
1
P-03062-38 (04/2024)
Nutrition Services
Aging Operations Manual
I. Introduction
This chapter pertains to nutrition services provided by elder nutrition programs funded in whole or in part with federal Older
Americans Act (OAA) Title III and state aging funds, unless otherwise specified.
Section 330 of the Older Americans Act (OAA) states that the purpose of the elder nutrition program is to:
• Reduce hunger, food insecurity, and malnutrition.
• Promote socialization of older adults.
• Promote the health and well-being of older adults by assisting them to gain access to other services.
Elder nutrition programs are administered at the local level by area agencies on aging (AAAs), county aging units (CAUs),
Tribal aging units (TAUs), and other OAA service providers, hereafter referred to collectively as “agencies.” Programs
assist older adults in gaining access to nutrition, disease prevention, and health promotion services to delay the onset of
adverse health conditions resulting from poor nutritional health or sedentary behavior.
Consistent with the objectives in the OAA, elder nutrition programs target services to older adults who have the greatest
economic or social need with particular attention to low-income, minority, and rural individuals. Per
sections 102 (23) and 102
(24) of the OAA, greatest economic need is defined as “need resulting from an income level at or below the poverty line,” and
greatest social need is defined as “need caused by noneconomic factors.” Noneconomic factors include physical and mental
disabilities; language barriers; and cultural, social, or geographic isolation, including isolation caused by racial or ethnic status,
that restrict the ability of an individual to perform normal daily tasks or threaten the capacity of the individual to live
independently.

2
P-03062-38 (04/2024)
II. Requirements for provision of nutrition services
Per section 307 of the OAA, AAAs may not provide nutrition services directly without prior approval from BADR (see
“Waiver for direct services” section of Aging Service Delivery
chapter of this manual). Per Wis. Stat. § 46.82, the duties of
CAUs and TAUs in Wisconsin include organizing and administering congregate meal programs that enable older individuals
and their families to secure a variety of services. Aging units must provide both congregate and home-delivered meals (HDMs)
as a condition of receiving federal and state aging funds. Provision of
carryout meals is optional.
A. Eligibility for services
Under the OAA, nutrition programs may not deny service based on United States citizenship or residency status. OAA
services should be targeted to older adults who are in greatest social and economic need, with no consideration of their
citizenship or residency status.
Residency within a particular county or Tribe in Wisconsin is not required for participation in congregate meals. A
nutrition program will not deny meals to senior dining participants who reside in counties or Tribes outside of its service
area if they meet other eligibility requirements. Such meals provided to eligible individuals can be reported and, if
eligible, claimed for the Nutrition Services Incentive Program (NSIP) by the program providing the meal.
A program may require residency within the county or Tribal service area for HDM participants or may provide HDM
services to individuals who reside outside of the county or Tribe. In such cases, an agreement with the county or Tribe of
residence may be appropriate.
Eligibility criteria for meal participants will be accessible to all potential participants, referral agencies, physicians,
public and private health organizations and institutions, and the public.

3
P-03062-38 (04/2024)
Nutrition programs will make every effort to provide meals to an older person who is eligible and has been determined to
need the service. However, services are not intended to reach every eligible individual in the community, which is why
the OAA requires nutrition programs to target and prioritize services to eligible individuals who are in greatest social and
economic need. Therefore, determination of need for congregate, carryout, and HDM services may be based on
additional criteria established by the AAA or the nutrition program (and approved by the AAA).
1. Eligibility for senior dining (congregate) meals
Per section 339 of the OAA, individuals eligible to receive a meal on a voluntary contribution basis at a senior
dining center are either:
• Aged 60 or older.
• A spouse of an individual who is aged 60 or older, regardless of the spouse’s age.
Section 339 of the OAA specifies that each AAA must allow nutrition programs the option to offer meals on a
voluntary contribution basis to individuals with disabilities who are younger than age 60 and reside with an eligible
older individual. Section 339 of the OAA also creates the option for nutrition programs to offer meals to individuals
with disabilities who are younger than age 60 and reside in a housing facility that is occupied primarily by older
individuals, and at which congregate nutrition services are provided. Such individuals are eligible to receive meals
only at the facility in which they reside.
The OAA defines a disability in section 102(13) as “a mental or physical impairment, or a combination of mental
and physical impairments, that results in substantial functional limitations in one or more of the following areas of
major life activity: self-care, receptive and expressive language, learning, mobility, self-direction, capacity for
independent living, economic self-sufficiency, cognitive functioning, and emotional adjustment.”
4
P-03062-38 (04/2024)
All nutrition program staff, guests, and volunteers who meet the criteria above are eligible program participants.
Participants are not required to provide proof of age or disability to participate. These individuals will be given the
opportunity to contribute to the cost of the meal in accordance with contribution procedures. Per section 339 of the
OAA, nutrition programs will conduct nutrition screening
as part of the program’s registration process.
2. Eligibility for HDMs
This section outlines eligibility criteria for meals delivered to an individual’s residence. See Eligibility for carryout
meals for eligibility criteria specific to carryout meals.
Any of the following individuals are eligible to receive HDMs on a voluntary contribution basis:
• A person aged 60 or older who:
o Is generally unable to leave their home unassisted by reason of accident, illness, disability, frailty, or
isolation.
o Is unable to independently obtain food and prepare adequate meals due to a lack of or inadequacy of
facilities; an inability to shop, cook, or prepare meals safely; or a lack of appropriate knowledge or skill.
o Lacks the support of family, friends, neighbors, or another meal support service in the home or community.
o Is unable to consistently access meals at a congregate dining location due to personal health reasons or other
reasons that make dining in a congregate setting inappropriate.
• A spouse of a person eligible for a HDM as described above, regardless of the spouse’s age.
Section 339 of the OAA specifies that each AAA must allow nutrition programs the option to offer meals on a
voluntary contribution basis to individuals with disabilities who are younger than age 60 and reside with an eligible
older individual.

5
P-03062-38 (04/2024)
The OAA defines a disability in section 102(13) as “a mental or physical impairment, or a combination of mental
and physical impairments, that results in substantial functional limitations in one or more of the following areas of
major life activity: self-care, receptive and expressive language, learning, mobility, self-direction, capacity for
independent living, economic self-sufficiency, cognitive functioning, and emotional adjustment.”
Participants are not required to provide proof of age or disability to participate. These individuals will be given the
opportunity to contribute to the cost of the meal in accordance with contribution procedures.
Authorization from a physician or other certified medical authority is not required for an individual to be eligible
for HDMs. An HDM screening
, on the other hand, is required to determine eligibility for HDM programs.
Circumstances that do require authorization from a program nutritionist or other medical authority include
accommodations of special dietary requests to provide
texture-modified meals (for example, ground meat,
thickened liquids, or pureed foods) or medically-tailored meals that require deviation from nutrition standards.
Nutrition programs cannot require HDM recipients to receive meals at a minimum frequency (for example, five
days per week) to participate.
a. HDM screening and assessment
Section 339 of the OAA requires nutrition programs to conduct nutrition screening and assessment for services.
Each HDM participant will be screened, assessed, and visited in their home to determine their need for nutrition
and other services.
(1) Determination of eligibility and screening
An initial determination of eligibility, including the registration and screening process, may be
accomplished via a detailed telephone or virtual interview that is completed by trained staff. Initial
interviews assist agencies in determining whether congregate, carryout, or HDMs are most appropriate for
the individual.

6
P-03062-38 (04/2024)
(2) In-home visits
An individual eligible for receiving HDMs will be screened and assessed
in their home to determine which
nutrition-related and other supportive services they may need, and then referred as necessary. In-home visits
provide agencies the opportunity to connect participants with education and other resources that will best
meet their nutritional and health needs in alignment with the purposes outlined in section 330 of the OAA.
In-home visits will be completed by trained staff, such as information and assistance specialists, community
health workers, or program nutritionists. Visits will be conducted no later than 12 weeks after beginning
meal service.
b. Determination of continued HDM eligibility
Annual screening and assessments are necessary to establish need for additional services as well as to determine
continued program eligibility. A full reassessment of continued need and eligibility for service will be done
every year. The time between assessments, and the type of assessment (for example, phone, visit, or outreach
worker), will depend on the type of disability, the degree of isolation, and the extent of other resources available
to the individual. For example, an individual just released from a hospital with a broken arm would probably be
reassessed in two to three months, while a relatively healthy individual with a physical disability who has close
extended family might not need reassessment for 12 months.
Most of the reassessment process can be conducted via phone or virtually; however, a home visit is required at
least annually to review any changes to the individual’s health and home environment that might warrant
connection to additional services or resources in alignment with the purposes outlined in section 330 of the
OAA. In-home visits will be conducted by trained staff.
7
P-03062-38 (04/2024)
3. Eligibility for carryout meals
Individuals eligible to receive a carryout meal on a voluntary contribution basis are either:
• Aged 60 or older.
• A spouse of an individual who is aged 60 or older, regardless of the spouse’s age.
Section 339 of the OAA specifies that each AAA must allow nutrition programs the option to offer meals on a
voluntary contribution basis to individuals with disabilities who are younger than age 60 and reside with an eligible
older individual. The OAA defines a disability in section 102(13) as “a mental or physical impairment, or a
combination of mental and physical impairments, that results in substantial functional limitations in one or more of
the following areas of major life activity: self-care, receptive and expressive language, learning, mobility, self-
direction, capacity for independent living, economic self-sufficiency, cognitive functioning, and emotional
adjustment.”
Participants are not required to provide proof of age or disability to participate. These individuals will be given the
opportunity to contribute to the cost of the meal in accordance with contribution procedures. Per section 339 of the
OAA, nutrition programs will conduct nutrition screening
as part of the program’s registration process.
Individuals for which carryout meals might be particularly appropriate include those who meet the eligibility
criteria above but who might not require a meal delivered to their residence. Examples include individuals who:
• Are unable to consume meals at a congregate dining location due to personal health reasons or other reasons
that make dining in a congregate setting inappropriate.
• Have access to transportation to pick up meals.
• Have supports in place to pick up meals on their behalf.

8
P-03062-38 (04/2024)
a. Carryout meal screening and assessment
Section 339 of the OAA requires nutrition programs to conduct nutrition screening and assessment for services.
Carryout meal participants may be screened via phone, virtually, or in person to determine the individual's need
for nutrition and other services. Because carryout meal participants may be receiving meals intermittently or
continuously for personal or programmatic reasons, a home visit is not required. Home visits are recommended
for carryout meal participants who are not receiving other nutrition services so that agencies may better assess
the level of support a participant needs based on their individual situation and connect participants with
education and other resources that will best meet their nutritional and health needs in alignment with the
purposes outlined in section 330 of the OAA.
b. Determination of continued carryout meal eligibility
A reassessment of available nutrition program resources and a participant’s continued need for carryout meals
will be done at least annually, depending on the extent of other resources available to the individual.
4. Volunteers under age 60
Section 339 of the OAA specifies that each AAA must allow nutrition programs the option to offer meals on a
contribution basis to individuals, regardless of age, who are providing volunteer services during the meal hours.
Meals served to volunteers who are under age 60 will be included in the NSIP meal count.
5. Staff under age 60
Nutrition programs may offer meals as a work benefit to staff under age 60 who provide direct service to the
nutrition program These individuals may be offered a meal if there are sufficient meals available for all eligible
participants. The decision to offer meals to staff under age 60 must be approved by the local commission on aging.

9
P-03062-38 (04/2024)
Meals served to staff members who are under age 60 will not be included in the NSIP meal count.
6. Caregivers
Caregivers who do not otherwise meet eligibility criteria for Title III-C nutrition program services may be eligible
to receive meals on a contribution basis through Title III-E caregiver support programs
or through other funding
sources. Federal and state nutrition program funds cannot be used to support these meals.
7. Eligibility for all others
All other people under age 60 may be served congregate or HDMs only if the total cost of providing the service is
paid by the individual, their family, or by another program or payor on the person's behalf. Documentation that full
payment has been made will be maintained by the nutrition program. These meals will not be included in the NSIP
meal count.
If the agency wishes to provide services to other people under age 60, they must use funding source(s) other than
federal OAA, state aging services, local match, and program income.
10
P-03062-38 (04/2024)
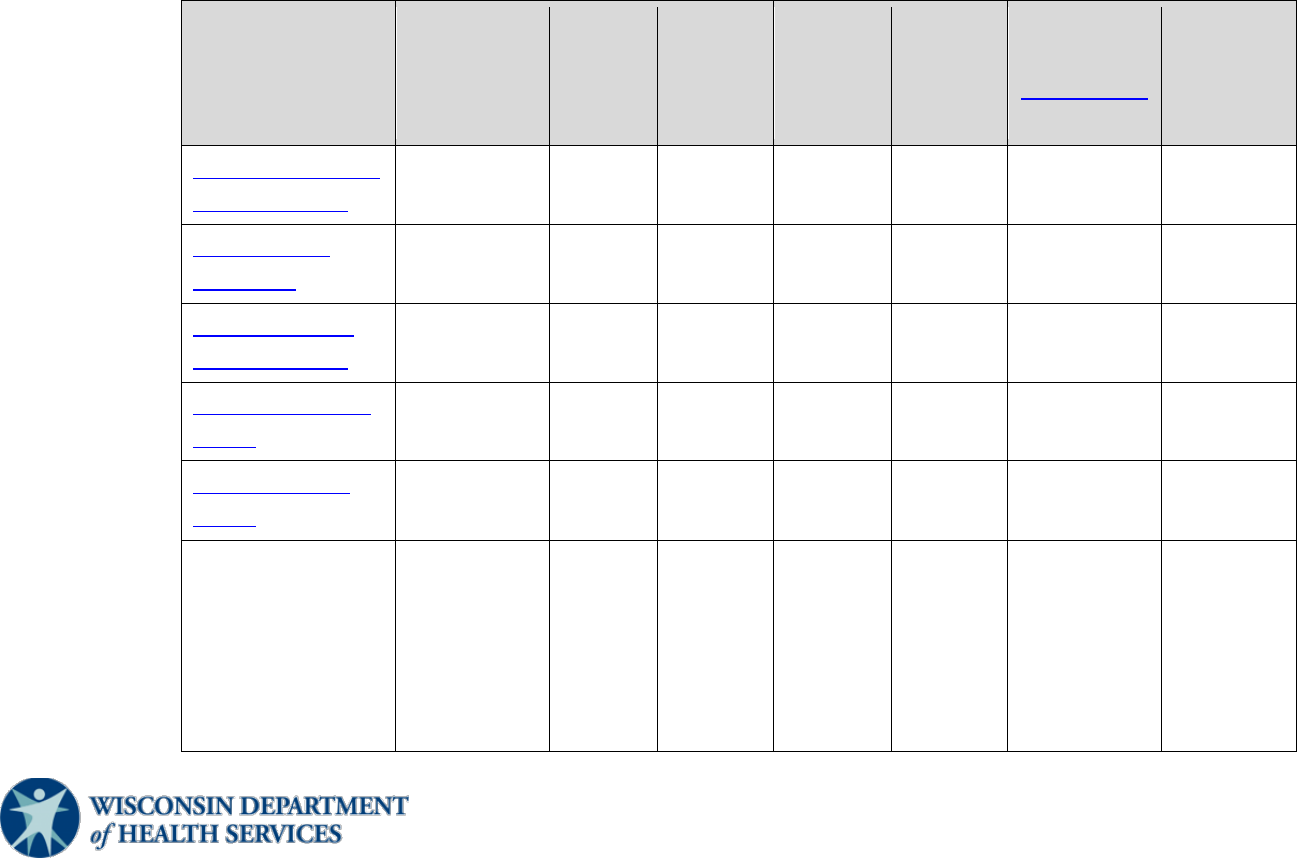
8. Participant eligibility at a glance
The table below summarizes policy and reporting information. See the corresponding section(s) for more
information.
Type of
participant
Offer on a
voluntary
contribution
basis
Recover
full cost
of meal
Included
in NSIP
count
Not
included
in NSIP
count
Local
approval
required
Registration
required
Report as
OAA Title
III meal
Title III congregate
meal participant
X no X no no X X
Title III HDM
participant
X no X no no X X
Title III carryout
meal participant
X no X no no X X
Staff person under
age 60
X no no X X no no
Volunteer under
age 60
X no X X X
All others (guests,
subcontracts such
as community-
based long-term
care, Head Start,
jail, etc.)
no X no X no no no

11
P-03062-38 (04/2024)
B. Level of service
1. Congregate meals
Congregate meals are meals provided by aging units or OAA service providers in a congregate or group setting.
Examples of congregate meals include meals eaten with another person either in-person or virtually, such as virtual
buddy systems or congregate settings (for example, via Zoom, FaceTime, or GoToMeeting) where people dine
together.
Section 331 of the OAA states that the Administration for Community Living (ACL) will make grants available for
the establishment and operation of elder nutrition programs that provide:
• At least one fresh, or otherwise appropriate, meal per day on five or more days per week in congregate settings.
• Nutrition education
, nutrition counseling, and other nutrition services, as appropriate, based on the needs of
meal participants.
To align with requirements in section 331 of the OAA, nutrition programs will, at a minimum, ensure that
congregate meals are available five days per week throughout the program’s service area, which means that some
dining centers might operate five days per week while others might operate fewer than five days per week so that
congregate meals can be provided in more communities throughout the service area.
When locating dining centers, nutrition programs should consider areas where there is significant social and
economic need, as required by the OAA. Low-income and low-access areas
within the service area, if applicable,
will have meals available five days per week. Per section 339 of the OAA, nutrition programs must locate
congregate nutrition services “in settings in as close proximity to the majority of eligible older individuals’
residences as feasible.” Therefore, nutrition programs should ensure that congregate meals are available five days
per week in communities where most older adults live. Section 331 of the OAA states that ACL may define by
regulation rural areas where providing meals at least five days per week is not feasible and that BADR, as
the state
agency, may approve a lesser frequency.

