
Document Management
and Imaging
TOOLKIT
American Health Information Management Association

Document Management and Imaging Toolkit
2 | AHIMA
Contents
Foreword........................................................................................................................................... 4
Authors and Acknowledgments ..................................................................................................... 4
Introduction—Transition to the EHR using Document Management and Imaging Systems .... 5
Current Landscape and Supporting the EHR ................................................................................ 5
» Today’s Document Management System(s) .........................................................................5
» Using Document Management as the Legal Archive ...........................................................6
» Record Retention and Destruction ...................................................................................... 6
» Disaster and Contingency Planning .....................................................................................7
Document Management Operations and Best Practices ...............................................................8
» Discharge Processing .............................................................................................................8
» Turnaround Time (TAT) ....................................................................................................... 8
» Scanning Preparation ............................................................................................................ 9
» Document Capture ................................................................................................................9
» Productivity Monitoring ...................................................................................................... 10
» Reporting ..............................................................................................................................12
» Staffing During Transition ................................................................................................... 13
System Design Options and Considerations ................................................................................14
» Document Retrieval, Viewing and Distribution.................................................................14
» Workflow ..............................................................................................................................14
» Chart Completion ................................................................................................................ 14
» Integration ............................................................................................................................ 15
Implementation and Leadership .................................................................................................. 15
» Determining the Information Technology Strategy ..........................................................15
» Clinical Systems .................................................................................................................... 15
» Scanning Implementation Options .....................................................................................16
» The Implementation Phase .................................................................................................17
» Implementation Team Roles and Responsibilities ............................................................. 17
» Project Sponsors ................................................................................................................... 17
» Project Charter and Scope ................................................................................................... 18
» Work Plan ............................................................................................................................. 18

Updated 2012
AHIMA | 3
» Conversion Options: Outsourcing ...................................................................................... 18
» Testing ...................................................................................................................................18
» Training................................................................................................................................. 19
» The Post-Implementation Phase ......................................................................................... 20
Case Study: “The EHRs Impact on Staffing and Turnaround Times:
Centralizing the HIM Department in a Multi-Facility Environment” ....................................... 21
Appendices
» A: Best Practices: Preparing and Scanning Documentation .............................................. 25
» B: Document Storage Options and File Size Calculations ................................................. 27
» C: Bar Code Information and Guidelines ........................................................................... 29
» D: Prepping Skill Set ............................................................................................................ 30
» E: Scanning Skill Set ............................................................................................................. 32
» F: Indexing Skill Set .............................................................................................................. 33
» G: Review and Quality Control Skill Set ............................................................................. 36
» H: DMS and EHR Points of Integration Table ................................................................... 38
Copyright ©2012 by the American Health Information Management Association. All rights reserved. Except as permitted
under the Copyright Act of 1976, no part of this publication may be reproduced, stored in a retrieval system, or transmitted,
in any form or by any means, electronic, photocopying, recording, or otherwise, without the prior written permission
of the AHIMA, 233 North Michigan Avenue, 21st Floor, Chicago, Illinois, 60601 (https://secure.ahima.org/publications/
reprint/index.aspx).
ISBN: 978-1-58426-394-4
AHIMA Product No.: ONB185012
AHIMA Staff:
Anne Zender, Editorial Director
Claire Blondeau, MBA, Managing Editor
Jessica Block, MA, Assistant Editor
Limit of Liability/Disclaimer of Warranty: This book is sold, as is, without warranty of any kind, either express or
implied. While every precaution has been taken in the preparation of this book, the publisher and author assume
no responsibility for errors or omissions. Neither is any liability assumed for damages resulting from the use of the
information or instructions contained herein. It is further stated that the publisher and author are not responsible for
any damage or loss to your data or your equipment that results directly or indirectly from your use of this book.
The websites listed in this book were current and valid as of the date of publication. However, web addresses and the
information on them may change at any time. The user is encouraged to perform his or her own general web searches
to locate any site addresses listed here that are no longer valid.
CPT® is a registered trademark of the American Medical Association. All other copyrights and trademarks mentioned
in this book are the possession of their respective owners. AHIMA makes no claim of ownership by mentioning
products that contain such marks.
For more information about AHIMA Press publications, including updates, visit www.ahima.org/publications/updates.aspx
American Health Information Management Association
233 North Michigan Avenue, 21st Floor
Chicago, Illinois 60601
ahima.org

Document Management and Imaging Toolkit
4 | AHIMA
Foreword
This toolkit has been developed to advance knowledge and
practice of document management and imaging and its role in
supporting the electronic health record (EHR).
It begins with the current document management and imaging
landscape in supporting the adoption of the EHR, continues
with document imaging operations and best practices, and
concludes with system design options, considerations, imple-
mentation, and leadership. The toolkit includes one case study
and eight appendices where more details, including tables, are
provided to enhance the main content.
Authors
Michelle Charette, RHIA
Kay Davis
Julie A. Dooling, RHIT
Kathy Downing, MA, RHIA, CHP, PMP
James Foster, MHA, RHIA
Jennifer Ingrassia, RHIA
Jamie McDonough, RHIA
Heather Rogers, MBA
Blake Sawyer
Traci Waugh, RHIA
Patrick Williamson
Acknowledgments
Cecelia Backman, MBA, RHIA, CPHQ
Jill S. Clark, MBA, RHIA
Angela Dinh Rose, MHA, RHIA, CHPS
Barry S. Herrin, JD, CHPS, FACHE
Sharon Silvochka, RHIA
Diana Warner, MS, RHIA, CHPS, FAHIMA
Lou Ann Wiedemann, MS, RHIA, FAHIMA, CPEHR
AHIMA e-HIM Work Group on
Electronic Document Management
as a Component of EHR:
Acknowledgements
This toolkit is based on a 2003 practice brief
originally developed by:
Beth Acker, RHIA
Maria A. Barbetta, RHIA
Kathy Downing, RHIA
Michelle Dougherty, RHIA
Deborah Fernandez, RHIA
Beth Friedman, RHIT
Nancy Gerhardstein, RHIT
Darice M. Grzybowski, MA, RHIA, FAHIMA
Beth Hjort, RHIA, CHP
Susan Hull, RHIA
Deborah Kohn, MPH, RHIA, CHE, CPHIMS
Amy Kurutz, RHIA, PMP
Roderick Madamba, RHIA
Therese M. McCarthy, RHIA
Pat McDougal, RHIT
William Kelly McLendon, RHIA
D’Arcy Myjer, PhD
Lori Nobles, RHIA
Jinger Sherrill, RHIA
Patty Thierry Sheridan, MBA, RHIA, FAHIMA
Michelle Wieczorek, RN, RHIT, CPHQ, CPUR
Sarah D. Wills-Dubose, MA, M.Ed., RHIA

Updated 2012
AHIMA | 5
Introduction
Transition to the Electronic Health Record using
Document Management and Imaging Systems
Document management systems (DMSs) continue to play a very
important part in capturing all the documentation needed to
tell the patient’s story. They allow for capture and simultaneous
access to needed documentation and chart completion and
provide a central repository of information. While the use
of paper will continue to decrease over time, document
management systems ultimately will support the electronic
health record (EHR) transition. These systems will manage
paper that continues to flow from the EHR, legacy systems, or
from external entities to ensure processes are fluid for users, and
act as a legal archive.
Assessing, selecting, implementing, and maintaining a DMS is
an investment. Optimizing your investment and leveraging
technology allows for cost savings and increased efficiencies.
During the EHR transition, it is important for the health
information management (HIM) professional to become and
stay involved in order to ensure the department’s processes
and integration points to the EHR are incorporated into
the project.
Meaningful use standards (and the accompanying opportunity
to receive federal subsidies) are driving the adoption of EHRs.
With the increased use of EHRs, it is more important than
ever for the information stored outside the EHR to be available
electronically. DMSs are a vital partner in capturing paper so
that information can be incorporated into or accessible from
the EHR.
Current Landscape and
Supporting the EHR
Today’s Document Management Systems
The terms Document Management System (DMS) and
Enterprise-wide Document Management System are frequently
used interchangeably. For the purpose of this toolkit, we will
focus on DMSs used in the HIM department to enable and
support the transition to the EHR. DMS simply refers to the
management of documents, and in this toolkit, we will be
referring to documents electronically captured for inclusion
in the health record.
The DMS is often referred to as the software used primarily
by HIM departments to handle the clinical and administrative
documents pertaining to a patient’s treatment. These are docu-
ments that are either unable to be built for use directly in the
EHR or have not yet been built. These documents are typically
scanned or acquired electronically post-discharge, but may also
be scanned or captured concurrent to the episode of care at
point of service. Other processes pertaining to the DMS include
chart completion, workflow, and release of information (ROI).
DMSs are also used throughout an organization to help reduce
the amount of paper that must be handled and tracked.
Organizations frequently use the same vendor for all their
document management needs, not only in HIM, but also in
areas such as human resources, patient financial services,
purchasing, registration, and the medical staff office, to name
a few, but it is the branching out to other business areas of
the organization that turns the DMS into an enterprise-wide
application.
Even as organizations make significant investments in a wide
range of separate patient-centric systems, there is a continued
need for DMS. DMS enables capture and access for many areas
across the enterprise. Multiple locations exist in the enterprise
where information regarding or influencing patient care can be
stored in the EHR. Although information can be captured and
accessed directly throughout these systems, the EHR is typically
the environment that holds this consolidated information.
The most important reason for acquiring and implementing a
DMS is to capture and manage the organization’s documents,
not to eliminate paper. Documents are organizational assets.
Organizations must respect the necessity and strategic impor-
tance of managing its document assets just like the organiza-
tion’s data, information, and cash assets.
Organizations must properly manage documents; their failure
to do so not only increases liability, but also risks information
loss that can significantly affect patient safety and quality of
care. Accordingly, many organizations are forming governance
committees to identify and establish ownership of information
repositories such as document management systems. When
HIM professionals assume ownership of the information, they
also assume stewardship or accountability for the decisions
made with regard to information management. When new
systems are implemented, integrations and migrations occur
to consolidate data or for decision making when archiving,
retrieving, retaining, or destroying information.
It is critical to incorporate process improvement principles
when working with people, processes, and technology. Until
the time that all internal and external (that is, outside the
organization) documents are captured, indexed, and distribut-
ed electronically to the EHR, technologies such as classification
recognition (such as bar coding, optical character recognition),
point of service scanning, and work flow enhancements will
continue to enhance productivity and help to achieve quality
standards in the DMS.

Document Management and Imaging Toolkit
6 | AHIMA
HIM professionals must be included in the DMS enterprise-
wide strategic plan to ensure that HIM standards of practice
(including regulatory requirements) are met as the organization
is crafting its strategy for years to come. The following questions
that pertain specifically to the HIM department should be con-
sidered as the overall institutional DMS strategy is developed:
» What are the long-term goals for the following HIM processes?
» Defining and maintaining the designated record set (DRS)
and legal health record (LHR)
- Accuracy, integrity, and accessibility of information
- Chart retrieval and viewing
- Document capture
- Chart completion, including electronic signature and
deficiency management
- ROI, including printing and exporting guidelines
- Coding, abstracting, and migrating to ICD-10-CM/PCS
- Transcription
- MPI maintenance
- Storage, retention, and destruction
- Downtime or contingency planning
- HIPAA, Joint Commission, CMS, and other regulatory
compliance
- Document management and information obligations
imposed by health information exchange and accountable
care organizations
» How do these HIM processes relate to clinical systems? For
example, how will verbal order signatures be tracked, who
will track them, and what impact will this have on computer-
ized provider order entry (CPOE) systems?
» How are documents created, generated, and transitioned for
CPOE implementation?
» What are the organizational goals surrounding decentralized
versus centralized scanning?
» How will seamless integration with clinical systems be
achieved?
» What HIM requirements are included in the organization’s
clinical health information systems and how will these be
incorporated into request for proposals (RFPs) and procure-
ment processes?
» What plans are instituted to promote physician and other
clinician acceptance of organization-wide electronic document
management? For example, will DMS functionality require
online medical record access and chart completion?
Using Document Management
as the Legal Archive
The legal health record (LHR) is comprised of those docu-
ments and data elements that a healthcare provider considers
its official record of patient care. The “source of truth” or the
official source system that you will use to respond to requests
for copies of the LHR must be identified and included in an
organization’s LHR definition. During the EHR transition, the
definition will need to be modified as documents move from
being captured in the DMS to being created or captured in the
EHR. There may be dual responsibilities for storing the LHR
where portions of the record are stored in multiple places after
a certain date if you are unable to integrate historical data from
your DMS into your EHR.
With the existence of preliminary and final versions of a
document, as well as original and corrected information, a
healthcare organization must address the management of
document versions. Once documentation has been made
available for patient care, it must be retained, managed, and
incorporated into the LHR whether or not the document
was authenticated. A decision must be made on whether all
versions of a document will be displayed or just the final, who
has access to the various versions of a document, and how the
availability of versions will be flagged in the health record.
Communication with stakeholders is critical when workflow
changes are implemented and a document in the DMS is now
being created and managed in the EHR. As more tools (such as
interfaces, integrations, and workflow) are introduced into the
organization, the processes in place and the flow of information
must be reconsidered to ensure that the process remains efficient
and information remains accurate. The tools available to manage
and access the medical record are changing and, therefore, so
must the approach to working with the new tools. Integration
tools between DMS and the EHR should decrease the amount of
manual work required to manage the health record, resulting in
increased efficiency and accuracy in processes.
For more information on integration, see “Integration” under
“System Design Options.”
Record Retention and Destruction
A provider’s records retention policy establishes how long an
organization should keep documents, the medium in which the
information will be kept, and where the records will be located.
Existing retention schedules will likely need to be updated to
reflect new document groupings when a new DMS is installed.
The record retention schedule is a critical component to plan-
ning a DMS implementation and works in conjunction with
the destruction policy (see below). The length of the retention

