
PCA-1-24-01886-POE-QRG_06182024
Overview
On Sept. 1, 2024, the Texas Health and Human Services Commission (HHSC) will implement a new
contract for STAR+PLUS. This new contract will change where UnitedHealthcare provides STAR+PLUS
Medicaid coverage. The HHSC began telling members about service area changes and STAR+PLUS plan
changes on March 1, 2024.
The following commonly asked questions aim to help provide clarification on:
• STAR+PLUS Service Delivery Area (SDA) updates for UnitedHealthcare
• New Texas STAR+PLUS plan options
• STAR+PLUS plan picking process and time frame
Commonly asked questions
Why are STAR+PLUS plan members receiving letters?
In service areas where managed care organizations (MCOs) are entering or exiting the market, HHSC’s
Enrollment Broker, who helps members sign up for coverage, is sending letters to all STAR+PLUS plan
members, including UnitedHealthcare members, to advise them of the STAR+PLUS plan picking time frame
and new plan options.
What letter are STAR+PLUS plan members being sent?
STAR+PLUS members are receiving different letter types based on their plan type (e.g., Medicaid Only,
Dual Eligible and STAR+PLUS Waiver). The language is the same with a few exceptions:
1. Health Plan Exiting the Service Area: Letters inform STAR+PLUS members to choose a new health
plan or the state will assign one for them
2. Health Plan Staying in the Service Area: Letters inform STAR+PLUS members that they can either
choose a new health plan or take no action and stay in their current plan
3. Toll-free Number to Call to Change Health Plans: Members receiving STAR+PLUS Home and
Community-Based Services program (sometimes called “STAR+PLUS Waiver”) are instructed to call a
different toll-free number than other members
4. Value Added Services (VAS) Comparison Charts: The VAS comparison charts attached to the letters
vary based on the member’s plan type (e.g., Medicaid Only, Dual Eligible and STAR+PLUS Waiver)
Texas STAR+PLUS membership overview
UnitedHealthcare Community Plan of Texas
Commonly asked questions
PCA-1-24-01886-POE-QRG_06182024
The STAR+PLUS Home and Community-Based Services program (also referred to as STAR+PLUS Waiver)
provides services that help people live at home who would otherwise need to be in a nursing facility. HHSC
assesses a person’s need for this program when they apply for Medicaid.
When will plan changes start?
The letters will instruct STAR+PLUS members to choose a health plan by a specific date, for coverage that
begins on Sept. 1, 2024.
Based on state sign-up cut-off dates, coverage will also begin on Sept. 1, 2024, for STAR+PLUS members
who submit a health plan choice by a specific date. Health plan selections made after this date will start on
Oct. 1, 2024.
What service area changes will start Sept. 1, 2024?
• Exiting: UnitedHealthcare will no longer service this area and the member will need to select a new plan
or they will be auto-assigned to a plan if they do not make their own selection
• Entering: UnitedHealthcare will be a plan option for STAR+PLUS members in these service areas
• No change: UnitedHealthcare will remain a plan health option in these service areas. Members do not
need to act if they would like to stay with our plan.