12
P-03062-38 (04/2024)
a. Restaurant model
A nutrition program may establish dining centers in restaurants, cafes, or other food service establishments.
When restaurant models are established, programs are encouraged to partner with locally owned businesses.
“Best practice” restaurant models, such as Wisconsin’s My Meal, My Way restaurant model, offer:
• Meals without reservations.
• Multiple menu options (i.e., choice of two or more meals), with a new menu option rotating in periodically.
• Tips included so that participants are not required to tip.
• Expanded serving times.
• Intergenerational and inclusive settings for dining.
• Coordinated transportation to and from the dining center.
• A dining center manager who greets eligible individuals and helps connect them with other community
services.
b. Voucher programs
A nutrition program may develop a system for issuing vouchers or coupons redeemable for meals at a
restaurant, café, or other food service establishment (see “Vouchers” section of Aging Service Delivery
chapter
of this manual). Prior to implementation, the nutrition program must receive approval from BADR. Aging units
or providers should contact the AAA as soon as they decide to implement a voucher model, so that the AAAs
can provide support and guidance related to feasibility and adherence to the intent of the OAA. AAAs will
make requests to implement voucher models to BADR on behalf of their aging units or service providers.
BADR will grant approval of new locations for one year as a pilot. AAAs are responsible for evaluating
program data and effectiveness in coordination with aging units and providers. BADR will review results before
granting permanent approval. Elements of evaluation will include, but are not limited to, whether:
13
P-03062-38 (04/2024)
• The voucher model is cost effective, for example:
o What are the total meal costs?
o What is the average daily participation?
o How much program income is generated?
• Services are equitably serving target populations outlined in the OAA.
• Participants are utilizing nutrition education services.
• Participants are utilizing other services and resources in the community that promote health.
The following sections detail standards that must be met when implementing voucher programs. This policy
does not apply to meal ticket systems, where tickets are distributed on a voluntary contribution basis for use at
traditional dining centers (see “Tickets” section of Aging Service Delivery
chapter of this manual).
(1) Requirements for nutrition programs
Each nutrition program will:
• Employ a full-time nutrition director. The nutrition program may need to employ the program
nutritionist for additional hours during the planning and implementation of new dining centers.
• Make monitoring visits to each participating food service establishment at least monthly during the pilot
phase and quarterly thereafter to ensure compliance with food safety and sanitation requirements and
nutrition program policies and procedures.
• Provide training to appropriate food service establishment staff on the following topics at least annually:
o Meal standards (including meal pattern requirements and component portion sizes)
o Nutrition program policies and procedures regarding voluntary contributions, confidentiality, and
carryout meals
o Voucher program policies and procedures regarding registering for the program and voucher
redemption (including sharing with the food service establishment the program-related outreach
materials sent to participants)
o Food safety practices for serving the older adult population
14
P-03062-38 (04/2024)
o Indicators of risk to look for in participant’s health or safety
• Have a procedure in place that addresses how misuse of vouchers by both participants and the food
service establishment will be addressed.
(2) Participant registration
The nutrition program will make voucher program materials, including registration forms, available to
eligible program participants at both the aging unit office and at dining locations where vouchers are
accepted.
(3) Voucher issuance and redemption
Local procedures must be established to determine the number of vouchers offered to each participant and to
prioritize issuance of vouchers
to those most in need, if necessary, due to availability of funding.
When an eligible participant redeems a voucher, the food service establishment is responsible for verifying
that the individual redeeming the voucher has registered for the nutrition program as an eligible participant.
Only one voucher can be redeemed per eligible participant per visit. The food service establishment is also
responsible for documenting the meal and/or food items that were provided to the participant (typically on a
receipt) and attaching the participant’s voucher. Food service establishments must submit this information
along with an invoice to the nutrition program according to the billing schedule agreed upon by both parties.
(4) Requirements for participating food service establishments
The food service establishment must:
• Be licensed, follow the Wisconsin Food Code
, and be inspected regularly by the local public health
department.
• Agree to provide meals that meet nutrition program standards.
• Meet accessibility and other dining center facility requirements.

15
P-03062-38 (04/2024)
(5) Requirements for written agreements
Before entering into an agreement with a prospective food service establishment, the nutrition director will
conduct an on-site visit to determine that nutrition program requirements can be met, and appropriate food
safety and sanitation practices are in place.
The nutrition program and the food service establishment must have a written agreement that addresses the
following, in addition to the requirements of contracts with meal providers and requirements for agreements
with restaurants:
• Procedures for tracking voucher usage and reporting to the nutrition program
• Procedures for evaluating service delivery, program quality, and participant satisfaction
Note that this list is not all-inclusive. Nutrition programs may add additional items to agreements as
necessary.
Nutrition programs will submit finalized written agreements to the AAA or BADR for review upon request.
AAAs may request draft agreements as part of the approval process for new voucher locations.
(6) Traditional restaurant dining centers versus voucher programs in restaurants
The following table summarizes the similarities and differences between traditional restaurant dining centers
and voucher programs in restaurant settings.
Characteristic Restaurant model
Voucher program
in a restaurant
Vouchers are provided for participants to redeem at
specified food service establishments.
No X

16
P-03062-38 (04/2024)
Characteristic Restaurant model
Voucher program
in a restaurant
Participants must register and be given the opportunity to
voluntarily contribute toward their meals.
X X
Participants meet at the food service establishment on a
specific day and during a specific time.
X No
Participants can eat at any time during which vouchers are
honored, typically at any time the facility is operating.
No X
A nutrition program representative is on site as a designated
dining center manager during mealtimes. The dining center
manager oversees administrative functions such as signing
in for meals, registering for the program, and collecting and
accounting for contributions made by participants. The
dining center manager also greets participants and serves as
a point of contact for the aging unit.
X No
Participants are given the opportunity to voluntarily
contribute on site at the food service establishment.
X No
The program nutritionist and nutrition director must
approve menus and/or food choices available to program
participants before they are offered.
X X
Specific menu(s) are planned and available for program
participants. All menus offered must meet the nutrition
program’s meal standards.
X X

17
P-03062-38 (04/2024)
Characteristic Restaurant model
Voucher program
in a restaurant
The food service establishment must be licensed, follow the
Wisconsin Food Code, and be inspected regularly by the
local public health department.
X X
The food service establishment must meet accessibility and
facility requirements.
X X
Tips for service staff must be included in the per-meal price
that the nutrition program pays the food service
establishment, unless otherwise approved by the AAA and
BADR.
X X
c. Waivers
Each aging unit or service provider will serve meals in a congregate setting at least once a day, five or more
days per week. Per section 339 of the OAA, in areas where such frequency is not feasible, a lesser frequency
must be approved by BADR through a written request. Aging units or providers should contact the AAA as
soon as the need for a waiver is identified. AAAs will consider the need for a waiver, provide support and
guidance as necessary, and make such requests to BADR on behalf of their aging units or service providers.
Requests must document, at a minimum:
• The need for the request (i.e., reasons that the program is unable to serve meals at least five days per week
throughout the service area).
• Steps that have been taken by the aging unit or provider and/or the AAA in attempts to mitigate the need for
a lesser frequency of meal provision.

18
P-03062-38 (04/2024)
• That the program can better serve target populations in a given location by decreasing days of service at
other locations.
AAAs must review existing waivers to determine any need for change and resubmit requests to BADR
annually. They must also provide support to nutrition programs to ensure that all older adults in the program’s
service area have reasonable access to congregate meals five days per week.
For facility changes, such as new dining centers and temporary or permanent
dining center closures, AAAs
must be notified, and in some cases provide written approval.
2. HDMs
Section 336 of the OAA states that ACL will make grants available for the establishment and operation of nutrition
programs that provide for older adults:
• At least one fresh, or otherwise appropriate, HDM per day on five or more days a week.
• Nutrition education
, nutrition counseling, and other nutrition services, as appropriate, based on the needs of
meal participants.
Section 336 of the OAA also states that ACL may define by regulation rural areas where providing meals at least
five days per week is not feasible and that BADR, as the state agency, may approve a lesser frequency
.
The nutrition program will promptly meet an eligible individual's request for HDMs and will continue to provide
those meals as long as the person needs them, and funding is available. If the HDM program is serving at capacity,
then eligible individuals will be put on a waiting list. Programs may provide two or three meals per day, seven days
per week, to those who need them and/or have no other assistance with their nutritional needs.
19
P-03062-38 (04/2024)
Nutrition programs are responsible for checking on participant’s well-being at the time of delivery, ensuring that
HDMs are delivered to eligible individuals, and ensuring that food is held at safe temperatures and protected from
contamination, animals, or pests. Nutrition program staff or volunteers must deliver meals into the hands of the
recipient, a caregiver, or another person designated by the recipient. Nutrition programs must have procedures in
place that ensure that HDMs are not left unattended if the client is not at home. If a participant does not answer the
door or is non-responsive, nutrition programs should specify procedures for drivers, such as when emergency
contacts or 911 should be called.
With advance notice, alternate delivery arrangements can be made for rare circumstances when an HDM recipient
will not be home to receive the meal. Acceptable examples of alternate delivery arrangements include delivering
two regular meals the day before, delivering a regular meal and a frozen meal the day, before or arranging for a
friend or family member to pick up the meal.
a. Carryout meals
Carryout meals are complete meals offered to participants who choose not to dine in a congregate setting and
instead take the entire meal from the point of service to be eaten at home or another location. Examples of
carryout meals include grab-and-go, pick-up, or drive-through meals. Carryout meals are handled differently
than congregate meal leftovers, in which the meal is consumed in a congregate setting and the participant
chooses to take home an uneaten portion
of it.
Because carryout meals are not provided to participants in a congregate setting, they are classified and reported
as HDMs. Title III-C2 funds
are used to fund carryout meal service. Nutrition programs may also utilize local
funds (beyond what is required for match) to fund carryout meals.
In alignment with the OAA requirements that services are targeted to older adults who have the greatest
economic or social need—paying particular attention to low-income, minority, and rural individuals—nutrition
programs should consider their overall capacity and whether providing carryout meals will contribute to a
waiting list for HDMs delivered to an individual’s residence.

20
P-03062-38 (04/2024)
Agencies offering carryout meals will establish a local procedure, reviewed by the AAA, which describes:
• When carryout meals will be offered, (for example, on a regular, ongoing basis versus only at times of
emergency or staff and/or volunteer shortage).
• How older adults receiving carryout meals will be served if resources are limited.
Carryout meals are subject to the same requirements as congregate and HDMs regarding nutrition education
,
collection of voluntary contributions, and food safety, unless otherwise specified in this chapter.
Nutrition programs offering carryout meals should continuously evaluate utilization of the carryout and
congregate dining models to ensure that those most in socioeconomic need are being provided sufficient access
to, and adequately served by, both service models.
b. Waivers
Each aging unit or contracted service provider for HDM services must provide meals five or more days per
week throughout the entire service area. Per section 336 of the OAA, in areas where such frequency is not
feasible, a lesser frequency must be approved by BADR through a written request. Aging units or providers
should contact the AAA as soon as the need for a waiver is identified. AAAs will consider the need for a
waiver, provide support and guidance as necessary, and make such requests to BADR on behalf of their aging
units or service providers.
Requests must document, at a minimum:
• The need for the request (i.e., reasons that the program is unable to provide meals at least five days per week
throughout the service area).
• Steps that have been taken by the aging unit or provider and/or the AAA in attempts to mitigate the need for
a lesser frequency of meal provision.

21
P-03062-38 (04/2024)
• How low-income and low-access areas within the service area, if applicable, will have meals available at
least five days per week.
• That the program can better serve target populations by decreasing days of service in particular areas (if
applicable).
AAAs must review existing waivers to determine any need for change and resubmit requests to BADR
annually. They must also provide support to nutrition programs to ensure that all older adults in the program’s
service area have reasonable access to HDMs five days per week.
3. Nutrition education
Section 339 of the OAA requires nutrition programs to conduct nutrition education. Nutrition education is defined
by ACL as a targeted program to promote better health by providing accurate and culturally sensitive nutrition,
physical fitness, or health (as it relates to nutrition) information and instruction to meal participants, older adults, or
caregivers in a group or individual setting. Information provided is both:
• Consistent with the current Dietary Guidelines for Americans
.
• Overseen by the program nutritionist, a dietitian, or individual of comparable expertise.
Nutrition education that is suitable to participant needs and interests will be provided a minimum of four times per
year (one time per quarter) to participants in congregate, carryout, and HDM programs. The education is more
effective when the information presented is relevant to a participant's personal, cultural, and socioeconomic
circumstances. When nutrition education is offered outside of the meal programs, participants must be given the
opportunity to voluntarily contribute toward the cost of the nutrition education service. Programs will, with the
advice and consent of nutrition advisory groups and/or the commission on aging, determine whether to set a
suggested contribution amount or contribution range.
Examples of education delivery include cooking demonstrations, educational taste-testing, presentations, and
lectures or small-group discussions, all of which may be augmented with printed materials.

22
P-03062-38 (04/2024)
• When offering food samples at a nutrition education event, food must be served in a safe and sanitary manner
consistent with food code
regulations and must be consistent with nutrition guidelines for the program.
• Nutrition education for HDM participants may consist solely of printed material. Nutrition education for
congregate participants, and to the extent feasible for carryout participants, should include a combination of in-
person or otherwise interactive opportunities with nutrition education provided by printed material.
The program nutritionist will provide input and will review and approve the content of nutrition education before it
is presented.
• Nutrition education topics that must be presented at least once per year include food safety and specific
nutrients of concern for older people, according to the most recent Dietary Guidelines for Americans
(examples
include vitamins B
12
and D).
• Participants will be involved in determining which additional topics to include.
Nutrition programs that need assistance with planning topics or presentations can contact their AAA or BADR for
resources on nutrition education.
4. Nutrition counseling
Section 339 of the OAA requires nutrition programs to provide nutrition counseling when appropriate, based on the
needs of participants and availability of a registered dietitian nutritionist (RDN). Nutrition counseling is a service
that aligns with the Nutrition Care Process of the Academy of Nutrition and Dietetics
(AND). It includes
individualized advice and guidance to older adults about options and methods for improving nutritional status.
Counseling should take into consideration the participant's desires, dietary intake, nutritional and health history,
medication usage, and chronic illnesses, along with cultural, socioeconomic, functional, and psychological factors.
Nutrition counseling will only be performed by an RDN.

23
P-03062-38 (04/2024)
Participants must be given the opportunity to voluntarily contribute toward the cost of the nutrition counseling
service. Programs will, with the advice and consent of nutrition advisory groups and/or the commission on aging,
determine whether to set a suggested contribution amount or contribution range.
Nutrition programs that need assistance with nutrition counseling can contact their AAA or BADR for nutrition
counseling resources.
5. Other nutrition-related services
Nutrition-related supportive services include providing access to food security and other nutrition programs and
food shopping assistance. These services may be provided using Title III-B funds and in some cases, Title III-C
funds. Nutrition programs can also request voluntary contributions from participants.
Section 339 of the OAA encourages agencies to provide medical information to meal participants, particularly
recipients of HDMs. Therefore, at least one time per year, nutrition programs will provide informational brochures
on how to get vaccinations that are typically recommended for older adults (for example, influenza, pneumonia,
shingles, COVID-19, and pertussis). The medical information provided must be approved by a qualified health care
professional, such as a physician or local health department official, and may consist solely of printed material.
a. Liquid nutritional supplements
Liquid nutritional supplements are high-calorie dietary supplement products designed to improve or maintain
the nutrient intakes of those who, because of physical, psychological, or medical problems, are unable to
consume adequate nutrients through traditional foods.
Supplements may be needed as an addition to a complete meal. If the nutrition program is supplying a meal that
includes a supplement, (that is, the participant receives a high-calorie, high-protein supplement in addition to an
HDM), Title III-C funds may be used to purchase the supplement along with the meal. The complete meal is
NSIP eligible.