Updated 2012
AHIMA | 7
period will determine in part the access, maintenance, and
migration activities that must be factored as part of the imaging
system’s ongoing maintenance and storage costs. Those costs will
continue to accrue for as long as the documents are retained.
All healthcare records, including those stored in a DMS, should
be maintained and disposed of as part of a legally accepted
information and records management policy in order to ensure
their acceptance as legal documents. Policies should include
descriptions of how long information must be maintained and
retained. They should be based on federal requirements and
the statute of limitations for each state, community practice,
and accreditation agency. The principles of retention and
destruction are critical to electronic discovery (e-discovery)
procedures and the use of electronic evidence. Legal counsel
should always be sought when constructing or revising these
policies.
While there are no set standards regarding how long the con-
verted records should be maintained, destruction of the paper
should be carried out in accordance with federal and state law
and pursuant to an approved organizational retention schedule
and destruction policy. The destruction policy must be clearly
communicated throughout the organization. AHIMA’s updated
“Retention and Destruction of Health Information” practice
brief will provide additional guidance on record retention stan-
dards and destruction of health information for all healthcare
settings.
Once a paper record has been converted to electronic media,
it is standard practice that the paper is boxed up after it has
been scanned, indexed, and released into the DMS or uploaded
to the EHR. The HIM department should provide adequate,
secure space for the retention of these records while they are
being processed and moved throughout the quality assurance
and corrections process.
Organizations should have processes in place to track complet-
ed records and the ability to run reports listing charts that have
been released to the DMS or EHR within a certain timeframe
to aid in identifying those charts that are eligible for destruc-
tion (for example, a report that shows all records that have
been released more than 90 days from today’s date).
Organizations should have a plan in place to destroy the
paper-based records that have been incorporated into the EHR
as soon as possible. The case can be made for destroying the
paper when users have confidence and trust that the informa-
tion has passed the quality assurance process, was properly
converted and readily available in the DMS.
Disaster and Contingency Planning
Preparing for disaster is a must whether it is a natural disas-
ter such as a flood or earthquake, a man-made disaster such
as theft or terrorism, or an unintended man-made disaster
such as an “error and omission” or fire due to a faulty system.
Developing a business continuity plan (BCP) is the overarch-
ing approach to business recovery; the BCP generally contains
individual plans for restoring departments back to business
quickly after any type of interruption that disrupts normal
healthcare operations.
A downtime or contingency plan focuses on sustaining a busi-
ness function during short interruptions that are not classified
as a disaster. Downtime may be planned or unplanned and
both scenarios must include alternative ways of conducting
business during this time. When creating a contingency plan,
management must consider the following:
» Identify personnel responsible for each portion of the con-
tingency plan, and include a list of duties for the staff when
systems are down. For example, consider redistribution of
workload so that all staff perform document preparation or
other paper-based activities until systems are restored.
» Determine which applications and computer systems the
HIM department relies upon in order to function.
» Identify the criticality of those applications and computer
systems.
» Create temporary work-around procedures that will be
implemented during system interruptions.
» Decide when and how to activate escalation procedures in
order to provide continuous patient care and maintain the
workflow of information for business operations.
» Decide how data captured on paper can be entered into the
DMS once systems have been restored.
» Determine a plan for varying lengths of downtime and how
staffing will be impacted. Consider differences in operations
when down time lasts for less than four hours, four to eight
hours, or more than a full shift.
» Determine a plan to validate system data for accuracy after
the DMS is restored.
For more information on developmental steps of a facility’s
disaster plan relative to the collection and protection of health
information, including a sample contingency plan, see the
updated “Disaster Planning for Health Information” practice
brief.

Document Management and Imaging Toolkit
8 | AHIMA
Document Management Operations
and Best Practices
Discharge Processing
Timely capture of information, whether post-discharge or
after a patient encounter, is critical. Discharge processing is a
fundamental process that ensures timely pick-up and receipt of
health information for scanning. Although this process is not
new to HIM, this process starts the turnaround time clock and
drives the entire document imaging process from beginning
to end or, in the DMS environment, from patient discharge to
availability in the EHR.
The remediation process includes tracking, accounting, and
following up on all discharges (inpatient, outpatient, emergency
department, and physician office, if applicable) to ensure all
information has been received. While HL7 and ADT feeds are
used for various reasons within a DMS, discharge processing
uses HL7 to facilitate remediation.
Organizational teamwork should be strongly encouraged
within this process. For documentation to be readily available
for scanning as soon as possible after the discharge, an inter-
nal policy that outlines expectations is suggested. Consider
the case of a patient returning to the emergency department
(ED) 24 hours following her initial visit and a subsequent visit
to a nursing floor. If the information from the initial visit has
not been completed by the clinician(s) in the ED and sent
for scanning, the patient’s health information is not available
to the healthcare team, which can create a patient safety risk.
Thus, a scramble ensues to find the record and have it scanned
immediately.
The following should be considered when making process
decisions:
» During what shift(s) will the records be picked up?
- A schedule that lists every day of the week with the pickup
location and time should be in place.
- Consideration must be given to heavy discharge times—if
your highest discharge time window is 5 to 7 p.m., then a
9 p.m. pickup may be in order.
- Holiday schedules should be made well in advance with
anticipation of volume uptake due to increase in discharges
prior to the actual holiday.
- Seasonality should also be considered when scheduling
records pickup, especially during flu and peak tourist
season(s).
» How will records be transported?
- If records are created at multiple locations, will a courier be
needed to transport records?
- What security protocols are in place to secure the protected
health information (PHI)?
» Is the scanning flow documented?
- Does your staff know how a chart moves through the
scanning process from beginning to end?
- Does the process consider all retrieval needs such as
coding, chart completion, ROI, audits, and readmissions
as in the example above?
- Do you have a procedure in place for scanner downtime?
- Do you have a procedure for when the paper record is
requested and needs either to be copied or taken out of the
department for patient care?
Turnaround Time
Turnaround time (TAT) starts at patient discharge and ends
when the images are released into the DMS or EHR.
The first step in calculating the desired TAT is to define the
parameters of TAT, such as
» What is the desired TAT to have records available post
discharge?
» Will each patient type or service type have its own TAT goal?
For example, will ED charts be held to a 12-hour TAT while
inpatient discharges are held to a 24-hour TAT?
» Will high dollar charts be processed first if TATs are not being
met?
» Will emergency department document types take priority
over loose sheet document types?
» Will certain discharges be best processed during a particular
shift?
Whether document management is performed in-house or
outsourced, TAT terms can be mutually agreed upon before
implementation begins. These metrics will assist in prioritizing
the chart procedure and can dictate the workflow of each day
starting with the chart collection schedule.
As a general rule, as part of the implementation process, it is
necessary to work with stakeholders such as clinicians, depart-
ment heads, and HIM staff to determine their requirements
and expectations surrounding documentation availability.
For example, ED records may need a faster TAT compared to
inpatient discharge records. The targeted TAT goal is 24 hours;
however, this goal is usually met only following a six-month
adjustment period post-implementation. Meeting TATs on

Updated 2012
AHIMA | 9
a consistent basis requires a “Plan-Do-Check-Act” cycle for
continuous quality improvement. It also requires management
to closely monitor and improve upon all areas of the scanning
process (prepping, scanning, indexing, quality assurance, and
identifying documents that can be computer output to laser
disc [COLD] fed to your DMS).
For more information on TATs, see the case study “The Elec-
tronic Health Record’s Impact on Staffing and Turnaround
Times: Centralizing the HIM Department in a Multi-Facility
Environment.”
Scanning Preparation
Chart preparation is the most time consuming and critical task
in the document imaging process. If the process is performed
correctly and efficiently from the beginning, it could reduce the
time spent manually indexing.
The document preparation process is the equivalent of chart
assembly and loose material sorting in the paper chart environ-
ment. The document preparation process involves grouping,
identifying, and preparing health record documents prior to
scanning so they can be captured efficiently.
Newer intelligent document recognition technologies can ease
the labor burden and quality issues associated with traditional
prepping. This technology can be used to classify document
types and patient demographic information.
Careful consideration must be given to handling “blank sides.”
The organization must create a plan and involve the technolo-
gy vendor and information technology in the decision making
process:
» Will the DMS capture all pages (front and back)?
» Consideration must be given to if the DMS technology has
the ability to delete blank pages or if staff will be trained on
identifying pages to be deleted?
» Who will have the rights to delete?
» In which phase of the process will this be performed? Will
blank pages be flagged at time of prepping such as page 4
of 4, caught during the QC process or will both teams be
responsible for monitoring and handling blank sides?
» Fee structures with third party vendors must be clearly
defined. It is critical that capture and charge of blank pages
be clearly defined and understood in the contract phase.
For additional information on productivity, see the Productiv-
ity Monitoring section of this toolkit. In addition, for informa-
tion on preparation, capture, and scanning best practices, see
Appendix A, “Best Practices: Preparing and Scanning Docu-
mentation.”
Document Capture
Understanding and managing the capture process is critical.
While document capture may be performed using a variety of
technologies, including scanners, electronic forms, electronic
transactions, cameras, voice, and video. For the purpose of this
toolkit, we will focus on scanning and electronic integrations.
Efficient document scanning can be achieved by utilizing a
centralized approach, a decentralized approach or a blended
or hybrid approach. Healthcare organizations must decide
which capture model will work best in their environment by
evaluating the size and type of organization, staffing, technol-
ogy, and other resources that are available to make the project
a success.
Centralized scanning requires that all documents within an
organization be sent to a central location for document capture
through high-volume scanning technology. Depending upon
the size of the organization, documents may be delivered
internally to the designated scanning location or they may be
delivered via courier.
Decentralized scanning requires small scanners being placed
at patient registration areas, nursing floors, physician office,
outpatient clinic locations, emergency departments, and other
on- or off-site locations. As paper documents are completed,
they can be scanned and indexed immediately or placed in a
queue for indexing later. Decentralized scanning allows more
of the documents to be captured prior to a patient’s discharge
rather than the scanning being done within HIM after dis-
charge. Registration information such as insurance cards and
advance directives can be available immediately for benefit
verification and patient care. Many organizations are using a
blended or hybrid approach to documentation, using central-
ized and decentralized scanning throughout their facilities. For
example, although a hospital may have a centralized scan-
ning location in the HIM department to scan post-discharge,
decentralized (point of care or point of service) scanning may
be used to capture documentation such as a driver’s license and
insurance card at registration that may be needed as the patient
moves through their visit.
Scanner size, speed, and functionality must be thoroughly
investigated before acquisition and implementation to under-
stand how the equipment will handle volume and certain doc-
ument types. It is critical to purchase a scanner that is capable
of handling expected volume particular to the organization’s
needs and scanner speed and functionality are directly related
to productivity. It is also important to know the functionality
of the equipment to evaluate document types for special han-
dling. For example, can the scanner accept scanning of strips
(such as telemetry) up to a certain length? Will the paper need
to be cut in the preparation stage?

Document Management and Imaging Toolkit
10 | AHIMA
When evaluating document capture methods, focusing on
capturing electronic transactions automatically will increase
the volume of capture at the beginning of the project since it
involves less labor. Electronic transactions include faxes, those
documents received via COLD or electronic record manage-
ment (ERM) systems.
It is important to consider data and image storage require-
ments as planning is underway for transition to a DMS. This
is important even if the organization intends to use an EHR
to store the majority of health information because electronic
storage needs for images can be quite large and will grow over
time.
For more information on data storage for scanned images,
refer to Appendix B, “Document Storage Options and File Size
Calculations.”
To enhance the document capture process, consideration
should be given to the following tools:
» Patient labels: Many organizations have policies that require
placement of a patient label on every page to identify the
patient. Data elements include the patient’s name, medical
record number, and other identifiers such as an encounter
number, visit number, etc. This practice follows best practice
and patient safety initiatives.
» Bar coded separator sheets: Many times form redesign takes
months to complete. However, scanning operations may need
to begin before this process is completed. Many systems allow
the use of bar-coded separator sheets for each section of the
record as a precursor to complete forms redesign. Inserted
into a chart during the prepping stage, the separator sheet
contains the bar code for the next group of documents (such
as nurses’ notes, orders, and such). This method requires
more preparation time than bar coded forms, but it can act
as an interim solution with higher accuracy and speed than
could be accomplished by manually indexing each form.
» Forms redesign: One of the goals of forms redesign is to
identify and describe the form characteristics required to
ensure successful form identification when using a DMS.
Complying with bar code design specifications will ensure
the highest level of accuracy when using bar code recogni-
tion software. It also helps to identify form characteristics
required to ensure better accuracy using forms recognition
features of an optical character recognition (OCR) or intel-
ligent character recognition (ICR) engine.
- Key points to consider include the following:
•Eachtypeofformneedsitsownbarcodesothatitcan
be automatically recognized when scanned.
•Formnamesshouldbeuniquetotheformandrecog-
nizable to the people who will be using the forms even
occasionally.
•Anyrequirementsforthetypeofformname,lengthof
name, bar code font, size of font, and such should care-
fully meet the requirements of the DMS and the EHR (if
applicable).
» Bar code types: The best approach to scanning health records
is to use 100 percent bar-coded forms. The longer an organi-
zation waits to incorporate 100 percent bar-coded forms, the
less productive the scanning process will be. Although this is
normally very difficult to achieve at the beginning of a scan-
ning project due to the volume of forms that need bar codes
and the presence of outside documents that are not consis-
tent in appearance, the process of bar coding forms should
begin as soon as possible.
» Code 3 of 9: Most DMSs support the Code 3 of 9 (also
referred to as Code 39) bar code standard (see example in
figure 1.1 below). This is an alphanumeric, self-checking,
variable-length code that employs five black bars and four
white bars to define a character. Furthermore, three of these
bars are wide, and six of these bars are narrow. The wide
bars or spaces are at least two, but preferably three, times
the width of the narrow bars or spaces. When implement-
ing DMS using bar codes, it is important to understand the
bar code specifications, the bar code content, and the issues
related to bar code placement on the form.
Figure 1.1—Sample 3 of 9 bar code
» 2D: In addition to the 3 of 9 bar code standard, additional
types of bar codes are growing in use in the United States
(see example figure 1.2). There has been rapid expansion of
the use of two dimensional (2D) bar codes in advertising and
other commercial settings, and we have begun to see applica-
tions for use in the healthcare environment.
Examples of 2D bar codes include QR codes, which can be
read by a cell phone with the correct application downloaded,
or through the use of Aztec bar codes. The 2D bar code
format has a few benefits over the 3 of 9 format, including
the ability to store a larger amount of data, direct a user to a
website, and enabling sorting or finding a particular form or
page. They also lend themselves to the ability of being used in
a more demanding environment such as in a clinical setting
where they can be used on the wrist or ankle bands for new-
borns. In this setting, the format is better suited to a small
size and curvature of the band when placed on an infant. It
will be important to consider the next generation of bar-

