS invited over 140 Medicare-certified hospices
to participate in the Model and increased the duration of the Model to 5 years.
Background: The History of Hospice
The first hospice – St. Christopher’s Hospice – was founded by
Dame Cicely Saunders in 1967 in London, England.
15
Recognized
as the founder of the hospice movement, Dame Cicely was
trained as a physician, nurse, and social worker, with a vision to
transform end-of-life care where pain and symptom control
would be linked with compassionate care, teaching, and clinical
research. Having volunteered at a hospital early in life and
witnessing the aftercare of patients with terminal illness, Dame
Cicely internalized what she saw and came to believe that
people should die with dignity, compassion, and respect.
Furthermore, she also introduced the idea that not being able to curie a patient was not a sign
of failure.
16
For these reasons, she pioneered research on the use of morphine for pain and
symptom control, and the efficacy of home care teams appropriate for end-of-life care. She also
developed bereavement service programs at St. Christopher’s Hospice to help families beyond
the death of the patient.
17
Dame Saunders’ original insights continue to be the founding
principles of hospice care today.
Defining Hospice Care
Hospice is grounded in the philosophical approach of providing person-centered care of body
and mind to terminally ill patients and their families. Eligibility for hospice includes eligibility for
Medicare Part A and a prognosis of six months or less if the disease runs its normal course. A
patient elects the hospice benefit based on an informed decision to waive the right to other
Medicare benefits. Hospice does not attempt to prolong life, but instead strives to improve the
quality of life for the time the patient has left.
Hospice care is delivered by an interdisciplinary care team which includes a physician, nurse,
social worker, and counselor as core disciplines. Other disciplines may also be involved in
providing care to the patient and family, including hospice aides, chaplains, therapists –
15
Dame Cicely Saunders. St. Christopher’s. http://www.stchristophers.org.uk/about/damecicelysaunders
16
Dame Cicely Saunders. The BMJ. https://www.bmj.com/content/suppl/2005/07/18/331.7509.DC1
17
Dame Cicely Saunders. StChristopher’s. http://www.stchristophers.org.uk/about/damecicelysaunders
“You matter because you are you, and
you matter to the end of your life. We
will do all we can not only to help you
die peacefully, but also to live until
you die.”
– Dame Cicely Saunders, nurse,
physician, social worker, writer, and
founder of hospice movement (1918 –
2005).
Purpose and Context
6
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
including physical therapists, occupational therapists, speech-language pathologists, art, music
and massage therapists. The services are developed as a part of the hospice’s plan of care,
together with the individual patient and their family and are adjusted as the patient’s illness
progresses.
Community-based palliative care provides pain and symptom management as well as
psychological and emotional support for those patients with advanced illness. If the palliative
care team believes that curative or aggressive treatment is no longer meeting the patient’s
goals of care, the physician or non-physician practitioner leading the care team may
recommend a transition to hospice care
18
. Although the curative treatments for the terminal
illness provided under palliative care cease when a patient enters hospice, some care that was
considered curative may be adapted or adjusted to be palliative in nature. The hospice will
help the patient and family adjust to the “new” modalities and realities of care and to make the
transition to hospice seamless. Pain and symptom management and other comfort care
services continue until the patient dies.
As of 2017, nearly 4,500 hospices were participating in the Medicare program in all 50 states.
The Medicare Payment Advisory Commission (MedPAC) reported hospice services in 2017
totaled $17.9 billion in Medicare expenditures.
19
In 2017, 1.5 million Medicare beneficiaries
received hospice services and 16.7 percent of those beneficiaries were discharged alive. The
patient may leave hospice care at any time by “revoking” their hospice benefits and returning
to regular fee-for-service Medicare. The hospice may discharge the patient alive for prolonged
prognosis, moving out of the hospice’s service area or for cause.
20
The Social Security Act contains a detailed definition of hospice care at Section 1861(dd).
“Hospice care” refers to when any of the following services or items are provided to a
terminally ill individual by a hospice program.
21
18
National Institute on Aging. What are Palliative Care and Hospice Care? 2017. https://www.nia.nih.gov/health/what-
are-palliative-care-and-hospice-care
19
Assessing Payment Adequacy and Updating Payments: Hospice Services. MedPAC presentation to MedPAC
commissioners dated December 7, 2018.
20
Medicare Program; FY 2019 Hospice Wage Index and Payment Rate Update and Hospice Quality Reporting
Requirements. The Federal Register May 8, 2018.
21
Compilation of The Social Security Laws. Part E – Miscellaneous Provisions. Social Security Administration.
https://www.ssa.gov/OP_Home/ssact/title18/1861.htm

Purpose and Context
7
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
Hospice Services:
o Nursing care provided by or under the supervision of a registered professional
nurse,
o Physical or occupational therapy, or speech-language pathology services,
o Medical social services under the direction of a physician,
o Services of a trained hospice aide approved by the Secretary and homemaker
services,
o Medical supplies (including drugs and biologicals) and the use of medical appliances,
while under such a plan,
o Physicians’ services,
o Short-term inpatient care (including both respite care and procedures necessary for
pain control and acute and chronic symptom management) in an inpatient facility
meeting such conditions as the Secretary determines to be appropriate to provide
such care, but such respite care may be provided only on an intermittent,
nonroutine, and occasional basis and may not be provided consecutively over longer
than five days,
o Counseling (including dietary counseling) with respect to care of the terminally ill
individual and adjustment to his death, and
o Any other item or service which is specified in the plan and for which payment may
otherwise be made under this title.
Source: The Social Security Act Section 1861(dd)(1)
Purpose and Context
8
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
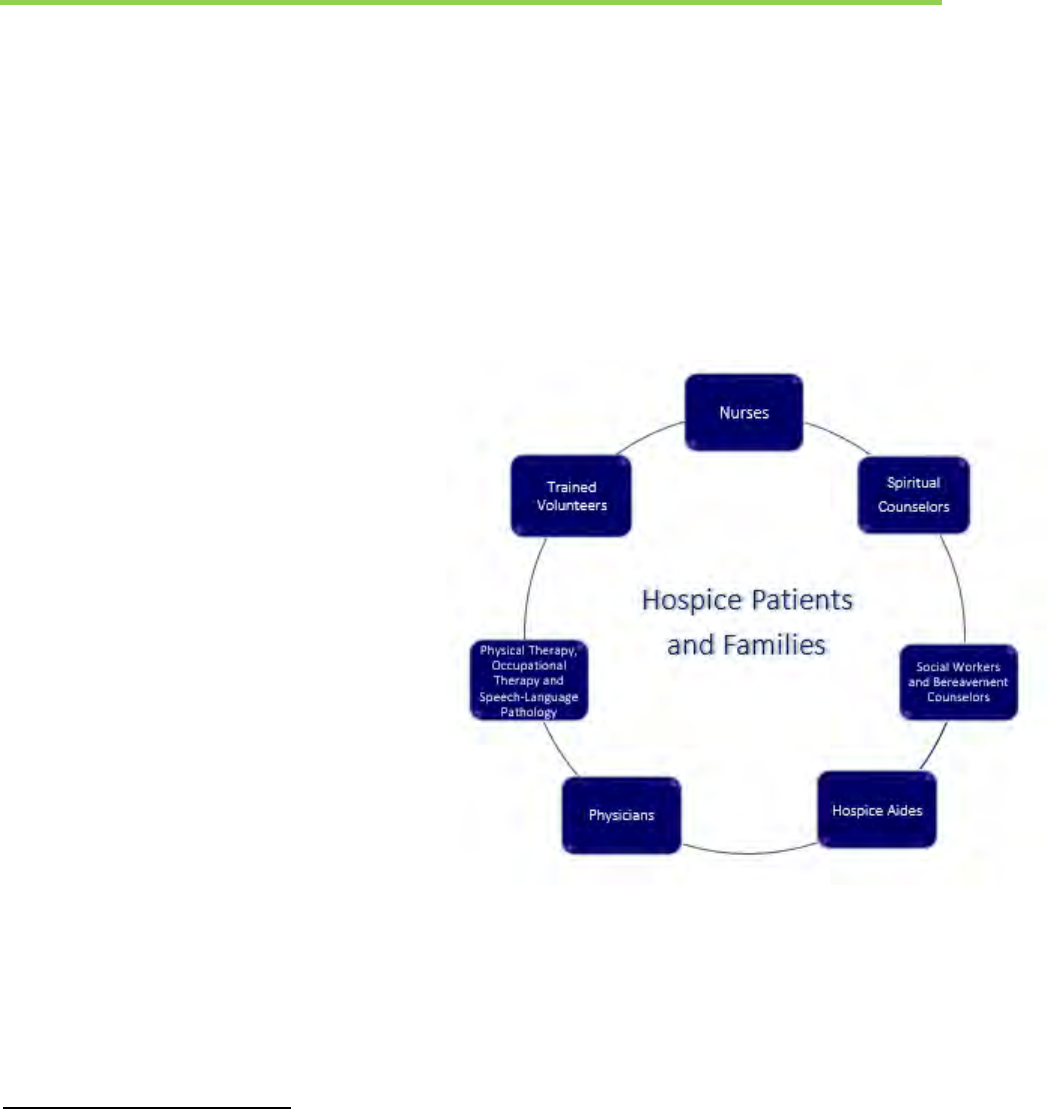
Hospice Care is Characterized by its Patient and Family-Centered, Holistic Approach
Findings from research studies with terminally ill patients indicate seven core domains of end-of-
life needs. These are (1) time, (2) social, (3) physiological, (4) death and dying, (5) safety, (6)
spirituality, (7) change & adaptation. The prevalence, rather than just the occurrence, of patients’
reported needs provides further insight into their relative importance.
22
Effective communication is
therefore a primary ingredient for understanding and assessing patients’ needs as a means of
providing optimal hospice care.
Hospice care focuses on promoting comfort
rather than prolonging life for patients with
terminal illnesses, which are illnesses with little
or no chance of recovery and that will most
likely result in death in the near future.
23,
24
Hospice care employs a patient and family-
centered, holistic approach, with the goal of
providing the best possible quality of care at the
end of life.
This goal is achieved through an interdisciplinary
care team (see Exhibit 1 containing the
interdisciplinary care team model)– consisting of
physicians specializing in hospice and palliative
medicine, nurses with education in caring for
dying patients, social workers, therapists,
chaplains and other spiritual leaders, hospice
aides and specially trained volunteers. The
integrated team provides pain and symptom
management to the patient and supports the family members both before and after the
patient’s death.
Not only will the patient benefit from family involvement during their time in hospice care
where family caregivers may provide support, comfort, and help with the patient’s daily
activities, but family members can be supported during the grief and bereavement process.
22
von Gunten C, Ferris F, Emanuel L: Ensuring Competency in End-of-Life Care. JAMA 2000, 284:3051-3057.
23
Torpy et al. Hospice Care. JAMA. 2012; 308 (2): 200. Doi:10.1001/jama.2012.621.
https://jamanetwork.com/journals/jama/fullarticle/1216479
24
Pace et al. Hospice Care. JAMA. 2006; 295(6): 712. Doi:10.1001/jama.295.6.712.
https://jamanetwork.com/journals/jama/fullarticle/202341
Exhibit 1: Hospice Interdisciplinary Care Team Model