24
P-03062-38 (04/2024)
Any nutrition program that offers liquid nutritional supplements as part of a complete meal may utilize Title
III-C funds but must follow all of the following procedures:
• The nutrition program will keep on file a written referral from a certified medical authority or the program
nutritionist that includes:
o The participant’s name.
o The reason the participant needs the supplement.
o The type and amount of supplement.
o The name and contact information of the referring certified medical authority or program nutritionist.
• At least once per year, the nutrition program will review each written referral with the certified medical
authority or program nutritionist and the participant or a representative of the participant.
• The nutrition program will only use products meeting the specifications in the referral.
• The nutrition program will handle all products in alignment with practices outlined in the
Wisconsin Food
Code.
A liquid supplement, when offered on its own or as a meal replacement, cannot be counted as a Title III-
C meal and is not NSIP eligible. Therefore, Title III-C funds may not be used in these situations. Either the
full cost of the liquid supplement must be recovered or Title III-B Supportive Services funds could be used to
provide this service on a voluntary contribution basis.
b. Adaptive devices
Nutrition programs will coordinate with the aging unit, aging and disability resource center (ADRC),
independent living center (ILC), or other organizations to make adaptive devices available for use upon request
to support the nutrition needs or preferences of participants who are blind or visually impaired; are Deaf, hard
of hearing, or Deaf-Blind; or have other special needs. Examples include weighted utensils or utensils with
specialized handles, divided plates, cups with handles, and nosey cups. Title III-B or III-C funds may be used
for adaptive devices. Consult BADR or the AAA for more information.

25
P-03062-38 (04/2024)
C. Prioritization of services
When nutrition program resources are fully committed and the program is unable to provide meals to all eligible
individuals on a contribution basis, it may become necessary to determine priorities of service or to create waiting lists
for services.
As long as the intent of the OAA remains intact, the OAA allows states, AAAs, and/or service providers to create
prioritization systems, create waiting lists if necessary, and seek payment for meals by establishing contracts and/or
offering private-pay meals for eligible individuals who might otherwise be placed on waiting lists.
AAAs may develop prioritization systems for their service area if systems are reviewed by BADR before
implementation. Any prioritization systems developed by aging units or providers must be submitted to the AAA for
review and approval before implementation. Tools used in prioritization must be user friendly, fair, and reliable and
target services to eligible individuals who are in greatest social and economic need, as required by the OAA, with
particular attention to older adults who are:
• Individuals with low incomes.
• People of color.
• Residents of rural communities.
• Individuals with limited English proficiency.
• Individuals at risk of institutional care.
In addition to the targeting requirements above, nutrition programs should use factors obtained through screening
processes as criteria for prioritization, such as:
• Food security and/or geographic access to food.
• Malnutrition risk.
• Nutrition risk score.
• Functional status (limitations in Activities of Daily Living and Instrumental Activities of Daily Living).

26
P-03062-38 (04/2024)
• Transportation access.
• Living situation (whether an individual lives alone or faces housing insecurity).
• Availability of other supports and services.
1. Waiting lists
If the program is operating at capacity and there is currently a waiting list for Title III-C nutrition services, nutrition
programs will offer placement on a waiting list to eligible individuals. The decision to place eligible recipients of a
meal on a waiting list, and their position on such a list, is based on greatest social and economic need in accordance
with the OAA and the prioritization and waiting list procedure established by the nutrition program in consultation
with the AAA. Each waiting list procedure established by the nutrition program must be submitted to the AAA for
review and approval before implementation so that AAAs can review service resource usage and efficiency,
offering technical assistance if necessary. AAAs will communicate status of their aging units’ and/or providers’
waiting lists to BADR at least quarterly.
2. Fee-for-service, private-pay systems
Private-pay systems, for which the older adult or their payor agrees to pay to receive services, are separate from
programs funded under the OAA. Nutrition programs may develop private-pay systems, but funds provided under
the OAA may not be used to support private-pay programs or any other services for which fees are required. Meals
served to clients participating in a fee-for-service, private-pay option may not be reported as NSIP meals in the
National Aging Program Information System (NAPIS) state program report.

27
P-03062-38 (04/2024)
Private-pay programs offered by agencies cannot compromise core responsibilities under the OAA. All individuals
eligible for OAA services must be offered the opportunity to receive OAA services on a contribution basis. If an
OAA nutrition program is at capacity, the nutrition program must give eligible individuals the opportunity to be
placed on a waiting list to receive OAA services. After the eligible individual is either placed on the waiting list or
declines placement on the waiting list, the individual can be offered available private-pay options. Agencies will
ensure that no eligible individual is pushed into a fee-for-service, private-pay option or denied service due to the
inability to contribute toward the cost of a meal.
3. Additional meals
When sufficient funding and resources are available, programs may offer additional HDMs to participants on a
voluntary contribution basis. Provision of such meals requires approval from the program nutritionist.
D. Nutrition program meals
Nutrition programs will provide fresh meals, made up of hot and/or cold items, whenever possible. Programs should
provide quality meal services according to the following hierarchy as resources and capacity are available:
1. Fresh (hot and/or cold) meal service.
2. Fresh (hot and/or cold) meal service with provision of a second meal at the same time, such as one hot and one cold
or frozen.
3. Provision of several frozen meals at a time with some fresh items, such as milk, bread, and/or fruit.
4. Provision of several frozen meals at a time.
5. Provision of several shelf-stable meals at a time with some fresh items.
6. Provision of several shelf-stable meals or Federal Emergency Management Administration (FEMA) meals only. This
should be a last resort, or a supplement to fresh or frozen meals.

28
P-03062-38 (04/2024)
A critical component of the HDM services elder nutrition programs provide is a well-being check. If several fresh,
frozen, or shelf-stable meals are provided at a time on an ongoing basis, either due to emergency response or other
reasons, nutrition programs should make a good-faith effort to check on participants on days when an in-person delivery
is not possible. Such efforts can be coordinated with existing staff or partners in the community.
If frozen meals are provided, nutrition programs will communicate with participants to ensure that they have suitable
appliances to safely hold and reheat the frozen meal. If shelf-stable meals are provided, nutrition programs will
communicate with participants to ensure that they can prepare food items for consumption if needed (for example, they
have safe water to add to items to reconstitute for consumption). If a program decides to purchase and distribute
commercially pre-packaged meals, these meals must meet OAA nutrition program guidelines.
1. Nutrition standards
Section 339 of the OAA requires nutrition programs to provide meals to each participating individual that:
• Comply with the most recent Dietary Guidelines for Americans
.
• Provide a minimum of 1/3 of the Dietary Reference Intakes (DRIs) established by the Food and Nutrition Board
of the Institute of Medicine of the National Academy of Sciences, Engineering, and Medicine.
• Are adjusted, to the maximum extent practicable, to meet any special dietary needs of program participants,
including culturally appropriate and medically tailored meals
.
The Elder Nutrition Program is an offer versus serve program. This means that a program is required to offer a
meal that meets nutrition standards, but participants can refuse food items. A refusal does not determine the meal’s
Title III or NSIP eligibility.
a. Dietary Guidelines for Americans and MyPlate food guidance system

29
P-03062-38 (04/2024)
The Dietary Guidelines for Americans is used as a guide for nutrition programs when planning, implementing,
and evaluating meals, nutrition services, and nutrition and health education. The Dietary Guidelines is the
cornerstone of federal nutrition policy and nutrition education activities. It is jointly issued and updated every
five years by the U.S. Department of Agriculture (USDA) and U.S. Department of Health and Human Services
(HHS). The Dietary Guidelines translates the nutrition-based recommendations from the DRI into food and
dietary recommendations. The USDA translates nutritional recommendations from the Dietary Guidelines for
Americans into visual food-based guidelines in the
MyPlate model.
b. Dietary Reference Intakes (DRI)
Established by the Food and Nutrition Board of the National Academy of Sciences' Institute of Medicine, the
DRIs provide nutrition guidance to the public and health professionals. The DRI reference values distinguish
between gender and different life stages.
If one meal is offered, each meal will provide a minimum of 33 1/3% of the current DRI. If two meals per day
are offered, the two meals combined will provide a minimum of 66 2/3% of the DRI. If three meals per day are
offered, the three meals combined will provide 100% of the DRI. Each meal itself does not need to provide
33 1/3% if more than one meal per day is offered.
c. Menu analysis
Each nutrition program is responsible for ensuring that meals planned and offered meet nutritional
requirements. Menus will be analyzed and proven to meet the minimum nutrient and meal pattern
standards
either by:
• Documenting adherence to a meal pattern specified within this manual.
• Conducting a nutrient analysis of all menus served in lieu of adhering to the meal pattern.
• A combination of both methods.

30
P-03062-38 (04/2024)
Documentation of these analyses must be filed with the nutrition program and retained for a minimum of three
years. The program nutritionist must complete and document the analysis before the menu is offered.
d. Meal pattern
Nutrition programs may choose to adhere to the meal pattern for some or all of their meals instead of
conducting a nutrient analysis. The meal pattern is used as a planning tool to ensure that the required types and
amounts of foods are offered. The following meal patterns provide specific meal components and serving sizes
based on the MyPlate food guidance system; however, it does not ensure that the meal pattern will meet
OAA
nutrition standards when meal components are combined. To ensure that these requirements are met, the meal
pattern may require inclusion of increased or additional servings of meal components.
(1) Example 1: Meal pattern (lunch and dinner)
Meal component
Minimum number of
servings per meal Serving size
Grains
1
One-ounce equivalent
Fruits and vegetables
3
1/2 cup fresh, frozen, or canned
(cooked or raw); 1/4 cup dried fruit;
1 cup raw leafy greens; 1/2 cup
100% fruit or vegetable juice
• Dark green vegetable
At least 1 serving per week*
• Red/orange vegetable
At least 2 servings per week*
• Beans, peas, and lentils
At least 1 serving per week*
• Starchy vegetable
At least 2 servings per week*
Milk and fortified soy beverages
1
8 fluid ounces or 1 cup

31
P-03062-38 (04/2024)
Meal component
Minimum number of
servings per meal Serving size
Protein foods
3 ounces
One-ounce equivalent
Fats and oils
1
1 teaspoon served on the side or
used in cooking
Dessert (optional)
1
1/2 cup
A fruit or vegetable contained in a
dessert may count toward the fruit or
vegetable component, respectively.
*Based on a 5-day week
(2) Example 2: Meal pattern (breakfast)
Meal component
Minimum number of
servings per meal Serving size
Grains
1
One-ounce equivalent
Fruits and vegetables
2*
1/2 cup fresh, frozen, or canned
(cooked or raw); 1/4 cup dried fruit;
1 cup raw leafy greens; 1/2 cup
100% fruit or vegetable juice
Milk and fortified soy beverages
1
8 fluid ounces or 1 cup
Protein foods
3 ounces
One-ounce equivalent

32
P-03062-38 (04/2024)
Fats and oils
1
1 teaspoon served on the side or
used in cooking
Additional required item
1
Choose one of the following:
• 1/2 cup serving of fruits or
vegetables
• 1 serving of grains
*Include a variety of fruits and/or vegetables throughout the week.
(3) Vegetarian meals
Vegetarian meals include tofu, soy products, beans, peas, lentils, nuts, and seeds as protein foods. Meats,
poultry, and seafood are not included. Lacto-ovo vegetarian meals include dairy and eggs as protein foods in
addition to protein foods for vegetarian meals.
e. Meal components
Information on each meal component is provided below. When questions arise for a food which is not
mentioned in the manual, such as whether a food fits into a certain category, or what a serving size should be,
the program nutritionist will contact the AAA or BADR for clarification.
(1) Grains
A serving size is a one-ounce equivalent. In order to count a particular food toward the grain requirement, at
least 1/4 serving must be offered.

33
P-03062-38 (04/2024)
Whole grains include all whole grain products and whole grains used as ingredients. Refined grains include
all refined grain products and refined grains used as ingredients.
At least half of all grains offered should be whole grain. Any refined grains offered should be enriched.
Whole grains should be enriched with folic acid.
Limit:
• Added sugars (particularly in grain-based desserts and ready-to-eat breakfast cereals), saturated fat, and
sodium (particularly in breads, tortillas, and crackers).
• Cakes, cookies, and other grain-based desserts to reduce refined grain intake and stay within
recommended calories.
Potatoes do not count as a grain meal component. Acceptable substitutes must be approved by the program
nutritionist.
Examples of allowable foods for the grains component and their serving sizes are available on the
Aging
SharePoint site.
(2) Fruit
The fruit component includes whole fruits and 100% fruit juice. Whole fruits include fresh, frozen, dried, or
canned options. Whole fruits can be served cooked or raw in whole form or cut, sliced, diced, or cubed. To
count a particular food toward the fruit requirement, at least 1/8 cup must be offered.
Nutrition programs are encouraged to incorporate a variety of colors of fruit into menus offered throughout
the week, not only to make meals more colorful and appealing but also to ensure a variety of nutrients and
phytochemicals are accessible to older adult participants. Examples of fruit component serving sizes are
available on the Aging SharePoint site
.

34
P-03062-38 (04/2024)
Juices served should be 100% juice and always pasteurized. At least half of the fruit served should come
from whole fruit, rather than 100% fruit juice. When serving canned fruit, choose options that are canned
with 100% juice or options lowest in added sugars.
(3) Vegetables
The vegetable component includes fresh, frozen, canned, and dried options, including 100% vegetable
juices. Vegetables may be served cooked or raw. Because beans, peas, and lentils have a similar nutrient
profile to foods in both the vegetable or protein foods group, they may be counted as either a vegetable or
protein food but not both in the same meal. To count a particular food toward the vegetable requirement, at
least 1/8 cup must be offered.
Based on their nutrient content, vegetables are organized into five subgroups
: dark green vegetables;
red/orange vegetables; starchy vegetables; beans, peas, and lentils; and other vegetables. Examples of
vegetables included in each of the five subgroups and serving sizes are available on the Aging SharePoint
site. Nutrition programs are required to incorporate all of the vegetable color subgroups into menus offered
throughout the week, not only to make meals more colorful and appealing but also to ensure a variety of
nutrients and phytochemicals are accessible to older adult participants.
No more than one serving of vegetables per meal may come from 100% vegetable juice. Offer fresh or
frozen vegetables whenever possible. If serving canned vegetables, programs are encouraged to choose
options that are lower in sodium. If instant or dehydrated potatoes are used, they must be enriched with
vitamin C. Limit the addition of salt, butter, or creamy sauces to vegetables.
(4) Milk and fortified soy beverages
Most fluid milk and fortified soy beverages offered will be low-fat or fat-free. Examples of allowable foods
for the milk and fortified soy beverages component and their serving sizes are available on the
Aging
SharePoint site. Serving sizes are generally 8 fluid ounces (1 cup) for milk and fortified soy beverages,
unless otherwise noted.

35
P-03062-38 (04/2024)
Cream, sour cream, and cream cheese are not included as allowable foods for the milk and fortified soy
beverages component because they are low in calcium. Other products sold as “milk” but made from plants
(for example, almond, rice, and coconut “milk”) may contain calcium and be consumed as a source of
calcium, but they are not included in this component because their overall nutritional content is not similar
to dairy milk and fortified soy beverages. However, in certain circumstances, milk substitutions with plant-
based products may be necessary to accommodate cultural preferences or special dietary needs
.
To meet vitamin D requirements, nutrition programs may need to serve milk and fortified soy alternatives
that have been fortified with vitamin D.
To meet the high calcium and vitamin D needs of the older adults served in the program, nutrition programs
will also need to incorporate dairy products into other menu items. For example, cheese and yogurt are
considered protein foods and could be offered in addition to milk. Ice cream, frozen yogurt, or pudding
made with milk, which are considered desserts, could also occasionally be offered in addition to milk.
(5) Protein foods
Protein foods include foods from both animal and plant sources. Meat and poultry can include both fresh or
processed options, but most meat and poultry offered should be fresh, frozen, or canned (such as chicken
breast or ground turkey) versus processed (such as hot dogs, sausages, ham, and lunch meats). Meat and
poultry offered should be lean or low fat.
Offering fish, seafood, beans, peas, and lentils more often and offering processed or high-fat meats (such as
hot dogs, sausages, and bacon) less often is encouraged to help older adults meet nutrient recommendations
and protein requirements.
Examples of allowable foods for the protein foods component and their serving sizes are available on the
Aging SharePoint site
. Serving sizes are generally one-ounce equivalents; however, meats, poultry, organ
meats, fish, and seafood are typically offered in three-ounce equivalent portions in meals. To count a
particular food toward the protein food requirement, at least 1/4 ounce equivalent must be offered.