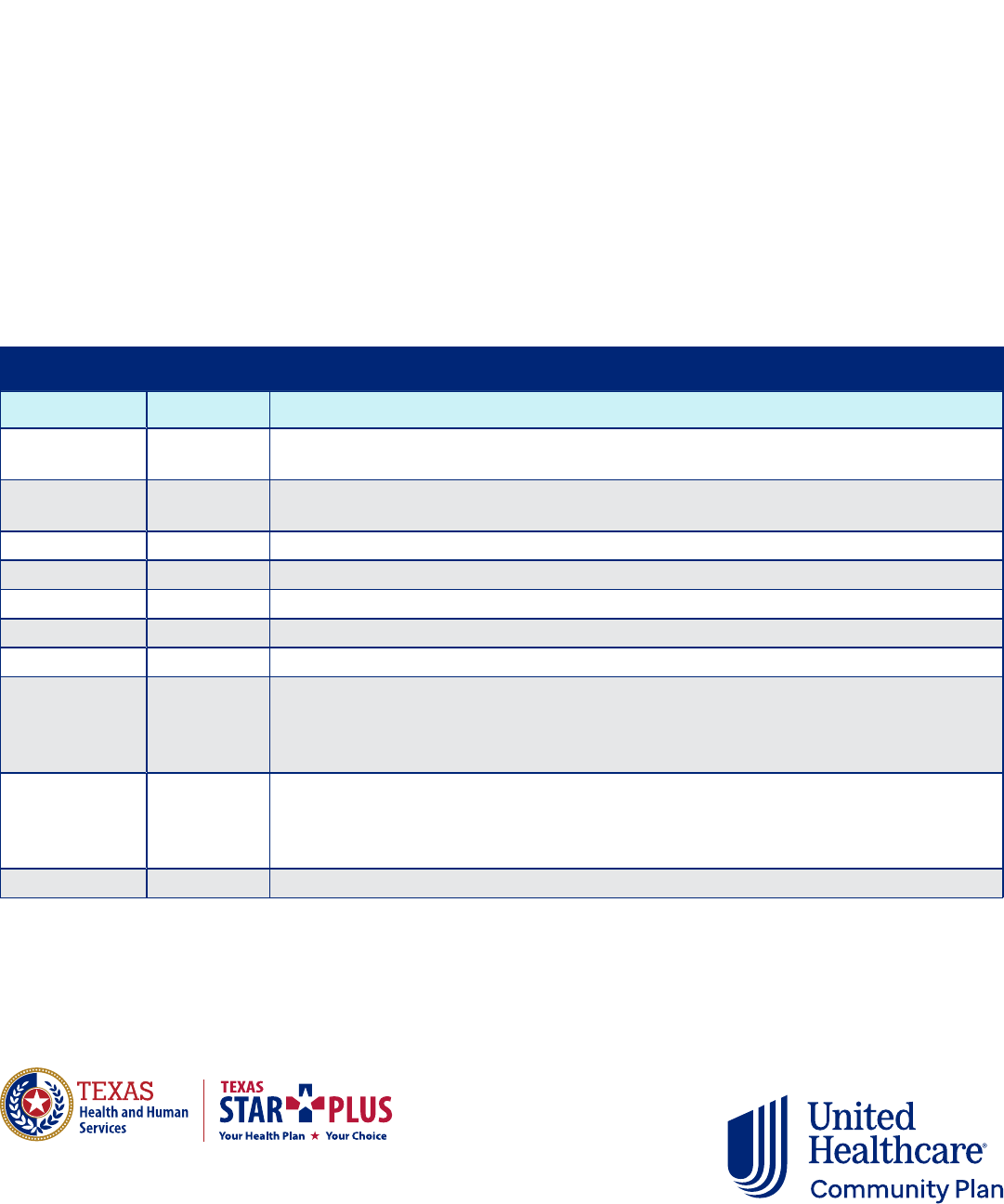
Service area changes
Area impact Service area Counties
Exiting Jefferson
Chambers, Hardin, Jasper, Jefferson, Liberty, Newton, Orange, Polk, San Jacinto,
Tyler, Walker
Exiting Nueces
Aransas, Bee, Brooks, Calhoun, Goliad, Jim Wells, Karnes, Kenedy, Kleberg, Live Oak,
Nueces, Refugio, San Patricio, Victoria
Entering Bexar Atascosa, Bandera, Bexar, Comal, Guadalupe, Kendall, Medina, Wilson
Entering Dallas Collin, Dallas, Ellis, Hunt, Kaufman, Navarro, Rockwall
Entering Hidalgo Cameron, Duval, Hidalgo, Jim Hogg, Maverick, McMullen, Starr, Webb, Willacy, Zapata
Entering Tarrant Denton, Hood, Johnson, Parker, Tarrant, Wise
No change Harris Austin, Brazoria, Fort Bend, Galveston, Harris, Matagorda, Montgomery, Waller, Wharton
No change
MRSA
Central
Bell, Blanco, Bosque, Brazos, Burleson, Colorado, Comanche, Coryell, DeWitt, Erath,
Falls, Freestone, Gillespie, Gonzales, Grimes, Hamilton, Hill, Jackson, Lampasas, Lavaca,
Leon, Limestone, Llano, Madison, McLennan, Milam, Mills, Robertson, San Saba,
Somervell, Washington
No change
MRSA
Northeast
Anderson, Angelina, Bowie, Camp, Cass, Cherokee, Cooke, Delta, Fannin, Franklin,
Grayson, Gregg, Harrison, Henderson, Hopkins, Houston, Lamar, Marion, Montague,
Morris, Nacogdoches, Panola, Rains, Red River, Rusk, Sabine, San Augustine, Shelby,
Smith, Titus, Trinity, Upshur, Van Zandt, Wood
No change Travis Bastrop, Burnet, Caldwell, Fayette, Hays, Lee, Travis, Williamson

PCA-1-24-01886-POE-QRG_06182024
Will all managed care STAR+PLUS members receive a letter?
