1
APPENDIX B
State-by-State Summary of Opioid Prescribing
Regulations and Guidelines
This document was developed by and used by permission from:
Corey Davis, JD
The Network for Public Health Law
Southeastern Region Office & the National Health Law Program

2
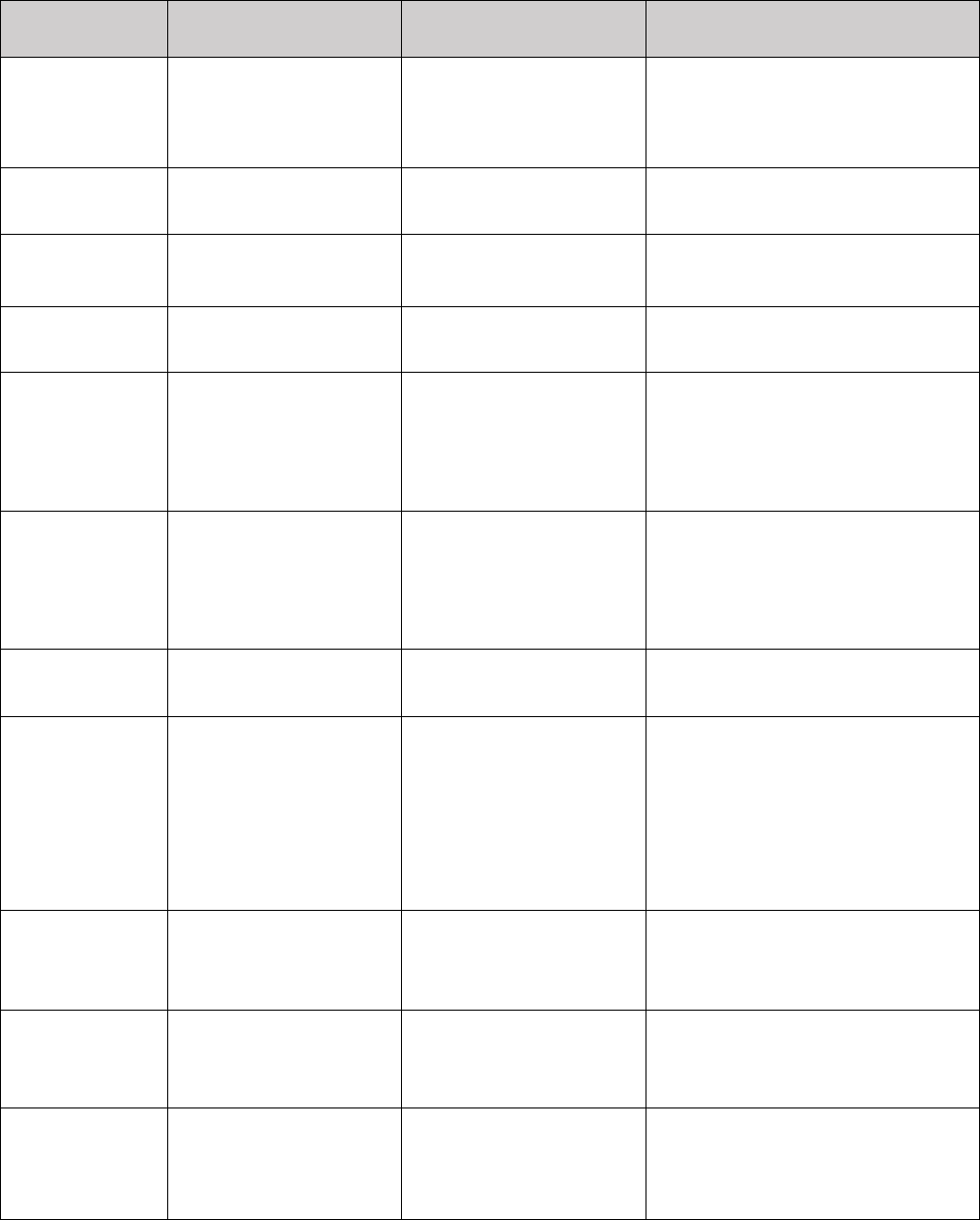
State-by-State Summary of Opioid Prescribing Regulations and Guidelines
Requirements with
the force of law
Quasi-regulatory
guidelines
Advisory Guidelines
Alabama
-Ala. Admin Code
§ 560-X-16-.20
(2014);
-Ala. Admin Code
§ 540-X-4-.09 (2013)
N/A
N/A
Alaska
N/A
N/A
Pending
Arizona
N/A
N/A
AZ Opioid Prescribing
Guidelines
Arkansas
Ark. Code Ann § 20-
7-703 (2015);
Executive Order
2016-06 (2016)
N/A
AR Emergency Department
Opioid Prescribing Guidelines
California
N/A
Guidelines for
Prescribing
Controlled Substances
for Pain
N/A
Colorado
DHCPF Opioid
Prescribing Policy
N/A
Joint Policy for Prescribing and
Dispensing Opioids
Connecticut
-Conn. Gen. Stat.
Ann. § 21a-254(9)
(2015);
-Conn. Gen. Stat. Ann
§ 17a-714a (2016)
N/A
CT Emergency Department
Opioid Prescribing Guidelines
Delaware
Del Admin. Code
C.S.A. 9.0 (2017)
N/A
-Guidelines for the Use of
Controlled Substances for the
Treatment of Pain;
-DE Emergency Department
Opioid Prescribing Guidelines
Florida
N/A
FL Boards of Medicine
and Osteopathic
Medicine’s General
Policies on Opioid
Prescribing
N/A
Georgia
Ga. Comp. R. & Regs.
360-3-.06 (2013)
N/A
N/A
Hawaii
N/A
N/A
Emergency Department Opioid
Prescription Guidelines
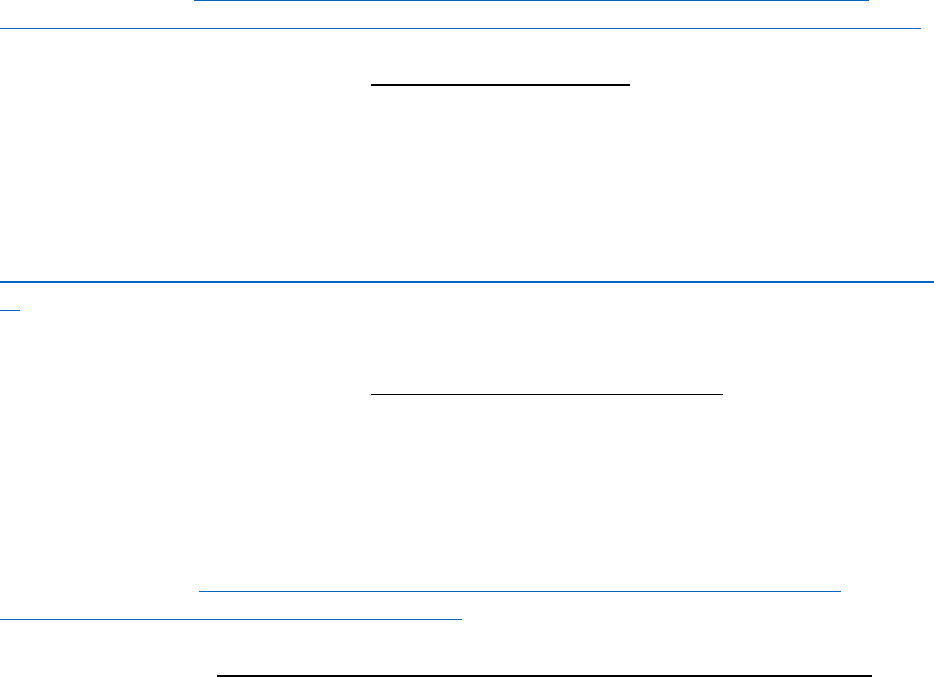
3
Requirements with
the force of law
Quasi-regulatory
guidelines
Advisory Guidelines
Idaho
N/A
Policy for the Use of
Opioid Analgesics in
the Treatment of
Chronic Pain
N/A
Illinois
N/A
N/A
N/A
Indiana
844 Ind. Admin.
Code 5-6-3 (2014)
N/A
N/A
Iowa
Iowa Admin. Code
§ 653-13.2 (2016)
N/A
N/A
Kansas
N/A
Joint Policy Statement
on the Use of
Controlled Substances
for the Treatment of
Pain
N/A
Kentucky
-201 Ky. Admin.
Regs. 9:260 (2013)
- Ky. Rev. Stat. Ann.
§ 218A.205(3)(b)
(2017)
Guidelines for the Use
of Controlled
Substances in Pain
Treatment
N/A
Louisiana
La. Stat. Ann. §
40:978 (2015)
N/A
N/A
Maine
-02-373 Me. Code R.
21 § II (2012);
-32 Me Rev. Stat.
Ann. § 3300-F
(2016);
-22 Me. Rev. Stat.
Ann. § 7253 (2016)
N/A
N/A
Maryland
Md. Code Ann.,
Health Occ. § 1-223
(2017)
N/A
MD Emergency Department
Opioid Prescribing Guidelines
Massachusetts
Mass. Ann. Laws ch.
94C, § 19D (2016)
Prescribing Practices
Policies and
Guidelines
MHA Guidelines for
Emergency Department Opioid
Management
Michigan
N/A
Guidelines for the Use
of Controlled
Substances for the
Treatment of Pain
N/A

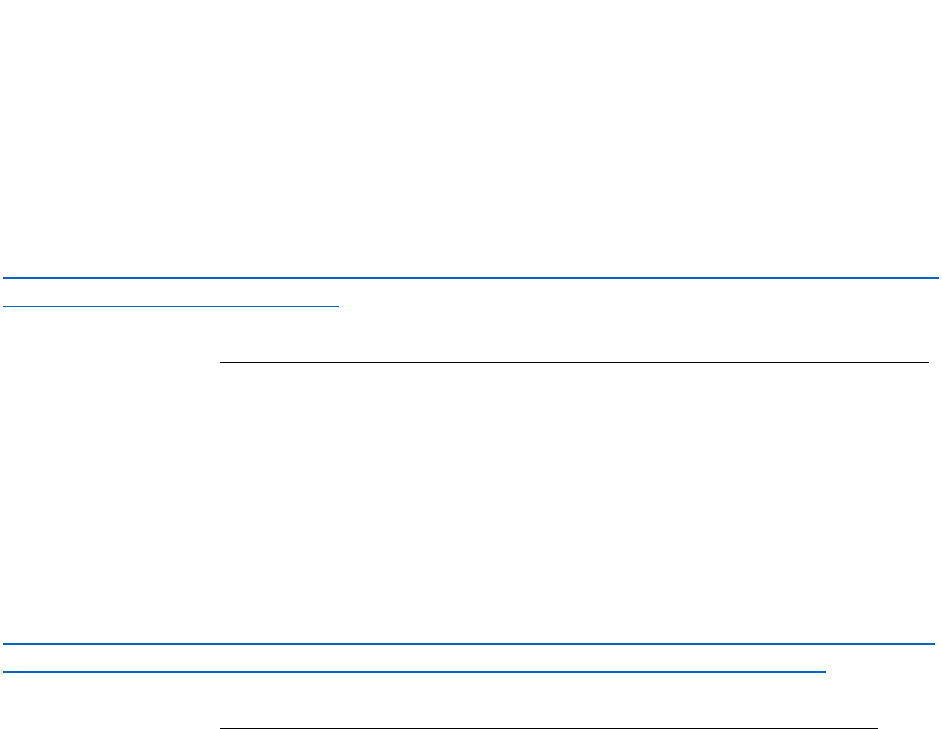
4
Requirements with
the force of law
Quasi-regulatory
guidelines
Advisory Guidelines
Minnesota
Minn. R. 5221.6110
(2015)
Joint Statement on
Pain Management
N/A
Mississippi
Miss. Admin. Code
30-17-2640:1.7
(2012)
N/A
N/A
Missouri
N/A
Guidelines for the Use
of Controlled
Substances for the
Treatment of Pain
N/A
Montana
N/A
N/A
Statement on the Use of
Controlled Substances in the
Treatment of Intractable Pain
Nebraska
N/A
Guidelines for the Use
of Controlled
Substances for the
Treatment of Pain
N/A
Nevada
Nev. Rev. Stat. Ann.
§ 639.23507 (2015)
N/A
NHA Guidelines for Controlled
Substance Prescriptions
New
Hampshire
N.H. Code Admin. R.
Med. 502 (2016);
N.H. Rev. Stat. Ann.
§ 318-B:39 (2016)
Board of Medicine
Guidelines for Pain
Management
N/A
New Jersey
-N.J. Admin. Code
§ 13:35-7.6 (2011);
-N.J. Rev. Stat.
§ 45:1-46.1(a)
(2015);
-N.J. Stat. Ann. §§
24:21-15.2 and 45:9-
22.19 (2017)
N/A
NJ Senate Resolution No. 60
(2016)
New Mexico
N.M. Code R.
§ 16.10.14.10 (2014)
N/A
NMHA Recommended Opioid
Risk-Reduction Strategies and
Prescribing Guidelines in NM
Emergency Departments
New York
-N.Y. Pub. Health
§3334-a(2) (2013);
-N.Y. Pub. Health
§ 3331(5) (2016)
N/A
NYC Emergency Department
Discharge Opioid Prescribing
Guidelines
North
Carolina
N/A
Policy for the Use of
Opioids for the
Treatment of Pain
N/A

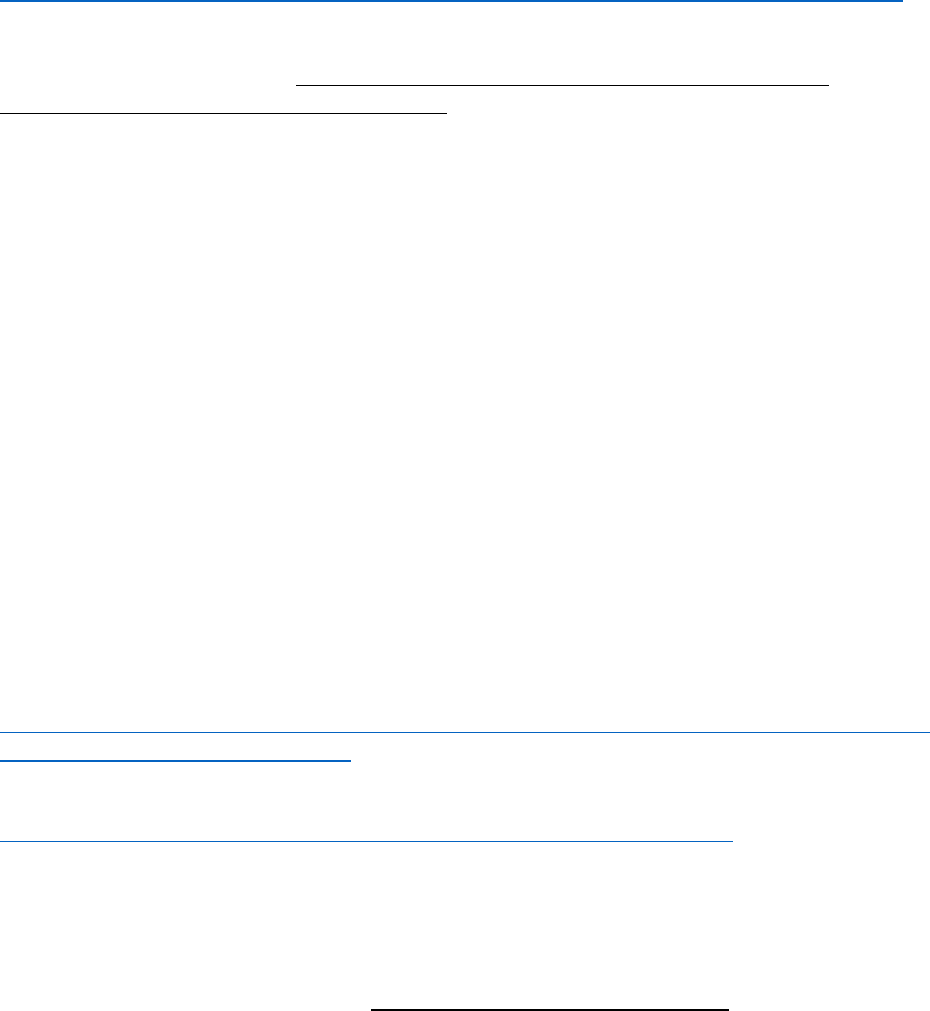
5
Requirements with
the force of law
Quasi-regulatory
guidelines
Advisory Guidelines
North Dakota
N/A
N/A
Safe Prescribing Tips for
Opioids
Ohio
-Ohio Admin. Code
4731-11-11 (2015);
-Pending
N/A
-Ohio Emergency and Acute
Care Facility Opioids and Other
Controlled Substances (OOCS)
Prescribing Guidelines;
-Ohio Guidelines for
Prescribing Opioids for the
Treatment of Chronic Non-
Terminal Pain 80 mg of MED
“Trigger Point”;
-Ohio Guideline for the
Management of Acute Pain
Outside of Emergency
Departments
Oklahoma
-Okla. Stat. Ann. Tit.
63, § 2-302(M)
(2010);
-OHCA’s Opioid
Analgesic Quantity
Limits
N/A
-OK Emergency Department
and Urgent Care Clinic Opioid
Prescribing Guidelines;
-Opioid Prescribing Guidelines
for OK Health Care Providers
in the Office-Based Setting
Oregon
N/A
N/A
-Oregon Pain Guidance
Treatment Guidelines;
-Oregon Opioid Prescribing
Guidelines
Pennsylvania
35 Pa. Cons. Stat. §
872.5
-PA Guidelines on the
Use of Opioids to
Treat Chronic Non-
Cancer Pain;
-PA Emergency
Department Pain
Treatment
Guidelines;
-PA Guidelines on the
Use of Opioids in
dental Practice
N/A
Rhode Island
-R.I. Admin. Code 31-
2-6:3.0 (2014);
-1956 R.I. Gen. Laws
Ann. § 21-28-3.20
(2016)
N/A
N/A
South
Carolina
SCDHHS’s Required
Use of SCRIPTS
Pain Management
Guidelines
N/A

6
Requirements with
the force of law
Quasi-regulatory
guidelines
Advisory Guidelines
South Dakota
N/A
Model Policy for the
Use of Controlled
Substances for the
Treatment of Pain
N/A
Tennessee
-Tenn. Code Ann. §
53-11-308 (20130;
-Tenn. Code Ann. §
53-10-310 (2016)
N/A
Clinical Practice Guidelines for
Outpatient Management of
Chronic Non-Malignant Pain
Texas
22 Tex. Admin. Code
§ 170.3 (2007)
N/A
N/A
Utah
Utah Code Ann. §§
58-37-6(7)(f)(iii)
and 58-37f-304(2)
(2017)
N/A
UT Clinical Guidelines on
Prescribing Opioids for
Treatment of Pain
Vermont
-Vt. Stat. Ann. Tit. 18,
§ 4289(d) (2014);
-VDH’s Rule
Governing the
Prescribing of
Opioids for Pain;
-VDH’s Prescription
Monitoring System
Rule
Policy on the Use of
Opioid Analgesics in
the Treatment of
Chronic Pain
Opiate Prescribing Guidelines
for VT Emergency
Departments
Virginia
Va. Code Ann. § 54.1-
2522.1 (2015)
N/A
-Medical Society of Virginia’s
Guidelines for the Use of
Opioids in the Management of
Chronic Non-Cancer Pain;
-Guidance on the Use of Opioid
Analgesics in the Treatment of
Chronic Pain;
-VA Hospital Emergency
Department Opioid
Prescribing Guidelines
Washington
Wash. Admin. Code
§ 246-919-850
(2011);
N/A
-WA Emergency Department
Opioid Prescribing Guidelines;
-Interagency Guidelines on
Prescribing Opioids for Pain
West Virginia
W. Va. Code Ann.
§ 60a-9-5a (2014)
N/A
Guidance for the Use and
Prescribing of Opioids in
Emergency Departments