Purpose and Context
9
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
Although hospice care does not aim for cure of the terminal illness, it may treat potentially
curable conditions such as pneumonia. Finally, while most hospice patients are older, this
type of care can be helpful for persons of any age suffering from any terminal illness.
The Location of Hospice Care
The most common setting for hospice care is the patient’s own home or wherever the
patient calls home, where more than 98 percent of days of care are currently provided.
25
This can include an assisted living facility, nursing home, residential hospice facility, or any
other living arrangement. For hospice patients whose care needs are complex, or whose
symptoms cannot be managed in any other setting, short term inpatient care can be
provided in a hospice inpatient facility, hospital, or skilled nursing facility. For patients
receiving hospice services at home, family caregivers (and friends) are trained to provide
basic care. They can administer medication, help the patient transfer from bed to chair,
and help the patient eat, drink, and bathe. When hospice staff are present in the home,
they assess physical and psychosocial symptoms, provide personal care services, provide
spiritual support, provide guidance to family members, and discuss concerns with patients
and their families.
26
25
Medicare Program; FY 2019 Hospice Wage Index and Payment Rate Update and Hospice Quality Reporting
Requirements. The Federal Register May 8, 2018.
26
Where can patients receive hospice care? American Hospice Foundation. 2014. https://americanhospice.org/learning-
about-hospice/what-are-the-different-loactions-where-patients-can-receive-hospice-care/

© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
Hospice use among Medicare beneficiaries has grown rapidly since its inception. This trend
varies by beneficiary characteristics, such as enrollment in traditional Medicare fee-for-service
(FFS) or Medicare Advantage (MA); Medicare-only beneficiaries or beneficiaries dually eligible
for Medicare and Medicaid; urban or rural residence; and age, gender, and race.
27
Characteristics by Medicare Eligibility Category, Age Group, and Urban vs Rural by Decedent
Table 1 shows the characteristics of Medicare beneficiaries using the hospice benefit. Hospice
use is generally higher among decedents in MA than in FFS (51.9 percent vs 48.7 percent,
respectively). Hospice use by decedent also varies for Medicare only and dually eligible
Medicare and Medicaid decedents (51.4 percent and 44.1 percent, respectively). Not
surprisingly, the rate of hospice use increases with age, with the highest prevalence among
decedents age 85 and older (59.1 percent).
27
Medicare Payment Advisory Commission (MedPAC). Report to the Congress: Medicare Payment Policy. Chapter 12:
Assessing payment adequacy and updating payments. March 2018.
Medicare Hospice
Patient Population
Characteristics
Medicare Hospice Patient Population
Characteristics
11
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
This finding is in contrast to the 30 percent of Medicare decedents under age 65. In addition,
hospice use is higher for urban than rural Medicare decedents ranging from 50.7 percent in
urban areas to 33.8 percent in frontier areas (Table 1).
28
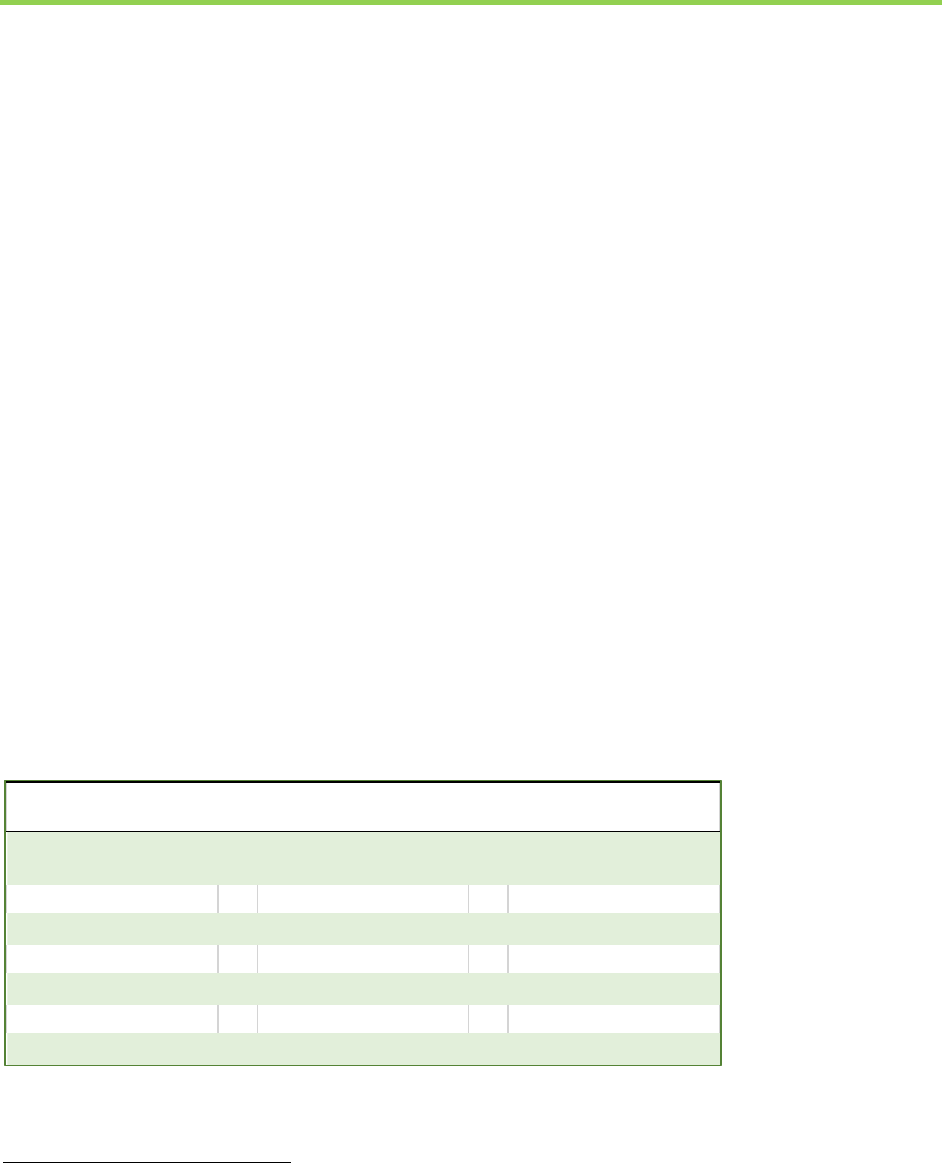
Table 1: Percent Hospice Use by Characteristics of Medicare Decedents (2016)
Decedent
Characteristics
2016 (%)
Decedent Age
2016 (%)
Decedent Location
2016 (%)
MA beneficiaries
51.9%
<65
30.1%
Urban
50.7%
FFS beneficiaries
48.7%
65-74
41.4%
Micropolitan
46.3%
Medicare only
51.4%
75-84
50.7%
Rural, adjacent
45.7%
Dual eligibles
44.1%
85+
59.1%
Rural, non-adjacent
40.2%
Frontier
33.8%
Source: Medicare Payment Advisory Commission (MedPAC) Report to the Congress: Medicare Payment Policy. Chapter 12: Assessing payment adequacy
and updating payments. March 2018
Characteristics by Disease Diagnosis
Differences in Medicare beneficiary use of hospice care are also evident by principal diagnosis.
Figure 2 shows the top hospice diagnoses among Medicare beneficiaries in 2016. As noted in
Figure 2, Medicare beneficiaries with any diagnosis are eligible for and receive hospice care. In
2016, twenty seven percent of Medicare beneficiaries entered hospice with a primary diagnosis
of cancer, higher than any other disease category.
29
As patients with other terminal diagnoses
experience the value of hospice, the relative proportion of hospice cancer patients has decreased
over time.
30
28
Medicare Payment Advisory Commission (MedPAC) Report to the Congress: Medicare Payment Policy. Chapter 12:
Assessing payment adequacy and updating payments. March 2018.
29
A Data Book: Health Care Spending and the Medicare Program. MedPAC, June 2018.
30
Aldridge, M.D., Canavan, M., Cherlin, E., Bradley, E. Has Hospice Use Changed? 2000-2010 Utilization Patterns. Med Care.
(January 2015). 53(1): 95–101. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4262565/pdf/nihms-630205.pdf

Medicare Hospice Patient Population
Characteristics
12
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
Figure 2: Hospice User Principal Diagnoses, 2016
Source: A Data Book: Health Care Spending and the Medicare Program. MedPAC, June 2018.
Cancer
27%
Cardiac and Circulatory
18%
Nervous System
Disorders Including
Dementia
23%
Respiritory
6%
Heart Failure
10%
Other
6%
Chronic Airway
Obstruction
5%
Digestive
2%
Genitourinary
3%
Principal Hospice Diagnoses, 2016
Cancer Cardiac and Circulatory
Nervous System Disorders Including Dementia Respiritory
Heart Failure Other
Chronic Airway Obstruction Digestive
Genitourinary

© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
Hospice Payment Model
The Medicare program pays an all-inclusive per diem payment to hospice providers. In
addition to covering the cost of hospice staff visits, this payment is also intended to cover
the costs of ancillary services a hospice incurs for management of the terminal illness and
related conditions, such as on-call services, care planning, drugs, medical equipment,
supplies, and patient transportation between sites of care that are specified in the plan of
care
31
.
After holding the hospice payment structure constant from 1983 to 2016, the Medicare FY
2019 payment structure was designed and implemented to better align with the costs of
providing hospice care throughout an episode, where more services are provided at the
beginning and end of an episode and fewer in between (see Figure 3). Medicare
beneficiaries have limited cost sharing for hospice services. For instance, only prescription
drugs and inpatient respite care are potentially subject to a small copay for cost sharing.
Hospices must also report either itemized charges for drugs and some Durable Medical
Equipment or a total charge on the claim form each month for each patient.
As distinguished by the location and intensity of the services provided, there are four
different levels of care, each with its own payment schedule as seen in Figure 3:
32
31
Medicare Program; FY 2019 Hospice Wage Index and Payment Rate Update and Hospice Quality Reporting Requirements.
Final Rule. August 2018.
32
CMS Transmittal CR10631 with FY 2019 Hospice Rates, retrieved on November 26, 2018 at
https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/2018Downloads/R4086CP.pdf
Hospice Payment

Hospice Payment
14
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
Figure 3: The Four Levels of Hospice Care with Medicare FY 2019 national rates
Note: Rates are geographically adjusted.
Routine Home Care
o The most common level of hospice
care—98 percent of all hospice
days
o Payment Schedule:
• Days 1-60 $196 per day
• Days 61+ $154 per day
Continuous Home Care
o Intended for the management of a
short-term crisis in the home that
involves eight or more hours of care
per day, primarily nursing care
o Payment Schedule:
• $41.56 per hour
Inpatient Respite Care
o Care provided in a facility setting
intended to give an informal
caregiver a break
o Payment Schedule:
• $176 per day
General Inpatient Care
o Provided in a hospital or hospice
independent facility on a short-term
basis to manage symptoms that
cannot be managed in another setting
o Payment Schedule:
• $758 per day
Hospice Payment Limits
The original design of the Medicare hospice benefit places limits on spending so that the
overall costs associated with Medicare hospice care are not more than the costs of
conventional care for patients at the end of life. For example, the aggregate cap on Medicare
payments for an individual hospice may not exceed the total number of Medicare
beneficiaries served by the hospice multiplied by the cap amount (about $29,205 for the
2019 cap year). If the annual calculation is more than the cap amount, the hospice must
repay the excess to the Medicare program.
33
33
Medicare Program; FY 2019 Hospice Wage Index and Payment Rate Update and Hospice Quality Reporting Requirements. Final Rule.
August 2018. https://www.federalregister.gov/documents/2018/08/06/2018-16539/medicare-program-fy-2019-hospice-wage-index-and-
payment-rate-update-and-hospice-quality-reporting

© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
In an increasingly value based marketplace, it is important to define “value.” Many researchers
agree that value in any industry should be centered on the customer; in the health care industry,
this means the patient. More specifically, value in health care is often defined as quality relative
to cost.
34, 35
Since health care delivery involves multiple health care professionals and providers,
value in health care is largely about coordinating care and reducing cost across all care providers
without compromising outcomes. Hospice is an early example of how interdisciplinary care and
coordination of services can produce value-based care. In this sense, hospice has demonstrated
its value since its inception in the U.S. Evidence of its value is threefold: 1) savings to the
Medicare program (the primary payer of hospice care in the US), 2) benefits to hospice patients
and bereaved family members, and 3) consumer and family satisfaction.
Quantifiable Savings to the Medicare Program
Considerable evidence supports the benefits of both inpatient and outpatient palliative care
under programs such as the Medicare Hospice Benefit, which is generally available to
individuals aged 65 years and older in the U.S. The following presents a summary of several
research studies showing the positive clinical impacts of hospice. which can translate into
direct savings to the Medicare program. Our literature review indicates that, depending on the
length of stay and characteristics of the patient population, the Medicare hospice benefit can
generate savings anywhere from $2,309 per hospice user
36
to $17,903 per hospice user.
37
34
Wegner, SE. Measuring Value in Health Care. North Carolina Medical Journal. July-August 2016. 77(4):276-278.
http://www.ncmedicaljournal.com/content/77/4/276.full
35
Porter, ME. What Is Value in Health Care? N Engl J Med 2010; 363:2477-2481. DOI:10.1056/NEJMp1011024.
https://www.nejm.org/doi/full/10.1056/nejmp1011024
36
Taylor Jr. et al. What length of hospice use maximizes reduction in medical expenditures near death in the US Medicare
program? June 2007. Social Science & Medicine 65 (2007): 1466-1478.
37
Obermeyer et al. Association Between the Medicare Hospice Benefit and Health Care Utilization and Costs for Patients
with Poor-Prognosis Cancer. JAMA. 2014; 312(18):1888-1896.
Evidence of the Hospice
Value Proposition
Evidence of the Hospice Value Proposition
16
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
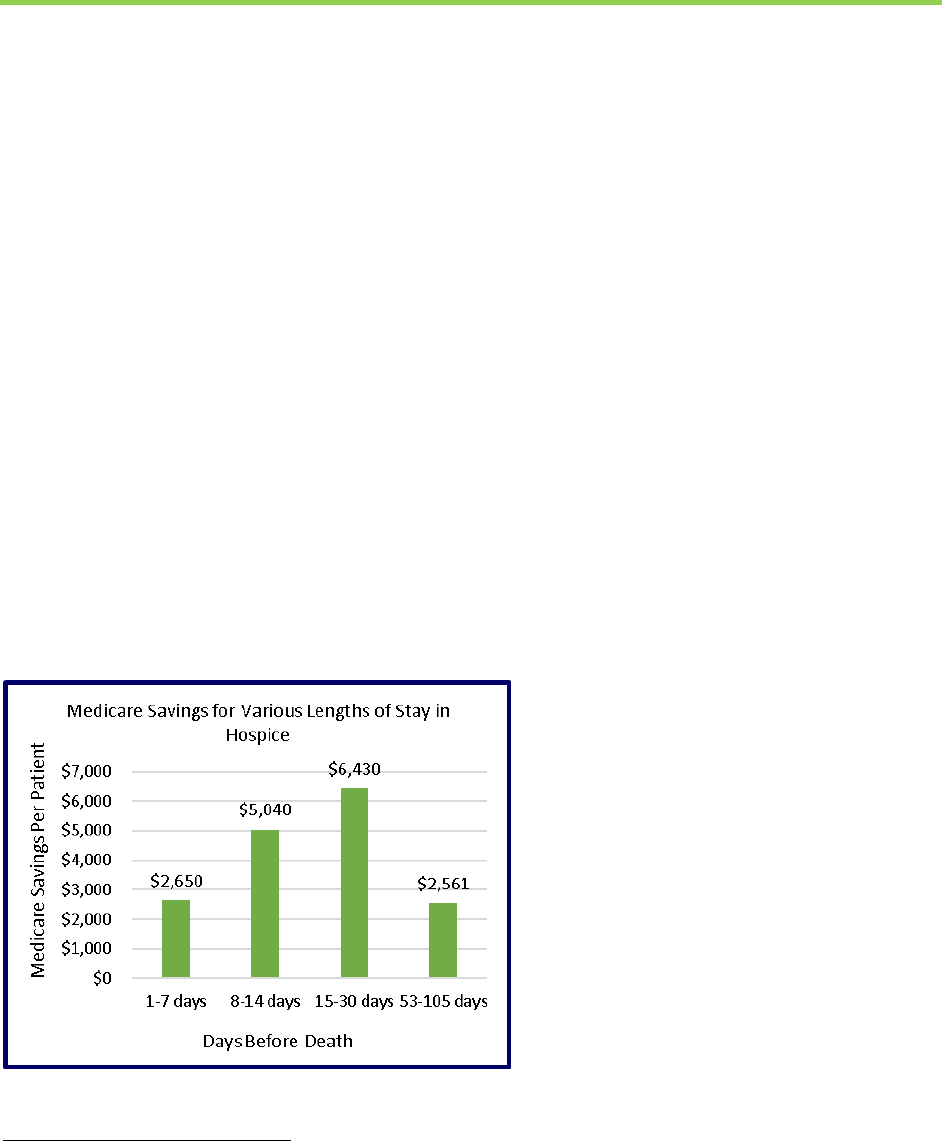
What length of hospice use maximizes reduction in medical expenditures
near death in the US Medicare program?
An early study by Taylor and colleagues had found that that hospice reduced Medicare program
expenditures during the last year of life by an average of $2,309 per hospice user, increasing to
$3,500 per user at a length of stay between 53 and 108 days.
38
More recently, in a study using
Health and Retirement Study data linked to Medicare claims, Kelley and colleagues found
Medicare savings among this group, but also found savings among those enrolled for 1 to 7 days
before death and also 8 to 14 days and 15 to 30 days. Savings were primarily from reductions in
the use of hospital and intensive care services at the end of life.
39
These results support the
earlier results from the Taylor study.
Study Population:
• Hospice Users: n = 1,064
• Non-hospice controls: n = 2,005
Findings: In a sample matched for individual health, functional, and social characteristics,
Medicare costs for patients enrolled in hospice were significantly lower than those of non-
hospice enrollees across all study periods (p<.01). The authors concluded that instead of
attempting to limit Medicare hospice participation, the Centers for Medicare and Medicaid
Services should focus on ensuring the timely enrollment of patients who desire the benefit.
Source: Kelley et al, 2013
38
38
Taylor Jr. et al. What length of hospice use maximizes reduction in medical expenditures near death in the US
Medicare program? June 2007. Social Science & Medicine 65 (2007): 1466-1478.
39
Kelley AS, Deb P, Qingling D, et al. (2013) Hospice enrollment saves money for Medicare and improves care quality
across a number of different lengths of stay. Health Affairs, Vol 32, No 3:552-561.
Evidence of the Hospice Value Proposition
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
Association between the Medicare Hospice Benefit and Health Care Utilization and
Costs for Patients with Poor Prognosis Cancer.
In this sample of Medicare fee-for-service beneficiaries with poor-prognosis cancer, those
receiving hospice care vs not (comparison group) had significantly lower rates of
hospitalization, intensive care unit admission, and invasive procedures along with
significantly lower total costs during the last year of life.
40
Study Population:
• Hospice Users: n = 18,165
• Non-hospice controls: n = 18,165
Findings: In a nationally representative 20 percent sample of fee-for-service Medicare
beneficiaries who died in 2011, the authors used a two-stage matching approach to create
pairs of beneficiaries with poor prognosis cancers (e.g., brain, pancreatic, metastatic
malignancies) who were as similar as possible, but had made different choices concerning
hospice enrollment at the same point in time before death.
The primary outcome was health care utilization in the last year of life, the secondary outcome
was total costs. Non-hospice beneficiaries had more hospitalizations, and higher rates of
intensive care admission and invasive procedures. Overall costs during the last year of life were
$71,517 for non-hospice vs $62,819 for hospice users, a statistically significant difference of
$8,697. Furthermore, a significantly lower percentage of hospice users died in the hospital or
SNF (14 percent vs. 74.1 percent for non-hospice beneficiaries).
Source: Obermeyer, et al (2014).
40
Ober Obermeyer et al. Association Between the Medicare Hospice Benefit and Health Care Utilization and Costs for Patients with Poor-
Prognosis Cancer. JAMA. 2014; 312(18):1888-1896.
Non-hospice, % (95% CI) Hospice, % (95% CI)
Hospital admission 65.1 (64.4-65.8) 42.3 (41.5-43.0)
ICU Admission 35.8 (35.1-36.5) 14.8 (14.3-15.3)
Invasive Procedures 51.0 (50.3-51.7) 26.7 (26.1-27.4)
Death in hospital or SNF 74.1 (73.5-74.8) 14.0 (13.5-14.5)
Long term hospital/SNF 23.9 (23.3-24.5) 10.5 (10.1-11.0)
Total Costs ($) 71,517 (70,543-72,490) 62,819 (62,082-63,557)
Care Utilization in the Last Year of Life