Updated 2012
AHIMA | 11
coding fonts as well as recognition capabilities when selecting
a document management vendor to ensure that needs will be
met as the technology evolves.
Figure 1.2.—Sample 2D bar code
See Appendix C, “Bar Code Information and Guidelines,” for
additional guidance.
Productivity Monitoring
The ability to monitor performance is vitally important when
managing the document imaging process whether the work is
being performed on- or off-site, by the organization’s employees
or by a third party such as a document imaging vendor. Setting
productivity expectations is critical to managing document
imaging, and the following guidance should be taken into
consideration when creating productivity monitoring standards.
Productivity monitoring starts with being able to adequately
measure processes. Charts vary greatly in size and image
count, so assigning a number of charts to a staff member who
prepares them is not an accurate measurement. Many organi-
zations use inches or weight to measure for performance and
whether manual entry or computer entry into the document
management system is used, a procedure should be in place
outlining the process and recording of numbers.
With the understanding that every organization has differ-
ent documentation practices, internal processes, approaches
to technology, and strategic goals, the following (figure 1.3)
recommendations are provided as a “general rule” to assist
with creating departmental or organizational standards. The
figure shows each production step from preparation to index-
ing with corresponding initial rates (typically during the first
six months following implementation) and final rates (those
rates at the highest end of the proposed goal). Rates below
are shown as images per hour (IPH) per person. They have
been shown to be typically observed for each process. To avoid
backlog situations, the prepping and indexing rates should
be closely coordinated. Prepping will typically be faster than
indexing in the beginning, which is why the initial rates listed
below show prep at a higher rate when compared to index-
ing. Managers should adjust staffing in these areas to meet
anticipated volumes and scanning throughput. Also, these
rates take into account that these tasks are the sole focus of the
staff member during this monitoring time when the volume is
maximized.
Figure 1.3 — Sample production rates
It is also very important to recognize that scanner metrics vary
depending upon the size and speed of the scanner. For example,
larger scanners used for volume scanning operate much
faster than a desktop scanner used to capture driver’s licenses,
advanced directives, and such. Standards should be tailored
to the type and speed of the scanner being used. For example,
a scanner that captures 2,500 images per hour would have a
maximum capture rate for volume or batch scanning.
Indexing programs can also vary depending upon the steps
involved in the process. The number of required fields and
processes will affect productivity.
Quality control (QC) should be included in every step of
the document imaging process, from receipt to release into
the DMS or EHR. A comprehensive and well-executed QC
program will help to create trust in record integrity for all users
of the health record, and it is an important component to the
overall success of the document imaging program. The goal of
the quality program is to achieve the highest level of accuracy
through index verification and scan quality.
The following should be considered when creating QC policy
and procedures:
» Consider overall organizational strategic goals when framing
DMS expectations and results.
» During prepping, QC measures may include whether or not
primary documents are included:
- Are documents in order according to specific prepping
guidelines set forth by the organization?
- Are missing information or documents present?
- Are flags or notes used properly to identify missing parts of
the chart?
» Image quality, as well as content legibility, should be reviewed
while identifying and validating data elements as defined by
the general business rules set forth by the organization:
- All pages should be oriented to the correct reading position.
Rotate any images that appear to be upside down or
sideways.

Document Management and Imaging Toolkit
12 | AHIMA
- Patient information on all pages must be verified with
accurate indexing to the patient, account, and document
types levels. One task may include matching the identify-
ing number (such as account number or medical record
number) and patient name on the bar code to the remaining
pages in the batch.
- Delete any blank pages without information as well as bleed
through pages. For more on blank sides, see section titled
“scanning preparation” contained within this document.
- A process should be in place to remediate the number of
physical images scanned to the number of images captured
in the software.
» While some organizations prefer to conduct QA reviews on
100 percent of scanned documents, others use a hybrid
approach including random sampling or a certain percentage
of documents to ensure accurate document capture. This
approach should be determined by each organization based
on what is right for its particular situation, taking risk,
staffing, and budget into consideration.
» Note: Some DMS solutions contain the ability to monitor the
entire scanning process (from prep to release) in real-time
and are able to provide quality reporting post scanning such
as number of imaged captures, number of blank pages, and
such.
Quality Point System
Staff can be evaluated using a quality point system in conjunc-
tion with metrics and number of errors. Depending on the
severity of an error, the employee would be assessed a certain
amount of points within a review period. Errors such as mixed
accounts or patients, missing images or pages, overlapping
pages, or poor-quality images could be considered a critical
or severe error while blank pages, unnecessary images, skewed
images, or an incorrect document type could be considered a
low-impact error. One formula that is used to measure quality
is the percentage of actual errors as compared to the total re-
cords processed divided by the total cost of operations (includ-
ing staff, hardware, software, furniture, space, maintenance,
supplies, and such). This figure is then divided by the time it
takes from receipt of the record to the time it is released into
the EHR. The result is typically are double digit numbers where
the higher value indicates better performance.
1
All quality pro-
grams should be reviewed by human resources and approved
by senior management prior to implementation.
Reporting
Communication through reporting is a vital component to
managing a DMS. It is important to work with the DMS
vendor to understand the system’s reporting capabilities and
to be able to differentiate between the various types of reports
(standard, ad hoc and custom) and to determine whether the
organization will incur additional costs as a result of any
custom reports. Prior to implementation, discussing reporting
options and capabilities with the organization’s DMS
vendor will help ensure the necessary reports will be
available at go-live.
When evaluating reporting, the following should be considered:
» It may be necessary to compare the new DMS system to a
previous DMS system to understand which reports should be
retained and which are no longer needed.
» How are reports generated? Can they be produced within the
DMS application, or are they produced external to the
application?
» If reports are generated external to the application, what
platform is used to generate reports? Is extra software or
hardware needed?
» What kind of reports can be produced? Is an internal report
writer needed?
» How often will reports be generated, and can they be auto-
matically scheduled?
» It is important to predefine “pages” versus “images” when
evaluating the report data. While one person may think that
a page consists of only one side, another may consider a page
as two sides. Often, “images” is used where one image equals
one side of the page.
Reporting is usually accomplished through the routine
reporting of information in status reports to key individuals
and groups. The following reports should be evaluated as the
organization implements DMS routine reporting:
Quality Reports: To measure quality output within all
functions according to the organization’s needs
» Breakdown by problem categories (such as mixed accounts,
mixed document, or poor image quality)
» Breakdown by error severity
» Breakdown by patient/service type
» Missing primary documents
» Overall quality with drill-down ability to the document
imaging specialist (employee) for each step of the process
Productivity Reports: To measure productivity in all
functions according to the organization’s needs
» Turnaround time (TAT)
- High level (entire TAT for all functions including prep, scan,

Updated 2012
AHIMA | 13
index, and QC)
- Specific charts or specific document type (such as loose) to
track increase or decrease in certain areas relating to EHR
implementation
- Each stage of the scan process (prep, scan, index, and QC)
- All with drill-down ability to measure the individual
document imaging specialist (employee)
- Criteria could include the following: User ID, total pages,
total documents, pages per hour, documents per hour,
average pages per batch and total hours spent performing
the task. Reports can be generated for scanning as well as
for indexing.
» Patient/service type
Operations: To assist in managing the day-to-day operations
of document imaging
» Managing discharge list
» Courier tracking
» Quality feedback
» Chart tracking
» Change request
» Destruction notification
Research: Reports to assist in finding a specific chart in the
scanning process
» By account number
» By medical record number
» By scan batch
» By box
Reporting from DMS document capture system: Reports that
may be available specifically from the scanning
application (usually separate from the DMS)
» Scanning productivity results
» Index productivity results
» TAT of each system
Staffing During Transition
For most organizations, the EHR transition will happen in
phases. The impact on staffing and operations must be consid-
ered, and skill sets need to be assessed throughout the process
to ensure the transition is successful.
Staffing concerns for document imaging can be different from
other HIM roles. All job descriptions will need to be reviewed
and revised to reflect new skill set(s). Like all HIM professionals,
the ideal candidate should be able to maintain accuracy, focus
on attention to detail, and uphold confidentiality, but an imag-
ing specialist also needs to be able to adapt to a production-
based environment, which requires an increased ability to
remain astutely focused, work independently, and not be easily
distracted. When recruiting for document imaging specialists,
reference appendices D, E, F, and G to identify appropriate skill
set and job description criteria in the following areas: Prepping,
scanning, indexing, review, and quality control.
Skill sets should be time-tested during the interview process to
evaluate how the candidate would perform in a high-production
environment. The ability to remain focused amid high levels of
activity and noise distractions is critical to the success of
the process.
Cross training is recommended for ensuring continuity of
operations in the event of a short-staffing circumstance as
well as for discovering whether others possess special talent or
interest in certain aspects of the operation. For information on
one organization’s experience with a DMS implementation in
a multi-facility environment, please refer to the attached case
interview, “The EHR’s Impact on Staffing and Turnaround
Times: Centralizing the HIM Department in a Multi-Facility
Environment.”
In addition, figure 1.3 is a scenario showing how to calculate
the number of staff needed. The scenario assumes the depart-
ment is capturing 3,500,000 images per year. The calculation is
(images per year)/(images per hour) × 2080 to get the number
of full-time equivalents (FTEs). It is very important to keep
in mind that the initial rates and images per hour (IPH) will
vary depending upon equipment and manufacturer. Before
determining these rates, consultation with the organization’s
scanning vendor is highly recommended.
Figure 1.4 Excerpt from “Document Management and Imaging Best
Practices to Manage Hybrid Records” Preconvention Workshop, 2011
AHIMA Convention Proceedings

Document Management and Imaging Toolkit
14 | AHIMA
System Design Options
and Considerations
DMSs include tools to assist in the transition to the EHR and
enhance integration. Document retrieval, viewing, distribution
and workflow, including chart completion, are all important
components to consider when attempting to leverage current
technology to boost EHR adoption. In addition, integration is
critical to achieving seamless EHR integration.
Document Retrieval, Viewing, and Distribution
Retrieving documents will depend on how a DMS is deployed.
In some cases it could be through the organization’s intranet,
the Internet, an application on the desktop, or within the
clinical system. Ideally, access is simple and does not require
the user to jump back and forth between systems.
Methods of viewing and retrieving documents should be
provided on-site in designated work areas or throughout the
organization. Remote viewing should be provided to authorized
users in particular to support viewing of documents from
physicians’ offices, remote completion of records, and remote
coding or other job functions that may work virtually. Basic
and advanced search methods should include filters and the
appropriate security measures to track access and to limit
access on a need-to-know basis.
Distribution of information must be managed by the organiza-
tion and should include the following options:
» Online viewing only for authorized users
» Online viewing and printing (generally only provided to
HIM staff to support release of information functions)
» Automatically fax for authorized users including scheduled
distribution (for example, carbon copies of ED notes to
the referring physician, scheduled at certain day(s) and/or
time(s))
In addition, it should be noted that if a vendor hosts or retains
the images or stores the record for the organization, it is a
business associate, and the organization would need to execute
a business associate agreement (BAA) that is compliant with
the new HITECH rules.
Workflow
Workflow is a critical component of a DMS because it enables
electronic routing and concurrent processing. Many tasks
traditionally performed within the HIM department now can
be performed remotely within the healthcare facility. Workflow
rules identify how documents tied to the tasks can be assigned,
routed, activated, and managed through these rules and
directed to a staff member for disposition. For example, when
the status of dictation changes from dictate to transcribe to
sign to signed, a chart completion workflow rule will automati-
cally update the status of the deficiency system without human
intervention and simultaneously send a request for dictation or
review and signature to the physician’s inbox.
Coding is another critical HIM workflow in that it enables
records to be distributed to coders’ work queues. Coders are
then able to perform their work using the EHR instead of the
paper record. They should be able to route records to supervi-
sors for coding questions, to physicians for coding query, or
to auditors for prebill review. Coding from the imaged record
or clinical system creates new opportunities to meet bill hold
requirements, manage space, and recruit coders.
The HIM department’s workflow changes significantly with the
implementation of a DMS. In the implementation phase, HIM
departments should articulate workflow assumptions, identify
changes, and make decisions regarding which process(es) to
implement.
Chart Completion
When converting from paper to electronic records, the chart
analysis and chart completion processes change. With chart
analysis, staff analyze records online instead of using the paper
charts. One of the largest workflows in a document manage-
ment system is most often chart completion, and within
this workflow is the ability to electronically edit (annotate a
scanned image), sign, add an addendum, and flag or tag defi-
cient documents to electronically allocate a deficiency to the
appropriate provider(s).
Electronic signature capability should exist for both scanned
documents and text documents that are interfaced. Workflow
rules can direct unsigned documents (scanned notes and dic-
tated reports) to a physician’s work queue either in the EHR or
the DMS where they can be signed, edited, or an updated with
an addendum. Updating documents and securing signatures
electronically automates the record completion process with
little human intervention.
Where in the workflow electronic signatures are captured
and where finalized documents will reside is a fundamental
decision that needs to be made when implementing the DMS
and transitioning to the EHR. For example, if the majority of
the facility’s documentation resides in the EHR with a robust
workflow, the organization may decide to capture and index
documents in the DMS with an upload into the EHR, where
that workflow is used to complete the record. However, on the
other hand, if the majority of the documentation is interfaced
and completed in the DMS, the organization may decide to
use the DMS to capture, index, complete, and store the health
record. For more information on the legal archive, see “Using
Document Management as the Legal Archive.”