7
Requirements with
the force of law
Quasi-regulatory
guidelines
Advisory Guidelines
Wisconsin
Wis. Stat. Ann.
§ 961.385 (2016)
WI Medical
Examining Board
Opioid Prescribing
Guidelines
N/A
Wyoming
N/A
WY Health Care
Licensing Boards’
Uniform Policy for the
Use of Controlled
Substances in the
Treatment of Pain
N/A
Alabama
Requirements with the force of law: Ala. Admin. Code § 540-X-4-.08 (2013).
In 2013, the Alabama Board of Medical Examiners amended its guidelines for the use of
controlled substances for treating pain. The guidelines include performing a patient
evaluation before prescribing opioids, obtaining informed consent from the patient for
opioid treatment, conduct periodic review of the opioid treatment, and maintain a
complete medical record of the patient’s treatment.
Link to the guidelines:
http://www.alabamaadministrativecode.state.al.us/docs/mexam/540-X-4.pdf
Requirements with the force of law: Ala. Admin. Code § 560-X-16-.20 (2014).
Effective October 1, 2013, Alabama’s Medicaid Agency limits the number of outpatient
pharmacy prescriptions to four brand names and five total drugs per month per adult
recipient. In no case can total prescriptions exceed ten per month per recipient.
Link to the rule: http://www.alabamaadministrativecode.state.al.us/docs/med/560-X-
16.pdf
Alaska
Advisory Guidelines: The Alaska Opioid Policy Task Force, within the Alaska Department of
Health and Social Services, has conducted several community meetings to discuss potential
opioid prescription guidelines and will provide recommendations to the governor and
Legislature in November 2016.
For more information, see http://dhss.alaska.gov/AKOpioidTaskForce/Pages/default.aspx.
Arizona
Advisory Guidelines: Arizona Opioid Prescribing Guidelines
Released in November 2014, these are a “voluntary consensus set of guidelines that
promote best practices for prescribing opioids for acute and chronic pain.” The guidelines
were endorsed by a number of state organizations, including the Arizona Medical
8
Association, the Arizona Hospital and Healthcare Association, and the Arizona Nurses
Association.
Summary of guidelines:
- Opioid medications should only be used for treatment of acute pain when the pain
severity warrants that choice, and non-opioid pain medications or therapies do not
provide adequate pain relief.
- When opioid medications are prescribed for treatment of acute pain, the number
dispensed should be no more than the number of doses needed.
- When opioid medications are prescribed for acute pain, patient should be counseled
that:
• Sharing with others is illegal.
• Medications should be stored securely.
• Medications should be disposed of properly when the pain has resolved to
prevent non-medical use of medications.
• Opioids are intended for short-term use only.
• Driving or operating machinery should be avoided if a patient is sedated or
confused while using opioids.
- Long acting opioids should not be used for treatment of acute pain, except in select
opioid tolerant patients, and limited situations.
- The continued use of opioids should be considered carefully, including assessing the
potential for misuse.
- The Arizona Controlled Substances PMP should be checked prior to prescribing
opioids and periodically if renewing opioid prescriptions.
- A comprehensive medical and pain related evaluation that includes assessing for
substance use, psychiatric comorbidities, and functional status should be performed
before initiating opioid treatment for chronic pain.
- The provider should assess for risk of misuse, addiction, or adverse effects, and
perform risk stratification before initiating opioid treatment.
- Initiating opioids in patients with CNTP should ideally be limited to the evidence-
based indication of short term therapy with the purpose of facilitating participation
in a comprehensive care plan; however, if chronic opioid therapy (COT) is
considered, a goal directed trial lasting 30-90 days should be the starting point.
- The provider should obtain and document informed consent including discussion of
risks, benefits, and conditions under which opioids are prescribed or discontinued.
- Clinicians treating patients with opioids for chronic pain should obtain and review
past records when possible.
- Clinicians should consider consultation, when available, for patients with: complex
pain conditions, serious co-morbidities including mental illness, a history or
evidence of current drug addiction or abuse, patients who are pregnant or
breastfeeding.
- An opioid treatment trial should be discontinued if the goals are not met or at any
point if the risks outweigh the benefits or if dangerous or illegal behaviors are
demonstrated.
- COT should be used in the lowest possible doses to achieve treatment goals. Opioid
related adverse events increase with doses >50-100 mg of morphine equivalent
9
dose per day (MEDD) and reaching these doses should trigger a re-evaluation of
therapy.
- Combined use of opioids and benzodiazepines should be avoided if possible.
Link to guidelines: http://www.azdhs.gov/documents/audiences/clinicians/clinical-
guidelines-recommendations/prescribing-guidelines/az-opiod-prescribing-guidelines.pdf
Requirements with the force of law: Executive Order 2016-06
On October 24, 2016, Governor Dough Ducey issued an executive order limiting all initial
prescriptions of opioids to no more than a seven-day dose. The order only applies to
situations in which the state is the payer, specifically for Medicaid beneficiaries and state
employees enrolled in the state health insurance plan.
Link to the Executive Order:
http://azgovernor.gov/sites/default/files/prescription_opioid_initial_fill_limitation_e.o_0.p
df
Arkansas
Requirements with the force of law: Ark. Code Ann. § 20-7-703 (2015).
This law requires Arkansas hospitals with an emergency department to adopt guidelines
concerning prescribing of opioids in the emergency department. The guidelines must
address treatment of chronic pain and acute pain; limits on amounts or duration of opioid
prescriptions; and identification of situations where opioid prescriptions should be
discouraged or prohibited.
Link to the statute: http://law.justia.com/codes/arkansas/2015/title-20/subtitle-
2/chapter-7/subchapter-7/section-20-7-703
Advisory Guidelines: Arkansas Emergency Department Opioid Prescribing Guidelines
Intended to help EDs reduce the inappropriate use of opioid analgesics while preserving
the vital role of the ED to treat patients with emergent medical conditions, these ED
prescribing guidelines were adopted by the Arkansas Department of Health, the Arkansas
Hospital Association, and the Arkansas Medical Society, among others.
Specific guidelines:
- One medical provider should provide all opioids to treat a patient’s chronic pain.
- The administration of intravenous and intramuscular opioids in the ED for the relief
of acute exacerbations of chronic pain is discouraged.
- Emergency medical providers should not provide replacement prescriptions for
controlled substances that were lost, destroyed or stolen.
- Emergency medical providers should not provide replacement doses of methadone
for patients in a methadone treatment program.
- Long-acting or controlled-release opioids (such as OxyContin®, fentanyl patches,
and methadone) should not be prescribed from the ED.
- EDs are encouraged to use the Arkansas PDMP on appropriate patients.
- Physicians should send patient pain agreements to local EDs and work to include a
plan for pain treatment in the ED.

10
- EDs are encouraged to photograph patients who present for pain related complaints
without a government issued photo ID.
- EDs should perform screening, brief interventions and treatment referrals for
patients with suspected prescription opiate abuse problems.
- The administration of Deme-rol® (Meperidine) in the ED is discouraged.
- For exacerbations of chronic pain, the emergency medical provider should contact
the patient’s primary opioid prescriber or pharmacy.
- The emergency medical provider should only prescribe enough pills to last until the
office of the patient’s primary opioid prescriber opens.
- Prescriptions for opioid pain medication from the ED for acute injuries, such as
fractured bones, in most cases should not exceed 30 pills.
- ED patients should be screened for substance abuse prior to prescribing opioid
medication for acute pain.
Ling to guidelines:
http://www.arkhospitals.org/Misc.%20Files/Arkansas%20Emergency%20Department%2
0Opioid%20Prescribing%20Guidelines.pdf
California
Quasi-regulatory guidelines: Guidelines for Prescribing Controlled Substances for Pain
These guidelines were adopted by the Medical Board of California in November 2014 with
the purpose of helping physicians improve outcomes of patient care to prevent overdose
deaths due to opioid use. The guidelines recommend that physicians proceed cautiously
(yellow flag warning) once the Morphine Equivalent Dose (MED) reaches 80 mg/day. When
higher doses are contemplated, referral to a specialist is recommended.
Link to guidelines: http://www.mbc.ca.gov/licensees/prescribing/pain_guidelines.pdf
Colorado
Advisory Guidelines: Joint Policy for Prescribing and Dispensing Opioids
In October 2014, the Colorado Department of Regulatory Agencies (DORA), in collaboration
with the Colorado Dental Board, the Colorado Medical Board, the State Board of Nursing,
and the State Board of Pharmacy, issued the Joint Policy for Prescribing and Dispensing
Opioids. The Policy recommended limiting opioid prescriptions to 90 days in duration, 120
MME, or certain formulations such as transdermal or long-acting preparations.
Link to guidelines:
http://www.painpolicy.wisc.edu/sites/www.painpolicy.wisc.edu/files/Colorado_Joint%20
Bd_Policy%20for%20Prescribing%20and%20Dispensing%20Opioids.pdf
Requirements with the force of law:
- In August 2014, the Colorado Department for Health Care Policy and Financing
(DHCPF), which administers the state’s Medicaid program, adopted the
recommendations of the Joint Policy and started limiting short-acting oral opioid
prescriptions to a maximum of four tablets a day or 120 tablets per 30 days.

11
For more information, see
https://www.colorado.gov/pacific/sites/default/files/Stakeholder%20communication%2
0regarding%20new%20short-acting%20opioid%20policy.pdf
- In February 2016, the DHCPF began limiting long-acting opioid prescriptions to a
maximum of 300 MME per day. The Department also announced that the short-
acting opioid policy would continue to be in effect.
For more information, see
https://www.colorado.gov/pacific/sites/default/files/MME%20Policy%20Update%20-
%20University.pdf
Connecticut
Advisory Guidelines: Connecticut Emergency Department Opioid Prescribing Guidelines
In January 2015, the Connecticut Hospital Association and the Connecticut College of
Emergency Physicians issued joint guidelines to “to assist emergency medical personnel
(EMPs) in addressing the care needs of persons who come to the Emergency Department
(ED), and who have a chronic pain condition that may involve the use of opioids.”
Specific guidelines include:
- The ED should coordinate the care of patients who frequently visit the ED, using an
ED care coordination program, to the extent possible.
- ED opioid prescriptions for acute injuries should be in an amount that will last until
the patient is reasonably able to receive follow-up care for the injury. In most cases,
this should not exceed thirty (30) pills.
- ED patients should be asked about a history of current substance abuse prior to
prescribing opioids for acute pain. Opioids should be prescribed with great caution
in the context of a substance abuse history.
- EMPs generally should not provide replacement prescriptions for controlled
substances that were lost, destroyed, or stolen.
- EMPs generally should not provide replacement doses for Methadone or Suboxone,
but special consideration may be given in the event of natural disasters or other
exigent circumstances.
- EMPs generally should not prescribe long-acting opioids (e.g. Oxycontin, Fentanyl
patches, and methadone) for acute pain management.
- EMPs should exercise caution when considering prescribing opioids for ED patients
in situations in which the identity of the individual cannot be verified.
Link to guidelines: http://csms.org/wp-content/uploads/2015/02/Opioid-Guidelines-
FINAL-1_20_2015.pdf
Requirements with the force of law: Conn. Gen. Stat. Ann. § 21a-254(9) (2015)
In 2015, Connecticut passed a law to require prescribers of opioids to review the patient’s
record on the state’s prescription monitoring program before initiating prescribing a
controlled substance. The statute provides as follows:
Prior to prescribing greater than a seventy-two-hour supply of any controlled
substance to any patient, the prescribing practitioner or such practitioner's authorized

12
agent shall review the patient's records in the electronic prescription drug monitoring
program established pursuant to this subsection.
Link to the CT’s amended controlled substance statute:
https://www.cga.ct.gov/2015/TOB/h/pdf/2015HB-06856-R00-HB.pdf
Requirements with the force of law: Conn. Gen. Stat. Ann. § 17a-714a (2016)
On May 27, 2016, the Governor of Connecticut signed HB 5053 into law to expand the
state’s effort to combat the opioid epidemic. The new law includes a provision to limit the
prescribing of opioid drugs by:
- prohibiting, for adult patients, an initial prescription of opioid drugs for longer than
seven days
- prohibiting, for minor patients, any prescriptions of opioid drugs for longer than
seven days and requiring the prescriber to discuss the risks associated with the
drug with the patient
- allowing, for both adult and minor patients, a prescriber to give more than a seven-
day supply of opioid drugs if, in the prescriber's professional medical judgement, the
acute or chronic pain condition requires it and requires the prescriber to note such
condition in the medical record
For more information, see
http://portal.ct.gov/Departments_and_Agencies/Office_of_the_Governor/Press_Room/Pres
s_Releases/2016/05-
2016/Gov__Malloy_Signs_Comprehensive_Bill_Combating_Opioid_Abuse_and_Launches_Str
ategic_Plan_to_Tackle_Addiction/
For the language of the statute, see https://www.cga.ct.gov/2016/ACT/pa/2016PA-00043-
R00HB-05053-PA.htm
Delaware
Requirements with the force of law: Del. Admin. Code C.S.A. 4.0 (2017)
In January 2017, the Delaware Department of State issued new regulations to address the
problem of opioid prescription abuse and misuse. The new regulations limit opioid
prescribing practices in the following ways:
- For an acute injury or procedure, a practitioner can prescribe a maximum initial
seven-day supply of an opioid medication before additional steps are required.
- For minors, practitioners are barred from issuing an opioid prescription for longer
than seven days and are required to discuss the reasons for why an opioid
prescription is necessary with the minor’s parents.
- Prescribing beyond a seven-day supply or for additional prescriptions after the first
seven-day supply, the practitioner will be required to check the patient’s
prescription history in the State’s PMP along with obtaining informed consent
from the patient for risks of such things as potential addiction, abuse, misuse, and
risks of life-threatening respiratory depression and accidental overdose, which can
be fatal.
13
- For patients being treated for chronic pain, practitioners will be required to check
the state’s PMP and administer a urine drug screening at least twice a year while
receiving chronic treatment with opioid medications. The practitioner must also
consider and discuss alternative treatment options with a patient, and conduct a
risk assessment to identify patients that are or may be at risk for dependence or
misuse of a prescribed opioid. A signed treatment agreement will also be required
for these patients.
For the language of the rule, see:
http://regulations.delaware.gov/AdminCode/title24/Uniform%20Controlled%20Substanc
es%20Act%20Regulations.shtml
Advisory Guidelines: Guidelines for Use of Controlled Substances for the Treatment of Pain
The Medical Society of Delaware issued advisory guidelines for prescribing opioids to treat
pain. Recommendations include performing a patient evaluation before prescribing
opioids, obtaining informed consent from the patient for opioid treatment, requiring a
written agreement outlining patient responsibilities if the patient is determined to be at
high risk for medication abuse or to have a history of substance abuse, conduct periodic
review of the opioid treatment, and maintain a complete medical record of the patient’s
treatment.
Link to guidelines:
http://www.medicalsocietyofdelaware.org/Portals/1/PMP/Guidelines%20for%20Control
led%20Substances%20for%20treatment%20of%20Pain%20April%202013.pdf
Advisory Guidelines: Delaware Emergency Department Opioid Prescribing Guidelines
Intended to help EDs reduce the inappropriate use of opioid analgesics while preserving
the vital role of the ED to treat patients with emergent medical conditions, these ED
prescribing guidelines were adopted by the Medical Society of Delaware.
Specific guidelines:
- One medical provider should provide all opioids to treat a patient’s chronic pain.
- The administration of intravenous and intramuscular opioids in the ED for the relief
of acute exacerbations of chronic pain is discouraged.
- Emergency medical providers should not provide replacement prescriptions for
controlled substances that were lost, destroyed or stolen.
- Emergency medical providers should not provide replacement doses of methadone
for patients in a methadone treatment program.
- Long-acting or controlled-release opioids (such as OxyContin®, fentanyl patches,
and methadone) should not be prescribed from the ED.
- EDs are encouraged to use the Arkansas PDMP on appropriate patients.
- Physicians should send patient pain agreements to local EDs and work to include a
plan for pain treatment in the ED.
- EDs are encouraged to photograph patients who present for pain related complaints
without a government issued photo ID.
- EDs should perform screening, brief interventions and treatment referrals for
patients with suspected prescription opiate abuse problems.

14
- The administration of Deme-rol® (Meperidine) in the ED is discouraged.
- For exacerbations of chronic pain, the emergency medical provider should contact
the patient’s primary opioid prescriber or pharmacy.
- The emergency medical provider should only prescribe enough pills to last until the
office of the patient’s primary opioid prescriber opens.
- Prescriptions for opioid pain medication from the ED for acute injuries, such as
fractured bones, in most cases should not exceed 30 pills.
ED patients should be screened for substance abuse prior to prescribing opioid medication
for acute pain.
Link to guidelines:
https://www.acep.org/uploadedFiles/ACEP/Membership/Sections_of_Membership/qips/
articles/Delaware%20Emergency%20DepartmentOpioid%20Prescribing%20Guidelines%
20Revised%201221....pdf
Florida
Quasi-regulatory guidelines: Florida State Opioid Prescribing Policy
The Florida Boards of Medicine and Osteopathic Medicine adopted a policy for the
prescribing of opioids that set the standard of care for the state. The guidelines include
performing a patient evaluation before prescribing opioids, obtaining informed consent
from the patient for opioid treatment, requiring a written agreement outlining patient
responsibilities if the patient is determined to be at high risk for medication abuse or to
have a history of substance abuse, conduct periodic review of the opioid treatment, and
maintain a complete medical record of the patient’s treatment.
Link to the policy: http://fapmmed.net/State_Opioid_Prescribing_Policy.pdf
Georgia
Requirements with the force of law: Ga. Comp. R. & Regs. 360-3-.06 (2013)
The Georgia Composite Medical Board issued regulations to establish the appropriate
standard of care with respect to the prescribing of controlled substances in 2013.
Requirements include:
- Physicians cannot delegate the dispensing of controlled substances to unlicensed
person.
- When initially prescribing a controlled substance for the treatment of pain or
chronic pain, a physician shall have a medical history of the patient, a physical
examination of the patient shall have been conducted, and informed consent shall
have been obtained.
- In the event of a documented emergency, a physician may prescribe an amount of
medication to cover a period of not more than 72 hours without a physical
examination.
- When a physician is treating a patient with controlled substances for pain or
chronic pain for a condition that is not terminal, the physician shall obtain or make
a diligent effort to obtain any prior diagnostic records relative to the condition for
which the controlled substances are being prescribed and shall obtain or make a
diligent effort to obtain any prior pain treatment records.

