
Student Health Program
2009-2010
Coulter Student Health Center
Counseling Center at Student Development and Academic Services
Student Health Insurance Plan (SHIP)
Athletic Trainer for Intercollegiate Athletes
Health Education and Wellness Programs
09COL1227

Dear CSM Student, Parent, or Guardian,
We are pleased to provide you with this brochure describing Mines Student Health Program. A healthy student body is
essential for a vibrant and dynamic learning environment and student success. The Student Health Program is
committed to assisting students in making healthier choices during their academic careers at the Colorado School of
Mines. The relationship between academic success and health is inseparable. Mines requires that all degree-seeking
students have adequate health insurance.
SSttuuddeennttss sshhoouulldd
:
• be proactive in addressing their health care issues.
• have access to timely and accurate health information and preventative measures.
• have quality health care that provides the least interruption of their academic progress, and not be hindered by the cost of obtaining the
care needed.
TThhee ffiivvee ccoommppoonneennttss ooff tthhee MMiinneess SSttuuddeenntt HHeeaalltthh PPrrooggrraamm aarree::
• Coulter Student Health Center • Health Information and Wellness Programs
• Student Health Insurance Plan (SHIP)* • Athletic Trainer for Intercollegiate Athletes
• Counseling Center at Student Development and Academic Services
Providing good health care supports academic success at Mines, through appropriate access to health care services, information, and the
highest possible quality of care. Primary care and mental health care services, paid through student fees, for all degree-seeking students,
is where our program starts. In cases where additional care is needed, health insurance is very important. Student and parents/guardians
must carefully consider their health insurance options to assure appropriate access to health care services, beyond Mines’ primary care and
mental health care, and have financial protection in the event of a major injury or illness.
AAccaaddeemmiicc SSuucccceessss aanndd HHeeaalltthh IInnssuurraannccee CCoonnssiiddeerraattiioonnss
• Minor injuries may require local care at a hospital, urgent care facility or specialist.
• Academic momentum should be supported by local access to follow-up care.
• Mental health care visits are best if access is within 2 miles.
• Students should not have to choose between paying for an education or paying for health care.
EEnnrroollllmmeenntt//WWaaiivveerr pprroocceessss ddeessiiggnneedd ttoo iimmpprroovvee tthhee hheeaalltthh iinnssuurraannccee ddeecciissiioonn pprroocceessss..
Online enrollment/waiver process: Completion is required for all US citizens for the SHIP. (International students and intercollegiate
athletes participating in NCAA-sanctioned sports can enroll in the SHIP online, but
mmuusstt
complete a paper waiver process.) The deadline
to waive the SHIP is September 9, 2009.
The SHIP cost for 2009-2010 is $780 per semester for single student coverage. The spring semester automatically includes summer
coverage. The average monthly cost of coverage is $130. We know of no other individual health insurance program available to Mines
students that provides comparable coverage at or below this cost. Many parents/guardians also find that the SHIP costs less than the
contributions required for employer sponsored health plans.
Our program provides Injury and Sickness coverage, as explained in this brochure, through the nation’s
largest health insurance organization, UnitedHealthcare. UnitedHealthcare StudentResources is also one
of the leading providers of health insurance coverage for college students. Our program has a fully insured
component (e.g., SHIP coverage) and a self-funded component (e.g., dental care services at the Coulter
Student Health Center). Other services provided to SHIP participants include after-hours phone
consultation and an improved process to obtain insurance identification cards.
Best wishes for a successful and healthy year.
Best Regards,
Ron Brummett, MBA, MA
Director of Student Services
EMERGENCIES
For life-threatening emergencies, students should call CSM Public Safety at 303-273-3333 and/or 911. If
appropriate, proceed directly to the nearest emergency room. For urgent health care situations, please call or visit the
Coulter Student Health Center. For psychological crisis situations on campus during normal CSM business hours,
please call the CSM Counseling Center at 303-273-3377.
* One Year Non-Renewable Term Policy underwritten by UnitedHealthcare Insurance Company

1
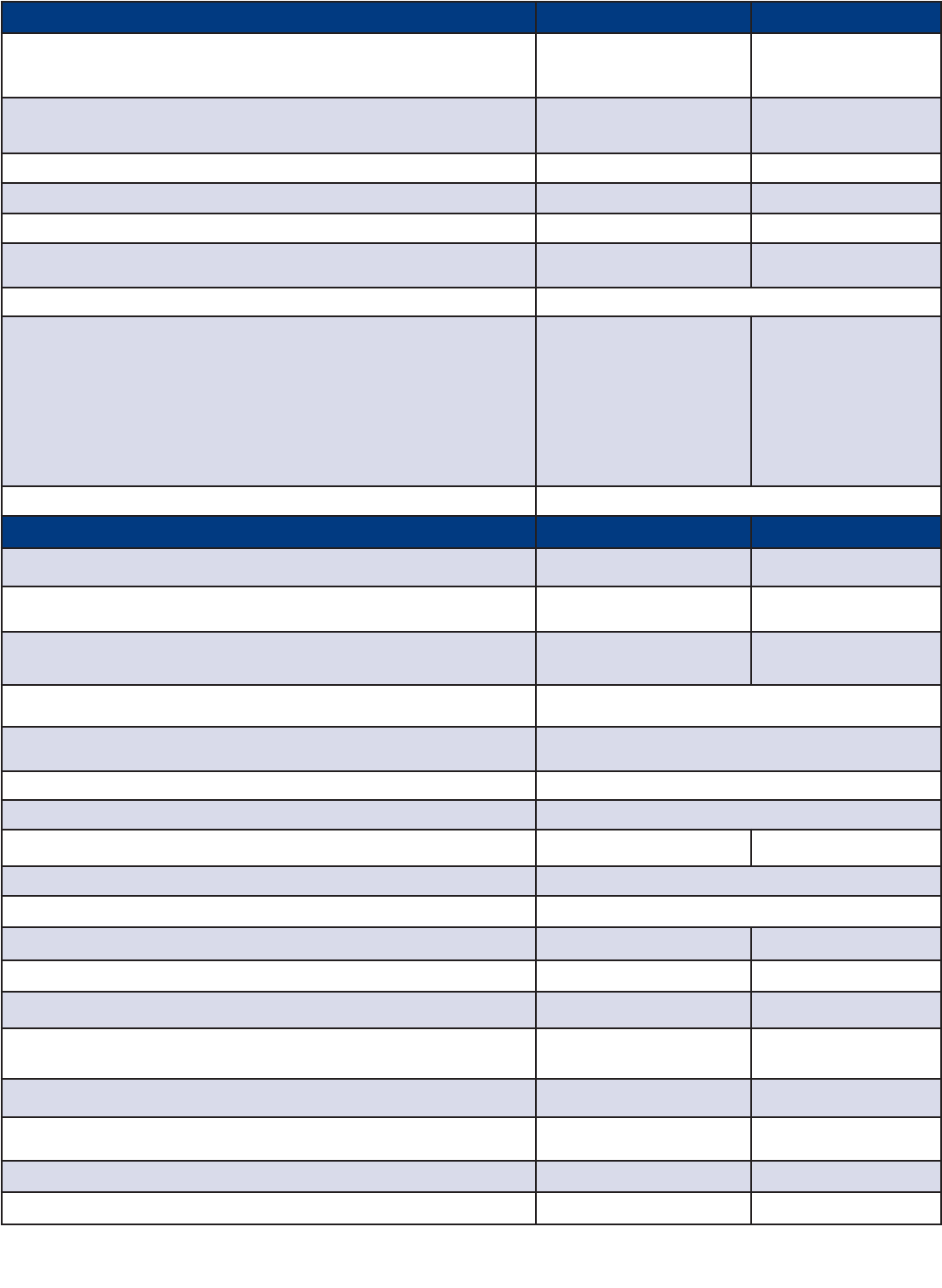
TABLE OF CONTENTS
CSM Health Insurance Requirement and Online Enrollment/Waiver Process . . . . . . . . . . . . . . . . . .2
Notices and Questions: Need More Information? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .3
Coulter Student Health Center . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .4
Dental Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .6
CSM Counseling Center . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .8
Student Health Insurance Plan (SHIP) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .10
Students Who Participate in NCAA-Sanctioned Intercollegiate Sports . . . . . . . . . . . . . . . . . . . . . .12
Pharmacy / Vision Benefits . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .13
SHIP Schedule of Coverage . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .14
State Mandates . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .16
The Colorado School of Mines Student Health Insurance Program Notice of Privacy Practices .20
Emergency Services for SHIP-Covered Persons . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .22
CSM Counseling Center Referral Benefit . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .23
Contact Section
Service Student Health Program Entity Phone Web Site
Primary Care and Dental Care
Coulter Student Health Center
After-Hours and Week-ends,
New West Physicians
(see below for 24-hour nurse/counseling-
line for SHIP-covered students)
303-273-3381
303-278-4600
http://healthcenter.mines.edu
www.nwphysicians.com (@Golden West
Location)
Counseling
Student Development and Academic
Services
303-273-3377 http://counseling.mines.edu
Sports Medicine for NCAA-
Sanctioned Intercollegiate Sports
CSM Athletic Trainer 303-273-3375 http://athletics.mines.edu
Emergencies and Crisis
Intervention
Life-Threatening Emergencies
CSM Public Safety
CSM Counseling
Suicide and Crisis Hot-Line
911
303-273-3333
303-273-3375
303-425-0300
N/A
http://publicsafety.mines.edu
http://counseling.mines.edu
www.suicidehotlines.com/colorado
Student Health Insurance Plan (SHIP)
On-Campus Service
CSM Student Health Insurance
Coordinator
303-273-3388 www.UHCSR.com/CSM
SHIP Benefits (including vision
care), Claims Information, and
Identification Cards
United Healthcare StudentResources
Pharmacy (Medco)
866-458-4954
877-417-7345
www.UHCSR.com/CSM
24-Hour Nurse/Counseling Line United Healthcare StudentResources 877-643-5130 www.liveandworkwell.com
Medical Evacuation United Healthcare StudentResources 877-488-9833 www.assistamerica.com/student
Confidential Secure Messaging
for Student Health Program
(available to all students
regardless of type of personal
health insurance coverage)
WordSecure for CSM Student Health
Program
303-273-3381
To subscribe visit:
https://csm.wordsecure.com/