Updated 2012
AHIMA | 15
As with all functions, policies, and procedures related to the
DMS will provide consistent guidance to all employees within
the organization. Policies and procedures should be reviewed
to ensure consistency with laws and guidelines established by
federal, state, regulatory, and accreditation (if applicable)
agencies. Administrative leadership, HIM, information
technology, information security, quality assurance, and
clinical staff should be included in the process of developing
enterprise DMS policies and procedures. The HIM department
will need to develop policies and procedures specific to the
document management system. The following are areas where
specific policy and procedures unique to DMS will need special
attention and guidance:
» Corrections: Policies and procedures should identify how
and by whom correction can be made. Business rules may
determine who can access and correct unsigned documents.
Organizations should develop guidelines for changes made to
signed and unsigned documents.
For example, if a document is changed or corrected, typically the
copy with the error is removed from view within the DMS.
However, a copy of the original document must be available
particularly if it was viewable and relied on by clinicians. It
is important that all staff are aware that these documents are
available if needed. Workflow should be evaluated for ensur-
ing corrected documents are redirected to the source of where
the initial incorrect document was created or received.
•Retraction, reassignment, resequencing: These terms have
different meanings and their corresponding action may differ.
Therefore, it is best to define these terms.
- Retraction A retraction is the action of correcting information
that was incorrect, invalid or made in error, and preventing its
display or hiding the entry or documentation from further
general views. However, the original information is available
in the previous version. An annotation should be viewable
to the clinical staff so that the retracted document can be
consulted if needed.
- Resequencing involves moving a document from one location
to another within the same episode of care, (e.g. a progress
note that was linked to the wrong date). No annotation of
this action is necessary.
- Reassignment (synonymous with misfiles) The process of
moving one or more documents from one episode of care to
another episode of care within the same patient record, (e.g.
the history and physical posted to the incorrect episode). An
annotation should be viewable to the clinical staff so that
the reassigned document can be consulted if needed.
3
Integration
Organizations have discovered that a DMS is a critical compo-
nent when transitioning to the EHR. DMS allows providers of
all sizes to move to an electronic record with minimal impact
on clinical areas. As federal regulations such as The Health
Information Technology for Economic and Clinical Health
Act (HITECH) push for digitized information, document
management and imaging can be a stepping stone or used in
conjunction with the best-of-breed systems that create an EHR.
For this reason, integration points are recommended in any
Request for Information (RFI) or Request for Proposal (RFP)
issued related to acquisition of DMS technology.
There are important technical considerations when evaluating
integration points between the DMS and the EHR. Refer to the
table in Appendix H, “Document Imaging and EHR Points of
Integration,” for high-level considerations that organizations
can use to coordinate an implementation plan or an ongoing
maintenance plan for DMS and EHR system configurations.
Implementation and Leadership
Regardless of the industry’s progress on the path to the EHR,
most healthcare organizations continue to utilize paper-based
health information. Doing so results in a hybrid health record
that is partially computer-generated and partially paper-based.
The goal of a DMS is not only to manage paper, but also to
manage all of the organization’s documents (computer-gener-
ated and paper-based).
The following are best practices detailing the key steps in
implementing a DMS.
Determining the Information Technology Strategy
AHIMA recommends that HIM computer systems comple-
ment the organization’s EHR and clinical decision support
systems that are acquired and installed in the healthcare orga-
nization. For this reason, asking questions about integration is
critical to the strategy discussion.
Clinical Systems
Clinical health information systems are used by care providers
to document the care provided to patients (such as computer-
ized physician order entry [CPOE] systems and clinical docu-
mentation systems). HIM professionals typically focus on how
to automate the familiar chart components, such as physician
progress notes, nurses’ notes, graphics, and ancillary notes.
In the past, clinical health information systems were created by
clinicians for clinicians with little thought about their impact
on HIM and other healthcare organization processes that work
in the background to support caregivers, such as the creation

Document Management and Imaging Toolkit
16 | AHIMA
and maintenance of the legal record and revenue collection.
Today’s newer generation systems include these supporting
process requirements. For example, many of these systems
include the document imaging technology component of a
DMS because supporting the process requirement of scanning
paper-based documents remains useful until all physician,
nursing, and ancillary documentation is captured in a digital
format at every healthcare organization.
Scanning Implementation Options
Scanning is one type of technology that can be used in a DMS.
It can be implemented as a stand-alone departmental solution
or one that integrates with existing clinical applications. Often
stand-alone solutions are installed in one or two departments
such as HIM or billing, solving problems inherent in the access,
movement, and storage of paper documents.
However, stand-alone scanning systems require implementers
to consider how they will interact with clinical systems. These
systems often stand on their own, with little connection with
other systems except to receive data through interfaces. If an
HIM department chooses this option, access to authorized
users outside of HIM should be provided in a manner that
does not require users to leave the clinical system to view
information in the DMS.
Several clinical vendors now include scanning as a component
of their clinical health information systems, thereby achieving
greater integration with clinical applications than their stand-
alone counterparts. It is becoming more common for clinical
vendors to include the breadth of required HIM functionality,
including scanning as a critical component.
The decision to purchase a scanning component as a stand-
alone system or to purchase it as part of a clinical system
should be based on where an organization is on the path to the
EHR. It should also be based on the functionality provided by
clinical vendors versus stand-alone scanning vendors.
If an organization decides to outsource its scanning to a docu-
ment management vendor, technology choices and the integra-
tion with the EHR are very important to the overall success of
the effort.
Planning Steps/Checklist: Once it is determined that the
document management implementation is moving forward,
the detailed planning steps must begin. To ensure a full return
on investment, it is important to complete each step with ad-
equate time for planning.
In addition, remember to include the appropriate stakeholders
(users, influencers, key decision makers, and such) in the plan-
ning process. Also include key players on the EHR task force,
and create a list of others who need to make a decision in the
planning component.
There are 11 key steps in the planning process:
1. Assembly: Ensure the record is in optimal physical order
for efficient processing for records to be scanned.
2. Types of records: Determine where each record type is
stored and how reconciliation (check in and account for
each chart, including outpatients’) will occur on a daily
basis
3. Forms inventory/format: Create inventory with a sample
of each form considering redesign needs.
4. Loose or late reports: Determine policy on receipt of loose
reports, adding in order or filing in back of chart, and codi-
fying once entered into system.
5. Physical layout of equipment: Determine workflow in
HIM department and consider the physical environment
for scanning equipment and staff.
6. Analysis, deficiency, and electronic signature process:
Ensure that the medical record is complete and that entries
are timely according to established rules and regulations.
7. Paper retention and destruction: Determine disposal
procedure for paper documents after scanning.
8. Communications: Ensure that all stakeholders receive
critical information about the new system and its impact.
9. Quality assurance: After documents are scanned, establish
indexing and quality control. Indexing is performed to
assign document names and encounter numbers to each
document. It is recommended that quality be performed
on 100 percent of images to review the quality of scanned
images. In addition to this initial quality control, ongoing
quality monitoring should be performed on a random basis.
10. Policy and procedures: Develop new policies and proce-
dures. Adapt existing policies to new processes related to
changes in workflow, access, storage and retention, and
such.
11. Legal considerations: The information stored is the entity’s
business record (in healthcare, the legal record). A plan to
house this information on media other than paper must be
scrutinized by legal counsel to ensure that the technology
being considered can comply with federal and state laws,
requirements for licensure, and credentialing, along with
operational needs and that it is consistent with existing
policies and procedures. There should also be a risk man-
agement component of the analysis to ensure that there
will be no compromise to patient care and that documents
required for lawsuits remain available. This latter consid-
eration may impact an organization’s decision on how to
proceed with storage and retrieval of documents already
scanned into the DMS.

Updated 2012
AHIMA | 17
The Implementation Phase
In the implementation phase, the real work begins. Establishing
a project management team, solidifying work plans and creat-
ing a management reporting methodology for the implementa-
tion will be accomplished during this phase. Workflow will be
redesigned and decisions will be made based on input from the
HIM department and the vendor’s project management team.
During the process, many workflows and schematics will be
designed and redesigned. Finally, the implementation phase
will include testing, training, and the system going live.
Project Management: A strong project management team and
plan will help ensure a smooth and successful transition to a
DMS. This section provides resources and guidance that are
typically involved in managing a DMS implementation. Please
note that this list may vary by vendor or by organization. How-
ever, it is critical that the organization receive commitments
from the vendor(s) that their implementation team members
will support the go-live timeline.
Implementation Team Roles and Responsibilities
Vendor Roles and Responsibilities
» Project manager: Manages overall project and the vendor
project team focusing on scope, time, cost, risk, and quality.
Works closely with the enterprise project manager through-
out the duration of the project.
» Application consultant: Provides expertise in configuring
the software product to meet the needs of the enterprise, in
addition to providing the enterprise with support to determine
how the product will work best within the organization.
» Programmers: Provide expertise in coding the software
product to meet the needs of the enterprise.
» Integration analysts: Provides expertise in developing inter-
faces and conversions to meet the needs of the project. In
addition, provides expertise on the database level requirements.
» System engineers: Provides expertise on replacing and
setting up the software.
Organization’s Roles and Responsibilities
» The project manager manages overall project and the en-
terprise project team focusing on scope, time, cost, risk, and
quality. The project manager works closely with the vendor
project manager throughout the duration of the project.
» The enterprise analyst is responsible for data collection,
coding and configuring tables, documenting end-user
functions, and analyzing system reports.
» Functional area managers are representatives from the de-
partments or areas that will be using the system. They
provide area-specific knowledge and are responsible for
providing input to work processes, test plans, staff training,
and policies and procedures.
» The steering committee is comprised of executive-level
representatives from various enterprise departments who
have a stake in the project. The project manager should be a
member of this committee.
» The interface analyst performs data collection, coding or
configuration, and testing for interfaces and also develops
technical specifications and test plans for interfaces.
» The network administrator evaluates and facilitates the
network level activities required by the project.
» The server administrator installs database-related software,
monitors system operations, and performs system mainte-
nance.
» The system administrator manages installation of hardware
and software required by the project.
» The desktop administrator is responsible for workstation
rollout required by the project.
» Super users provide application support to end users during
and after activation.
» Training resources (training coordinator, trainers) manage
the training process by determining training needs,
developing training plans and classes, and performing
end-user training.
Project Sponsors
Because the implementation of DMS and its components are
far-reaching in terms of organizational impact, involved and
committed sponsorship of the project is critical to successful
implementation. The sponsors of the project are the visible
champions and organizational spokespersons for the project.
The importance of their role as key communicators to the senior
leadership team and clinicians cannot be underestimated.
Project sponsorship should come from within the senior
leadership of the HIM, information technology, finance, and
clinical departments. Sponsors typically have a vested interest
in the achievement of the goals set forth in the project charter.
Because the goals of a DMS project typically range from the
tactical (such as enabling the medical record to be concurrently
accessed by multiple users) to financial (decrease the cost of
offsite storage) to technological (decrease the page to page re-
sponse time for the EHR), there usually are multiple sponsors.
Each sponsor brings unique perspectives to the oversight com-
mittee and can be instrumental in broadening the understand-
ing of the DMS throughout the organization. As decisions need

Document Management and Imaging Toolkit
18 | AHIMA
to be made that may impact the workflow of different constitu-
ent departments, project sponsors should be called upon as
negotiators who work on behalf of the project team to secure
buy-in and cooperation with necessary changes.
In addition, if the organization has organizational behavior
or change management processes, those individuals or groups
should be engaged as well to facilitate the adoption of the
process by the staff and clinicians.
Project Charter and Scope
The project charter is developed in collaboration with the
vendor and the oversight committee. This document serves as
a summary of the current environment, defined scope of the
project, goals and objectives, change control procedures, team
responsibilities, staffing requirements, project monitoring, and
escalation procedures for issues or concerns that develop dur-
ing the implementation phase. Although all components of the
project charter are important, adhering to the agreed project
scope is critical to keeping the implementation phase on time
and on budget.
The project scope is a list of items that will be addressed during
the implementation phase of the project. This list is utilized to
define specific deliverables with clarification of expectations
for each item. In a DMS project, this may include items such as
which interfaces will be developed, the types of workflow tools
that will be enabled, and the type of storage solutions that will
be implemented. There is a shared motto, “if it is not docu-
mented on the project plan, it will not be done.”
The project scope is mutually determined and agreed to by
both the vendor and the organization. It also is an important
point of reference for the duration of the project to reorient the
various teams working on implementation to the agreed-upon
deliverables for the project. Failure to maintain the project
within scope (“scope creep”) can often prolong the duration
of the project and place it over budget. Out of scope requests
that are brought forth by various constituents of the project
are often added to a future considerations list. This list is often
used post-implementation to determine needed enhancements
to the end product.
Work Plan
The project work plan is used to guide the execution of the
project. The work plan identifies tasks to be completed as a
part of the project and assigns resources to those tasks. In
addition, the work plan includes hours and durations estimated
to complete tasks, as well as the sequencing of the tasks.
The major phases of the system development life cycle (SDLC)
is the traditional way to plan and implement an information
system in an organization. The major phases of the cycle are
planning, analysis, design, implementation, and maintenance.
Conversion Options: Outsourcing
In preparing for implementation, the healthcare organiza-
tion must consider its options for converting existing files and
evaluating the staff resources available. Outsourcing may be a
consideration for the conversion process as well as providing
day-forward scanning on site.
Many organizations decide to contract with a document imag-
ing vendor to assist with processing of any scanning backlog
prior to the go-live date. While some organizations decide to
use their own staff for day-forward scanning, others decide to
totally outsource the entire scanning function including staff.
The agreement with a scanning vendor should encompass
technology and staffing for document imaging services 24
hours a day, every day. Some organizations decide to house the
vendor’s employees on site, while others decide to transport
documents to a centralized vendor location.
Testing
Prior to going live, proactive steps should be taken to test the
DMS thoroughly. Testing should be directed toward identify-
ing and addressing any configuration problems, errors, bugs in
the software, or user errors. Use a plan to ensure that the DMS
is tested in the manner for which it is intended to be used by
staff. Although the vendor may anticipate many scenarios, it is
impossible to identify every possible scenario that the organi-
zation may encounter. The plan should include exactly what
will be tested and who will be responsible. Testing is beneficial
because it:
1. Mirrors the actual production system
2. Can be done repeatedly in order to operate without failure
3. Can be done comprehensively as per design
4. Can be done by super-users who will be familiar with IT
issues
5. Allows users to play an important role in testing the system.
Note: The criteria for acceptance testing should be agreed to in
the contract prior to its execution.