15
- When a physician determines that a patient for whom he is prescribing controlled
scheduled substances is abusing the medication, then the physician shall make an
appropriate referral for treatment for substance abuse.
- When prescribing a Schedule II or III controlled substance for 90 consecutive days
or greater for the treatment of chronic pain arising from conditions that are not
terminal or patients who are not in a nursing home or hospice, a physician must
have a written treatment agreement with the patient and shall require the patient
to have a clinical visit at least once every three months, while treating for pain, to
evaluate the patient's response to treatment.
- The requirement of a visit at a minimum of once every three months can be waived
and the clinical visit be at least once per year if the doctor determines there is a
substantial hardship and documents such hardship in the patient's record or if the
morphine equivalent daily dose (“MEDD”) is 30 mg. or less.
Link to the guidelines: http://rules.sos.state.ga.us/GAC/360-3-.06
Hawaii
Advisory Guidelines: Emergency Department Opioid Prescription Guidelines
With the purpose of ensuring and protecting the appropriate use of prescription opioid
medications, while attempting to reduce opioid abuse and diversion in the state, the Hawaii
Chapter of the American College of Emergency Physicians adopted the following guidelines
for the prescribing of opioid medications in emergency departments:
- Consider short-acting opioid analgesics for the treatment of acute pain only when
the severity of the pain is reasonably assumed to warrant their use.
- If opioid analgesics are prescribed, use the lowest possible safe and effective dose.
- Prescribe short courses of opioid analgesics for acute pain. Most patients require no
more than three days of medication.
- Avoid prescribing long-acting or controlled-release opioid analgesics.
- Consider accessing Hawaii’s PMP for information on the patient’s controlled
substance prescription history before providing opioid prescriptions. To assess for
opioid abuse or addiction, consider using targeted history or validated screening
tools.
- Consider risk factors for respiratory depression and use caution when prescribing
opioid analgesics to patients being treated with benzodiazepines or other opioids.
- Avoid administering intravenous or intramuscular opioid analgesics for acute
exacerbations of chronic pain.
- One medical provider should provide all opioid medications to treat a patient’s
chronic pain.
- Avoid providing replacement prescriptions for controlled substances that were lost,
destroyed, or stolen. Replacement doses of methadone should not be provided in
the emergency department.
- Attempt to coordinate the care of patients who frequently seek care in the ED
among emergency, primary care, and specialty providers. Primary care and pain
management physicians should make patient pain agreements accessible to local
emergency departments and work to include a plan for pain treatment in the ED.
16
- Provide information about the risks of opioid analgesics, including overdose and
addiction, along with information about proper storage and disposal to those
receiving a prescription.
- Hospitals are required by law to provide a medical screening examination to
determine if a patient has an emergency medical condition. The law does not
require physicians to use opioid analgesics to treat pain.
Link to guidelines:
http://www.hawaiiacep.org/uploadedFiles/Hawaii/Opioid%20Guidelines%20Final.pdf
Idaho
Quasi-regulatory guidelines: Idaho Board of Medicine Policy for the Use of Opioid
Analgesics in the Treatment of Chronic Pain
In September 2013, the Idaho Board of Medicine adopted a new policy regarding the use of
opioids for treating chronic pain. The policy included guidelines like:
- The medical record should document the presence of one or more recognized
medical indications for prescribing an opioid analgesic.
Such an evaluation should be completed before a decision is made as to whether to
prescribe an opioid analgesic.
- Assessment of the patient’s personal and family history of alcohol or drug abuse and
relative risk for medication misuse or abuse should be part of the initial evaluation
and should be completed prior to a decision as to whether to prescribe opioid
analgesics.
- Where available, the state PDMP should be consulted to determine whether the
patient is receiving prescriptions from any other physicians.
- Safer alternative treatments should be considered before initiating opioid therapy
for chronic, non-malignant pain. Opioid therapy should be presented to the patient
as a therapeutic trial for a defined period of time (usually no more than 90 days). A
decision to continue opioid therapy beyond the trial period should reflect a careful
evaluation of benefits versus adverse events and/or potential risks.
- Periodic drug testing may be useful in monitoring adherence to the treatment plan,
as well as in detecting the use of non-prescribed drugs.
Link to guidelines:
https://bom.idaho.gov/BOMPortal/BOM/PDF%20FORMS/ModelPolicyUseofOpioidAnalge
sicsinTreatmentofChronicPain.pdf
For more information, see:
https://www.idmed.org/idaho/assets/files/AM2016/DuBose_Addt.pdf
Illinois
No data found.
Indiana
Requirements with the force of law: 844 Ind. Admin. Code 5-6-3 (2014)

17
In September 2014, the Indiana Medical Licensing Board adopted a rule that regulates
physicians engaged in the practice of pain management prescribing.
Summary of requirements:
- The rule only applies if a patient has been prescribed:
• more than 60 opioid containing pills a month for more than three
consecutive months;
• a morphine equivalent dose of more than 15mg per day for more than three
consecutive months;
• a transdermal opioid patch for more than three consecutive months;
• tramadol, but only if the patient’s tramadol dose reaches a morphine
equivalent dose of more than 60mg per day for more than three consecutive
months; or
• a hydrocodone extended release medication that is not in abuse deterrent
form.
- Physicians must perform an initial evaluation, discuss the risks and benefits of
opioids, review a treatment agreement, schedule periodic visits, run a PDMP report
at the outset of an opioid treatment plan and annually thereafter, and order drug
testing as necessary.
- When a patient’s opioid dose reaches 60 mg MED/day, a face to face review of the
treatment plan and patient evaluation must be scheduled, including consideration of
a referral to a specialist.
- If treatment continues with an MED of more than 60 mg/day, the physician must
develop a revised assessment and treatment plan for ongoing treatment, if the
physician continues to provide ongoing opioid treatment.
For the language of the rule, see http://www.ismanet.org/pdf/legal/FinalRule102516.pdf
For a summary of the rule, see
http://www.ismanet.org/pdf/legal/IndianaPainManagementPrescribingFinalRuleSummar
y.pdf
Iowa
Requirements with the force of law: Iowa Admin. Code § 653-13.2 (2016)
In September 2016, the Iowa Medicine Board adopted an amendment to the regulations
concerning the management of chronic pain. The new rule requires opioid-prescribing
physicians to adhere to the CDC guidelines when prescribing opioids for chronic pain to
patients 18 years of age and older.
For the language of the amendment, see
https://medicalboard.iowa.gov/iowa_code/proposed%20rules/pdf/ARC%202535C%20-
%20Chapter%2013_CDC%20Guidelines%20for%20Prescribing.pdf
For more information, see
http://www.medicalboard.iowa.gov/Board%20News/2016/Press%20release%20-
%20Board%20adds%20CDC%20guideline%20on%20opioid%20prescribing%20to%20lis

18
t%20of%20resources%20for%20physicians%20who%20treat%20chronic%20pain%20-
%20%20August%2029%202016.pdf
Kansas
Quasi-regulatory guidelines: Joint Policy Statement of the Boards of Healing Arts, Nursing
and Pharmacy on the Use of Controlled Substances for the Treatment of Pain
In June 2002, the Kansas Boards of Healing Arts, Nursing, and Pharmacy issued a joint
statement describing what the Boards considered to be the best practices for prescribing
opioids to treat acute pain. Recommendations include performing a patient assessment
before prescribing opioids, obtaining informed consent from the patient for opioid
treatment, requiring a written agreement outlining patient responsibilities if the patient is
determined to be at high risk for medication abuse or to have a history of substance abuse,
conduct periodic review of the opioid treatment, and maintain a complete medical record
of the patient’s treatment.
Link to the Joint Statement:
http://www.ksbn.org/positionstatements/joint_policy_statement.pdf
Kentucky
Requirements with the force of law: 201 Ky. Admin Regs. 9:260 (2013)
In 2013, the Kentucky Board of Medical Licensure adopted new Professional Standards for
the Prescribing or Dispensing of Controlled Substances in different situations. Some of
these requirements include:
- Obtaining an appropriate medical history relevant to the medical complaint,
including a history of present illness
- Obtaining and review a KASPER (Kentucky’s PDMP) report for that patient for the
twelve (12) month period immediately preceding the patient encounter, and
appropriately utilize that information in the evaluation and treatment of the patient;
- After examining the benefits and risks of prescribing or dispensing a controlled
substance to the patient, including non-treatment or other treatment, make a
deliberate decision that it is medically appropriate to prescribe or dispense the
controlled substance in the amount specified;
- Not prescribe or dispense a long-acting or controlled-release opioid (e.g. OxyContin,
fentanyl patches, or methadone) for acute pain that is not directly related to and
close in time to a specific surgical procedure;
- Explain to the patient that a controlled substance used to treat an acute medical
complaint is for time-limited use, and that the patient should discontinue the use of
the controlled substance when the condition requiring the controlled substance use
has resolved; and
- Explain to the patient how to safely use and properly dispose of any unused
controlled substance.
Similar requirements were adopted for opioid prescribing in other situations, including
long-term opioid therapy and opioid prescribing in emergency departments.
Link to the statute: http://www.lrc.state.ky.us/kar/201/009/260.htm

19
Link to statute summary:
http://kbml.ky.gov/hb1/Documents/Summary%20of%20201%20KAR%209_260.pdf
Quasi-regulatory guidelines: Guidelines for the Use of Controlled Substances in Pain
Treatment
The Kentucky Board of Medical Licensure issues advisory guidelines for prescribing
opioids to treat acute pain. Recommendations include performing a patient evaluation
before prescribing opioids (including analyzing the patient’s KASPER report), obtaining
informed consent from the patient for opioid treatment, requiring a written agreement
outlining patient responsibilities if the patient is determined to be at high risk for
medication abuse or to have a history of substance abuse, conduct periodic review of the
opioid treatment, and maintain a complete medical record of the patient’s treatment
Link to the guidelines: http://www.kentucky.com/latest-
news/article40998984.ece/BINARY/Kentucky%20Board%20of%20Medical%20Licensure
's%20guidelines%20for%20the%20use%20of%20controlled%20substances%20in%20pa
in%20treatment
Requirements with the force of law: Ky. Rev. Stat. Ann. § 218A.205(3)(b) (2017)
In 2017, Kentucky enacted an act to limit prescriptions of opioid prescriptions to a three-
day supply. The act prohibits practitioners from issuing a prescription for a Schedule II
substance for more than three days if the prescription is intended to treat pain as an acute
medical condition. The following exceptions apply:
- The practitioner believes that more than a three-day supply is necessary to treat the
patient’s pain as an acute medical condition and the practitioner documents the
condition and the lack of alternative options;
- Prescription issued to treat chronic pain;
- Prescription issued to treat pain associated with a cancer diagnosis;
- Prescription issued as part of a narcotic treatment program;
- Prescription issued to treat pain following a major surgery or the treatment of
significant trauma;
- The substance is dispensed or administer directly to an ultimate user in an inpatient
setting;
- Any additional treatment scenario deemed medically necessary by the state
licensing board in consultation with the Kentucky Office of Drug Control Policy
Link to the enacted act:
http://www.lrc.ky.gov/recorddocuments/bill/17RS/HB333/bill.pdf
Louisiana
Requirements with the force of law: La. Stat. Ann. § 40:978 (2015)
In 2015, Louisiana amended its controlled substances statute to limit opioid prescriptions
to ten (10) days if the prescribing physician is not licensed by the state of Louisiana and the
drug prescribed is a Schedule II or Schedule III opioid derivative. In 2016, the statute was
again amended to add an exception to this requirement for diagnosis of cancer or terminal
illness.

20
Link to the amended statute: http://law.justia.com/codes/louisiana/2014/code-
revisedstatutes/title-40/rs-40-978
Maine
Requirements with the force of law: 02-373 Me. Code R. 21 § II (2012)
In 2013, the Maine Boards of Osteopathic Licensure, Licensure in Medicine, Dental
Examiners, Nursing, and Podiatric Medicine issued a joint statement on the use of
controlled substances for treatment of pain. The regulations were adopted as part of the
Maine Code of Rules and include performing a patient evaluation before prescribing
opioids (including analyzing the patient’s PDMP record), obtaining informed consent from
the patient for opioid treatment, requiring a written agreement outlining patient
responsibilities if the patient is determined to be at high risk for medication abuse or to
have a history of substance abuse, conduct periodic review of the opioid treatment, and
maintain a complete medical record of the patient’s treatment
Link to the regulations:
https://www1.maine.gov/osteo/administrative/chaptertwentyone.pdf
Requirements with the force of law: 32 Maine Rev. Stat. Ann. § 3300-F (2016)
In 2016, the Main Legislature amended the state’s statute related to professional licensing
to adopt the following limitations on prescribers’ practices: a licensed physician whose
scope of practice includes prescribing opioid medication may not prescribe:
- To a patient any combination of opioid medication in an aggregate amount in excess
of 100 morphine milligram equivalents (MME) of opioid medication per day;
- To a patient who, on the effective date of this section, has an active prescription for
opioid medication in excess of 100 MME of an opioid medication per day, an opioid
medication in an amount that would cause that patient's total amount of opioid
medication to exceed 300 MME of opioid medication per day; except that, on or after
July 1, 2017, the aggregate amount of opioid medication prescribed may not be in
excess of 100 MME of opioid medication per day;
- On or after January 1, 2017, within a 30-day period, more than a 30-day supply of an
opioid medication to a patient under treatment for chronic pain.
- On or after January 1, 2017, within a 7-day period, more than a 7-day supply of an
opioid medication to a patient under treatment for acute pain.
Exceptions to these requirements include 1) when prescribing opioid medication for pain
associated with active and aftercare cancer treatment, palliative care, end-of-life and
hospice care, and medication-assisted treatment (MAT); and 2) when directly ordering or
administering benzodiazepine or opioid medication to a person in an emergency room
setting, an inpatient hospital setting, a long-term care facility, or a residential care facility.
Link to the statute: https://legislature.maine.gov/legis/statutes/32/title32sec3300-F.html
Requirements with the force of law: 22 Maine Rev. Stat. Ann § 7253 (2016)

21
The legislature also added a provision to the state’s Controlled Substances Prescription
Monitoring Act that requires, upon initial prescription of a benzodiazepine or an opioid
medication to a person and every 90 days for as long as that prescription is renewed, a
prescriber to check prescription monitoring information for records related to that person.
This provision takes effect on January 1, 2017.
Link to the statute: https://legislature.maine.gov/legis/statutes/22/title22sec7253.html
Maryland
Advisory Guidelines: Maryland Emergency Department Opioid Prescribing Guidelines
In September 2015, the Maryland Hospital Association, in conjunction with the Maryland
Chapter of the American College of Emergency Physicians, developed opioid prescribing
guidelines to be used in emergency departments in the state. The guidelines include:
- Hospitals, in conjunction with ED personnel, should develop a process to screen for
substance misuse that includes services for brief intervention and referrals to
treatment programs for patients who are at risk for developing, or who actively
have, substance use disorders.
- When possible, ED providers, or their delegates, should consult the Maryland
Prescription Drug Monitoring Program (PDMP) before writing an opioid
prescription.
- Hospitals should develop a process to share the ED visit history of patients with
other providers and hospitals that are treating the patients by using CRISP,
Maryland’s health information exchange.
- For acute exacerbations of chronic pain, the ED provider should attempt to notify
the patient’s primary opioid prescriber or primary care provider of the visit and the
medication prescribed.
- ED providers should not provide prescriptions for controlled substances that were
lost, destroyed, or stolen. Further, ED providers should not provide doses of
methadone or buprenorphine for patients in a treatment program, unless the dose is
verified with the treatment program and the patient’s ED evaluation and treatment
has prevented them from obtaining their scheduled dose.
- Unless otherwise clinically indicated, ED providers should not prescribe long-acting
or controlled-release opioids, such as OxyContin®, fentanyl patches, and
methadone.
- When opioid medications are prescribed, the ED staff should counsel the patient:
• to store the medications securely, not share them with others, and dispose of
them properly when their pain has resolved;
• to use the medications only as directed for medical purposes; and
• to avoid using opioids and concomitant sedating substances due to the risk of
overdose.
- As clinically appropriate and weighing the feasibility of timely access for a patient to
appropriate follow-up care and the problems of excess opioids in communities, ED
providers should prescribe no more than a short course and minimal amount of
opioid analgesics for serious acute pain, lasting no more than three days.

22
Link to the guidelines: http://www.mhaonline.org/docs/default-
source/Resources/Opioid-Resources-for-Hospitals/maryland-emergency-department-
opioid-prescribing-guidelines.pdf?sfvrsn=2
Requirements with the force of law: Md. Code Ann., Health Occ. § 1-223 (2017)
Since 2017, Maryland provides that, “on treatment for pain, a health care provider, based
on the clinical judgment of the health care provider, shall prescribe: (1) the lowest effective
dose of an opioid; and (2) a quantity that is no greater than the quantity needed for the
expected duration of pain severe enough to require an opioid that is a controlled dangerous
substance […].” The following circumstances are exempted:
- Opioid prescribed for a substance-related disorder;
- Opioid prescribed for pain associated with a cancer diagnosis;
- Opioid prescribed for pain experienced while the patient is receiving end-of-life,
hospice, or palliative care services; or
- - opioid prescribed for chronic pain
Link to the enacted bill: http://mgaleg.maryland.gov/2017RS/bills/hb/hb1432T.pdf
Massachusetts
Quasi-regulatory guidelines: Prescribing Practices Policies and Guidelines
In 2015, the Massachusetts Board of Registration in Medicine amended its prescribing
guidelines to address the opioid epidemic. The Board adopted the Massachusetts Medical
Society’s Opioid Therapy and Physician Communication Guidelines. The guidelines include
directions for opioid therapy for acute pain and chronic pain.
Summary of guidelines for acute pain:
- Physicians must be familiar with and follow the requirements of the law and
regulations on use of the prescription monitoring program prior to initiating opioid
treatment.
- Patients should be screened or assessed for pregnancy, personal or family histories
of substance use disorder, mental health status, or relevant behavioral issues.
- Physicians prescribing opioids should inform their patients about the cognitive and
performance effects of these prescriptions.
- When clinically indicated, opioids should be initiated as a short-term trial to assess
the effects and safety of opioid treatment on pain intensity, function, and quality of
life. In most instances, the trial should begin with a short-acting opioid medication.
- The starting dosage should be the minimum dosage necessary to achieve the desired
level of pain control and to avoid excessive side effects.
- Duration should be short term with possible partial fill prescriptions or short term,
low dosage sequential prescription approaches considered.
- Concurrent prescriptions should be reviewed, including paying close attention to
benzodiazepines and other medications that may increase the risks of harm
associated with opioid use.
- Patients should be counseled to store the medications securely, never share with
others, and properly dispose of unused and expired prescriptions.

23
Summary of guidelines for chronic pain:
- Threshold for Considering Pain Chronic:
• The MMS supports a duration of treatment of 90 days, consistent with the,
rather than morphine equivalents to trigger these guidelines.
• This time period should trigger a face-to-face reevaluation of the treatment
provided to date, its long-term efficacy, and risks of continued opioid
therapy.
- A detailed reevaluation of the patient’s history and a physical should be done as
soon as possible after the 90-day threshold is reached.
- The physician should do a risk of substance abuse assessment (the physician should
consider the use of appropriate baseline urine drug testing if the risk assessment or
other evidence indicates there may be issues with use of other drugs).
- The physician should tailor a diagnosis and treatment plan with functional goals at
the initial 90-day threshold visit and every 60 to 90 days thereafter
Link to the Board’s guidelines: http://www.mass.gov/eohhs/docs/borim/policies-
guidelines/policy-15-05.pdf
Link to the MMS’s guidelines: http://www.massmed.org/Advocacy/Key-Issues/Opioid-
Abuse/Opioid-Therapy-and-Physician-Communication-Guidelines-(pdf)/
Advisory Guidelines: Massachusetts Hospital Association Guidelines for Emergency
Department Opioid Management
The MHA Substance Use Disorder Prevention and Treatment Task Force developed opioid
prescribing guidelines to be used in emergency departments in the state. The guidelines
include:
- Hospitals, in conjunction with ED personnel, should develop a process to screen for
substance misuse that includes services for brief intervention and referrals to
treatment programs for patients who are at risk for developing substance use
disorders.
- When possible, ED providers, or their delegates, should consult the Maryland PDMP
before writing an opioid prescription.
- Hospitals should develop a process to share the ED visit history of patients with
other providers and hospitals that are treating the patients by using CRISP,
Maryland’s health information exchange.
- For acute exacerbations of chronic pain, the ED provider should attempt to notify
the patient’s primary opioid prescriber or primary care provider of the visit and the
medication prescribed.
- ED providers should not provide prescriptions for controlled substances that were
lost, destroyed, or stolen. Further, ED providers should not provide doses of
methadone or buprenorphine for patients in a treatment program, unless the dose is
verified with the treatment program.
- Unless otherwise clinically indicated, ED providers should not prescribe long-acting
or controlled-release opioids, such as OxyContin®, fentanyl patches, and
methadone.