CSM Health Insurance Requirement
All degree-seeking students who are (1) United States citizens
or permanent residents, (2) international students regardless of
degree seeking status, or (3) INTERLINK students must have
health insurance that meets or exceeds CSM’s coverage
requirements.
International and NCAA Student Athletes
International students and INTERLINK students cannot use the
on-line system to waive enrollment in the SHIP; they can only
use this system to enroll themselves in the SHIP. International
students must contact the International Student Program office
if they have embassy/other-sponsored coverage that they would
like considered by CSM for waiver of SHIP coverage.
Students participating in NCAA-sanctioned intercollegiate
sports cannot use the on-line system to waive enrollment in
the SHIP; they can only use this system to enroll themselves
in the SHIP. Athletes should contact Jennifer McIntosh, the
Head Athletic Trainer, if they wish to waive enrollment in the
SHIP.
Annual On-Line Enrollment/Waiver Process –
September 9, 2009 deadline!
SSttuuddeennttss rreeqquuiirreedd ttoo hhaavvee hheeaalltthh iinnssuurraannccee ccoovveerraaggee wwiillll bbee
aauuttoommaattiiccaallllyy eennrroolllleedd iinn tthhee SSHHIIPP aanndd cchhaarrggeedd $$778800 oonn
ttuuiittiioonn//ffeeee bbiilllliinngg iiff tthheeyy ddoo nnoott ccoommpplleettee tthhee oonn--lliinnee wwaaiivveerr
pprroocceessss bbyy SSeepptteemmbbeerr 99,, 22000099 ffoorr tthhee ffaallll sseemmeesstteerr aanndd
JJaannuuaarryy 2288,, 22001100 ffoorr sspprriinngg aanndd ssuummmmeerr ccoovveerraaggee..
Students
are strongly encouraged to use the on-line system to either
enroll or waive SHIP coverage. Using the default, automatic
enrollment in the SHIP will delay your access to an insurance
identification card and result in your receiving numerous email
notices about the SHIP enrollment/waiver deadline. Graduate
students must complete the enrollment process even though
their academic departments may be paying for the cost of the
SHIP.
Upon a student’s bona fide request and submission of
appropriate documentation, the School may grant a waiver of
the insurance requirement based on the student’s sincerely-held
religious belief which prevents the student from buying or having
health insurance. All waiver requests must be submitted in
writing and will be reviewed by the Student Health Insurance
Coordinator.
DO NOT FALSIFY YOUR PERSONAL INSURANCE
INFORMATION REQUIRED FOR WAIVING SHIP
COVERAGE. Students who falsify insurance information
may be required to enroll in the SHIP as an Unqualified Late
Enrollee, which includes both cost and benefit penalties.
Sanctions by CSM may also be imposed if students are
found to have intentionally falsified an official CSM required
document.
Requests for waiving SHIP coverage after the deadlines
stated above will be considered on an individual case basis
with presumption against students who were automatically
enrolled in the SHIP rather than using the on-line
enrollment/waiver system. If granted, SHIP waiver requests
after the enrollment/waiver deadline will be subject to a $60
late waiver fee for requests submitted prior to October 9,
2009 (February 28, 2010, for spring semester). This fee
increases to $120 for late waiver fee requests submitted
prior to November 9, 2009 (March 28, 2010, for spring
semester). Otherwise, refunds of the cost of SHIP coverage
will only be made upon the entry of any covered person into
the armed services of any country. A pro-rated refund will be
returned to such person upon request to the Insurance
Coordinator at the CSM Student Health Center.
Instructions for Using the SHIP On-Line
Enrollment/Waiver Process
Login to Trailhead and click on the Self Service button. Next,
click on the Student link, then the Registration link. Near the
bottom of the list, click on “Enroll/Waive in Student Health
Insurance Plan (SHIP)” and follow the instructions on the
page that appears. A confirmation page will appear indicating
your waiver has been approved or denied. Please print this
page for your records. An additional confirmation will be sent
to your Mines email address. If you encounter problems or
have questions, contact the Student Insurance Coordinator
at the Student Health Center at 303-273-3388 or subscribe
to WordSecure (see Table of Contents page) and send
message using the web-based system to the Student
Insurance Coordinator.
Enrolling Your Dependents in SHIP
Enrolling dependents in the SHIP cannot be done through the on-
line system. Students wanting to enroll a spouse or child(ren) in
the SHIP must visit the Student Insurance Coordinator’s office at
the Student Health Center to complete an enrollment form and
have the additional cost of coverage added to their tuition/fee
billing.
Other SHIP Eligibility Provisions
Please see page 11 for other provisions relating to access to
SHIP coverage in the event you involuntarily lose your group
health insurance coverage during the plan year (see Qualified
Late Enrollee provisions).
CSM HEALTH INSURANCE REQUIREMENT AND
ONLINE ENROLLMENT/WAIVER PROCESS
2

The Colorado School of Mines complies with the Health
Insurance Portability and Accountability Act of 1996. Privacy
policies for the Coulter Student Health Center and the
Counseling Center may be obtained by visiting either facility
or at the following websites.
http://healthcenter.mines.edu
http://counseling.mines.edu
NOTICES
The SHIP provided by CSM complies with the standards for
student health insurance/benefit programs recommended by
the American College Health Association.
www.acha.org
QUESTIONS — NEED MORE INFORMATION?
For further information, please contact:
CSM NCAA Intercollegiate Athletics at (303) 273-3375
Student Health Insurance Plan at (303) 273-3388
(email: SHI[email protected])
Student Development and Academic Services at (303) 273-3377
UnitedHealthcare StudentResources at (866) 458-4954 or
www.UHCSR.com/CSM
Preferred providers also may be found at this website.
The SHIP complies fully with Title IX of the Education
Amendments of 1972, Section 504 of the Rehabilitation Act
of 1973, and the Age Discrimination Act of 1975, as all three
laws were amended by the Civil Rights Restoration Act of
1987. Pregnancy benefits are provided on the same basis as
any other temporary disability. The Consolidated Omnibus
Budget Reconciliation Act of 1986 (COBRA) does not apply
to plans that are not employer-sponsored.
Kathryn van Susante
Student Health Insurance (SHIP)
Coordinator
3

4
Overview
The Coulter Student Health Center (http://healthcenter.mines.edu)
offers a variety of services which meet the health care needs of
most students. Every effort is made to help students obtain
appropriate consultation or referral when additional or special
services are required.
The clinic is staffed by nationally certified nurse practitioners
and registered nurses. Physician coverage is provided by a
group of family practice physicians who are on site from
3:00pm-4:45pm Monday-Friday, and are on call at all times.
Eligibility for Services
Students who are enrolled in at least four credit hours pay a
Health Center fee which allows access to services provided
at the Student Health Center. INTERLINK students are
eligible to use the Student Health Center only during their
session at CSM. Spouses may be seen at the Health Center,
for the same per semester fee as students. Spouses do not
have access to dental services provided at the Student
Health Center. The Student Health Center does not provide
services for children, faculty, staff or campus visitors.
Students may only be seen during the session in which they
are enrolled and paying fees.
Mark Pattridge, Medical Director of the Coulter Student Health Center, is
board certified in Family Medicine. He completed his residency/internship at
St. Mary’s Hospital in Grand Junction, Colorado. He has been affiliated with
the SHC for more than 20 years and has served as the Medical Director for the
past 12 years.
He maintains a family practice in Golden, New West Family Physicians. This
practice provides medical coverage for the SHC Monday – Friday 3:00-4:45
pm during the academic year. Drs. Julia Atkins, Harold Richardson, and
Patricia Brumbaugh share this coverage as well as phone consultation on
nights and weekends.
Debra Roberge, Director of the Coulter Student Health Center, is a board
certified Adult Nurse Practitioner. She has worked in college health for over 20
years. She received her Master’s Degree in Primary Care/NP from Boston
College.
COULTER STUDENT
HEALTH CENTER
EMERGENCIES
For life-threatening emergencies, students should call CSM Public Safety at 303-273-3333 and/or 911. If appropriate,
proceed directly to the nearest hospital emergency room. For urgent health care situations, please call or visit the Coulter
Student Health Center. For psychological crisis situations on campus during normal CSM business hours, please call the
CSM Counseling Center at 303-273-3377.

5
Services Provided Without Charge:
●
Over-the-counter medications (Advil, Tylenol, cold
medications, Mylanta, etc.)
●
Evaluation and treatment for common illnesses and
injuries.
●
Evaluation and treatment for depression, anxiety and other
uncomplicated mental health concerns.
●
Throat cultures.
●
Wart treatment with liquid nitrogen
(Wed. & Thurs.: 9-11:30 am and 1-2:30 pm).
●
Allergy shots given during doctors' hours until 4:15 pm.
Serum and instructions must be provided by the student.
●
Women's health care (annual women’s health exams must
be scheduled by appointment).
●
Safe sex education, condoms, and contraception options.
●
Brochures and information about various health related
topics (nutrition, STDs, AIDS, smoking, alcohol abuse,
etc.).
●
Crutches, knee braces, and heating pads can be checked
out for a short period of time.
●
Certain prescription medications (antibiotics, pain medications,
skin ointments, etc.).
●
Unlimited doctor visits during the academic year
(Mon.-Fri.: 3:00-4:45 pm).
●
Suturing of simple lacerations during doctors' hours,
wound care supplies, suture (stitches) removal.
●
MMR and tetanus (as result of injury) vaccines (when
available).
●
PPD (tuberculosis) skin test.
●
Flu shots (late October or early November while supplies last).
Services Available for an Additional Fee
●
PAP smears and other lab tests are available through the
Health Center; students will be billed for these tests.
●
Tetanus update
●
Hepatitis A/B combo immunization
●
Hepatitis A immunization
●
Hepatitis B immunization
●
Meningitis immunization
●
Gardasil/HPV
●
Dental Services
Health Center staff will facilitate referrals to
specialists/facilities for treatment not available at the
Student Health Center.
Location and Accessibility
The Student Health Center is located at 17th and Elm, across
from the IM field (and just to the south of the Student
Recreation Center). The building is handicapped accessible.
Hours of Services, Appointments, and Contact
Information
Clinic hours are Monday-Friday, 8:00am to 12:00pm and
1:00pm to 4:45pm (refer also to the Dental Clinic section for
dental care service hours).
Most services are provided without an appointment. Services
at the Dental Clinic and annual women’s health exams require
an appointment.
The Coulter Student Health Center telephone number is
303-273-3381. Students are encouraged to subscribe to our
secure messaging program to communicate with all student
health program staff at Colorado School of Mines, including
many of our affiliated external service companies. Students
may subscribe using their CSM email addresses by visiting
our secure web site at https://csm.wordsecure.com.
Confidentiality
The Coulter Student Health Center complies with both the
Health Insurance Portability and Accountability Act of 1996
(HIPAA) and all applicable State of Colorado laws and
regulations pertaining to the confidentiality of health records.
Certain educational records and other personal information is
governed by the Family Educational Rights and Privacy Act
(FERPA) rather than HIPAA.
Please review the complete Notice of Privacy Practices
statement in this brochure. Your health records and medical
information will be kept confidential by the Coulter Student
Health Center, except as specifically provided for in our
privacy policies and/or as pursuant to a valid release of health
records and medical information.