36
P-03062-38 (04/2024)
Fillers or breading used in preparation may not be counted as part of the portion weight. Inedible parts, such
as bone, skin, and sometimes fat, may also not be counted as part of the portion.
Any item labeled with the wording “imitation” cheese or cheese “product” does not meet the nutrient
requirements and cannot be counted as a protein food. Cheese must be pasteurized, and soft cheeses such as
feta, brie, camembert, blue-veined cheeses, and queso fresco should be used with extreme caution, as they
are at increased risk for contamination with Listeria monocytogenes.
Fish and seafood lower in methylmercury is encouraged, such as salmon, anchovies, sardines, Pacific
oysters, trout, tilapia, shrimp, catfish, crab, and flounder.
(6) Fats and oils
Fats and oils may be offered as a spread, dip, or topping for a menu item. Wisconsin Stat. § 97.18 prohibits
the use of colored oleomargarine or margarine at a public eating place as a substitute for table butter unless
it is ordered by the customer. If a nutrition program chooses to offer margarine in addition to butter,
customers (i.e., participants) must be told which spread is margarine and which one is butter.
(7) Dessert
If dessert is offered as a complement to a meal, it should be included in the nutrient analysis of the menu.
Fruits or vegetables offered as a dessert or contained in a dessert may count toward the fruit or vegetable
component, respectively, if at least 1/8 cup of fruits or vegetables exists within each serving.

37
P-03062-38 (04/2024)
f. Nutrient analysis of menus
Nutrition programs may choose to conduct a nutrient analysis of some or all menus they serve, in lieu of
adhering to the meal pattern, to ensure compliance with nutrient standards based on the most current Dietary
Guidelines for Americans and DRIs. The analysis must be prepared and signed by the program nutritionist. If
the analysis is performed by the food vendor, the program nutritionist must evaluate the analysis documentation
and approve the menus.
Nutrient analysis requires standardized recipes and accurate portion sizes, along with utilization of a food
database designed to analyze menus for nutrients. Nutrient analysis may be beneficial for programs that
purchase commercially prepared meals or for programs that contract with larger vendors who can readily supply
the analysis, recipes, and/or types and brands of food products that are used.
(1) When one meal option is offered each day
One meal option means all components of the meal are standardized and there is no choice in variation of
meal components.
In these cases, the weekly average of nutrient content from each meal served during that week is used for
evaluation purposes.
(2) When one meal option is offered each day, but variations of meal components are available
Examples of variations in meal components includes if the participant has a choice of potato or a choice
between different types of milk.
In these cases, individual item choices for each meal component are analyzed and averaged and then added
to the other meal components to get a nutrient analysis for the meal. A weekly average of the nutrient
content from each meal during that week is used for evaluation purposes.

38
P-03062-38 (04/2024)
(3) When multiple meal options are offered each day
An example of multiple meal options is a My Meal, My Way restaurant model that offers four meal options
each day and the options are the same each day.
In these cases, the nutrient analyses for all meal options are averaged to find the overall nutrient analysis for
each day. Each day’s nutrient analysis is then used to calculate the weekly average of nutrient content.
(4) Nutrient standards
The Target column in the table below shows the minimum nutrient standards required for nutrition program
meals, unless otherwise noted in the Acceptable range column. The standards were established in
alignment with DRIs for older adult populations, taking into consideration nutrients of concern specified in
the Dietary Guidelines for Americans
for the general public and older adult population. A weekly average of
nutrient content of meals may be used to evaluate compliance with nutrient standards.

39
P-03062-38 (04/2024)
Nutrient standards for nutrition program meals
Nutrient Target*
Acceptable range (if
applicable)
Calories
725 calories
600–800 calories
Protein
25 g
Carbohydrates**
44 g**
Dietary fiber
8 g
Saturated fat
< 10% of calories or
approximately 7 g
Calcium
400 mg
Potassium
1300 mg
1100–1700 mg
Sodium
1100 mg
765–1200 mg
Vitamin B12
0.8 mcg
Vitamin D***
120 IU
*This is the minimum required amount per meal unless otherwise noted in the Acceptable range column.
**A minimum target of 44 grams of carbohydrates per meal is recommended for the nutrition program’s
general population but not required.
*** Minimum requirements for vitamin D are difficult to reach without using fortified foods or
supplements. Nutrition education will be provided to participants about the selection of foods that are good
sources of vitamin D at least annually.

40
P-03062-38 (04/2024)
2. Hydration
The Dietary Guidelines for Americans states that many older adults do not drink enough fluids to stay hydrated. It
is important that older adults drink plenty of water to prevent dehydration and aid in the digestion of food and
absorption of nutrients, so congregate meal programs should offer water in addition to meals.
3. Meal service and portion sizes
Each program will use standardized portion control procedures to ensure that each offered meal is uniform and
satisfies meal pattern requirements. Standard portions may be altered to be less than the standard serving of an item
only at the request of a participant or if a participant declines an item. NSIP meal eligibility is not affected when a
participant declines menu items. Do not offer less-than-standard portions as a means of "stretching" available food
(for example, to serve additional people).
4. Menu development
Nutrition programs are ultimately responsible for ensuring that meals meet program requirements. The program
nutritionist will plan or oversee the planning of menus. Dietetic professionals are trained and skilled at considering
multiple factors when planning menus and will collaborate with the nutrition director, caterer, cooks, and dining
center staff when planning menus. Menus, where feasible, will take into consideration
religious, cultural, and
overall preferences of participants and the older adults within the nutrition program’s service area, in accordance
with section 339 of the OAA.
Menus will be:
• Shared with participants at each congregate dining center and on the aging unit’s or provider’s website.
• Shared in formats that are legible and easy to read in the language of most of the participants, if not in several
languages.
• Kept on record for three years, to include the menu served each day for each location.

41
P-03062-38 (04/2024)
• Provided in large print (fonts 14 point or larger). If this is not possible, have a large-print version available for
those who are visually impaired.
Each program will retain documentation of its menu development process which includes:
• Use of written, standardized recipes.
• Process for review and approval of menus by the program nutritionist.
• Procedures for revising menus after they have been approved.
5. Self-service food bars
The OAA allows salad and self-service food bars to be counted as a full meal if they meet the nutritional and other
requirements in the OAA. If salad or self-service bars are being offered as a complete meal (with the addition of
milk) rather than a complement to a nutrition program meal, nutrition programs must ensure that all required
components are prepared and offered in sufficient quantities so that all participants can take a meal that meets
nutrition standards.
Nutrition programs must identify the food components that constitute a complete OAA meal(s) near to or at the
beginning of the serving line(s). Nutrition programs have the discretion to determine the best way to present this
information, including how to clarify which foods must be selected from the salad or self-service bar to create a
complete OAA meal.
6. Special meals
Section 339 of the OAA states that, to the maximum extent practicable, meals provided through the OAA are
adjusted to meet any special dietary needs of program participants, including meals adjusted for cultural
considerations and preferences and medically tailored meals. As with all menus, special meals must be reviewed
and approved by the program nutritionist.

42
P-03062-38 (04/2024)
a. Culturally appropriate meals
Per the Dietary Guidelines for Americans, the food groups include a broad variety of nutrient-dense food and
beverage choices, so that in every setting, across all cultures, and at any age or budget, there are foods and
beverages that can fit within the Dietary Guidelines framework; and therefore, the nutrition program’s nutrition
standards.
Nutrition programs should rely on the expertise of program nutritionists and the input of older adults in their
service area to create culturally appropriate menus.
(1) Native traditional or indigenous foods
Nutrition programs are permitted to accept donations of and serve locally grown and raised
traditional or
indigenous foods at public facilities and nonprofit facilities, including those operated by Native American
Tribal Nations and facilities operated by organizations that primarily serve Native people.
As with all menus, menus containing traditional foods must be reviewed and approved by the program
nutritionist to ensure nutritional adequacy and compliance.

43
P-03062-38 (04/2024)
b. Meals that accommodate food allergies
Nutrition programs are strongly encouraged to explore the feasibility and cost-effectiveness of providing special
meals for participants with food allergies. The Americans with Disabilities Act (ADA) considers some food
allergies, such as allergies to nuts or fish, to be disabilities that require reasonable accommodations. Reasonable
accommodations should not be overly expensive or burdensome to the nutrition program (see
ADA Title II:
State and Local Government Activities). The presence of food allergies may require procedures to avoid cross-
contact of the allergenic food with other foods. Modifications that are reasonable can include product
substitution, menu choice, and other strategies. The nutrition program may consider developing a plan based on
their resources and available products and include the participant in determining the preferred alternative for the
best outcome. If the severity of the food allergy requires a meal with significant alterations to the types of food
required in the regular meal pattern, a statement from a physician or the program’s nutritionist to document the
allergy is recommended.
BADR strongly advises agencies to consult with their legal counsel for additional guidance and to include
disclaimers and identification of items containing common allergens on menus, especially in cases when it is
determined that reasonable accommodations cannot be made. Screening for food allergies and intolerances
during the program registration process is also recommended.
c. Medically tailored meals
In cases when the participant needs meals to treat a variety of diseases and disorders, medically tailored meals
are encouraged. These meals could change the meal pattern significantly by either limiting or eliminating one or
more of the menu items or by limiting the types of foods allowed. This may result in a meal that deviates from
the meal pattern and/or nutrient standards of the program.
Medically tailored meals might include:
• Renal diet.

44
P-03062-38 (04/2024)
• Low residue meal.
• Gluten-free meal.
If the nutrition program offers medically tailored meals that deviate from the meal pattern or nutrient standards
of the program:
• A written diet order from a certified medical authority or the program’s nutritionist must be on file with the
nutrition program.
• At least once per year, the program nutritionist must review each written diet order with the certified
medical authority (if applicable) and the participant or a representative of the participant. The diet order
should be updated accordingly.
• Special meal types and component amounts must adhere as closely as possible to the meal pattern and the
nutrient standards of the program.
d. Texture-modified meals
Texture-modified meals may be acceptable for participants who have chewing and/or swallowing problems. A
texture-modified meal might include ground meat, mechanical soft foods, thickened liquids, or pureed foods.
Note: Clear-liquid meals and full-liquid meals are not allowed.
Any nutrition program that offers texture-modified meals must ensure that meals are prepared by a foodservice
operation that has sufficient training in preparing texture-modified meals. A written diet order from a certified
medical authority or the program’s nutritionist must be on file with the nutrition program if the meal deviates
from the meal pattern or nutrient standards of the program and will be reviewed with the participant or a
representative of the participant at least annually.

45
P-03062-38 (04/2024)
E. Food safety
Section 339(2)(F) of the OAA requires programs to provide meals that "comply with applicable provisions of State or
local laws regarding the safe and sanitary handling of food, equipment, and supplies used in the storage, preparation,
service and delivery of meals to an older individual."
Safe food practices by nutrition programs cannot be compromised. In all phases of the food service operation, nutrition
programs will adhere to state, Tribal, and local fire, health, sanitation, and safety regulations applicable to the types of
food-preparation and meal-delivery systems used by the program.
1. Wisconsin Food Code
The State of Wisconsin Department of Agriculture, Trade and Consumer Protection (DATCP) develops sets of laws
for restaurants and other food service establishments. The Wisconsin Food Code
, based on the U.S. Food and Drug
Administration's recommended model food code, is the state law that the OAA, as noted above, requires
Wisconsin’s elder nutrition programs to follow.
2. Obtaining food for meals
Per the Wisconsin Food Code, all nutrition programs will obtain food from sources that comply with applicable
local, Tribal, state, and federal statutes, regulations, and ordinances. The Wisconsin Food Code specifies
requirements for obtaining specific foods, such as eggs, food in hermetically sealed containers (for example, canned
goods), milk and milk products, fish, shellfish, wild mushrooms, and game animals.
Food prepared in a private home cannot be used or offered for human consumption as part of a nutrition program
meal.

46
P-03062-38 (04/2024)
3. Use of donated or discounted food
Using donated or discounted food from a food bank can significantly reduce food costs. Nutrition programs may
use contributed and discounted foods only if they meet the same standards of quality, sanitation, and safety as those
that apply to foods purchased from commercial sources.
Acceptable items include:
• Fresh fruits and vegetables received clean and in good condition, and not cut, skinned, peeled, or otherwise
processed.
• Eggs that are intact (that is, in the shell with no cracks). Note that if eggs are not pasteurized, they can only be
used if prepared and served in compliance with the Wisconsin Food Code’s recommendations for highly
susceptible populations.
• Game animals and fish that meet requirements in the Wisconsin Food Code or applicable Tribal food code.
• Food collected from a food bank that can be prepared and served before the use-by date.
In accordance with the Wisconsin Food Code, unacceptable items include:
• Food that has passed its use-by date.
• Home-canned or preserved foods.
• Foods cooked or prepared in an individual's home.
• Road-killed deer or game.
• Wild game donated by hunters, unless permitted by applicable Tribal food code.
• Fish donated by sportsmen, unless permitted by applicable Tribal food code.
• Alcoholic beverages.
A local nutrition program may determine and specify with a local policy that it does not wish to incorporate
donated or discounted foods into its menus.

47
P-03062-38 (04/2024)
If a participant wishes to bring in an “unacceptable” donated food to share with participants, such as a birthday cake
prepared in a private home, it is permitted only if the food is kept completely separate from the nutrition program’s
food and if participants are informed that these items were prepared in a private home and may not have been
prepared using standard practices that comply with the Wisconsin Food Code
.
a. Tribal nutrition programs
Nutrition programs operated in public and nonprofit facilities, including those operated by Native Tribal
Nations and facilities operated by organizations that primarily serve Native elders, may accept donated food if
the Tribal Nation’s food code permits food donations and considers the food to be from an approved source.
Programs that choose to accept the donation of traditional food must follow Tribal Nation law regarding the
safe preparation and service of food in public or nonprofit facilities. Licensure and regular inspections of all
facilities involved in the flow of food from the time the food is obtained until it is served to an elder is strongly
encouraged to ensure food safety.
4. Food temperatures
The federal and state standard for receiving, holding, and serving temperatures for potentially hazardous TCS
(time/temperature control for safety) foods is no higher than 41 ºF for cold foods and no lower than 135 ºF for hot
foods.
Nutrition programs must monitor food temperatures with regularly calibrated thermometers. Follow the
manufacturer’s directions regarding calibration. Calibrate thermometers:
• At least once per week.
• After they have been bumped or dropped.
• Anytime it is suspected the thermometer has lost calibration.

48
P-03062-38 (04/2024)
Food temperatures should be monitored for compliance with the Wisconsin Food Code at the following times, at a
minimum:
• At the time of food arrival (for catered operations)
• At the time of service (for senior dining meals)
• At the time of packaging (for off-site delivery, including HDMs)
• Every four hours while the food is being held until all the meals are served to participants
Each nutrition program will have written procedures for handling TCS foods that do not meet or maintain correct
temperatures. Food temperature records are to be kept on file for a period of one year.
a. Receiving prepared food
TCS prepared hot food and hot food items that arrive at a temperature below 135 °F can be accepted and
reheated to 165 °F only if:
• There is clear documentation of the time the food was cooked, and that the food was cooked to the proper
temperature.
• There is clear documentation of the time the food left the preparation facility, that the food left the
preparation facility at the proper temperature, and that the time between when the food left the preparation
facility and the food being received by the nutrition program does not exceed two hours.
• The food can be reheated to the proper temperature so that the time in which the food was below required
temperatures is less than two hours and can be documented as such.
TCS prepared cold food and raw cold food items that arrives at a temperature higher than 41 °F can be accepted
and cooled to proper temperatures only if:
• There is clear documentation of the time the food was prepared, and that the food was held at the proper
temperature.

49
P-03062-38 (04/2024)
• There is clear documentation of the time the food left the preparation facility and that it was at the proper
temperature when it left.
• There is clear documentation that the food temperature never exceeded 45 °F .
The following foods will be rejected:
• Foods that do not meet temperature requirements above
• Frozen foods that show signs of temperature abuse (for example, ice crystals)
• Foods that are past their expiration dates when received
In catered operations, food transport slips that document the time and temperature of the food when it left the
preparation facility are required. Contract language should state that rejected food will be returned to the
caterer. Either the monetary value of the rejected food should be subtracted from the reimbursement to the
caterer for that day or the caterer should immediately supply a substitute item that complies with nutrition
program guidelines for meal service that day.
b. Serving and holding food
Food temperatures at the time of service or delivery must be no less than 135 °F for hot foods and no more than
41 °F for cold foods.
Food quality and safety is best ensured when the time between the end of preparation of either hot or cold food
and service or delivery to the participant is kept to a minimum.
Food establishments that primarily serve a highly susceptible population, which includes the elder nutrition
program, should hold TCS foods with temperature control. In alignment with § 3−501.19(e) of the Wisconsin
Food Code, time as a public health control may not be used as a method to avoid compliance with temperature
requirements.