Evidence of the Hospice Value Proposition
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
Cost Savings and Enhanced Hospice Enrollment with a Home-Based Palliative Care
Program Implemented as a Hospice-Private Payer Partnership.
The aim of the study was to evaluate the clinical impact of a home-based palliative care
program, Home Connections, implemented as a partnership between a not-for-profit hospice
and two private insurers. Measured outcomes included 1) advance directive completion, 2) site
of death, 3) symptom severity over time, 4) program satisfaction, 5) hospice referral and 6)
average length of stay.
The Center for Hospice & Palliative Care (Cheektowaga, New York) established Home
Connections (HC), a home-based palliative care program, in 2008. HC serves Erie County,
New York, and is available to adult patients, 18 years or older, with advanced chronic illness.
HC serves patients upstream from the Medicare Hospice Benefit, so patients may still be
receiving aggressive or cure-focused treatments and do not necessarily have an expected
prognosis of six months or less.
Study Population:
• Included in Analyses: n = 499
• Hospice enrolled: n = 147
Findings: A prospective, observational study of a single cohort of commercially insured
patients by Kerr et al. (2014) found that an overall savings of $4,628 ($10,712 - $6,084) was
associated with hospice enrollment per user per month for the last 3 months of life. The
amount of savings was almost doubled to $7,172 ($13,846 - $6,674) when researchers looked
at only the last two weeks of life for these patients.
41
41
Kerr et al. Cost Savings and Enhanced Hospice Enrollment with a Home-Based Palliative Care Program Implemented as
a Hospice-Private Payer Partnership. J Palliative Med, 2014; 17(12).
$6,084
$6,674
$10,712
$13,846
$0
$5,000
$10,000
$15,000
Last 3 months of life Last two weeks of life
Expenditures
Timeframe
Expenditures for the last 3 Months, 2 Weeks of Life; Hospice
vs Non-Hospice
Hospice User Non-Hospice User

Evidence of the Hospice Value Proposition
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
What length of hospice use maximizes reduction in medical expenditures
near death in the US Medicare program?
The Duke cost study, a seminal retrospective case/control study of Medicare beneficiaries by
Taylor Jr. and colleagues
42
found that hospice use reduced Medicare program expenditures
during the last year of life by an average of $2,309 per hospice user:
Study Population:
• Hospice Users: n = 1,819
• Non-hospice controls: n = 3,638
Finding: Savings are most pronounced during the user’s last 72 days of life;
• starting with $10 on the 72
nd
day
• increasing to $750 on the day of death
When differentiating the study population by primary condition for hospice admission and
examining a length of stay between the last 58-103 days of life this average saving increased
to:
• around $3,500 per user for primary conditions other than cancer; and
• a maximum reduction of about $7,000 in Medicare expenditures per user with a
primary diagnosis of cancer.
42
Taylor Jr. et al. What length of hospice use maximizes reduction in medical expenditures near death in the US Medicare
program? June 2007. Social Science & Medicine 65 (2007): 1466-1478.

Evidence of the Hospice Value Proposition
20
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
Cost Savings Associated with Expanded Hospice Use in Medicare.
This study examined hospice savings to Medicare by simulating various uptake percentages of
hospice care by decedent Medicare beneficiaries with terminal cancer and by the duration of
hospice stay. Based on a regression model estimating difference in weekly costs between
matched hospice and nonhospice beneficiaries, as a function of age, sex, HRR, comorbidity,
and time from diagnosis to death. Using coefficients from this model, the authors estimated
costs for all beneficiaries with poor-prognosis cancers at the beneficiary-week level, under
hypothetical scenarios of increased hospice uptake. Specifically, the authors varied the
percentage of beneficiaries enrolled in hospice (assigning a random sample of f = 20 percent,
40 percent, … 100 percent of all beneficiaries to hospice) and length of hospice stay (setting
length to w = 2, 4, 8, … 24 weeks for all those assigned to hospice).
Findings: Estimated annual cost savings ranged from $316 million if 20 percent of the
decedent beneficiaries used hospice care for a duration of 4 weeks to $2.43 billion if 100
percent of the decedent beneficiaries used hospice care for a duration of 24 weeks. The
study was based on the estimate that about 60 percent of decedent Medicare beneficiaries
enter hospice care for an average stay of under two weeks, the hospice program could save
the Medicare program $705 million annually. In addition, since the general consensus is that
the most reasonable length of stay is three months, and at the estimate of 60 percent
hospice uptake, an annual savings of $1.34 billion could be achieved.
Annual Cost Savings by Hospice Uptake and Duration of Hospice Stay ($ MILLIONS)
Hospice
Uptake
Medicare
Decedent
(%)
Duration of Hospice Stay (weeks)
2
4
8
12
16
20
24
20%
$237
$316
$411
$446
$466
$484
$487
40%
$469
$630
$825
$890
$935
$965
$970
60%
$705
$940
$1,235
$1,340
$1,395
$1,445
$1,455
80%
$940
$1,260
$1,645
$1,785
$1,860
$1,925
$1,940
100%
$1,175
$1,570
$2,060
$2,230
$2,330
$2,410
$2,430
Source: Powers et al. Cost Savings Associated with Expanded Hospice Use in Medicare. J Palliative Med. 2015 May 1; 18(5):400-401.
43
43
Powers et al. Cost Savings Associated with Expanded Hospice Use in Medicare. J Palliative Med. 2015 May 1; 18(5):400-401.

Evidence of the Hospice Value Proposition
21
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
The value proposition of the hospice program is demonstrated by the numerous research
studies showing Medicare savings associated with the program.
The weight of the evidence is
that appropriate use of hospice can generate savings in Medicare across all lengths of stay,
and savings are more pronounced for patients with more comorbidities and longer stays in
hospice.
There is growing evidence that hospice provides high-value, high-quality and effective
care, that patients and families choose hospice as a benefit under Medicare because of
the holistic care that is provided to patients and their families, as well as the potential for
cost savings, as demonstrated by studies that span four decades of quantitative and
qualitative research.
Studies as well as real life patient stories have consistently demonstrated the positive impact
hospice conveys to those suffering with advanced and terminal illnesses and their primary
caretakers.
44, 45, 46, 47, 48,
Documented Benefits to Hospice Patients and Families
Hospice provides patients the choice of managing pain and symptoms of terminal illnesses
and being comfortable in the last months of life. Hospice use is not “giving up.” In a study
of 1,970 propensity-score-matched individuals with advanced
cancer and their family members, Kumar and colleagues.
examined the association between receipt of hospice and the
relief of common pain and anxiety symptoms, patient-goal
attainment, and quality of end-of-life care; and found that not
only do families of patients enrolled in hospice more often
report that patients received “just the right amount” of pain
medication, they are also more likely to report that the
patient’s end-of-life wishes were followed, and the patient had
“excellent” quality of care during the end stage of life.
49
The authors also reported that
longer hospice stays were associated with higher patient and family satisfaction and those
44
Kumar et al. Family Perspectives on Hospice Care Experiences of Patients with Cancer. Journal of Clinical Oncology.
February 1, 2017. 35(4): 432-439. DOI:10.1200/JCO.2016.68.9257.
45
Teno JM et al. Timing of referral to hospice and quality of care: length of stay and bereaved family members’
perceptions of the timing of hospice referral. J pain Symptom Manage. 2007 Aug; 34(2): 120-5. Epub 2007 Jun 21.
https://www.ncbi.nlm.nih.gov/pubmed/17583469
46
Gazelle, Gail. Understanding Hospice – An Underutilized Option for Life’s Final Chapter. N Engl J Med 2007; 357(4): 321-
324.
47
Hospice Stories. Pathways. 2018. https://www.pathwayshealth.org/hospice-stories/
48
Supporting Patients with Special Needs. CareDimensions.2018. https://www.caredimensions.org/about-
us/newsroom/patient-stories.cfm?story=18&title=Supporting%20Patients%20with%20Special%20Needs
49
Kumar et al. Family Perspectives on Hospice Care Experiences of Patients with Cancer. Journal of Clinical Oncology.
February 1, 2017. 35(4): 432-439. DOI:10.1200/JCO.2016.68.9257.
“Hospice is the only health care
program that takes care of both
the patients and their family
members.”
~ Vincent Mor, Ph.D., Professor of
Health Services, Policy and Practice.
Brown University.