Updated 2012
AHIMA | 19
Training
Training users and the leadership team is a crucial step in the
implementation of a DMS. A well-designed training program
or plan will:
» Improve the chance of the DMS being properly implemented,
» Improve users’ attitudes and behaviors toward the changes
created by the DMS, and
» Make a key contribution toward a successful conversion to a
DMS.
A training plan should identify:
» Who will be trained (users, end users, and leadership team)
» What is being covered
» How they are going to be trained (materials, handouts,
lecture, slides, and such.)
» In what format they will be trained (classroom, distance
education, etc.)
» When they are going to be trained (timeline, length of
session)
» How often training will occur (initial, retrain, refresh, or
annual)
» Costs of additional or follow-up training.
DESCRIPTION
Target Audience
•Identifywhoisgoingtobetrained(leadershipandendusers).
•Understandingtheroleoftheuserandtheirskilllevelhelpspreparethetrainerand
can provide assistance when answering questions.
Course/Class Description
•Thegoalsandobjectivesoftheclassesmustbeclearandwell-dened.
•Theobjectivesassistthetrainerindevelopingtheprogramcontent.
Trainer/s
•Technicalpeopleshouldnotbetrainers.Useaprofessionaltrainerwhoknowshowto
educate and understands adult learning techniques, learning styles, and the psycho-
logical factors that impact users’ perceptions and their ability to learn.
•Atrain-the-trainerplanmaybeadvantageouswhenpreparingtoprovidetrainingon
various shifts. The plan provides the assistance of additional trainers, which is effective
when providing many training classes to a large number of staff.
Training Setting
•Thetrainingenvironmentmustcontributetothelearningprocessbymakingsurethat
the users are physically, socially, and psychologically comfortable.
•Acomputertrainingroomisaplus.
•Sometrainingmaybedonebyadistanceeducationoptiontoallowtrainingatthe
employee’s convenience whether they are on-site or remote staff.
Schedule/Class Duration
•Numerousapplicationswillincreasetheamountoftimerequiredfortraining.This
means that users need to spend more time in class and away from their work responsi-
bilities.
•Trainingsessionsshouldbeasclosetothego-livedateaspossible.Shorter,more
frequent classes may improve the amount of information users can absorb at one time
and improve the ability to schedule staffing coverage.
•Iftrainingistobeprovidedduringworkhours,astrategywillneedtobedeveloped
for backfilling staff and clinicians while they attend the training. Considerations also
include whether these positions need to be covered by other staff, if clinicians need
to alter their schedules, and if training is provided in the evenings or on weekends to
avoid or minimize schedule disruptions.
•Ongoingtrainingandsupportaftergo-live.Userswillhaveadditionalquestionsand
need support after they have had hands-on experience with the system.
Training Plan Outline

Document Management and Imaging Toolkit
20 | AHIMA
DESCRIPTION
Training Aids
•Keepinmindadultlearningprinciplesandstyleswhencreatingeducationalmaterials.
The trainer may find that using the computer along with a workbook with procedure
steps is helpful. Handouts, reference aids, and storyboards from the vendor can be
helpful.
Evaluate
•Determinewhethertogivetheusersawrittenexamorapracticalevaluation.Evalua-
tion of the training technique provides feedback regarding the users’ reaction and the
trainers’ abilities. Post testing after training is an effective way to measure users’ skills
and knowledge. The evaluation also provides feedback regarding the ability of the users
to transfer and apply skills and knowledge learned in training to actual work setting.
Follow-up
•Follow-upduringtherstgo-livewillimmediatelyhelptheuserswiththetransferof
knowledge learned in training to the real environment. This will also provide an op-
portunity to communicate any changes that have occurred during the period between
the training and go-live.
Ongoing Training
•Trainingisongoing.TrainingdoesnotendoncetheDMSisinproduction.New
employees, new releases, new policies and procedures will create the need to review and
redefine training continuously.
•Annualtrainingshouldbeconductedasarefresherandplacewherenewideasor
processes can be shared.
Ensure that training and user manuals are readily available. One option is to have an electronic format of the manuals residing on
the healthcare organization’s intranet for easy access.
Note: The training budget and expectations should be agreed
to in the contract prior to its execution.
The Post-Implementation Phase
The DMS is live and operational and the organization is one
step closer to a complete EHR. In the post-implementation
phase, workflows will be refined, revisions will be made to
staffing and skill sets, and the process of reviewing documents
will increase. Newly created file space will require management
decisions while the project team determines how to provide
ongoing training and maintenance of the system. Finally, to
ensure the organization realizes the return on investment and
benefits promised by the DMS, take time to measure your
success. Vendor expectations in the post-implementation
environment, including costs for additional services and
support, must be clearly defined.

Updated 2012
AHIMA | 21
Case study based on interview with Suzanne
Layne, RHIT, corporate director of health
information management service at Main
Line Health, February 2012
Suzanne Layne, RHIT, is the corporate director of health
information management services for Main Line Health, a
multi-entity health system in suburban Philadelphia. She has
held several director positions in California and Pennsylvania
during her 25-year HIM career. Layne is an integral partici-
pant in enterprise record management and revenue cycle
management. She is a key member of the RAC committee, IT
steering committee, and patient safety and quality committee.
Layne has successfully installed multiple EMR systems and has
consolidated five hospitals’ HIM services into a centralized,
off- site location. An RHIT with a bachelor of science degree in
technical management, Layne is currently completing a
Master’s of Leadership Development degree at Penn State.
Introduction
Main Line Health in suburban Philadelphia is an integrated
healthcare delivery system made up of five hospitals—four
acute care hospitals and one inpatient rehabilitation facility.
Two years ago, Main Line Health went live on an electronic
(HIM) module, brought their legal health record online, and
moved to a centralized, integrated model for managing their
HIM functions.
System Design and Standardization
Across Facilities
Main Line’s goal with system design was to build once and
deploy the model across all facilities. One of their strategies was
to keep document indexing to a minimum. The acute facilities
and the rehabilitation facility met to discuss how to standard-
ize forms across facilities. Discussions included decisions like
“a progress note is a progress note no matter which facility
this is for.” Main Line started out with 28 document types for
scanning as part of this process. Two years later they have 30
scanned document types across all facilities.
Main Line also plans to implement the ability to capture the
patient’s signature directly onto an electronic form such as a
consent form. One of the biggest challenges to implement-
ing this feature is the variety of patient forms in the ambula-
tory settings. Many physicians have their own special sheet of
discharge instructions for the patient to sign. Main Line’s goal
is to standardize these forms, have them electronically signed,
and make them viewable via a patient portal.
Main Line’s plan is to have more documents electronically fed
into their document management system and thus decrease the
scanned paper over time. Right now, about 40 percent of the
patient’s record is scanned. Their goal is to have no more than
10 percent of documents scanned as more systems are set up to
feed their document management system electronically.
All documentation is now online including the forms inven-
tory. The forms inventory used to be kept in big binders which
got out of order and would often disappear. Now an online
spreadsheet houses the information and includes cross refer-
ences to ease searching. The actual forms are scanned and
attached to the spreadsheet so staff can bring up the form. The
forms spreadsheet is kept in a shared drive for all employees to
access—no printing allowed! Everyone has grown to like the
electronic solution.
Staffing Model
Main Line previously had one HIM manager at each facility for
a total of five managers. As part of their centralization, these
managers moved from their facilities to a central location and
became specialized by function rather than by facility. The goal
of centralization was to ensure that everyone had a job and was
on board with the transition. Since the transition, one manager
has resigned and the centralized HIM department now has one
director and four managers.
The four managers are now organized by function (for ex-
ample, transcription, record processing and storage, and release
of information) rather than by facility. Managers still maintain
a liaison role with the campus that they came from, but their
focus is now a function-based role. The fifth manager position
will be filled with a supervisor position focusing on release
of information around ARRA, patient portal, and regulatory
needs. Supervisors are also function-based rather than site-
based. Managers’ offices are at the centralized facility but they
spend one to two days per week visiting their campuses. Super-
visors are on site at each facility.
Part of the move to paperless records includes getting the staff
to recognize that the HIM department of the future needs to
be more technologically savvy. Main Line Health is striving
to get everyone to function using as little paper as possible.
Layne, the HIM director, has implemented paperless tools with
her staff. For example, employees use an Excel spreadsheet to
submit their time, coders clock time electronically, and vaca-
tion requests are electronic. Additionally, in their document
imaging system, coding and HIM work queues are electronic—
no stacks of paper charts waiting to be processed— charts are
online. The staff is encouraged to use critical thinking in a
virtual flow.
The EHR’s Impact on Staffing and Turnaround Times:
Centralizing the HIM Department in a Multi-Facility Environment

Document Management and Imaging Toolkit
22 | AHIMA
The staff was centralized in two phases. Anyone who did
prepping and scanning was moved to the centralized facility
in phase one. Managers, analysts, and release of information
staff moved to the centralized facility in phase two. Coders and
transcriptionists were moved home except for two coders who
chose to work on-site. The coding supervisory team is located
at the centralized location to facilitate meetings and ICD-10
planning.
There are two pay grades for employees who are responsible for
getting the medical record online. Data processing technicians
are responsible for document preparation, filing and scanning
loose sheets, sending paper records to storage, and high vol-
ume scanning. Additionally, data quality control technicians
are responsible for data integrity, quality control, and making
sure that loose material is filed correctly in the chart. Staff in the
HIM department at Main Line Health is structured to work in a
job description below their current job but not above it. Qual-
ity control technicians must be able to prep and scan, but data
processing technicians are not expected to do quality control.
Communication and Training
Communication was even more important than the project
team thought it was going to be. Nursing was notified that the
paper was going away. After go-live the HIM staff still got calls
for charts and it took a long time for the clinical staff to realize
that the legal medical record now resided in the document
management system. While there were delayed learning curves
in some areas, the HIM department reported through the chief
medical officer at the time of the transition, so the team had
great physician support. For physicians who had been practicing
for a long time and who were resistant to giving up their paper
charts, the HIM staff did one-on-one training.
The management team also found it was very important to
communicate early and often with the HIM team to ease
unrest and answer questions. Looking back, managers realized
they should have had more formal communications early on.
Later in the program they implemented a newsletter titled On
the Same Page, which helped to keep the staff informed.
Main Line did not want to reduce or eliminate staff with their
move to the online health record. Everyone got a job in the new
structure and 94 percent of the staff got the job they wanted.
Also, new positions were created as part of the centralization.
An assistant system administrator position was created at each
facility since the HIM managers were all located at the central
offices. Additionally, two lead positions were created at the
central location—one over document processing and one over
quality control.
The staff was given homework assignments to help with their
scanning education. Two weeks of homework was assigned
before go-live. Staff was asked to scan inpatient and outpatient
test batches. In addition to training the team, the homework
did uncover some unexpected backend workflow issues. For
example, a lot of forms were not bar coded in the behavioral
health center and discharges were not being sent over in a
timely manner. The goal was to scan all paper 24 to 48 hours
post discharge.
Since the go-live of the new system, many of the staff have
shown a renewed interest in returning to school and learning
new technology. Staff benefits include tuition reimbursements
and ability to participate in satellite classrooms. Main Line
Health has established a relationship with higher education
schools in their area, and they are able to provide their staff
with continuing education opportunities right at their facility.
Storage and Destruction of Paper Records
Main Line Health’s policy is to store the paper record for six
months after the quality control process for the online record
is complete. Main Line Health would like to reduce the length
of time they retain paper to 90 days eventually. The director
of safety and risk, in-house legal counsel, and the compliance
officer do not feel that the HIM staff is ready for this yet. One
challenge that the HIM department is still trying to overcome
is improving scanning reliability. For some employees, a 100
percent quality check of scanned images is still needed while
for other employees a sampling or spot check is sufficient. The
goal is to be able to move to a sample quality check for all
scanning specialists.
Once the paper has been scanned it is shipped to a short-term
storage facility located at one of the Main Line properties. Ev-
ery month a truck comes to this property and shreds any paper
that is seven months old or older.
Main Line Health chose not to back-scan paper records prior
to the implementation of their document imaging system.
They have a separate off-site storage facility for the legal medi-
cal records that are still in paper form.
Benefits of Centralization and Online Records
The biggest benefits that Main Line Health realized with their
move to an online record were reclaimed real estate and the
cross training of teams.
Main Line Health’s centralized HIM department is now housed
in an off-site facility that is much less costly than the previous
real estate each HIM department occupied at the individual
Main Line Health facilities. That unoccupied real estate at the