6
DENTAL CARE
Mission
The Dental Clinic at the Coulter Student Health Center
emphasizes patient education to prevent disease and
provides treatment options when procedures are needed.
Dental treatment is provided in the same non-threatening,
responsive, and considerate manner that students have come
to expect of all health care services at the Coulter Student
Health Center.
Eligibility and Fees
All CSM students who are enrolled in four credit hours and
who have paid the Health Center Fee are eligible for services
at the Dental Clinic. In most cases, treatment will require a
copayment. Students enrolled in the SHIP will receive priority
in scheduling appointments and will pay approximately 50%
less for dental care than students not participating in the
SHIP.* Students may only be seen during the session in which
they are enrolled and paying fees.
Telephone
Appointments: (303) 273-3381
Routine Appointment Hours of Service**
Tuesday 8:00 AM – 4:30 PM
Wednesday 8:00 AM – 4:30 PM
Friday 8:00 AM – 4:30 PM
Dental Clinic copayments
CCoovveerreedd SSeerrvviicceess SSHHIIPP PPrriivvaatteellyy
CCoovveerreedd IInnssuurreedd
SSttuuddeennttss** SSttuuddeennttss
EExxaammiinnaattiioonnss
Initial, with X-rays as needed $ 10.00 $ 20.00
Emergency exam with
X-rays as needed $ 0 $ 15.00
PPrreevveennttiivvee//DDiiaaggnnoossttiicc
Prophylaxis/hour
(includes recall exam) $ 15.00 $ 30.00
Four bitewing X-rays $ 10.00 $ 15.00
Sealant per tooth $ 10.00 $ 15.00
Full Mouth X-rays $ 15.00 $ 25.00
Peri-Apical films $ 0 $ 5.00
Vitality Testing $ 0 $ 10.00
Fluoride Treatment $ 5.00 $ 10.00
RReessttoorraattiivvee
Amalgam-I surface $ 20.00 $ 30.00
Amalgam-2 surfaces $ 25.00 $ 35.00
Amalgam-3 surfaces $ 30.00 $ 40.00
Amalgam-4 surfaces $ 35.00 $ 45.00
Resin-I surface $ 20.00 $ 30.00
Resin-2 surfaces $ 25.00 $ 35.00
Resin-3 surfaces $ 30.00 $ 40.00
Resin-4 surfaces $ 35.00 $ 45.00
Dental care is one of the services most valued by students at CSM
Jeanette Courtad, DDS
Staff Dentist
*Discount provided by CSM’s Dental Clinic. Dental care is
not provided by or underwritten by UnitedHealthcare
Insurance Company
.
**One third of the available appointment times will be reserved
for SHIP participants.
Students will be charged for missed appointments if they do not
call to cancel 24 hours prior to the scheduled appointment.
Hours of dental service may be reduced during semester breaks
and summer sessions.
FFeeeess aarree dduuee aatt tthhee ttiimmee ooff sseerrvviiccee.. TThhee HHeeaalltthh CCeenntteerr ddooeess nnoott
bbiillll,, aanndd ccaann oonnllyy aacccceepptt cchheecckkss oorr ccaasshh..

7
CCoovveerreedd SSeerrvviicceess
SSHHIIPP PPrriivvaatteellyy
CCoovveerreedd IInnssuurreedd
SSttuuddeennttss** SSttuuddeennttss
EEmmeerrggeennccyy
Pulpectomy/pulpotomy $ 20.00 $ 30.00
Sedative Filling/interim
restoration $ 15.00 $ 25.00
PPeerriiooddoonnttiiccss
Limited scaling/root cleaning $ 25.00 $ 35.00
Perio scaling/root
planing/per hour $ 35.00 $ 50.00
Perio maintenance $ 20.00 $ 30.00
Limited Scaling $ 25.00 $ 35.00
OOrraall SSuurrggeerryy
Extraction (simple) $ 30.00 $ 40.00
Incision &
Drainage Abscess $ 15.00 $ 20.00
RReeffeerrrraallss
Referrals will be made to qualified community specialists as
needed for services such as wisdom teeth extraction, root
canal treatment, periodontal evaluation and treatment,
orthodontics (braces), splints (night guards), bleaching, and
TMD or TMJ problems. These services are not covered by the
Dental Clinic.
SSeerrvviicceess eeiitthheerr NNoott PPrroovviiddeedd
bbyy oorr EExxcclluuddeedd ffrroomm tthhee DDeennttaall CClliinniicc
• More than two cleanings per benefit year unless
prescribed by the dentist
• Root Canals
• Crowns
• Bridges
• Dentures
• Complex Extractions
• Emergency care or other treatment rendered at
places other than the Coulter Student Health Center
Dental Clinic (including referrals)
• Any service or supply not listed in this brochure as a
covered service
The dental clinic is staffed by a dentist, a dental assistant,
and a dental hygienist and provides basic dental services
such as exams, cleaning, x-rays, simple restorations and
education regarding good dental hygiene. Dental services
are provided on a fee-for-services basis and are available to
all students who have paid the Health Center fee. Students
enrolled in CSM's Student Health Insurance Plan will receive
dental care for reduced fees.*

8
CSM COUNSELING CENTER
Overview
Counseling services are provided by Student Development and
Academic Services at CSM (http://counseling.mines.edu). A
student development approach to counseling focuses on the
developmental needs of students that typically occur between
the ages of 18 and 22. These needs include learning how to
develop, maintain and nurture relationships. Programs and
services address ways students can learn to cultivate healthy
lifestyles, leadership skills, assertiveness skills, communication
skills, and identify and minimize high-risk behaviors, including
use and abuse of alcohol and other drugs.
To best serve CSM students, we balance our student
development approach with professional mental health services.
Individual, short-term professional counseling is available to help
students identify personal, academic and/or career challenges,
and to learn positive coping skills to manage their lives.
Counselors are trained and experienced in providing crisis inter-
vention services as well as consultation regarding crises in order
to prevent, resolve, and/or minimize the effects of crisis on the indi-
vidual and the CSM community. Counseling appointments may be
scheduled from 8:00am-5:00pm, Monday through Friday. Office
hours vary during the summer session.
SSttuuddeennttss iinn ccrriissiiss ddoo nnoott
nneeeedd aann aappppooiinnttmmeenntt ttoo bbee sseeeenn ffoorr ccoouunnsseelliinngg sseerrvviicceess..
Eligibility for Services
All students enrolled at CSM for four or more credit hours are
eligible to use the counseling and crisis intervention services
available from Student Development and Academic Services.
INTERLINK students are also eligible to use these services.
There is no charge to students for counseling services. Students
enrolled in fewer than four credit hours must pay all fees,
including student service fees, to be eligible for counseling
services. Spouses of students are not eligible for services unless
they are also a CSM student.
Services Provided Without Charge
Individual counseling sessions are provided without charge for
eligible undergraduate and graduate students. Examples of the
reasons students seek counseling services include the
following:
●
Depression, anxiety, and other behavioral health concerns
that are common for college students.
●
Stress Management
●
Problem Solving
●
Time Management
●
Decision Making
●
Goal Setting
●
Relationships
●
Making positive lifestyle choices
●
Personal wellness
●
Increasing self-confidence
Crisis intervention and consultation services are also available.
Students who need long-term services will be referred to
community mental health care providers (including psychiatrists,
psychologists, and other licensed mental health care providers).
As noted throughout this brochure, adequate health
insurance coverage is essential to ensuring students
have appropriate access to health care services.
Ron Brummett, MBA, MA
Director of Student Services

9
Location and Accessibility
Student Development and Academic Support Services is located
at the north end of the first floor of the Ben E. Parker Student
Center, Suite 8. The building is handicapped accessible.
Hours of Service, Appointments, and Contact
Information
Counseling appointments may be scheduled from 8:00am-
5:00pm, Monday through Friday. Office hours vary during the
summer session. Students in crisis do not need an appointment
to be seen for counseling services. The Student Development
and Academic Services telephone number is 303-273-3377.
Students are encouraged to subscribe to our secure messaging
program to communicate with all student health program entities
at Colorado School of Mines, including many of our affiliated
external service companies. Students may subscribe using their
CSM email addresses by visiting our secure web site at
https://csm.wordsecure.com. Students may, subject to
conditions established by their counselor, use the secure
messaging system. Appointments, however, must be scheduled
by telephone or by visiting the Counseling Center.
Professional Staff
The professional staff includes licensed professional
counselors, psychologists, and social workers. All professional
staff have experience and specialized training in meeting the
counseling needs of college students.
CSM Counseling Center
(continued)
Confidentiality
Student Development and Academic Services complies with
both the Health Insurance Portability and Accountability Act of
1996 (HIPAA) and applicable State of Colorado laws and
regulations pertaining to confidentiality of health records. In
some instances, certain educational records and other personal
information is governed by the Family Educational Rights and
Privacy Act (FERPA) rather than HIPAA. Please review the
complete Notice of Privacy Practices statement in this brochure.
Your health records and medical information will be kept
confidential by Student Development and Academic Services,
except as specifically provided for in our privacy polices
and/or as pursuant to a valid release of health records and
medical information.

10
CSM has one of the nation’s best values for a student health insurance program.
IImmppoorrttaanntt PPooiinnttss ttoo CCoonnssiiddeerr
Good health is essential to academic success, and adequate
health insurance is essential to receive high quality health care.
Unexpected medical bills can also threaten the ability to complete
an education if students are uninsured or have inadequate
coverage. Health insurance is particularly important as primary
care and mental health care services provided by CSM are limited
as explained in this brochure.
●
The CSM Student Health Insurance Plan (SHIP) provides out-
standing coverage at a cost well below many comparable indi-
vidual health insurance policies. The SHIP is less expensive
than dependent coverage provided under many employer-
sponsored group health insurance plans.
●
Many employer-sponsored group health insurance plans do not
cover part-time students, or contain upper age limits. Also,
students who have declared financial independence from their
parents are no longer eligible to be covered as dependents
under employer-sponsored health insurance plans.
●
Students covered under a managed care type of health
insurance may not have full access to health care providers
while in the Denver area. This is a particularly important
consideration for students needing access to mental health
care providers.
●
For UnitedHealthcare preferred providers, the SHIP features
copayments rather than deductibles. Copayments are a
convenient way to pay your share of health care expenses.
●
NCAA intercollegiate athletes may be taking significant financial
risk if they do not enroll in the Student Health Insurance Plan.
They must confirm that their personal health insurance will cover
injuries resulting from the practice or play of intercollegiate
sports. See page 12 for more details.
●
The SHIP includes an annual vision exam benefit. See page 13
for details.
●
The SHIP includes special medical evacuation and repatriation
coverage for all international students. The SHIP also includes
special medical evacuation and repatriation coverage for SHIP
participants who travel abroad.
SHIP Overview
The Colorado School of Mines is pleased to offer a student
health insurance plan that is one of the best in the country for
scope of coverage and program value. This program provides
world-wide coverage for injury and sickness, on- or off-campus.
This fully insured plan is underwritten by UnitedHealthcare
Insurance Company and administered by UnitedHealthcare
StudentResources.*
SHIP Student Eligibility
Unless otherwise specified in this brochure, all degree-seeking
students who are United States Citizens or permanent residents
must have health insurance that meets or exceeds CSM’s
coverage requirements. International students and INTERLINK
students are only allowed to waive enrollment in the SHIP if they
have coverage that has been pre-approved by CSM for waiver
of SHIP coverage.
Upon a student’s bona fide request and submission of
appropriate documentation, the School may grant a waiver of
the insurance based on the student’s sincerely-held religious
belief which prevents the student from buying or having health
insurance. All waiver requests must be submitted in writing and
will be reviewed by the Student Health Insurance Coordinator.
All eligible students must meet the following additional
requirements:
1. Students must be enrolled in the SHIP prior to the
enrollment/waiver deadline for each coverage period, which
is the last day of any coverage period to drop a class without
a “W”. Students who waive coverage for the fall semester
will not be allowed to change this decision for the
spring/summer or summer coverage periods except as
specifically allowed for Qualified Late Enrollees (refer to
Voluntary SHIP Participation). Requests for rescission of a
SHIP waiver request will not be considered after the
enrollment/waiver deadline.
2. Students must attend regularly scheduled classes for the
first 31 days of each coverage period unless the student has
an approved medical withdrawal from CSM.
3. The student has not been enrolled in the SHIP for more than
nine years while in a single degree program.
4. Students may be required to establish that they are pursuing
a degree and making normal progress toward degree
completion.
5. Refer to the page 12 for special insurance requirements for
students who participate in NCAA-sanctioned intercollegiate
sports.
STUDENT HEALTH
INSURANCE PLAN (SHIP)
*Some components of the program (such as limited dental care benefits at the Coulter Student Health Center) are self-funded by CSM. This means a portion of
the cost of the plan is retained by CSM to provide certain benefits through special arrangements on a direct funding basis. CSM also retains funds to pay for
administrative costs associated with providing the SHIP.