Evidence of the Hospice Value Proposition
22
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
who receive hospice care are more likely to die in their preferred place.
50
Similarly, in a
collaborative study between the NHPCO and the Brown University Medical School,
researchers found that being referred to hospice “too late” was associated with more
unmet needs, higher reported concerns, and lower satisfaction.
51
Site of death has been suggested as a quality measure for end-of-life care. Population
surveys indicate a majority of respondents (including those with a serious or terminal
illness) report wanting to die at home, in actuality most still die in an institutional setting.
52
Patient Experiences
To put the many statistics presented earlier in this report into perspective, the New England
Journal of Medicine provided case studies of the benefits of hospice from a patient’s view.
53
50
Ibid.
51
Teno JM et al. Timing of referral to hospice and quality of care: length of stay and bereaved family members’
perceptions of the timing of hospice referral. J pain Symptom Manage. 2007 Aug; 34(2): 120-5. Epub 2007 Jun 21.
https://www.ncbi.nlm.nih.gov/pubmed/17583469
52
Teno J M, Gozalo PL, Bynum J p w, et al. Change in end-of-life care for Medicare beneficiaries: Site of death, place of
care, and healthcare transitions in 2000, 2005, and 2009. JAMA. February 6, 2013. Vol 309, No.5: 470-477.
53
Porter, ME. What Is Value in Health Care? N Engl J Med 2010; 363:2477-2481. DOI:10.1056/NEJMp1011024.
https://www.nejm.org/doi/full/10.1056/nejmp1011024
Mr. G
Mr. G is an 83 years old patient admitted to
hospice due to class IV heart failure, end-stage
coronary artery disease, and insulin-dependent
diabetes. Relieved that hospice does not actually
mean imminent death, Mr. G started his hospice
care because he did not want to be re-
hospitalized. Not only did the interdisciplinary
team manage his pain and anxiety, they also
attended to his and his wife’s non-medical needs.
Mr. G was helped to dress and take care of
personal hygiene an hour each day for 5 days a
week and had a social worker who assisted with
grocery shopping and provided companionship.
Because Mr. G thought his illness was a sign of
divine punishment, the social worker brought on a
hospice chaplain to the care team, all the while
attending to family member’s fear about the
future.
Emma
Emma received her breast cancer diagnosis just
days after her honeymoon with husband Jim. Two
years later, when Emma’s disease progressed, she
was referred to her hospice team of nurse, social
worker, and hospice aide. To honor Emma’s
request, the social work taught her breathing and
guided meditation techniques designed specifically
for cancer patients, allowing Emma to be an active
participant in her own care. When her condition
further deteriorated, the hospice team gently
informed Emma’s family members. At the end,
Emma was able to pass away peacefully at her own
home, with her support system – husband, sister,
father, and mother-in-law – by her bedside. Jim
later wrote “the hospice staff was terrific. They
helped ease her pain with their care and
treatment. I really appreciated their assistance in
doing so.”

Evidence of the Hospice Value Proposition
23
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
These personal experiences, regardless of the age of the patient, location of their care or principal
diagnosis for hospice admission, are examples of testimonies to the patient’s perceived value of
this interdisciplinary approach to coordinated care, which includes both the patient and their
family. Hospice fulfills patients’ specific yet diverse needs, often expanded beyond what
traditional curative treatment can do.
Family Members’ Experiences
In addition to the psychosocial benefits to the patient, benefits of hospice are available to dying
patients’ family members, those who are left behind.
54
Studies have consistently demonstrated
the importance of hospice care to bereaved family members. In conducting their prospective,
longitudinal, multisite study of patients with advanced cancer and their caregivers, Wright et al.
found that even after adjusting for caregivers’ baseline mental
health, mourning caregivers whose loved ones died in an
intensive care unit (ICU) and hospital were more likely to
develop psychiatric symptoms than their counterparts whose
loved ones died at home under hospice care.
55
Bereaved
caregivers of non-hospice patients also demonstrated an
increased risk for post-traumatic stress disorder (PTSD),
suggesting that caregivers’ experiences at the ICU and hospital
may be traumatic.
To expand upon this effect, a prospective cohort study of 174 primary family caregivers of
cancer patients who enrolled in hospice examined the association between hospice length
of stay and depressive disorders in caregivers. The findings demonstrate that in
comparison to caregivers whose loved ones stayed in hospice for a longer period of time,
caregivers of patients enrolled in hospice for 3 or fewer days were significantly more likely
to develop major depressive disorder, 24.1 percent compared to 9.0 percent for those with
a longer stay in hospice. The effect remained true after adjusting for confounding factors.
56
54
Naierman N and Johanna Turner. Debunking the Myths of Hospice. American Hospice Foundation.
https://americanhospice.org/learning-about-hospice/debunking-the-myths-of-hospice/
55
Wright et al. Place of Death: Correlation With Quality of Life of Patients With Cancer and Predictors of Bereaved
Caregivers’ Mental Health. J Clin Oncol. 2010 Oct 10; 28(29): 4457-4464.
56
Bradley EH et al. Depression among surviving caregivers: does length of hospice enrollment matter? Am J Psychiatry.
2004 Dec; 161(12): 2257-62.
Studies have demonstrated the
beneficial effects on outcomes when
palliative care/hospice services are
introduced into routine cancer care.
~ May et al. Palliative Care Teams’ Cost-
Saving Effect Is Larger for Cancer Patients
with Higher Numbers of Comorbidities.
Health Affairs 2016, 35(1): 44-53

© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
As noted above, although the majority of the people expressed the desire to die at home,
20 percent of Medicare patients still die in the hospital.
57, 58
In fact, two independent
studies reported that as of 2017, more than forty million Americans with serious health
problems do not have access to hospice and palliative care.
59, 60
Despite the benefits of hospice care being widely reported, why does hospice still remain
an underutilized service? The answer may lie within some of the myths and
misunderstandings surrounding this program. These beliefs can include, but are by no
means limited to, belief that: 1) hospice is a place, 2) hospice means giving up on life, 3)
hospice hastens death, 4) hospice requires family involvement or 5) hospice is only
appropriate for the last few days of life.
61, 62
These widely held beliefs are discussed below.
57
Teno, J.M., Gozalo, P., Trivedi, A.N,, Bunker, J., Ogarek, J., Mor, V. Place of Care in Advanced Cancer: Site of Death, Place
of Care, and Health Care Transitions Among US Medicare Beneficiaries, 2000-2015. Journal of the American Medical
Association. July 17, 2018. https://jamanetwork.com/journals/jama/article-abstract/2686318
58
Percent of Death Occurring in Hospital. The Dartmouth Atlas of Health Care.
http://www.dartmouthatlas.org/data/table.aspx?ind=15
59
Kelley AS. Defining “serious illness.” J Palliat Med. 2014;17(9):985.
60
Schoenman JA. The concentration of health care spending. National Institute for Health Care Management Research
and Educational Foundation. 2012.
61
Temel et al. Early Palliative Care for Patients with Metastatic Non-Small-Cell Lung Cancer. N Engl J Med 2010; 363:733-
742. https://www.nejm.org/doi/full/10.1056/NEJMoa1000678
62
Connor, SR et al. Comparing Hospice and Nonhospice Patient Survival Among Patients Who Die Within a Three-Year
Window. Journal of Pain and Symptom Management 2007; 33(3):238-246.
https://www.nhpco.org/sites/default/files/public/JPSM/march-2007-article.pdf
Hospice: A Service
Underutilized