24
- When opioid medications are prescribed, the ED staff should counsel the patient:
• to store the medications securely, not share them with others, and dispose of
them properly when their pain has resolved;
• to use the medications only as directed for medical purposes; and
• to avoid using opioids and concomitant sedating substances due to the risk of
overdose.
- ED providers should prescribe no more than a short course and minimal amount of
opioid analgesics for serious acute pain, lasting no more than three days.
Link to the guidelines:
https://www.mhalink.org/AM/Template.cfm?Template=/CM/ContentDisplay.cfm&Conten
tID=50511&FusePreview=True&WebsiteKey=a3f1fffe-a9f6-4b95-a06a-a551e90c7801
Requirements with the force of law: Mass. Ann. Laws ch. 94C, § 19D (2016)
In March 2016, Massachusetts adopted opioid prescribing limitations. The limitations do
not apply to medications designed for the treatment of substance abuse or opioid
dependence. The requirements of the new law are:
- When issuing a prescription for an opiate to an adult patient for outpatient use for
the first time, a practitioner shall not issue a prescription for more than a 7-day
supply. A practitioner shall not issue an opiate prescription to a minor for more than
a 7-day supply at any time and shall discuss with the parent or guardian of the
minor the risks associated with opiate use and the reasons why the prescription is
necessary.
- If, in the professional medical judgment of a practitioner, more than a 7-day supply
of an opiate is required to treat the adult or minor patient’s acute medical condition
or is necessary for the treatment of chronic pain management, pain associated with
a cancer diagnoses or for palliative care, then the practitioner may issue a
prescription for the quantity needed to treat such acute medical condition, chronic
pain, pain associated with a cancer diagnosis or pain experienced while the patient
is in palliative care. The condition triggering the prescription of an opiate for more
than a 7-day supply shall be documented in the patient’s medical record and the
practitioner shall indicate that a non-opiate alternative was not appropriate to
address the medical condition.
Link to the statute:
https://malegislature.gov/Laws/GeneralLaws/PartI/TitleXV/Chapter94C/Section19D
Michigan
Quasi-regulatory guidelines: Guidelines for the Use of Controlled Substances for the
Treatment of Pain
In 2002, the Michigan Boards of Medicine and Osteopathic Medicine & Surgery adopted its
guidelines for the prescribing of controlled substances for the treatment of pain. The
guidelines, which do not have the force of law, include performing a patient evaluation
before prescribing opioids, obtaining informed consent from the patient for opioid
treatment, requiring a written agreement outlining patient responsibilities if the patient is

25
determined to be at high risk for medication abuse or to have a history of substance abuse,
conduct periodic review of the opioid treatment, and maintain a complete medical record
of the patient’s treatment
Link to the guidelines:
https://www.michigan.gov/documents/mdch_MI_guidelines_91795_7.pdf
Minnesota
Quasi-regulatory guidelines: Joint Statement on Pain Management
In 2015, the Minnesota Boards of Medical Practice, Nursing, and Pharmacy updated their
Joint Statement on Pain Management to “add guidance regarding appropriate prescribing
with emphasis on the critical balance between pain management and the potential misuse
of controlled substance medications.”
Summary of guidelines:
- Consistently and thoroughly assess all patients for pain. Conduct a comprehensive
risk assessment and review all medications and therapies from all sources.
- Utilize the Minnesota PMP prior to prescribing or dispensing controlled
substances in an effort to identify additional prescribers and medications to
inform decision making.
- Collaborate using a multi-disciplinary approach to identify all treatment options
including pharmacologic and non-pharmacologic modalities. Consider the
integration of non-medication and multi-modality therapeutic approaches.
- Consider non-opioid alternatives and start patients on the lowest effective dose
when initiating pharmacologic therapy. Carefully consider the risks associated
with the combination of an opioid and benzodiazepine.
- Obtain informed consent and consider a written treatment agreement and
monitoring plan to promote adherence to the treatment plan and goals. Provide
the patient with information regarding the benefits and risks of opioid therapy.
- Conduct urine drug screening, as appropriate.
- Educate patients about the safe use, storage, and disposal of opioid medications as
well as the consequences for misuse or illegal use of prescribed medications.
- Re-evaluate and document the patient’s pain, functionality, and response to
treatment using consistent and developmentally appropriate tools. Make
adjustments as needed and exercise increased clinical vigilance for patients using
high-dose opioids.
- Direct patients in need of substance use disorder evaluations or treatment to
appropriate providers, when applicable.
- Consider equipping patients at risk of an overdose with an opioid antagonist.
- Develop safe and effective strategies for discontinuing chronic opioid therapies.
Link to the guidelines:
https://mn.gov/boards/assets/Joint%20Statement%20on%20Pain%20Management%20
2015_tcm21-90718.pdf
Requirements with the force of law: Minn. R. 5221.6110 (2015)

26
Under Minnesota regulations, before prescribing long-term opioids, practitioners are
required to:
- Affirm that the patient cannot maintain functions of daily life without the
medication, doesn’t have somatic symptoms disorder, doesn’t have a history of
failure to comply with treatment, and doesn’t have substance abuse disorder;
- Ensure that all other pain management options have been exhausted;
- Determine whether the following circumstances are present, and whether they
constitute contraindications for long-term opioid use: history of respiratory
depression, pregnancy or planned pregnancy, history of substance abuse, suicide
risk, poor impulse control, and regular engagement in unsafe activity for a patient
on opioids;
- Complete a scientific assessment to determine the patient’s risk for abuse;
- Explain the potential consequences and complications of long-term opioids to the
patient;
- Enter into a written contract with the patient that includes a provision for drug
testing at the doctor’s discretion.
Link to the rule: https://www.revisor.mn.gov/rules/?id=5221.6110
Mississippi
Requirements with the force of law: Miss. Admin. Code 30-17-2640:1.7 (2012)
In 2012, the Mississippi Board of Medical Licensure adopted a new rule for the prescribing
of controlled substances to treat chronic (non-terminal) pain. The rule includes, among
others, the following requirements:
- No physician shall administer, dispense or prescribe a controlled substance or
other drug having addiction-forming and addiction-sustaining liability that is
nontherapeutic in nature or non-therapeutic in the manner the controlled
substance or other drug is administered, dispensed or prescribed.
- No physician shall administer, dispense or prescribe a controlled substance for
treatment of chronic pain to any patient who has consumed or disposed of any
controlled substance or other drug having addiction-forming and addiction-
sustaining liability other than in strict compliance with the treating physician's
directions
- Repetitive or continuing escalations should be a reason for concern and a re-
evaluation of the present treatment plan shall be undertaken by the physician.
This statute provides exceptions for situations such as emergency treatment and treatment
in hospitals to maintain or detoxify a person as an incidental adjunct to medical or surgical
treatment of a condition other than addiction.
Link to the regulations:
http://www.painpolicy.wisc.edu/sites/www.painpolicy.wisc.edu/files/Mississippi%20Me
dical%20Board%20Regulations_1.pdf
Missouri

27
Quasi-regulatory guidelines: Guidelines for the Use of Controlled Substances for the
Treatment of Pain
In 2007, the Missouri Board of Healing Arts issued guidelines on prescribing of controlled
substances to “clarify the Boards’ position on pain control, to alleviate physician
uncertainty and to encourage better pain management.” The guidelines include performing
a patient evaluation before prescribing opioids, obtaining informed consent from the
patient for opioid treatment, requiring a written agreement outlining patient
responsibilities if the patient is determined to be at high risk for medication abuse or to
have a history of substance abuse, conduct periodic review of the opioid treatment, and
maintain a complete medical record of the patient’s treatment.
Link to the guidelines:
http://www.painpolicy.wisc.edu/sites/www.painpolicy.wisc.edu/files/MO_CSGUIDE_0.pdf
Montana
Advisory Guidelines: Statement on the Use of Controlled Substances in the Treatment of
Intractable Pain
In 2002, the Montana Board of Medical Examiners issued a statement on the use of opioids
and other controlled substances for the treatment of pain. The guidelines include
performing a patient evaluation before prescribing opioids, obtaining informed consent
from the patient for opioid treatment, conduct periodic review of the opioid treatment, and
maintain a complete medical record of the patient’s treatment.
Link to the statement:
http://indianapainsociety.org/fileuploads/OpioidPolicies/MontanaMedicalBoardOpioidGu
idelines.pdf
Nebraska
Quasi-regulatory guidelines: Guidelines for the Use of Controlled Substances for the
Treatment of Pain
On June 17 2016, the Nebraska Board of Medicine and Surgery reaffirmed its guidelines for
the prescribing of opioids to treat pain. The guidelines include performing a patient
evaluation before prescribing opioids, obtaining informed consent from the patient for
opioid treatment, requiring a written agreement outlining patient responsibilities if the
patient is determined to be at high risk for medication abuse or to have a history of
substance abuse, conduct periodic review of the opioid treatment, and maintain a complete
medical record of the patient’s treatment.
Link to the guidelines:
http://dhhs.ne.gov/publichealth/Licensure/Documents/GuidelinesForUseOfContSubst.pdf
Nevada
Requirements with the force of law: Nev. Rev. Stat. Ann. § 639.23507 (2015)
Since 2015, Nevada requires prescribers of controlled substances to obtain a patient
utilization report regarding the patient from the prescription monitoring program before
initiating a prescription for a controlled substance. This requirement is triggered if 1) the
patient is a new patient of the practitioner, or 2) the prescription is for more than 7 days

28
and is part of a new course of treatment for the patient. By reviewing the patient utilization
report, the practitioner must assess whether the prescription for the controlled substance
is medically necessary.
Link to the statute: https://www.leg.state.nv.us/nrs/NRS-639.html#NRS639Sec23507
Advisory Guidelines: Nevada Hospital Association Guidelines for Controlled Substance
Prescriptions
In February 2016, the NHA adopted guidelines for hospitals to address the misuse of
controlled substance prescriptions. The guidelines establish best practices for prescribers
and pharmacists for screening and prescribing controlled substances and opioid
antagonists in a hospital emergency department or practitioners discharging an in-patient
to home.
Link to NHA’s press release:
https://nvha.net/News/Docs/2016_News_Release.PMP_and_Opioids.pdf (the guidance
document is currently unavailable online)
New Hampshire
Quasi-regulatory guidelines: Board of Medicine Guidelines for Pain Management
The New Hampshire Board of Medicine adopted voluntary guidelines for physicians
prescribing opioids to treat pain. The guidelines include performing a patient evaluation
before prescribing opioids, obtaining informed consent from the patient for opioid
treatment, requiring a written agreement outlining patient responsibilities if the patient is
determined to be at high risk for medication abuse or to have a history of substance abuse,
conduct periodic review of the opioid treatment, and maintain a complete medical record
of the patient’s treatment.
Link to the guidelines: https://www.nh.gov/medicine/aboutus/pain.htm
Requirements with the force of law: N.H. Rev. Stat. Ann. § 318-B:39 (2016)
This law requires prescribers to query the prescription drug monitoring program when
prescribing schedule II, III, and IV opioids for the management or treatment of pain and
then periodically (at least twice per year), except when controlled medications are to be
administered to patients in a health care setting, and when treating acute pain associated
with serious traumatic injury, post-surgery, or with an acute medical condition for no more
than 30 days.
Requirements with the force of law: N.H. Code Admin. R. Med. 502 (2016)
The New Hampshire Board of Medicine’s new requirements for physicians who prescribe
opioids went into effect on January 1, 2017. First, the new rule requires physicians to query
the prescription drug monitoring program to obtain a history of schedule II-IV controlled
substances dispensed to a patient, prior to prescribing an initial schedule II, III, and IV
opioids for the management or treatment of this patient’s pain and then periodically and at
least twice per year. Physicians are exempted from this requirement when controlled
medications are to be administered to patients in a health care setting, or when treating
29
acute pain associated with serious traumatic injury, post-operatively, or with an acute
medical condition for no more than 30 days. The requirements also limit doses of opioids
prescr4ibed in emergency settings to a maximum of seven days. The rule includes
requirements for both acute pain treatment and chronic pain treatment.
Requirements for acute pain treatment include:
- Conduct and document a physical examination and history;
- Consider the patient’s risk for opioid misuse, abuse, or diversion and prescribe for
the lowest effective dose for a limited duration;
- Document the prescription and rationale for all opioids;
- Ensure that the patient has been provided information that contains the following:
• Risk of side effects, including addiction and overdose resulting in death;
• Risks of keeping unused medication;
• Options for safely securing and disposing of unused medication;
• Danger in operating motor vehicle or heavy machinery
Requirements for chronic pain treatment include:
- Conduct and document a history and physical examination;
- Conduct and document a risk assessment, including, but not be limited to, the use of
an evidence-based screening tool;
- Document the prescription and rationale for all opioids;
- Prescribe for the lowest effective dose for a limited duration;
- Utilize written informed consent that explains the following risks associated with
opioids:
• Addiction;
• Overdose and death;
• Physical dependence;
• Physical side effects;
• Hyperalgesia;
• Tolerance; and
• Crime victimization;
- Create and discuss a treatment plan with the patient.
- Utilize a written treatment agreement that is included in the medical record, and
specifies conduct that triggers the discontinuation or tapering of opioids;
- Document the consideration of a consultation with an appropriate specialist in the
following circumstances:
• When the patient receives a 100 mg morphine equivalent dose daily for
longer than 90 days;
• When a patient is at high risk for abuse or addiction; or
• When a patient has a co-morbid psychiatric disorder;
- Require periodic review and follow-up at least every 4 months;
- Require random and periodic urine drug testing at least annually for all patients
using opioids for longer than 90 days;
- The prescriber may forego the requirements for a written treatment agreement and
for periodic drug testing for patients:
30
• Who are residents in a long-term, non-rehabilitative nursing home facility
where medications are administered by licensed staff; or
• Who are being treated for episodic intermittent pain and receiving no more
than 50 dose units of opioids in a 3-month period.
Link to the rule: https://www.oplc.nh.gov/medicine/documents/med502-adopted.pdf
New Jersey
Requirements with the force of law: N.J. Admin. Code § 13:35-7.6 (2011)
This rule imposes the following limits on the prescribing of controlled substances:
- When prescribing, dispensing or administering controlled substances, a practitioner
shall ensure that a patient's medical history has been taken and physical
examination accomplished, including any history of substance abuse and the nature,
frequency and severity of any pain.
- With respect to Schedule II controlled substances, a practitioner shall not authorize
a quantity calculated to exceed 120 dosage units or a 30–day supply, whichever is
less.
- A practitioner may exceed the 120 dosage unit or 30–day supply limitations for
Schedule II controlled substances in the following circumstances:
• For the 120 dosage unit limitation, the practitioner follows a plan designed to
achieve effective pain management, which has been tailored to the needs of a
patient who is suffering pain from cancer, intractable pain or terminal illness.
• With regards to the 30-day supply limitation, a practitioner may prescribe
the use of an implantable infusion pump which is utilized to achieve pain
management for patients suffering from cancer, intractable pain or terminal
illness. A prescription for such an implantable infusion pump may provide up
to a 90-day supply, as long as the physician evaluates and documents the
patient's continued need at least every 30 days; and
• With regards to the 30-day supply limitation, a practitioner may prescribe
multiple prescriptions authorizing a patient to receive a total of up to a 90-
day supply of a Schedule II controlled dangerous substance provided that.
- When controlled substances are continuously prescribed for management of pain
for three months or more, the practitioner:
• Shall review, at a minimum of every three months, the course of treatment,
any new information about the etiology of the pain and the patient's progress
toward treatment objectives;
• Shall remain alert to problems associated with physical and psychological
dependence; and
• Shall periodically make reasonable efforts, unless clinically contraindicated,
to stop the use of the controlled substance, decrease the dosage, try other
drugs such as nonsteroidal anti-inflammatories, or treatment modalities in
an effort to reduce the potential for abuse or the development of physical or
psychological dependence.
- A practitioner managing pain in a patient with a history of substance abuse shall
exercise extra care by way of monitoring and possible consultation with addiction
specialists.
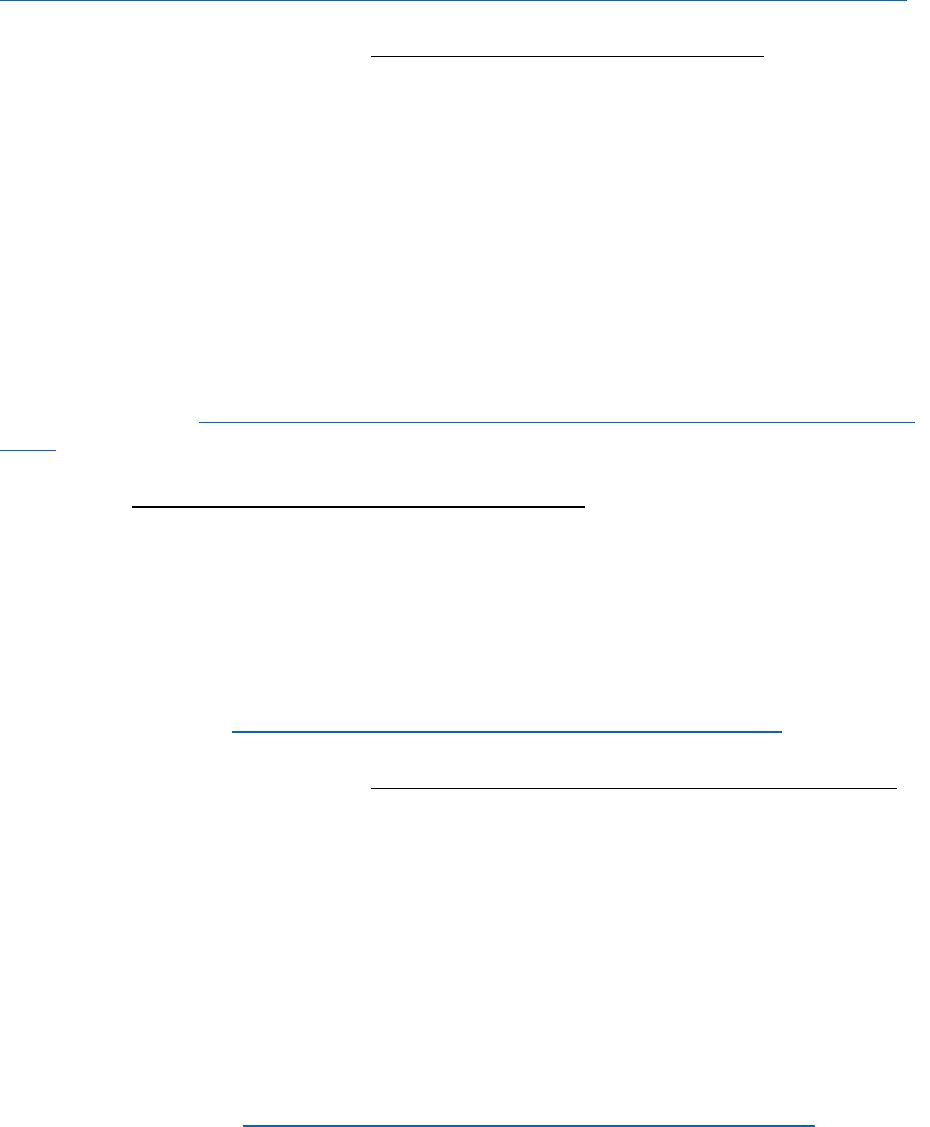
31
- The practitioner shall keep accurate and complete patient records.
Link to the statute:
http://www.painpolicy.wisc.edu/sites/www.painpolicy.wisc.edu/files/NJ_mbreg3_0.pdf
Requirements with the force of law: N.J. Rev. Stat. § 45:1-46.1(a)(1) (2015)
Since 2015, New Jersey requires prescribers to access prescription monitoring information
before prescribing opioids and other controlled substances to a patient. The statute
provides as follows:
[A] practitioner or other person who is authorized by a practitioner to access
prescription monitoring information […] shall access prescription monitoring
information the first time the practitioner or other person prescribes a Schedule II
controlled dangerous substance to a new patient for acute or chronic pain. In addition,
for any prescription of a Schedule II controlled dangerous substance for a new or
current patient for acute or chronic pain, […] a practitioner or other authorized person
shall access prescription monitoring information on a quarterly basis during the period
of time the patient continues to receive such prescriptions.
Link to the statute: http://law.justia.com/codes/new-jersey/2015/title-45/section-45-1-
46.1/
Resolutions: New Jersey Senate Resolution No. 60 (2016)
The New Jersey Senate Resolution No. 60 “urge[d] the State Board of Medical Examiners to
adopt the CDC Guideline for Prescribing Opioids for Chronic Pain, United States 2016 in
order to improve patient safety, educate patients about the risks and benefits of opioid use
as a pain management treatment, and reverse the cycle of opioid pain medication misuse
that is contributing to the opioid overdose epidemic in New Jersey.” As of October 2016, the
CDC guidelines have yet to be adopted by the New Jersey Board of Medical Examiners.
Link to the resolution: ftp://www.njleg.state.nj.us/20162017/SR/60_I1.PDF
Requirements with the force of law: N.J. Stat. Ann. §§ 24:21-15.2 and 45:9-22.19 (2017)
In 2017, New Jersey enacted one of the most aggressive acts to prevent opioid overdoses.
Beginning May 2017, the state will limit the initial prescriptions of opioid to treat acute or
chronic pain to a five-day supply. The prescriber must also (1) take and document the
results of a thorough medical history, including the patient's experience with non-opioid
medication and non-pharmacological pain management approaches and substance abuse
history; (2) conduct, as appropriate, and document the results of a physical examination;
(3) develop a treatment plan, with particular attention focused on determining the cause of
the patient's pain; (4) access relevant prescription monitoring information under the
state’s PDMP. Subsequent prescriptions of Schedule II controlled substances must be
limited to a maximum of 30-day supply.
Link to the enacted act: http://www.njleg.state.nj.us/2016/Bills/PL17/28_.PDF
New Mexico