11
Annual Open Enrollment
Students who waive enrollment in the SHIP are not eligible
for enrollment until the next annual open enrollment period,
except for provisions established for Qualified Late Enrollees.
For example, a student who waives enrollment in the SHIP for
the fall semester is not eligible to enroll in the subsequent
Spring/Summer coverage period. Note that students who are
covered by the SHIP for the spring semester automatically
have coverage through the summer, including students who
are graduating in May. Students not participating in
intercollegiate sports may withdraw from the SHIP at the
beginning of the spring/summer coverage period (not
applicable to summer) if they acquire health insurance that
qualifies for waiving SHIP enrollment. This option is not
available to students who participate in NCAA-sanctioned
sports.
Voluntary SHIP Eligibility Classes
Spouses and children of SHIP-covered students are also
eligible for participation in the SHIP. Eligible dependents are
the spouse (except in the event of divorce or annulment) and
unmarried children younger than 19 years of age. There are
also certain rules that apply for newborn coverage and adding
dependents that can be found at www.UHCSR.com/csm.
Pro-rated costs are available for newly acquired dependents.
Students who are in good academic standing and take an
approved leave of absence from CSM, including Cooperative
Education students and students enrolled in the International
Student Exchange Program, may request continuation in the
SHIP for a period not exceeding two academic semesters.
Such students must be enrolled in the SHIP in the period of
coverage immediately preceding the period of absence.
Spouses and dependents of such students are similarly
eligible for coverage.
Qualified Late Enrollees
An eligible student will only be allowed to enroll in the SHIP
after the applicable enrollment/waiver period if proof is
furnished that the student became involuntarily ineligible for
coverage under another group’s insurance plan during the 30
days immediately preceding the date of the request for late
enrollment in the SHIP. In such cases, the student’s effective
date of coverage under the SHIP will be the first day of the
month in which the student involuntarily loses coverage. The
30-day period in the provision may be extended if the student
can establish that he or she was unaware of the involuntary
loss of coverage. Refunds of premiums are allowed only upon
entry into the armed forces.
UnitedHealthcare StudentResources maintains its right to
investigate student status and attendance records to verify
that the policy eligibility requirements have been met. If
UnitedHealthcare StudentResources discovers the eligibility
requirements have not been met, its only obligation is to
refund premiums. Dependent eligibility expires concurrently
with that of the insured student.
Unqualified Late Enrollees
Any eligible student who is subject to the Colorado School of Mines’
insurance requirement and is found to be uninsured during the Plan
Year (and is not a Qualified Late Enrollee) or their plan
coverage does not meet CSM’s requirements will be required to enroll
in the SHIP under policy #2009-4059-2. Unqualified Late Enrollees
cannot purchase dependent cov-
erage under the SHIP until the next
Annual Open Enrollment Period.
Unqualified Late Enrollees will be
subject to a pre-existing condition
limitation that includes a six-month
look-back period for diagnosis or
treatment and a six-month waiting
period for benefits for any pre-exist-
ing condition to begin. The cost of
the SHIP is not pro-rated for
Unqualified Late Enrollees.
CCoovveerraaggee PPeerriioodd aanndd
EEffffeeccttiivvee DDaattee
aanndd TTeerrmmiinnaattiioonn DDaattee
2009
Fall Semester
August 25, 2009
January 12, 2010
2010
Spring/Summer
January 13, 2010
August 24, 2010
2010
Spring/Summer*
January 13, 2010
August 24, 2010
Only for students and
dependents not enrolled in the
SHIP in the Fall Semester.
2010
Field Session
May17, 2010
August 24, 2010
Only for students first
enrolling at CSM
2010
Summer Only
June 21, 2010
August 24, 2010
Only for students first
enrolling at CSM
Student/NCAA Student Athlete $780 $780 $1,037 $662 $467
Spouse $2,456 $2,456 $3,271 $1,774 $1,252
Child(ren) $1,660 $1,660 $2,216 $1,346 $951
Spouse and Child(ren) $4,116 $4,116 $5,487 $3,120 $2,203
2009/2010 SHIP Costs and Coverage Dates
Effective dates may be earlier for NCAA-intercollegiate athletes or other students required to be at CSM prior to start of school.
*These rates are calculated using similar average monthly costs as charged to students/dependents who are enrolled for both fall and spring/summer coverage periods.

12
NCAA Student Athletes
Students who will be participating in NCAA-sanctioned
intercollegiate sports at the Colorado School of Mines are
subject to additional insurance requirements as specified
below. The requirements apply even if the student is only
trying out for a team or is only engaged in a single day of
intercollegiate sports practice activities.
AAtthhlleetteess wwiillll nnoott bbee
aalllloowweedd,, eeffffeeccttiivvee tthhee 22000088--22000099 ppllaann yyeeaarr,, ttoo cchhaannggee tthheeiirr
ddeecclliinnaattiioonn ooff S
SHHIIPP ccoovveerraaggee aanndd eennrroollll iinn tthhee SSHHIIPP aatt tthhee
sspprriinngg sseemmeesstteerr..
To enroll in or waive SHIP coverage, athletes engaged in
NCAA-sanctioned intercollegiate sports must complete a
special enrollment/waiver form and submit it to the Athletic
Department. You will not be allowed to participate in
intercollegiate practice or play until this form is completed and
submitted to the Athletic Department.
Please make note of the following.
●
If you waive participation in the SHIP, you and your
parent/guardian accept financial responsibility for any
expenses or illnesses resulting from the practice or play of
NCAA-sanctioned intercollegiate sports. This liability
includes: (1) any expense limited or excluded by the NCAA
catastrophic insurance and (2) the $75,000 deductible
under the policy. The NCAA catastrophic insurance policy
is available for review at the CSM Athletic Department.
●
If you enroll in the SHIP and you comply with the
preauthorization for care requirements, you will be
responsible only for the copayments, deductibles, and any
ineligible charges under the program.
●
The cost of the SHIP for students who are engaged in the
practice or play of intercollegiate sports will no longer be
subject to a surcharge. The cost for students who
participate in NCAA-sanctioned intercollegiate sports will
be the same as for all other students who participate in the
SHIP.
●
If you waive participation in the SHIP and will be relying on
employer-sponsored health plan coverage, you must
confirm that your plan will cover injuries resulting from the
practice or play of intercollegiate sports. Students and
parents should use caution in relying on employer-
sponsored health coverage as some plans have adopted
exclusions for professional sports or organized sports such
as intercollegiate athletics
NCAA Coverage for Catastrophic Intercollegiate
Athletic Injury
NCAA catastrophic coverage is provided, without charge, to
all CSM students who participate in NCAA-sanctioned
intercollegiate athletics, regardless of participation in the
SHIP. This coverage is provided through the National
Collegiate Athletic Association. The NCAA coverage has two
levels of financial liability for students: (1) any expense limited
or excluded by the NCAA catastrophic insurance and (2) the
$75,000 deductible under the policy. This coverage also
includes important benefits other than reimbursement of
medical expenses (e.g., college education benefits and
assimilation/rehabilitation benefits).
STUDENTS WHO PARTICIPATE IN NCAA-
SANCTIONED INTERCOLLEGIATE SPORTS

13
Preferred Plan
The school has selected a Preferred health plan that gives you
the opportunity to save by offering a higher benefit level when
you see preferred providers. This plan offers the typical health
plan benefits, plus many services that you may not expect
from a PPO — including some preventive care and
prescription drugs. When you see preferred providers, they
will take care of all the necessary paperwork for you. With this
plan, you may select any doctor or hospital you wish. You will
receive benefits for most covered services even if you choose
to receive care from an out-of-network provider — but you will
pay a greater share of the cost. Please note that out-of-
network care is not covered for certain specialized services.
Refunds
RReeffuunnddss ooff pprreemmiiuummss wwiillll bbee mmaaddee uuppoonn tthhee eennttrryy ooff aannyy
ccoovveerreedd ppeerrssoonn iinnttoo tthhee aarrmmeedd ffoorrcceess ooff aannyy ccoouunnttrryy..
A pro-
rated refund will be returned to such person upon request.
Students who withdraw from CSM for non-medical reasons
prior to the last day of any semester to drop a class without a
“W” are not eligible for the SHIP coverage for that semester.
Students must notify the Registrar’s Office of such withdrawal
and the entire cost of the coverage for that semester will be
refunded, including dependent coverage.
SSuucchh ssttuuddeennttss wwiillll
nnoott bbee eennttiittlleedd ttoo aannyy bbeenneeffiittss aanndd nnoo ccllaaiimmss wwiillll bbee hhoonnoorreedd..
NNoo ootthheerr rreeffuunnddss wwiillll bbee iissssuueedd..
Identification Cards
Students and dependents covered by the SHIP may request
Identification Cards using the Internet. Students may log on
to the UnitedHealthcare StudentResources website at
www.UHCSR.com on or after the following dates for the
2009-2010 academic year.
Fall Semester: October 1, 2009
Spring Semester: February 15, 2010*
Summer Session: July 15, 2010*
*Students enrolling for the fall semester do not have to re-
order identification cards for the spring/summer coverage
periods. These dates are only for new students first enrolling
at CSM during these periods.
Understanding the Network
The SHIP is a PPO plan provided through UnitedHealthcare
Insurance Company – the largest insurance company in the
country. UnitedHealthcare has negotiated discounted service
rates in order to provide the best healthcare value to you.
The plan encourages you to use preferred providers to
maximize your healthcare dollars. Using preferred providers
results in a lower deductible and a lower out-of-pocket
maximum. Out-of-network service charges by physicians and
facilities are also higher since they have not agreed to
provide a discount on their services.
Want to see if your doctor is in the UnitedHealthcare Choice Plus
PPO network? Go to www.UHCSR.com/CSM to search for
participating providers. You can also call Customer Service at
866-458-4954. Customer Service Representatives are available
from 7 a.m. to 7 p.m., Central Time, Monday through Friday.
Pharmacy Benefits
The SHIP includes benefits for outpatient prescription drugs
when dispensed by UnitedHealthcare Network Pharmacy
(UHPS). Please refer to the Schedule of Medical Expense
Benefits, page 15, for information. For a full description of
pharmacy benefits, including the terms, limitations, and
additional pharmacy specific exclusions, please refer to the
plan brochure available on-line at www.UHCSR.com/CSM.
Vision Benefits
The SHIP includes a vision exam once per policy year and the
benefit is available from either a preferred provider or out-of-
network provider. Please refer to the Schedule of Medical
Expense Benefits, page 14, for additional information.
Discount Vision benefits through UnitedHealth Allies
®
SHIP participants will also have access to a discount program
from UnitedHealth Allies that provides point of service discounts
on vision care including optometry, mail order vision products and
laser vision correction. Vision discounts range from 10% to 50%
on vision services. This is a discount program, not insurance.
Your UnitedHealth Allies I.D. card will be delivered in the same
envelope as your SHIP I.D. card. Simply register at
sr.unitedhealthallies.com using the member number on the
UnitedHealth Allies I.D. card to search for vision providers in the
area and secure your guaranteed discount.