No, only STAR+PLUS members who are experiencing a change in health plan options in their service area will
receive a letter.
Will STAR+PLUS members receive more mailings?
HHSC is planning to send out reminder letters in June 2024.
How do STAR+PLUS members select a plan?
The letter sent to STAR+PLUS members will have steps on the different ways they can select a plan. It will also
include value-added services comparison charts to help with plan comparisons.
STAR+PLUS members can select a plan:
• Online: Complete the form at yourtexasbenefits.com
• By mail: Complete the forms enclosed with the letter and return by mail to the address provided in the letter
• By fax: Complete the forms enclosed with the letter and fax to 855-671-6038
• By phone:
– Broker who helps members sign up for coverage (STAR+PLUS Waiver Plan): 877-782-6440
– Broker who helps members sign up for coverage (Non-Waiver Plan): 800-964-2777
• In person: Go to txmedicaidevents.com for dates and times of in-person options
Do all UnitedHealthcare members need to take action?
No, members in service areas where UnitedHealthcare will continue to provide coverage (Harris, MRSA Central,
MRSA Northeast and Travis service areas) do not need to return STAR+PLUS sign-up forms or take any other
action if they would like to continue services with us.
Members within Jefferson and Nueces service areas will need to take action to select a new plan, as we will no
longer service these areas. If they do not select a health plan, HHSC will assign one for them.
What happens if an STAR+PLUS member does not select a plan?
STAR+PLUS members whose health plans are exiting their service areas will need to select a new plan or they will
be auto-assigned to a plan.
Current UnitedHealthcare members will remain in UnitedHealthcare if they take no action, except for members
within Jefferson and Nueces service areas, as we will no longer service these areas. See the table above for
service area changes and county breakdown.
Why can’t the member continue with UnitedHealthcare or see UnitedHealthcare as an
option on the letter?
Members should know:
• They will remain with our health plan until the end of August 2024
• They will need to choose another plan
– If they do not choose a plan, they will be auto-assigned to a new plan
• We will coordinate with their new health plan to make the transition as seamless as possible by sharing
authorization and service plan history

PCA-1-24-01886-POE-QRG_06182024
© 2024 United HealthCare Services, Inc. All Rights Reserved.
How will existing prior authorizations be handled for members currently
receiving services?
Upon notice from a member, provider or exiting MCO of an existing prior authorization, UnitedHealthcare
will ensure members receive continued authorization of those services in the same amount, duration and
scope for the shortest period of the following:
• 6 months after the transition to a new MCO
• Until the end of the current authorization period
• Until UnitedHealthcare has evaluated and assessed the member and issued or not approved a new
prior authorization
The existing MCO should send all active authorizations to UnitedHealthcare so we can continue services.
During this time, a member assessment will be needed to find out if issuing new prior authorizations
are necessary.
Where can members find more about Medicaid plans and coverage?
• Online: uhccp.com/Texas
• In person: Go to txmedicaidevents.com for dates and times of in-person Medicaid events
Questions? We’re here to help.
If you have questions, go to UHCprovider.com/networkhelp, where you can chat with a live advocate
from 7 a.m.–7 p.m. CT. Or, go to UHCprovider.com/TXcommunityplan > Contact Us for ways to call or
email us.