Updated 2012
AHIMA | 23
healthcare facilities has quickly been spoken for. One facility
has been able to build a large expansion to their outpatient car-
diology services area due to the HIM department moving out.
There is now more parking for patients at each facility since
HIM staff have moved off-site.
Also, moving 10,000 square feet of HIM space out of the care-
givers’ area to real estate that does not need to be accredited by
the Department of Health (since no care is given), has been a
huge cost savings for the healthcare institution. In addition, the
centralization of the team has led to a further cost savings due
to a reduction in equipment needed. For example, only one
supply cabinet is needed, and the team is able to share supplies
such as toner, paper, and rubber bands where previously these
had to be maintained for each facility.
With all HIM resources in one location, Main Line Health
has been able to standardize jobs across facilities. The oldest
records are scanned first, no matter from which facility. This
allows staff to get all documents scanned within 24 to 36 hours
of the record’s arrival at the central facility. Records arrive first
thing in the morning from each of the sites. Every day a courier
delivers yesterday’s inpatient discharges along with records of
outpatient and emergency room visits. More than 95 percent
of yesterday’s records arrive in that one delivery, so the HIM
department no longer gets a delivery later in the day. Each site’s
records are color coded so that staff can tell from which facility
a record originated. HIM staff is organized into functional
teams by color, and each team has a team captain. Team
captains are rotated between teams and also given
some supervisory responsibility and encouraged to promote
collaborative spirit across teams. With this approach, Layne has
found that her teams are now starting to self-correct issues and
are realizing when to ask for assistance from a leader.
Improved Metrics
Another area where Main Line Health has enjoyed huge im-
provements is in HIM department metrics. Analysis time has
decreased significantly across all facilities. Before centralization,
one site had pretty good turnaround times—about three to five
days. Another facility struggled with 10-day turnaround times
and yet another averaged between 15 and 23 days. Now all
records from all facilities are scanned into the system within 24
to 36 hours and have undergone analysis within 48 hours. Four
staff members monitor and maintain the analysis and reanaly-
sis queues for all five facilities. Physicians receive records to
complete within two to three days of discharge. Dictations now
flow in real time—they are available on the physician’s online
work-list as soon as they are dictated. Due to the real-time
dictations, by the time records reach analysis, a large percent of
chart deficiencies are already complete.
Prior to implementing their online medical record, Main Line
Health’s chart delinquency rates were in the high 20 to low 30
percent range. Delinquency rates are now in the two to four
percent range. In addition to faster analysis turnaround times,
deficiency letters are e-mailed to physicians so they receive
them more quickly. Online medical records are available any-
where, anytime, so records can be completed remotely. Physi-
cians can access their records from the floor if they have a few
minutes between cases or even when they are on vacation.
Overall, Main Line Health has seen many benefits to imple-
menting one electronic medical record across all facilities and
centralizing HIM operations. They have reclaimed real estate
to be used for patient care, cross-trained their staff and their
management team, recognized economies of scale in one
department for all five facilities, and have greatly improved
their department metrics. But perhaps their biggest gain is the
collaborative spirit and the insight into planning for the future
of the ever-changing healthcare environment.

24 | AHIMA
Document Management and Imaging Toolkit
Notes
1. IOD Incorporated. “Improving Outcomes in Document
Imaging and Conversion: New Methodologies to Measure
Scan Capture Performance in HIM.” 2011. Available at www.
iodincorporated.com/wp-content/uploads/2011/09/
FINAL-QPI-WHITE-PAPER-11-8-11.pdf.
2. AHIMA. “Amendments in the Electronic Health Record
Toolkit.” 2012. Available at www.ahima.org.
References
AHIMA. “Managing the Transition from Paper to EHRs.”
(Updated November 2010.) Available in the HIM Body of
Knowledge at www.ahima.org.
AHIMA. “Migrating from Paper to EHRs in Physician Practices.”
Journal of AHIMA 81, no.11 (November–December 2010): 60-
64. Available in the HIM Body of Knowledge at www.ahima.
org.
AHIMA. Pocket Glossary of Health Information Management
Technology. 3rd ed. Chicago, IL: AHIMA Press, 2012.
AHIMA. “Retention and Destruction of Health Information.”
Updated August 2011. Available in the HIM Body of Knowl-
edge at www.ahima.org.
AHIMA e-HIM Work Group on Electronic Document
Management as a Component of EHR. “Electronic Document
Management as a Component of the Electronic Health Record
(AHIMA Practice Brief).” October 2003. Available in the HIM
Body of Knowledge at www.ahima.org.
AHIMA Task Force on Healthcare Quality and Patient Safety
“HIM Functions in Healthcare Quality and Patient Safety.”
Journal of AHIMA 82, no. 8 (Aug 2011): 42–45. Available in the
HIM Body of Knowledge at www.ahima.org.
Amatayakul, Margaret K. Electronic Health Records: A Practical
Guide for Professionals and Organizations. 4th ed. Chicago, IL:
AHIMA Press, 2009.
Brodnik, Melanie S., Mary Cole McCain, Laurie A. Rinehart-
Thompson, and Rebecca B. Reynolds. Fundamentals of Law for
Health Informatics and Information Management. Chicago, IL:
AHIMA Press, 2009.
Dooling, Julie. “Managing Records between the EDMS and
EHR: Monitoring, Evaluating, and Redesigning Workflows.”
Journal of AHIMA 82, no. 2 (February 2011): 38–39.
Johns, Merida. Health Information Management Technology: An
Applied Approach. 3rd ed. Chicago, IL: AHIMA Press, 2011.
LaTour, K.L., and S.E. Eichenwald Maki. Health Information
Management: Concepts, Principles, and Practice. 3rd ed.
Chicago, IL: AHIMA Press, 2010.
Rinehart-Thompson, Laurie A. “Record Retention Practices
among the Nation’s ‘Most Wired’ Hospitals.” Perspectives in
HIM 5, no. 8 (June 2008): 1–15. Available at http://perspectives.
ahima.org.
Servais, Cheryl E., Neil S. Olderman, and Kelly A. Trahan. The
Legal Health Record. Chicago, IL: AHIMA Press, 2008.
Walsh, Tom, et al. Medical Records Disaster Planning, A Health
Information Manager’s Survival Guide. Chicago, IL: AHIMA,
2009.
Warner, Diana. “The EHR’s Impact on Staffing Models.”
Journal of AHIMA 82, no. 9 (September 2011): 44–45.

AHIMA | 25
Prepping
» Confirm patient name, medical record number, and
account number on each page. This information should be
documented on both sides of the page for best practice and
patient safety.
» Place all “like” document types together in chronological or
reverse chronological order (dependent upon organizational
policy).
» Repair all torn or wrinkled pages.
» Remove all staples and clips from each page.
» If applicable, remove NCR copies and keep the originals.
» Original documents that are not legible should be stamped to
indicate “poor quality.”
» Third party barcodes should be blacked out or covered to
prevent the application from reading the barcode incorrectly.
» Perforated forms should be torn apart for scanning or kept
intact and oversized document settings should be used in the
scanning process.
- By tearing apart perforated forms, the entire batch can be
scanned under one document size setting.
- Some technology can sense the difference between legal size
documents (8 ½ x 14) and letter size (8 ½ x 11) documents
and adjust accordingly. This option should reduce the
up-front documentation preparation time.
- Most scanners have a maximum setting available, and the
scanner will detect the width and length that the input of
the scanner can accommodate.
- Oversized documents must be scanned under the appro-
priate oversize setting. They can be scanned in the same
batch; however, they should be placed at the beginning or
end of a batch, and the paper size setting must be changed.
Although scanning time is interrupted with this process,
manual indexing can be avoided.
- Booklets and “foldouts” (such as nurses’ flow sheets) should
have a perforation at the “bound” or “foldout” edges for
ease of separation into 8 ½ -by-11-inch pages during
scanning preparation.
- Some foldout forms have a data column on the fold. These
forms must be redesigned so that the perforation or “cut-
out” is not on the data column. Note that a minimum inch
(1”) “neutral zone” on either side of the perforation or “cut-
line” is recommended to ensure data is not lost.
» White paper is recommended for all documents that will be
scanned because white will provide the best results for bar
code identification, optical character recognition (OCR),
viewing, and such.
» Shading of “bars” that contain text is not recommended
because the text typically will not be readable after scanning.
» If colors are required for ease of manual identification, a
color border around the edge with a white center is recom-
mended.
» A minimum of 20 lb. weight bond paper is recommended for
best scanning results.
» 24 lb. weight is recommended for double-sided forms to pre-
vent bleed-through of ink and information during scanning.
» Do not use glue on the leading edge of a form. The edge that
has been separated curls and will be misfed into the scanner.
Also, the glue will build up quickly on the rollers and cause
jamming.
» Note that portrait docs will typically be three-hole punched
at the top so they can be put into a medical record chart
holder (left-hand side of landscape docs will be three-hole
punched).
» Holes across the top of a page could result in paper not being
fed properly or paper jams if the holes have been ripped and
are not taped.
» Note potential for three-hole punch on left side of some por-
trait docs (and the tops of some landscape docs) for standard
three-ring-binder applications.
» When designing forms, it is important to not place informa-
tion on the “back” side of the page in the same area as the bar
code is on the opposite side. This could bleed-through during
scanning and cause the bar code to be unreadable on the
scanned image.
» Avoid small type; 8 point or larger is recommended.
» If applicable and available, encounter or batch cover sheets
as well as visit cover sheets for each record (visit or account)
should be utilized:
» Encounter or batch cover sheets will identify the batch, the
patient and the encounter to where the scanned document
will be indexed.
» Visit cover sheets will identify the existence of several visits or
encounters in one batch.
Best Practices: Preparing and Scanning Documentation
Appendix A