Maximum Lifetime Benefit $2,000,000
Deductible, Preferred Provider: $0
Deductible, Out-of-Network: $1,000
(Per Insured Person) (Per Policy Year)
Deductible, Out-of-Network: $3,000
(Aggregate) (Per Family) (Per Policy Year)
Coinsurance, Preferred Provider:
90% except as noted
Coinsurance, Out-of-Network:
70% except as noted
Max = Maximum
PA = Preferred Allowance
U&C = Usual & Customary Charges
14
INPATIENT Preferred Provider Out-of-Network
Hospital Expense, daily semi-private room rate; general nursing care provided by the Hospital;
Hospital Miscellaneous Expenses, such as the cost of the operating room, laboratory tests, x-ray
examinations, anesthesia, drugs (excluding take home drugs) or medicines, therapeutic services,
and supplies. In computing the number of days payable under this benefit, the date of admission
will be counted, but not the date of discharge.
90% of PA / $250 copay
per admission
70% of U&C /
$750 Deductible
per admission
Routine Newborn Care, while Hospital Confined; and routine nursery care provided
immediately after birth. 4 days Hospital Confinement expense maximum.
Paid as any other Sickness
Physiotherapy, (Includes occupational and speech therapy. 30 non-acute days maximum Per
Policy Year.)
Paid under Hospital Expense
Surgeon’s Fees, in accordance with data provided by Ingenix. If two or more procedures are
performed through the same incision or in immediate succession at the same operative session,
the maximum amount paid will not exceed 50% of the second procedure and 50% of all
subsequent procedures.
90% of PA 70% of U&C
Assistant Surgeon
90% of PA 70% of U&C
Anesthetist, professional services in connection with inpatient surgery.
90% of PA 70% of U&C
Registered Nurse’s Services, private duty nursing care. 90% of PA 70% of U&C
Physician’s Visits, benefits do not apply when related to surgery.
90% of PA 70% of U&C
Pre-Admission Testing, payable within 3 working days prior to admission. Paid under Hospital Miscellaneous Expenses
Psychotherapy (other than for Biologically-Based Mental Illness.)
See Benefits for Psychotherapy
Biologically-Based Mental Illness
See Benefits for Biologically Based Mental Illness
OUTPATIENT Preferred Provider Out-of-Network
Surgeon’s Fees, in accordance with data provided by Ingenix. If two or more procedures are
performed through the same incision or in immediate succession at the same operative session,
the maximum amount paid will not exceed 50% of the second procedure and 50% of all
subsequent procedures.
90% of PA 70% of U&C
Day Surgery Miscellaneous, related to scheduled surgery performed in a Hospital, including
the cost of the operating room; laboratory tests and x-ray examinations, including professional
fees; anesthesia; drugs or medicines; and supplies. Usual and Customary Charges for Day
Surgery Miscellaneous are based on the Outpatient Surgical Facility Charge Index.
90% of PA /
$250 copay
70% of U&C /
$750 Deductible
Assistant Surgeon
90% of PA 70% of U&C
Anesthetist, professional services administered in connection with outpatient surgery.
90% of PA 70% of U&C
Physician’s Visits, benefits for Physician’s Visits do not apply when related to surgery or
Physiotherapy.
100% of PA / $25 copay per
visit
70% of U&C / $25
Deductible per visit
The Policy provides benefits for the Usual and Customary Charges incurred by an Insured Person for loss due
to a covered Injury or Sickness up to the Maximum Lifetime Benefit of $2,000,000.
The Preferred Provider for this plan is UnitedHealthcare Choice Plus PPO.
If care is received from a Preferred Provider any Covered Medical Expenses will be paid at the Preferred
Provider level of benefits. In all other situations, reduced or lower benefits will be provided when an Out-of-
Network provider is used.
PPrreeffeerrrreedd PPrroovviiddeerr OOuutt--ooff--PPoocckkeett MMaaxxiimmuumm::
The Company will pay 90% of Preferred Allowance for Preferred
Providers up to $1,000 Per Insured Person Per Policy Year or $3,000 Aggregate Maximum Per Insured Family,
Per Policy Year. Once the Insured or Family out-of-pocket maximum has been satisfied, additional Covered
Medical Expenses will be paid at 100% of Preferred Allowance, up to a Lifetime Maximum Benefit of
$2,000,000 Per Insured Person. Copayments do not apply to the Preferred Provider out-of-pocket maximum.
OOuutt--ooff--NNeettwwoorrkk OOuutt--ooff--PPoocckkeett MMaaxxiimmuumm::
After the Deductible has been satisfied, the Company will pay 70%
of Usual & Customary Charges up to $3,000 Per Insured Person, Per Policy Year or $9,000 Aggregate
Maximum Per Insured Family, Per Policy Year. Once the Insured or Family out-of-pocket maximum has been
satisfied, additional Covered Medical Expenses will be paid at 100% of Usual & Customary Charges, up to a
Lifetime Maximum Benefit of $2,000,000 Per Insured Person. Copayments and per service Deductibles do
not apply to the Out-of-Network out-of-pocket maximum.
All maximums are combined Preferred Provider and Out-of-Network, unless noted below.
Benefits will be paid up
to the Maximum Benefit for each service as scheduled below. Covered Medical Expenses include:
SHIP SCHEDULE OF
COVERAGE
15
OUTPATIENT continued Preferred Provider Out-of-Network
Physiotherapy, Benefits are limited to one visit per day. (Includes occupational and speech
therapy. 20 visits maximum Per Policy Year.) (For children up to age 5, benefits are limited to
20 therapy visits each per policy year each for physiotherapy, occupational, and speech
therapy.)
90% of PA / $25
copay per visit
70% of U&C
Medical Emergency, attending Physician’s charges and the use of the emergency room and
supplies. Treatment must be rendered within 72 hours from time of Injury or first onset of
Sickness. Copay/Deductible waived if admitted.
90% of PA / $100 copay per
visit
90% of U&C / $100
Deductible per visit
(Includes all ancillary charges)
Diagnostic X-ray Services
90% of PA 70% of U&C
Laboratory Services
90% of PA 70% of U&C
Radiation Therapy & Chemotherapy
90% of PA 70% of U&C
Tests & Procedures, diagnostic services and medical procedures performed by a Physician,
other than Physician’s Visits, Physiotherapy, X-Rays and Lab Procedures.
90% of PA 70% of U&C
Psychotherapy (other than for Biologically-Based Mental Illness.) See Benefits for Psychotherapy page 17
Prescription Drugs, Prescription medications are categorized within three tiers. Each tier is
assigned a copay, which is an amount you pay when you fill a prescription at a participating retail
pharmacy or refill your ongoing prescription through the network mail-order pharmacy service.
Tier 4 prescriptions are for self-administered injectables only.
Mail order is available through UHPS at 2.5 times the retail copay up to a 90 day supply. The
maximum copay for mail-order Tier 4 self-administered injectables is $500 maximum.
Benefits are also available for smoking cessation Prescription Drugs when enrolled in an
approved UHPS smoking cessation counseling program up to a $250 per insured Per Policy
Year / $500 Maximum Lifetime Benefit.
UnitedHealthcare Network
Pharmacy (UHPS) up to a 31-day
supply per prescription.
Tier 1: $15 copay per prescription.
Tier 2: $40 copay per prescription.
Tier 3: $60 copay per prescription.
Tier 4: 30% copay per prescription
not to exceed $250 maximum
copay per prescription.
No Benefits
Biologically-Based Mental Illness
See Benefits for Biologically Based Mental Illness page 17
OTHER Preferred Provider Out-of-Network
Ambulance Services, (Copay/Deductible is per trip.)
100% of PA / $200 copay
100% of U&C / $200
Deductible
Air Ambulance
90% of PA /
$5,000 maximum per trip
90% of U&C /
$5,000 maximum per trip
Durable Medical Equipment, a written prescription must accompany the claim when
submitted. Replacement equipment is not covered. Exception: See Benefits for Prosthetic
Devices
90% of PA / $1000 maximum
Per Policy Year
No Benefits
Consultant Physician Fees, when requested and approved by the attending
Physician.
Paid as a Physician’s Visit
Alcoholism/Drug Abuse
Paid as any other Sickness
See Benefits for Biologically Based Mental Illness
Maternity
Paid as any other Sickness
Complications of Pregnancy
Paid as any other Sickness
Organ Transplants
90% of PA / $250 copay per
admission
No Benefits
Voluntary Termination of Pregnancy
No Benefits
NCAA Sanctioned Intercollegiate Sports Benefit, $75,000 max Per Injury
Paid as any other Injury
Annual Gynecological Exam, (This benefit is not subject to the Policy Deductible.)
90% of PA / $25 copay per visit 70% of U&C
Acupuncture, (12 visits maximum Per Policy Year.)
90% of PA / $25 copay per visit 70% of U&C
Vision, (One exam Per Policy Year) (The eye exam exclusion will be waived and benefits will
be paid as specified not to exceed one exam Per Policy Year.)
100% of PA / $20 copay
100% of U&C / $20
Deductible
Skilled Nursing Care, (Limited to 30 days Per Policy Year in and out-of-network combined.
Copayment waived if admitted directly to a skilled nursing facility from an inpatient acute
facility.)
90% of PA / $250 copay
per admission
70% of U&C / $750
Deductible per admission
Home Health Care, (Limited to 60 visits Per Policy Year.)
90% of PA / $25 copay per visit No Benefits
Hospice Care, (30 inpatient days maximum Per Policy Year/91 outpatient days maximum Per
Policy Year. Visit maximums are in and out-of-network combined.)
90% of PA 70% of U&C
Urgent Care
90% of PA / $35 copay per visit 70% of U&C
Dental, (Injury to Sound, Natural teeth only.)
90% of U&C 90% of U&C