50
P-03062-38 (04/2024)
Time as a public health control may only be used by elder nutrition programs operating their own licensed
cooking and preparation facilities. Written plans must be created and reviewed by local public health officials
during the facility’s inspection. In alignment with the Wisconsin Food Code, written plans are food specific. In
other words, plans are not a general practice that apply to most food items served by the nutrition program.
Written plans will document when use of time as a public health control begins and ends and will specify
methods of compliance where the program can document that meals left the facility at proper temperatures and
were delivered within four hours. When time as a public health control is used, all remaining food after service
or delivery must be discarded.
All nutrition programs must have equipment that maintains the safe temperature of all menu items from the end
of the cooking process through the end of the serving or delivery period.
Vehicles used in the transportation of bulk food or HDMs will be equipped with clean containers or cabinets to
store the food while in transit. The containers or cabinets will be constructed in a way that prevents food
contamination by dust, insects, animals, vermin, or infection. The containers or cabinets will also be capable of
maintaining a temperature at or above 135 °F or a temperature at or below 41 °F until the food is delivered to
the dining center or to the HDM recipient.
(1) Salad and self-service bars
Nutrition programs with self-service bars must have food safety procedures in place to ensure safe foods for
participants. Factors such as layout and space available in the serving area, equipment available to protect
the food on the bar from contamination, staffing available to monitor the bar during meal service, and
training for staff and participants must be considered in determining how to safely incorporate a bar into the
nutrition program. Salad and self-service bar equipment must comply with requirements for self-service
equipment outlined in the Wisconsin Food Code and by local public health officials.

51
P-03062-38 (04/2024)
c. Heating and reheating food
Nutrition programs must use equipment that is capable of heating and reheating food to required temperatures
within required timeframes. Hot-holding equipment, such as steam tables, and crockpots or slow cookers may
not be used to heat or reheat TCS foods.
d. Meal delivery
Food will be delivered at safe temperatures to prevent foodborne illness.
• Hot food will be maintained and delivered at 135 °F or above unless the program meets requirements for use
of time as a public health control
.
• Cold food will be maintained and delivered at 41 °F or below unless the program meets requirements for use
of time as a public health control
.
• Frozen food will be maintained and delivered in a solid frozen state.
Leaving meals outside, in coolers, or otherwise unattended is prohibited.
(1) HDM test trays
To ensure food safety for HDMs, the program will test HDMs for temperature compliance no less than
quarterly. This can be done by transporting an extra meal on an HDM route and taking the temperature of
the meal after all other meals have been delivered or at the time the driver returns to the HDM dispatch site.
All menu items that require temperature control must be tested each time and the temperatures documented,
along with any corrective action taken.
If routes remain consistent and documented temperatures of quarterly test trays show that food is maintained
at proper temperatures, more frequent test trays are not required. However, if route times increase, if there is
staff or volunteer driver turnover, if equipment used is changed, or if there are other changes that could
affect temperature compliance, programs must retest HDM temperatures at the end of the route.

52
P-03062-38 (04/2024)
e. Bare-hand contact with ready-to-eat food
Because nutrition programs primarily serve a population that is highly susceptible to foodborne illness, bare-
hand contact with ready-to-eat foods is prohibited. Gloves, deli paper, tongs, or other suitable utensils should be
used to handle ready-to-eat foods.
f. Effective hair restraints
Staff and volunteers must wear hair restraints, such as hats, hair coverings or nets, beard restraints, and clothing
that covers body hair, which are designed and worn to effectively keep their hair from contacting exposed food,
clean equipment, utensils, linens, and unwrapped single-service and single-use articles such as disposable cups
and utensils. This does not generally apply to staff and volunteers in the dining area who are greeters or serve as
wait staff if they present a minimal risk of contaminating exposed food or food-contact surfaces.
5. Instructions for participants
Program staff and volunteers will educate participants on safe food handling practices. Written instructions will be
given to participants for safe handling and reheating of HDMs, carryout meals, and parts of congregate meals taken
home upon initiation of the service and at least annually thereafter. All home-delivered and carryout meals will be
clearly marked with the date the meal was served or a date by which the meal should be consumed.
6. Taking food home
Senior dining participants have the option to take home any part of a meal served to them at a dining center. The
safety of food after it has been served to a participant and when it has been removed from the dining center is the
responsibility of the participant. Over-ordering or over-producing food for the specific intent of producing leftovers
that can be taken home is not allowed.

53
P-03062-38 (04/2024)
7. Foodborne illness outbreaks
If a nutrition program suspects a foodborne illness outbreak, the following should be done at the local level:
• Gather information (for example, contact information for affected people, food eaten that caused the outbreak,
time of onset and description of symptoms from affected people).
• Notify the local public health department. Provide appropriate documentation, such as temperature logs, Hazard
Analysis Critical Control Point (HACCP) documents, and staff files.
• Set the suspected product aside, away from program-related food, if any remains. Include a label with “Do Not
Use” and “Do Not Discard” on the product.
• Log information about the suspected product. This might include a product description, production date, and lot
number. The sell-by date and pack size should also be recorded.
• Maintain a list of food handlers scheduled at the time of the suspected contamination. Interview them
immediately about their health status.
Nutrition programs suspecting a foodborne illness outbreak must also report the foodborne illness to the AAA and
BADR.
III. Collaborating with other programs
A. Collaborating with aging programs
1. Supportive services
Nutrition services provide an important link to other supportive in-home and community-based services such as
homemaker and personal care, transportation, physical activity, and home repair and modification programs.

54
P-03062-38 (04/2024)
2. Caregiver support programs
Caregivers who do not otherwise meet eligibility criteria for Title III-C nutrition services may be eligible to receive
meals, nutrition counseling, or nutrition education as a supplemental service of the
National Family Caregiver
Support Program (NFCSP) or Alzheimer’s Family Caregiver Support Program (AFCSP). Caregiver support
program coordinators will complete a caregiver needs assessment to determine need for nutrition services in
coordination with the nutrition program. Per AFCSP policy, completion of
DHS form F-02425 is required to
purchase home-delivered or congregate meals. The caregiver’s signature ensures that they are aware they are
choosing to use their limited AFCSP funds to pay for the full cost of the meal. It is also best practice to use form
F-02425 with caregivers enrolled in NFCSP as a way to coordinate among the two programs and the caregiver. For
those enrolled in NFCSP, an opportunity to voluntarily contribute towards the meal will be provided in accordance
with OAA Title III-E requirements, and program income will be used to expand Title III-E services.
3. Health promotion programs
Nutrition services provide an important link to both evidence-based and non-evidence-based health promotion
programs, such as chronic disease self-management programs and falls prevention programs. Some evidence-based
and non-evidence-based health promotion programs can also be provided as nutrition education.
4. Adult protective services
All regular nutrition program staff and volunteers need to know the signs of abuse, neglect, and exploitation and be
able to identify participants who may be at risk of abuse, neglect, self-neglect, self-harm, or financial exploitation
and who need adult protective services (APS). When staff or volunteers identify customers who may need elder
abuse or adult protective services, nutrition directors should provide or facilitate access to those services through
cooperation with APS and/or the ADRC.

55
P-03062-38 (04/2024)
5. Elder benefit specialist (EBS) program
Elder benefit specialists (EBSs), as stated in Wis. Stat. § 46.81, offer “information, advice, and assistance to older
individuals related to individual eligibility for, and problems with, public benefits and services and to health care
financing, insurance, housing, and other financial and consumer concerns.” The EBS program gives priority to
those in highest social and economic need and addresses legal and benefit issues related to basic needs, such as
food. Nutrition services participants may need assistance in accessing benefits, such as FoodShare. Through in-
home screenings and assessments, nutrition programs may identify other benefits or services that nutrition program
participants need, such as housing assistance or health insurance.
6. Transportation services
Per Section 321 of the OAA, transportation services provided under the OAA should facilitate access to nutrition
services. Nutrition programs should collaborate with transportation service providers to ensure access to nutrition
services whenever feasible.
7. Title VI programs
AAAs, CAUs, and OAA service providers of nutrition services should coordinate with Title VI programs,
especially if a Title VI program (e.g., Tribal lands) exists within their service area. Nutrition programs can:
• Work with Title VI programs to ensure that Native elders are aware of Title III nutrition services.
• Share nutrition program information.
• Work with Title VI programs to ensure culturally appropriate services are available to Native elders when
feasible.
• Include representation from Title VI programs and/or Native elders on the nutrition advisory council.

56
P-03062-38 (04/2024)
B. Collaborating with ADRC programs
1. Information and assistance
The ADRC’s information and assistance (I&A) specialists and Tribal aging and disability resource specialists
(ADRSs) listen to and support older adult customers and customers with disabilities, assessing their needs and
personal preferences, identifying the most appropriate resource(s) to meet their needs, helping them to connect with
service provider(s), and providing information to meet their needs using a person-centered approach. Services may
be provided in person at the person's home or at the ADRC as an appointment or walk-in, over the telephone,
virtually, via email, or through written correspondence. Nutrition programs may collaborate with the ADRC’s
information and assistance specialists to connect older adults with nutrition services, complete service registrations,
or conduct in-home screening for HDMs
.
C. Collaborating with other community programs
1. USDA Supplemental Nutrition Assistance Program (FoodShare Wisconsin)
Nutrition programs will assist participants to take advantage of benefits available to them under the Supplemental
Nutrition Assistance Program (SNAP). In Wisconsin, this program is called FoodShare
. FoodShare uses an
electronic benefit transfer (EBT) system in the form of a benefit card, which is used like a credit card. With help
from the benefit specialist, nutrition programs can assist participants in applying for and using FoodShare benefits.

57
P-03062-38 (04/2024)
2. The Emergency Food Assistance Program
The Emergency Food Assistance Program (TEFAP) is a federally funded program that provides food assistance to
individuals with low incomes. Food is distributed through local agencies, such as food pantries and prepared meal
sites such as soup kitchens or emergency shelters. Nutrition programs can partner with TEFAP to help older adults
stock their pantries with food for household use. AAAs and local nutrition service providers may work with TEFAP
to help stock and operate a mobile food pantry. These mobile units may go to senior housing, a local on-site pantry
at the congregate site that disburses foods for congregate or home-delivered participants before a storm or use foods
from TEFAP to assemble grocery bags for older adults.
3. Senior Farmers Market Nutrition Program
The Senior Farmers Market Nutrition Program (SFMNP) is a program authorized through the federal Farm Bill.
The program serves lower income adults aged 60 and older who live in participating counties in Wisconsin. The
program provides annual vouchers that eligible older adults can use to buy local, fresh foods from farmers markets,
roadside stands, and community-supported agriculture (CSA) programs. In many areas of the state, aging units and
ADRCs are the local agencies that distribute vouchers to eligible older adults, so nutrition programs can distribute
vouchers to eligible older adults at aging units, ADRCs, or congregate dining locations. Nutrition programs can
also collaborate with SFMNPs on provision of nutrition education and assist in providing older adults with access
to farmers markets.
4. Commodity Supplemental Food Program
The Commodity Supplemental Food Program (CSFP) is a program that serves lower income adults aged 60 and
older who are in participating areas of Wisconsin. The program provides free monthly food boxes to eligible
individuals. Nutrition programs can help increase access to this program for eligible older adults. Nutrition
programs can also collaborate with CFSPs on provision of nutrition education.

58
P-03062-38 (04/2024)
5. Child and Adult Care Food Program
The Child and Adult Care Food Program (CACFP) operates in some non-residential adult day care centers that
serve adults aged 60 and older. The program provides reimbursement for nutritious snacks and meals to older adults
enrolled in participating adult day care centers. Nutrition programs can potentially operate CACFP as a separate
program in adult day care settings.
6. Adult day care programs or other programs serving older adults
Nutrition programs are not required to provide meals to adult day care participants or participants of other programs
that serve older adults. However, nutrition directors may plan with such programs to provide meals or other
nutrition services, if desired.
For a nutrition program to report meals provided to an adult day care center as an OAA congregate meal, all of the
following must be true:
• The meal must be provided to a participant eligible for congregate meals.
• The meal must be offered in a congregate setting.
• Participants must be offered the opportunity to contribute toward the cost of their meal in accordance with
Section 315 of the OAA.
• The meal must not be part of the cost of the adult day care service to the program participant. (Section 315 of
the OAA prohibits cost sharing for congregate meals.)
The nutrition program will charge the adult day care program for the total cost (at a minimum) of providing meals
or other nutrition services to its participants if any of the following is true:
• The adult day care program wants the nutrition program to provide meals to the adult day care program as a
caterer.
• The adult day care program includes a meal in the cost that it charges to adult day care participants.

59
P-03062-38 (04/2024)
• The adult day care participant does not meet eligibility requirements to participate in the congregate nutrition
program (for example, if under 60 years old).
A written agreement for provision of services should exist between both programs. The agreement may also include
supplemental information, such as:
• Who will provide supervision of the adult day care or other program’s participants while at dining centers?
• Is it necessary to make reservations in advance?
• Under what other circumstances may participants attend the dining center?
7. Intergenerational partnerships
Section 339 of the OAA encourages joint arrangements with schools and other organizations serving meals to
children to promote intergenerational meal programs.
a. Local schools
Since 1973, two nutrition programs for elder adults have existed in Wisconsin. Both programs are open to older
adults and provide opportunities for older adults to maintain and improve their diets:
• Elder nutrition improvement program: Wisconsin Stat. § 115.345
authorizes the establishment of an
elder nutrition improvement program in Wisconsin’s public schools. It places the administrative
responsibility for the program with the Department of Public Instruction (DPI). The law provides the
participating school districts with sum-sufficient funding for supplemental payments, not to exceed 15% of
the cost of the meal or $0.50 per meal, whichever is less. School participation in the program is voluntary.
• Title III OAA elder nutrition program: BADR (within the Department of Health Services) is the state
agency responsible for the administration of the Title III elder nutrition program under the OAA. Title III
elder nutrition programs are subject to the federal regulations and state policies referenced in this chapter.

60
P-03062-38 (04/2024)
While each of the elder nutrition programs may operate separately and independently, the Wisconsin legislature
directs that the programs cooperate to take advantage of the cash benefits and intergenerational opportunities
available under both programs:
"The Departments of Health and Social Services (now known as the Department of Health
Services) and Public Instruction shall develop procedures for facilitating participation by public
school districts as food service providers in nutrition programs financed under Title III-C of the
Older Americans Act."
BADR and the DPI School Nutrition Team have developed policies and procedures for congregate nutrition
programs, which school districts follow in their efforts to develop joint agreements. As they are updated, copies
of the joint agreement guidelines are sent to the school districts and to nutrition programs. The joint agreement
can be found at the DPI School Nutrition Team website
.
b. Summer Food Service Program
The Summer Food Service Program (SFSP) is a federally funded, state-administered program that reimburses
program operators who serve free healthy meals and snacks to children and teens in low-income areas during
the summer months, when children do not have access to school meals. Nutrition programs could apply to be a
program sponsor with DPI or partner with existing SFSP sponsors to co-host meals for SFSP and congregate
dining participants.
8. Community-based residential facilities
Nutrition programs are not required to provide meals to residents of group living homes, assisted living facilities, or
other community-based residential facilities. If such facility does not offer meals to its residents, and the nutrition
program decides to enter into an arrangement to provide OAA meals, contact the AAA for guidance and technical
assistance.

61
P-03062-38 (04/2024)
9. Other organizations purchasing nutrition services
Per section 212 of the OAA, agencies may enter into agreements with for-profit organizations whereby they
provide nutrition services to individuals or entities not otherwise receiving services through the OAA. In this case,
the agency is selling services and therefore acting as a retail food establishment. Contact the local public health
department to determine if additional licensing regulations or Wisconsin Food Code requirements apply.
a. Community-based long-term care programs
Community-based long-term care programs, such as Family Care, IRIS (Include, Respect, I Self-Direct), and
other Medicaid waiver programs, can contract with nutrition programs to provide meals to long-term care
program clients. Managed care organizations operating community-based long-term care programs do a
functional screen to determine which services a client needs. Programs are self-directed, so the client has a role
in working with their care manager to select which needed services (per the functional screen) to include in their
authorized care plan. Depending on the program, the care manager may lead the budgeting process and
selection of appropriate services, or the client may have a more significant role working in coordination with
their care manager to select the services within their budget.
According to federal Medicaid guidance
, “Medicaid is generally the ‘payer of last resort,’ meaning that
Medicaid only pays claims for covered items and services if there are no other liable third party payers for the
same items and services.” However, “Medicaid will pay for a service if there is another party that may—but is
not legally obligated to—pay for the service. […] Under the OAA, there is a source of funding to cover some
services that are also covered by Medicaid. Individuals, however, are not legally entitled to receive services
through the OAA, and thus the OAA program has no legal obligation to cover those services. Since the OAA
program is not legally liable for the service, the OAA does not fall within the definition of ‘third party.’
Accordingly, Medicaid will pay for a service even if the OAA program would also pay for the service.”