32
Advisory Guidelines: New Mexico Hospital Association-Recommended Opioid Risk-
Reduction Strategies and Prescribing Guidelines in New Mexico Emergency Departments
The NMHA Behavioral Health Task Force developed opioid prescribing guidelines to be
used in emergency departments in the state. The guidelines include:
- Hospital ED personnel should develop a process to screen for substance misuse and
abuse that includes services for brief intervention and referrals to treatment
programs for patients who are at risk for developing, or who actively have,
substance use disorders.
- Hospital ED personnel should develop a process to document an appropriate pain
assessment as well as a reason pain medication was denied to meet CMS standards
for pain assessment and treatment; the patient should receive this information too.
- EDs should develop processes to facilitate appropriate provider or provider
delegate consultations of the NM PMP prior to writing opioid prescriptions.
- Hospitals should support timely implementation and the use of the ED Information
Exchange to reduce risk associated with frequent ED visits and potential for
multiple narcotic or benzodiazepine prescriptions.
- Hospitals should support processes for ED provider notification of a patient’s
primary opioid prescriber or primary care provider when prescriptions for acute
exacerbations of chronic pain are made.
- ED providers and hospital-based pharmacies should be encouraged to prescribe
nasal naloxone and provide education to at-risk patients (e.g., patients on high
dose/quantity narcotic prescriptions, patients with accidental prescription or illicit
narcotic overdoses, etc.) and their families/friends.
Link to the guidelines: http://nmhanet.org/files/Documents/Emergency-Medicine-
Controlled-Substance-Administration-and-Prescribing-Guidelines.pdf
Requirements with the force of law: N.M. Code R. § 16.10.14.10 (2014)
Since 2014, New Mexico requires physicians to obtain a patient PMP report for the
previous twelve months before prescribing, ordering, administering or dispensing a
controlled substance listed in Schedule II, III, or IV. This provision is triggered if the patient
is a new patient of the practitioner (in which situation a patient PMP report for the
previous twelve months shall only be required when drugs are prescribed for a period
greater than 10 days). Moreover, during the continuous use of opioids by established
patients a PMP report shall be requested and reviewed a minimum of once every six
months.
Link to the statute: http://164.64.110.239/nmac/parts/title16/16.010.0014.htm
New York
Advisory Guidelines: NYC Emergency Department Discharge Opioid Prescribing Guidelines
In 2013, the New York City Department of Health and Mental Hygiene released guidelines
to provide recommendations for opioid analgesic prescribing to patients being discharged
from EDs. The guidance includes the following recommendations:
- Consider short-acting opioid analgesics for the treatment of acute pain only when
the severity of the pain is reasonably assumed to warrant their use.
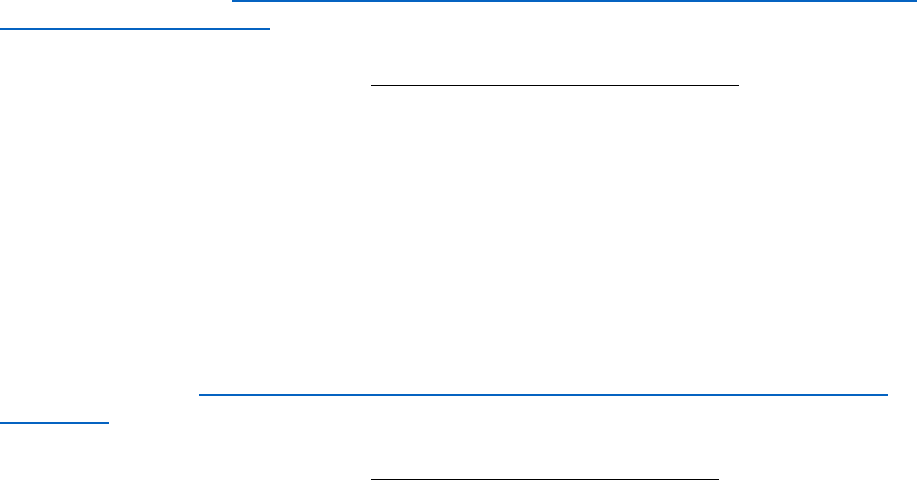
33
- Start with the lowest possible effective dose if opioid analgesics are considered for
the management of pain.
- Prescribe no more than a short course of opioid analgesics for acute pain. Most
patients require no more than three days.
- To assess for opioid misuse or addiction, prescribers can access the New York State
Controlled Substance Information (CSI) on Dispensed Prescriptions Program for
information on patients’ controlled substance prescription history.
- Avoid initiating treatment with long-acting or extended-release opioid analgesics.
- Address exacerbations of chronic or recurrent pain conditions with non-opioid
analgesics, nonpharmacological therapies, and/or referral to specialists for follow-
up, all as clinically appropriate.
- Avoid when possible prescribing opioid analgesics to patients currently taking
benzodiazepines and/or other opioids. Consider other risk factors for consequential
respiratory depression.
- Attempt to confirm with the treating physician the validity of lost, stolen, or
destroyed prescriptions. If considered appropriate, replace the prescription only
with a one-to two-day supply.
- Provide information about opioid analgesics to patients receiving a prescription,
such as the risks of overdose and dependence/ addiction, as well as safe storage and
proper disposal of unused medications.
Link to the guidelines: https://www1.nyc.gov/assets/doh/downloads/pdf/basas/opioid-
prescribing-guidelines.pdf
Requirements with the force of law: N.Y. Pub. Health § 3334-a(2) (2013)
Since 2013, the State of New York requires physicians to access the state’s prescription
monitoring program before initiating a controlled substance treatment. The statute
provides as follows:
Every practitioner shall consult the prescription monitoring program registry prior to
prescribing or dispensing any controlled substance […], for the purpose of reviewing a
patient's controlled substance history as set forth in such registry; provided, however,
that nothing in this section shall preclude an authorized practitioner, other than a
veterinarian, from consulting the registry at his or her option prior to prescribing or
dispensing any controlled substance
Link to the statute: http://law.justia.com/codes/new-york/2015/pbh/article-33/title-
4/3343-a/
Requirements with the force of law: N.Y. Pub. Health § 3331(5) (2016)
In 2016, the New York Legislature amended the state’s controlled substances statute to
include a provision that limits the doses of opioids physicians are allowed to prescribe.
Opioid prescriptions are limited to seven days for first time users for treatment of acute
pain. Practitioners can issue refills after subsequent consultations that they deem
appropriate up to a 30-day supply. Finally, the new act requires regulations to articulate
circumstances where one-time prescription between 30 and 90 days is warranted.

34
Link to the enacted act:
http://assembly.state.ny.us/leg/?default_fld=&leg_video=&bn=A10727&term=&Summary
=Y&Actions=Y&Memo=Y&Text=Y
North Carolina
Quasi-regulatory guidelines: Policy for the Use of Opiates for the Treatment of Pain
In June 2014, the North Carolina Medical Board issued guidelines for the use of opioids in
treating pain. The guidelines include, among others:
- Patient evaluation and risk stratification should be performed before initiating
opioid treatment.
- Information from the North Carolina Controlled Substance Reporting System
(NCCSRS) should be part of every patient’s initial evaluation and subsequent
monitoring program.
- Development of opioid treatment plan and goals should be established before
initiating opioid treatment.
- Physicians should obtain informed consent and written agreement before
prescribing opioids.
- Safer alternative treatments including non-pharmacologic and minor interventions
and first line pharmacotherapy with over the counter medications, non-steroidal
anti-inflammatory drugs, and acetaminophen should be considered before initiating
opioid therapy.
- When the decision to use an opiate has been made, it should be presented to the
patient as a therapeutic trial or test for a defined period of time (usually no more
than 90 days) and with specified evaluation points.
- The Board expects physicians who prescribe opiates to help insure that naloxone is
readily available to patients who are identified as being at risk of an opiate overdose
- When initiating opioid therapy, the lowest dose possible should be given to an
opioid naïve patient and titrated to affect while monitoring for complications.
Opioid therapy should begin with a short acting drug and rotate to a long
acting/extended release if indicated. A decision to continue opioid therapy beyond
the trial period should reflect a careful evaluation of benefits, adverse events, and
potential risks.
- The physician should regularly review the patient’s progress, including any new
information about the etiology of the pain or the patient’s overall health and level of
activities.
- Periodic drug testing may be useful in monitoring adherence to the treatment plan,
as well as in detecting the use of non-prescribed drugs.
Link to the guidelines:
http://www.ncmedboard.org/images/uploads/other_pdfs/Policy_for_the_Use_of_Opiates_f
or_the_Treatment_of_Pain_June_4_2014.pdf
North Dakota
Advisory Guidelines: Safe Prescribing Tips for Opioids

35
The North Dakota Department of Human Services issued tips for safe opioid prescribing
practices in their Medicaid Pharmacy Program Quarterly Newsletter. Some of the
recommendations include:
- Individualize treatment.
- Consider long-acting preparations.
- When opioids are used to treat chronic pain, they should be considered one portion
of a multimodal treatment plan. The treatment plan should acknowledge that the
patient is likely to benefit from a range of therapies, both pharmacologic and non-
pharmacologic.
- In patients with chronic pain, opioid therapy should be considered after the patient
has tried and failed non-opioid therapy as well as non-pharmacologic pain therapy.
- Educate patients and get a written treatment agreement
- Refer patients with complicated cases to a specialist.
- Random urine drug screening may be important, even before an opioid is
prescribed. This can be an important part of the patient history as it can screen for
the presence of illegal drugs, unreported prescribed medications, or unreported
alcohol use prior to starting therapy
- Consider tamper-resistant products. The tamper-resistant products should be
considered in all patients and not just those exhibiting potential abuse behaviors.
Link to the recommendations:
http://www.hidesigns.com/assets/files/ndmedicaid/newsletters/ND%20newsletter1_rev.
pdf
Ohio
Advisory Guidelines: Ohio Emergency and Acute Care Facility Opioids and Other Controlled
Substances (OOCS) Prescribing Guidelines
In April 2012, the Ohio Department of Health, in collaboration with the Ohio Hospital
Association, the Ohio State Pharmacists Association, among others, issued guidelines for
the prescribing of opioids in emergency and acute care settings.
Specific guidelines:
- OOCS for acute pain, chronic pain and acute exacerbations of chronic pain will be
prescribed in emergency/acute care facilities only when appropriate based on the
patient’s presenting symptoms, clinical examination, and risk for addiction.
• Doses of OOCS for routine chronic pain or acute exacerbations of chronic
pain will typically NOT be given in injection (IM or IV) form.
• Prescriptions for chronic pain will typically NOT be provided if the patient
has either previously presented with the same problem or received an OOCS
prescription from another provider within the last month.
• IV Demerol (Meperidine) for acute or chronic pain is discouraged.
- Emergency medical clinicians will not routinely provide:
• Replacement prescriptions for OOCS lost, destroyed or stolen.
• Replacement doses of Suboxone, Subutex or Methadone for patients in a
treatment program.

36
• Long‐acting or controlled‐release opioids (such as OxyContin®, fentanyl
patches, and methadone).
- Prior to making a final determination regarding whether a patient will be provided a
prescription for OOCS, the emergency clinician or facility:
• Should search the Ohio Automated Rx Reporting System (OARRS) or other
prescription monitoring programs, per state rules.
• Reserves the right to perform a urine drug screen or other drug screening.
- Prior to making a final determination regarding whether a patient will be provided a
prescription for an OOCS, the emergency clinician should consider the following
options:
• Contact the patient’s routine provider who usually prescribes their OOCS.
• Request a consultation from their hospital’s palliative or pain service (if
available), or an appropriate sub‐specialty service.
• Perform case review or case management for patients who frequently visit
the emergency/ acute care facilities with pain‐related complaints.
• Request medical and prescription records from other hospitals, provider’s
offices.
• Request that the patient sign a pain agreement that outlines the expectations
of the emergency clinician with regard to appropriate use of prescriptions for
OOCS.
- Except in rare circumstances, prescriptions for OOCS should be limited to a three‐
day supply.
- Each patient leaving the emergency/acute care facility with a prescription for OOCS
should be provided with detailed information about the addictive nature of these
medications, the potential dangers of misuse and the appropriate storage and
disposal of these medications at home.
Link to the guidelines: http://www.healthy.ohio.gov/-
/media/HealthyOhio/ASSETS/Files/edguidelines/EGs-no-poster.pdf?la=en
Advisory Guidelines: Ohio Guidelines for Prescribing Opioids for the Treatment of Chronic,
Non-Terminal Pain 80 mg of Morphine Equivalent Daily Dose (MED) “Trigger Point”
In October 2013, the Ohio Opiate Action Team (part of the Governor’s cabinet), issued
recommendations for the treatment of chronic, non-terminal pain with opioids.
Specific guidelines:
- Providers should first consider non-pharmacologic and non-opioid therapies.
Providers should exercise the same caution with tramadol as with opioids.
- Providers must avoid Long-Term and Co-Prescribing.
- Providers should avoid starting a patient on long-term opioid therapy when treating
chronic pain. Providers should also avoid prescribing benzodiazepines with opioids.
- Providers treating chronic, non-terminal pain patients who have received opioids
equal to or greater than 80 mg MED for longer than three continuous months should
strongly consider doing the following:
• Reestablish informed consent, including providing the patient with written
information on the potential adverse effects of long-term opioid therapy.

37
• Review the patient’s functional status and documentation,
• Review the patient’s progress toward treatment objectives for the duration
of treatment.
• Utilize OARRS as an additional check on patient compliance.
• Reconsider having the patient evaluated by one or more other providers who
specialize in the treatment of the area, system, or organ of the body
perceived as the source of the pain.
- For providers treating acute exacerbation of chronic, nonterminal pain, clinical
judgment may not trigger the need for using the full array of reassessment tools.
Link to the guidelines:
http://mha.ohio.gov/Portals/0/assets/Initiatives/GCOAT/Guidelines-Chronic-Pain.pdf
Requirements with the force of law: Ohio Admin. Code 4731-11-11 (2015)
Since 2015, the Ohio State Medical Board requires physicians to obtain and review an
OARRS report to help determine if it is appropriate to prescribe an opioid analgesic,
benzodiazepine, or reported drug to a patient unless one of the following exceptions apply:
- The reported drug is prescribed or personally furnished to a hospice patient in a
hospice care program or any other patient diagnosed as terminally ill;
- The reported drug is prescribed for administration in a hospital, nursing home, or
residential care facility;
- The reported drug is prescribed or personally furnished in an amount indicated for
a period not to exceed seven days;
- The reported drug is prescribed or personally furnished for the treatment of cancer
or another condition associated with cancer; and
- The reported drug is prescribed or personally furnished to treat acute pain resulting
from a surgical or other invasive procedure or a delivery.
Link to the statute: http://codes.ohio.gov/oac/4731-11-11v1
Advisory Guidelines: Ohio Guideline for the Management of Acute Pain Outside of
Emergency Departments
In 2016, the Ohio Opiate Action Team issued recommendations for the prescribing of
opioids for treatment of acute pain outside of emergency rooms.
Specific guidelines:
- Assessment and Diagnosis of Patient Presenting with Pain. A specific diagnosis
should be made, when appropriate, to facilitate the use of an evidence-based
approach to treatment.
- Upon determining the symptoms fit the definition of acute pain, both the provider
and patient should discuss the risks/benefits of pharmacologic therapy.
- Non-pharmacologic therapies should be considered as first-line therapy for acute
pain.
- Non-opioid medications should be used with non-pharmacologic therapy.
- Reserve opioids for acute pain resulting from severe injuries or medical conditions,
surgical procedures, or when non-opioid options are ineffective or contraindicated.

38
- Appropriate risk screening should be completed (e.g. age, pregnancy, high-risk
psychosocial environment, personal or family history of substance use disorder).
- Provide the patient with the least potent opioid to effectively manage pain. A
morphine equivalence chart should be used if needed.
- Prescribe the minimum quantity needed with no refills based on each individual
patient, rather than a default number of pills.
- Consider checking Ohio Automated Rx Reporting System (OARRS) for all patients
who will receive an opiate prescription
- Avoid long-acting opioids (e.g. methadone, oxycodone ER, fentanyl).
- Use caution with prescribing opioids with patients on medications causing central
nervous system depression (e.g. benzodiazepines and sedative hypnotics) or
patients known to use alcohol.
- Discuss with the patient a planned wean off opioid therapy, concomitant with
reduction or resolution of pain.
- Discuss proper secure storage and disposal of unused medication to reduce risks to
the patient and others.
- Remind the patient that it is both unsafe and unlawful to give away or sell opioid
medication, including unused or leftover medication.
Link to the guidelines:
http://mha.ohio.gov/Portals/0/assets/Initiatives/GCOAT/Guidelines-Acute-Pain-
20160119.pdf
Link to the Ohio Guidelines Factsheet:
http://mha.ohio.gov/Portals/0/assets/Initiatives/GCOAT/20160112-GCOAT-Prescribing-
Guidelines-Summary.pdf
Requirements with the force of law: Adoption by professional boards pending
In March 2017, Gov. Kasich announced that the Ohio Medical Board, together with the
Boards of Pharmacy, Dentistry, and Nursing, will be adopting new regulations
implementing limits on opioid prescribing. In general:
- Practitioners may prescribe no more than seven days of opiates for adults;
- Practitioners may prescribe no more than five days of opiates for minors;
- The total morphine equivalent dose (MED) of a prescription for acute pain cannot
exceed an average of 30 MED per day;
- Health care providers can prescribe opiates in excess of the new limits only if they
provide a specific reason in the patient’s medical record.
- Prescribers will be required to include a diagnosis or procedure code on every
controlled substance prescription, which will be entered into Ohio’s PDMP, OARRS.
The new limits do not apply to opiates prescribed for cancer, palliative care, end-
oflife/hospice care or medication-assisted treatment for addiction.
Link to the announcement:
http://www.pharmacy.ohio.gov/Documents/Pubs/NewsReleases/2017/New%20Limits%

39
20on%20Prescription%20Opiates%20Will%20Save%20Lives%20and%20Fight%20Addic
tion.pdf
Link to FAQ on the new rules:
http://www.pharmacy.ohio.gov/Documents/Pubs/Special/ControlledSubstances/New%2
0Limits%20on%20Prescription%20Opiates%20for%20Acute%20Pain%20-
%20Frequently%20Asked%20Questions.pdf
Oklahoma
Requirements with the force of law: Okla. Stat. Ann. tit. 63, § 2-302(M) (2010)
Since 2010, Oklahoma requires physicians who prescribe methadone to check the patient’s
record at the state’s prescription monitoring program (PMP). The statute provides as
follows:
Beginning November 1, 2010, each registrant that prescribes, administers or dispenses
methadone shall be required to check the prescription profile of the patient on the
central repository of the Oklahoma State Bureau of Narcotics and Dangerous Drugs
Control.
Link to the statute: http://law.justia.com/codes/oklahoma/2015/title-63/section-63-2-
302/
Advisory Guidelines: Oklahoma Emergency Department (ED) and Urgent Care Clinic (UCC)
Opioid Prescribing Guidelines
In 2013, an interdisciplinary group of health care practitioners in Oklahoma, that included
the Oklahoma Board of Nursing, the Oklahoma State Medical Association, the Oklahoma
Department of Mental health and Substance Abuse Services, among others, published a set
of recommendations for physicians and other providers prescribing opioids for treating
acute and chronic pain in office-based settings.
- Consider opioid medications for the treatment of acute pain only when the severity
of the pain is reasonably assumed to warrant their use.
- When administering or prescribing opioids, it is suggested that health care
providers start with the lowest possible effective dose for the management of pain.
- When prescribing opioids for acute pain, prescribe no more than a short course,
except in special circumstances. Most patients require opioids for no more than
three days of pain control, with a maximum of 30 pills in most cases.
- Providers should query the Oklahoma PMP for patients presenting with acute pain,
prior to prescribing opioid medication.
- In patients who routinely take opioids for chronic pain, it is ideal that one health
care provider provide all opioid prescriptions. When an exception occurs and
another provider deems it necessary to prescribe opioids, Oklahoma PMP data
should be reviewed, and only enough pills prescribed, if indicated, to last until the
office of the patient’s primary opioid prescriber opens.
- Health care providers should not provide replacement prescriptions for lost,
destroyed or stolen controlled substances.
- Long-acting or controlled-release opioids (such as OxyContin®, fentanyl patches,
suboxone, and methadone) should not be prescribed from the ED/UCC.