16
STATE MANDATES
Benefits for Prosthetic Devices
Benefits will be paid for the Usual and Customary Charges for the
purchase of Prosthetic Devices.
Prosthetic device means an artificial device to replace, in whole or in part,
an arm or leg.
Benefits are limited to the most appropriate model that adequately meets
the medical needs of the Insured as determined by a Physician. Repairs
and replacements of Prosthetic Devices are also covered unless
necessitated by misuse or loss.
Benefits shall be subject to all Deductible, copayment, coinsurance,
limitations, or any other provisions of the policy.
Benefits for Telemedicine Services
Benefits will be paid for Covered Medical Expenses on the same basis as
services provided through a face-to-face consultation for services
provided through Telemedicine for an Insured residing in a county with
one hundred fifty thousand or fewer residents. “Telemedicine” means the
use of interactive audio, video, or other electronic media to deliver health
care. The term includes the use of electronic media for diagnosis,
consultation, treatment, transfer of medical data and medical education.
The term does not include services performed using a telephone or
facsimile machine.
Nothing in this provision shall require the use of Telemedicine when in-
person care by a participating provider is available to an Insured Person
within the Company’s network and within the Insured’s geographic area.
Benefits shall be subject to all Deductible, copayment, coinsurance,
limitations, or any other provisions of the policy.
Benefits for Mammography
Benefits will be paid for the actual expense incurred up to $90.00 for
low-dose screening mammography for the presence of occult breast
cancer. Benefits will be provided according to the following guidelines:
1. A single baseline mammogram for women thirty-five to thirty-nine years
of age.
2. A mammogram not less than once every two years for women forty
years of age and under fifty years of age or more often for women with
risk factors to breast cancer if recommended by her Physician.
3. A mammogram every year for women fifty to sixty-five years of age.
“Low-dose mammography” means the x-ray examination of the breast,
using equipment dedicated specifically for mammography including but
not limited to the x-ray tube, filter, compression device, screens, films, and
cassettes, with an average radiation exposure delivery of less than one rad
mid-breast, with two views for each breast.
The policy Deductible will not be applied to this benefit.
Benefits shall be subject to all copayment, coinsurance, limitations or any
other provisions of the policy.
Benefits for Diabetes
Benefits will be paid for the Usual and Customary Charges for all
medically appropriate and necessary equipment, supplies, and outpatient
diabetes self-management training and educational services including
nutritional therapy if prescribed by a Physician.
Diabetes outpatient self-management training and education shall be
provided by a Physician with expertise in diabetes.
Benefits shall be subject to all Deductible, copayment, coinsurance,
limitations, or any other provisions of the policy.
Benefits for Cervical Cancer Vaccines
Benefits are payable for the cost of cervical cancer vaccinations for all
female Insured Persons under the age of 20 for whom a vaccination is
recommended by the Advisory Committee on Immunization practices of
the United States Department of Health and Human Services.
Benefits for Medical Foods
Benefits are payable for Medical Foods needed to treat inherited
enzymatic disorders caused by single gene defects involved in the
metabolism of amino, organic, and fatty acids as specified below.
If the policy provides benefits for Prescription Drugs, benefits will be paid
the same as any other Sickness for Medical Foods, to the extent medically
necessary, for home use for which a Physician has issued a written, oral
or electronic prescription. Benefits will not be provided for alternative
medicine.
Coverage includes but is not limited to the following diagnosed
conditions: phenylketonuria; maternal phenylketonuria; maple syrup urine
disease; tyrosinemia; homocystinuria; histidinemia; urea cycle disorders;
hyperlysinemia; glutaric acidemias; methylmalonic acidemia; and
propionic acidemia. Benefits do not apply to cystic fibrosis patients or
lactose- or soy-intolerant patients.
There is no age limit on the benefits provided for inherited enzymatic
disorders except for phenylketonuria. The maximum age to receive
benefits for phenylketonuria is twenty-one years of age; except that the
maximum age to receive benefits for phenylketonuria for women who are
of child-bearing age is thirty-five years of age.
Medical foods means prescription metabolic formulas and their modular
counterparts, obtained through a pharmacy that are specifically designed
and manufactured for the treatment of inherited enzymatic disorders
caused by single gene defects involved in the metabolism of amino,
organic, and fatty acids and for which medically standard methods of
diagnosis, treatment, and monitoring exist. Such formulas are specifically
processed or formulated to be deficient in one or more nutrients and are
to be consumed or administered enterally either via tube or oral route
under the direction of a Physician.
Benefits shall be subject to all Deductible, copayment, coinsurance,
limitations, or any other provisions of the policy
.

17
Benefits for Prostate Cancer Screening
Benefits will be paid for actual charges incurred up to $65 for an annual
screening by a Physician for the early detection of prostate cancer.
Benefits will be payable for one screening per year for any male Insured
50 years of age or older. One screening per year shall be covered for any
male Insured 40 to 50 years of age who is at risk of developing prostate
cancer as determined by the Insured’s Physician. The screening shall
consist of the following tests:
1) A prostate-specific antigen (PSA) blood test; and
2) Digital rectal examination.
The policy Deductible will not be applied to this benefit and this benefit
will not reduce any diagnostic benefits otherwise allowable under the
policy.
Benefits shall be subject to all copayment, coinsurance, limitations, or any
other provisions of the policy.
Benefits for Biologically Based Mental Illness
Benefits will be paid the same as any other Sickness for the
treatment of Biologically Based Mental Illness. The benefit provided
will not duplicate any other benefits provided in this policy.
“Biologically Based Mental Illness” means schizophrenia,
schizoaffective disorder, bipolar affective disorder, major depressive
disorder, specific obsessive-compulsive disorder, and panic
disorder.
“Mental Disorder” means posttraumatic stress disorder, drug and
alcohol disorders, dysthymia, cyclothymia, social phobia,
agoraphobia with panic disorder, and general anxiety disorder.
Mental Disorder also includes anorexia nervosa and bulimia nervosa
to the extent those diagnoses are treated on an out-patient, day
treatment, and in-patient basis, exclusive of residential treatment.
Benefits shall be subject to all Deductible, copayment, coinsurance,
limitations, or any other provisions of the policy.
Benefits for Psychotherapy
Benefits will be paid the same as any other Sickness at a
coinsurance percentage of 50% for Psychotherapy treatment
subject to the following provisions:
Inpatient or Partial Hospitalization Benefits:
Benefits are limited to 45 days for inpatient care or 90 days for
Partial Hospitalization care in any 12-month period. For the purpose
of computing the period for which benefits are payable, the following
will apply:
1) Two days of Partial Hospitalization shall reduce by one day the 45
days for inpatient care. One day of inpatient care shall reduce by
two days the 90 days available for Partial Hospitalization.
2) Each day of inpatient confinement under this benefit or each two
days of Partial Hospitalization shall reduce by one day, the total
days available for all Sicknesses for any one 12-month period.
Partial Hospitalization, for the purposes of this benefit, means
continuous treatment for at least three hours, but not more than 12
hours during a 24-hour period.
Outpatient Benefits:
Treatment will be provided for outpatient services furnished by 1) a
comprehensive health care service corporation; or 2) a Hospital, a
community mental health center; or 3) other mental health clinic
approved by the Colorado Department of Human Services to provide
such care; or 4) a registered professional nurse; or 5) a licensed
clinical social worker, acting within the scope of license; or 6)
furnished by or under the supervision of a licensed Physician or
psychologist.
Except as stated below, all such services must be provided by or
under the supervision of a licensed Physician or licensed
psychologist; and records must show that the licensed Physician or
psychologist, saw the patient or had a written summary of
consultations or a personal consultation with the therapist at least
once each 90 days.
Covered services under this benefit, which can legally be furnished
by a registered professional nurse or licensed clinical social worker,
acting within the scope of his or her license, will not require the
supervision of a Physician or psychologist. Reimbursement may be
made directly to such provider.
Outpatient Benefits are limited to $5,000 in any 12-month period.
Benefits shall be subject to all Deductible, copayment, coinsurance,
limitations, or any other provisions of the policy.
Benefits for Child Health Supervision Services
Benefits will be paid for the Usual and Customary charges for Child
Health Supervision Services from birth up to the age of 13. Benefits are
payable on a per visit basis to one health care provider per visit.
Child Health Supervision Services rendered during a periodic review are
covered only to the extent such services are provided during the course
of one visit by, or under the supervision of a single Physician, Physician’s
assistant or Registered Nurse.
Child Health Supervision Services means the periodic review of a child’s
physical and emotional status by a Physician or other provider as above.
A review shall include but not be limited to a history, complete physical
examination, developmental assessment, anticipatory guidance, appropri-
ate immunizations, preventative services, and laboratory tests in keeping
with prevailing medical standards.
Immunizations are based on the recommended childhood immunization
schedule and the recommended immunization schedule for children who
start late or who are more than 1 month behind published by the CDC.
Recommended schedules are available from:
Advisory Committee on Immunization Practices,
www.cdc.aov/nip/acip;
American Academy of Pediatrics, www.aap.org;
American Academy of Family Physicians, www.aafp.org.
The policy Deductible and dollar limits will not be applied to this benefit.
Benefits shall be subject to all copayment, coinsurance, limitations, or any
other provisions of the policy.