62
P-03062-38 (04/2024)
Nutrition programs must have a contract, memorandum of understanding, or other written agreement between
the agencies providing each program, which aligns with the requirements of section 212 of the OAA. In
accordance with section 321(d) of the OAA, programs must also recover the full cost of each meal sold to the
community-based long-term care program, including overhead and administration, so that Title III funds or
resources are not used to subsidize these meals. Because these meals are not funded with Title III funding or
resources, they are not subject to most Title III rules. For example, an HDM screening and assessment
is not
required to be performed by the nutrition program if the community-based long-term care program has
determined meals are needed for its client.
IV. Operational policies and procedures
A. Statutory references
• Older Americans Act, reauthorized in 2020 and amended through Public Law 116-131
• Wisconsin State Statutes, Chapter 448, "Medical Practices," Subchapter V, Dietitians Affiliated Credentialing Board
• Wisconsin Food Code
• Wisconsin State Statutes, Chapter 115
• Wisconsin State Statutes, Chapter 46.80
B. Agency requirements
1. Staffing
a. Nutrition program staff and volunteers

63
P-03062-38 (04/2024)
Each agency will employ for the nutrition program an adequate number of qualified staff, supplemented as
necessary by qualified consultants, to ensure the provision of program leadership, planning, food service
management, nutrition services, and other services.
Nutrition programs must comply with applicable personnel policies and with the requirements stated in this
chapter.
b. Nutrition program director
A full-time nutrition director at both the AAA and aging unit level is responsible for the day-to-day
management and administrative functions of the program.
Aging unit nutrition directors are responsible for ensuring that the following tasks are accomplished:
• Planning, developing, implementing, and coordinating all programs and services included within the
nutrition program
• Preparing and enforcing local nutrition program policies and procedures
• Developing and maintaining good working communication with the AAA for all aspects of the nutrition
program
• Advocating on behalf of older adults with community members, governing agencies, and policy makers as
well as local, state, and federal legislators and lawmakers
• Attending public hearings and meetings relating to legislative proposals for older adults as directed by the
aging unit
• Developing and maintaining a good public relations program, including outreach via public appearances and
local newspapers, radio, and other media
• Obtaining input from older adult participants regarding service delivery, including listening and responding
to concerns

64
P-03062-38 (04/2024)
• Maintaining, informing, and seeking advice from the nutrition advisory council and ensuring that the
members of the council are active in advocating for and promoting the program, as well as assisting with
decisions that affect service delivery
• Recruiting, screening, interviewing, hiring, training, and supervising all part-time and full-time personnel
affiliated with the nutrition program
• Recruiting, training, and recognizing volunteers for the nutrition program
• Preparing contract applications, job descriptions, bid specifications and proposals, and budget proposals in a
timely and proper manner, as directed
• Contracting for provision of food stuffs, food service equipment, supplies, and facilities according to the
procurement procedures of the designated authority and as described in this manual
• Developing and provide training programs for nutrition program staff and volunteers
• Participating in the planning of and ensure all appropriate staff and volunteers attend regional annual
nutrition program staff and volunteer training
• Ensuring the ongoing practice of safe food handling by developing and enforcing local procedures related to
food safety and sanitation and by ensuring all training and certification requirements
are met by nutrition
staff and volunteers
• Ensuring that all required registration, screening, and assessments for nutrition program participants are
completed
• Developing fiscal procedures for the nutrition program
• Maintaining all accounts and records required by the nutrition program
• Compiling, organizing, and preparing reports and materials for the aging unit and other key agencies as
directed (this includes the county or Tribal aging unit, the AAA, and BADR)
• Coordinating access to other aging services for at-risk participants
• Implementing auditing controls to continuously measure program effectiveness and costs
• Monitoring each dining center annually to evaluate the provision of nutrition services.
• Identifying program problems and recommend remedial measures
• Carrying out all other duties and activities of this position as assigned to the holder of this position

65
P-03062-38 (04/2024)
If a county or Tribal aging unit is unable to hire a full-time nutrition director or employ a full-time equivalent
for a nutrition director, the aging unit must submit a waiver request to the AAA that clearly demonstrates that
the size of the program or other conditions indicate that a part-time position is adequate. Waivers will be
documented and re-evaluated by the AAA once every aging plan cycle.
c. Nutrition program dining center managers
All congregate dining centers and locations where carryout meals are distributed to participants must be
supervised by a designated dining center manager.
The dining center manager, under the supervision of the nutrition program director, actively supervises the safe
and sanitary service of congregate and carryout meals and all other related nutrition program activities. The
dining center manager will ensure that the following tasks are accomplished:
• Greeting participants
• Providing continual outreach to new participants
• Obtaining feedback and responding to concerns from participants regarding service delivery
• Advocating on behalf of older adults with community members as well as local, state, and federal
lawmakers and policy makers
• Verifying that participants have registered
• Handling all participant contributions appropriately
• Enforcing policies and procedures related to food safety and sanitation
• Providing quality assurance for food or for food-vendor contracts
• Keeping records of program data
• Scheduling and/or supervising other staff or volunteers
• Ensuring safety of meal service locations through collaboration with facility owners and local regulatory
agencies
• Attending annual regional nutrition program staff training

66
P-03062-38 (04/2024)
Important skills and qualities to consider when hiring dining center managers include customer service skills,
food-handling experience, first-aid certification, group leadership experience, problem-solving abilities, and a
warm, non-judgmental personality.
d. Nutrition program nutritionist
Section 339 of the OAA requires that meal providers solicit the expertise of a dietitian or other individual with
equivalent education and training in nutrition science.
Each AAA and aging unit must employ or retain the services of a qualified dietitian or nutritionist who is
responsible to the nutrition director. If the program nutritionist is subcontracted, the program nutritionist’s tasks
should be specified in the service contract
.
ACL’s Nutrition and Aging Resource Center states that, at a minimum, the program nutritionist can provide
advice on how to:
• Implement the nutrition standards and requirements.
• Ensure adherence to the nutrition standards and requirements by reviewing and approving menus offered to
program participants and routinely monitoring meals offered.
• Develop food service contracts, contracts with food suppliers, and/or contracts with food service
management companies.
• Assist in food service and food safety management.
• Assist in quality and quantity meal production by working with program staff regarding food preparation
techniques and portioning of menu items.
• Plan to meet nutrition needs of older adults in both non-emergency and emergency situations.
• Address issues of hunger, food insecurity, malnutrition, health promotion, and chronic disease management
in older adults through involvement in nutrition screening
processes or referrals to additional nutrition
services for high-risk participants.

67
P-03062-38 (04/2024)
• Meet requirements for nutrition education by overseeing nutrition education programs and curriculum
offered.
• Meet requirements for nutrition counseling by coordinating and/or providing nutrition counseling services.
(1) Program nutritionist qualifications
In Wisconsin’s nutrition program, a "dietitian or other individual with equivalent education and training in
nutrition science" will have one or more of the following qualifications:
• Certified Dietitian
Certified Dietitians (CD) hold a current certification with the
Wisconsin Department of Safety and
Professional Services and are certified as a dietitian under the Wisconsin State Statutes (2015),
Chapter 448, "Medical Practices," Subchapter V, Dietitians Affiliated Credentialing Board. Verification
of certification can be done online at the Wisconsin Department of Safety and Professional Service’s
website.
• Registered Dietitian or Registered Dietitian Nutritionist
Registered Dietitians (RD) or Registered Dietitian Nutritionists (RDN) hold a current registration with
the Commission on Dietetic Registration
. To verify whether or not someone is a registered dietitian,
contact the Commission on Dietetic Registration of the Academy of Nutrition and Dietetics.
• Nutrition and Dietetics Technician, Registered or Dietetic Technician, Registered
Nutrition and Dietetics Technicians, Registered (NDTR) or Dietetic Technicians, Registered (DTR) hold
a current dietetic technician registration with the Commission on Dietetic Registration
. To verify
whether or not someone is a NDTR or DTR, contact the Commission on Dietetic Registration of the
Academy of Nutrition and Dietetics.

68
P-03062-38 (04/2024)
• Comparable education, experience, and authorization
Per section 339 of the OAA, if a dietitian or other individual with equivalent education and training in
nutrition science is not available, an individual with comparable expertise in the planning of nutritional
services may be acceptable with authorization from the AAA dietitian or the BADR nutrition
coordinator. Those not likely to receive approval include nurses, dietary managers, dietary supervisors,
and cooks unless they can prove an extensive, well-rounded education and experience in the major areas
of dietetic practice.
e. Other required staff capacity
In addition to staff requirements listed above, each aging unit will have accounting and clerical capacity
sufficient to fulfill the nutrition program's budgetary, fiscal, reporting, and record-keeping responsibilities.
f. Volunteers
To the extent feasible, the nutrition program will provide opportunities for voluntary participation of individuals
in all aspects of program operations.
g. Background checks for HDM drivers
To help ensure the safety of HDM participants, nutrition programs must conduct a background check for each
paid and volunteer HDM driver. At a minimum, paid nutrition program staff must conduct a search on the
Wisconsin Circuit Court Access (WCCA) website and the U.S. Department of Justice National Sex Offender
Public Website (NSOPW). Both searches can be conducted free of charge. If such searches reveal a concern,
nutrition programs must conduct a name-based background check through the Wisconsin Department of Justice
Crime Information Bureau’s Centralized Criminal History (CCH) database. There is a cost associated with this
background check.

69
P-03062-38 (04/2024)
If local policies for conducting background checks are stricter, such as requiring CCH checks on all paid and
volunteer drivers, such policies and procedures should be followed.
A nutrition program may refuse to hire an individual or refuse to allow an individual to volunteer based on a
conviction only if the circumstances of the conviction substantially relate to the requirements of the HDM
driver position and present a concern for the safety of HDM recipients.
2. Nutrition advisory council
Section 339(2)(G) of the OAA requires that meal providers solicit the advice and expertise of meal participants and
other individuals knowledgeable about the needs of older individuals. The nutrition program of each aging unit will
establish a nutrition advisory council that is separate from any other advisory group of the aging unit to assist in
evaluating, promoting, planning, and advocating for the nutrition program and its participants (see “Requirements
for the ADRC Board and Commission on Aging” section of Governing Boards, Commissions, and Committees
chapter of this manual). The nutrition advisory council will advise the nutrition director on all matters relating to
nutrition and nutrition-supportive services within the program area. All recommendations and suggestions of the
council will be in accord with federal and state policies and will take into consideration the nutrition budget.
a. Council roles and responsibilities
Council members will:
• Represent and speak on behalf of the nutrition participants and program.
• Advocate on behalf of older adults with community members, governing agencies, and policy makers, as
well as local, state, and federal legislators and lawmakers.
• Assist in publicizing the nutrition program and reaching out to potential new participants.
• Make recommendations to the nutrition director and the aging unit about locations, days, and hours of
dining center operations.
• Make recommendations to the nutrition director about dining center accessibility and age-friendliness.

70
P-03062-38 (04/2024)
• Advise and make recommendations to the nutrition director and aging unit about supportive social services
to be conducted at dining centers.
• Give support and assistance to the ongoing development of the nutrition program.
• Seek input, in cooperation with the nutrition director, from program participants and others in the
community to evaluate the impact, value, and quality of the nutrition program.
The intent of the nutrition advisory council is to function as a partner in improving the nutrition program.
Council members can assist in securing funding by volunteering their time to raise funds for the program,
developing and maintaining community partnerships, and promoting activities including advertising and
outreach to the community.
b. Membership and structure
More than one-half of the council membership will consist of adults aged 60 and older. The remaining council
membership should include broad representation from caregivers, community leaders, and public and private
agencies that are knowledgeable and interested in the senior dining and HDM programs, such as local hospitals
or University of Wisconsin-Extension.
c. Meetings
The council will meet as often as is necessary, but no less than quarterly. Meetings must be open, with notices
posted in accordance with the Open Meetings Law
. Minutes for all nutrition advisory council meetings will be
kept in accordance with nutrition program recordkeeping requirements.
3. Facilities
The nutrition program, nutrition advisory council, and commission on aging will jointly plan for establishing,
remodeling, or closing of facilities, such as dining centers, central or on-site kitchens, and other food preparation or
distribution facilities.

71
P-03062-38 (04/2024)
Aging units and providers will include the AAA in the planning process and obtain timely approval from the AAA
prior to instituting changes.
Nutrition programs will consider the following:
• The cost of providing meals
• How changes will affect service to participants
• The costs involved in establishing, remodeling, or relocating a facility
• Public input from interested parties, especially older adult citizens
a. Dining centers
The facility will comply with all applicable state and local health, fire, safety, and sanitation regulations. When
determining the appropriateness of a dining center, nutrition programs will consider, at a minimum:
• Available parking.
• Ease of entry and adequate emergency exits.
• Appropriate design and placement of tables, chairs, and equipment.
• Size and scope of restrooms, stairs, elevators, and/or ramps.
• Availability of fire extinguishers and other fire suppression systems.
• Adequacy of heating and cooling systems.
(1) Location
Dining centers must be in a facility where eligible individuals will feel free to attend. The dining center
must be free of architectural barriers that limit the participation of older adults and be compliant with
accessibility standards set forth by the Americans with Disabilities Act (ADA). Nutrition staff will make
efforts to promote an inclusive environment and reduce or eliminate barriers to participation for all older
adults, both physical and otherwise.

72
P-03062-38 (04/2024)
(a) Senior or community centers
Dining centers located in senior or community centers must be open to the public so that older adults,
regardless of residency or membership, are welcome to attend. Nutrition programs and senior or
community centers will establish procedures that ensure coordination between the nutrition program and
the center. Written grievance procedures will be established to address potential conflicts between the
nutrition program and center staff or volunteers. Job descriptions, organizational charts, or other written
material necessary for identifying program responsibilities and relationships will be developed.
(b) Communities of faith
Dining centers located in buildings used for worship by communities of faith must be open to the public
so that older adults, regardless of whether they are members of the community of faith, are welcome to
attend.
(c) Housing facilities
For a dining center to be located within public or private housing facilities, most residents of such
facilities must be age 60 or older. Such dining centers must be open to the public so that older adults,
regardless of whether they reside in the housing facility, are welcome to attend.
The nutrition program and the facility will establish procedures that ensure coordination between the
nutrition program, the housing facility, and its residents. Written grievance procedures will be
established to address potential conflicts between the nutrition program and the housing facility or its
residents.
(d) Restaurants
When considering a restaurant-based dining center, the nutrition program is responsible for ensuring that
the restaurant:

73
P-03062-38 (04/2024)
• Follows the Wisconsin Food Code and is licensed and inspected regularly by the local public health
department.
• Provides meals to program participants that meet nutrition program standards for meals.
• Meets accessibility requirements.
• Has appropriate emergency preparedness procedures that can accommodate an older adult
population.
A nutrition program representative must be present on site as a designated dining center manager during
mealtimes. The dining center manager serves as a connection to and point of contact for the aging unit
and its services, as well as performs the general responsibilities of
nutrition program dining center
managers and ensures that the restaurant does not make unapproved substitutions for menu items.
Restaurant staff are not permitted to function as dining center managers.
The restaurant may plan menus and food item choices, but the nutrition program’s program nutritionist
and nutrition director must approve menus and/or food choices available to program participants before
they are offered. Procedures must be in place for:
• Communicating and approving menus, menu changes, and substitutions between the restaurant and
the nutrition program.
• Explaining and advertising menus and/or food choices to participants in a clear manner.
• Communicating to participants that they may purchase additional beverages and food at an
additional cost.
Programs contemplating a new restaurant dining center should contact the AAA and/or BADR for
technical assistance.
74
P-03062-38 (04/2024)
b. Facility agreement
Before entering into an agreement with a facility, the nutrition director will conduct an on-site visit to determine
that nutrition program requirements can be met.
Each program will have written agreements with the owners of all facilities used as dining centers, including
those donated for use at no cost. The agreements will specify who is responsible for the following, if applicable:
• Care and maintenance of the facility, specifically including kitchen, equipment, restrooms, and other areas
of common use
• Utility costs
• Safety inspections
• Licensing by the public health department
• Insurance coverage
• Security procedures
• Emergency preparedness and evacuation procedures
• Snow and ice removal
Note that this list is not all-inclusive. Nutrition programs may add additional items to agreements as necessary.
A copy of the written agreement will be provided to the AAA upon request.
(1) Agreements with restaurants
The nutrition program and the restaurant must have a written agreement that addresses the following in
addition to the requirements of contracts with meal providers and nutrition program facilities
:
• A price per meal that the nutrition program pays the restaurant and whether tips for service staff are
included.