40
- The emergency health care provider should only prescribe enough pills to last until
the office of the patient’s primary opioid prescriber opens.
- The administration of intravenous and intramuscular opioids for the relief of
exacerbations of chronic pain is discouraged, except in special circumstances.
- Use caution when prescribing opioid medications to patients currently taking
benzodiazepines and/or other opioids.
- Provide information about opioid medications to patients receiving an opioid
prescription, such as the risks of overdose and addiction.
- Health care providers are encouraged to consider non-pharmacological therapies
and/or referral to specialists for follow-up, as clinically appropriate.
Link to the guidelines:
http://www.okoha.com/Images/OHADocs/Patient%20Safety/Opiod%20Guidelines/Oklah
oma_ED_Guidelines_FINAL%20with%20logos%20v2.pdf
Advisory Guidelines: Opioid Prescribing Guidelines for Oklahoma Health Care Providers in
the Office-Based Setting
In September 2014, an interdisciplinary group of health care practitioners in Oklahoma,
that included the Oklahoma Board of Nursing, the Oklahoma State Medical Association, the
Oklahoma Department of Mental health and Substance Abuse Services, among others,
published a set of recommendations for physicians and other providers prescribing opioids
for treating acute and chronic pain in office-based settings.
Specific guidelines for treating acute pain:
- Opioids should only be used for treatment of acute pain when the severity of the
pain warrants that choice and after determining that other non-opioid pain
medications or therapies will not provide adequate pain relief.
- Providers should query the Oklahoma Prescription Monitoring Program (PMP) for
patients presenting with acute pain, prior to prescribing an opioid medication. In
circumstances where a patient’s pain is resulting from an objectively diagnosed
disease process or injury, a provider may prudently opt not to review the Oklahoma
PMP.
- When opioids are prescribed for treatment of acute pain, the number of doses
dispensed should be no more than the number of doses needed based on the usual
duration of pain severe enough to require opioids for that condition.
- When opioids are prescribed for treatment of acute pain, the patient should be
counseled to store the medications securely and never to share with others.
- Long duration-of-action opioids (e.g., methadone, buprenorphine, fentanyl,
extended release oxycodone, and morphine) are rarely indicated for treatment of
acute pain.
- The use of opioids should be re-evaluated carefully, including assessing the
potential for abuse, if persistent pain suggests the need to continue opioids. Health
care providers should query the Oklahoma PMP as part of this re-evaluation
process.
- Health care providers should generally not provide replacement prescriptions for
opioids that have been lost, stolen, or destroyed.

41
Specific guidelines for treating chronic pain:
- Alternatives to opioid treatment should be tried, or previous attempts documented,
before initiating opioid treatment.
- A comprehensive evaluation should be performed before initiating opioid treatment
for chronic pain.
- The health care provider should screen for risk of abuse or addiction before
initiating opioid treatment.
- Prior to the initial prescribing of opioid medications, health care providers should
query the Oklahoma Prescription Monitoring Program (PMP).
- When opioids are used for the treatment of chronic pain, a written treatment plan
should be established that includes measurable goals for reduction of pain and
improvement of function.
- Opioids should be initiated as a short-term trial to assess the effects of opioid
treatment on pain intensity, function, and quality of life.
- Regular visits for evaluation of progress toward goals should be scheduled during
the period when the dose of opioids is being adjusted. During this period and until
the patient is clinically stable and judged to be compliant with therapy, it is
recommended that the health care provider check the Oklahoma PMP more
frequently.
- Once a stable dose has been established, regular monitoring should be conducted at
face-to-face visits during which treatment goals, analgesia, activity, adverse effects,
and aberrant behaviors are monitored. The Oklahoma PMP should be queried at
least once per year for patients receiving opioid treatment for chronic pain.
- Opioid treatment should be discontinued if adverse effects outweigh benefits or if
aberrant, dangerous, or illegal behaviors are demonstrated.
- Health care providers should generally not provide replacement prescriptions for
opioids that have been lost, stolen, or destroyed.
- The administration of intravenous and intramuscular opioids for the relief of
exacerbations of chronic pain is discouraged, except in special circumstances.
- Long-acting opioids should only be prescribed by health care providers familiar
with their indications, risks, and need for careful monitoring.
- When opioids are prescribed for treatment of chronic pain, the patient should be
counseled to store the medications securely and never to share with others.
Link to the guidelines:
https://www.ok.gov/health2/documents/UP_Oklahoma_Office_Based_Guidelines.pdf
Requirements with the force of law: Opioid Analgesic Quantity Limits
In November 2014, the Oklahoma Health Care Authority (OHCA), which administers the
state’s Medicaid program, implemented a quantity limit on coverage of short-acting opioid
prescription. Chronic opioid analgesic quantity limits apply to short-acting opioid therapies
greater than 10 days. This is triggered when a member receives a prescription greater than
10-day supply and the quantity is greater than four per day. For therapies determined to be
long-term (greater than 10-day supply), the maximum quantity that will be reimbursed is
four dosage units per day.

42
Link to OHCA’s opioid prescribing policy:
https://www.okhca.org/providers.aspx?id=11146
Oregon
Advisory Guidelines: Oregon Pain Guidance Pain Treatment Guidelines
In 2016, the Oregon Pain Guidance, a group of physicians, nurse practitioners, pharmacists,
and other health care providers, updated its guidance for physicians prescribing opioids to
treat pain. The updated guidelines endorsed and incorporated the CDC’s 12 recommended
guidelines and incorporated guidelines from the Washington state AMDG guidelines. The
guidelines include, among others, the following axioms:
Guidelines for acute pain:
- For most injuries and minor procedures (e.g., dental extraction, sports injuries),
prescribe no more than a three-day supply or 10 doses of a short-acting opioid.
- For more severe injuries (e.g., fractures), prescribe no more than a seven-day supply
of a short-acting opioid.
- Do not prescribe extended-release opioids for acute pain.
Guidelines for chronic conditions with acute pain flares
- Do not use opioids for acute flares of non-specific musculoskeletal pain, headaches,
or fibromyalgia.
- For acute flares of other chronic conditions (e.g., osteoarthritis, sickle cell anemia),
limit prescribing to a three-day supply of a short-acting opioid. In rare instances, up
to a seven-day supply may be appropriate.
- Check the state Prescription Drug Monitoring Program (PDMP) with any first opioid
prescription.
Guidelines for subacute (6–12 weeks) opioid use and transition to chronic opioid therapy
(>12 weeks)
- Don’t start long-term use of opioids without a visit devoted to evaluation of
suitability of long-term opioid use and discussion of all opioid risks and realistic
benefits.
- Use non-opioid alternatives (non-opioid analgesics, graded exercise, cognitive
behavioral therapy, mindfulness, and relaxation techniques).
- Unless opioid use has resulted in clinically meaningful improvement in pain and
function (at least 30% improvement documented with validated instruments),
discontinue prescribing.
- If opioid use results in clinically meaningful improvement in pain and function, use
best-practice screenings for opioid-related risks. Assess signs of prescription opioid-
use disorder by asking the patient or family members about history of substance
abuse.
- At every prescribing visit for opioids, the total opioid dose should be recorded using
an online calculator and measures of pain and function using brief validated
instruments.
Guidelines for chronic opioid use (>12 weeks)
- Do not prescribe chronic opioids for non-specific musculoskeletal pain, headache or
fibromyalgia.

43
- Do not combine opioids with benzodiazepines, muscle relaxants, or sedative
hypnotics.
- Repeat PDMP check and urine drug screen (UDS) periodically, based on risk.
- Avoid exceeding 90 mg/day MED. For patients with one or more risk factors (e.g.,
history of substance-use disorder, tobacco users, mental health disorders, cannabis-
use disorder), do not prescribe more than 50 mg/day MED.
- Non-pharmacological alternatives to opioids should be used and incented for most
chronic-pain conditions
- Periodically ask if the patient would like to consider trying a gradual opioid taper to
reduce dose or discontinue use.
- MED calculators (not all of which agree with each other) can help you determine the
dosage equivalency of one opioid when compared to another. It is wise to use MED
calculations very conservatively and use 25 to 50% of the calculated dose when
switching between opioids.
Link to the guidelines: http://professional.oregonpainguidance.org/wp-
content/uploads/sites/2/2014/04/OPG_Guidelines_2016.pdf
Advisory Guidelines: Oregon Opioid Prescribing Guidelines
In January 2017, the Oregon Opioid Prescribing Guidelines Task Force adopted the CDC
Guideline for Prescribing Opioids for Chronic Pain as the foundation for opioid prescribing
for Oregon. The Task Force also adopted several additional guidelines specific to the state,
including recommending that prescribers consult the state’s PDMP before prescribing
opioids.
Link to the guidelines:
https://www.oregon.gov/obnm/rules/opioidprescribingguidelines.pdf
In May 2017, the Oregon Legislature passed HB 2114, which requires health care
professional boards in the state to provide notice about the Oregon Opioid Prescribing
Guidelines to practitioners regulated by each board not later than January 1, 2018.
Link to the enacted bill:
https://olis.leg.state.or.us/liz/2017R1/Downloads/MeasureDocument/HB2114
Pennsylvania
Quasi-regulatory guidelines: Pennsylvania Guidelines on the Use of Opioids to Treat
Chronic Non-Cancer Pain
In July 2016, the Pennsylvania Board of Medicine voted to adopt guidelines published in
2014 for the prescribing of opioids for non-cancer-related pain.
Summary of guidelines:
- Before initiating chronic opioid therapy, conduct and document a history, including
documentation and verification of current medications, and a physical examination.
- Opioids should rarely be used as a sole treatment modality. Rather, opioids should
be considered as a treatment option within the context of multimodality therapy.

44
- When starting chronic opioid therapy, provider should discuss the risks and benefits
associated with treatment, so that the patient can make an informed decision.
- Initial treatment with opioids should be considered by clinicians and patients as a
therapeutic trial to determine whether chronic opioid therapy is appropriate.
- Patient’s opioid selection, initial dosing, and dose adjustments should be
individualized according to the patient’s health status, previous exposure to opioids,
response to treatment, and predicted or observed adverse events.
- Caution should be used in patients also taking benzodiazepines.
- Clinicians should carefully consider if doses above 100 mg/day of oral morphine or
its equivalent are indicated.
- Clinicians should reassess patients on chronic opioid therapy periodically and as
warranted by changing circumstances.
- Clinicians should carefully monitor patients for aberrant drug-related behaviors.
Link to the guidelines:
http://www.ddap.pa.gov/Document%20Library/Prescriber%20Guidelines%20on%20the
%20Use%20of%20Opioids%20to%20Treat%20Chronic%20Noncancer%20Pain.pdf
Quasi-regulatory guidelines: Pennsylvania Emergency Department (ED) Pain Treatment
Guidelines
In July 2016, the Pennsylvania Board of Medicine voted to adopt guidelines published in
2014 for the prescribing of opioids in EDs.
Summary of guidelines:
- Discharge prescriptions should be limited to the amount needed until follow-p and
typically should not exceed seven days.
- When selecting a medication for pain control the provider should consider non-
opioid medications as alternative or concurrent therapy.
- When opioids are indicated, the provider should choose the lowest potency opioid
necessary to relive the patient’s pain.
- An ED provider should only dispense the amount of opioid medication needed to
control the patient’s pain until they are able to acce3ss a pharmacy.
- ED providers should not prescribe long acting opioid agents, such as morphine or
methadone, unless coordinated with outpatient provider
- The patient should not receive opioid prescriptions for chronic or recurrent pan
from multiple providers.
- Upon development of a controlled substances database in Pennsylvania, ED
providers should access it as indicated.
- ED providers should not replace lost or stolen prescriptions for controlled
substances.
- ED providers should not fill prescriptions for patients who run out of pain
medications.
- Patients whose behavior raises the provider’s concern for addiction should be
encouraged to seek detoxification assistance.

45
Link to the guidelines:
http://www.dos.pa.gov/ProfessionalLicensing/BoardsCommissions/Documents/PA%20G
uidelines%20Emergency%20Department.pdf
Quasi-regulatory guidelines: Pennsylvania Guidelines on the Use of Opioids in Dental
Practice
In July 2016, the Pennsylvania Board of Dentistry voted to adopt guidelines published in
2014 for the prescribing of opioids in to relive dental pain.
Summary of guidelines:
- Before initiating pain therapy, conduct and document a medical history, including
documentation and verification of current medications, and a physical examination.
- Clinicians should administer non-steroidal anti-inflammatory drugs (NSAIDs), as
first-line analgesic therapy, unless contraindicated.
- Clinicians should consider the use of local anesthetic techniques.
- If an opioid is to be administered, the dose and duration of therapy should be for a
short period of time, and for conditions that typically are expected to be associated
with more severe pain.
- When opioids are indicated, the provider should choose the lowest potency opioid
necessary to relieve the patient’s pain.
- Long-acting opioids or extended-release preparations are contraindicated for the
treatment of acute procedural pain.
- The provider should assess the risk for drug-drug interactions before prescribing
analgesics.
- Opioids should not be administered in combination with benzodiazepines or other
centrally acting sedating medications.
- Care should be used when prescribing opioid combination product medications, to
ensure that the total dose of acetaminophen does not exceed 3,000 mg/day in
adults.
- Upon development of a controlled substances database by the state of Pennsylvania,
providers should access the database as indicated.
- Unless the clinician has training and experience in the use of opioids for the
treatment of non-cancer pain, long acting or extended-release opioids should not be
prescribed
- A patient whose behavior raises concern for the presence of a substance use
disorder should be encouraged to seek evaluation and possible treatment for this
condition through his or hers primary medical care provider.
- In general, it is not proper to prescribe opioids absent a face-to-face patient
evaluation.
- Providers should provide patients with instructions on safe disposal of unused
medications, including opioids.
Link to the guidelines:
https://www.pamedsoc.org/PAMED_Downloads/opioid_dental_prescribing_guidelines3_1
3_15.pdf?utm_source=PDF&utm_medium=web&utm_campaign=DentalGuidelines
Requirements with the force of law: 35 Pa. Cons. Stat. § 872.8 (2016)