26 | AHIMA
Appendix A
Capture and Scanning Process
» Always verify scanner settings before scanning pages.
» Batches may be scanned vertically or horizontally. Remember
to select the correct barcode orientations when scanning ver-
tically or horizontally if not using enhanced barcode recogni-
tion. If you do not select it correctly, bar-coded documents
may not be read, resulting in the batch requiring manual
indexing.
» It is recommended that a batch not exceed one inch in thick-
ness, or 100 pages, to allow for timely processing of the batch
and to reduce the amount of rescan if an error occurs.
» Interactive scanning and document modification
- Is used mostly for rescanning or replacing documents.
Usually a lower speed or flat-bed type scanner to especially
handle odd-sized documents.
- Is recommended with the use of a smaller desktop scanner
for loose sheet or point of service scanning because of the
delay in the start of scanning on larger models.
» Loose material is commonly scanned under a batch header
sheet and is manually indexed if account number bar-coding
is not used on forms.
» Determining the most appropriate scanner settings can be a
very time consuming process. It is important to create a batch
that contains a variety of forms commonly found in a medi-
cal record at the institution. This batch can be used to test
and modify the scanner settings to achieve the most legible
images.
» It has been found that EKGs are more legible if scanned on
a low speed scanner using grey scale or color settings. New
high-speed scanners have provided sufficient quality for
scanned EKG images.
» Simplex (single-sided) mode scanning should only be used if
all the documents within the batch are set up as single-sided
documents in the scanning software. All blank back page
sides of the page will be ignored and deleted without requir-
ing manual intervention. If simplex mode is used on a batch
with two-sided documents, the outcome typically results in
having to rescan the entire batch.
» Some scanning teams set the scanner timeout to zero so
that it never times out, reducing the chance for unnecessary
downtime. Scanner timeout settings can be different based
on your scanner model.
» If you have a jam or a timeout on the scanner, scanner
settings should be verified.
» Maintenance on the scanner depends on the amount of paper
scanned in a day. To assist with high quality scans, daily tasks
(or following each shift) should include vacuuming the
scanner and cleaning the rollers and image guides.
» Fly paper, alcohol free pads, a soft clean cloth, and a vacuum
are some of the cleaning supplies you can use. It is important
to follow the maintenance and cleaning regimens that are
recommended by the scanner manufacturer.
» Use antistatic mats under all scanners that stand on the floor
directly to reduce the amount of friction generated.
» Calibrate scanners at least daily using proper calibration
paper.
» Hole-punched documents periodically jam the scanner. This
is caused by the placement of the hole on the page and how it
passes over the scanner cameras. For that reason, some scan-
ning teams scan landscape on the clean (not punched) edge.
» To assist the rollers in pulling one sheet at a time through the
scanner, scan operators should fan the batch before placing it
into the feeder.
» It is an option to end each job, let the scanner time out after
each batch, or continue placing batches in the scanner until
all are scanned. Each institution must determine which is
more efficient for the staff and environment based on the
scanner model.
» When scanning a batch that contains the same document
type but different patients, it should be possible to print
batch header sheets from the system that include the
document type on the page. This allows the indexing team to
select certain batches if there is a large backlog of a particular
document type.
» When using multiple barcodes (account, MRN, or document
type), batch header sheets should not be needed. Proper
barcode configurations, document type, and MRN/Visit
persistence modes are required for accurate auto-indexing.
» A mnemonic descriptor or inventory number may be used in
systems that do not recognize bar codes.
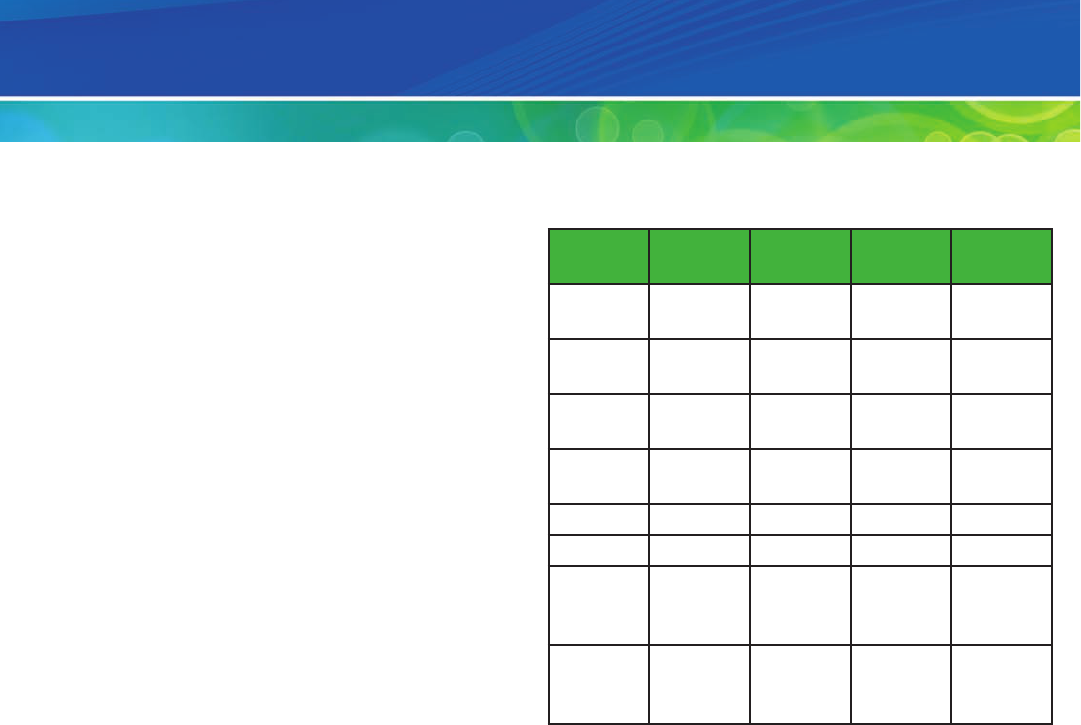
AHIMA | 27
The following are concepts related to document imaging:
» Network connectivity: Storage devices accessible from any
point on a network
» File system: The actual logical file allocation and storage
structure, how a database stores its information for retrieval.
Typically optical disks required a specialized, proprietary file
system to manage the optical platters and jukeboxes along
with magnetic storage.
» Hierarchical storage management: The management of
information through the use of multiple devices that handle
the information at different points in its life cycle. An
example might be to place the documents on magnetic,
move them to optical, and later archive the optical to tape.
» Backup and redundancy: The mechanisms, both hardware
and software, that keep copies of documents and system
information to ensure data recovery upon catastrophic sys-
tem failure or data loss
» Direct attached storage: Magnetic storage that attaches
directly to a server, not necessarily through a network
» Application service provider (ASP) based storage:
Managing documents and information via web access on
servers and remotely located storage devices
Performance Implications
Choosing a document format requires a balance between
performance, image quality, and storage limitations. If we use
the page sizes described above, you can expect the following
amount of data to flow through your network. We will assume
that we have documents that are two pages in length.
File Sizes
The following is a sampling of scans performed using a desk-
top Fujitsu fi-4120C scanner. Photoshop Elements was used
to accept the image from the scanner and encode it with the
appropriate format. The application used to encode an image
does not affect the actual size of the image as the calculation ei-
ther follows a precise algorithm (such as BMP) or a proprietary
compression algorithm (such as PNG). These sizes represent a
single-sided medical form. For multi-paged documents, take
the file size number (below) and multiply it by the total num-
ber of pages.
Color
Mode
Paper
Size
DPI File
Format
File Size
(KB)
24-Bit
Color
8.5x11 150 JPG/M
Quality
345
24-Bit
Color
8.5x11 150 JPG/H
Quality
1,090
24-Bit
Color
8.5x11 100 PNG 593
24-Bit
Color
8.5x11 200 PNG 1,341
B&W 8.5x11 200 PNG 66
B&W 8.5x11 300 PNG 127
B&W 8.5x11 200 TIFF
CCIITT
G4
45
B&W 8.5x11 300 TIFF
CCIITT
G4
95
Software applications have limited opportunities to reduce the
actual storage size of an image; however, they can improve or
degrade the quality of the image. Many vendors use the VRS
(Virtual Rescan) software published by Kofax Inc. to perform
barcode reading and to auto-improve the document before
the software receives it. The document is often significantly
improved before being stored. If you compare the scanning
results of Photoshop versus the files enhanced by Kofax VRS,
it will be found that those documents have better quality.
Storage Requirement Calculations
How do you calculate the storage requirements for a
particular format?
To answer this question, there is a series of calculations in
order to estimate storage. A color bit map file format (BMP)
size is calculated as follows:
Scan Width 8 inches
Scan Height 11 inches
DPI 150 (Dots Per inch)
Pixel Width 8 in X 150 DPI = 1,275 pixels
Pixel Height 11 in X 150 DPI = 1,650 pixels
Color Depth 24 Bit
Pixel Total 1,265 X 1,650 = 2,103,750
Document Storage Options and File Size Calculations
Appendix B

28 | AHIMA
In addition, color depth must be considered. The color depth
above (best quality) is 24 bit. Since there are 8 bits in a byte, we
have 3 bytes, or a color depth of a factor of 3. This means that
it takes 3 bytes to store every pixel. To calculate the final size of
this bit map, we multiple the pixel total, which is 2,103,750, by
3. The final size of this image would be 6,311,250 or roughly
6 megabytes (MB). This same file saved as a BMP color 16 bit
would be roughly 4MB because the bit depth would apply a
factor of 2 (color depth) to the total pixel count
How do you scan and store a 150 DPI color JPEG and have a
file size of 300KB or 300,000 bytes?
The answer is compression. The JPEG image format compress-
es the image pixels by combining like pixel colors and “remem-
bering” where they go. The higher the compression ratio, the
smaller the size but more data is removed. So, if you started
out with 6,311,250 bytes and reduced it down to 300,000 then
you effectively removed 6,011,250 bytes of data. When you are
working with photographs, compression is often easy because
there are so many like colors and repeatable patterns. Scanning
a text-based document, then storing it in JPEG format some-
times proves to be problematic because of the data loss and
precision required. If a person was reading a glucose level of
190 as 100, that might be a significant problem for clinical care
or medical research.
When saving to a JPEG file format, select the compression
factor to apply. Most software applications display the choice as
Low, Medium and High with degrees of precision in between
each category.
Every image format uses a different compression mechanism.
From an industry perspective, TIFF with G4 compression
or PNG is recommended for text-based documents. JPG is
recommended for photographic images.
It is important to note in the following chart that the file sizes
are per page. Multiply the individual page size by the number
of pages in the document to determine total storage space
required.
Color Format
DPI
DPI Page Size
(KB)
SAN size
for 10MM
Pages
B&W PNG 200 50 0.5 TB
B&W PNG 300 100 1 TB
Color24 PNG 150 650 6 TB
Color24 PNG 200 1,481 14 TB
Color24 JPG/6 150 275 2.5 TB
Color24 JPG/8 150 350 3.3 TB
Color24 JPG/12 150 830 8 TB
B&W PNG 200 50 0.5 TB
Appendix B

AHIMA | 29
Code 39 Supports the Following Characters:
» Twenty-six uppercase letters (A through Z)
» Ten digits (0 through 9)
» Seven special characters: minus sign (-), period (.), dollar
sign ($), forward slash mark (/), plus sign (+), percent sign
(%), and space ( )
» Start and stop characters, represented by an asterisk (*)
Code 39 Is in the Following Format:
» A leading “quiet” (blank) zone
» The start character (*)
» Data characters, with characters separated by an
inter-character gap (blank space)
» The stop character (*)
» A trailing “quiet” (blank) zone
Two-dimensional (2D) Matrix Barcode:
» Encodes text or raw data in a pattern of black and white
square modules
» Usual data size is from a few bytes up to 2 kilobytes.
» By adding error correction codes (according to the ECC200
standard) the symbols can be read even if they are partially
damaged.
» Technical Data
- Normative standards: The normative standards for the Data
Matrix barcode symbology are called ISO/IEC 16022:2000
and ISO/IEC 24720:2006 (ISO International Standard).
- DataMatrix data capacity: A single DataMatrix symbol can
theoretically hold up to 3116 digits, 2335 alphanumeric
characters, or 1556 bytes. Due to internal data compression
algorithms the exact data capacity depends on the struc-
ture of the data to be encoded. The maximum Data Matrix
capacity is also influenced by available printing space and
the printer resolution.
- The default character set is Latin-1 or ANSI ASCII (equiva-
lent to ECI 000003).
- Data Matrix supports the ‘Structured Append’ feature. Up
to 16 DataMatrix symbols can be concatenated (linked).
If a scanner or decoder supports this feature, it returns the
concatenated data content in the correct order.
- Data Matrix printing quality: To optimize barcode quality a
DataMatrix symbol should not be printed with dots smaller
than 4 to 5 device pixels.
Bar Code Content
If standard forms are currently identified using a numeric
or alphanumeric character string (such as MC1234), then
configure the imaging bar code using that same numeric or
alphanumeric string.
Bar codes can be used to identify the document or encounter
number.
Placement of Bar Codes on Forms
When determining bar code placement on a form, it is
important to consider the location of any addressographs or
stick-on labels that may be applied to each document type.
Also, the bar code may be preprinted on a form or printed on
an adhesive-backed label that is manually applied to the form
prior to scanning. There should be one bar code per form, and
it should be placed in an area with the proper leading and
trailing quiet zones as previously described. If the form’s
corners will be susceptible to wear, curling, fraying, or tearing,
placement in these areas should be avoided.
» A unique bar code is recommended for the front page of
every document that will be scanned and indexed. This means
- A unique bar code must be on the front side of a duplex
document (required to ensure both sides [image] are
properly indexed in the correct page order).
- A unique bar code must be on the front side of a multi-page
document (required to ensure all sides are properly
indexed). Length of document is determined by a setup value.
- A bar code is not required on the back (“ blank” ) side of
simplex documents, as these pages may be scanned in a
batch that is being scanned in duplex mode, but they will
not be indexed.
- All bar codes should be oriented to the same direction,
either parallel to the direction that the paper travels or
perpendicular. This will make scanning and reading of the
bar codes more efficient and consistent.
The bar code must be surrounded on all sides (above, below, to
the left, and to the right) by at least 0.25 inches of blank or clear
space. This blank space comprises the leading and trailing “quiet”
zones discussed in the preceding section of this document.
Print sample bar-coded forms to use for testing. If the location
of the bar code is causing difficulty, reposition it. Each form
should be scanned 30 to 50 times to test for a successful read-
ing. Only when you are satisfied that a code and orientation is
correct, and has been successfully tested multiple times, should
you conduct a full form redesign and printing.
Bar Code Information and Guidelines
Appendix C
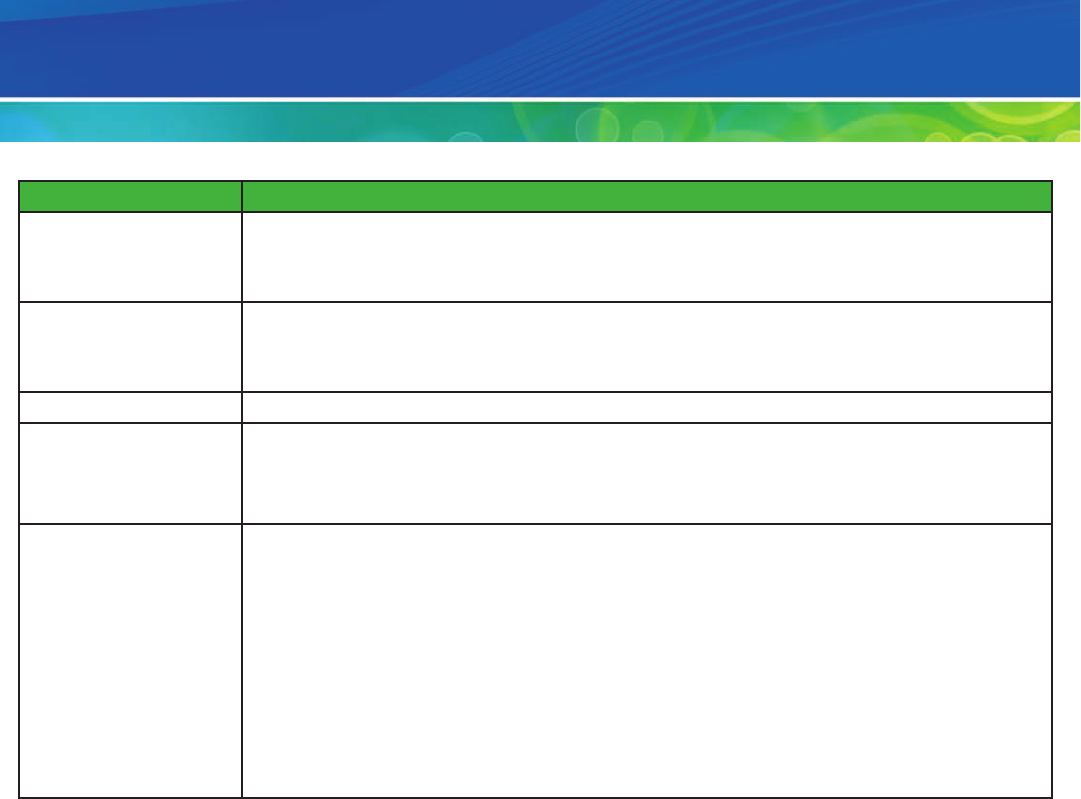
30 | AHIMA
Appendix D
Prepping
Skill Set Traits
» Quick hand-eye coordination
» The ability to detect errors, locate certain information on any type of document, and quickly
organize them by alphabetical or chronological order without error
Level » Entry level
» Prepares documents for scanning into the electronic document management system. Examines
pages and verifies patient identification on each page.
Education » High school graduate or equivalent with GED
Experience » Experience in health information management department preferred
» Good oral communication skills
» Basic computer skills preferred
Required Skills » Knowledge of health record format and content for all visit types
» Ability to examine the record and verify patient identification
» Ability to examine a form and determine its proper placement within the record
» Ability to identify nonstandard forms and determine action required
» Ability to navigate the patient registration system
» Ability to push or lift up to 30 pounds
» Detail oriented
» Ability to evaluate and process a certain volume of documents per hour (set forth by organization)