Hospice: A Service Underutilized
25
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
Common Misconceptions That Lead to Underutilization of Hospice
• Hospice is a place: As discussed above, hospice is not a place, but rather a concept of care that can
take place anywhere the patient wishes. The place of care can range from the patient’s home or
anywhere the patient calls home, to an assisted living facility, to a nursing home, to another group
living situation, to a hospital.
• Hospice is only when there is no hope: Instead of viewing hospice as a hopeless last resort, hospice
care has the capability of showing patients and their caregivers how fulfilling the end of life can be
by focusing on personal, familial, and spiritual connections. In fact, many family members report
looking back and cherishing their hospice experience.
•
• Hospice hastens death: Studies have consistently suggested that patients enrolled in hospice live
longer than those who did not. Connor et al studied 4,493 Medicare beneficiaries with congestive
heart failure or some of the most common types of cancer for hospice admission and found that
patients who received hospice services lived on average 29 days longer than those in the non-
hospice comparison group. A 2010 study by Temel et al. echoed such results and reported that for
patients with metastatic non-small-cell lung cancer, recipients of hospice services lived a median of
11.6 months compared to patients who did not receive hospice care (8.9 months).
• Hospice requires help from family members: Contrary to the belief that hospice requires family
presence, this is not a must. In fact, the hospice program recognizes that a dying patient may live
alone or have family members who are unable to provide care. In those cases, hospices coordinate
community resources to make such care possible.
Hospice is only for the last few days of life: Hospice is presented as an option to patients and their
families when a terminally ill patient is given a prognosis of six months. A patient may choose to enter
or leave hospice at any point during this time. If a patient enters hospice early on, there is greater
opportunity to realize the value of hospice in managing symptoms, providing more opportunities for
family time and making them more comfortable in their final days.

Hospice: A Service Underutilized
26
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
Physician Attitudes Toward Hospice
Physician readiness is often a contributing factor to underutilization of hospice.
Prognostication is challenging, and survival estimates are typically inaccurate.
63
Oncologists
and other physicians can view the death of a patient as a professional failure.
64
As a way to ease patient anxiety and to increase patient and family hope, physicians often
resort to “increasing the quantity rather than quality of life”.
65
These reactions stem from the
fundamental resistance to confronting death by both the physician and the patient, to which
modern medical advancements have heretofore contributed. Physicians may also have the
view that hospice is reserved for patients whose death is imminent, not that hospice is a well-
coordinated program that focuses on helping patients to live as comfortably as possible during
the end stage of life.
Death is arguably the most fearful and difficult phase of life, for both patients and their
families. The hospice program, originated in England and first established in the U.S. in
1974, is a holistic approach designed to alleviate both the physical and emotional pain of
the dying as well as those who are left behind. The benefits of hospice have long provided
value to Medicare and other patients and families as they struggle to reconcile often
conflicting emotions. Its emphasis on being patient-centered and family oriented, and on
providing physical and spiritual comfort during times of stress and uncertainty are well
documented.
As a well-structured and integrated program within the Medicare FFS program, numerous
studies have shown favorable financial and clinical results. Yet, the program continues to
be underutilized. Including the misconceptions already discussed, a patient’s own cultural
beliefs, referral to hospice as an indication of physician and/or family failure, and a patient
or family’s inability to recognize that the end of life is near. However, as baby boomers age,
many will likely live with chronic illnesses and cancer (estimated to increase by 67 percent
between 2010 and 2030),
66
making the appropriate use of hospice care more critical than
ever.
The Medicare Care Choice Model (MCCM): Expanding the Hospice Concept
As with any program of care, changes in the hospice program are inevitable as the value-
based health care marketplace forces providers to continually refine and improve their care
63
Myers J, Selby D. Personalizing prognosis in a patient with serious illness. CMAJ. 2014;186(3):169-70
64
Cancer care during the last phase of life. American Society of Clinical Oncology. J Clin Oncol 1998; 16:1986-96.
65
Gazelle, Gail. Understanding Hospice – An Underutilized Option for Life’s Final Chapter. N Engl J Med 2007; 357(4): 321-
324.
66
Cancer increasing as babyboomers age. University of Pennsylvania School of Nursing. November 27, 2013. ScienceDaily.
https://www.sciencedaily.com/releases/2013/11/131127170055.htm

Hospice: A Service Underutilized
27
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
offerings. CMS has recently taken the initiative to test a health care delivery and payment
model. The model offers a new option for Medicare beneficiaries with advanced life-limiting
illness which would provide traditional hospice services, such as comprehensive medical,
psychosocial, and spiritual palliative care services from selected hospice providers, while
continuing to concurrently receive services provided by other Medicare providers, including
care for their terminal condition. This model is referred to as the Medicare Care Choice
Model (MCCM) and began in 2014. At the time of this writing, approximately 97 hospices are
participating in the Model.
The MCCM aims to evaluate whether eligible Medicare and dually eligible beneficiaries would
elect to receive palliative and supportive care services typically provided by hospice if they
could also continue to receive curative treatment for their terminal condition, and how this
flexibility impacts quality of care and patient, family and caregiver satisfaction. Beneficiaries
must be diagnosed with one of the following terminal illnesses: 1) advanced cancer, 2) chronic
obstructive pulmonary disease, 3) congestive heart failure, or 4) human immunodeficiency
virus/acquired immunodeficiency syndrome (HIV/AIDS).
67
The model exposes a larger group of
providers and beneficiaries to the benefits of availing themselves of the integrated, patient and
family-centered program of hospice.
The MCCM is designed to: 1) increase access to supportive care services provided by hospice, 2)
improve quality of life and patient/family satisfaction, and 3) inform new payment systems for
the Medicare and Medicaid programs.
Due to widespread interest, CMS expanded the model from an originally anticipated 30
Medicare-certified hospices to more than 140 Medicare-certified hospices and extended the
duration of the MCCM from three to five years. Participating hospice programs were
randomly assigned to one of two cohorts.
The first cohort began providing services to beneficiaries on January 1, 2016, and the second
cohort began providing services on January 1, 2018. Based on feedback from MCCM
participants and industry stakeholders, some MCCM eligibility criteria have been changed
since model initiation with the goal of facilitating wider beneficiary participation. Although
initial enrollment in the demonstration was lower than expected, evaluation studies have
been positive.
68
Importantly, more than four out of five MCCM enrollees (83 percent)
elected the Medicare hospice benefit after an average of two months in MCCM and one
month prior to death.
67
https://innovation.cms.gov/initiatives/medicare-care-choices/
68
Centers for Medicare and Medicaid Services. Medicare Care Choices Model First and Second Years Evaluation Report.
https://www.cms.gov/newsroom/fact-sheets/medicare-care-choices-model-mccm-first-two-years

© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
How Could the Medicare Hospice Benefit be Restructured in the Future?
Considerable evidence suggests that the last phase of life often involves some days, weeks, and
months prior to death, which are accompanied by significant emotional distress and financial
expense. For patients and their families, there are few care decisions that are more intense yet
uncertain than those made near the end of life. The availability of end-of-life care that seeks to
provide a unique holistic and person-centered approach is of paramount importance. Expanding
the utilization of hospice requires overcoming the challenging misconceptions noted in the
previous chapters as these misconceptions stem from a lack of accurate information.
Several factors make this policy brief particularly timely and relevant, not the least of
which is the rapidly increasing number of older Americans with some combination of
frailty, physical and cognitive disabilities, chronic illness, and functional limitations.
Evidence continues to mount that goals of care discussions lead to better outcomes,
particularly improved quality of life near the end of life and reduced costs. Life threatening
illness, whether it can be cured or controlled, carries significant burden of suffering for
patients and their families and that this suffering is and can be effectively addressed by the
Discussion: Policy
Considerations for the
Future of Hospice