18
Benefits for Therapies for Congenital Defects and Birth
Abnormalities
Benefits will be paid the same as any other Sickness for physical,
occupational and speech therapy for congenital defects and birth
abnormalities for covered Dependent children beginning after the first 31
days of life to five years of age.
Benefits will be paid for the greater of the number of such visits provided
under the policy or twenty visits per year for each therapy. Benefits will be
provided without regard to whether the condition is acute or chronic and
without regard to whether the purpose of the therapy is to maintain or to
improve functional capacity.
Benefits shall be subject to all Deductible, copayment, coinsurance,
limitations, or any other provisions of the policy.
Benefits for Cleft Lip or Cleft Palate
Benefits will be paid the same as any other Sickness for treatment of
newborn children born with cleft lip or cleft palate or both. Benefits shall
include the medically necessary care and treatment including oral and
facial surgery; surgical management; the medically necessary care by a
plastic or oral surgeon; prosthetic treatment such as obturators, speech
appliances, feeding appliances; medically necessary orthodontic and
prosthodontic treatment; habilitative speech therapy, otolaryngology
treatment; and audiological assessments and treatment.
Benefits shall be subject to all Deductible, copayment, coinsurance,
limitations, or any other provisions of the policy.
Benefits for Hospitalization and General Anesthesia for
Dental Procedures for Dependent Children
Benefits will be paid the same as any other Sickness for general
anesthesia, when rendered in a Hospital, outpatient surgical facility, or
other facility licensed pursuant to Colorado Statute Section 25-3-101,
and for associated Hospital or facility charges for dental care provided to
a Dependent child. Such Dependent child shall, in the treating Physician’s
opinion, meet one or more of the following criteria:
1. The child has a physical, mental, or medically compromising condition;
2. The child has dental needs for which local anesthesia is ineffective
because of acute infection, anatomic variations, or allergy;
3. The child is an extremely uncooperative, unmanageable, anxious, or
uncommunicative child or adolescent with dental needs deemed
sufficiently important that dental care cannot be deferred; or
4. The child has sustained extensive orofacial and dental trauma.
Benefits shall be subject to all Deductible, copayment, coinsurance,
limitations, or any other provisions of the policy.
Benefits for Colorectal Cancer Screening
Benefits will be paid for the total costs of tests related to preventive
health care services for the early detection of colorectal cancer and
adenomatous polyps.
Benefits will be provided for an average risk adult Insured Person
who is asyptomatic and age 50 or older. Benefits will also be
provided for an Insured Person who is at high risk for colorectal
cancer and who has:
1. A family medical history of colorectal cancer;
2. A prior occurrence of cancer or precursor neoplastic polyps;
3. A prior occurrence of chronic digestive disease condition such as
inflammatory bowel disease, Crohn’s disease, or ulcerative colitis;
or
4. Other predisposing factors as determined by Insured Person’s
health care provider.
The policy Deductible will not be applied to this benefit.
Benefits shall be subject to all copayment, coinsurance, limitations,
or any other provisions of the policy.
Benefits for Hearing Aids for Minor Children
Benefits will be paid for Covered Medical Expenses for Hearing Aids
for a Minor Child who has a hearing loss that has been verified by a
licensed Physician and a licensed Audiologist. The Hearing Aid shall
be medically appropriate to meet the needs of the Minor Child
according to accepted professional standards.
Benefits shall include the purchase of the following:
1. Initial Hearing Aids and replacement Hearing Aids not more
frequently than every five years;
2. A new Hearing Aid when alterations to the existing Hearing Aid
cannot adequately meet the needs of the Minor Child; and
3. Services and supplies including, but not limited to, the initial
assessment, fitting, adjustments, and auditory training that is
provided according to professional standards.
“Hearing Aid” means amplification technology that optimizes
audibility and listening skills in the environments commonly
experienced by the patient, including a wearable instrument or
device designed to aid or compensate for impaired human hearing.
“Hearing Aid” shall include any parts or ear molds.
“Minor Child” means an Insured Person under the age of eighteen.
Benefits shall be subject to all Deductible, copayment, coinsurance,
limitations, or any other provisions of the policy.

19
Exclusions and Limitations
No benefits will be paid for: a) loss or expense caused by,
contributed to, or resulting from; or b) treatment, services or
supplies for, at, or related to:
1. Learning disabilities, behavioral problems, and Attention
Deficit Hyperactivity Disorder testing (treatment is covered),
conceptual handicap, developmental delay or disorder or
mental retardation;
2. Biofeedback;
3. Chronic pain disorders;
4. Circumcision;
5. Cosmetic procedures, except cosmetic surgery required to
correct an Injury for which benefits are otherwise payable
under this policy, removal of warts;
6. Dental treatment, except for accidental Injury to Sound,
Natural Teeth;
7. Elective Surgery or Elective Treatment;
8. Elective abortion;
9. Eye examinations, eye refractions, eyeglasses, contact
lenses, prescriptions or fitting of eyeglasses or contact
lenses, vision correction surgery, or other treatment for
visual defects and problems; except when due to a disease
process; or except as specifically provided in the policy;
10. Health spa or similar facilities; strengthening programs;
11. Hearing examinations or hearing aids, except as specifically
provided in the policy; or other treatment for hearing defects
and problems. "Hearing defects" means any physical defect
of the ear which does or can impair normal hearing, apart
from the disease process;
12. Hirsutism; alopecia;
13. Hypnosis;
14. Injury or Sickness for which benefits are paid or payable
under any Workers' Compensation or Occupational
Disease Law or Act, or similar legislation;
15. Injury sustained by reason of a motor vehicle accident to the
extent that benefits are paid or payable by any other valid
and collectible insurance;
16. Inpatient convenience items such as guest meals,
telephone, televisions;
17. Investigational services;
18. Medical and non-medical self-care or self-help training,
recreation therapy, educational therapy, dance therapy, art
therapy;
19. Prescription Drugs, services or supplies as follows:
a) Therapeutic devices or appliances, including: hypoder-
mic needles, syringes, support garments and other non-
medical substances, regardless of intended use; except
as provided under Benefits for Diabetes;
b) Immunization agents, biological sera, blood or blood
products administered on an outpatient basis;
c) Drugs labeled, “Caution - limited by federal law to
investigational use” or experimental drugs;
d) Products used for cosmetic purposes;
e) Drugs used to treat or cure baldness; anabolic steroids
used for body building;
f) Anorectics - drugs used for the purpose of weight control;
g) Fertility agents or sexual enhancement drugs, such as
Parlodel, Pergonal, Clomid, Profasi, Metrodin,
Serophene, or Viagra;
h) Growth hormones; or
i) Refills in excess of the number specified or dispensed
after one (1) year of date of the prescription.
20. Reproductive/Infertility services including but not limited
to: family planning; fertility tests; infertility (male or
female), including any services or supplies rendered for
the purpose or with the intent of inducing conception;
premarital examinations; impotence, organic or
otherwise; tubal ligation; vasectomy; sexual reassignment
surgery; reversal of sterilization procedures;
21. Routine Newborn Infant care, well-baby nursery and
related Physician charges in excess of 48 hours for
vaginal delivery or 96 hours for cesarean delivery. If forty-
eight hours following a vaginal delivery falls after 8 p.m.,
coverage shall continue until 8 a.m. the following morning.
If ninety-six hours following the cesarean section falls
after 8 p.m., coverage shall continue until 8 a.m. the
following morning;
22. Routine physical examinations and routine testing;
preventive testing or treatment; screening exams or
testing in the absence of Injury or Sickness; except as
specifically provided in the policy;
23. Temporomandibular joint dysfunction; deviated nasal
septum, including submucous resection and/or other
surgical correction thereof; except for treatment of
chronic purulent sinusitis;
24. Supplies, except as specifically provided in the policy;
25. Surgical breast reduction, breast augmentation, breast
implants or breast prosthetic devices, or gynecomastia;
except as specifically provided in the policy;
26. Treatment in a Government hospital, unless there is a
legal obligation for the Insured Person to pay for such
treatment;
27. War or any act of war, declared or undeclared; or while in
the armed forces of any country other than the United
States (a pro-rata premium will be refunded upon request
for such period not covered); and
28. Weight management, weight reduction, nutrition programs,
treatment for obesity, surgery for removal of excess skin or fat.

20
THIS NOTICE DESCRIBES HOW MEDICAL INFORMATION
ABOUT YOU MAY BE USED AND DISCLOSED AND HOW YOU
CAN GET ACCESS TO THIS INFORMATION. PLEASE REVIEW
IT CAREFULLY.
Explanation of Forms. The Colorado School of Mines Student
Health Program (the "SHP") handles medical information about you.
The handling of this information is regulated by law. To comply with
the applicable law, the SHP requires you to receive this notice and,
in some circumstances, to sign an authorization form.
The SHP is allowed by law to use and disclose information about
you for the purposes essential to providing care, including, but not
limited to, treatment, payment collection, and operating the SHP.
An authorization allows the SHP to use and disclose information
about you for any other reason that is listed in the authorization. The
SHP may condition enrollment or eligibility on the provision of an
authorization only if the authorization is for determining enrollment or
eligibility. Other rules about your rights regarding medical information
are described in this notice.
Types of Uses and Disclosures. Medical information about you
may be used or disclosed by the SHP for treatment, payment, and
health care operations. Treatment includes consultation, diagnosis,
provision of care and referrals. Payment includes all activities
necessary for billing and collection, such as claims processing.
Health care operations includes everything the SHP does to assess
the quality of care, teach and develop staff, and manage the SHP’s
operations. Some examples of uses and disclosures are below.
Example of Treatment Disclosure. The SHP may disclose medical
information about you to your treating physician, a hospital or other
providers to help them diagnose and treat an injury or illness.
Example of Payment Disclosure. The SHP may disclose medical
information about you when health plans or insurers, Medicare,
Medicaid, or other payors require the information before paying for
your health care services.
Example of Health Care Operations Use. The SHP may use medical
information about you when it hires new staff whose education and
development requires information about the medical needs of our
patients.
Other Uses and Disclosures. The SHP may use or disclose your
medical information in the following situations without your
authorization. These situations include:
As Required By Law. The SHP may use or disclose your medical
information to the extent that the use or disclosure is required by law.
The use or disclosure will be made in compliance with the law and
will be limited to the relevant requirements of the law. You will be
notified, as required by law, of any such uses or disclosures.
Public Health. The SHP may disclose your medical information for
public health activities and purposes to a public health authority that
is permitted by law to collect or receive the information. The
disclosure will be made for the purpose of controlling disease, injury
or disability. The SHP may also disclose your medical information, if
directed by the public health authority, to another government
agency that is collaborating with the public health authority.
Communicable Diseases. The SHP may disclose your medical
information, if authorized by law, to a person who may have been
exposed to a communicable disease or may otherwise be at risk of
contracting or spreading the disease or condition.
Health Oversight. The SHP may disclose your medical information to
a health oversight agency for activities authorized by law, such as
audits, investigations, and inspections. Oversight agencies seeking
this information include government agencies that oversee the health
care system, government benefit programs, other government
regulatory programs and civil rights laws.
Abuse or Neglect. The SHP may disclose your medical information
to a public health authority that is authorized by law to receive
reports of child abuse or neglect. In addition, the SHP may disclose
your medical information to the governmental entity or agency
authorized to receive such information if the SHP believes that you
have been a victim of abuse, neglect or domestic violence. In this
case, the disclosure will be made consistent with the requirements
of applicable federal and state laws.
Food and Drug Administration. The SHP may disclose your medical
information to a person subject to the jurisdiction of the Food and
Drug Administration if that person has responsibility to report
adverse events, product defects or problems, or biologic product
deviations; to track products; to enable product recalls, repairs or
replacements; or, to conduct post marketing surveillance.
Legal Proceedings. The SHP may disclose your medical information
in the course of any judicial or administrative proceeding, in
response to an order of a court or administrative tribunal (to the
extent such disclosure is expressly authorized by such order), and,
under certain conditions, in response to a subpoena, discovery
request or other lawful process.
Law Enforcement. The SHP may also disclose your medical
information for law enforcement purposes so long as applicable legal
requirements are met. These law enforcement purposes include: (1)
disclosure pursuant to legal processes or as otherwise required by
law, (2) disclosure in response to limited information requests by a
law enforcement official for identification and location purposes, (3)
disclosure to a law enforcement official in response to information
pertaining to victims of a crime, (4) disclosure to a law enforcement
official in connection with a suspicion that death may have occurred
as a result of criminal conduct, (5) disclosure to a law enforcement
official in the event that a crime occurs on the premises of the SHP,
and (6) disclosure to a law enforcement official in connection with a
medical emergency (not on the CSM’s premises) when it is likely that
a crime has occurred.
Coroners, Funeral Directors, and Organ Donation. The SHP may
disclose your medical information to a coroner or medical examiner
for identification purposes, for determining cause of death or for the
coroner or medical examiner to perform other duties authorized by
law. The SHP may also disclose your medical information to a funeral
director, as authorized by law, in order to permit the funeral director
to carry out the director’s duties. The SHP may disclose such
information in reasonable anticipation of death. Your medical
information may also be used and disclosed to organ procurement
organizations for cadaveric organ, eye or tissue donation purposes.
THE COLORADO SCHOOL OF MINES
NOTICE OF PRIVACY PRACTICES