AHIMA | 31
Appendix D
Prepping
Core Competencies » Verify the chart remains in the appropriate order.
» Check that documents contain appropriate patient identification (Account Number, MRN or Last
Name, First Name).
» Remove any interfaced or electronically generated documents (those that do not contain changes
or hand-written notes added), per defined document rules determined during the implementation
process.
» Accurately assign index as outlined in the Document Matrix.
» Remove any remaining staples, paper clips, and other binding materials from all pages.
» Repair tears, holes and rough edges with transparent tape.
» Put tape over sticky materials.
» Unfold bent corners, and straighten curled edges.
» For any documents on card stock or manila, such as Kardex or ambulance run sheets, make a photo-
copy before scanning.
» Divider tabs or stickers that may “hang” over the edge of the document may be cut off, per defined
document rules determined during the implementation process.
» Duplicate copies will be identified as trash or ‟not to be scanned.” Staff will follow established proce-
dures for these documents, typically either placing in shred bin or at back of chart.
» Mount and tape down any sheets less than 8.5 by 11 inches on an 8.5-by-11-inch sheet.
» For sheets with rhythm strips or other mounted documents, tape down the top of the strip so it
does not catch in the automatic document feeder (if you will be scanning in “Portrait” mode).
» Perforate and number multipage forms into single pages so as not to destroy any information.
» Documents that are of poor quality and may not scan well will be marked with a Poor Quality
Original (“PQO”) stamp.
» Verify 100 percent of patient name, MRN, and account number at the start of every chart and on
every page in the record, front and back.
» Verify 100 percent of episode or encounter numbers at the start of every visit.
» Provide 100 percent quality check for proper patient identification and document irregularities.
» Arrange multipage documents in date order, either chronological or reverse chronological, per
department guidelines.
» Ensure all pages are in the same proper orientation.
» If a document is identified as likely to result in poor image quality once scanned, photocopy the
document, adjusting the copy contrast (lightness and darkness). This may help improve the quality
of the scanned image. If improvement is not noted, follow departmental guidelines for processing
poor-quality originals.
» Once all documents are prepped for scanning, clip them together, and place them at the front of
the folder. Set them aside until you are ready to deliver them to the scanning staff. Segregation
of these documents in the folder allows all of the record to stay together (that is, in the patient’s
folder), and the scanning staff can select only the part of the record that is to be scanned.

32 | AHIMA
Scanning
Skill Set Traits » Quick hand-eye coordination
» Ability to read moving objects and if possible, have experience with scanning equipment
Level » Entry level
» Scans documents into the electronic document management system. Examines pages and
verifies patient identification on each page. Appropriately batches documents. Maintains
scanning equipment
Education » High school graduate or equivalent with GED
Experience » Experience in health information management department preferred
» Good oral communication skills
» Basic computer skills preferred
Required Skills » Knowledge of health record format and content for all visit types
» Ability to examine the record and verify patient identification
» Ability to examine standard and nonstandard forms and determine their appropriateness for
inclusion in the health record
» Ability to perform troubleshooting, routine maintenance, and adjust settings on the scanning
equipment
» Ability to perform computer functions
» Good hand-eye coordination
» Good verbal communication skills
» Ability to push or lift up to 30 pounds
» Detail oriented
» Ability to evaluate and process a certain volume of documents per hour (set forth by organization)
Appendix E

AHIMA | 33
Appendix E
Scanning
Core Competencies » Perform daily maintenance of the scanner
» Calibrate the scanner for proper image quality
» “Fan” the stack of documents to be scanned in order to make sure the documents separate easily
and that any previous hole punches or stapled pages do not stick together. Purpose: reduce the
number of automatic document feeder misfeeds.
» Once records are scanned, remove them from the scanner’s out tray. Begin process of verifying the
quality and accuracy of the scans. With the records face-up, view the hard copy and the scanned
image to confirm all images can be read and all pages were captured. This can be done by flipping
through the hard copies as you verify each image, page by page. Purpose: Reduce the number of
rescans as a result of poor image quality or skipped pages.
» As images are reviewed, change the rotation, switch sides, and the like, as needed. For example,
documents that are typically viewed in “landscape” orientation should be rotated so they pres-
ent to the end user in landscape mode. If a document was sent through the scanner so that the
back page was scanned as the front page, switch sides to put the images in the appropriate order.
Purpose: Improve the readability and use of the images by the end user.
» If an image is identified as poor quality, adjust the scan sensitivity or use the copy machine to
enhance the quality of the document to be scanned. Once the scan sensitivity is changed or the
document is enhanced via the copy machine, re-place the image. Purpose: Reduce the number of
records returned for rescan as a result of poor image quality.
» Once initial quality review has been completed, transfer the folder to Assign Document ID.
Clip or bundle the hard-copy pages together and forward them for document ID assignment.
Purpose: The process of document ID assignment will provide a second review to identify
issues with image quality or skipped pages. The hard-copy record must be available in order to
accomplish this.

34 | AHIMA
Appendix F
Indexing
Skill Set Traits » Able to identify objects and detect errors quickly
» Good computer skills
» Proficient with 10-key entry and typing
Level » Intermediate level
» Manually indexes documents to the correct level as established by facility policy. Minimizes
duplicate records and overlap entries. Verifies data integrity. Coordinates information with master
patient index, patient registration modules, and various other ancillary departments and modules
Education » High school graduate or equivalent with GED
» Associate degree: RHIT preferred
Experience » Experience in health information management department preferred
» Good oral communication skills
» Basic computer skills preferred
Required Skills » Knowledge of medical record format and content for all patient records
» Competent knowledge and understanding of anatomy
» Competent knowledge of medical terminology
» Ability to review record and verify patient identification
» Strong computer skills
» Good verbal, written, and computer communication skills
» Ability to perform job function and make decisions without direct supervision
» Detail oriented
» Ability to evaluate and process a certain volume (encounters, sections, or documents) per hour
(set forth by organization)
» Ability to interact with customers

AHIMA | 35
Appendix F
Indexing
Core Competencies » Monitor the manual indexing queue of unassigned images.
» Prioritize the batches in the queue and retrieve the batches for processing.
» Confirm that all records ready for indexing have been received.
» Review each electronic image within the batch. Compare with hard copy to confirm image
quality, appropriate order and appropriate rotation.
» Determine the correct patient name, medical record number, account number, document type,
or section (if appropriate).
» Index the image (encounter, section, or document) appropriately by required patient data
elements according to facility specific guidelines.
» Review and determine if image should be
- Added as a new document to an existing record
- Replacing a page within an existing record
- Deleted
» Bar code recognition of the client’s documents
» Optical mark recognition
» Advanced forms recognition
» Automated forms classification
» Manual key entry of data
» 100 percent Quality Review of indexing parameters and patient identification
» Delete episodes when applicable.
» Add episodes when appropriate.
» Revise episodes when appropriate.
» Relocate episode when appropriate.
» Return for re-scan any images not appropriate for permanent storage.

36 | AHIMA
Appendix G
Review and Quality Control
Skill Set Traits » Able to identify objects and detect errors quickly
» Good computer skills
» Proficient with 10-key entry and typing
Level » Intermediate level
» Reviews the electronic document management system and records contained within for
appropriate image quality and indexing
Education » Associate degree: RHIT preferred
» High school graduate or equivalent with GED
Experience » Minimum of three years HIM experience (mandatory) or associate degree: RHIT
» Good oral and written communication skills
» Basic computer skills
Required Skills » Knowledge of medical record format and content for all patient records
» Competent knowledge and understanding of anatomy
» Competent knowledge of medical terminology
» Ability to review record and verify patient identification
» Strong computer skills
» Good verbal, written, and computer communication skills
» Ability to perform job function and make decisions without direct supervision
» Detail oriented
» Ability to evaluate and process a certain volume (encounters, sections, or documents) per hour
(set forth by organization)
» Ability to interact with customers

AHIMA | 37
Appendix G
Review and Quality Control
Core Competencies » Determine the readiness of the batch for the quality control process
» Locate the electronic document for verification against the paper batch
» Review each image in the batch and verify the following:
- Correct patient name and account level
- Proper indexing level (encounter, section, or document)
- Image quality (readable, orientation, multiple sides, double-feeds, etc.)
» For each page scanned or indexed with errors
- Rearrange out of order images within the electronic document;
- Relocate electronic images that are incorrectly filed in another document;
- Relocate electronic images or documents that are incorrectly filed in an encounter;
- Replace electronic images that have unacceptable image quality or have been updated; and
- Modify the indexing as appropriate.

38 | AHIMA
Document Management System (DMS) and Electronic Health Record (EHR)
Points of Integration
The table below displays some important
technical considerations for integrating
a document management system (DMS)
with the electronic health record (EHR).
It is organized by function and area of
administration.
The integration points are grouped by
functionality and by the organizational
area responsible for building, imple-
menting, or administrating them. Some
integration points have been duplicated
across administrative areas to indi-
cate the need for inter-organizational
coordination or to suggest the most ap-
propriate administrator(s) to build and
monitor a particular function. However,
this will vary from organization to orga-
nization.
It should be noted that the integration
points listed are not intended to be an
exhaustive list, but rather a general set
of high-level considerations that an
organization could use to coordinate
an implementation plan or an ongoing
maintenance plan for most EHR/DMS
system configurations.
Appendix H
continued on pages 39

AHIMA | 39
DMS and EHR Points of Integration (cont.)
Appendix H
continued on pages 40
Functions
Areas of
Administration
Interfaces/HL7
Messaging Scanning
Document,
Note and
Transcription Type
Development and
Reconcilliation
HIM Chart
Completion
Viewing Scanned
Documents
Release of
Information
IT/Network/
Desktop/
Hardware
Administration
» Identify and
map all inbound
and outbound
message types
for ADT and
MDM messages
in interfaces
middleware
» Consider needs
for order-level
scanning mes-
sages (if used)
» Consider merge,
unmerge, and
overlay messages
for MPI
reconciliation
» User Active
Directory setup
(if required by
system)
» Consider client/
workstation vs.
Citrix deploy-
ment approaches
» Scanner drivers
set up/push
» Imaging software
and associated.
files package set
up and push
» Consider PC
performance
requirements
» Digital photo
capture set up (if
supported)
» Consider
support or help
desk needs
» Consider
downtime/
DR measures for
scanning and
hardware main-
tenance
» Set up and verify
translation (or
similar) tables
» Provider or HIM
user security or
Active Direc-
tory set up (if
required by
system)
» Citrix server set
up and replica-
tion
» Workstation
profile set up
» User security/
active directory
build (if required
by DMS)
» Consider image
rendering latency
times
» Consider PC
vs. thin client
performance
» Consider down-
time or DR
measures for
viewing scans
» Print server con-
figuration/setup
» Consider how
print files will be
saved/retrieved
on network
drives
» User security/
active
directory build
(if required by
DMS)

40 | AHIMA
Appendix H
Functions
Areas of
Administration
Interfaces/HL7
Messaging Scanning
Document,
Note and
Transcription Type
Development and
Reconcilliation
HIM Chart
Completion
Viewing Scanned
Documents
Release of
Information
EHR
Administration
» Identify/map all
inbound,
outbound mes-
sage types for
ADT and MDM
messages for
EHR integration
and build
» Consider ap-
propriate patient
encounter types
and statuses used
» Determine MPI
reconciliation
workflow
» Consider setup
needed for
scanning if
initiated from
EHR (custom
buttons,
executable
paths, API
configuration,
.ini, .xml files,
etc.)
» Build/set up of
document,
transcription
and note types
» Consider set up,
mapping and
placement of
scanned
document
links in
clinical views
» Build/set up of
document,
transcription
and note types
» Consider set up,
mapping and
placement
of scanned
document links
in clinical views
» User security
setup
» Verify set up
and mapping
of scanned
document links
in clinical views
» Print server
configuration/
setup
» Determine
scanned
document type
inclusion/
exclusion criteria
» User security set
up
DMS and EHR Points of Integration (cont.)
continued on pages 41

AHIMA | 41
Appendix H
Functions
Areas of
Administration
Interfaces/HL7
Messaging Scanning
Document,
Note and
Transcription Type
Development and
Reconcilliation
HIM Chart
Completion
Viewing Scanned
Documents
Release of
Information
Document
Management
System
Administration
» Identify and map
all inbound and
outbound
message types
for ADT and
MDM messages
for DMS build
» Consider needs
for
order-level
scanning
messages (if
used)
» Consider merge/
unmerge/overlay
messages for
MPI reconcili-
ation
» Build provider
and HIM user
security that
supports AD and
EHR set up
» Consider client/
workstation vs.
Citrix deploy-
ment
approaches
» Consider use and
need for web-
based
approaches
» Scanner drivers
set up
» Setup for digital
photo capture
setup (if
supported)
» Downtime,
system upgrade,
update, and
ongoing
maintenance
» Build document
types and related
security as re-
quired for DMS
to integrate with
EHR
» Provider and
HIM user secu-
rity that supports
AD/EHR/DMS
set up
» Provider flat file
build and ongo-
ing maintenance
» Document type
and note type
set up
» DMS deficien-
cies set up that
integrates with
EHR set up
» Sign or decline
workflow to inte-
grate with EHR
» User security set
up that supports
AD/EHR/DMS
needs
» Consider use/
need for
web-based
approaches
» Scanned docu-
ment type
inclusion/
exclusion criteria
» User security
set up
DMS and EHR Points of Integration (cont.)