46
In 2016, the Pennsylvania Assembly amended the state statute that requires prescribers to
check the state’s PDMP before prescribing controlled substances to also require
prescribers to query the system each time a patient is prescribed an opioid. The statute
reads as follows:
(a) System query — A prescriber shall query the system:
(1) for each patient the first time the patient is prescribed a controlled substance by
the prescriber for purposes of establishing a baseline and a thorough medical record;
(2) if a prescriber believes or has reason to believe, using sound clinical judgment, that
a patient may be abusing or diverting drugs; or
(3) each time a patient is prescribed an opioid drug product or benzodiazepine by the
prescriber.
(a.1) Query not required – If a patient has been admitted to a licensed health care
facility or is in observation status in a licensed health care facility, the prescriber does
not need to query the system after the initial query […] as long as the patient remains
admitted to the licensed health care facility or remains in observation status in a
licensed health care facility.
Requirements with the force of law: 35 Pa. Cons. Stat. § 52A03 (2016).
Pennsylvania also amended its laws regulating opioid prescribing to minors in 2016. The
amended statute prohibits prescriber from prescribing more than a seven-day supply of a
controlled substance containing an opioid to a minor.
Link to the enacted act language:
http://www.legis.state.pa.us/cfdocs/legis/li/uconsCheck.cfm?yr=2016&sessInd=0&act=1
25
Requirements with the force of law: 35 Pa. Cons. Stat. § 873.3 (2016).
As with minors, Pennsylvania also now prohibits prescribers from prescribing more than a
seven-day supply of opioids to persons receiving care in emergency departments.
Link to the enacted act language:
http://www.legis.state.pa.us/cfdocs/legis/li/uconsCheck.cfm?yr=2016&sessInd=0&act=1
22
Link to the language of the enacted statute:
http://www.legis.state.pa.us/CFDOCS/Legis/PN/Public/btCheck.cfm?txtType=HTM&sessY
r=2015&sessInd=0&billBody=S&billTyp=B&billNbr=1202&pn=2199
Rhode Island
Requirements with the force of law: R.I. Admin. Code 31-2-6:3.0 (2014)
In March 2015, the Rhode Island Department of Health amended the Rules and Regulations
for Pain management, Opioid Use, and the Registration of Distributors of Controlled
Substances to update the minimum requirements for prescribing opioids for pain
management. The updated requirements include:
- The practitioner shall obtain, evaluate and document the patient's health history
and physical examination in the health record prior to treating for chronic pain.
47
- Prescribing opioids for an acute injury shall be for a reasonable duration consistent
with community standards for the pain that is being treated
- If prescribing opioids, the practitioner will advise patients specifically about adverse
risks of taking alcohol or other psychoactive medications, tolerance, dependence,
addiction overdose or death if acute or long term use.
- The PMP shall be reviewed prior to starting any opioid.
- Chronic pain patients who receive opioid medication(s) shall have a written patient
treatment agreement which shall become part of their medical record.
- Periodic reviews, including an in-person visit, shall take place at intervals not to
exceed twelve months.
- For patients the practitioner is maintaining on continuous opioid therapy for pain
for six months or longer, the practitioner shall review information from the PMP at
least every twelve months.
- The consideration, and documentation of consideration, for consultation threshold
for adults is 120 milligrams morphine equivalent dose per day (MED) (oral). In the
event a practitioner prescribes a dosage amount that meets or exceeds the
consultation threshold of 120 milligrams MED (orally) per day, a consideration of
consultation with a Pain Medicine Physician is required, and must be documented in
the medical record.
- For patients on long-acting opioids, including methadone, practitioners shall
monitor use closely, especially upon initiation and following any dose increases.
- Patients who receive long-acting opioid medication(s) on a long term basis (ninety
(90) days or greater) shall have a written patient treatment agreement, which shall
become part of their medical record.
Link to the regulations:
http://sos.ri.gov/documents/archives/regdocs/released/pdf/DOH/8003.pdf
Requirements with the force of law: 1956 R.I. Gen. Laws Ann. § 21-28-3.20 (2016)
Since June 28, 2016, Rhode Island requires physicians to consult the state’s PMP prior to
prescribing opioids. The statute also limits the dosing of opioids for acute pain
management of outpatient adults to 30 MME daily for up to a 20 doses. The law provides as
follows:
(b) The prescription-monitoring program shall be reviewed prior to starting any
opioid. A prescribing practitioner […] shall review the prescription-monitoring
program prior to refilling or initiating opioid therapy with an intrathecal pump. For
patients the prescribing practitioner is maintaining on continuous opioid therapy for
pain for three (3) months or longer, the prescribing practitioner shall review
information from the prescription-monitoring program at least every three (3)
months. […]
(c) The director of health shall develop regulations for prescribing practitioners on
appropriate limits of opioid use in acute pain management. Initial prescriptions of
opioids for acute pain management of outpatient adults shall not exceed thirty (30)
morphine milligram equivalents (MMEs) total daily dose per day for a maximum total
of twenty (20) doses, and, for pediatric patients, the appropriate opioid dosage
maximum per the department of health.
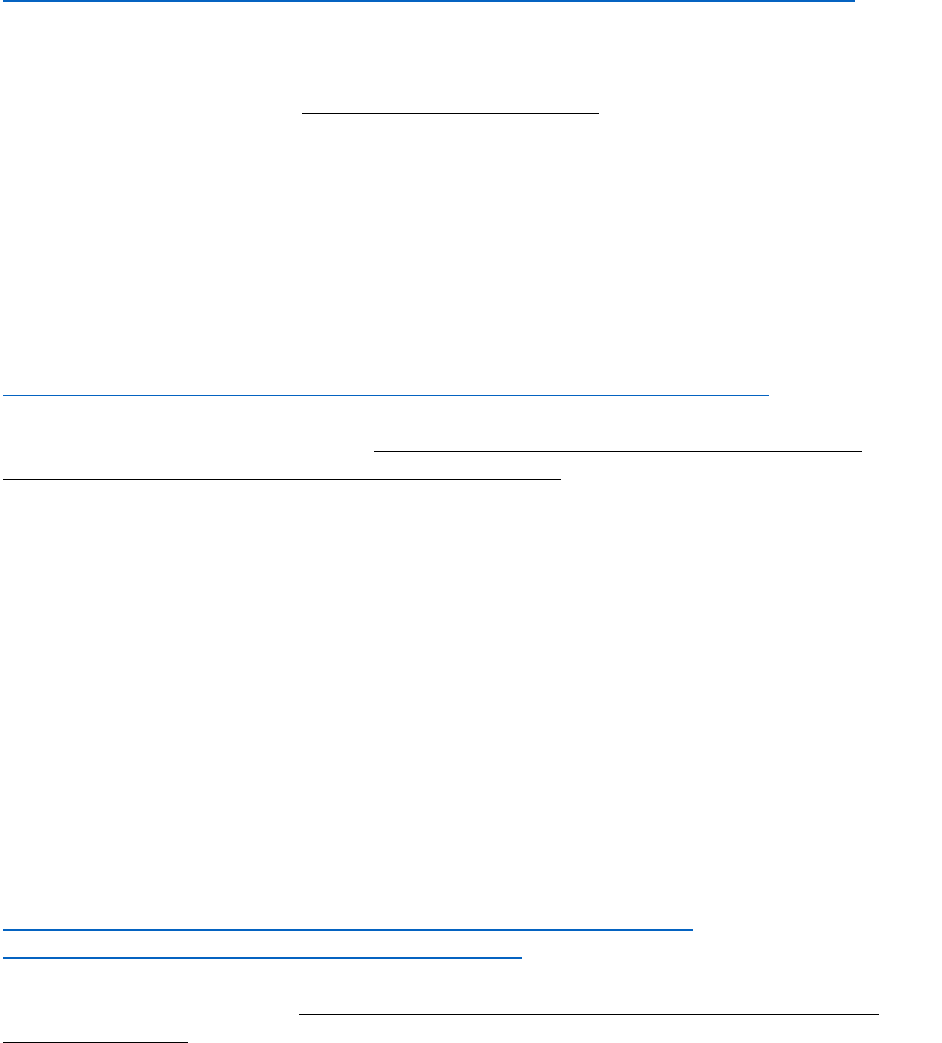
48
Link to the language of the approved bill:
http://webserver.rilin.state.ri.us/BillText/BillText16/SenateText16/S2823Aaa.pdf
South Carolina
Quasi-regulatory Guidelines: Pain Management Guidelines
In 2009, the South Carolina Board of Medical Examiners approved guidelines for the use of
controlled substances for treatment of pain. The guidelines include performing a patient
evaluation before prescribing opioids, obtaining informed consent from the patient for
opioid treatment, requiring a written agreement outlining patient responsibilities if the
patient is determined to be at high risk for medication abuse or to have a history of
substance abuse, conduct periodic review of the opioid treatment, and maintain a complete
medical record of the patient’s treatment.
Link to the guidelines:
http://www.llr.sc.gov/POL/medical/index.asp?file=Policies/MEPAIN.HTM
Requirements with the force of law: Required Use of the South Carolina Reporting &
Identification Prescription Tracking System (SCRIPTS)
Since April 1, 2016, the South Carolina Department of Health and Human Services
(SCDHHS) requires that providers verify Medicaid members' controlled substance
prescription history before issuing prescriptions for opioids. Failure to consult the South
Carolina Reporting and Identification Prescription Tracking System (SCRIPTS) database
may result in loss of Medicaid payments for the office visit during which the prescription
was given. For Medicaid members treated chronically with controlled substances, SCDHHS
will require that SCRIPTS be consulted at the initiation of therapy and at least every 90
days thereafter. The new policy exempts the following situations from the requirement:
- Issuance of less than a five-day supply of a controlled substance.
- Issuance of controlled substance prescription to a Medicaid member enrolled in
hospice.
- Instances where a controlled substance is administered by a licensed health care
provider.
Link to SCDHHS’s bulletin on the new policy:
https://www.scdhhs.gov/sites/default/files/SCRIPTS%20Bulletin-
%20%28v15%29%20w%20CLS%20signature.pdf
South Dakota
Quasi-regulatory guidelines: Model Policy for the Use of Controlled Substances for the
Treatment of Pain
In 2004, the South Dakota State Board of Medical and Osteopathic Examiners issued
guidelines on the prescribing of controlled substances for treating pain. The guidelines
include performing a patient evaluation before prescribing opioids, obtaining informed
consent from the patient for opioid treatment, requiring a written agreement outlining
patient responsibilities if the patient is determined to be at high risk for medication abuse
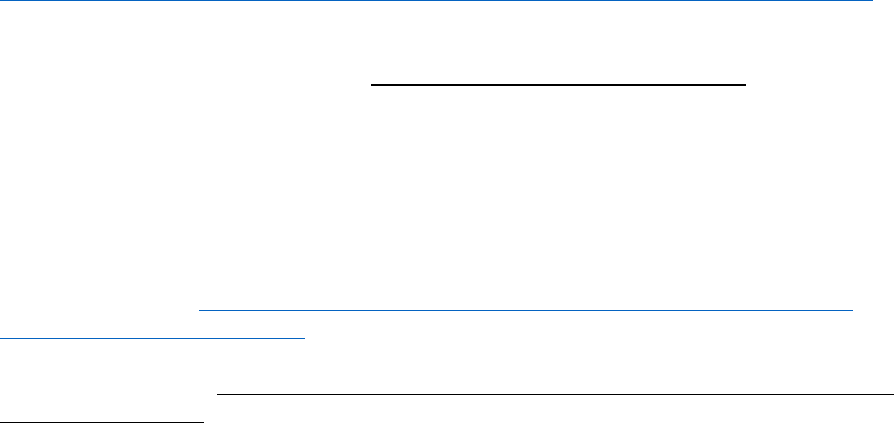
49
or to have a history of substance abuse, conduct periodic review of the opioid treatment,
and maintain a complete medical record of the patient’s treatment.
Link to the guidelines:
http://www.painpolicy.wisc.edu/sites/www.painpolicy.wisc.edu/files/SD_model.pdf
Tennessee
Requirements with the force of law: Tenn. Code Ann. § 53-11-308 (2013)
In 2013, the Tennessee Legislature amended its controlled substances statute to add
limitations to the prescribing of opioids. The amended statute prohibits dispensing of
prescriptions for any opioids or benzodiazepines in quantities greater than a 30-day
supply. The statute also requires prescribers of opioids, benzodiazepines, barbiturates, or
carisoprodol to patients who are in chronic, long-term drug therapy for 90 days or longer
to consider mandatory urine testing.
Link to the statute: http://law.justia.com/codes/tennessee/2014/title-53/chapter-
11/part-3/section-53-11-308
Advisory Guidelines: Clinical Practice Guidelines for Outpatient Management of Chronic
Non-Malignant Pain
In 2014, the Tennessee Department of Health issued guidelines for the prescribing of
opioids to treat chronic non-malignant pain. The guidelines include recommendations
regarding patient evaluation prior to initiating the opioid treatment and recommendations
as to the proper dosing of opioid that should be prescribed. Some of the guidelines include:
- A patient should be prescribed a maximum of four doses of a short-acting opioid
per day.
- Prescribers who are not pain medicine specialists shall not prescribe methadone
for a chronic pain condition.
- Prescribers shall not prescribe buprenorphine in the form of oral or sublingual
buprenorphine for chronic pain condition.
- Benzodiazepines should be generally avoided in combination with opioid therapy.
- When the opioid dose reaches 120mg MEDD and the benzodiazepines are being
used for mental health purposes, the provider shall refer to a mental health
professional to assess necessity of benzodiazepine medication.
- Buprenorphine/naloxone combinations shall be avoided for chronic pain.
- The initiation of opioids should be presented to the patient as a therapeutic trial.
- When initiating opioid therapy, the lowest dose of opioids should be given to an
opioid naïve patient and then titrated to effect.
- Informed consent for the use of opioids in treating pain must be obtained prior to
initiating treatment.
- Providers must continually monitor the patient for signs of abuse, misuse or
diversion.
- All chronic opioid therapy should be handled by a single provider or practice.
- Opioids should be used at the lowest effective dose. A provider should not use
more than one short-acting opiate concurrently.

50
- Patients on opioid doses of 120mg MEDD or greater should be referred to a pain
specialist for a consultation and/or management.
- Providers must continually monitor the patient for signs of abuse, misuse or
diversion.
- ED physicians should keep the specialist and the primary care provider informed
about changes in a patient’s condition and any emergent incidents or conditions.
- Opioids are to be discontinued when the risks, side effects, lack of efficacy or
presence of medication or aberrant behavior outweigh the benefits.
Link to the guidelines:
https://www.tn.gov/assets/entities/health/attachments/ChronicPainGuidelines.pdf
Requirements with the force of law: Tenn. Code Ann. § 53-10-310 (2016)
Since 2013, providers in Tennessee are required to check the state’s controlled substance
database or have a healthcare practitioner delegate check the database before prescribing
or dispensing a controlled substance if the healthcare practitioner is aware or reasonably
certain that a person is attempting to obtain a Schedule II-V controlled substance, which
includes, among other, opioids and benzodiazepines.
Texas
Requirements with the force of law: 22 Tex. Admin. Code § 170.3 (2007)
In 2007, the Texas Medical Board adopted regulations with regards to treating pain with
controlled substances. The guidelines set the appropriate standard of care in those
situations and have been amended twice, in 2014 and 2016. The guidelines include
performing a patient evaluation before prescribing opioids (including reviewing
prescription data and history related to the patient contained in the state’s prescription
drug monitoring program (PDMP)), obtaining informed consent from the patient for opioid
treatment, conduct periodic review of the opioid treatment, and maintain a complete
medical record of the patient’s treatment.
Link to the regulation:
https://texreg.sos.state.tx.us/public/readtac$ext.TacPage?sl=R&app=9&p_dir=&p_rloc=&p
_tloc=&p_ploc=&pg=1&p_tac=&ti=22&pt=9&ch=170&rl=3
Utah
Advisory Guidelines: Utah Clinical Guidelines on Prescribing Opioids for Treatment of Pain
In 2009, the Utah Department of Health adopted recommended guidelines for physicians
prescribing opioids for treating pain.
Summary of guidelines for Opioid Treatment for Acute Pain
- Opioid medications should only be used for treatment of acute pain when the
severity of the pain warrants that choice and after determining that other non-
opioid pain medications or therapies will not provide adequate pain relief.
- When opioid medications are prescribed, the number dispensed should be no more
than the number of doses needed based on the usual duration of pain..

51
- When opioid medications are prescribed for treatment of acute pain, the patient
should be counseled to store the medications securely, to not share with others, and
to dispose of medications properly when the pain has resolved.
- Long duration-of-action opioids should not be used for treatment of acute pain,
- Methadone is rarely if ever indicated for treatment of acute pain.
- The use of opioids should be reevaluated carefully, including assessing the potential
for abuse, if persistence of pain suggests the need to continue opioids.
Summary of guidelines for Opioid Treatment for Chronic Pain:
- A comprehensive evaluation should be performed before initiating opioid
treatment.
- Alternatives to opioid treatment should be before initiating opioid treatment.
- The provider should screen for risk of abuse or addiction before initiating
treatment.
- When opioids are to be used for treatment of chronic pain, a written treatment plan
should be established that includes measurable goals for reduction of pain and
improvement of function.
- The patient should be informed of the risks and benefits and any conditions for
continuation of opioid treatment.
- Opioid treatment for chronic pain should be initiated as a treatment trial, usually
using short-acting opioid medications.
- Regular visits with evaluation of progress against goals should be scheduled during
the period when the dose of opioids is being adjusted (titration period).
- Once a stable dose has been established (maintenance period), regular monitoring
should be conducted at face-to-face visits.
- Continuing opioid treatment after the treatment trial should be a deliberate decision
that considers the risks and benefits of chronic opioid treatment for that patient.
- An opioid treatment trial should be discontinued if the goals are not met and opioid
treatment should be discontinued at any point if adverse effects outweigh benefits.
- Clinicians treating patients with opioids for chronic pain should maintain records
documenting the evaluation of the patient, treatment plan, etc.
- Clinicians should consider consultation for patients with complex pain conditions,
patients with serious co-morbidities including mental illness, patients who have a
history or evidence of current drug addiction or abuse.
- Methadone should only be prescribed by clinicians who are familiar with its risks
and appropriate use, and who are prepared to conduct the necessary careful
monitoring.
Link to the guidelines:
http://www.health.utah.gov/prescription/pdf/guidelines/final.04.09opioidGuidlines.pdf
Requirements with the force of law: Utah Code Ann. §§ 58-37-6(7)(f)(iii) and 58-37f-
304(2) (2017)
In 2017, Utah enacted a law to limit the number of days for which an opioid may be
prescribed. Prescribers can prescribe up to a 7-day supply for an acute condition. If the
prescriber determines that a higher dose is needed in the case of prescriptions issued for a

52
surgery, the prescriber must not prescribe a dose exceeding a 30-day supply. The law
exempts pharmacists from verifying that a prescription is in compliance with these
requirements. The enacted law also requires prescribers to check the PDMP database for
information about the patient when prescribing more than a 3-day supply of opioids for the
first time, unless the prescription is for post-surgical treatment and is a 30-day or less
supply.
Link to the enacted legislation: https://le.utah.gov/~2017/bills/static/HB0050.html
Vermont
Requirements with the force of law: Vt. Stat. Ann. tit. 18, § 4289(d) (2014)
Since 2014, Vermont law requires health care providers to query the Vermont Prescription
Monitoring System (VPMS) with respect to an individual patient’s record in all the
following circumstances:
- At least annually for patients who are receiving ongoing treatment with an opioid or
controlled substance;
- When starting a patient on an opioid or controlled substance for non-palliative long-
term pain therapy of 90 days or more;
- The first time the provider prescribes an opioid or controlled substance written to
treat chronic pain; and
- Prior to writing a replacement prescription for an opioid or controlled substance.
In 2016, the Vermont Legislature amended the statute to direct the state’s Commissioner of
Health to adopt rules on prescribing opioids after consulting with the Controlled
Substances and Pain Management Advisory Council, which may include number and time
limits on pills prescribed.
For the enacted legislation, see
http://legislature.vermont.gov/assets/Documents/2016/Docs/ACTS/ACT173/ACT173%2
0As%20Enacted.pdf
Quasi-regulatory guidelines: Policy on the Use of Opioid Analgesics in the Treatment of
Chronic Pain
In 2014, the Vermont Board of Medical Practice updated its policy on the use of opioids for
treating chronic pain to incorporate the latest best practices and new developments in the
healthcare profession regarding the safe and effective use of controlled substances to treat
pain.
Summary of guidelines:
- For every patient, the initial work-up should include a systems review and relevant
physical examination, as well as laboratory investigations
- Assessment of the patient’s personal and family history of alcohol or drug abuse and
relative risk for medication misuse or abuse should be completed prior to a decision
as to whether to prescribe opioid analgesics
- The decision to initiate opioid therapy should be a shared decision between the
physician and the patient.
- If opioids are prescribed, the patient (and possibly family members) should be
counseled on safe ways to store and dispose of medications

53
- Safer alternative treatments should be considered before initiating opioid therapy
for chronic, nonmalignant pain.
- Opioid therapy should be presented to the patient as a therapeutic trial or test for a
defined period of time (usually no more than 90 days) and with evaluation points.
- When initiating opioid therapy, the lowest dose possible should be given to an
opioid naïve patient. It is generally suggested to begin opioid therapy with a short
acting opioid and consider rotating to a long-acting/extended release opioid only if
indicated.
- Physician should regularly review the patient’s progress, including any new
information about the etiology of the pain or the patient’s overall health and level of
function
- Periodic drug testing may be useful in monitoring adherence to the treatment plan,
as well as in detecting the use of non-prescribed drugs
Link to the guidelines:
http://healthvermont.gov/hc/med_board/documents/opioid_pain_treatment_policy.pdf
Advisory Guidelines: Opiate Prescribing Guidelines for Vermont Emergency Departments
In 2014, Vermont ED Directors issued a consensus statements outlining their
recommended guidelines for prescribing opioids in EDs. The guidelines include:
- Providers are encouraged to review the Vermont Prescription Monitoring System
(VPMS) prior to treating or prescribing opiates for patients with high risk features.
- Any patient receiving parenteral narcotics should be appropriately monitored with
inclusion of either pulse oxymetry or capnography.
- Patients presenting to the acute care setting requesting rapid escalation of
treatment for chronic pain or requesting parenteral administration of opiates
should be considered to be at high risk for injury or abuse.
- A urine drug screen may be considered prior to initiating treatment.
- Concurrent use of non-prescribed controlled or illegal substances is considered to
be a risk factor for overdose or abuse.
- Long-acting opiates including fentanyl patch, MS Contin, and OxyContin should
generally not be initiated by acute care providers.
- Acute care providers should only prescribe scheduled doses of long-acting opiates
as part of an established outpatient plan for chronic pain management.
- Due to low safety margin, drug interaction and risk of seizure, IV Demerol
(meperidine) for treatment of acute or chronic pain is discouraged.
- Acute care providers should not prescribe replacements for narcotics that have
been lost, stolen, or destroyed or continuation of treatment for patients who have
run out of narcotics early or while their usual provider is off duty.
- Providers should not provide replacement doses of Suboxone, Subutex or
methadone.
- Acute care providers should not initiate outpatient treatment for chronic pain using
long-acting opiate preparations
- Three days is the recommended maximum duration for treatment prescribed from
the acute care setting, depending on the condition and clinical judgment.