21
Research. The SHP may disclose your medical information to
researchers when the research has been approved by an institutional
review board that has reviewed the research proposal and
established protocols to ensure the privacy of your medical
information.
Criminal Activity. Consistent with applicable federal and state laws,
the SHP may disclose your medical information, if the SHP believes
that the use or disclosure is necessary to prevent or lessen a serious
and imminent threat to the health or safety of a person or the public.
The SHP may also disclose your medical information if it is
necessary for law enforcement authorities to identify or apprehend
an individual.
Military Activity and National Security. When the appropriate
conditions apply, the SHP may use or disclose the medical
information of individuals who are Armed Forces personnel (1) for
activities deemed necessary by appropriate military command
authorities; (2) for the purpose of a determination by the Department
of Veterans Affairs of eligibility for benefits, or (3) to foreign military
authority if you are a member of the foreign military services. The
SHP may also disclose your medical information to authorized
federal officials for conducting national security and intelligence
activities, including for the provision of protective services to the
President or others legally authorized.
Workers’ Compensation. Your medical information may be disclosed
by the SHP as authorized to comply with workers’ compensation
laws and other similar legally established programs.
Required Uses and Disclosures. Under the law, the SHP must make
disclosures to you when required by the Secretary of the
Department of Health and Human Services to investigate or
determine our compliance with applicable law.
Others Involved in Your Healthcare. Unless you object in
writing to the Privacy Official, the SHP may disclose to a member of
your family, a relative, a close friend or any other person whom you
identify, your medical information that directly relates to that person’s
involvement in your health care. If you are unable to agree or object
to such a disclosure, the SHP may disclose such information as
necessary if the SHP determines that it is in your best interest based
on the SHP’s professional judgment. The SHP may use or disclose
your medical information to notify or assist in notifying a family
member, personal representative or any other person that is
responsible for your care of your location, general condition or death.
Finally, the SHP may use or disclose your medical information to an
authorized public or private entity to assist in disaster relief efforts
and to coordinate uses and disclosures to family or other individuals
involved in your health care.
Authorized Uses and Disclosures. Additional uses and
disclosure may be made if you have given written authorization,
which may be revoked at any time in writing delivered to the Privacy
Official or the Privacy Official’s designee, except to the extent the
SHP acted in reliance on the authorization.
Restrictions. You have the right to request restrictions on the use
and disclosure of medical information about you; however, the SHP
will only be bound by the restrictions if the SHP notifies you that it
agrees with them. Confidentiality. You have the right to have the SHP
use only confidential means of communicating with you about
medical information. This means you may have information delivered
to you at a certain time or place, or in a manner that keeps your
information confidential. Access. You have the right to see and
receive a copy of information about you kept by the SHP under most
circumstances.
Amendment of Health Information. You have the right to have
the SHP amend its records of information about you. The SHP may
refuse to amend information that is accurate, that was created by
someone else, or is not disclosable to you.
Accounting. You have the right to request in writing a list of
disclosures of your medical information made by the SHP, which
includes the purposes and recipients of the information.
Copy. You have the right to receive a paper copy of this notice.
Amendment of Policies and Procedures. The SHP reserves its
rights to make changes to the privacy policies and procedures in
accordance with the applicable terms of such policies and
procedures with respect to changes.
Privacy Notice. The SHP is required by law to keep medical
information about you private and to give you this notice. The SHP
must abide by this notice. However, the SHP reserves the right to
amend this notice and make such change applicable to all medical
information maintained by SHP. Any revised notice will be provided
to enrollees by the SHP.
HIPAA and FERPA. With respect to student health information, the
SHP also complies with the requirements set forth in The Family
Educational Rights and Privacy Act (FERPA).
Complaints. If you believe your privacy rights have been violated
you may submit a written complaint to the Privacy Official, Coulter
Student Health Center, The Colorado School of Mines, Golden,
Colorado 80401. You may also complain to the Secretary of the U.S.
Department of Health and Human Services. The SHP will not
retaliate against you for making a complaint.
Effective Date. This notice is effective from April 14, 2004 until
revised by the SHP.

22
Participation in the SHIP provides emergency services for students who travel abroad.
Scholastic Emergency Services (SES)
International Travel Emergency Assistance, Medical
Evacuation and Repatriation Program
An International Travel Emergency Assistance, Medical
Evacuation and Repatriation Program is included for students
and dependents covered by the Student Health Insurance
Plan. The cost for this program is included in charges for the
SHIP coverage, and the service is provided by SES. SES
utilizes highly trained, multilingual coordinators and board
certified physicians in conjunction with an extensive
information and communication system to assist travelers
worldwide. SES offers prompt, professional help in any
medical or personal emergency, 24 hours a day.
SES Services
●
Worldwide 24-hour toll-free telephone assistance in
locating the nearest, most appropriate medical care.
●
Overcoming language barriers by directing the SHIP-
covered persons to English speaking doctors or
translators.
●
Monitoring progress during the course of medical
treatment and recovery, including arranging for necessary
specialists upon a doctor’s request.
●
Maintaining contact with family, personal physician, and
CSM, as appropriate.
●
Assistance in coordinating admission into hospitals or
other care facilities.
●
Coordination of direct payments or deposits to health care
providers.
●
Management, coordination, and payment of emergency
medical evacuations or repatriation.
●
Coordination of emergency blood and medication
transfers.
●
Preplanning of medical support in remote areas.
●
Emergency message transmittal services.
●
Emergency international funds transfer capabilities.
●
Travel assistance for a family member wishing to be with a
patient hospitalized for more than seven days (includes
payment of round-trip economy airfare to the place of
hospitalization).
●
Assistance for unattended dependent children (includes
payment of one-way economy airfare to the place of
residence with an escort if required).
●
Assistance in making arrangements for interrupted travel
plans resulting from an emergency situation.
●
Knowledgeable legal referral service.
●
Assistance with travel problems such as lost or stolen
passports.
Locating Medical Services
SES has a database of thousands of international providers.
These providers encompass doctors, hospitals, clinics, air
ambulance companies, and others. Providers are carefully
selected based on the medical specialty, location, language,
and office hours. In addition, SES Assistance Specialists are
multilingual and highly trained.
Payment of Medical Bills
The SHIP coverage may provide benefits for medical
expenses incurred while traveling abroad (refer to the Student
Health Insurance Plan for coverage of such expenses). SES
includes coverage for expenses associated with a medically
necessary evacuation, but all other medical bills are the
responsibility of the insured. SES will coordinate all billing
and insurance verifications, including settling any guarantee
of payment. This ensures that there is no delay or denial of
medical treatment because of an inability to make payment.
Special Information for CSM International Students
Enrolled in the SHIP
International students enrolled in the SHIP are covered by
SES (as explained in this brochure) while they are outside the
United States as part of CSM-sponsored travel. Also,
international students enrolled in the SHIP are covered by
SES for medical evacuation and repatriation while they are at
CSM.
EMERGENCY SERVICES FOR
SHIP-COVERED PERSONS

23
Special CSM Counseling Center
Referral Benefit
SHIP-covered persons have access to a Special CSM
Counseling Center Referral Benefit for mental health
care/chemical dependence treatment for covered students who
receive a referral to a community psychiatrist, psychologist,
certified addictions counselor, or other licensed mental health
care therapists from the CSM Counseling Center. This is a
separate benefit from the mental health care coverage shown in
the SHIP Schedule of Coverage that is administered by
UnitedHealthcare StudentResources. This means you may
obtain outpatient mental health care services, without first
receiving a referral from the CSM Counseling Center, if you
choose to use the schedule of benefits that is administered by
UnitedHealthcare StudentResources.
This Special CSM Counseling Center Referral Benefit only
applies if you receive a referral from the Counseling Center
and you obtain services from a licensed mental health care
professional who has entered into a service agreement with
the Colorado School of Mines.
The Special CSM Counseling Center Referral Benefit will pay
up to thirty (30) visits each plan year. The first visit will be paid
in full (no copayment) and the second through the 30th visits
will be subject to a $10 copayment.
Your therapist must obtain authorization for continued
services from the Director of the Counseling Center at CSM
at the 9th visit and again at the 19th visit. You will not be
required to pay any additional fee beyond the $10 copayment.
No part of this benefit is indemnified by UnitedHealthcare
Insurance Company. UnitedHealthcare Insurance Company
also has no responsibility for administration of Special CSM
Counseling Center Referral Benefit claims or covered person
eligibility determinations.
Laboratory Charges at the Coulter Student Health
Center
Except for routine physical examinations, laboratory charges
incurred by covered SHIP participants will be covered at 100
percent when laboratory specimens are obtained at the Coulter
Student Health Center. Students are not required to submit
claims. No part of this benefit is indemnified by UnitedHealthcare
Insurance Company. UnitedHealthcare StudentResources also
has no responsibility for administration of laboratory claims or
covered person eligibility determinations.
Insurance Plans, Funding, and
Indemnification of Risk
The Dental Clinic at the Coulter Student Health Center is not
a participating provider with private dental insurance plans. A
billing statement students may submit to private dental
insurance plans will be provided upon request.
Funding for construction of the Dental Clinic at the Coulter
Student Center was derived from use of reserve funds from
the Student Health Program and the Coulter Foundation
Fund. Funding for dental care benefits is derived from a
capitation payment each semester within the cost of student
only coverage.
No part of the self-funded dental benefits, laboratory charges at
the Coulter Student Health Center, or Special CSM Counseling
Center Referral Benefits, is indemnified by UnitedHealthcare
Insurance Company. UnitedHealthcare Insurance Company also
has no responsibility for administration of dental claims,
laboratory charges at the Coulter Student Health Center, or
Special CSM Counseling Center Referral Benefits.
Membership Brochure
This brochure is not a contract with UnitedHealthcare Insurance
Company. It provides a summary of the benefits and limitations
of the SHIP. If there is any difference between this brochure and
the policy, the provisions of the policy on file with the school will
govern. For a full description of coverage under the SHIP,
including benefits, exclusions, any reductions and limitations and
the terms under with the coverage may remain in force, refer to
the plan brochure which is available on-line or at the CSM
Coulter Student Health Center.
COBRA and Extension of Eligibility/Benefits
The Student Health Program is not subject to the extension of
eligibility provisions required under Consolidated Omnibus
Budget Reconciliation Act of 1986 (COBRA). Accordingly,
the Student Health Program does not provide an extension of
eligibility provision or any extension of benefit provision,
unless specifically provided for under the terms and
conditions of the program.

Student Health Program
Coulter Student Health Center
Colorado School of Mines
Golden, CO 80401