Discussion: Policy Considerations for the Future
29
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
Medicare Hospice Benefit. Hospice can help ensure that the patient's final time is spent in
comfort and that the family's needs are attended to both before and after the patient dies.
In this section of the paper, we discuss several ideas that are currently being put forward by
both providers and policymakers concerning updating or restructuring the Medicare Hospice
Benefit to better align with the systematic movement toward value-based care across the
continuum.
Additionally, the hospice patient mix is changing, necessitating a re-examination of the
various features of the hospice benefit, such as the 6- month prognosis eligibility
requirement.
69
Since data show that increasingly more patients enter hospice due to
nervous system disorders and dementia- related conditions, instead of cancer, it could be
beneficial to remove this regulation thus allowing hospices to provide longer care to those
patients who are in need.
70
While these conditions are generally terminal, their duration
can be longer than six months and this more extended duration of terminal illness should
not mean that these patients do not qualify for hospice.
A couple of model initiatives have recently been introduced by CMS (e.g., the Medicare
Care Choices Model (MCCM) and the Medicare Advantage Value Based Insurance Design
(VBID) Model). Ideas being tested include the provision of concurrent care, extending the
prognosis requirement to 12 or 18 months, and better integrating community-based
palliative care with hospice care to more broadly create a full continuum of advanced
illness care. Under VBID, Medicare Advantage organizations are able to propose reduced
cost-sharing and/or additional supplemental benefits, including non-primarily health
related supplemental benefits, for targeted enrollees.
A full continuum of care would mean that patients and their families can access needed
services as they are able to grasp the finality of an advanced or terminal illness. The MCCM
allows for the patient to receive services without a requirement to elect the Medicare
hospice benefit and waive other parts of Medicare. Some patients and families cannot fully
accept the idea of forgoing curative care when they first receive a terminal diagnosis. Over
time, as they are able to accept the situation, families are better able to recognize that
interventions solely to preserve life may not be in the best interests of their family member.
69
National Hospice and Palliative Care Organization. Facts and Figures: Hospice Care in America. 2017 Edition.
https://www.nhpco.org/sites/default/files/public/Statistics_Research/2017_Facts_Figures.pdf
70
Medicare Program; FY 2019 Hospice Wage Index and Payment Rate Update and Hospice Quality Reporting Requirements. Federal
Register, May 8, 2018.

Discussion: Policy Considerations for the Future
30
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
In 2021, the Medicare Advantage VBID model will add hospice benefits to those MA plans
who apply. This will allow CMS to test the inclusion of hospice in MA through a model, with
opportunities for learning and adjusting the model parameters.
How can policy support better coordination of the hospice benefit with Medicare
fee-for-service or Medicare Advantage?
Hospice care provides services for a terminal illness and the related conditions. Some
Medicare beneficiaries utilizing hospice may experience a condition that is unrelated to the
reason for their hospice stay. In these cases, beneficiaries may receive traditional Medicare or
private insurance services and the hospice will typically coordinate and collaborate with other
providers to ensure a seamless care continuum.
In some cases, providing primary care providers education on advance care planning and
goals of care discussions could also improve timely access to hospice care for terminally ill
individuals and foster better coordination of hospice with other types of care. Policies that
support physicians’ best judgment provide a safe harbor for those providers making difficult
decisions concerning a terminal patient’s prognosis and determining hospice eligibility.
CMS has begun developing a comprehensive assessment instrument for hospice care to
align with other Post-Acute Care (PAC) settings, where feasible and practical.
71
The Hospice
Evaluation and Assessment Reporting Tool (HEART) is an instrument that must include the
ability to establish goals of care consistent with goals and preferences, and values the
person and caregiver in the care continuum with an emphasis on physical, psychosocial,
spiritual, and emotional support. CMS is working diligently to develop the instrument after
pilot testing provided feedback for developers.
71
CMS Hospice Quality Reporting Program at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-
Instruments/Hospice-Quality-Reporting/HEART.html, accessed March 1, 2019

Discussion: Policy Considerations for the Future
31
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
What policies can enable hospice to be more widely utilized?
Another barrier that needs to be addressed is the limited number of hospice care
specialists. Only recently (in 2008) did the American Board of Medical Specialties begin to
certify physicians in the practice of hospice and palliative medicine.
Training in hospice and palliative medicine involves
“skilled communication with patients and families in the
context of serious illness, safe and effective symptom
management, and psychosocial assessment and support”,
which many U.S. physicians lack. Yet, financial support for
such training depends predominantly on philanthropy
rather than Medicare-funded graduate medical education
(GME) dollars. This shortage in training and funding also
exists in other fundamental disciplines of a hospice team:
nursing, social work, and chaplaincy. Increased training
and organized financial support can extend the benefits of
hospice care to those who have little knowledge or who
are unaware of it.
72
A bill currently under consideration in
the Congress will help address the shortage in training and funding.
HR 647, The Palliative Care and Hospice Education and Training Act
(PCHETA) addresses a shortage in the healthcare workforce focusing
on hospice and palliative care by establishing Palliative Care and
Hospice Education Centers, Expanding Palliative care Research,
Providing Academic and Career incentive awards and establishing a
national awareness campaign.
As the U.S. population ages and the number of Medicare eligible
individuals grows, professionals trained in palliative care will
continue to be in high demand. Age-related diseases such as
Alzheimer’s disease are catching up to terminal cancer diagnoses as
being top primary diagnoses for patients entering hospice care. The
future of hospice depends on the specialized skills and expertise of
professionals equipped to serve these patients and their families.
72
Meier et al. A National Strategy for Palliative Care. Health Affairs 2017; 36(7):1265-1273.
“Hospice is many things.
Hospice is home care with
inpatient back-up facilities.
Hospice is pain control.
Hospice is skilled nursing.
Hospice is a doctor and a
clergyman coming to your
home…But most of all,
hospice is the humanization
of our health care system.” –
Senator Edward Kennedy, 1978
“The really important thing is
meeting patients and families
where they are and delivering the
level of care that most effectively
addresses their physical,
psychosocial, and spiritual
suffering. That may be palliative
care, or it may be hospice. At best,
it’s palliative care now, with a
timely transition to hospice when
curative care is no longer effective
or desired.”
Jennifer Moore Ballentine, Executive
Director CSU Institute for Palliative Care

Discussion: Policy Considerations for the Future
32
© 2019 Dobson DaVanzo & Associates, LLC. All Rights Reserved.
Summary
The purpose of this policy brief is to provide stakeholders with information on the history
of hospice and the hospice value proposition. In so doing, the paper provides a context as
well as a platform for dialogue concerning the above considerations. The following action
items have been identified as opportunities for advancing the hospice value proposition:
o Preserve the integrity of the hospice benefit as Medicare Advantage (MA) plans,
ACOs and other organizational delivery forms as they expand in coming years
o Ensure CMMI accountability for transparency and inclusion of
stakeholder feedback for MA VBID model and hospice, as well as the
Alternative Payment Model for serious illness.
o Concurrently coordinate the hospice benefit with medical and psychological care
under all Medicare payment models
o Develop legislation that will provide patients and families living with
serious illness knowledge and access to information and services.
Direct CMMI to conduct a demonstration that will allow an
interdisciplinary team to provide home-based palliative care services
and assistance in developing goals of care and treatment options, as
well as advance care planning.
o Expand timely access to hospice and palliative care based on the individual’s unique
care needs
o Re-introduce and enact the Rural Access to Hospice (S. 980/H.R. 1828
in 115
th
Congress) legislation to allow physicians and other non-
physician practitioners in Rural Health Clinics and Federally Qualified
Health Centers to serve as a patient’s attending physician when they
elect hospice.
o Ensure high-quality supply of hospice care providers and professionals who are
poised to address the rapidly aging population seeking hospice and palliative care
o Enact PCHETA (H.R. 647) as bipartisan legislation in both the House and
Senate to strengthen education and training opportunities for
physicians and other practitioners.