54
- All patients prescribed an opiate should be assessed for potential drug interactions
which could potentiate the respiratory depression effects.
Link to the guidelines:
http://legislature.vermont.gov/assets/Documents/2016/WorkGroups/Senate%20Health
%20and%20Welfare/Bills/S.201/W~Dr.%20Mark%20Depman~Opioid%20Presribing%2
0Guidelines~1-27-2016.pdf
Requirements with the force of law: Rule Governing the Prescribing of Opioids for Pain
Effective July 2017, Department of Health regulations limit the initial dose of opioids a
physician can prescribe to 7 days. The rule also incorporates previous prescribing
guidelines including:
- The prescriber shall conduct and document a medical and physical examination as
part of the patient’s medical record when prescribing opioids for chronic pain
- The prescriber shall evaluate and document benefits and relative risks, including the
risk for misuse, abuse, diversion, addiction, or overdose, for the individual patient of
the use of opioids prior to writing an opioid prescription for chronic pain.
- Prior to prescribing an opioid for the treatment of chronic pain, the prescriber shall
consider and document in the patient’s medical record:
• Non-opioid alternatives up to a maximum recommended by the FDA,
including non-pharmacological treatments;
• Trial use of the opioid;
• Any applicable requirements to query the Vermont Prescription Monitoring
System
• That the prescriber has asked the patient if he or she is currently, or has
recently been, dispensed methadone from an OTP or prescribed and taken
any other controlled substance.
- For patients prescribed opioids for 90 days or more for chronic pain, the prescriber
shall receive a signed Informed Consent from the patient.
- The prescriber shall consider referring a patient for a consultation with an
appropriate specialist when the patient is not meeting the goals of treatment despite
escalating doses of controlled substances or when the patient is at high risk for
substance misuse, abuse, diversion, addiction, or overdose as determined by the
patient’s history or a screening.
- Prior to prescribing a dose of opioids, or a combination of opioids, that exceeds 120
MED/day the prescriber of opioids to treat chronic pain shall document in the
patient’s medical record:
• A reevaluation of the effectiveness and safety of the patient's pain
management plan, including an assessment of the patient’s adherence to the
treatment regimen;
• The potential for the use of non-opioid and non-pharmacological alternatives
for treating pain;
• A functional status examination of the patient;

55
• A review of the patient’s agreement and informed consent, making any
necessary revisions, including pill counts and directly observed urine testing
to monitor adherence and possible use of other substances;
• An assessment of any co-morbid conditions affected by treatment with
opioids. This may be best conducted by a mental health or addictions
professional.
Link to the rule:
http://www.healthvermont.gov/sites/default/files/documents/2016/12/REG_opioids-
prescribing-for-pain.pdf
Requirements with the force of law: Vermont Prescription Monitoring System Rule
In August 215, the Vermont Department of Health issued a rule to implement the state’s
statute that requires physicians to query the VPMS before prescribing opioids for treating
pain.
Summary of situations when prescribers of opioids are required to query the VPMS:
- The first time the provider prescribes an opioid Schedule II, III, or IV controlled
substance written to treat pain when such a prescription exceeds 10 pills or the
equivalent;
- When starting a patient on a Schedule II, III, or IV controlled substance for
nonpalliative long-term pain therapy of 90 days or more;
- Prior to writing a replacement prescription for a Schedule II, III, or IV controlled
substance;
- At least annually for patients who are receiving ongoing treatment (treatment
without meaningful interruption) with an opioid Schedule II, III, or IV controlled
substance;
- The first time a provider prescribes a benzodiazepine;
- When a patient requests an opioid prescription or a renewal of an existing
prescription for pain from an Emergency Department or Urgent Care prescriber if
the prescriber intends to write a prescription for an opioid;
- With the exception of prescriptions written from an OTP, prior to prescribing
buprenorphine or a drug containing buprenorphine to a Vermont patient for the
first time and at regular intervals thereafter, and:
o At regular intervals thereafter, but no less than twice annually; and
o No fewer than two times annually thereafter; and
o Prior to writing a replacement prescription.
- In the case of an OTP, prior to prescribing buprenorphine, methadone, or a drug
containing buprenorphine to a Vermont patient for the first time, and:
o Annually thereafter; and
o Any other time that is clinically warranted.
- Prior to prescribing buprenorphine or a drug containing buprenorphine that
exceeds the dosage threshold approved by the Vermont Medicaid Drug Utilization
Review Board and published in its Preferred Drug List, prescribers must receive
prior approval from the Chief Medical Officer or Medical Director of the Department
of Vermont Health Access or designee

56
Link to the rule:
http://www.healthvermont.gov/sites/default/files/documents/2016/12/REG_vpms-
20170701.pdf
Virginia
Advisory Guidelines: Medical Society of Virginia’s Guidelines for the Use of Opioids in the
Management of Chronic Non-Cancer Pain
The Medical Society of Virginia adopted recommendations for physicians treating chronic,
non-cancer-related pain prescribing opioids. The guidelines include performing a patient
evaluation before prescribing opioids, obtaining informed consent from the patient for
opioid treatment, conduct periodic review of the opioid treatment, and maintain a
complete medical record of the patient’s treatment.
Link to the guidelines: http://www.druglibrary.net/schaffer/asap/virginia1.htm
Quasi-regulatory guidelines: Guidance on the Use of Opioid Analgesics in the Treatment of
Chronic Pain
In 2013, the Virginia Board of Medicine updated its guidelines on the use of opioid
analgesics to treat pain by adopting the Federation of State Medical Board’s new guidelines.
The guidelines include:
- The medical record should document the presence of one or more recognized
medical indications for prescribing an opioid analgesic and reflect an appropriately
detailed patient evaluation.
- Treatment of a patient who has a history of substance use disorder should, if
possible, involve consultation with an addiction specialist before opioid therapy is
initiated (and follow-up as needed).
- The state PDMP should be consulted to determine whether the patient is receiving
prescriptions from any other physicians.
- Safer alternative treatments should be considered before initiating opioid therapy
for chronic, non-malignant pain. Opioid therapy should be presented to the patient
as a therapeutic trial or test for a defined period of time (usually no more than 90
days) and with specified evaluation points.
- The physician should regularly review the patient’s progress. When possible,
information about the patient’s response to opioid therapy should be obtained from
family members or other close contacts, and the state PDMP.
- Periodic drug testing may be useful in monitoring adherence to the treatment plan,
as well as in detecting the use of non-prescribed drugs.
Link to the guidelines: http://www.dhp.virginia.gov/medicine/guidelines/85-24.pdf
Requirements with the force of law: Va. Code Ann. § 54.1-2522.1 (2015)
Since 2015, Virginia law requires prescribing physicians to request information from the
state’s PMP at the time of initiating a new course of treatment to a human patient that
includes the prescribing of opioids anticipated to last more than 14 consecutive days. This
information should be used for the purpose of determining what, if any, other covered

57
substances are currently prescribed to the patient. The following situations are exempted
from this requirement:
- The opioid is prescribed to a patient currently receiving hospice or palliative care;
- The opioid is prescribed to a patient as part of treatment for a surgical or invasive
procedure and such prescription is not refillable;
- The opioid is prescribed to a patient during an inpatient hospital admission or at
discharge;
- The opioid is prescribed to a patient in a nursing home or a patient in an assisted
living facility that uses a sole source pharmacy;
- The PMP is not operational or available due to a temporary technological or
electrical failure or natural disaster; or
- The prescriber is unable to access the PMP due to emergency or disaster and
documents such circumstances in the patient's medical record.
Effective July 2019, however, this requirement will be as follows:
Prescribers […] shall, at the time of initiating a new course of treatment to a human
patient that includes the prescribing of benzodiazepine or an opiate anticipated at the
onset of treatment to last more than 90 consecutive days, request information from the
[PMP] for the purpose of determining what, if any, other covered substances are
currently prescribed to the patient.
Link to the statute: http://law.lis.virginia.gov/vacode/title54.1/chapter25.2/section54.1-
2522.1/
Advisory Guidelines: Virginia Hospital Emergency Department Opioid Prescribing
Guidelines
In January 2016, the Virginia Hospital & Healthcare Association’s Board of Directors
produced recommendations for setting general standards of care on opioid prescribing in
Virginia’s EDs. The guidelines include:
- A provider outside the ED should provide all opioids to treat any patient’s chronic
pain.
- Administering intravenous or intramuscular opioids in the ED for the relief of acute
exacerbation of chronic pain is generally discouraged.
- Prescriptions for opioids from the ED should be written for the shortest duration
appropriate. This generally should be for no more than three days.
- Hospitals, in conjunction with ED personnel, should develop a process to screen for
substance misuse.
- When patients present with acute chronic pain, it is recommended that a summary
of the ED care is communicated to the primary opioid prescriber or primary care
provider.
- ED providers should not dispense prescriptions for controlled substances that were
lost, destroyed, stolen, or finished prematurely.
- ED providers, or their designees, are encouraged to consult Virginia’s PMP before
writing opioid prescriptions for acutely painful conditions.
- ED providers, in general, should not provide replacement doses of methadone or
buprenorphine for patients participating in an opioid treatment program.

58
- ED providers should not prescribe long‐acting or controlled release opioids, such as
oxycodone, fentanyl patches, or methadone.
- ED providers are strongly discouraged from prescribing buprenorphine products.
Link to the guidelines: http://vacep.org/wp-content/uploads/2016/06/VHHA-VACEP-
Opioid-Guidelines.pdf
Washington
Requirements with the force of law: Wash. Admin. Code § 246-919-850 (2011)
In 2011, the Washington Department of Health adopted a rule regulating the prescribing of
opioids for pain treatment. Some of the prescribing requirements include:
- For patients who are stable involving non-escalating daily doses of 40 mg MED/day
or less, periodic reviews shall take place annually.
- Mandatory consultation threshold for adults is 120 mg MED/day (oral).
- In the event a physician prescribes a dosage that meets or exceeds the consultation
threshold, a consultation with a pain management specialist is required.
- The physician shall document each mandatory consultation.
- Recommended that a practitioner not prescribe more than an average of MED of
120 mg without either the patient demonstrating improvement in function or
without first obtaining a consultation from a pain management expert.
Link to the regulation: http://apps.leg.wa.gov/documents/laws/wsr/2011/12/11-12-
025.htm
Advisory Guidelines: Washington Emergency Department Opioid Prescribing Guidelines
In 2012, the Washington State Medical Association, the Washington State Hospital
Association, the American College of Emergency Physicians, Washington Chapter, and the
Emergency Nurses Association, Washington State Council, adopted recommendations for
physicians prescribing opioids in EDs in Washington state. The guidelines include:
- One medical provider should provide all opioids to treat a patient’s chronic pain.
- The administration of intravenous and intramuscular opioids in the ED for the relief
of acute exacerbations of chronic pain is discouraged.
- Emergency medical providers should not provide replacement prescriptions for
controlled substances that were lost, destroyed or stolen.
- Emergency medical providers should not provide replacement doses of methadone
for patients in a methadone treatment program.
- Long-acting or controlled-release opioids (such as OxyContin®, fentanyl patches,
and methadone) should not be prescribed from the ED.
- EDs should perform screening, brief interventions and treatment referrals for
patients with suspected prescription opiate abuse problems.
- The administration of Demerol® (Meperidine) in the ED is discouraged.
- For exacerbations of chronic pain, the emergency medical provider should contact
the patient’s primary opioid prescriber or pharmacy. The emergency medical
provider should only prescribe enough pills to last until the office of the patient’s
primary opioid prescriber opens.

59
- Prescriptions for opioid pain medication from the ED for acute injuries, such as
fractured bones, in most cases should not exceed 30 pills.
- ED patients should be screened for substance abuse prior to prescribing opioid
medication for acute pain.
Link to the guidelines:
http://www.maineacep.org/uploadedFiles/Maine/edopioidabuseguidelinesfinal.pdf
Advisory Guidelines: Interagency Guidelines on Prescribing Opioids for Pain
In 2015, the Washington State Agency Medical Directors Group (AMDG) approved the third
and current version of its guidelines for prescribing opioids for treating pain. The
guidelines are divided into four phases of treatment.
Acute Phase (0-6 weeks):
- Check the state’s Prescription Monitoring Program (PMP) before prescribing.
- Don’t prescribe opioids for non-specific back pain, headaches, or fibromyalgia.
- Prescribe the lowest necessary dose for the shortest duration.
- Opioid use beyond the acute phase is rarely indicated.
Perioperative pain:
- Evaluate thoroughly preoperatively: check the PMP and assess risk for over-
sedation and difficult-o-control pain.
- Discharge with acetaminophen, NSAIDs, or very limited supply (2–3 days) of short-
acting opioids for some minor surgeries.
- For patients on chronic opioids, taper to preoperative doses or lower within 6
weeks following major surgery.
Subacute phase (6–12 weeks):
- Don’t continue opioids without clinically meaningful improvement in function
(CMIF) and pain.
- Screen for comorbid mental health conditions and risk for opioid misuse using
validated tools.
- Recheck the PMP and administer a baseline urine drug test (UDT) if planning to
prescribe opioids beyond 6 weeks.
Chronic phase (>12 weeks):
- Continue to prescribe opioids only if there is sustained CMIF and no serious adverse
events, risk factors, or contraindications.
- Repeat PMP check and UDT at frequency determined by the patient’s risk category.
- Prescribe in 7-day multiples to avoid ending supply on a weekend.
- Don’t exceed 120 mg/day MED without a pain management consultation.
Link to the guidelines:
http://www.agencymeddirectors.wa.gov/Files/2015AMDGOpioidGuideline.pdf
Link to the guidelines’ summary: http://www.agencymeddirectors.wa.gov/Files/FY16-
288SummaryAMDGOpioidGuideline_FINAL.pdf
West Virginia
Requirements with the force of law: W. Va. Code Ann. § 60a-9-5a (2014)

60
Since 2014, West Virginia law requires physicians to check the state PMP before
prescribing opioids. The statute provides:
Upon initially prescribing or dispensing any pain-relieving controlled substance for a
patient and at least annually thereafter should the prescriber or dispenser continue to
treat the patient with controlled substances, all persons with prescriptive or
dispensing authority […] shall access the West Virginia Controlled Substances
Monitoring Program database for information regarding specific patients for whom
they are providing pain-relieving controlled substances as part of a course of treatment
for chronic, nonmalignant pain but who are not suffering from a terminal illness. [...]
Link to the statute: http://www.legis.state.wv.us/WVCODE/Code.cfm?chap=60a&art=9#09
Pursuant to this statute, several professional boards have adopted regulations requiring
prescribers to check the state’s PMP before prescribing opioids:
Board of Dentistry: W. Va. Code R. §§ 5-10-3.2 – 5-10-3.6 (2014)
Board of Medicine: W. Va. Code R. §§ 11-10-3.2 – 11-10-3.5 (2014)
Board of Examiners for Registered Nurses: W. Va. Code R. §§ 19-14-3.2 – 19-14-3.6 (2014)
Board of Osteopathic Medicine: W. Va. Code R. §§ 24-7-3.2 – 24-7-3.5 (2014)
Advisory Guidelines: Guidance for Use and Prescribing of Opioids in Emergency
Departments
In November 2015, the West Virginia Hospital Association adopted guidance for the
prescribing of opioids in EDs across the state.
Summary of guidelines:
- One medical provider should provide all opioids to treat a patient’s chronic pain.
- A prescription for a controlled substance should not be given to a patient without a
government issued photo ID.
- The administration of intravenous and intramuscular opioids in the ED for the relief
of acute exacerbations of chronic pain is discouraged.
- Emergency medical providers should not provide replacement prescriptions for
controlled substances that were lost, destroyed or stolen.
- Emergency medical providers should not provide replacement doses of methadone
for patients in a methadone treatment program.
- Emergency medical providers should not provide replacement doses of methadone
for patients in a methadone program without consultation with the program.
- The ED will not prescribe or dispense suboxone.
- Long-acting or controlled-release opioids (such as OxyContin®, fentanyl patches,
and methadone) should not be prescribed from the ED.
- Prescriptions for opioids from the ED for acute injuries will cover the shortest
appropriate time. If the emergency provider does elect to provide pain medication
for chronic pain, it will be enough to cover until the next business day.
- Hospital ED providers should consult the West Virginia Controlled Substance
Automated Prescription program (CSAPP) before writing a controlled substance
prescription.
Link to the guidelines: http://www.wvha.org/getmedia/94a27c11-c3d5-4709-9c7c-
8e29378c58ee/Opioid-Guidelines-Toolkit.pdf.aspx

61
Requirements with the force of law: In October 2016, the Office of the Governor of West
Virginia announced that the state’s Department of Health and Human Resources will adopt
the guidelines on opioid prescribing issued by the CDC. The state intends to implement
these guidelines to reduce the opportunity for opioid overuse and abuse while preserving
access to necessary drugs.
For more information, see http://www.wvgazettemail.com/news-health/20161018/wv-
to-follow-cdc-guidelines-for-prescribing-opioids
Wisconsin
Quasi-regulatory guidelines: Wisconsin Medical Examining Board Opioid Prescribing
Guideline
In June 2016, the Wisconsin Medical Examining Board adopted guidelines to help providers
make informed decisions about acute and chronic pain treatment with the use of opioids.
The guidelines excluded patients who are in cancer treatment, palliative care, or end-of-life
care.
Summary of guidelines:
- In treating acute pain, if opioids are at all indicated, the lowest dose and fewest
number of opioid pills needed should be prescribed. In most cases, less than 3 days’
worth are necessary, and rarely more than 5 days’ worth.
- Opioids should not be prescribed unless there is a medical condition present which
would reasonably be expected to cause pain severe enough to require an opioid.
- Opioids should not necessarily be the first choice in treating acute or chronic pain.
- Don’t use opioids routinely for chronic pain. When opioids are used, combine them
with non-pharmacologic or non-opioid pharmacologic therapy.
- Patients should not receive opioid prescriptions from multiple physicians.
- Physicians should avoid prescribing controlled substances for patients who have
run out of previously prescribed medication or have had previous prescriptions lost
or stolen.
- Physicians should avoid using intravenous or intramuscular opioid injections for
patients with exacerbations of chronic non-cancer pain in the ED or urgent care
setting.
- Physicians are encouraged to review the patient’s history of controlled substance
prescriptions using the Wisconsin PDMP data to determine whether the patient is
receiving opioid dosages or dangerous combinations.
- Prescribing of opioids is not encouraged in patients concurrently taking
benzodiazepines or other respiratory depressants.
- Opioids should be prescribed in the lowest effective dose.
- If daily doses for chronic pain reach 50 morphine milligram equivalents (MMEs),
additional precautions should be implemented. Given that there is no evidence base
to support efficacy of doses over 90 MMEs, with dramatically increased risks, dosing
above this level is strongly discouraged.

62
- The use of methadone is not encouraged unless the practitioner has extensive
training or experience in its use.
- During initial opioid titration, practitioners should re-evaluate patients every 1-4
weeks.
- During chronic therapy, patients should be seen at least every 3 months, more
frequently if they demonstrate higher risk.
- Practitioners should consider prescribing naloxone for home use in case of overdose
for patients at higher risk.
Link to the guidelines:
http://dsps.wi.gov/Documents/Board%20Services/Other%20Resources/MEB/MEB_Guid
elines.pdf
Requirements with the force of law: Wis. Stat. Ann. § 961.385(cs) (2016)
Effective April 2017, Wisconsin law requires a practitioner to review a patient's records
under the state’s PMP before the practitioner issues an opioid prescription order for the
patient.
This requirement does not apply under the following circumstances:
- The patient is receiving hospice care.
- The prescription order is for a number of doses that is intended to last the patient 3
days or less and is not subject to refill.
- The monitored prescription drug is lawfully administered to the patient.
- Due to emergency, it is not possible for the practitioner to review the patient's
records under the PMP before the practitioner issues a prescription order for the
patient.
- The practitioner is unable to review the patient's records under the PMP because
the digital platform for the program is not operational or due to other technological
failure if the practitioner reports that failure to the board.
Link to the statute: https://docs.legis.wisconsin.gov/statutes/statutes/961/III/385
Wyoming
Quasi-regulatory guidelines: Wyoming Health Care Licensing Boards’ Uniform Policy for
the Use of Controlled Substances in the Treatment of Pain
In February 2009, the Wyoming Board of Medicine adopted the state’s licensing boards’
Uniform Policy on the use of controlled substance to treat pain. The guidelines include
performing a patient assessment before prescribing opioids, obtaining informed consent
from the patient for opioid treatment, requiring a written agreement outlining patient
responsibilities if the patient is determined to be at high risk for medication abuse or to
have a history of substance abuse, conduct periodic review of the opioid treatment, and
maintain a complete medical record of the patient’s treatment.
Link to the guidelines:
http://www.painpolicy.wisc.edu/sites/www.painpolicy.wisc.edu/files/WY_joint.pdf

63
This document was developed by and used by permission from:
Corey Davis, JD
The Network for Public Health Law
Southeastern Region Office & the National Health Law Program