75
P-03062-38 (04/2024)
• Statements of compliance with Wisconsin Food Code and nutrition program requirements, such as
training requirements for food service establishment staff and public health licensing and inspections.
c. Facility changes
AAAs must be notified, and in some cases provide written approval, in advance for changes related to nutrition
program facilities. The AAA will notify BADR in writing of all dining center facility change approvals. Aging
units and providers must include AAAs early in the planning process as facility changes are considered.
The following table shows reporting and approval requirements for facility changes.
Facility change
Written requests
for AAA approval
required
Required
timeframe for
approval or
notification
Change required
in aging plan
Notification to
program
participants
required
New dining center Yes
60 days prior to
opening
Yes Yes
Relocation Yes
60 days prior to
relocation
Yes
Yes, at least 30
days prior to
relocation
Permanent closure Yes
60 days prior to
closure
No
Yes, at least 30
days prior to last
day of meal service
Permanent change
to days of service
Yes
60 days prior to
change
No Yes

76
P-03062-38 (04/2024)
Facility change
Written requests
for AAA approval
required
Required
timeframe for
approval or
notification
Change required
in aging plan
Notification to
program
participants
required
Temporary closure
(longer than one
week)
No, but written
notification is
required
When the program
becomes aware of
the need to close
temporarily
No Yes
Temporary change
to days of service
(longer than one
week)
No, but written
notification is
required
When the program
becomes aware of
the need to close
temporarily
No Yes
(1) New dining centers
Requests for approval will include:
• The need for the change.
• Proof that the program has sufficient resources necessary to support the change.
• Written approval by the local commission on aging and the local advisory council.
(2) Permanent closure of dining centers
Requests for approval will include:
• The reasons for the dining center closure, such as lack of attendance, inability to meet minimum
standards and/or other requirements, loss of resources, or other justifiable reasons.

77
P-03062-38 (04/2024)
• Details about the communities that will be affected, including the level of socioeconomic need and
identification within OAA target populations.
• Written approval by the local commission on aging and the local advisory council.
The AAA will review the rationale and determine that all options have been exhausted for keeping the
dining center open or for relocating it. If there remains a need for service in the area, efforts should be made
to develop a new dining center and/or provide support for participants to attend another existing dining
center.
(3) Temporary closure of dining centers
Notifications will include:
• Specification of the affected days.
• An explanation of how the program will meet participants' nutritional needs during the closure.
4. Liability insurance
Each nutrition program will carry liability insurance sufficient to cover its operation. Programs should seek
guidance from their agency's legal staff or corporation council.
C. Supervision
1. Students working in the program
When dietetic or nutrition students perform activities of the program nutritionist, they will be supervised by a
qualified nutritionist through regular evaluation, either on site or after extensive training and orientation.
78
P-03062-38 (04/2024)
2. Aging unit and provider monitoring responsibilities
Aging units and OAA service providers will conduct and document on-site monitoring visits of each congregate
dining center at least annually and an on-site review of the HDM packaging and delivery process at least annually.
3. AAA monitoring responsibilities
AAAs are responsible for monitoring the programmatic and fiscal performance of the nutrition program, its aging
units or providers of nutrition services, and their OAA activities for quality and effectiveness. A full monitoring
review of each nutrition service provider must be conducted at least once every plan cycle and will include an on-
site visit of a congregate dining center and an on-site review of the HDM packaging and delivery process.
Monitoring of other aspects of the program may be done virtually or as a desk review.
D. Allowable funding source(s) and expenses
1. Funding sources
The nutrition program is funded by
a combination of federal and state funds, local public and private funds, and
participant contributions.
a. OAA Title III-A or Nutrition Services Incentive Program (NSIP)
Per section 311 of the OAA, NSIP provides additional grant funding to states, territories, and eligible Tribal
organizations to use exclusively to purchase domestically produced food for elder nutrition program congregate
meals and HDMs.

79
P-03062-38 (04/2024)
b. OAA Title III-B
Title III-B funds may be used to fund nutrition services such as nutrition education, nutrition counseling, and
provision and/or delivery of food and nutritional supplements.
c. OAA Title III-C1
Title III-C1 funds may be used to provide congregate meals, nutrition education, nutrition counseling, and other
nutrition services approved in advance by BADR.
d. OAA Title III-C2
Title III-C2 funds may be used to provide HDMs (including carryout meals), nutrition education, nutrition
counseling, and other nutrition services approved in advance by BADR. Title III-C2 funds may be used to
purchase grocery food items for grocery delivery, but C2 funds may not be used to fund the cost of delivering
grocery items, which is a service funded by Title III-B.
(1) Transfers of Federal OAA funds
BADR may elect to request transfers of federal OAA funds between Title III-B, Title III-C1, and
Title III-C2 from ACL on behalf of AAAs.
e. State general purpose revenue (GPR)
DHS provides state funding for HDM programs and a supplement to the federal congregate meal program funds
that promotes expansion of senior dining programs throughout the state. DHS allocates state funds for both
congregate and HDMs based on the intra-state funding formulas developed by DHS and approved by ACL
under the state aging plan.

80
P-03062-38 (04/2024)
f. State Senior Community Services program
Agencies may choose to use the state-funded Senior Community Services Program funds for nutrition program
services.
g. Local funding
Local funds contributed to the nutrition program from local public or private governments, agencies, or
organizations can be used for the required match. Local fund expenditures used for match must follow rules of
the program and service for which they were contributed.
Local funding may include the following sources:
• Endowments made from community foundations to the nutrition program
• Donations or gifts from local civic groups, businesses, community members, or other organizations to
support nutrition program operations
• Revenue generated from the sales of meals or other nutrition services to other organizations through
contracts
• Proceeds from organized fundraising activities to support nutrition program services
h. Program income
Program income is defined as gross income earned by the grantee and all sub-grantees that is directly generated
by or earned because of nutrition program services that are wholly or partially supported by the OAA. Program
income is used to expand the service for which the program income was generated. Contributions will be
handled in accordance with federal and state policy.

81
P-03062-38 (04/2024)
(1) Voluntary contributions
Section 315 of the OAA prohibits cost sharing for congregate and HDM services, and Wisconsin does not
permit cost sharing for other nutrition services. Agencies will not means-test for any service or deny
services to any individual who does not contribute toward the cost of the service. There will be no cost-
share requirement or fee charged to nutrition program participants. Participants must be given the
opportunity to voluntarily contribute toward the cost of services provided (see “Voluntary Contributions”
section of Aging Service Delivery
chapter of this manual).
Per Section 315 of the OAA, AAAs will consult with aging units, service providers, and older adults in the
AAA’s planning and service area to determine the best method for accepting voluntary contributions for
nutrition services.
Nutrition programs will provide participants with written information related to voluntary contributions.
Each congregate dining center and carryout distribution location will provide written information related to
voluntary contributions at the point of service, and HDM participants will receive such written information
upon registering and annually thereafter. Information should be in large print and will include:
• The suggested contribution (if applicable).
• Total meal cost
.
• A statement about the sources of funds used for programs.
• The stipulation that no eligible participant will be denied a meal based on ability to contribute toward
the cost of the meal.
(2) Contribution letters
If contribution letters are used for the senior dining or HDM program, all letters must include the following
unaltered sentences to ensure consistency of messaging around contributions to program participants (see
“Contribution Letters” section of Aging Service Delivery
chapter of this manual).

82
P-03062-38 (04/2024)
We are required to provide you the opportunity to contribute to the cost of this service. The actual
cost to our agency to provide this meal is $[per-meal cost]/meal. Contributions to help offset the cost
of meals are essential to maintaining nutrition services for our community’s older adults.
Contributions from participants, their families, and others directly fund the meals we provide and
are combined with federal, state, and local funds to provide this service.
Please contribute what your budget allows. You will not be denied a meal if you are unable to
contribute. We are committed to protecting the privacy of your contributions.
(3) Ticket systems
Programs may institute a system of issuing tickets for nutrition services provided by the aging unit or
provider (see “Ticket systems” section of Aging Service Delivery
chapter of this manual).
(4) Revenue from fee-for-service private-pay systems
Per section 212 of the OAA, any amount of payment to an agency under an agreement for a fee-for-service
private-pay system that exceeds reimbursement of the agency’s costs must be used to provide, or support the
provision of, services under the OAA (see “Fee-for-service private-pay system” section of
Aging Service
Delivery chapter of this manual).
2. USDA Supplemental Nutrition Assistance Program (SNAP)/FoodShare Wisconsin
Nutrition programs may apply to accept FoodShare benefits as a voluntary contribution from participants.
3. Meal cost analysis
Calculating total meal cost is essential to good food service management. This information is important for
determining a suggested per-meal contribution and for informing participants of the total cost of a meal.

83
P-03062-38 (04/2024)
If the nutrition program provides meals through fee-for-service private-pay systems or to non-eligible participants,
such as community-based long-term care (or Medicaid waiver) program recipients, visitors, daycare programs,
Head Start, or jails, the nutrition program must document a total-meal-cost analysis of the Title III resources used
for preparing the meals; this way the nutrition program may be reimbursed for meals purchased (see “Fee-for-
service private-pay system” section of Aging Service Delivery
chapter of this manual).
Any OAA funds used by the aging unit or provider to pay part or all of a cost incurred in developing and providing
a private pay meal must be recovered by the aging unit or provider, and fair market rates must be charged to
individuals or entities purchasing services. AAAs, aging units, or service providers will implement systems for
private pay meals in accordance with federal and state policies related to documentation of all costs incurred, funds
spent and reimbursed, and net proceeds. Per section 212 (e) of the OAA, “the term ‘cost’ means an expense,
including an administrative expense, incurred by a [AAA, aging unit, or provider] in developing or providing [a
meal] … whether the [AAA, aging unit, or provider] contributed funds, staff time, or other plant, equipment, or
services to meet the expense.”
a. Total meal cost calculation
Each program must calculate the total meal cost at least annually, using the required meal cost tool developed
by BADR (see “Meal Cost Tool” section of Elder Nutrition Program SharePoint page
), although it is
recommended that this tool is used every six months to analyze costs to produce a meal. This calculation should
be completed each year when complete financial information from the previous calendar year is available,
typically in late spring or summer.
E. Policy requirements

84
P-03062-38 (04/2024)
1. Grievance and complaint procedures
The program will have a written grievance procedure to provide a means to address significant participant
complaints. All program participants will be made aware of the grievance procedure. The procedure will include
who to contact in the agency to handle the grievance and the procedures that the agency will follow.
Section 306 of the OAA requires AAAs to provide a grievance procedure to older adults who are dissatisfied with
or denied services under Title III of the OAA, including nutrition services.
2. Codes of conduct and behavioral policies
Aging units and service providers, whether they are stand-alone or integrated with the ADRC, are required to
establish a code of conduct and behavioral policy for participants of OAA programs.
3. Procurement
Procurement is the process of buying services or property. In the nutrition program, services or property purchased
may include food, equipment, supplies, or subcontracts with caterers, restaurants, nutrition educators, program
nutritionists, or outreach workers. Nutrition programs are responsible for developing procurement and purchasing
procedures that comply with federal, state, and local laws, regulations, and standards.
Section 339 of the OAA encourages nutrition programs to identify potential partnerships and contracts with local
producers and providers of locally grown foods to support meals that include such foods where feasible; therefore,
nutrition programs should provide preference to local producers and providers in procurement processes.
85
P-03062-38 (04/2024)
b. Contracts and agreements
When nutrition programs purchase meals, services, space, or equipment, all contracts will be in compliance
with federal, state, and local procurement standards, including policies described in
the Contract Administration
chapter of this manual. Nutrition programs will submit contracts to the AAA or BADR for review upon request.
Contracts should contain all applicable general contract elements in addition to other elements described in this
chapter.
(1) Contracts with meal providers
A written contract must be established when a nutrition program contracts with a private company to
provide meals. In this case, the meal provider provides only meals and does not manage any aspect of the
nutrition program.
Meal provider contracts may be obtained only with vendors who supply meals from premises which have a
valid permit, license, or certificate issued by the regulatory authority. The service provider will comply with
all state and local laws, ordinances, and codes for establishments which prepare, handle, and serve food to
consumers, either on the premises or elsewhere.
Section 339 of the OAA encourages aging units and providers to engage in contracts that limit the amount
of time meals must spend in transit before they are consumed. Before entering into an agreement with a
prospective meal provider, the nutrition director will conduct an on-site visit of the meal provider’s facilities
to determine that nutrition program requirements can be met, and appropriate food safety and sanitation
practices are in place.
Nutrition programs are responsible for quality assurance monitoring of contracts. For example, part of
contract monitoring quality assurance should include comparing the menus and the details of the nutrient
analysis with what foods and serving sizes are provided by the meal provider.

86
P-03062-38 (04/2024)
(2) Agreements between nutrition programs
Nutrition programs may contract with another nutrition program to provide meals without undergoing a
competitive procurement process, but nutrition programs are encouraged to compare pricing.
When nutrition programs purchase meals or services from another nutrition program, there will be a written
contract between the two programs, which must be signed by authorized representatives of both parties
before the date the service is to start.
When entering into an agreement, the following should be considered, especially if a program is providing
additional services beyond provision of food:
• Which program is providing the meals?
• What will the price per meal be?
• If HDMs are being provided, which program is doing HDM screening and/or determination of
eligibility?
• Which program is delivering meals?
• Which program is counting meals for NSIP and NAPIS reporting?
• Which program is collecting voluntary contributions from the participants?
4. Gift certificates
Nutrition programs can sell gift certificates for meals. As long as the participant using the gift certificate is
registered and eligible
for services, the certificate can be sold on a voluntary contribution basis. Gift certificates for
use by non-eligible individuals must be sold for the total meal cost.
5. Reducing food waste: second helpings and leftovers
Each program will implement procedures designed to minimize food waste. At a minimum, programs will:

87
P-03062-38 (04/2024)
• Evaluate and minimize the difference between the number of meals prepared or received from the vendor and
the number of meals served.
• Review portion control methods with the staff and, when applicable, the food provider, to ensure that all
participants are receiving equivalent amounts of food and to reduce the amount of leftover food.
• Offer second helpings to participants at dining centers when feasible. Offer second helpings to participants in a
fair manner.
• Educate participants on safe food-handling practices. The safety of food, after it has been served to a participant
and when it has been removed from the dining center, is the responsibility of the participant.
• Provide participants with only new, unused containers for taking home uneaten food
, if the nutrition program
chooses to provide containers.
When feasible, leftover food from on-site cooking facilities may be incorporated into subsequent senior dining or
HDMs, if cooled and handled according to the Wisconsin Food Code
guidelines. This includes re-serving leftovers
as individual frozen meals. Programs that use this option will have a written procedure and documentation, such as
temperature logs, which show that food can be frozen safely within the proper timeframes.
6. Prayer at dining centers
Each participant has a free choice whether to pray, either silently or audibly. The prayer or other religious activity
is not to be officially sponsored, led, or organized by people administering the nutrition program or dining centers,
including program volunteers while they are volunteering.
F. Training and certification requirements
1. Nutrition program director training
All nutrition directors will be oriented and trained to perform their assigned responsibilities and tasks. AAAs and/or
BADR will provide orientation to nutrition directors.

88
P-03062-38 (04/2024)
Nutrition directors must receive a minimum of 10 hours of training annually. Training hours can be obtained
through:
• Regional nutrition director trainings or meetings.
• Wisconsin Association of Nutrition Directors conferences.
• Attendance at the regional planning committee meetings for annual nutrition program staff and volunteer
training (one hour maximum).
• Attendance at the annual nutrition program staff and volunteer training (one hour maximum).
• Attendance at other trainings, conferences, or webinars approved by the AAA and/or BADR.
2. Nutrition program staff and volunteer training
All other staff, paid and volunteer, will be oriented and trained to perform their assigned responsibilities and tasks.
All paid staff must receive a minimum of six hours of training annually. Nutrition program volunteers who serve as
dining center or kitchen managers must also receive a minimum of six hours of training annually. Training hours
can be obtained through:
• Attendance at locally held nutrition program meetings and trainings for staff and/or volunteers (one hour
maximum from each). Nutrition directors are strongly encouraged to hold quarterly meetings and/or trainings
with dining center managers.
• Attendance at the annual nutrition program staff and volunteer training (four hours maximum). This is
coordinated by BADR, the AAAs, and regional planning committees, and is usually held each year in the fall.
A minimum number of annual training hours is not required for all other nutrition program volunteers. However,
orientation and training must be provided by the nutrition program and will include all applicable mandatory topics,
along with any other training appropriate for the task(s) for which the volunteer is responsible (see “Training”
section of Elder Nutrition Program SharePoint page
). Those who volunteer or have direct contact with food are held
to the same standards (for example, sanitation standards) that apply to “regular” employees.

89
P-03062-38 (04/2024)
All paid staff and regular nutrition program volunteers, unless otherwise noted, will receive training on mandatory
topics at least once during the three-year aging plan period. Contact BADR or the AAAs for recommendations on
available training. BADR and/or the AAA may define additional mandatory topics as necessary.
At the discretion of the nutrition director, other topics that are deemed valuable may be presented to staff and
volunteers and may count towards the required training hours. Additional topics will be provided based on the tasks
for which a staff member or volunteer is responsible. Additional topics must be relevant and useful by the nutrition
program to enrich and further the training and professionalism of its staff and volunteers to better serve the older
adults in their communities. Additional topics will only be allowed if the mandatory training topics are all
completed.
a. Annual regional staff and volunteer training
All nutrition directors are expected to participate on a regional planning committee for annual nutrition staff and
volunteer trainings. Nutrition directors are also expected to ensure that all regular dining center managers attend
a regional training.
3. Required food safety and sanitation training
This section describes food safety and sanitation requirements for nutrition directors and staff.
a. New staff and volunteer orientation
All new staff and volunteers that have contact with food must have a general orientation on safe food handling
and sanitation practices, outlined in this operations manual and the Wisconsin Food Code
, on or before their
first day of work.

90
P-03062-38 (04/2024)
b. Wisconsin food protection manager certification
In order to comply with section 2-102.11 of the Wisconsin Food Code and Wis. Stat. § 97.33 (1r), Wisconsin
food protection manager certification is required for:
• Nutrition program directors.
• All lead and substitute cooks at a central kitchen or on-site cooking senior dining center in which nutrition
program meals are prepared and/or cooked.
It is recommended that at least one staff person or volunteer who is a Certified Food Protection Manager
(CFPM) be on duty at a location where food is stored, packaged, or served to consumers to align with the
requirements in section 2-102.11 of the Wisconsin Food Code and Wis. Stat. § 97.33 (1r).
The nutrition director will obtain training and pass the applicable exam within 90 days of beginning the
nutrition director position. Lead and substitute cooks will obtain training and pass the applicable exam within
90 days of beginning the food-handling position.
The AAA may grant an extension of the 90-day period up to 180 days when any of the following applies:
location and/or travel issues, timing of available courses, or significant personal scheduling issues. However,
the nutrition director is responsible for requesting the extension before the end of the 90-day period.
(1) Obtaining CFPM certification
The Wisconsin Department of Agriculture, Trade and Consumer Protection (DATCP), Division of Food and
Recreational Safety, approves courses that meet the criteria for the CFPM certification. A comprehensive
list of approved courses (such as ServSafe) and Wisconsin course providers are available on the
DATCP
Food Manager Requirements webpage. Courses are typically available through BADR, the AAAs, technical
colleges, and individual consultants, among others.
To obtain or renew a CFPM certification, a nutrition program staff person or volunteer must:
91
P-03062-38 (04/2024)
• Complete a state-approved certification course.
• Take and pass a state-approved certification exam.
(2) Renewing CFPM certification
All CFPM certifications expire five years from the date of issuance. There are two available renewal
options:
(a) If the nutrition program retains five or more staff or volunteer food handlers where meals are
being prepared and/or cooked
Staff or volunteers must take a state-approved CFPM course and pass an approved exam to maintain
their certification. Recertification courses are not accepted. A comprehensive list of approved courses
(such as ServSafe) and Wisconsin course providers are available on the
DATCP Food Manager
Requirements webpage.
Note: A “food handler” is defined by DATCP as anyone who handles or assembles food in a food
establishment. Examples include chefs, line cooks, and servers who assemble food or package HDMs.
Processing of food includes canning, extracting, fermenting, distilling, pickling, freezing, baking,
drying, smoking, grinding, cutting, mixing, coating, stuffing, packing, bottling, packaging, or any other
treatment or preservation process. Other examples include chopping, dicing, cooking, cooling, reheating,
and assembling salads.
(b) If the nutrition program retains less than five staff or volunteer food handlers where meals are
being prepared and/or cooked
Staff or volunteers may take a state-approved food safety training for small operators
, without an
examination, in lieu of the CFPM course and exam. Contact DATCP for a list of approved courses.

92
P-03062-38 (04/2024)
Note that this is not the same license as a CFPM and cannot be used in locations that retain five or more
food handlers. This option also only applies to renewals, not initial certifications. All individuals must
initially obtain a CFPM certification in order to be eligible to choose this renewal option.
Individuals who do not renew in accordance with this section must complete the initial CFPM
certification again. Certifications may not lapse more than 90 days.
c. Serving Safe Food (SSF) certification
The Serving Safe Food (SSF) course and exam were developed by BADR and the Wisconsin Association of
Nutrition Directors (WAND) to meet the food safety and sanitation training requirements for staff, including
senior dining center managers, whose work duties include hot and cold food holding, serving, and clean up, but
no preparation or cooking.
The SSF certification course includes a minimum of two hours of training including a presentation and a take-
home exam. Upon successful completion of the course and passing of the exam, a five-year certificate is issued
by BADR.
The course may be taught by anyone who has a current Wisconsin CFPM certification. Individuals who are
eligible to teach the SSF course must use only the required materials developed and/or reviewed by BADR.
Nutrition programs may use SSF to teach general food safety and sanitation classes or lectures. No alterations to
the materials may be made. If changes are made to any materials, the individual(s) will not be eligible for
certification, unless an exception has been granted by BADR prior to the course taking place.
The required materials used to teach the SSF course can be obtained on the
Elder Nutrition Program SharePoint
site.

93
P-03062-38 (04/2024)
Serving Safe Food certification is required, at a minimum, for dining center managers at senior dining centers
where food is not prepared or cooked. At a minimum, at least one staff person or volunteer with a Serving Safe
Food certification must always be on duty at such locations. It is recommended that other staff working in a
food-handling capacity at such locations also maintain a Serving Safe Food certificate.
Staff and volunteers for whom this policy applies will obtain training and pass the applicable exam within
90 days of beginning the food-handling position. The AAA may grant an extension of the 90-day period up to
180 days when any of the following applies: location and/or travel issues, timing of available courses, or
significant personal scheduling issues. However, the nutrition director is responsible for requesting the
extension before the end of the 90-day period.
Serving Safe Food certification must be renewed every five years by retaking the course and passing the
applicable exam. The course will be completed and the exam submitted to BADR for grading in advance of the
certification’s expiration date.
d. Food allergies
To comply with sections 2-102.11 and 2-103.11 of the Wisconsin Food Code, staff and volunteers of the
nutrition program must be adequately trained in food allergy awareness as it relates to their assigned duties.
G. Reporting requirements
As a state receiving federal OAA funds, BADR is required by ACL to report on the performance of agencies in carrying
out activities designated under the OAA. Agencies are required to comply with all federal and state data collection and
reporting requirements.

94
P-03062-38 (04/2024)
1. Participant registration and screening
a. Registration systems
A participant registration or intake system assists in eligibility determination and ensures the collection of
required program data
. All nutrition program participants are required to meet eligibility requirements and
register before participating in the nutrition program, and at least annually thereafter.
Nutrition program staff are responsible for informing participants about why information is being collected,
how the provision of such information is tied to program funding, how the information will be used, and how
their confidentiality is being protected.
b. Screening
Section 339 of the OAA requires nutrition programs to conduct nutrition screening and assessment. Screening is
the process of identifying individuals who may be at risk for a condition or in need of a service. All participants
receiving services will receive a nutrition screen at least once per year.
(1) DETERMINE Your Nutritional Health screening tool
The federally required screening tool is the "DETERMINE Your Nutritional Health" checklist and is
reported as part of the NAPIS report. Nutrition programs are required to keep the wording of the questions,
the order of the questions, and all scoring and point values the same. People who score six points or higher
meet the screening criteria for “high nutrition risk.”

95
P-03062-38 (04/2024)
(2) Malnutrition Screening Tool
Malnutrition is a physical state of unbalanced nutrition. It can mean undernutrition or overnutrition.
Sections 102 (14) (B) and 330 of the OAA highlight the nutrition program’s purposes to both reduce
malnutrition and assist in access to malnutrition screening. It is also the
position of the Academy of
Nutrition and Dietetics that “based upon current evidence, the Malnutrition Screening Tool should be used
to screen adults for malnutrition.” Therefore, nutrition programs are required to include the Malnutrition
Screening Tool questions as part of registration and screening for congregate, carryout, and HDM services.
Nutrition programs are required to keep the wording of the questions, the order of the questions, and all
scoring and point values the same.
(3) Food insecurity screening tool
Food insecurity exists whenever it’s difficult to access nutritionally adequate, safe, and acceptable food in a
socially acceptable way. To align with section 330 of the OAA, which highlights the nutrition program’s
purpose in reducing hunger and food insecurity, nutrition programs are required to include the
Hunger Vital
Sign™ food insecurity screening tool as part of registration and screening for congregate, carryout, and
HDM services. Nutrition programs are required to keep the wording of the questions, the order of the
questions, and all scoring and point values the same.
Based on their identified needs, nutrition programs will provide program participants at high nutrition risk
with recommendations and referrals to other services or programs. For example, a high-risk participant
might be referred to a program nutritionist, healthcare provider, or dietitian for nutrition counseling, or the
participant might be referred to a local food assistance program. The participant might also be connected
with other aging services, such as in-home personal care or transportation to grocery stores or a congregate
dining center.

96
P-03062-38 (04/2024)
2. Services
a. NSIP qualified meals
BADR submits an annual meal count to ACL, which includes all eligible meals served during the previous
federal fiscal year (FFY), October 1 through September 30. This meal count is used by ACL to calculate NSIP
grants for the next FFY.
Meals must meet the following requirements to be included in the NSIP meal count:
• The meal has been served to a participant who is eligible under the OAA and has not been means-tested for
participation.
• The meal is compliant with the nutrition requirements
.
• The meal is served by an eligible agency.
• The meal is served to an individual who has an opportunity to contribute.
If a meal does not meet all requirements, it cannot be included in the NSIP meal count.
b. Meal forecasting
Programs should maintain an accurate and well-organized system so staff will know how many meals to order
or prepare.

97
P-03062-38 (04/2024)
c. Undeliverable meals and “no-shows”
The program should have a local procedure in place that addresses meals for consistent “no-shows” at senior
dining centers and “undeliverable” HDMs. Programs cannot charge an individual for a meal that is reserved and
not eaten or an undeliverable meal without a clear procedure in place that has been shared with participants, but
the program could ask for a suggested contribution toward these meals. Meals not actually served to a
participant cannot be included in Title III or NSIP meal counts.
3. Recordkeeping
The agency will develop and maintain records in accordance with state policy and program reporting requirements
.
Program records will be retained for a minimum of three years, with the exception of temperature logs, which must
only be retained for one year. Original paper records in which duplicate information has been entered electronically
(for example, paper registration forms) may be discarded after one year.
Nutrition program records and reports will be made available for audit, assessment, or inspection by authorized
representatives of the AAA and/or BADR.
a. Participant confidentiality
The nutrition program will ensure that participant information will be kept confidential according to state policy
(see “Privacy and confidentiality” section of Aging Service Delivery
chapter of this manual).
H. Planning requirements

98
P-03062-38 (04/2024)
1. Participant input
Section 339 (2) (G) of the OAA requires that meal providers solicit input from participants. Section 306 of the
OAA further requires that AAAs must consider the views of nutrition services recipients in their policies and the
development and administration of their area plans
.
A system will be developed to formally assess, at least once per year, the satisfaction of senior dining and HDM
participants for both food quality and delivery of services. This can be accomplished through comment cards,
customer satisfaction surveys, taste tests, or pilot menus.
ACL encourages the use of survey questions that assess program outcomes. Outcome-based survey questions
developed by BADR must be provided to participants no less than once per aging plan cycle. Survey results will be
reported to the AAA and BADR as requested.
2. County and Tribal aging unit plans
County and Tribal aging units are responsible for preparing and developing aging plans every three years that
contain goals related to nutrition program services.
3. Area plans
Per section 306 of the OAA, each AAA designated under section 305 (a) (2) (A) will prepare and develop an area
plan for their planning and service area every three years that will:
• Provide for nutrition services through a comprehensive and coordinated system.
• Determine the extent of need for nutrition services in the area, taking into consideration the number of older
individuals in the planning and service area who are in greatest social and economic need.
• Evaluate the effectiveness of the use of resources in meeting such need.

99
P-03062-38 (04/2024)
I. Emergency preparedness
Nutrition programs need to identify and plan for their roles in natural disasters, pandemics, and other emergencies,
including roles in emergency preparedness planning, response, and recovery. Although nutrition programs are not
emergency service providers, they must be prepared and have the ability to recognize, manage, and respond to
emergencies proficiently (see “Requirements for Recognizing and Responding to Emergencies” section of the
Emergency Preparedness
chapter of this manual).
Nutrition services should be considered essential. Therefore, each program will develop and have available written plans
that promote the continuity of operations in emergency situations. Note that plans should be flexible rather than
prescriptive, as it is impossible to anticipate all emergencies. Plans should focus on identifying possible methods of
communication, opportunities for collaboration, and options available for diversion or adjustment of service in various
situations.
Nutrition directors are responsible for communicating such plans regularly with staff and volunteers so that staff and
volunteers know their roles in emergency preparedness and response. Plans will also include processes for training staff
and volunteers based on their roles.
1. Recognizing and responding to participant emergencies
Nutrition program staff need to be trained on how to identify a participant that might be experiencing an emergency
(see “Recognizing and Responding to Customer Emergencies” section of the Emergency Preparedness
chapter of
this manual). In a congregate dining center, this might be a medical emergency such as a heart attack or stroke, or it
could be another type of emergency such as suicidal ideation or violence. On an HDM route, in addition to the
examples that might be observed in a congregate dining center, drivers may identify other emergencies such as
those related to the home environment (for example, the smell of natural gas, smoke, lack of heat or air
conditioning, and other safety issues).

100
P-03062-38 (04/2024)
When an emergency is identified, staff and volunteers should follow protocols for participant emergencies outlined
in the nutrition program’s emergency preparedness plan, such as contacting the aging unit or service provider, the
participant’s identified emergency contact(s), adult protective services
, and/or 911.
2. Community-level emergency and disaster preparedness and response
Nutrition programs need to identify and plan for what their role will be in the case of a community-level emergency
(see “Community-Level Emergency and Disaster Preparedness and Response” section of the
Emergency
Preparedness chapter of this manual). Community-level emergencies might include emergencies affecting
community dining centers or HDM routes, such as fires, explosions, power outages, floods, or sewer back-ups.
Community-level emergencies might also include more widespread emergencies, such as natural disasters or
pandemics. Nutrition programs should proactively engage in planning activities to prevent or minimize disruption
of services. If services are halted because of an emergency, programs will do the following:
• Contact participants, either directly or through an automated service.
• Implement procedures for checking on the well-being of participants, particularly if services will be suspended
for multiple days.
• Distribute information to participants on how to stock an emergency food shelf.
a. Emergencies involving dining centers and HDM routes
Each program will ensure that preparation has taken place at each location where nutrition services are being
provided (for example, dining centers, HDM distribution locations, kitchens, and locations where nutrition
education or counseling services are provided) for procedures to be followed in case of an emergency. In
addition, staff and volunteers delivering meals will be trained in methods of handling emergencies.
Emergency information and resources will be readily available at locations where services are offered,
including home-delivery vehicles. Tests of alarms, emergency-related equipment, participant notification
procedures, and/or evacuation procedures will be conducted at least annually.

101
P-03062-38 (04/2024)
b. Widespread community emergencies
Nutrition programs will participate in the service area response to disasters as requested and appropriate.
Response may include collaboration with local emergency management, public health, or
other programs and
organizations.
Nutrition programs will plan for community-level emergencies by (as applicable):
• Considering whether program resources such as central and/or on-site kitchens could be made available for
area-wide emergency response, such as for food preparation, use of equipment, or storage of food or
supplies.
• Considering accessibility of neighboring sites, within the county or Tribal lands as well as neighboring
county and Tribal dining centers, to support the continuation of service in the event of an emergency.
• Including a provision in vendor contracts for the caterer to provide emergency rations in the event of
disaster, if able.
• Developing relationships with other possible local vendors, such as hospitals, nursing homes, faith-based
organizations, and local restaurants and caterers, to provide meals if the primary caterer is unable to.
• Including a provision in the vendor contract for said agency to have a plan in place in the event of a disaster
or emergency. This should be planned and agreed upon by both parties.
• Contacting the owners of the dining centers to determine the feasibility of utilizing their available space if
needed in the event of an emergency.

102
P-03062-38 (04/2024)
3. Emergency meals
In preparation for emergencies that may disrupt regular meal service, nutrition programs may provide shelf-stable
or frozen emergency meals to program participants for later use. If emergency meals are delivered or taken home to
consume, the meals are reported as home-delivered or carryout meals. When program participants consume their
meals during an emergency, nutrition programs may deliver additional meals for replenishment. To count a meal as
NSIP-eligible, emergency meals must meet NSIP requirements, including nutrition standards.
Because it is
impossible to know when emergency meals are consumed, meals are reported at the time of distribution or delivery.
